Supplemental Digital Content is available in the text
Keywords: emergency department, nonurgent, Taiwan Triage and Acuity Scale, triage, vital sign
Abstract
Nonurgent emergency department (ED) patients are a controversial issue in the era of ED overcrowding. However, a substantial number of post-ED hospitalizations were found, which prompted for investigation and strategy management. The objective of this study is to identify risk factors for predicting the subsequent hospitalization of nonurgent emergency patients. This was a retrospective study of a database of adult nontrauma ED visits in a medical center for a period of 12 months from January 2013 to December 2013. Patient triages as either Taiwan Triage and Acuity Scale (TTAS) level 4 or 5 were considered “nonurgent.” Basic demographic data, primary and secondary diagnoses, clinical parameters including blood pressure, heart rate, body temperature, and chief complaint category in TTAS were analyzed to determine if correlation exists between potential predictors and hospitalization in nonurgent patients.
A total of 16,499 nonurgent patients were included for study. The overall hospitalization rate was 12.47 % (2058/16,499). In the multiple logistic regression model, patients with characteristics of males (odds ratio, OR = 1.37), age more than 65 years old (OR = 1.56), arrival by ambulance (OR = 2.40), heart rate more than 100/min (OR = 1.47), fever (OR = 2.73), and presented with skin swelling/redness (OR = 4.64) were predictors for hospitalization. The area under receiver-operator calibration curve (AUROC) for the prediction model was 0.70. Nonurgent patients might still be admitted for further care especially in male, the elderly, with more secondary diagnoses, abnormal vital signs, and presented with dermatologic complaints. Using the TTAS acuity level to identify patients for diversion away from the ED is unsafe and will lead to inappropriate refusal of care for many patients requiring hospital treatment.
1. Introduction
Nonurgent visits are defined as patients with problems that are not likely life-threatening nor required immediate attention and the care can be safely delayed.[1,2] In this era of emergency department (ED) overcrowding, the management of nonurgent visits to the ED are a controversial issue in the literatures.[1–5] Taiwan has implemented a new 5 acuity triage system, Taiwan Triage and Acuity Scale (TTAS), in 2010. TTAS was modified from Canadian Triage and Acuity Scale (CTAS) and was shown to be a reliable system.[6,7] Patients with TTAS levels 1–3 need resuscitation, emergent, or urgent care requiring timely physician evaluation, whereas patients with TTAS levels 4 and 5 are with less urgent or nonurgent conditions for whom physician assessment can more safely be delayed. In our previous study, we found patients with TTAS levels 4 and 5 comprised about 30% of all ED patients.[6,7]
Nonurgent ED patients have negatively impacted on crowding, and unnecessary costs, whereas some authors have advocated diverting nonurgent patients away from to ED to help reduce delays and improve access for sicker patients.[8–13] In the absence of valid measures, most administrators still believe that less or nonurgent problems should be treated in alternate health care settings, such as outpatient clinics or family physician offices rather than overburdened EDs.[14–16] Indiscriminately redirecting patients, identified as nonurgent, to alternative care facilities is highly debated as it generates ethical and patient safety issues.[5,9,12,17] Previous studies have examined whether nonurgent ED patients can be safely deferred to alternate health care settings, and have identified unintended consequences of adverse outcomes in patients with unrecognized high risk conditions.[16,18–19]
A recent Canadian study identified a significant number of CTAS level 4 and 5 hospital admissions and concluded that using CTAS acuity as the lone criterion to redirect patients away from the ED is unsafe.[18] In our previous study, we also found that 10.1% of the low urgency (TTAS level 4 and 5) patients were admitted.[7] Recently Lin et al had showed that age more than 65 and arrival by ambulance may be predictors of admission in nonurgent patients in three Canadian EDs; however, factors associated with admission in nonurgent patients remained to be a multifactorial issue.[20] This study is to identify risk factors more comprehensively for predicting the subsequent hospitalization of nonurgent emergency patients.
2. Methods
This study is a retrospective database patient cohort analysis using the adult nontrauma ED visits in a medical center located in northern Taiwan during January 1–December 31, 2013. All ED patients triaged as TTAS level 4 or 5 were considered nonurgent and included in the study. To have a more comprehensive approach, this study has collected all variables available from the information system and electronic medical chart. The study variables include: age, sex, TTAS, chief complaint, triage level, vital signs taken at triage (including BP, heart rate, respiratory rate, and body temperature), primary diagnosis, and secondary diagnosis recorded by emergency physician at ED database using International Classification of Diseases (9th revision) Clinical Modification (ICD-9-CM) coding system at ED and final disposition. Variables of vital signs were further categorized as high/medium/low systolic blood pressure (SBP > 180 mmHg/111–180 mmHg/≤ 110 mmHg),[21] tachycardia (HR >100 times/min), fever (BT ≥ 38C), and tachypnea (RR > 20 breaths/min). The respiratory rates in our nonurgent population were all less than 20 breaths/min, and the O2 saturation were all above 94%, so the tachypnea category was excluded from the analysis. This study was approved by institutional ethics review board (#102–3459B) with a waiver of patient consent proviso.
Data are presented as mean ± standard deviation (SD) for numerical variables and as frequency (%) for categorical variables. The two sample t test was used to compare the difference of numerical variables between the two study groups, whereas the χ2 test was employed to compare categorical variables between groups. Univariate analysis was performed to screen the variables before multiple regression analysis. Multivariable logistic regression analysis was applied to determine factors associated with hospitalization. The significant factors associated with hospitalization were scored and summed up by multiplying their nearest integer of odds ratio (OR) with the original values. The performance of these factors to predict hospitalization was then calculated by the area under receiver-operator calibration curve (AUROC).
3. Results
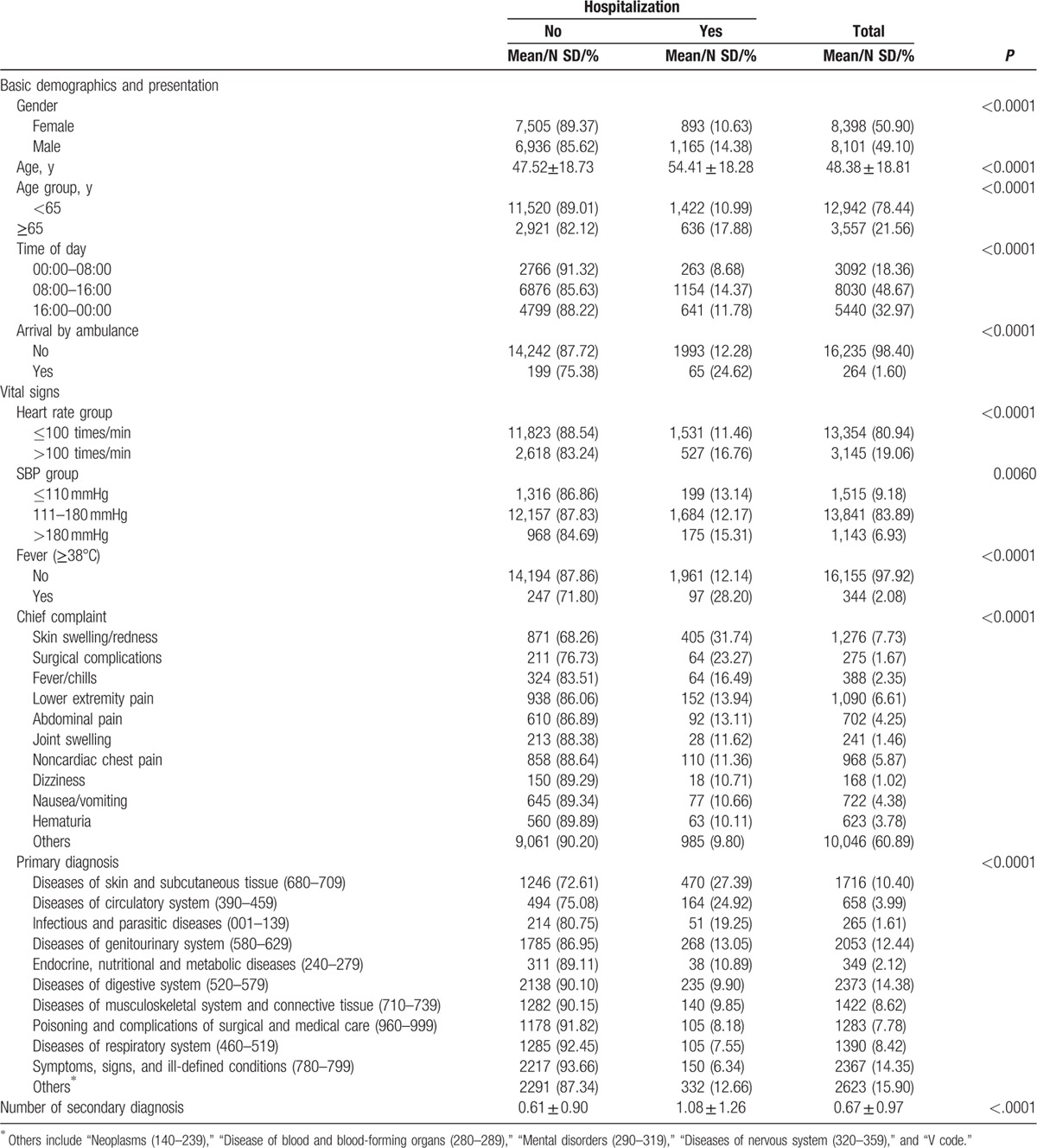
A total of 16,499 nonurgent patients (Levels 4 and 5) were extracted from 79,455 adult ED nontrauma patients in an ED during January 01–December 31, 2013. The overall hospitalization rate of the nonurgent patients was 12.47 % (2058/16,499). All study variables were found to have a statistically significant association with hospitalization. Among the basic demographics and presentation factors, the hospitalization rate of males (14.38%) and elderly (17.88%) were significantly higher than the other groups. Nonurgent patients who arrived at ED by ambulance (24.62%) also had a higher hospitalization rate. Reviewing the vital signs, those patients with higher heart rates, lower SBP, and fever were more likely to be admitted. Patients with skin swelling/redness (31.74%) or surgical complications (23.27%) had higher hospitalization rates. The top 10 reasons of adult nonurgent ED patients admitted to the hospital are listed in Table 1. These conditions accounted for over 80% of all admissions in our population. Disease of skin and subcutaneous tissue (27.39%) was the most common condition admitted followed by disease of circulatory system (24.92%); infectious and parasitic diseases (19.25%); disease of genitourinary system(13.05%); endocrine, nutritional and metabolic diseases(10.89%); disease of digestive system(9.90%); disease of musculoskeletal system and connective tissue(9.85%); poisoning and complications of surgical and medical care(8.18%); disease of respiratory systems(7.55%); and symptoms, signs, and ill-defined conditions(6.34%). Patients with more number of secondary diagnoses had a higher likelihood of hospitalization (Table 1).
Table 1.
The comparison of study variables between hospitalized and nonhospitalized non-urgent ED patients.
The top 10 secondary diagnoses of admitted nonurgent patients are listed in appendix A. The most frequently seen secondary diagnosis was endocrine, nutritional and metabolic diseases (12.22%) followed by disease of genitourinary system (10.19%), disease of circulatory system (10.10%), disease of digestive system (9.96%), neoplasms (6.04%), disease of musculoskeletal system and connective tissue (4.33%), disease of respiratory system (4.10%), mental disorders (1.26%), disease of nervous system (0.99%), and disease of blood and blood-forming organs (0.99%).
In the multiple logistic regression model, patients with characteristics of males (OR = 1.37; 95% confidence interval [CI] = 1.24–1.51), age more than 65 years (OR = 1.56; 95% CI = 1.39–1.74), arriving between 08:00 and 16:00 (OR = 1.53; 95% CI = 1.32–1.77), arriving by ambulance (OR = 2.40; 95% CI = 1.78–3.23), heart rate more than 100/min (OR = 1.47; 95% CI = 1.31–1.65), fever (OR = 2.73; 95% CI = 2.06–3.60), more number of secondary diagnosis (OR = 1.47; 95% CI = 1.41–1.54), and presenting chief complaint as skin swelling/redness (OR = 4.64; 95% CI = 3.45–6.24) or surgical complications (OR = 3.05; 95% CI = 2.06–4.53) were associated with higher likelihood of hospitalization (Table 2). The AUROC of predictive hospitalization, which calculated by combining factors in multiple logistic regression model into a scoring index was found to be 0.70 (Fig. 1).
Table 2.
A multiple logistic regression model for hospitalization of nonurgent ED patients.
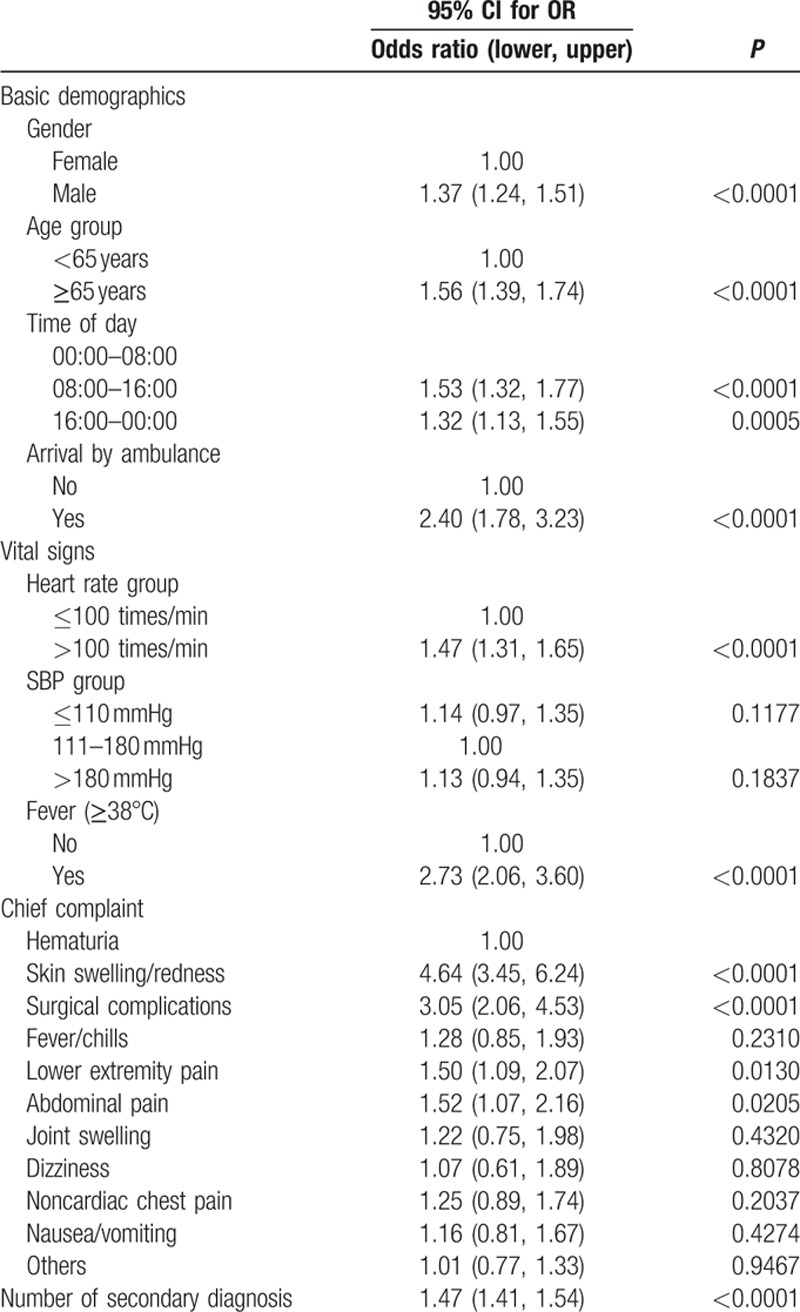
Figure 1.
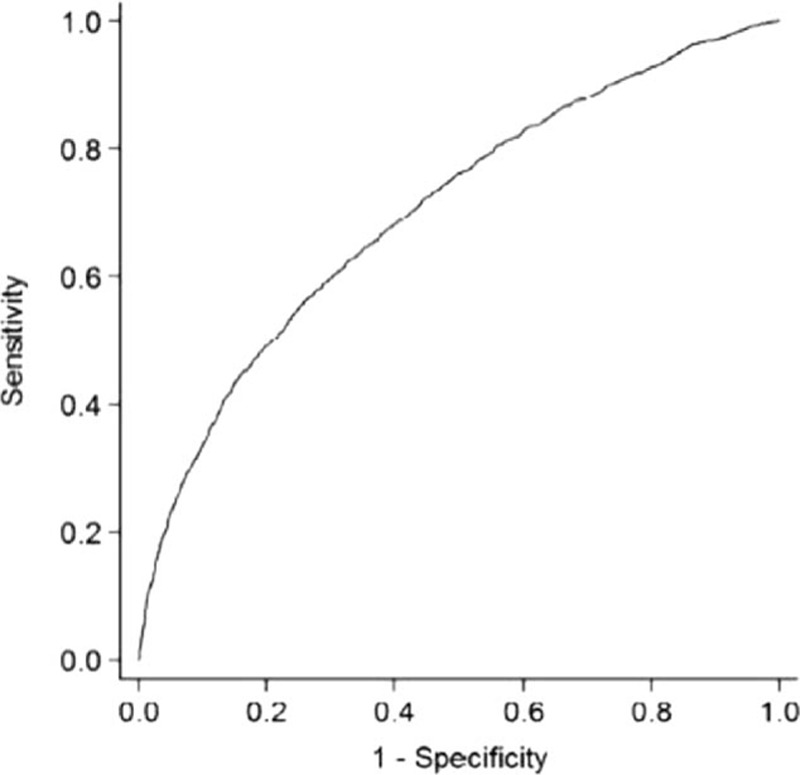
The predictability of score combining factors derived from multiple logistic regression to hospitalization (AUROC = 0.70).
4. Discussion
This study has identified that a significant number of nonurgent ED patients (Levels 4 and 5) in a five-level acuity triage system, TTAS, are still being admitted to hospital. The results are consistent with several previous studies providing further evidence that diverting non-urgent patients away from the ED may lead to denial or delay of appropriate care.[11,13,16,18]
It is important to emphasize that TTAS, similar to CTAS was developed to support triage nurses prioritize emergency patients based on presenting acuity or risk.[22] Both triage system effectively discriminates high, intermediate, and low acuity patients, and ensure the most needed patients to receive prompt treatments.[7,22] The high discriminant ability of these triage systems also allowed for better streaming of patients, optimizing patient, and provider resources placement, and to deliver the most appropriate care to the correspondent group of patient.[7,22] TTAS was not designed as a tool to triage nonurgent patient away from the ED.
Our study demonstrates that, male patients, older patients, patients with more secondary diagnoses, skin swelling/redness complaints, or with surgical complications, and patients with abnormal vital signs (tachycardia and fever) were more likely to be hospitalized. As TTAS was develop to prioritizes incoming patients at initial triage and identify the most seriously ill patients who cannot wait to be seen as TTAS 1, 2, or 3, patients with cutaneous problems might be initially assigned as nonurgent at triage. After examination by the physician, there might turn out to be severe skin infections that required intravenous antibiotics and required admission to hospital for treatment. On the other hand, patients with surgical complications would often return to ED early for evaluation if anything wrong happened. For example, a patient with vague abdominal pain (pain scale < 4) after laparotomy may be assigned as TTAS level 4, may later be proved to be mechanical ileus after serial examinations and then be admitted.
Older people are an increasing population in EDs in many countries.[23–27] They often present with atypical symptoms and signs and multiple comorbidities that complicate diagnosis and treatment.[25,27–29] Reports had shown that nonurgent elderly patients admitted to hospitals are characterized with very old age, male gender, low levels of education, widowhood, living alone, previous use of EDs or hospitals, and functional impairment.[30–32] In our series, elderly patients (≥65 years) accounted for 21.56% of nonurgent group and 17.88% of them were hospitalized comparing to 10.99% of younger group. These results are comparable to a study that examined predictors for hospitalization in a CTAS nonurgent group.[32] The authors had advocated to adopt age more than 65 years as modifies in CTAS in order to improve the discriminatory and predictive power to identify patients who require hospitalization.[32] In our studies, we also identified that elderly patients who arrived by ambulance had a higher admission rate, these findings were also comparable to previous studies.[20,33] Frailty may be an implication of such patient's manifestations. The characteristics of aging, comorbid status, and possible mobility problems (arriving by ambulance) among such patients are components of frailty.[34] It is suggested that applying frailty as a modifier in TTAS in order to reflect the severity and needs of ED interventions and the subsequent hospitalization care is appropriate in the future.
Our study showed that tachycardia (HR > 100) and fever of 38°C or more were associated with higher admission in non-urgent group. Although the TTAS hemodynamic criteria stated that, the patients could be assigned into level 3 if their vital signs were at the upper and lower ends of normals and were related to presenting complaint. However, based on our observation, patients with a slightly high body temperature (e.g., 38°C–39°C) or heart rate (e.g., 110 bpm) and no appearantly in distress conditions were assigned into nonurgent group. Our result stresses the importance of vital signs in predicting the subsequent hospitalization among nonurgent triaged patients. Triage nurses should be more concerned about the role of abnormal vital signs in the disease progression under different chief complaints. For instance, patients with a fever of 38°C or more under infectious etiologies could be adversely progressed over time, which can be considered upgraded.
This study has a number of limitations. First, the data were collected from a single medical center. Findings, such as admission rates and types of modifying features, may vary in regional or community ED settings. Second, cautiousness is suggested to generalize the results to trauma ED patients because we only collected nontrauma patients for the analyses in this study. Third, Taiwan has a universal national health insurance system allowing patients to access the health care facilities of their choosing. Different health care systems may pose diverse accessibility to the ED facilities. Forth, prospective validation of these findings is warranted.
5. Conclusion
Non-urgent patients might still be admitted for further care especially in male, the elderly, with more secondary diagnoses, abnormal vital signs, and presented with dermatologic complaints. Using the TTAS acuity level to identify patients for diversion away from the ED is unsafe and will lead to inappropriate refusal of care for many patients requiring hospital treatment.
Acknowledgments
The authors thank Professor M. J. Bullard for his advice and help in editing the manuscript. Special thanks for the statistical support from the Healthy Aging Research Center at Chang Gung University, Taiwan.
Supplementary Material
Footnotes
Abbreviations: CTAS = Canadian Triage and Acuity Scale, ED = emergency department, TTAS = Taiwan Triage and Acuity Scale.
C-JN and P-JL contributed equally to this article.
Funding/Support: This study was supported by a grant from the Taiwan Ministry of Health and Welfare (DOH-TD-M113-100004) and Ministry of Science and Technology, Taiwan (contract number MOST 103-2314-B-182A-019, NSC-101–2410-H-182-015, NSC-102-2410-H-182-010-MY2, NSC-103–2410-H-161-001 and NSC-104-2410-H-182–028-MY2) and the Healthy Aging Research Center of Chang Gung University (fund number EMRPD1B0351, EMRPD1C0301, EMRPD1D0911, EMRPD1E1691, and EMRPD1F0301).
The authors report no conflicts of interest.
Supplemental Digital Content is available for this article.
References
- 1.Afilalo J, Marinovich A, Afilalo M, et al. Nonurgent emergency department patient characteristics and barriers to primary care. Acad Emerg Med 2004; 11:1302–1310. [DOI] [PubMed] [Google Scholar]
- 2.Durand AC, Gentile S, Devictor B, et al. ED patients: how nonurgent are they? Systematic review of the emergency medicine literature. Am J Emerg Med 2011; 29:333–345. [DOI] [PubMed] [Google Scholar]
- 3.FitzGerald G, Jelinek GA, Scott D, et al. Emergency department triage revisited. Emerg Med J 2009; 27:86–92. [DOI] [PubMed] [Google Scholar]
- 4.Hoot NR, Aronsky D. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med 2008; 52:126–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cunningham PJ, Clancy CM, Cohen JW, et al. The use of hospital emergency departments for nonurgent health problems: a national perspective. Med Care Res Rev 1995; 52:453–474. [DOI] [PubMed] [Google Scholar]
- 6.Ng CJ, Hsu KH, Kuan JT, et al. Comparison between Canadian triage and acuity scale (CTAS) and Taiwan triage system (TTS) in emergency departments. J Formos Med Assoc 2010; 109:828–837. [DOI] [PubMed] [Google Scholar]
- 7.Ng CJ, Yen ZS, Tsai JC, et al. Validation of the Taiwan Triage and Acuity Scale: a new computerized five-level triage system. Emerg Med J 2010; 28:1026–1031. [DOI] [PubMed] [Google Scholar]
- 8.Derlet RW, Richards JR. Overcrowding in the nation's emergency departments: complex causes and disturbing effects. Ann Emerg Med 2000; 35:63–68. [DOI] [PubMed] [Google Scholar]
- 9.Lowe RA, Bindman AB, Ulrich SK, et al. Refusing care to emergency department of patients: evaluation of published triage guidelines. Ann Emerg Med 1994; 23:286–293. [DOI] [PubMed] [Google Scholar]
- 10.Baker DW, Stevens CD, Brook RH. Determinants of emergency department use by ambulatory patients at an urban public hospital. Ann Emerg Med 1995; 25:311–316. [DOI] [PubMed] [Google Scholar]
- 11.Young GP, Wagner MB, Kellermann AL, et al. Ambulatory visits to hospital emergency departments. Patterns and reasons for use. 24 Hours in the ED study group. JAMA 1996; 276:460–465. [DOI] [PubMed] [Google Scholar]
- 12.Kellermann AL. Nonurgent emergency department visits. Meeting an unmet need. JAMA 1994; 271:1953–1954. [PubMed] [Google Scholar]
- 13.Gill JM, Reese IV CL, Diamond JJ. Disagreement among health care professionals about the urgent care needs of emergency department patients. Ann Emerg Med 1996; 28:474–479. [DOI] [PubMed] [Google Scholar]
- 14.Sempere-Selva T, Peiró S, Sendra-Pina P, et al. Inappropriate use of an accident and emergency department: magnitude, associated factors, and reasons—an approach with explicit criteria. Ann Emerg Med 2001; 37:568–579. [DOI] [PubMed] [Google Scholar]
- 15.Field S, Lantz A. Emergency department use by CTAS Levels IV and V patients. Can J Emerg Med 2006; 8:317–322. [DOI] [PubMed] [Google Scholar]
- 16.Derlet RW, Kinser D, Ray L, et al. Prospective identification and triage of nonemergency patients out of an emergency department: a 5-year study. Ann Emerg Med 1995; 25:215–218. [DOI] [PubMed] [Google Scholar]
- 17.Birnbaum A, Gallagher J, Utkewicz M, et al. Failure to validate a predictive model for refusal of care to effect of low-complexity patients. Acad Emerg Med 1994; 1:213–217. [DOI] [PubMed] [Google Scholar]
- 18.Vertesi L. Does the Canadian Emergency Department Triage and Acuity Scale identify non-urgent patients who can be triaged away from the emergency department? Can J Emerg Med 2004; 6:337–342. [DOI] [PubMed] [Google Scholar]
- 19.Washington DL, Stevens CD, Shekelle PG, et al. Safely directing patients to appropriate levels of care: guideline-driven triage in the emergency service. Ann Emerg Med 2000; 36:15–22. [DOI] [PubMed] [Google Scholar]
- 20.Lin D, Worster A. Predictors of admission to hospital of patients triaged as nonurgent using the Canadian Triage and Acuity Scale. CJEM 2013; 15:353–358. [DOI] [PubMed] [Google Scholar]
- 21.Russ S, Jones I, Aronsky D, et al. Placing physician orders at triage: the effect on length of stay. Ann Emerg Med 2010; 56:27–33. [DOI] [PubMed] [Google Scholar]
- 22.Bullard MJ, Chan T, Brayman C, et al. Revisions to the Canadian Emergency Department Triage and Acuity Scale (CTAS) Guidelines. CJEM 2014; 16:1–5. [PubMed] [Google Scholar]
- 23.Baum SA, Rubenstein LZ. Old people in the emergency room: age-related differences in emergency department use and care. J Am Geriatr Soc 1987; 35:398–404. [DOI] [PubMed] [Google Scholar]
- 24.Samaras N, Chevalley T, Samaras D, et al. Older patients in the emergency department: a review. Ann Emerg Med 2010; 56:261–269. [DOI] [PubMed] [Google Scholar]
- 25.Aminzadeh F, Dalziel WB. Older adults in the emergency department: a systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Ann Emerg Med 2002; 39:238–247. [DOI] [PubMed] [Google Scholar]
- 26.Hu SC, Yen D, Yu YC, et al. Elderly use of the ED in an Asian metropolis. Am J Emerg Med 1999; 17:95–99. [DOI] [PubMed] [Google Scholar]
- 27.Salvi F, Morichi V, Grilli A, et al. The elderly in the emergency department: a critical review of problems and solutions. Intern Emerg Med 2007; 2:292–301. [DOI] [PubMed] [Google Scholar]
- 28.Rutschmann OT, Chevalley T, Zumwald C, et al. Pitfalls in the emergency department triage of frail elderly patients without specific complaints. Swiss Med Wkly 2005; 135:145–150. [DOI] [PubMed] [Google Scholar]
- 29.Grossmann FF, Zumbrunn T, Frauchiger A, et al. At risk of undertriage? Testing the performance and accuracy of the emergency severity index in older emergency department patients. Ann Emerg Med 2012; 60:317–325. [DOI] [PubMed] [Google Scholar]
- 30.Burns E. Older people in accident and emergency department. Age Ageing 2001; 30 suppl 3:3–6. [DOI] [PubMed] [Google Scholar]
- 31.McCusker J, Karp I, Cardin S, et al. Determinants of emergency department visits by older adults: a systematic review. Acad Emerg Med 2003; 10:1362–1370. [DOI] [PubMed] [Google Scholar]
- 32.Gregoratos G. Clinical manifestations of acute myocardial infarction in older patients. Am J Geriatr Cardiol 2001; 10:345–347. [DOI] [PubMed] [Google Scholar]
- 33.Sun Y, Heng BH, Tay SY, et al. Predicting hospital admissions at emergency department triage using routine administrative data. Acad Emerg Med 2011; 18:844–850. [DOI] [PubMed] [Google Scholar]
- 34.Xue Q-L. The frailty syndrome: definition and natural history. Clin Geriatr Med 2011; 27:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


