Abstract
Objective
Although e-cigarette popularity has increased substantially in recent years in the United States, it is unclear whether e-cigarette use has extended to immigrants in the United States. We characterized differences in ever and current use of e-cigarettes among non-U.S. citizens, naturalized U.S. citizens, and U.S. natives.
Methods
We used cross-sectional data from the 2014 National Health Interview Survey to measure the prevalence of e-cigarette ever and current use by immigration status, characterized as U.S. native, naturalized U.S. citizen, and non-U.S. citizen. We used multivariate logistic regression to examine the association between e-cigarette use and immigration status adjusting for demographic characteristics, socioeconomic status, and history of tobacco use. We also stratified the use of e-cigarettes by cigarette smoking status and analyzed the impact of length of residency and country of origin on e-cigarette use among immigrants.
Results
Naturalized U.S. citizens and non-U.S. citizens had a similar prevalence of e-cigarette use, which was significantly lower than the prevalence among U.S. natives. After adjusting for covariates, naturalized U.S. citizens had 38% lower odds and non-U.S. citizens had 54% lower odds of ever using e-cigarettes than U.S. natives. Non-U.S. citizens were less likely than U.S. natives to currently use e-cigarettes. Among both current smokers and nonsmokers of tobacco cigarettes, non-U.S. citizens were less likely than U.S. natives to indicate current e-cigarette use. U.S. immigrants with >5 years residency were more likely than U.S. immigrants with <5 years residency to try e-cigarettes.
Conclusion
Although non-U.S. citizens are less likely than U.S. natives to currently use e-cigarettes, e-cigarette use may increase with length of residency in the United States.
E-cigarettes, which are battery-powered devices that vaporize a liquid solution to deliver nicotine to users, have recently gained popularity in the United States.1 Total advertising expenditures on e-cigarettes nearly tripled from 2011 to 2012, and they have been marketed as healthier than regular cigarettes, socially acceptable in public environments, and helpful for smoking cessation.2–5 Awareness of e-cigarettes has also grown substantially; the proportion of U.S. adults reporting ever using e-cigarettes increased from 3.3% to 8.5% from 2010 to 2013.3,6–13 More than one in three current cigarette smokers has tried e-cigarettes,6 and annual e-cigarette sales more than doubled from 2012 to 2013, reaching $636.2 million.14
However, concerns have been raised about e--cigarette use. For example, until May 2016, they were not regulated by the U.S. Food and Drug Administration,15 and the safety of long-term e-cigarette use is unknown.1,4,16–22 Prior to May 2016, the lack of e-cigarette regulation in the United States contrasted with policies in Mexico and 25 other countries that have banned the sale of e-cigarettes, as well as 21 countries that restrict their sale or marketing.23 Use of e-cigarettes among adolescents may also be increasing in the United States.24–33 A 2016 article showed that 11.6% of high school students had used e-cigarettes within the previous month in Connecticut.34 Although e-cigarettes do not contain tobacco, they can be a potent nicotine delivery device and, thus, have the potential to be a gateway to smoking by creating a nicotine addiction. A 2015 study in California showed that high school students may be more likely to initiate tobacco use after experimental use of e-cigarettes.31 Using National Youth Tobacco Survey data, Cardenas et al. found that adolescents who ever used e-cigarettes were twice as likely as nonusers to report trying cigarettes within the previous year.35
Several studies have examined tobacco use in immigrant populations. U.S. immigrants are substantially less likely than U.S. natives to use tobacco, although differences between these two populations vary by sex and country of origin.36–43 For example, Acevedo-Garcia et al. reported that immigrants had 40% lower odds of smoking daily compared with U.S. natives.37 The likelihood of smoking among U.S. immigrants also increases with acculturation measures, such as length of U.S. residency and language.43–46 One study showed that the odds of smoking were 39% higher for immigrants with $15 years of U.S. residency than for those with <10 years of U.S. residency.46
Research on e-cigarette use among immigrants is limited. A study published in 2016 that investigated e-cigarette use by citizenship status among 1,052 adolescents in California found that adolescents who were non-U.S. citizens were substantially less likely than adolescents who were U.S. natives to ever use an e-cigarette in their lifetime, adjusting for confounding factors.47 To our knowledge, no study has examined e-cigarette use by immigrant adults; thus, it is unclear whether data on tobacco use among immigrant adults extend to e-cigarette use. We used nationally representative data to characterize differences in both current and ever use of e-cigarettes among non-U.S. citizens, naturalized U.S. citizens, and U.S. natives. We also compared the likelihood of e-cigarette use by immigration status and tobacco smoking status.
METHODS
Data and sample
We used cross-sectional data from the 2014 National Health Interview Survey (NHIS) to measure the prevalence of e-cigarette use by immigration status.48 We used data from 2014 because it was the first survey year in which the NHIS asked questions about e-cigarette use. The NHIS is an ongoing, nationally representative annual in-person survey of the U.S. civilian, noninstitutionalized population, maintained by the National Center for Health Statistics, Centers for Disease Control and Prevention. The dataset originally consisted of 36,697 respondents aged ≥18 years. After we excluded 2,305 (6.3%) observations with missing values, our final analytical sample size was 34,392.
Measures
Our two outcomes of interest were self-reported prevalence of (1) ever using and (2) currently using e-cigarettes. Respondents were asked, “Have you ever used an e-cigarette, even one time?” We categorized those who answered “yes” to this question as e-cigarette ever users. The NHIS followed up with this question by asking, “Do you now use e-cigarettes?” among respondents who reported having used e-cigarettes at least once. Possible answers included “every day,” “some days,” and “not at all.” Those reporting use as “every day” or “some days” were categorized as current e-cigarette users.
To create our primary independent variable of interest, immigration status, we used place of birth and current citizenship status to categorize respondents as U.S. native, naturalized U.S. citizen, or non-U.S. citizen. We defined U.S. natives as people born in the United States, naturalized U.S. citizens as those who were not born in the United States but had citizenship, and non-U.S. citizens as those who were neither born in the United States nor had U.S. citizenship.
We included demographic and socioeconomic variables for the multivariate analyses, including age (18–39, 40–59, and ≥60 years), sex, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, and non-Hispanic other [e.g., Asian, American Indian/Alaska Native]), educational attainment (<high school, high school, and ≥some college), marital status (married vs. unmarried), and poverty status (family income <100% of the federal poverty level [FPL] vs. ≥100% FPL). We included traditional cigarette smoking status as a covariate because e-cigarette use may substitute for tobacco use. We defined respondents who smoked <100 cigarettes in their lifetime as nonsmokers and respondents who smoked ≥100 cigarettes in their lifetime as current or former smokers, depending on if they reported regularly using tobacco products. These control variables are consistent with previous studies examining cigarette use.37,49 Finally, for both naturalized U.S. citizens and non-U.S. citizens, we included their length of residency in years in the United States, categorized as 0–4 or ≥5 years. We adapted this categorization from previous tobacco studies using length of residency for immigrants.45,50
Statistical analyses
We performed univariate analyses to characterize the distribution of all variables of interest and covariates, stratified by immigration status. We used Pearson's c2 test to measure the significance of disparities in prevalence of e-cigarette use (ever use and current use) by immigration status. We then used multivariate logistic regression models to examine the associations between types of e-cigarette use and immigration status. Afterward, we stratified these associations by current cigarette smokers, former smokers, and nonsmokers. We also examined length of U.S. residency and country of origin among naturalized U.S. citizens and non-U.S. citizens as potential confounding factors in e-cigarette use. We used Stata® version 13.0 to adjust for the complex survey design of the NHIS in all analyses using survey weights.51 Percentages were weighted using the survey weights provided by the NHIS.
RESULTS
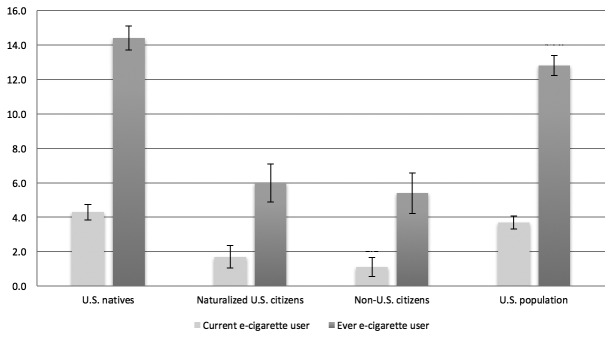
Of the 34,392 respondents in our sample, 28,094 (81.7%) were U.S. natives, 3,212 (9.3%) were naturalized U.S. citizens, and 3,086 (9.0%) were non-U.S. citizens. More than half of non-U.S. citizens (53.5%), 38.4% of U.S. natives, and 27.1% of naturalized U.S. citizens were aged 18–39 years. Nearly two-thirds of non-U.S. citizens were Hispanic. Non-U.S. citizens were more likely than U.S. natives and naturalized U.S. citizens to have less than a high school education and to live in poverty. However, U.S. natives and naturalized U.S. citizens had similar socioeconomic status. Both naturalized U.S. citizens and non-U.S. citizens were substantially less likely than U.S. natives to be either current or former smokers. Among U.S. immigrants, 18.1% of non-U.S. citizens and 2.0% of naturalized U.S. citizens had <5 years of U.S. residency (Table 1). Among the 34,392 respondents, 4,292 (12.8%) indicated using e-cigarettes at least once and 1,231 (3.7%) indicated currently using them. Naturalized U.S. citizens and non-U.S. citizens had a similar prevalence of ever or currently using e-cigarettes, and both prevalences were substantially lower than that of U.S. natives (Figure).
Table 1.
Weighted percentage distribution of characteristics for adult respondents, by immigration status,a National Health Interview Survey, 2014b
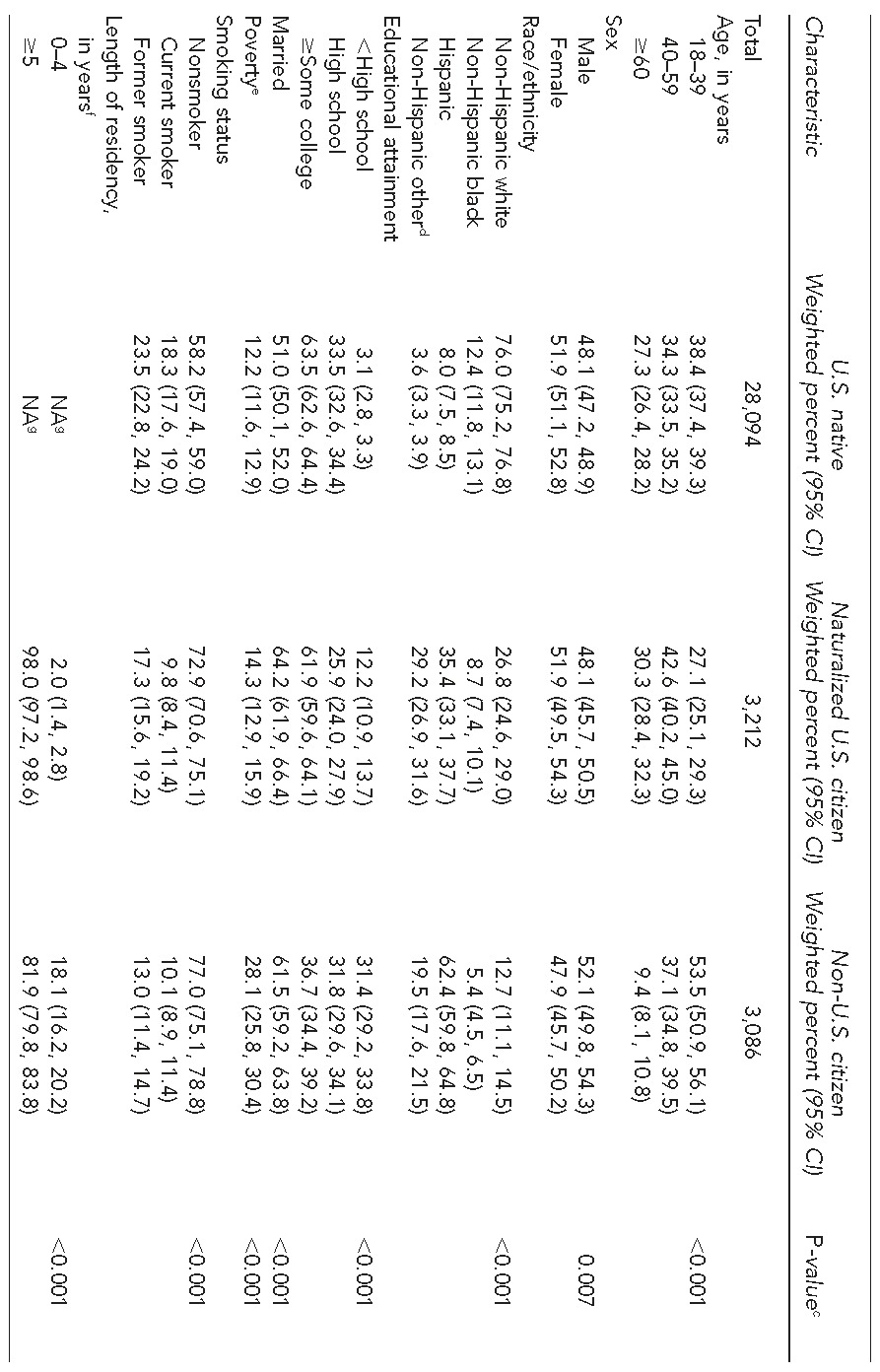
Based on 34,392 respondents
Data source: Centers for Disease Control and Prevention (US). National Health Interview Survey 2014 [cited 2016 Apr 8]. Available from: http://www.cdc.gov/nchs/nhis/nhis_2014_data_release.htm
cPearson's c2 test was used to measure differences by immigrant status.
dNon-Hispanic other included Asian, American Indian/Alaska Native, and other races/ethnicities.
ePoverty was defined as family income, 100% of the federal poverty level.
fA total of 32 immigrants did not report their length of stay.
gLength of residency in the United States was only defined for immigrants in our data.
CI = confidence interval
NA = not applicable
Figure.
Weighted percentage of ever and current use of e-cigarettes, by immigration status,a National Health Interview Survey, 2014b
aBased on 34,492 respondents. Estimates are weighted and adjusted for complex survey design of the National Health Interview Survey. Error bars indicate 95% confidence intervals.
bData source: Centers for Disease Control and Prevention (US). National Health Interview Survey 2014 [cited 2016 Apr 8]. Available from: http://www.cdc.gov/nchs/nhis/nhis_2014_data_release.htm
In the multivariate logistic regression analysis, after controlling for demographic characteristics, socioeconomic status, and cigarette smoking status, naturalized U.S. citizens (adjusted odds ratio [AOR] = 0.62, 95% confidence interval [CI] 0.46, 0.82) and non-U.S. citizens (AOR=0.46, 95% CI 0.34, 0.63) had lower odds than U.S. natives of ever using e-cigarettes. For current e-cigarette use, differences between naturalized U.S. citizens and U.S. natives were not significant. However, non-U.S. citizens had lower odds of current e-cigarette use than U.S. natives (AOR=0.44, 95% CI 0.24, 0.82). Additionally, respondents who were older, non-Hispanic black, Hispanic, and married had a lower likelihood of ever using e-cigarettes, whereas respondents with a higher education and a history of tobacco use had a higher likelihood of ever using e-cigarettes. Results were similar for current e-cigarette use except that the AOR for Hispanic was not significant (Table 2). When we defined the age groups as 18–25, 26–35, 36–45, 46–59, and ≥60 years, the results did not change significantly.
Table 2.
Multivariate logistic regression analysis of the association between e-cigarette use and immigration status,a by characteristics, National Health Interview Survey, 2014b
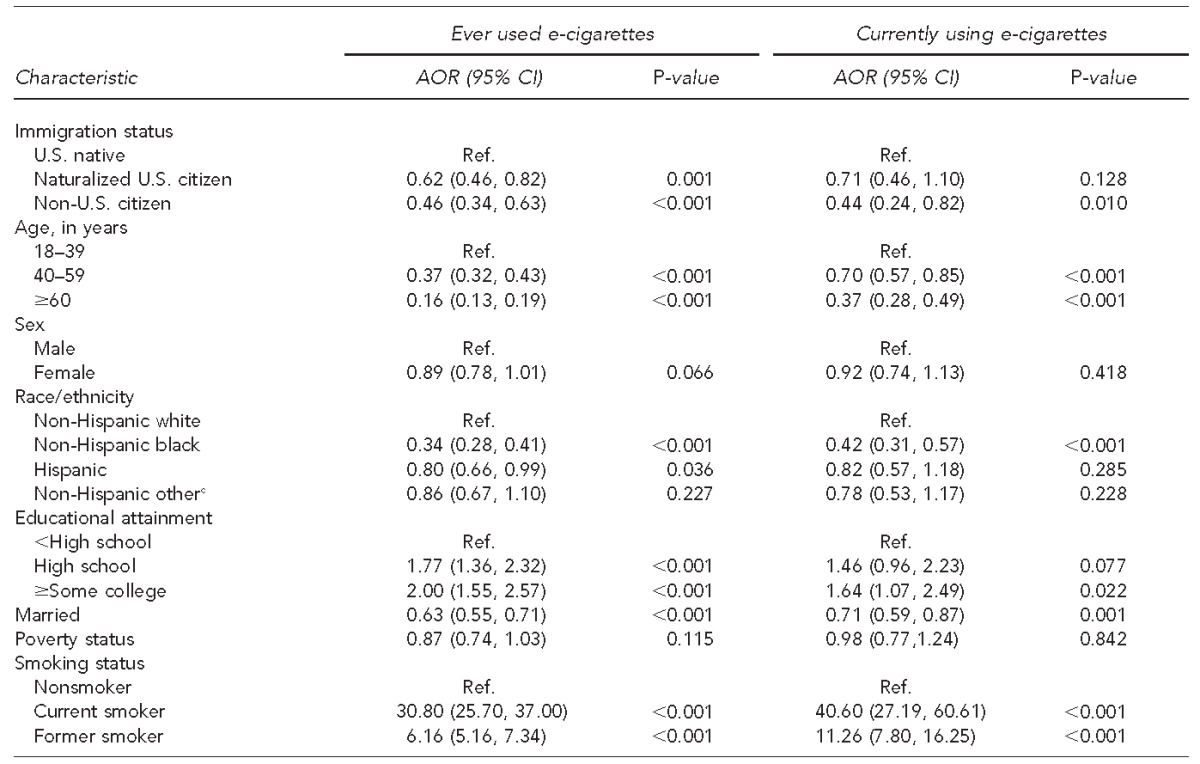
Based on 34,392 respondents; adjusted for age (18–39, 40–59, and $60 years), sex, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, and non-Hispanic other [e.g., Asian, American Indian/Alaska Native, other races/ethnicities]), educational attainment (<high school, high school, and ≥some college), marital status (married vs. unmarried), and poverty status (family income <100% federal poverty line [FPL] vs. ≥100% FPL), and smoking history (nonsmoker, current smoker, and former smoker).
Data source: Centers for Disease Control and Prevention (US). National Health Interview Survey 2014 [cited 2016 Apr 8]. Available from: http://www.cdc.gov/nchs/nhis/nhis_2014_data_release.htm
cNon-Hispanic other included Asian, American Indian/Alaska Native, and other races/ethnicities.
AOR = adjusted odds ratio
CI = confidence interval
Ref. = reference group
Among the 6,082 current cigarette smokers, non-U.S. citizens were less likely than U.S. natives to ever or currently use e-cigarettes. Non-U.S. citizens who were former smokers also had lower adjusted odds of ever using e-cigarettes than U.S. natives (AOR=0.56, 95% CI 0.32, 0.97). Among the 20,497 nonsmokers, naturalized U.S. citizens had lower adjusted odds of ever using e-cigarettes than U.S. natives (AOR=0.46, 95% CI 0.27, 0.79). Non-U.S. citizens who never smoked were also significantly less likely than U.S. natives who never smoked to currently use e-cigarettes (AOR=0.09, 95% CI 0.02, 0.53) (Table 3).
Table 3.
Multivariate logistic regression showing adjusted odds ratios of e-cigarette use by immigration status among adult respondents, stratified by smoking status,a National Health Interview Survey, 2014b
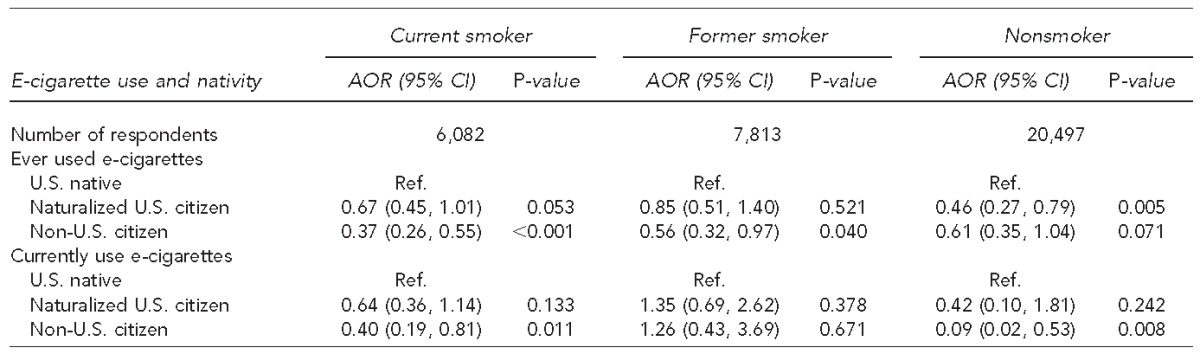
Based on 34,392 respondents. Covariates included age (18–39, 40–59, and $60 years), sex, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, and non-Hispanic other [e.g., Asian, American Indian/Alaska Native, other races/ethnicities]), educational attainment (<high school, high school, and ≥some college), marital status (married vs. unmarried), and poverty status (family income <100% federal poverty line [FPL] vs. ≥100% FPL), and smoking history (nonsmoker, current smoker, and former smoker).
Centers for Disease Control and Prevention (US). National Health Interview Survey 2014 [cited 2016 Apr 8]. Available from: http://www.cdc.gov/nchs/nhis/nhis_2014_data_release.htm
AOR = adjusted odds ratio
CI = confidence interval
Ref. = reference group
In other analyses, we adjusted for length of U.S. residency among naturalized U.S. citizens and non-U.S. citizens. Immigrants with ≥5 years of U.S. residency were more likely than immigrants with <5 years of U.S. residency to ever use e-cigarettes (AOR=1.98, 95% CI 1.20, 3.28), but length of U.S. residency was not significant for current e-cigarette use. When we performed sensitivity analyses using alternative categorizations of length of U.S. residency (i.e., 0–4, 5–9, ≥10 years), the results were similar. Immigrants from Mexico, Central America, or the Caribbean Islands were less likely than U.S. natives to ever (AOR=0.54, 95% CI 0.37, 0.78) or currently (AOR=0.37, 95% CI 0.19, 0.75) use e-cigarettes.
DISCUSSION
Previous research suggests that U.S. immigrants are less likely than U.S. natives to use tobacco.36–43 A 2015 study in California showed that adolescents who were non-U.S. citizens were unlikely to ever use e-cigarettes.47 However, to our knowledge, no research has examined whether these findings extend to the use of e-cigarettes by U.S. immigrant adults. Our univariate results suggest that naturalized U.S. citizens and non-U.S. citizens are more than 60% less likely than U.S. natives to ever use e-cigarettes. Relative to U.S. natives, we found that non-U.S. citizens had less than half the adjusted odds of ever or currently using e-cigarettes. Among current or former cigarette smokers, non-U.S. citizens were also significantly less likely than U.S. native to have ever used e-cigarettes.
The reasons for our findings on the lower rate of e-cigarette use among U.S. immigrants compared with U.S. natives are unclear. Previous research suggests that immigrant families tend to stigmatize substance use (e.g., smoking and alcohol).52,53 This finding was reflected in a study by Osypuk and Acevedo-Garcia that examined attitudes toward tobacco-control policies by immigrant communities in the United States and found that immigrants were twice as likely as U.S. natives to support smoke-free policies in public environments.54 This negative attitude toward smoking among immigrants may extend to e-cigarettes. Immigrants from Mexico or the 46 other countries that have banned or placed restrictions on e-cigarette sales and marketing may also be less likely than U.S. natives to initiate e-cigarette use in the United States, which is supported by our findings on country of origin.23
Geographic location in the United States may also partially explain our findings. For example, one study found that e-cigarette retailers were less likely to locate near residential areas with high proportions of racial/ethnic minority groups than in areas with smaller proportions of minority populations, including Hispanic communities. This locational decision by e-cigarette retailers may limit access to e-cigarettes among immigrant populations. It is also unclear if e-cigarette prices are higher in immigrant communities when there are fewer retailers. Unlike tobacco smokers, consumers of e-cigarettes have been found to be sensitive to e-cigarette pricing.55
Few studies have reported national estimates of e-cigarette use among adults, but evidence suggests that e-cigarette use is on the rise.6,8 For example, the percentage of adults in the United States who had used e-cigarettes increased from 3.4% in 20108 to 8.5% in 2013.6 Using 2014 NHIS data, we found that one in eight adults in the United States has now tried an e-cigarette at least once, and nearly 4.0% are current e-cigarette users.48 As noted previously, despite concerns about the safety of e-cigarettes and whether or not they serve as a gateway to tobacco use, use of e-cigarettes has continued to grow.16–18,32,57,58 In January 2014, more than 450 e-cigarette brands offered nearly 8,000 unique flavors.59 Much e-cigarette marketing has focused on them being healthier than tobacco use and socially acceptable in public environments.2–5 These messages may resonate with segments of the population that are usually not likely to smoke tobacco, such as those who are highly educated. Interestingly, our multivariate regression results showed that college education was associated with 64% higher adjusted odds of current e-cigarette use—and twice the odds of ever using e-cigarettes—compared with less than a high school education. This finding contrasts with previous research that showed a strong negative association between college education and tobacco smoking.60 Further research is needed to explore whether U.S. immigrants, particularly non-U.S. citizens, are more aware of the health concerns of e-cigarette use or less receptive to the marketing used by e-cigarette producers than U.S. natives.
One reason for e-cigarettes' popularity may be the perception that they can aid with tobacco cessation.9,12 A study by Schmidt et al. documented that the two dominant reasons for initiating e-cigarette use among adults were to try something new and to try to quit or reduce tobacco use.12 Our multivariate regression results showed that current and former smokers were more likely than nonsmokers to currently use e-cigarettes. Although smokers may turn to e-cigarettes for help with smoking cessation, King et al. found that exposure to e-cigarette cues may increase the -probability of relapse into smoking among those who have successfully quit smoking.61
However, e-cigarettes may also serve as a gateway to future tobacco use.59 For example, a 2013–2014 study of high school students in Hawaii found that willingness to smoke tobacco was higher among the 18% of students using e-cigarettes than among nonusers.60 A recent national longitudinal study using data from 2012–2014 showed that e-cigarette users at baseline were about eight times more likely than nonusers of e-cigarettes to start smoking tobacco cigarettes within one year.24 A study of e-cigarette advertising found that 6% of nonsmokers were receptive to trying e-cigarettes after viewing the advertisement.63 Our data showed that 3.3% of all NHIS respondents had tried e-cigarettes despite never having used tobacco. However, we also found that nonsmoking non-U.S. citizens were less likely than U.S. natives to initiate e-cigarette use.
Numerous studies have suggested that acculturation may lead to poor health outcomes over time among immigrants.43–46 Our results show that non-U.S. citizens had lower odds than U.S. natives of ever or currently using e-cigarettes after adjusting for confounding factors. However, it seems likely that acculturation will decrease these differences over time. In fact, our multivariate regression analyses showed that the differences in the likelihood of e-cigarette use between naturalized U.S. citizens and U.S. natives were smaller or not significant compared with the differences between non-U.S. citizens and U.S. natives. We also found that naturalized U.S. citizens and non-U.S. citizens living in the United States ≥5 years were twice as likely to try e-cigarettes as those with <5 years of U.S. residency. Thus, we expect e-cigarette use to rise among U.S. immigrants who reside for a longer time in the United States, and the use of e-cigarettes is likely to be substantially higher for the U.S. native-born children of U.S. immigrants compared with first-generation U.S. immigrants.
Strength and limitations
An advantage of our estimates of e-cigarette use compared with previous studies is that the NHIS is an in-person survey, whereas previous studies used Internet-based surveys resulting in potential selection bias. However, this study had several limitations. First, the NHIS did not provide detailed information on e-cigarette use, such as number of cartridge refills per day and reasons for initiating use. Thus, we were unable to examine differences in these characteristics by immigration status. Second, we could not determine temporality of tobacco smoking and e-cigarette use because the NHIS dataset is cross-sectional. Without this information, we were not able to measure the effect of e-cigarette use on subsequently quitting smoking or reducing the use of tobacco cigarettes. In addition, data on e-cigarette use are self-reported and, thus, subject to recall bias. Because the NHIS was implemented only in English and Spanish, U.S. immigrants who could not speak either language were not interviewed. Those with only limited language proficiency might also have chosen not to participate in the survey, which may have led to selection bias. Finally, because of a lack of data, we could not relate differences in U.S. immigrant use of e-cigarettes to geographical location or pricing.
CONCLUSION
Our findings suggest that differences exist in the use of e-cigarettes between naturalized U.S. citizens and non-U.S. citizens compared with U.S. natives even after controlling for demographics, socioeconomic status, and history of tobacco use. This finding is consistent with other literature showing that immigrants have lower rates of tobacco use than U.S. natives. However, immigrants' e-cigarette use may increase with length of residency in the United States. Future research is warranted to investigate the safety of e-cigarette products as an alternative to tobacco cigarettes, and how family and neighborhood-level factors influence e-cigarette use among immigrants.
Footnotes
This research was based on public-use secondary data files; therefore, institutional review board approval was not required.
REFERENCES
- 1.Rahman MA, Hann N, Wilson A, Worrall-Carter L. Electronic cigarettes: patterns of use, health effects, use in smoking cessation and regulatory issues. Tob Induc Dis. 2014;12:21. doi: 10.1186/1617-9625-12-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Paradise J. Electronic cigarettes: smoke-free laws, sale restrictions, and the public health. Am J Public Health. 2014;104:e17–8. doi: 10.2105/AJPH.2014.301890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tan ASL, Bigman CA. E-cigarette awareness and perceived harmfulness: prevalence and associations with smoking-cessation outcomes. Am J Prev Med. 2014;47:141–9. doi: 10.1016/j.amepre.2014.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Protano C, Di Milia LM, Orsi GB, Vitali M. Electronic cigarette: a threat or an opportunity for public health? State of the art and future perspectives. Clin Ter. 2015;166:32–7. doi: 10.7417/CT.2015.1799. [DOI] [PubMed] [Google Scholar]
- 5.Kim AE, Arnold KY, Makarenko O. E-cigarette advertising expenditures in the U.S., 2011–2012. Am J Prev Med. 2014;46:409–12. doi: 10.1016/j.amepre.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 6.King BA, Patel R, Nguyen KH, Dube SR. Trends in awareness and use of electronic cigarettes among US adults, 2010–2013. Nicotine Tob Res. 2015;17:219–27. doi: 10.1093/ntr/ntu191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Regan AK, Promoff G, Dube SR, Arrazola R. Electronic nicotine delivery systems: adult use and awareness of the “e-cigarette” in the USA. Tob Control. 2011;22:19–23. doi: 10.1136/tobaccocontrol-2011-050044. [DOI] [PubMed] [Google Scholar]
- 8.Pearson JL, Richardson A, Niaura RS, Vallone DM, Abrams DB. E-cigarette awareness, use, and harm perceptions in US adults. Am J Public Health. 2012;102:1758–66. doi: 10.2105/AJPH.2011.300526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choi K, Forster J. Characteristics associated with awareness, perceptions, and use of electronic nicotine delivery systems among young US Midwestern adults. Am J Public Health. 2013;103:556–61. doi: 10.2105/AJPH.2012.300947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhu SH, Gamst A, Lee M, Cummins S, Yin L, Zoref L. The use and perception of electronic cigarettes and snus among the U.S. population. PLoS One. 2013;8:e79332. doi: 10.1371/journal.pone.0079332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Giovenco DP, Lewis MJ, Delnevo CD. Factors associated with e-cigarette use: a national population survey of current and former smokers. Am J Prev Med. 2014;47:476–80. doi: 10.1016/j.amepre.2014.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schmidt L, Reidmohr A, Harwell TS, Helgerson SD. Prevalence and reasons for initiating use of electronic cigarettes among adults in Montana, 2013. Prev Chronic Dis. 2014;11:E204. doi: 10.5888/pcd11.140283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boyle RG, Amato MS, Rode P, Kinney AM, St Claire AW, Taylor K. Tobacco use among Minnesota adults, 2014. Am J Health Behav. 2015;39:674–9. doi: 10.5993/AJHB.39.5.9. [DOI] [PubMed] [Google Scholar]
- 14.Giovenco DP, Hammond D, Corey CG, Ambrose BK, Delnevo CD. E-cigarette market trends in traditional U.S. retail channels, 2012–2013. Nicotine Tob Res. 2015;17:1297–83. doi: 10.1093/ntr/ntu282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Food and Drug Administration (US) FDA takes significant steps to protect Americans from dangers of tobacco through new regulation [news release]; 2016 May 5 [cited 2016 Apr 10] Available from: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm499234.htm.
- 16.Gualano MR, Passi S, Bert F, La Torre G, Scaioli G, Siliquini R. Electronic cigarettes: assessing the efficacy and the adverse effects through a systematic review of published studies. J Public Health (Oxf) 2014;37:488–97. doi: 10.1093/pubmed/fdu055. [DOI] [PubMed] [Google Scholar]
- 17.Pisinger C, Døssing M. A systematic review of health effects of electronic cigarettes. Prev Med. 2014;69:248–60. doi: 10.1016/j.ypmed.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 18.Odum LE, O'Dell KA, Schepers JS. Electronic cigarettes: do they have a role in smoking cessation? J Pharm Pract. 2012;25:611–4. doi: 10.1177/0897190012451909. [DOI] [PubMed] [Google Scholar]
- 19.Oh AY, Kacker A. Do electronic cigarettes impart a lower potential disease burden than conventional tobacco cigarettes? Review on e-cigarette vapor versus tobacco smoke. Laryngoscope. 2014;124:2702–6. doi: 10.1002/lary.24750. [DOI] [PubMed] [Google Scholar]
- 20.Orr MS. Electronic cigarettes in the USA: a summary of available toxicology data and suggestions for the future. Tob Control. 2014;23(Suppl 2):ii18–22. doi: 10.1136/tobaccocontrol-2013-051474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rom O, Pecorelli A, Valacchi G, Reznick AZ. Are e-cigarettes a safe and good alternative to cigarette smoking? Ann N Y Acad Sci. 2015;1340:65–74. doi: 10.1111/nyas.12609. [DOI] [PubMed] [Google Scholar]
- 22.Voigt K. Smoking norms and the regulation of e-cigarettes. Am J Public Health. 2015;105:1967–72. doi: 10.2105/AJPH.2015.302764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Institute for Global Tobacco Control. Baltimore: Johns Hopkins Bloomberg School of Public Health; 2015. Country laws regulating e-cigarettes: a policy scan. Also available from: http://globaltobaccocontrol.org/e-cigarette/country-laws-regulating-e-cigarettes [cited 2016 May 6] [Google Scholar]
- 24.Primack BA, Soneji S, Stoolmiller M, Fine MJ, Sargent JD. Progression to traditional cigarette smoking after electronic cigarette use among US adolescents and young adults. JAMA Pediatr. 2015;169:1018–23. doi: 10.1001/jamapediatrics.2015.1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barrington-Trimis JL, Berhane K, Unger JB, Cruz TB, Huh J, Leventhal AM, et al. Psychosocial factors associated with adolescent electronic cigarette and cigarette use. Pediatrics. 2015;136:308–17. doi: 10.1542/peds.2015-0639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Roditis ML, Halpern-Felsher B. Adolescents' perceptions of risks and benefits of conventional cigarettes, e-cigarettes, and marijuana: a qualitative analysis. J Adolesc Health. 2015;57:179–85. doi: 10.1016/j.jadohealth.2015.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Camenga DR, Cavallo DA, Kong G, Morean ME, Connell CM, Simon P, et al. Adolescents' and young adults' perceptions of electronic cigarettes for smoking cessation: a focus group study. Nicotine Tob Res. 2015;17:1235–41. doi: 10.1093/ntr/ntv020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kong G, Morean ME, Cavallo DA, Camenga DR, Krishnan-Sarin S. Reasons for electronic cigarette experimentation and discontinuation among adolescents and young adults. Nicotine Tob Res. 2015;17:847–54. doi: 10.1093/ntr/ntu257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pentz MA, Shin H, Riggs N, Unger JB, Collison KL, Chou CP. Parent, peer, and executive function relationships to early adolescent e-cigarette use: a substance use pathway? Addict Behav. 2015;42:73–8. doi: 10.1016/j.addbeh.2014.10.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Krishnan-Sarin S, Morean ME, Camenga DR, Cavallo DA, Kong G. E-cigarette use among high school and middle school adolescents in Connecticut. Nicotine Tob Res. 2015;17:810–8. doi: 10.1093/ntr/ntu243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Leventhal AM, Strong DR, Kirkpatrick MG, Unger JB, Sussman S, Riggs NR, et al. Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. JAMA. 2015;314:700–7. doi: 10.1001/jama.2015.8950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lippert AM. Do adolescent smokers use e-cigarettes to help them quit? The sociodemographic correlates and cessation motivations of U.S. adolescent e-cigarette use. Am J Health Promot. 2015;29:374–9. doi: 10.4278/ajhp.131120-QUAN-595. [DOI] [PubMed] [Google Scholar]
- 33.Porter L, Duke J, Hennon M, Dekevich D, Crankshaw E, Homsi G, et al. Electronic cigarette and traditional cigarette use among middle and high school students in Florida, 2011–2014. PLoS One. 2015;10:e0124385. doi: 10.1371/journal.pone.0124385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Morean ME, Kong G, Camenga DR, Cavallo DA, Simon P, Krishnan-Sarin S. Latent class analysis of current e-cigarette and other substance use in high school students. Drug Alcohol Depend. 2016;161:292–7. doi: 10.1016/j.drugalcdep.2016.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cardenas VM, Evans VL, Balamurugan A, Faramawi MF, Delongchamp RR, Wheeler JG. Use of electronic nicotine delivery systems and recent initiation of smoking among US youth. Int J Public Health. 2016;61:237–41. doi: 10.1007/s00038-015-0783-7. [DOI] [PubMed] [Google Scholar]
- 36.Wilkinson AV, Spitz MR, Strom SS, Prokhorov AV, Barcenas CH, Cao Y, et al. Effects of nativity, age at migration, and acculturation on smoking among adult Houston residents of Mexican descent. Am J Public Health. 2005;95:1043–9. doi: 10.2105/AJPH.2004.055319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Acevedo-Garcia D, Pan J, Jun HJ, Osypuk TL, Emmons KM. The effect of immigrant generation on smoking. Soc Sci Med. 2005;61:1223–42. doi: 10.1016/j.socscimed.2005.01.027. [DOI] [PubMed] [Google Scholar]
- 38.Tong E, Saito N, Tancredi DJ, Borges G, Kravitz RL, Hinton L, et al. A transnational study of migration and smoking behavior in the Mexican-origin population. Am J Public Health. 2012;102:2116–22. doi: 10.2105/AJPH.2012.300739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bosdriesz JR, Lichthart N, Witvliet MI, Busschers WB, Stronks K, Kunst AE. Smoking prevalence among migrants in the US compared to the US-born and the population in countries of origin. PLoS One. 2013;8:e58654. doi: 10.1371/journal.pone.0058654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Salas-Wright CP, Vaughn MG, Clark TT, Terzis LD, Córdova D. Substance use disorders among first- and second- generation immigrant adults in the United States: evidence of an immigrant paradox? J Stud Alcohol Drugs. 2014;75:958–67. doi: 10.15288/jsad.2014.75.958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Almeida J, Johnson RM, Matsumoto A, Godette DC. Substance use, generation and time in the United States: the modifying role of gender for immigrant urban adolescents. Soc Sci Med. 2012;75:2069–75. doi: 10.1016/j.socscimed.2012.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Maher JE, Boysun MJ, Rohde K, Stark MJ, Pizacani BA, Dilley J, et al. Are Latinos really less likely to be smokers? Lessons from Oregon. Nicotine Tob Res. 2005;7:283–7. doi: 10.1080/14622200500056259. [DOI] [PubMed] [Google Scholar]
- 43.Kaplan RC, Bangdiwala SI, Barnhart JM, Castañeda SF, Gellman MD, Lee DJ, et al. Smoking among U.S. Hispanic/Latino adults: the Hispanic community health study/study of Latinos. Am J Prev Med. 2014;46:496–506. doi: 10.1016/j.amepre.2014.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Li K, Wen M. Substance use, age at migration, and length of residence among adult immigrants in the United States. J Immigr Minor Health. 2013;17:156–64. doi: 10.1007/s10903-013-9887-4. [DOI] [PubMed] [Google Scholar]
- 45.Rodriquez EJ, Stoecklin-Marois MT, Hennessy-Burt TE, Tancredi DJ, Schenker MB. Acculturation-related predictors of very light smoking among Latinos in California and nationwide. J Immigr Minor Health. 2015;17:181–91. doi: 10.1007/s10903-013-9896-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Koya DL, Egede LE. Association between length of residence and cardiovascular disease risk factors among an ethnically diverse group of United States immigrants. J Gen Intern Med. 2007;22:841–6. doi: 10.1007/s11606-007-0163-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Alcalá HE, Albert SL, Ortega AN. E-cigarette use and disparities by race, citizenship status and language among adolescents. Addict Behav. 2016;57:30–4. doi: 10.1016/j.addbeh.2016.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.National Center for Health Statistics (US) National Health Interview Survey 2014 [cited 2016 Apr 8] Available from: http://www.cdc.gov/nchs/nhis/nhis_2014_data_release.htm.
- 49.Borges G, Medina-Mora ME, Orozco R, Fleiz C, Cherpitel C, Breslau J. The Mexican migration to the United States and substance use in northern Mexico. Addiction. 2009;104:603–11. doi: 10.1111/j.1360-0443.2008.02491.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gorman BK, Lariscy JT, Kaushik C. Gender, acculturation, and smoking behavior among U.S. Asian and Latino immigrants. Soc Sci Med. 2014;106:110–8. doi: 10.1016/j.socscimed.2014.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.StataCorp. Stata®: Version 13.0. College Station (TX): StataCorp; 2013. [Google Scholar]
- 52.Qureshi A, Garcia Campayo J, Eiroa-Orosa FJ, Sobradiel N, Collazos F, Febrel Bordejé M, et al. Epidemiology of substance abuse among migrants compared to native born population in primary care. Am J Addict. 2014;23:337–42. doi: 10.1111/j.1521-0391.2013.12103.x. [DOI] [PubMed] [Google Scholar]
- 53.Schwartz SJ, Weisskirch RS, Zamboanga BL, Castillo LG, Ham LS, Huynh QL, et al. Dimensions of acculturation: associations with health risk behaviors among college students from immigrant families. J Couns Psychol. 2011;58:27–41. doi: 10.1037/a0021356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Osypuk TL, Acevedo-Garcia D. Support for smoke-free policies: a nationwide analysis of immigrants, US-born, and other demographic groups, 1995–2002. Am J Public Health. 2010;100:171–81. doi: 10.2105/AJPH.2009.160218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rose SW, Barker DC, D'Angelo H, Khan T, Huang J, Chaloupka FJ, et al. The availability of electronic cigarettes in U.S. retail outlets, 2012: results of two national studies. Tob Control. 2014;23(Suppl 3):iii10–6. doi: 10.1136/tobaccocontrol-2013-051461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Huang J, Tauras J, Chaloupka FJ. The impact of price and tobacco control policies on the demand for electronic nicotine delivery systems. Tob Control. 2014;23(Suppl 3):iii41–7. doi: 10.1136/tobaccocontrol-2013-051515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Biener L, Hargraves JL. A longitudinal study of electronic cigarette use among a population-based sample of adult smokers: association with smoking cessation and motivation to quit. Nicotine Tob Res. 2015;17:127–33. doi: 10.1093/ntr/ntu200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bhatnagar A, Whitsel LP, Ribisl KM, Bullen C, Chaloupka F, Piano MR, et al. on behalf of the American Heart Association Advocacy Coordinating Committee, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Quality of Care and Outcomes Research. Electronic cigarettes: a policy statement from the American Heart Association. Circulation. 2014;130:1418–36. doi: 10.1161/CIR.0000000000000107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhu SH, Sun JY, Bonnevie E, Cummins SE, Gamst A, Yin L, et al. Four hundred and sixty brands of e-cigarettes and counting: implications for product regulation. Tob Control. 2014;23(Suppl 3):iii3–9. doi: 10.1136/tobaccocontrol-2014-051670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.de Walque D. Does education affect smoking behaviors? Evidence using the Vietnam draft as an instrument for college education. J Health Econ. 2007;26:877–95. doi: 10.1016/j.jhealeco.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 61.King AC, Smith LJ, McNamara PJ, Matthews AK, Fridberg DJ. Passive exposure to electronic cigarette (e-cigarette) use increases desire for combustible and e-cigarettes in young adult smokers. Tob Control. 2015;24:501–4. doi: 10.1136/tobaccocontrol-2014-051563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wills TA, Sargent JD, Knight R, Pagano I, Gibbons FX. E-cigarette use and willingness to smoke: a sample of adolescent non-smokers. Tob Control. 2015;25:e52–9. doi: 10.1136/tobaccocontrol-2015-052349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Smith DM, Bansal-Travers M, O'Connor RJ, Goniewicz ML, Hyland A. Associations between perceptions of e-cigarette advertising and interest in product trial amongst US adult smokers and non-smokers: results from an Internet-based pilot survey. Tob Induc Dis. 2015;13:14. doi: 10.1186/s12971-015-0039-6. [DOI] [PMC free article] [PubMed] [Google Scholar]