Abstract
Objective. To determine if exposure to an intervention course impacts pharmacy students’ mental health stigma (MHS) and mental health knowledge (MHK).
Methods. A one-group pre/posttest intervention study of third-year pharmacy students (N=120) was conducted. Dependent variables were subdomains of MHS (recovery, safety, disclosure, separation, comfort) which were measured on a 5-point Likert scale (1=strongly disagree; 5=strongly agree). Mental health knowledge was measured with 10 true/false questions. The 2.5-hour intervention included presentations, videos, discussions, and active-learning exercises. Pre/posttests were administered, and data were analyzed using paired t tests and McNemar’s tests.
Results. Among responding students (n=88; 73.3% response rate), the following stigma subdomains significantly decreased after the intervention for depression and schizophrenia: recovery, safety, separation, and comfort. Mental health knowledge scores significantly increased from 5.9 (1.5) to 6.8 (1.5).
Conclusion. Pharmacy students’ MHS and MHK related to depression and schizophrenia can be improved through a brief and interactive anti-stigma intervention.
Keywords: stigma, mental health, intervention, pharmacy student, social distance
INTRODUCTION
The World Health Organization (WHO) estimates that 450 million people around the world have a mental disorder.1 In the United States, mental illness statistics are also alarming. It is estimated that 50% of Americans will suffer from mental illness in their lifetime,2 and one in four Americans will battle a mental illness in a given year.3 The staggering presence of mental illness in the United States and other populations indicate that there is a high likelihood of personally experiencing mental illness or knowing someone with a mental illness.
Key approaches to addressing mental illness include the use of effective behavioral therapies and medications. For example, psychotherapy, family, cognitive-behavioral, electroconvulsive therapy, and medications have been effective in treating mental illness.4 Despite the availability of effective treatment, research indicates that patients with mental illness are less likely to seek treatment and that more than 60% of people living with mental illness do not receive treatment.5 In addition, studies show that medication adherence is suboptimal, with rates ranging from 20% to 70%.6,7 As medication experts, pharmacists can play a key role in assisting patients with medication-related education and therapy management, especially medication adherence.
Stigmatizing attitudes may serve as a factor in patient medication nonadherence.8,9 According to Link and Phelan, stigma exists “when elements of labeling, stereotyping, separation, status loss, and discrimination co-occur in a power situation...”10 The process of mental illness stigma first occurs when an individual identifies and “labels” the difference between themselves and a person with a mental illness. Negative attributes (ie, stereotypes) are then attached to this acknowledged difference. The individual then develops an “us” vs “them” outlook that causes “separation.” Lastly, those with mental illness experience status loss and discrimination. Through this process of stigma, attitudes can negatively impact care seeking, as well as long-term treatment participation (eg, medication adherence) among mentally ill patients.8,9,11
Pharmacists report positive attitudes regarding providing mental health medication information, discussing options for managing adverse effects, and assessing patient knowledge and understanding of their disease state.12,13 Yet, despite positive attitudes towards providing pharmacy services to patients with mental illness, pharmacists report low rates of actual service provision.12,14-16 Pharmacists are significantly more willing to provide pharmacy services to patients with physical illness conditions (eg, asthma, cardiovascular disease) than those with mental illness,12,14-16 which may be an indicator of mental health stigma (MHS). In addition, studies have shown that pharmacists have high levels of social distance (ie, unwillingness to interact) and possess stereotypical beliefs about patients with mental illness. Furthermore, pharmacists with more negative attitudes are less willing to provide pharmacy services to patients with depression or schizophrenia.13,17,18
While stigma is related to mental health counseling and service provision, lack of training or education is also a barrier.12,17 In pharmacy, a limited body of research highlights the benefit of training programs for reducing social distance and improving attitudes about mental illness, which, in turn, increases counseling frequency and enhances the quality of care provided to patients living with mental illness.19-25 Pharmacy students report higher levels of stigmatization than pharmacists regarding schizophrenia.24,26,27 Because pharmacy students are the next generation of pharmacists, it is important to examine their perceptions regarding stigma towards patients with mental illness. Although there is evidence supporting intervention success in decreasing stigma among pharmacy students in other countries, the literature lacks generalizability to United States pharmacy students. Additionally, the few studies conducted in the United States used elective courses where enrollment is voluntary and used consumer educators as part of the interventions, neither of which may be feasible if resources are limited. Finally, stigma is multifaceted and can exist when elements of labeling, stereotyping, separation, status loss, and discrimination exist. Pharmacy literature either measures stigma as social distance or separation alone or as a general stigma construct that does not represent subdomains as described by Link and Phelan.10 It is important to explore additional stigma subdomains so that more targeted interventions can be developed.
While several studies measure changes in stigma, attitudes toward mental illness, and attitudes toward providing pharmacy services,22,24,25,28 few examine mental health knowledge (MHK) among pharmacy students. Among published studies, MHK was operationalized in various ways including focusing on identifying medications or specific mental illnesses and recognizing recommended interventions.24,29 These knowledge studies are limited as they do not include other important issues such as disease prevalence, mental illness symptomology, or information regarding untreated mental illness outcomes, all of which are important when treating these patients.
The study objectives were to determine: if exposure to an intervention course impacts pharmacy students’ stigma towards depression and schizophrenia (using multiple subdomains); if pharmacy students’ change in schizophrenia stigma (from pre to post intervention) will differ from their change in depression stigma; and if exposure to an intervention course impacts pharmacy students’ mental health knowledge.
METHODS
To assess pharmacy students’ training needs for addressing MHS and MHK, a 1-group pre/post training program was developed and implemented at the University of Texas at Austin College of Pharmacy. All third-year pharmacy students (N=120) enrolled in a 3-credit hour pharmacoeconomics course during spring 2014 participated in the intervention program. Student pharmacists enrolled in this course were chosen because they had already completed their mental health pharmacotherapy module.
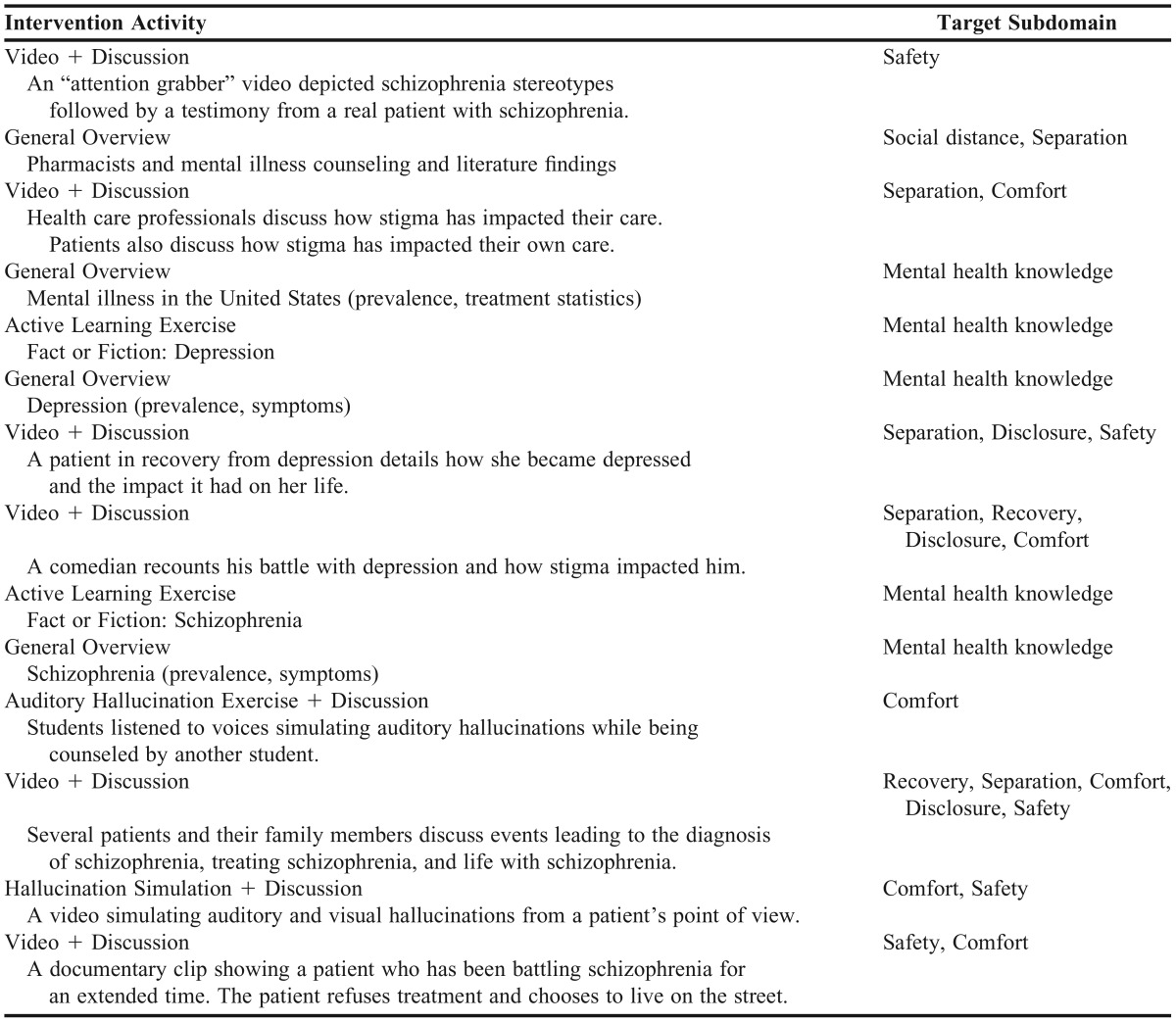
The intervention was conducted over two class periods (2.5 hours total) and included presentations, videos, discussion, and active-learning exercises (Table 1). The presentations focused on prevalence data, signs and symptoms of depression and schizophrenia, a summary of pharmacy and mental health literature, and several video clips of health care providers and patients discussing stigma and their lived experiences in delivering and receiving mental health care. Immediately after each video, participants were asked to reflect and share their comments in a class discussion led by the primary researcher. Active-learning exercises were designed to engage participants and encourage reflection. For example, in one active-learning exercise titled “Fact or Fiction,” the primary researcher read a statement, and participants were asked to hold up a sign that read “fact” or “fiction.” When a statement caused disagreement, participants were asked to discuss with their peers and then the researcher moderated a class discussion. Intervention materials were created by using available literature and searching the Internet for videos and active-learning exercises. The fact or fiction exercise was developed to stimulate discussion among students. Videos were identified by the researchers to address specific stigma subdomains.
Table 1.
Anti-Stigma Intervention and Target Subdomain
An anonymous survey was administered immediately before and after the intervention. Students created a code based on an algorithm to facilitate matching of pre/posttest responses, while maintaining anonymity. The survey focused on depression and schizophrenia because these mental illnesses had been examined the most in the literature. Additionally, depression and schizophrenia were the focus of this study because they exemplified the range of MHS. Society is more familiar with depression, and they tend to stigmatize schizophrenia more.30-32 Beliefs and perceptions regarding MHS were operationalized based on the following subdomains: recovery (possibility of recovering from a mental illness and living a fulfilling life, 5 items); safety (posing a danger to others, 4 items); disclosure (willingness to disclose a personal mental illness, 3 items); separation (willingness to interact in social situations with a person living with mental illness, 10 items); and comfort (relating to or feeling comfortable with a person with mental illness, 5 items). Separation was measured using the 8-item Social Distance Scale (SDS), which is valid and reliable, in addition to two items derived from the literature.33-35 Other subdomain measures were adapted from previously validated surveys14,24,36-40 or were generated by the authors based on the literature. All stigma subdomain items (N=27) were measured on a 5-point Likert scale [strongly disagree (1) to strongly agree (5)], with higher numbers representing more negative attitudes. Mental health knowledge included content regarding prevalence of mental illness and the symptomology of mental disease and it was measured using 10 true/false statements. Information regarding demographics (ie, age, gender, race, education) and mental health issues (ie, personal history with mental illness and interest in psychiatric clinical rotations) was collected. The survey was pilot-tested prior to the intervention with four health outcomes graduate students and two faculty members. Minimal wording changes were made as a result of the pilot-test.
The study was approved by The University of Texas at Austin Institutional Review Board. Data were analyzed using SAS, v9.3 (SAS Institute Inc., Cary North Carolina). Descriptive statistics were computed for all variables. Paired t tests were used to compare participant Likert scale MHS subdomain mean scores before and after the intervention. McNemar’s tests were used to compare frequencies of correctly answered MHK statements before and after the intervention.
RESULTS
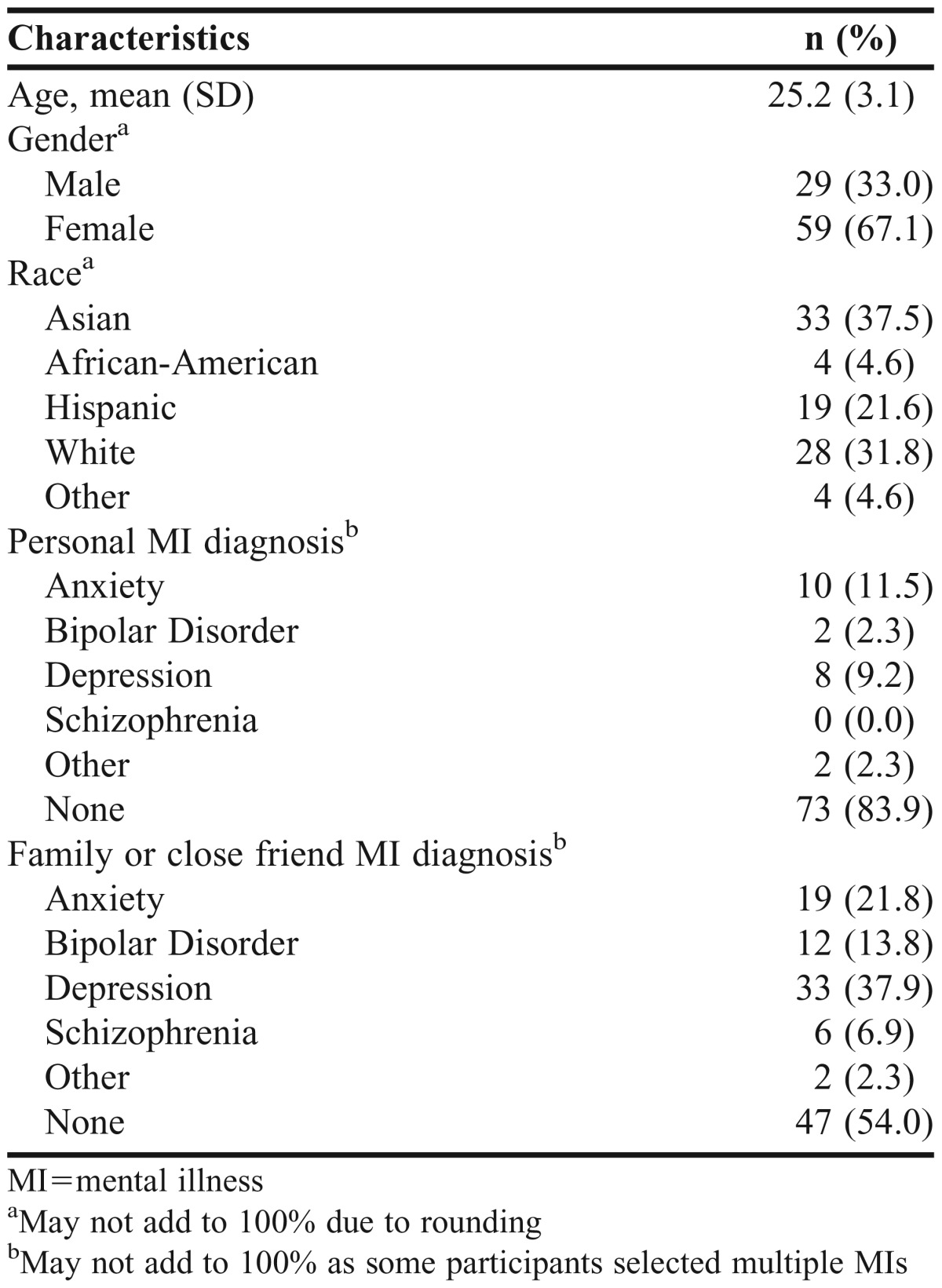
Of the 120 students who participated in the first day of the intervention, 120 students completed the pretest survey. Of these 120 students, 88 students completed the second day of the intervention and posttest survey (73.3% response rate). Results presented below include students who completed both surveys. The demographic characteristics of participants are detailed in Table 2. Students were 25.2 (SD=3.1) years old (range 22-39), primarily female (67.1%), and the majority were either Asian (37.5%) or White (31.8%). Of the students who completed both surveys, 11.5% reported being diagnosed with anxiety, 9.2% with depression, 2.3% with bipolar disorder, and 2.3% with some other mental illness. Forty-six percent of the students had a family member or close friend diagnosed with a mental illness.
Table 2.
Demographic Characteristics of Participants (N=88)
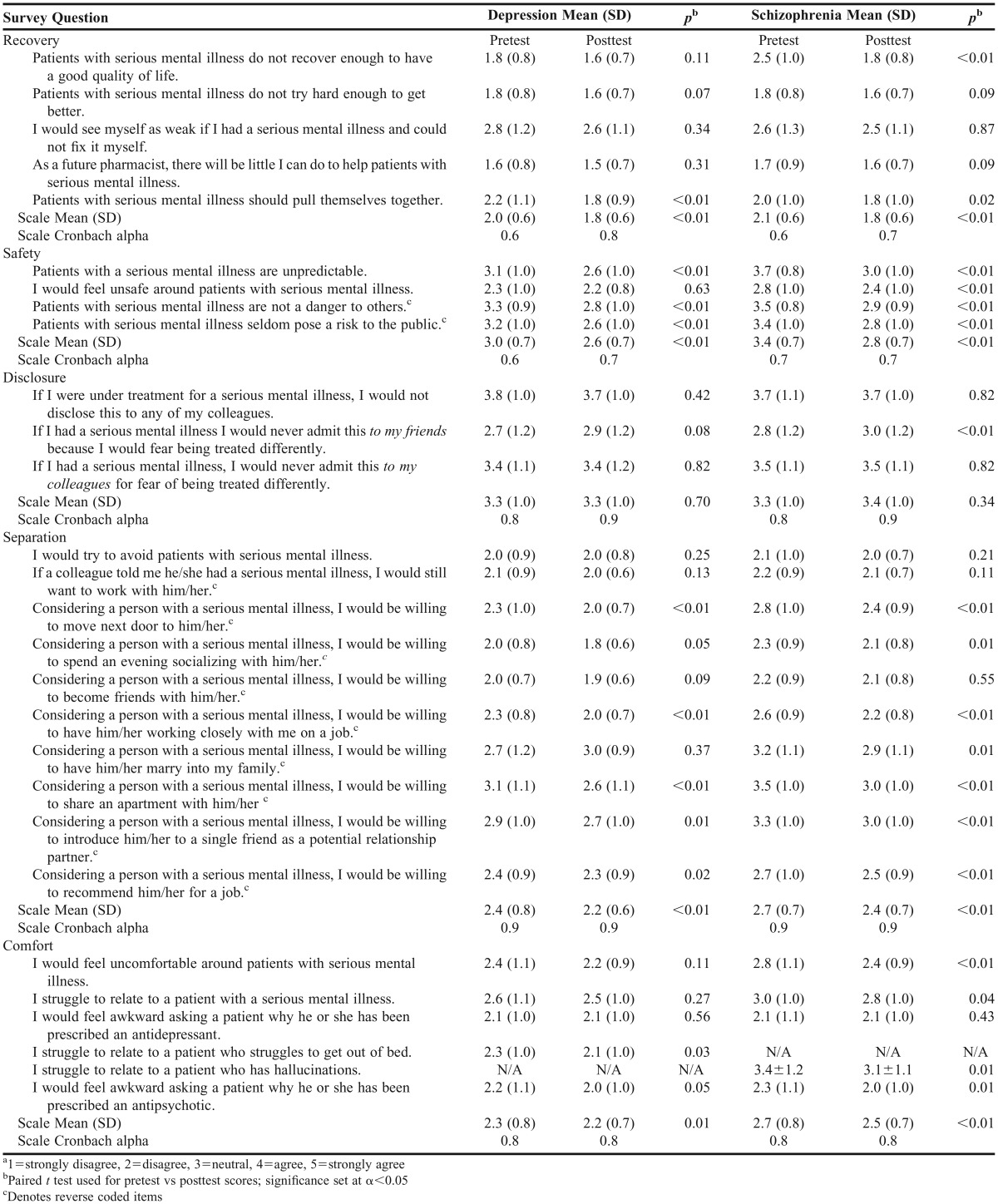
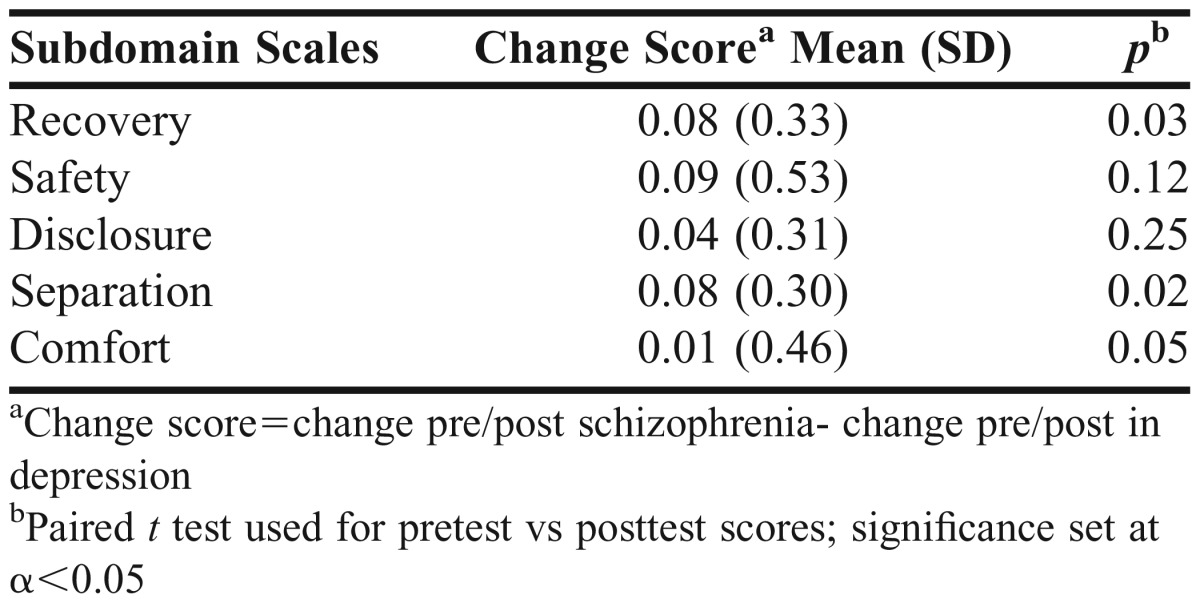
Overall, pharmacy student stigma toward depression and schizophrenia decreased after the intervention (Table 3). Students had significantly less stigma with the following subdomains: recovery, safety, separation, and comfort stigma (p<0.01). However, no differences were observed with the disclosure subdomain. Furthermore, when comparing schizophrenia and depression, there were significant differences in change scores before and after the intervention. Recovery and separation change scores for schizophrenia were significantly greater (ie, larger decreases in stigma) than the respective change scores for depression (Table 4).
Table 3.
Comparison of Mean Pretest and Posttest Scores for Depression and Schizophreniaa (N=88)
Table 4.
Change Scores between Depression and Schizophrenia for Stigma Subdomain Scales (N=88)
Overall, students disagreed (recovery scale mean range 1.8 to 2.1 for both pretest and posttest scores) that patients were unable to recover from a mental illness. Students had more negative perceptions about recovery and quality of life for patients with schizophrenia than for those with depression at baseline (Item 1: depression vs schizophrenia means 1.8 vs 2.5, respectively). However, after the intervention, student perceptions were similar (depression vs schizophrenia means 1.6 vs 1.8, respectively). Students’ stigmatizing attitudes were lower (more positive) for the recovery subdomain compared to all other subdomains. Scale reliability ranged from 0.6 to 0.8.
Of the five stigma subdomains, the largest change from before to after the intervention occurred with safety (scale mean change: depression, 0.4; schizophrenia, 0.6, p<0.01). Overall at baseline, students were “neutral” regarding their views that patients with mental illness are unsafe. Also, students had more negative perceptions of safety regarding schizophrenia than with depression (scale means: 3.4 vs 3.0, respectively). After the intervention, students felt more disagreeable about patients being unsafe. Scale reliability ranged from 0.6 to 0.7.
Overall, students remained neutral towards disclosing depression or schizophrenia to others from before to after the intervention (scale mean range: 3.3 to 3.4). Item 11, which focused on disclosing mental illness to friends, had the lowest mean score for both schizophrenia and depression when compared to the other two items in the disclosure subdomain that focused on disclosing to colleagues. This lowest mean score (Item 11) means that students felt more comfortable disclosing a mental illness to their friends than to their colleagues (Items 10 and 12). Additionally, Item 11 for schizophrenia was the only item that had a significant change, which was an increase (ie, students were less comfortable disclosing a mental illness to friends) after the intervention (preintervention: 2.8; postintervention: 3.0, p=0.01). Scale reliability ranged from 0.8 to 0.9.
At baseline, students disagreed overall that they desired separation from people with depression and were neutral towards separation from people with schizophrenia (scale means: 2.4 and 2.7, respectively). After the intervention, students’ were less disagreeable, meaning that they embraced closer interactions with patients with depression and schizophrenia (scale means: 2.2 and 2.4, respectively; p<0.01). In addition, students desired more separation from patients with schizophrenia than from those with depression. For both depression and schizophrenia, students desired more separation from people with mental illness in situations involving marrying into their family (Item 19), sharing an apartment (Item 20), and introducing them to single friends for romantic relationships (Item 20), before and after the intervention. Scale reliability was 0.9.
Overall, at baseline students disagreed that they were uncomfortable around patients with depression, while they were neutral regarding comfort around patients with schizophrenia (scale means 2.3 and 2.7, respectively). The only significant change from before to after the intervention in the comfort subdomain involved depression, where students were better able to relate to patients who struggle to get out of bed [Item 26 (pre: 2.3; post: 2.1)]. Students disagreed that they would feel awkward asking a patient why they were prescribed an antidepressant for both depression and schizophrenia (pre: 2.1 and 2.1, respectively). These scores did not change after the intervention for depression or schizophrenia. Students also disagreed that they would feel awkward asking a patient why he or she was prescribed an antipsychotic for both depression and schizophrenia (post 2.0 and 2.0, respectively). Scale reliability was 0.8.
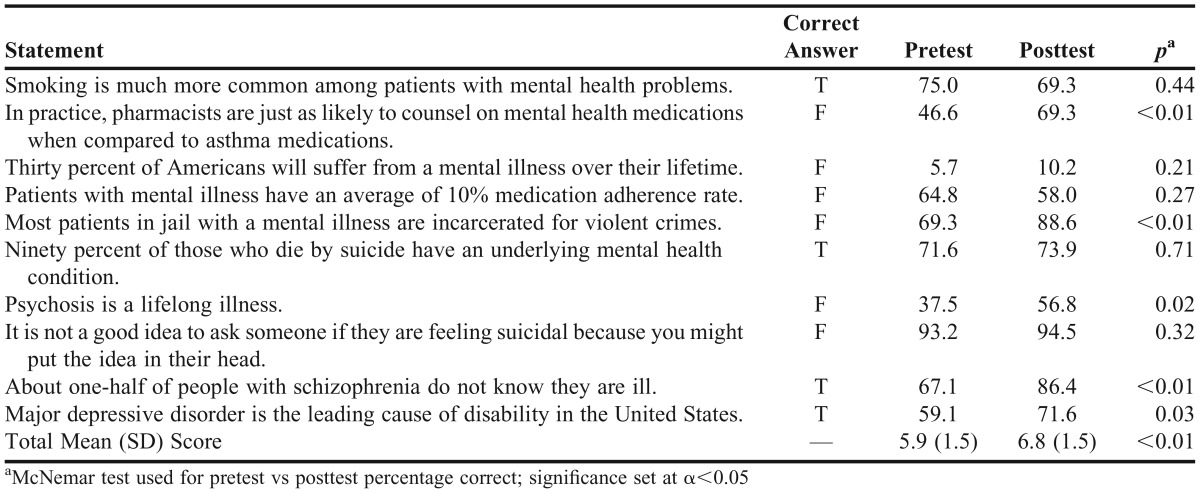
Overall, MHK significantly increased after the intervention (Table 5). The mean number of correct responses increased from 5.9 (1.5) preintervention to 6.8 (1.5) postintervention (p<0.01). McNemar’s test revealed that the percentage of correct responses after the intervention significantly differed (p<0.05) for five of the 10 items that related to prevalence of pharmacy counseling, outcomes associated with mental illness, and the symptomology of mental illness. Improvements for those five questions ranged from 19 percentage points to 23 percentage points.
Table 5.
Percentage of Correct Responses to Mental Health Knowledge Statements (N=88)
DISCUSSION
This study provided evidence that a brief anti-stigma intervention was effective in reducing MHS and increasing MHK among third-year pharmacy students. MHS subdomains of recovery, safety, separation, and comfort each decreased from before to after the intervention for depression and schizophrenia. In addition, pharmacy students reported increased MHK regarding prevalence of mental illness counseling, outcomes and symptomology. One important finding was that our brief intervention was successful in changing perceptions of a heavily stigmatized mental disorder, schzopherenia, which was illustrated by significant reductions in stigma recovery and separation subdomains, compared to depression.
When comparing changes in stigma subdomains from before to after the intervention, safety-related concerns were particularly reduced, demonstrated by greater mean changes. This may indicate that safety issues play a major role in stigma associated with people living with mental illness. These finding seem plausible, as fears of danger and unpredictability are common stereotypes associated with those living with mental illness.41,42 In addition, these stigmatizing attitudes, more predominantly with schizophrenia, have been linked to media influence.43,44 Knowing this, the intervention began with a stereotypical video depicting a preview for a horror movie titled “Schizo.” The clip ends with a man having tea with a friend and explains that he has schizophrenia and that there is nothing scary about him. The purpose of this video was to encourage students to reflect on their own personal biases.
Out of the four items in the safety domain, Item 7, which states, “I would feel unsafe around patients with serious mental illness,” was the only item stated in first person and it had the smallest change from before to after the intervention. Also, this item had the lowest mean score on the pretest and posttest for depression and schizophrenia. This means that students reported lower stigmatization when the statement reflected a personal element (ie, “I would feel…”) vs more general (ie, “Patients with serious mental illness are…”). This may expose an interesting aspect of assessing stigma. It is possible that students’ perceptions of mental illness changed specifically when expressing their own feelings as opposed to perceptions regarding general statements. Perhaps the use of personal pronouns may have influenced students to respond with social desirability, thus not reflecting how they truly feel, but with a politically correct response.
Further review of stigma subdomains indicated that, similar to preintervention findings for safety, students also desired more separation from patients living with schizophrenia compared to those living with depression. Congruent with previous studies,22,24,25,28,45,46 our study showed significant decreases in separation stigma postintervention. Higher scores (more stigmatizing attitudes) were associated with more personal social relationships such as marriage or sharing living space as opposed to lower scores (less stigmatizing) for less personal social relationships such as being a coworker or living next door. Although for most of the items, students’ stigma levels decreased significantly, items associated with more personal social relationships remained higher postintervention. This may indicate that the intervention was unable to fully influence stigma regarding highly personal and/or close relationships.
The recovery subdomain generally had the lowest scale means compared to other stigma subdomains, indicating that students had less stigmatizing views towards recovery of people living with depression and schizophrenia. Students viewed schizophrenia as a disease that significantly impacted quality of life compared to depression prior to the intervention. However, after the intervention, students’ perceptions regarding quality of life for both disease states were more similar. This may serve as a motivator for future pharmacists to emphasize treatment adherence, especially with medications.
Student’s expressed feeling more comfortable around patients living with depression compared to those living with schizophrenia. After the intervention, students were better able to relate to a patient living with depression who struggles to get out of bed. This is a particularly interesting finding because although students are more exposed to depression in general, they may not be exposed to lived experiences of the illness, which was depicted through video clips during the intervention. This highlights the importance of including this element in interventions focusing on mental illness. General disease knowledge or pharmacotherapy knowledge of depression and its signs and symptoms does not necessarily translate into understanding, relating to, or empathizing with people living with mental illness.
Items focusing on students’ comfort (ie, items 25 and 28) with inquiring why a patient was prescribed an antidepressant or antipsychotic medication, respectively, revealed subtle, but interesting findings. Whether an antidepressant medication was used for depression or schizophrenia, or an antipsychotic was used for depression, students expressed similar levels of comfort. However, when an antipsychotic was used to treat schizophrenia, students had a significantly lower level of comfort. These findings highlight that there is something unique, not about antipsychotic use (because of similar findings with its use and antidepressant use in depression), but about antipsychotic use in patients with schizophrenia. Student’s familiarity with depression as a disease state is perhaps strong enough to overcome any discomfort associated with antipsychotic medications. After the intervention, the level of comfort was similar for both medication categories for depression and schizophrenia. This revealed that although students had more stigmatizing attitudes towards schizophrenia and schizophrenia-related medications, these attitudes were improved through the intervention.
While improvements in recovery, safety, separation, and comfort stigma were observed, disclosure stigma did not change. In this study, disclosure was operationalized as one’s willingness to share personal mental illness with a colleague or friend. Pharmacy students’ more negative disclosure attitudes from before to after the intervention highlight the existence of shame or embarrassment that students may attach to mental illness, despite having a better understanding of illnesses and patients’ lived experiences. This finding is particularly interesting because one could argue that, if we have positive attitudes about mental illness, we should be more willing to disclose personal information about it. Another viewpoint is that disclosure depends more on one’s perception of others’ stigma and less on one’s own attitudes. Social comparison theory suggests that people form their opinions and attitudes by comparing them to other significant people, and, if their attitudes are different, they are likely to align more with the attitudes of the significant group of people.47 Rickles et al explored social comparison theory among pharmacists and found that pharmacists perceived themselves as having less stigmatizing attitudes towards people with depression and schizophrenia than other pharmacists.17 For our study, despite having positive attitudes toward a mental illness, participants’ fear that others they consider important have negative attitudes may discourage them from disclosing. More research is needed to explore the relationship between anti-stigma interventions and disclosure.
There is growing body of literature that supports the use of consumer educators (ie, patients with the disease state of interest) in pharmacy curricula and interventions. The addition of consumer educators to pharmacy training significantly improves pharmacy student attitudes towards mental illness above standardized pharmacy mental health training.22,25,48 Nguyen et al compared a face-to-face consumer educator intervention with film based interventions and found that both interventions had an equally positive impact on key items relating to MHS.46 The current study showed significant improvements in stigma perceptions without the use of consumer educators, but through role-playing, active-learning exercises, and patient videos. In fact, our study had similar findings to those of Nguyen et al’s46 when comparing safety and recovery questions. This suggests that our study’s intervention without consumer educators produced similar results to a consumer educator intervention. Comparable outcomes between consumer educator interventions and our study may suggest that helping students connect abstract concepts (eg, stigma related to mental illness) to a lived experience is more important than the mode by which it occurs. The ability to decrease pharmacy student MHS through a 2.5-hour intervention using video, role-playing, and active-learning exercises may be preferable for colleges and schools of pharmacy that do not have access to consumer educators because of geographical location, financial resources, lack of trained consumer educators, or scheduling difficulties. Additionally, this intervention may be of interest to schools of pharmacy as it addresses several of the Center for the Advancement of Pharmacy Education (CAPE) 2013 Outcomes.49 For example, under domain 4, “Personal and Professional Development,” subdomain 1 calls for self-awareness in which students “examine and reflect on personal knowledge, skills, abilities, beliefs, biases, motivation, and emotions that could enhance or limit personal and professional growth.” In another example, the sixth subdomain communication, under domain 3 “Approach to Practice and Care,” calls for students to “effectively communicate verbally and nonverbally when interacting with an individual, group, or organization.”
Mental health knowledge significantly improved after the intervention. However, this improvement should be considered in light of scale reliability issues. Items related to prevalence of pharmacy mental illness counseling, outcomes, and symptomology significantly improved. Students were unaware that pharmacists were less likely to counsel on mental health medications than on other disease states. Raising awareness of a problem is an important step in inspiring and effecting change. In terms of symptomatology, pharmacy students recognized that psychosis is not a lifelong illness and that some individuals living with schizophrenia do not know they are ill. This significant increase in the percentage of correct responses highlights the value of exposing students to the lived experiences, including examples of patients who have recovered. Simply providing a list of symptoms and definitions may not accurately reflect symptoms in real life.
The results from this study should be viewed in light of several limitations. First, the MHK and several MHS subdomain scale reliabilities were suboptimal. This may have occurred because the MHK construct content was not effectively addressed in the intervention and some of the MHS subdomains were newly created. More refined scales would yield better reliability. Another potential limitation is that the posttest was administered immediately after the intervention. Thus, the impact of the intervention can not be extrapolated to a longer follow up period. Although intervention effects in pharmacy students can last for up to 12 months,23 more research is needed to determine longitudinal impact. Additionally, social desirability may have been present because of the self-report and sensitive nature of the study. However, students generated a unique code, which rendered the survey anonymous, thus limiting the impact of socially desirable responses. Finally, the results from this study may have limited generalizability to other schools of pharmacy or to students outside of the third year.
CONCLUSION
Implementing brief and interactive mental health training programs that incorporate both didactic and media-based teaching approaches for future pharmacists may be a useful method in increasing MHK and diminishing MHS. Additionally, individually measuring MHS subdomains allow for a deeper understanding of what drives attitudes towards mental illness and for the opportunity to tailor future interventions to address specific needs.
ACKNOWLEDGMENTS
The authors would like to thank Dr. Karen Rascati for allowing us to use her course to deliver and test the intervention. We would also like to express our appreciation to the P3 students who participated.
REFERENCES
- 1.World Health Organization. Mental health: Strenthening our response. WHO Media centre. 2010; updated 2016. http://www.who.int/mediacentre/factsheets/fs220/en/. Accessed November 19, 2013.
- 2.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stern TA, Rosenbaum JF, Fava M, Biederman J, Rauch SL. Massachusetts General Hospital Comprehensive Clinical Psychiatry. Philadelphia, PA: Elsevier Health Sciences; 2008. [Google Scholar]
- 5.Substance Abuse and Mental Health Services Administration. Mental Health, United States, 2010. 9th Ed. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012. [PubMed] [Google Scholar]
- 6.Velligan DI, Weiden PJ, Sajatovic M, et al. The expert consensus guideline series: adherence problems in patients with serious and persistent mental illness. J Clin Psychiatry. 2009;70(Suppl 4):1–46. [PubMed] [Google Scholar]
- 7.Julius RJ, Novitsky MA, Jr, Dubin WR. Medication adherence: a review of the literature and implications for clinical practice. J Psychiatr Pract. 2009;15(1):34–44. doi: 10.1097/01.pra.0000344917.43780.77. [DOI] [PubMed] [Google Scholar]
- 8.Sirey JA, Bruce ML, Alexopoulos GS, et al. Perceived stigma as a predictor of treatment discontinuation in young and older outpatients with depression. Am J Psychiatry. 2001;158(3):479–481. doi: 10.1176/appi.ajp.158.3.479. [DOI] [PubMed] [Google Scholar]
- 9.Kikkert MJ, Schene AH, Koeter MW, et al. Medication adherence in schizophrenia: exploring patients’, carers’ and professionals’ views. Schizophr Bull. 2006;32(4):786–794. doi: 10.1093/schbul/sbl011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. 2001;27(1):363–385. [Google Scholar]
- 11.Clement S, Schauman O, Graham T, et al. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med. 2014;45(1):11–27. doi: 10.1017/S0033291714000129. [DOI] [PubMed] [Google Scholar]
- 12.Scheerder G, De Coster I, Van Audenhove C. Pharmacists’ role in depression care: a survey of attitudes, current practices, and barriers. Psychiatr Serv. 2008;59(10):1155–1160. doi: 10.1176/ps.2008.59.10.1155. [DOI] [PubMed] [Google Scholar]
- 13.Liekens S, Smits T, Laekeman G, Foulon V. Factors determining social distance toward people with depression among community pharmacists. Eur Psychiatry. 2012;27(7):528–535. doi: 10.1016/j.eurpsy.2010.12.009. [DOI] [PubMed] [Google Scholar]
- 14.Cannon-Breland ML, Westrick SC, Kavookjian J, Berger BA, Shannon DM, Lorenz RA. Pharmacist self-reported antidepressant medication counseling. J Am Pharm Assoc. 2013;53(4):390–399. doi: 10.1331/JAPhA.2013.12112. [DOI] [PubMed] [Google Scholar]
- 15.Phokeo V, Sproule B, Raman-Wilms L. Community pharmacists’ attitudes toward and professional interactions with users of psychiatric medication. Psychiatr Serv. 2004;55(12):1434–1436. doi: 10.1176/appi.ps.55.12.1434. [DOI] [PubMed] [Google Scholar]
- 16.Liekens S, Smits T, Laekeman G, Foulon V. Pharmaceutical care for people with depression: Belgian pharmacists’ attitudes and perceived barriers. Int J Clin Pharm. 2012;34(3):452–459. doi: 10.1007/s11096-012-9628-0. [DOI] [PubMed] [Google Scholar]
- 17.Rickles NM, Dube GL, McCarter A, Olshan JS. Relationship between attitudes toward mental illness and provision of pharmacy services. J Am Pharm Assoc. 2010;50(6):704–713. doi: 10.1331/JAPhA.2010.09042. [DOI] [PubMed] [Google Scholar]
- 18.O’Reilly CL, Bell JS, Kelly PJ, Chen TF. Exploring the relationship between mental health stigma, knowledge and provision of pharmacy services for consumers with schizophrenia. Res Social Adm Pharm. 2013;11(3):e101–e109. doi: 10.1016/j.sapharm.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 19.Bell JS, Whitehead P, Aslani P, Sacker S, Chen TF. Design and implementation of an educational partnership between community pharmacists and consumer educators in mental health care. Am J Pharm Educ. 2006;70(2):Article 28. doi: 10.5688/aj700228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liekens S, Vandael E, Roter D, et al. Impact of training on pharmacists’ counseling of patients starting antidepressant therapy. Patient Educ Couns. 2014;94(1):110–115. doi: 10.1016/j.pec.2013.09.023. [DOI] [PubMed] [Google Scholar]
- 21.Liekens S, Smits T, Laekeman G, Foulon V. A depression training session with consumer educators to reduce stigmatizing views and improve pharmacists’ depression care attitudes and practices. Am J Pharm Educ. 2013;77(6):Article 120. doi: 10.5688/ajpe776120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bell JS, Johns R, Rose G, Chen TF. A comparative study of consumer participation in mental health pharmacy education. Ann Pharmacother. 2006;40(10):1759–1765. doi: 10.1345/aph.1H163. [DOI] [PubMed] [Google Scholar]
- 23.O’Reilly CL, Bell JS, Chen TF. Consumer-led mental health education for pharmacy students. Am J Pharm Educ. 2010;74(9):Article 167. doi: 10.5688/aj7409167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.O’Reilly CL, Bell JS, Kelly PJ, Chen TF. Impact of mental health first aid training on pharmacy students’ knowledge, attitudes and self-reported behaviour: a controlled trial. Aust N Z J Psychiatry. 2011;45(7):549–557. doi: 10.3109/00048674.2011.585454. [DOI] [PubMed] [Google Scholar]
- 25.Gable KN, Muhlstadt KL, Celio MA. A mental health elective to improve pharmacy students’ perspectives on mental illness. Am J Pharm Educ. 2011;75(2):Article 34. doi: 10.5688/ajpe75234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bell J, Aaltonen S, Airaksinen MS, et al. Determinants of mental health stigma among pharmacy students in Australia, Belgium, Estonia, Finland, India and Latvia. Int J Soc Psychiatry. 2010;56(1):3–14. doi: 10.1177/0020764008097621. [DOI] [PubMed] [Google Scholar]
- 27.Bell JS, Johns R, Chen TF. Pharmacy students’ and graduates’ attitudes towards people with schizophrenia and severe depression. Am J Pharm Educ. 2006;70(4):Article 77. doi: 10.5688/aj700477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dipaula BA, Qian J, Mehdizadegan N, Simoni-Wastila L. An elective psychiatric course to reduce pharmacy students’ social distance toward people with severe mental illness. Am J Pharm Educ. 2011;75(4):Article 72. doi: 10.5688/ajpe75472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McKee BD, Larose-Pierre M, Rappa LR. A survey of community pharmacists and final-year student pharmacists and their perception of psychotherapeutic agents. J Pharm Pract. 2015;28(2):166–174. doi: 10.1177/0897190013515709. [DOI] [PubMed] [Google Scholar]
- 30.Angermeyer MC, Matschinger H. Public beliefs about schizophrenia and depression: similarities and differences. Soc Psychiatry Psychiatr Epidemiol. 2003;38(9):526–534. doi: 10.1007/s00127-003-0676-6. [DOI] [PubMed] [Google Scholar]
- 31.Crisp AH, Gelder MG, Rix S, Meltzer HI, Rowlands OJ. Stigmatisation of people with mental illnesses. Br J Psychiatry. 2000;177(1):4–7. doi: 10.1192/bjp.177.1.4. [DOI] [PubMed] [Google Scholar]
- 32.Lauber C, Nordt C, Falcato L, Rössler W. Factors influencing social distance toward people with mental illness. Community Ment Health J. 2004;40(3):265–274. doi: 10.1023/b:comh.0000026999.87728.2d. [DOI] [PubMed] [Google Scholar]
- 33.Corrigan PW, Green A, Lundin R, Kubiak MA, Penn DL. Familiarity with and social distance from people who have serious mental illness. Psychiatr Serv. 2001;52(7):953–958. doi: 10.1176/appi.ps.52.7.953. [DOI] [PubMed] [Google Scholar]
- 34.Penn DL, Guynan K, Daily T, Spaulding WD, Garbin CP, Sullivan M. Dispelling the stigma of schizophrenia: what sort of information is best? Schizophr Bull. 1994;20(3):567–578. doi: 10.1093/schbul/20.3.567. [DOI] [PubMed] [Google Scholar]
- 35.Link BG, Cullen FT, Frank J, Wozniak JF. The social rejection of former mental patients: understanding why labels matter. Am J Sociol. 1987;92(6):1461–1500. [Google Scholar]
- 36.Bell JS, Aaltonen SE, Bronstein E, et al. Attitudes of pharmacy students toward people with mental disorders, a six country study. Pharm World Sci. 2008;30(5):595–599. doi: 10.1007/s11096-008-9211-x. [DOI] [PubMed] [Google Scholar]
- 37.Gabbidon J, Clement S, van Nieuwenhuizen A, et al. Mental illness: Clinicians’ Attitudes (MICA) scale – psychometric properties of a version for healthcare students and professionals. Psychiatry Res. 2013;206(1):81–87. doi: 10.1016/j.psychres.2012.09.028. [DOI] [PubMed] [Google Scholar]
- 38.Jorm AF, Korten AE, Jacomb PA, Christensen H, Henderson S. Attitudes towards people with a mental disorder: a survey of the Australian public and health professionals. Aust N Z J Psychiatry. 1999;33(1):77–83. doi: 10.1046/j.1440-1614.1999.00513.x. [DOI] [PubMed] [Google Scholar]
- 39.Kassam A, Papish A, Modgill G, Patten S. The development and psychometric properties of a new scale to measure mental illness related stigma by health care providers: the Opening Minds Scale for Health Care Providers (OMS-HC) BMC Psychiatry. 2012;12(1):62. doi: 10.1186/1471-244X-12-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.O’Reilly CL, Bell JS, Chen TF. Pharmacists’ beliefs about treatments and outcomes of mental disorders: a mental health literacy survey. Aust N Z J Psychiatry. 2010;44(12):1089–1096. doi: 10.3109/00048674.2010.512864. [DOI] [PubMed] [Google Scholar]
- 41.Link BG, Phelan JC, Bresnahan M, Stueve A, Pescosolido BA. Public conceptions of mental illness: labels, causes, dangerousness, and social distance. Am J Public Health. 1999;89(9):1328–1333. doi: 10.2105/ajph.89.9.1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Angermeyer MC, Dietrich S. Public beliefs about and attitudes towards people with mental illness: a review of population studies. Acta Psychiatr Scand. 2006;113(3):163–179. doi: 10.1111/j.1600-0447.2005.00699.x. [DOI] [PubMed] [Google Scholar]
- 43.Philo G, Secker J, Platt S, Henderson L, McLaughlin G, Burnside J. The impact of the mass media on public images of mental illness: media content and audience belief. Health Educ J. 1994;53(3):271–281. [Google Scholar]
- 44.Stuart H. Media portrayal of mental illness and its treatments. CNS drugs. 2006;20(2):99–106. doi: 10.2165/00023210-200620020-00002. [DOI] [PubMed] [Google Scholar]
- 45.Buhler AV, Karimi RM. Peer-level patient presenters decrease pharmacy students' social distance from patients with schizophrenia and clinical depression. Am J Pharm Educ. 2008;72(5):Article 106. doi: 10.5688/aj7205106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nguyen E, Chen TF, O’Reilly CL. Evaluating the impact of direct and indirect contact on the mental health stigma of pharmacy students. Soc Psychiatry Psychiatr Epidemiol. 2012;47(7):1087–1098. doi: 10.1007/s00127-011-0413-5. [DOI] [PubMed] [Google Scholar]
- 47.Festinger L. A theory of social comparison processes. Human Relations. 1954;7(2):117–140. [Google Scholar]
- 48.Patten SB, Remillard A, Phillips L, et al. Effectiveness of contact-based education for reducing mental illness-related stigma in pharmacy students. BMC Med Educ. 2012;12(1):120. doi: 10.1186/1472-6920-12-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Medina MS, Plaza CM, Stowe CD, et al. Center for the Advancement of Pharmacy Education 2013 Educational Outcomes. Am J Pharm Educ. 2013;77(8):Article 162. doi: 10.5688/ajpe778162. [DOI] [PMC free article] [PubMed] [Google Scholar]