Abstract
Background:
Several studies have shown that smoking, as a modifiable risk factor, can affect tuberculosis (TB) in different aspects such as enhancing development of TB infection, activation of latent TB and its related mortality. Since willingness to quit smoking is a critical stage, which may lead to quit attempts, being aware of smokers’ intention to quit and the related predictors can provide considerable advantages.
Materials and Methods:
In this cross-sectional study, subjects were recruited via a multi-stage cluster sampling method. Sampling was performed during 2012–2014 among pulmonary TB (PTB) patients referred to health centers in Tehran implementing the directly observed treatment short course (DOTS) strategy and a TB referral center. Data analysis was conducted using SPSS version 22 and the factors influencing quit intention were assessed using bivariate regression and multiple logistic regression models.
Results:
In this study 1,127 newly diagnosed PTB patients were studied; from which 284 patients (22%) were current smokers. When diagnosed with TB, 59 (23.8%) smokers quit smoking. Among the remaining 189 (76.2%) patients who continued smoking, 52.4% had intention to quit. In the final multiple logistic regression model, living in urban areas (OR=8.81, P=0.003), having an office job (OR= 7.34, P=0.001), being single (OR=4.89, P=0.016) and a one unit increase in the motivation degree (OR=2.60, P<0.001) were found to increase the intention to quit smoking.
Conclusion:
The study found that PTB patients who continued smoking had remarkable intention to quit. Thus, it is recommended that smoking cessation interventions should be started at the time of TB diagnosis. Understanding the associated factors can guide the consultants to predict patients’ intention to quit and select the most proper management to facilitate smoking cessation for each patient.
Keywords: Tuberculosis, Pulmonary; Smoking Cessation; Intention
INTRODUCTION
Several studies have shown that smoking can affect TB in different aspects such as enhancing the development of TB infection, activation of latent TB and related mortality (1). These effects might be due to extensive exposure to cigarette smoke (2). TB is considered as one of the main causes of death in the world, particularly in the Asia and Africa. In 2006, 2.9 million new cases of TB and 7.1 million deaths from this disease were reported in developing countries (3). The majority of TB-related morbidity and mortality occurs in developing countries, where smoking is also a major health issue (4). On the other hand, tobacco use is the most preventable cause of death and as the second leading cause of death in the world; one out of every ten deaths among adults is due to smoking. It is expected that by 2030, the annual death rate from tobacco consumption reaches 8 million (5). The issue of smoking cessation should be considered as an integral part of TB control programs. Accordingly, much has been done for smoking cessation in TB patients by the International Union Against Tuberculosis and Lung Diseases (IUATLD) (6). However, its efficacy for TB control has not yet been established (7). Being aware of the patients’ intention to quit smoking and the related factors can assist the therapist to obtain better quit results during the treatment course (8). As mentioned in health behavior theories, willingness to quit is the main prerequisite for quit attempts (9).
Health problems can influence a smoker’s positive intention to quit (10). Other factors such as age, gender, nicotine dependence, motivation factor, self-efficacy and previous quit attempts can also affect one’s quit intention and cessation results (11, 12). Knowledge about a patient’s intention to quit and its predictive factors can help the consultant to choose an appropriate cessation method to achieve a better progress during treatment (13).
Tobacco use and TB are major health hazards, many aspects of which are still unclear. Therefore, this study aimed to determine the intention to quit and its associated factors among smokers newly diagnosed with PTB.
MATERIALS AND METHODS
In this cross-sectional study, subjects were recruited through a multi-stage cluster sampling method. Overall, there are 230 health centers in Tehran. These centers are categorized into three groups based on their geographical location and each group is under supervision of one medical university. There are eight comprehensive health centers in each group, implementing the DOTS strategy. Because each comprehensive health center was regarded as a cluster and the homogeneity between the samples in a comprehensive health center was assumed to be higher than the homogeneity of different comprehensive health centers, and also all comprehensive health centers are under the supervision of Ministry of Health, we considered two comprehensive health centers in each section. Masih Daneshvari TB center that has referrals from all over the Tehran city was also considered as one of our sampling sources.
All the newly diagnosed sputum smear positive and smear negative PTB patients (defined as any bacteriologically confirmed or clinically diagnosed case of TB involving the lung parenchyma or the tracheobronchial tree who has never been treated for TB or has not taken anti-TB drugs for at least one month) referred to the aforementioned seven sampling centers during 2012–2014 were included in the study. The inclusion criteria were as follows:
Category I patients: Newly-diagnosed PTB patients based on treatment guidelines of the World Health Organization (WHO)(14); age ≥18 years; Iranians or Afghans who could speak Farsi.
The exclusion criteria were:
Multi-drug resistance; co-infection with HIV/AIDS; category II patients; recurrence, treatment failure or treatment errors; category III patients; chronic TB; not willing to participate in the study; unable to communicate or understand the written consent form.
Smoking status was considered based on the patients’ self-reports of tobacco consumption, according to the WHO and IUATLD documents (15). After explaining the study, patients willing to participate completed the written consent form and were included in the study. Data were gathered through face to face interviews, in which predesigned questionnaires were completed by the interviewers, recording information about smoking history, nicotine dependence, reason for smoking and intention to quit based on the WHO standard tests (13). Intention to quit was defined as whether the patient was willing to quit within the next month or not. Motivation degree was evaluated by asking the patients to assess their motivation to quit smoking on a scale of one to 10. Self-confidence score was also determined on a scale of one to 10, evaluating the patients’ confidence to quit smoking (13).
All the data were entered into SPSS software twice. Analysis was performed by SPSS version 22 software. Since continuous variables (age, smoking initiation age, pack/year) were not normally distributed, logarithm conversion was used to create normal distribution. The Student t-test was used for comparison of continuous variables and Pearson’s chi-square test with the Fisher’s exact test were used for qualitative variables. To investigate the factors influencing intention to quit smoking, bivariate regression and multiple logistic regression models were used.
RESULTS
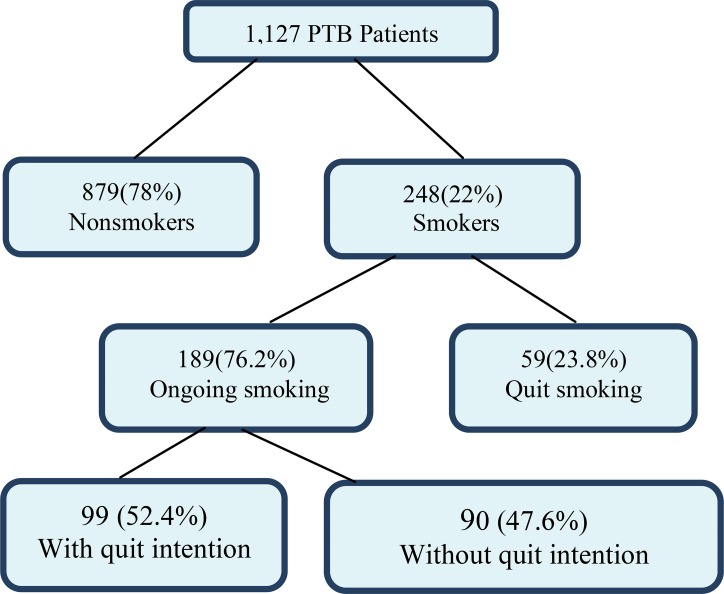
In this study, 1,127 newly diagnosed PTB patients referring to comprehensive health centers and a tuberculosis referral center were included; out of which 624 (55.4%) were males. There were 879 (78%) nonsmokers and 248 (22%) patients were current smokers including 228 (20.2%) daily smokers and 20 (1.8%) occasional smokers. When diagnosed with TB, 59 smoker patients (23.8%) quit smoking. The remaining 189 (76.2%) patients continued smoking despite PTB diagnosis (Figure 1).
Figure 1.
The study flow chart
The mean age of the patients who continued smoking was 41.27±12.01 years. Table 1 shows the other demographic characteristics of the smokers. Regarding the patients’ smoking status, 183 (96.8%) were daily smokers while six patients (3.2%) were occasional smokers. Although age of smoking initiation ranged from six to 45 years, the average age of smoking initiation was 20 years. The number of cigarettes smoked varied from 0.5 to three packs per day. The overall average of daily cigarette consumption was 19.5 cigarettes. After PTB diagnosis, 99 patients (52.4%) had intention to quit in the next month. The smoking status of the patients with regard to their intention to quit is depicted in Table 2.
Table 1.
Demographic characteristics of ongoing smoker PTB patients
| Factor | Intention to quit (in the next month) | Total | ||
|---|---|---|---|---|
| Yes n (%) | No n (%) | |||
| Sex | Male | 93 (50.8) | 90 (49.2) | 183 (100) |
| Female | 6 (100) | 0 (0) | 6 (100) | |
| Nationality | Afghan | 1 (4.8) | 20 (95.2) | 21 (100) |
| Iranian | 98 (58.3) | 70 (41.7) | 168 (100) | |
| Living Area | Rural | 13 (30.2) | 30 (69.8) | 43 (100) |
| Urban | 86 (58.9) | 60 (41.1) | 146 (100) | |
| Marital Status | Married | 33 (35.1) | 61 (64.9) | 94 (100) |
| Single | 66 (69.5) | 29 (30.5) | 95 (100) | |
| Occupation* | Manual | 41 (41) | 59 (59) | 100 (100) |
| Office-worker | 55 (67) | 27 (32.9) | 82 (100) | |
| Illiterate | 5 (35.7) | 9 (64.3) | 14 (100) | |
| Education | Under diploma | 63 (54.3) | 53 (65.7) | 116 (100) |
| High school diploma | 20 (41.7) | 28 (58.3) | 48 (100) | |
| Academic | 11 (100) | 0 (0) | 11 (100) | |
| Underlying disease | No | 95 (51.4) | 90 (48.6) | 185 (100) |
| Yes | 4 (100) | 0 (0) | 4 (100) | |
Different total; due to missing variable
Table 2.
Smoking status according to the intention to quit smoking in the next month
| Factor | Intention to quit smoking (in the next month) | Total | P-value | ||
|---|---|---|---|---|---|
| No | Yes | ||||
| Reason of smoking* | Relaxation | 8 (100%) | 0 (0%) | 8 (100%) | |
| Pleasure | 1 (7.7%) | 12 (92.3%) | 13 (100%) | <0.001 | |
| Addiction | 32 (41.6%) | 45 (58.4%) | 77 (100%) | ||
| Habitual | 58 (66.7%) | 29 (33.3%) | 87 (100%) | ||
| Past quit attempt | No | 50 (37.3%) | 84 (10.9%) | 134 (100%) | <0.001 |
| Yes | 49 (89.1%) | 6 (6%) | 55 (100%) | ||
| Smoking initiation age | 19.30±8.92 | 20.94±5.98 | 20.15±7.66 | 0.29 | |
| Packs/Year | 24.78±30.25 | 21.47±21.02 | 23.19±26.16 | 0.36 | |
| Nicotine dependence | 4.73±2.68 | 4.80±2.64 | 4.76±2.67 | 0.02 | |
| Motivation degree | 7.14±2.83 | 3.45±1.79 | 5.45±3.02 | <0.001 | |
| Self-confidence score | 6.36±2.83 | 3.31±1.82 | 4.97±2.84 | <0.001 | |
Different total; due to missing variable
Based on the bivariate analysis of the factors affecting intention to quit within the next month, Iranians were significantly more likely to have intention to quit compared to Afghans (P<0.001, OR=28.00, 95%CI=3.67–213.51), as well as past quit attempts (P<0.001, OR=13.72, 95%CI=5.48–34.33). Moreover, we found that being single, working in office and living in urban areas had significant associations with smoking (Table 3).
Table 3.
Factors affecting the intention to quit by multiple logistic regression models
| Factor | Crude | Adjusted | |||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | P-value | OR | 95% CI | P-value | ||
| Living Area | Rural | 3.30 | 1.59–6.86 | 0.001 | 8.81 | 2.05–37.90 | 0.003 |
| Urban | |||||||
| Marriage | Married | 4.20 | 2.29–7.72 | <0.001 | 4.89 | 1.33–17.91 | 0.016 |
| Single | |||||||
| Occupation | Manual | 2.93 | 1.59–5.39 | 0.001 | 7.34 | 2.32–23.27 | 0.001 |
| Office-worker | |||||||
| Smoking Initiation age | 1.01 | 0.96–1.04 | 0.12 | 0.97 | 0.91–1.03 | 0.41 | |
| Nicotine dependence | 1.03 | 0.92–1.15 | 0.19 | 0.57 | 0.14–2.20 | 0.42 | |
| Motivation degree | 3.21 | 2.23–4.62 | <0.001 | 2.60 | 1.59–4.26 | <0.001 | |
| Self-confidence score | 2.48 | 1.88–3.29 | <0.001 | 0.75 | 0.49–1.13 | 0.17 | |
Since the factors such as age, sex, education, reason of smoking, number of cigarettes smoked per day and the packs/year were not found to significantly affect the outcome in bivariate statistical analysis, their odds ratio were not calculated and these factors were not included in multiple regression models. In spite of the significant effect of nationality and past quit attempt history on patient’s intention to quit in bivariate analysis (P<0.001, P<0.001), these factors were not entered into the multiple logistic regression model due to the low number of cases in one of the groups. In the final multiple logistic regression model, living in urban areas, office jobs, being single and a one unit increase in the motivation scale significantly increased the intention to quit smoking (Table 3).
DISCUSSION
Tuberculosis and smoking are known as two intertwined epidemics that lead to six million deaths per year (16). Smoking increases the risk of infection and TB in such a way that 20% of the total TB burden has been attributed to tobacco use (17). In the past decade, the rate of tobacco use related morbidity and mortality in developing countries was doubled and it is estimated that in the next 20 years, 80% of the morbidity and mortality from smoking occurs in developing countries (18). If preventive measures are not taken to stop smoking and health providers do not provide quit advice and smoking cessation interventions for the smokers, this health hazard will probably result in the deaths of more than a hundred million people (19). In response to the evidence on the harmful effects of smoking on TB, inclusion of smoking cessation interventions in TB treatment programs is firmly recommended (20). It is observed that the intention to stop smoking is clearly correlated with the rate of successful smoking cessation and it is one of the key steps for quitting (21). Being aware of the patients’ smoking status, their intentions to quit and the influencing factors can help consultants to choose the best method based on individual characteristics.
Rate of smoking cessation in people who have a serious desire to quit is higher than in others (22); accordingly, it is important to specify the characteristics related to smokers’ intention to quit (23). The current study found that 22% of the newly diagnosed PTB patients were smokers and 16.8% continued smoking despite the TB diagnosis. The prevalence of smoking among PTB patients seemed to be higher than the 14.2% prevalence rate reported in a normal Iranian population (15–64 year olds) (18).
In our study, 96.8% of smoker PTB patients were males and only 3.2% were females. These figures seem to be compatible with the results obtained for a normal Iranian population reporting that 24% of men and 4.3% of women were smokers (18), which was most likely due to the socio-cultural factors. In our study, 52.4% of smokers were willing to quit within the next month. In a research conducted in Canada, one-third of patients aged 45 years or older had planned to stop smoking in the near future (23). In Vietnam, the intention to quit within the next month in healthy smokers was 36%, and in studies in India, China and Thailand, this figure was reported to be 12%, 24% and 30%, respectively (24,25). Accordingly, it seems that the quit intention among PTB patients is higher than in healthy smoker population. Of course, the conditions of TB patients increase the probability of successful smoking cessation (26–28). In this study, intention to quit in patients with higher self-confidence scores was significantly higher than in the others. Other studies have also shown that the probability of success of patients in quitting with higher self-confidence scores is greater than those with lower self-confidence scores (29). Quitting smoking is a dynamic process that requires repeated quit attempts (30). One of the remarkable findings of our research was the correlation between previous quit attempts and the intention to quit smoking, which is congruent with the findings of other studies (31–35). This indicates that tobacco users require multiple quit attempts before their final quit process (30). Therefore this factor should be considered in the process of smoking cessation.
Through logistic regression analysis, this study showed that living in urban areas, office work, being single and high level of motivation increased the intention to quit among the patients. Other evidence also supports the relationship between the intention to quit and the occupational status (36–38) but no other studies have mentioned a correlation between marital status and the intention to quit. The number of daily cigarettes smoked and nicotine dependence were not found to affect the intention to quit in this model, however, studies in the US and Canada on healthy smokers have confirmed this relationship (39).
In order to yield better smoking cessation results, consultants need to know the patient’s dependence, motivation degree and readiness, so that the therapists can provide the proper techniques and methods for the smokers to quit (13). This study found that the intention to quit smoking in newly diagnosed PTB patients was remarkable. In general, it is suggested that for successful smoking cessation programs, therapists should pay attention to smokers who are at the stage of pre-contemplation and contemplation (40) and it is never too late for the health care staff to provide smoking cessation interventions (23).
As it is recommended that smoking cessation interventions be started at the time of TB diagnosis, understanding these associated factors can guide the consultants to predict the patient’s quit intention to some extent and choose the most proper intervention to facilitate quitting in each case, so that the practitioners can help smoker PTB patients to progress through stages of change and continuously reduce the prevalence of smoking in this population. Also, these data can be used to motivate policy makers and stakeholders to include smoking cessation plans in the national TB control programs.
Limitations
Cross-sectional nature of this study does not allow evaluation of the causal relationship between factors and smoking cessation, and its prognostic factors. Thus, further prospective studies are required. Meanwhile, as this study was conducted on patients with newly diagnosed PTB, its results cannot be generalized to all TB patients.
Acknowledgments
We appreciate health care providers, stakeholders and TB referral center’s staff who cooperated in conducting this study. Also, we acknowledge the National Research Institute of Tuberculosis and Lung Disease and Shahid Beheshti University of Medical Sciences for funding this project.
REFERENCES
- 1. Pai M, Mohan A, Dheda K, Leung CC, Yew WW, Christopher DJ, Sharma SK. Lethal interaction: the colliding epidemics of tobacco and tuberculosis. Expert review of anti-infective therapy. 2007; 5(3: 385– 91. [DOI] [PubMed] [Google Scholar]
- 2. den Boon S, van Lill SW, Borgdorff MW, Verver S, Bateman ED, Lombard CJ, et al. Association between smoking and tuberculosis infection: a population survey in a high tuberculosis incidence area. Thorax 2005; 60 (7): 555– 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mohajan HK. Tuberculosis is a Fatal Disease among Some Developing Countries of the World. American Journal of Infectious Diseases and Microbiology 2015; 3 (1): 18– 31. [Google Scholar]
- 4. Brunet L, Pai M, Davids V, Ling D, Paradis G, Lenders L, et al. High prevalence of smoking among patients with suspected tuberculosis in South Africa. European Respiratory Journal 2011; 38 (1): 139– 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. WHO report on the global tobacco epidemic , 2008. The MPOWER packgage. Geneva: , World Health Organization; , 2008. . [Google Scholar]
- 6. Slama K, Chiang CY, Enarson DA, Hassmiller K, Fanning A, Gupta P, et al. Tobacco and tuberculosis: a qualitative systematic review and meta-analysis. Int J Tuberc Lung Dis 2007; 11 (10): 1049– 61. [PubMed] [Google Scholar]
- 7. van Zyl Smit RN, Pai M, Yew WW, Leung CC, Zumla A, Bateman ED, et al. Global lung health: the colliding epidemics of tuberculosis, tobacco smoking, HIV and COPD. Eur Respir J 2010; 35 (1): 27– 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Stockings E, Bowman J, McElwaine K, Baker A, Terry M, Clancy R, et al. Readiness to quit smoking and quit attempts among Australian mental health inpatients. Nicotine Tob Res 2013; 15 (5): 942– 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gould GS, Watt K, McEwen A, Cadet-James Y, Clough AR. Predictors of intentions to quit smoking in Aboriginal tobacco smokers of reproductive age in regional New South Wales (NSW), Australia: quantitative and qualitative findings of a cross-sectional survey. BMJ Open 2015; 5 (3): e007020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. West R, Hardy A. Beginning the journey: addiction as choice. In: Theory of addiction. Oxford: : Blackwell Publishing Ltd; ; 2006. Chapter3. p. 29–74. [Google Scholar]
- 11. Caponnetto P, Polosa R. Common predictors of smoking cessation in clinical practice. Respir Med 2008; 102 (8): 1182– 92. [DOI] [PubMed] [Google Scholar]
- 12. Vangeli E, Stapleton J, Smit ES, Borland R, West R. Predictors of attempts to stop smoking and their success in adult general population samples: a systematic review. Addiction 2011; 106 (12): 2110– 21. [DOI] [PubMed] [Google Scholar]
- 13. Slama K, Chiang CY, Donald A. . Enarson. Tobacco cessation interventions for tuberculosis patients: a guide for low-income countries . International union against tuberculosis and lung disease; 2008.
- 14. World Health Organization Treatment of tuberculosis: guidelines. World Health Organization; 2010. [PubMed] [Google Scholar]
- 15. Slama K, Chiang CY, Enarson DA. Tobacco cessation and brief advice. Int J Tuberc Lung Dis 2007; 11 (6): 612– 6. [PubMed] [Google Scholar]
- 16. World Health Organization WHO Report on the Global Tobacco Epidemic , 2011. . Geneva: : World Health Organization; , 2011 [accessed 2015 Dec 11]. [Google Scholar]
- 17. Lin HH, Ezzati M, Murray M. Tobacco smoke, indoor air pollution and tuberculosis: a systematic review and meta-analysis. PLoS Med 2007; 4 (1): e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Heydari G, Jianfar G, Alvanpour A, Hesami Z, Talischi F, Masjedi MR. Efficacy of telephone quit-line for smokers in Iran: 12 months follow up results. Tanaffos 2011; 10 (3): 42. [PMC free article] [PubMed] [Google Scholar]
- 19. Mackay J, Eriksen M, Shafey O. The Tobacco Atlas. 2nd Atlanta, GA: : American Cancer Society; . 2006; p: 22– 55. [Google Scholar]
- 20. Bates MN, Khalakdina A, Pai M, Chang L, Lessa F, Smith KR. Risk of tuberculosis from exposure to tobacco smoke: a systematic review and meta-analysis. Arch Intern Med 2007; 167 (4): 335– 42. [DOI] [PubMed] [Google Scholar]
- 21. Balmford J, Borland R, Burney S. The influence of having a quit date on prediction of smoking cessation outcome. Health Educ Res 2010; 25 (4): 698– 706. [DOI] [PubMed] [Google Scholar]
- 22. Ajzen I. The theory of planned behavior . Organizational behavior and human decision processes . 1991. ; 50 (2):179–211. [Google Scholar]
- 23. Leatherdale ST, Shields M. Smoking cessation: intentions, attempts and techniques. Health Rep 2009; 20 (3): 31– 9. [PubMed] [Google Scholar]
- 24. Li L, Borland R, Yong HH, Fong GT, Bansal-Travers M, Quah AC, et al. Predictors of smoking cessation among adult smokers in Malaysia and Thailand: findings from the International Tobacco Control Southeast Asia Survey. Nicotine Tob Res 2010; 12 Suppl: S34–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Siahpush M, Borland R, Yong HH, Kin F, Sirirassamee B. Socio-economic variations in tobacco consumption, intention to quit and self-efficacy to quit among male smokers in Thailand and Malaysia: results from the International Tobacco Control–South-East Asia (ITC–SEA) survey. Addiction 2008; 103 (3): 502– 8. [DOI] [PubMed] [Google Scholar]
- 26. Shin SS, Xiao D, Cao M, Wang C, Li Q, Chai WX, et al. Patient and doctor perspectives on incorporating smoking cessation into tuberculosis care in Beijing, China. Int J Tuberc Lung Dis 2012; 16 (1): 126– 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pradeepkumar AS, Thankappan KR, Nichter M. Smoking among tuberculosis patients in Kerala, India: proactive cessation efforts are urgently needed. Int J Tuberc Lung Dis 2008; 12 (10): 1139– 45. [PubMed] [Google Scholar]
- 28. Ng N, Padmawati RS, Prabandari YS, Nichter M. Smoking behavior among former tuberculosis patients in Indonesia: intervention is needed. Int J Tuberc Lung Dis 2008; 12 (5): 567– 72. [PubMed] [Google Scholar]
- 29. Zhu WH, Yang L, Jiang CQ, Deng LZ, Lam TH, Zhang JY, et al. Characteristics of smokers and predictors of quitting in a smoking cessation clinic in Guangzhou, China. J Public Health (Oxf) 2010; 32 (2): 267– 76. [DOI] [PubMed] [Google Scholar]
- 30. Fiore MC, Jaen CR, Baker T, Bailey WC, Benowitz NL, Curry SE, et al. Treating tobacco use and dependence: 2008 update . Rockville, MD: : US Department of Health and Human Services; . 2008. May 27. [Google Scholar]
- 31. Tsoh JY, Tong EK, Gildengorin G, Nguyen TT, Modayil MV, Wong C, et al. . Individual and family factors associated with intention to quit among male Vietnamese American smokers: implications for intervention development. Addict Behav 2011; 36 (4): 294– 301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Yu DK, Wu KK, Abdullah AS, Chai SC, Chai SB, Chau KY, et al. Smoking cessation among Hong Kong Chinese smokers attending hospital as outpatients: impact of doctors’ advice, successful quitting and intention to quit. Asia Pac J Public Health 2004; 16 (2): 115– 20. [DOI] [PubMed] [Google Scholar]
- 33. Haddad LG, Petro-Nustas W. Predictors of intention to quit smoking among Jordanian university students. Can J Public Health 2006; 97 (1): 9– 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hyland A, Borland R, Li Q, Yong HH, McNeill A, Fong GT, et al. Individual-level predictors of cessation behaviours among participants in the International Tobacco Control (ITC) Four Country Survey. Tob Control 2006; 15 Suppl 3: iii83–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Panda R, Venkatesan S, Persai D, Trivedi M, Mathur MR. Factors determining intention to quit tobacco: exploring patient responses visiting public health facilities in India. Tob Induc Dis 2014; 12 (1): 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kabat GC, Wynder EL. Determinants of quitting smoking. Am J Public Health 1987; 77 (10): 1301– 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Marques-Vidal P, Melich-Cerveira J, Paccaud F, Waeber G, Vollenweider P, Cornuz J. Prevalence and factors associated with difficulty and intention to quit smoking in Switzerland. BMC Public Health 2011; 11: 227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Karvonen-Gutierrez CA, Ewing LA, Taylor NJ, Essenmacher CA, Duffy SA. Ethnicity predicts perceptions of smoking and smoking cessation among veterans. J Psychiatr Ment Health Nurs 2012; 19 (3): 203– 10. [DOI] [PubMed] [Google Scholar]
- 39. Fagan P, Augustson E, Backinger CL, O'Connell ME, Vollinger RE, Jr, Kaufman A, et al. Quit attempts and intention to quit cigarette smoking among young adults in the United States. Am J Public Health 2007; 97 (8): 1412– 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Yang G, Ma J, Chen A, Zhang Y, Samet JM, Taylor CE, et al. Smoking cessation in China: findings from the 1996 national prevalence survey. Tob Control 2001; 10 (2): 170– 4. [DOI] [PMC free article] [PubMed] [Google Scholar]