Abstract
Background
The combined therapy of bevacizumab (BEV) with taxane (paclitaxel or docetaxel) has shown an improvement on progression-free survival (PFS) and objective remission in Her2-negative patients with locally recurrent or metastatic breast cancer (LR/MBC). However, there was no benefit in overall survival (OS). The aim of this study was to evaluate the efficacy and safety of adding an agent to the BEV/taxane regimens for the treatment of Her2-negative patients with LR/MBC in a first-line setting.
Materials and methods
We searched PubMed, Web of Science, EMBASE, EBSCO, and the Cochrane Library databases for eligible trials. A meta-analysis was performed using Review Manager 5.0 freeware package. We calculated the hazard ratio (HR) for PFS and OS. The odds ratio (OR) was used to calculate objective response rate (ORR) and grade 3/4 drug-related adverse events. The heterogeneity of study outcomes was calculated by the χ2 test or I2 statistics.
Results
A total of 1,124 patients from seven randomized controlled trials were analyzed. Our meta-analysis showed that the ORR was significantly improved in the BEV/taxane-based triplet group when compared with the BEV/taxane-based doublet group (OR =1.31, 95% confidence interval [CI]: 1.03–1.67, P=0.03). A subset analysis showed that a similar result was achieved in the triplet group in which a cytotoxic agent was added (OR =1.46, 95% CI: 1.09–1.95, P=0.01). However, the PFS and OS had no statistically significant differences between the two groups (HR =0.87, 95% CI: 0.68–1.13, P=0.31; HR =0.98, 95% CI: 0.82–1.16, P=0.78, respectively). Regarding safety, thromboembolic events, fatigue, and diarrhea (all $grade 3) were more frequently observed in the BEV/taxane-based triplet group (OR =3.8, 95% CI: 1.86–7.79, P=0.0003; OR =1.55, 95% CI: 1.05–2.27, P=0.03; OR =2.1, 95% CI: 1.29–3.41, P=0.003, respectively). Other toxic effects had no statistically significant differences between the two groups.
Conclusion
Our results showed that adding an agent to BEV/taxane treatment regimens did not significantly improve PFS and prolong OS, except for conferring a significant advantage toward improved ORR in the first-line therapy for Her2-negative patients with LR/MBC. However, its side effects are predictable and manageable.
Keywords: bevacizumab, paclitaxel, docetaxel, breast cancer, meta-analysis
Introduction
Worldwide, locally recurrent or metastatic breast cancer (LR/MBC) is one of the most frequently diagnosed forms of female malignant tumor and one of the most common causes of female cancer-related mortality.1 Chemotherapy was required for patients with LR/MBC to prolong the survival, although surgery is the standard treatment if the disease has not spread prior to being resectable. In the past few decades, many chemotherapeutic agents have been used for the treatment of patients with LR/MBC. However, the overall survival (OS) duration has changed little and the 5-year survival rate of patients is only 23%.
Recently, newer approaches to Her-2-negative LR/MBC therapy have focused on targeting to inhibit angiogenesis, which is responsible for both poor prognosis and increased relapse rate. One of the most important stimulators of angiogenesis is vascular endothelial growth factor (VEGF); VEGF-mediated angiogenesis appears to play a pivotal role in the growth and metastatic potential of breast cancer.2,3 Bevacizumab (BEV), the first anti-VEGF humanized monoclonal antibody approved by the US Food and Drug Administration (FDA) to treat several tumors, could inhibit proliferation of vascular endothelial cells by blocking the binding of VEGF to its receptors.4,5 Although the clinical value of BEV in Her-2-negative patients with LR/MBC is controversial, it remains a promising strategy for treating Her-2-negative LR/MBC.
Meanwhile, preclinical evidence shows that taxane also has strong antiangiogenic activity except for its cytotoxic effects,6 indicating possible synergies with other agents targeting VEGF. Thus, taxane, as an antiangiogenic biological agent, is clinically used in combination with BEV for the first-line treatment of Her2-negative LR/MBC patients. Some studies7–9 demonstrated that BEV/taxane doublet treatments significantly improved progression-free survival (PFS) and objective response rate (ORR) of Her2-negative patients with LR/MBC; however, no benefit of meaningful OS could be proved in these studies. Moreover, the clinical outcomes were also inconsistent when adding an agent to the combined therapy of BEV and taxane in Her2-negative patients with LR/MBC.
For a more comprehensive and accurate understanding of the value of the addition of an agent to the combined therapy of BEV and taxane, we conducted a meta-analysis based on available randomized controlled trials (RCTs) to systematically assess the clinical efficacy of BEV/taxane-based triplet regimens relative to BEV/taxane-based doublet regimens in the treatment of Her2-negative patients with LR/MBC in terms of OS, PFS, and response rate. We also extensively discuss the possible reasons for controversy surrounding the addition of an agent to BEV/taxane regimens.
Materials and methods
Search strategy
Two experienced investigators (XQ Liu and XD Liu) independently performed an electronic search of literature from January 2000 to October 2015 employing PubMed, Web of Science, EMBASE, EBSCO, and the Cochrane Library databases. Searches were limited to human clinical trials published in English and were conducted using the following MESH terms: “bevacizumab”, “paclitaxel”, “docetaxel”, and “breast neoplasm” and the text words: “metastatic breast cancer”, “breast carcinoma”, and “chemotherapy”. When titles and/or abstracts fit the objectives, the full article was retrieved. The reference lists of every retrieved article and previous systematic review were scrutinized to identify additional trials not included in the electronic databases. Any discordance about study inclusion between the two investigators was resolved by following a discussion until a consensus was reached on the final interpretation of the data.
Inclusion criteria
Eligible studies had to meet the following inclusion criteria: 1) studies were RCTs and published in English; 2) patients had histologically confirmed Her2-negative LR/MBC; 3) studies were designed to receive BEV/taxane-based triplet regimens versus BEV/taxane-based doublet regimens as the first-line treatment; and 4) original literature outcomes included ORR, PFS, OS, and toxic effects evaluated according to the National Cancer Institute common terminology criteria for adverse events (CTCAE) Version 3.0.
Exclusion criteria
The exclusion criteria for retrieved studies were: 1) a lack of basic data necessary for our research or that the basic data were incomplete and 2) we chose the most recent literature to avoid duplication if there was repetition of the same or similar reports. In addition, articles were excluded if they did not satisfy one or more inclusion criteria.
Data extraction
The same two investigators independently extracted data using a prepared information form. The following data were extracted from the included studies: 1) basic patient characteristics, such as the number of intention-to-treat (ITT) patients, age of the participants, hormone receptor status, prior treatments, number of metastatic sites, and the Eastern Cooperative Oncology Group scale performance status; 2) description of interventions; treatment outcomes in terms of ORR, PFS, and OS; and the adverse reaction of patients according to CTCAE; and 3) study design (concealment of treatment allocation and blinding). When necessary, we attempted to contact the corresponding authors directly to seek missing data not reported in the published manuscripts. Any disagreement was discussed and resolved by consensus in a meeting with a third investigator.
Quality assessment
The methodological quality of the RCTs included in the meta-analysis was assessed by the same two investigators according to a modified Jadad score.10 Assessment scores were as follows: 1) randomization method: 2 points for appropriate, 1 point for not clear, and 0 point for inappropriate; 2) blinding of outcomes: 2 points for appropriate, 1 point for not clear, and 0 point for inappropriate; and 3) description of follow-up situation if the patients were lost to follow-up, exit from or breach of the treatment regimen: 1 point for ITT analysis and 0 point for no description. The overall scores ranged from 0 to 5. Scores of 0–2 and 3–5 were classified as low- and high-quality studies, respectively. Disagreements were also settled by following a discussion among authors.
Statistical analysis
Statistical analyses were performed using the Review Manager 5.0 freeware package. We calculated the hazard ratio (HR) for PFS and OS. The odds ratio (OR) was used to calculate the ORR and grade 3/4 drug-related adverse events. The HR and its 95% confidence interval [CI] were obtained from the articles directly, and we extracted data from the Kaplan–Meier survival curve as reported by Parmar et al,11 if the value was not given in the article. The heterogeneity of study outcomes was calculated by the χ2 test or I2 statistics. Heterogeneity was considered statistically significant when the P-value was <0.05 or I2 was >50%. If significant heterogeneity existed, data were analyzed using a random-effect model. Otherwise, a fixed-effect model was employed. Analyses were performed according to the ITT principle. Results were presented in all figures as conventional meta-analysis forest plots. A two-sided P-value of <0.05 was judged to indicate a statistically significant difference for all analyses. Sensitivity analyses were performed using the studies with high quality (Jadad score ≥3) to assess reliability. Publication bias was assessed by visually inspecting a funnel plot.
Results
Characteristics of the eligible studies
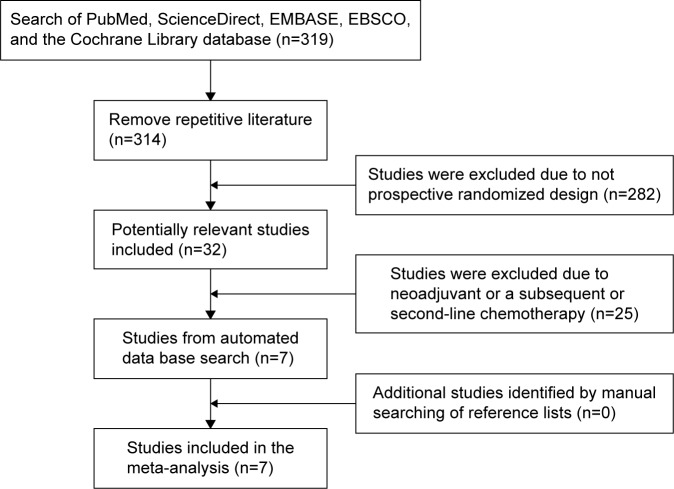
A total of 319 articles related to the analysis were found from the electric literature and subjected to the selection process (Figure 1). Finally, seven RCTs with 1,124 patients met the inclusion criteria and were included in the meta-analysis.12–18 Of the seven articles, three13–15 were designed to receive the BEV/taxane regimens with the addition of a cytotoxic agent and four12,16–18 with the addition of a biologic agent versus the BEV/taxane doublet regimens. The baseline characteristics of the included studies are listed in Table 1. There were most common points in terms of patient eligibilities in all inclusion trials, including patients with histologically confirmed HER2-negative locally advanced or metastatic breast cancer were eligible if the life expectancy was not <12 weeks; patients had to have completed any prior (neo) adjuvant chemotherapy at least 6 months before enrollment and any prior taxane-containing therapy at least 12 months before enrollment. Prior hormonal therapy for hormone receptor-positive disease was allowed. Prior exposure to BEV was not permitted. Except for the study reported by Diéras et al,17 patients with brain metastases were eligible if they had received treatment of the central nervous system disease and were free of neurological symptoms.
Figure 1.
Flow diagram of the study selection process.
Table 1.
Baseline characteristics of included trials
| First author/year | Treatment arms | No of patients, n | Age, years (range) | ECOG PS, n (%)
|
HR-positive tumors, n (%) | Prior (neo)adjuvant CT, n (%)
|
No of metastaticsites, n (%) | Outcome measures | Jadad scores | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | Taxane | Anthracycline | ||||||||
| Mayer et al12 2010 | P 90 mg/m2 days 1, 8. 15 + B 10 mg/m2 days 1, 15 q4w | 23 | 52 (29–80) | 12 (52) | 11 (48) | 0 | 18 (78) | NR | NR | NR | AEs | 2 |
| P 90 mg/m2 days 1, 8. 15 + B 10 mg/m2 days 1, 15 + Sun 37.5 mg/m2 daily for 21 days q4w | 23 | 58 (34–81) | 11 (50) | 11 (50) | 0 | 17 (74) | NR | NR | NR | |||
| Brufsky et al13 2011 | P 90 mg/m2 days 1, 8. 15 + B 10 mg/m2 days 1, 15 q4w | 94 | 57.5 (30.8–83.8) | 57 (60.6) | 37 (39.4) | 0 | ER: 60 (63.8) PR: 42 (44.7) |
33 (35.1) | NR | NR | ORR, PFS, OS, AEs | 3 |
| P 90 mg/m2 days 1, 8. 15 + B 10 mg/m2 days 1, 15 + Gem 1,500 mg/m2 days 1, 15 q4w | 93 | 55.2 (37.1–79.7) | 60 (64.5) | 31 (33.3) | 0 | ER: 67 (73) PR: 57 (61.3) |
32 (34.4) | NR | NR | |||
| Lam et al14 2014 | P 90 mg/m2 days 1, 8. 15 + B 10 mg/m2 days 1, 15 q4w | 156 | 56 (34–74) | 81 (52) | 75 (48) | 0 | 132 (85) | NR | 81 (52) | <3: 80 (51); ≥3: 76 (49) | ORR, PFS, OS, AEs | 3 |
| P 90 mg/m2 days 1, 8 + B 15 mg/m2 day 1 + Cap 825 mg/m2 twice daily on days 1–14 q3w | 156 | 56 (32–76) | 82 (53) | 74 (47) | 0 | 133 (85) | NR | 78 (50) | <3: 94 (60); ≧3: 61 (39) | |||
| Lück et al15 2015 | D 75 mg/m2 day 1 or P 80 mg/m2 days 1, 8. 15 + B 15 mg/m2 day 1 q4w | 116 | 57 (33–80) | 83 (72.2) | 29 (25.2) | 3 (2.6) | 90 (77.6) | NR | NR | ≤3: 99 (85.3); >3: 17 (14.7) | ORR, PFS, | 3 |
| D 75 mg/m2 day 1 or P 80 mg/m2 days 1, 8. 15 + B 15 mg/m2 day 1 + Cap 1,800 mg/m2 days 1–14 q4w | 111 | 57 (31–78) | 87 (78.4) | 18 (16.2) | 6 (5.4) | 86 (77.5) | NR | NR | ≦3: 92 (82.9); >3: 19 (17.1) | |||
| Diéras et al16 2015 | P 90 mg/m2 days 1, 8. 15 + B 10 mg/m2 days 1, 15 q4w | 62 | 51.5 (37–69) | 37 (59.7) | 25 (40.3) | 0 | NR | NR | NR | <3: 35 (56.5); ≧3: 27 (43.5) | ORR, PFS, OS, AEs | 5 |
| P 90 mg/m2 days 1, 8. 15 + B 10 mg/m2 days 1, 15 + Ona 10 mg/kg days 1, 15 q4w | 63 | 53 (35–79) | 35 (55.6) | 28 (44.4) | 0 | NR | NR | NR | <3: 36 (57.1); ≧3: 27 (42.9) | |||
| Diéras et al17 2015 | P 90 mg/m2 days 1, 8. 15 + B 10 mg/m2 days 1, 15 + placebo q4w | 56 | 51.5 (31–74) | 60 | 40 | 0 | 45 (78) | 11 (19) | NR | ≦3: 79; >3: 21 | ORR, PFS, AEs | 5 |
| P 90 mg/m2 days 1, 8. 15 + B 10 mg/m2 days 1, 15 + Tre 10 mg/kg once a week q4w | 58 | 56.5 (32–75) | 61 | 38 | 2 | 45 (80) | 10 (18) | NR | ≦3: 79; >3: 21 | |||
| Yardley et al18 2015 | P 90 mg/m2 days 1, 8. 15 + B 10 mg/m2 days 1, 15 q4w | 57 | 57 (25–79) | NR | NR | NR | 45 (79) | 19 (33) | 6 (10) | <3: 23 (41); ≧3: 34 (59) | ORR, PFS, OS, AEs | 5 |
| P 90 mg/m2 days 1, 8. 15 + B 10 mg/m2 days 1, 15 + Eve 10 mg, once daily on day 1 q4w | 56 | 61 (30–77) | NR | NR | NR | 44 (79) | 24 (43) | 4 (7) | <3: 28 (550); ≧3: 28 (50) | |||
Abbreviations: ECOG, Eastern Cooperative Oncology Group; PS, performance status; HR, hormone receptor; CT, chemotherapy; P, paclitaxel; B, bevacizumab; NR, no report; Sun, sunitinib; AEs, adverse events; ER, estrogen receptor; PR, progesterone receptor; Gem, gemcitabine; ORR, objective response rate; PFS, progression-free survival; OS, overall survival; Cap, capecitabine; D, docetaxel; Ona, onartuzumab; Tre, trebananib; Eve, everolimus.
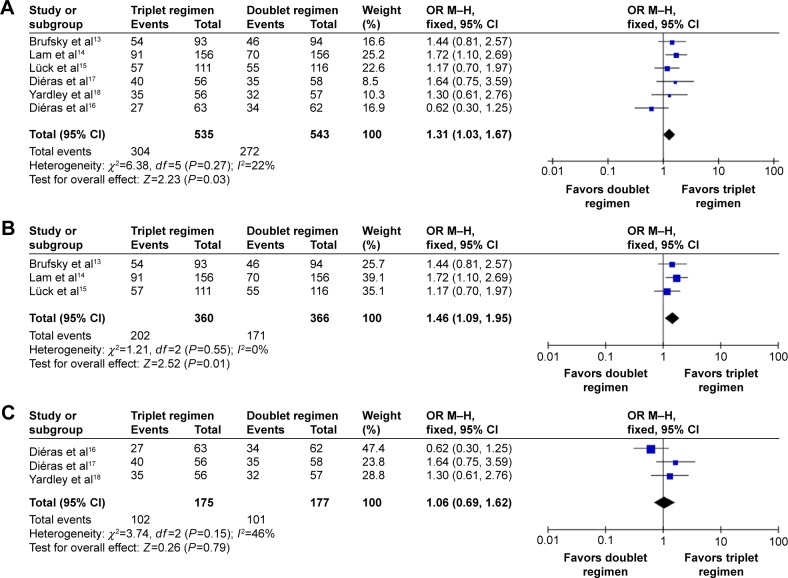
Objective response rate
Among the seven included trials, six trials13–18 reported the outcome measure of ORR and 1,078 patients were included in the analysis. The pooled analysis of ORR showed that BEV/taxane-based triplet regimens were associated with significantly high ORR when compared with BEV/taxane-based doublet regimens in the first-line treatment of Her2-negative LR/MBC (OR =1.31, 95% CI: 1.03–1.67, P=0.03; Figure 2A). Similarly, a subset analysis showed that adding a cytotoxic agent to BEV/taxane therapy was associated with significantly improved ORR when compared with BEV/taxane-based doublet therapy (OR =1.46, 95% CI: 1.09–1.95, P=0.01; Figure 2B). No statistical significance was achieved when a biologic agent was added (OR =1.06, 95% CI: 0.69–1.62, P=0.79; Figure 2C). A fixed-effect model was used because no significant heterogeneity was found between the trials from the χ2 test (I2=22%, P=0.27; I2=0%, P=0.55; I2=46%, P=0.15, respectively).
Figure 2.
Forest plot displaying the meta-analysis of objective response rate.
Notes: (A) BEV/taxane-based triplet therapy versus BEV/taxane doublet therapy; (B) BEV/taxane therapy with the addition of a cytotoxic agent versus BEV/taxane doublet therapy; (C) BEV/taxane therapy with the addition of a biologic agent versus BEV/taxane doublet therapy.
Abbreviations: BEV, bevacizumab; OR, odds ratio; M–H, Mantel–Haenszel; CI, confidence interval.
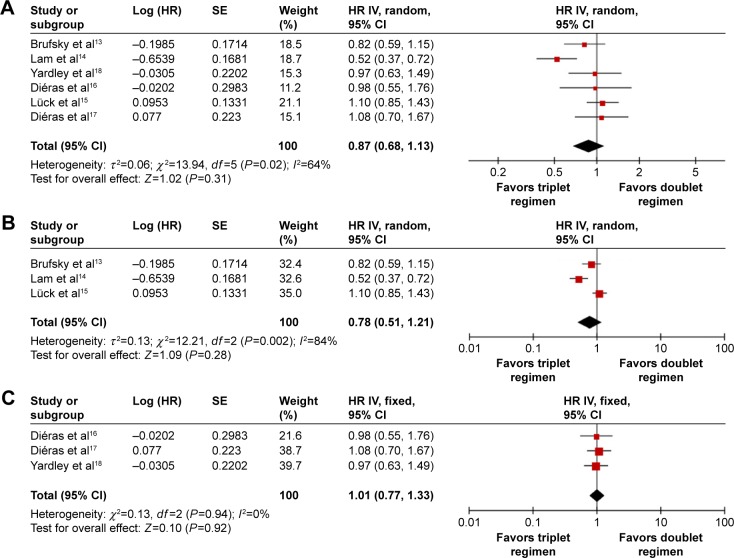
Progression-free survival
PFS was selected as the outcome measure in the six trials.13–18 The pooled HR for PFS demonstrated that there was no statistically significant difference between the two regimens as the first-line treatment for Her2-negative patients with LR/MBC (HR =0.87, 95% CI: 0.68–1.13, P=0.31; Figure 3A). A subset analysis showed that adding a cytotoxic agent to BEV/taxane therapy did not significantly improve the PFS when compared with the BEV/taxane-based doublet therapy (HR =0.78, 95% CI: 0.51–1.21, P=0.28; Figure 3B). A random-effect model was employed because significant heterogeneity was found between the trials (I2=64%, P=0.02; I2=84%, P=0.002, respectively). Similarly, no statistical significance was found when a biologic agent was added (HR =1.01, 95% CI: 0.77–1.33, P=0.92; Figure 3C). A fixed-effect model was used because no significant heterogeneity was found between the trials (I2=0%, P=0.94).
Figure 3.
Forest plot displaying the meta-analysis of progression free survival.
Notes: (A) BEV/taxane-based triplet therapy versus BEV/taxane doublet therapy; (B) BEV/taxane therapy with the addition of a cytotoxic agent versus BEV/taxane doublet therapy; (C) BEV/taxane therapy with the addition of a biologic agent versus BEV/taxane doublet therapy.
Abbreviations: BEV, bevacizumab; HR, hazard ratio; SE, standard error; IV, inverse variance; CI, confidence interval.
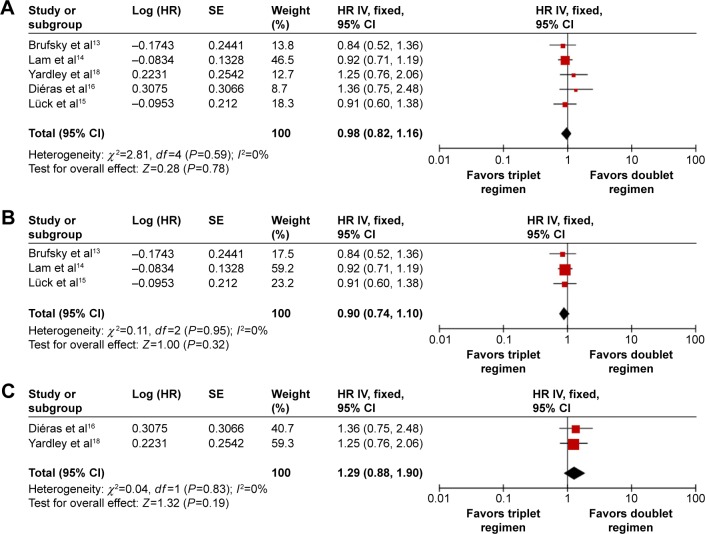
Overall survival
Data for OS were available from five trials.13–16,18 The BEV/taxane-based triplet therapy did not show a significant advantage over the BEV/taxane-based doublet therapy for Her2-negative LR/MBC in the first-line setting. The pooled HR for OS indicated that there was no significant difference between the groups of the BEV/taxane-based triplet therapy and the BEV/taxane-based doublet therapy (HR =0.98, 95% CI: 0.82–1.16, P=0.78; Figure 4A). Similarly, a subset analysis showed that adding neither a cytotoxic agent nor a biologic agent to BEV/taxane therapy was associated with a significant improvement in the OS when compared with the BEV/taxane-based doublet therapy (HR =0.90, 95% CI: 0.74–1.10, P=0.32; HR=1.29, 95% CI: 0.88–1.90, P=0.19, respectively; Figure 4B and C). A fixed-effects model was used because heterogeneity between trials was not significant (I2=0.0%, P=0.59; I2=0.0%, P=0.95; I2=0.0%, P=0.83, respectively).
Figure 4.
Forest plot displaying the meta-analysis of overall survival.
Notes: (A) BEV/taxane-based triplet therapy versus BEV/taxane doublet therapy; (B) BEV/taxane therapy with the addition of a cytotoxic agent versus BEV/taxane doublet therapy; (C) BEV/taxane therapy with the addition of a biologic agent versus BEV/taxane doublet therapy.
Abbreviations: BEV, bevacizumab; HR, hazard ratio; SE, standard error; IV, inverse variance; CI, confidence interval.
Safety
Common drug-related adverse events were reported in all included trials, and the majority were mild (grade 1) or moderate (grade 2) in severity. The focus of our analysis is grade 3 or 4 adverse events, which are listed in Table 2. Incidences of neutropenia and neutropenic fever were not significantly different between the groups treated with the BEV/taxane-based triplet regimens and the BEV/taxane-based doublet regimens (OR =1.54, 95% CI: 0.91–2.61, P=0.11; OR =1.59, 95% CI: 0.68–3.73, P=0.28, respectively). Incidences of thrombosis were higher with the BEV/taxane-based triplet therapy compared with the BEV/taxane-based doublet therapy (OR =3.8, 95% CI: 1.86–7.79, P=0.0003). When nonhematological adverse events were compared, significantly more grade 3–4 fatigue and diarrhea occurred in the BEV/taxane-based triplet therapy group (OR =1.55, 95% CI: 1.05–2.27, P=0.03; OR =2.1, 95% CI: 1.29–3.41, P=0.003, respectively). However, there were no statistically significant differences in nausea, hypertension, and peripheral neuropathy between the two arms.
Table 2.
Outcome of grade 3 or 4 toxicity meta-analysis comparing BEV/taxane-based triplet therapy with BEV/taxane doublet therapy
| Adverse events | Trials, n | Triplet regimen, n (grade 3/grade 4) | Doublet regimen, n (grade 3/grade 4) | Heterogeneity
|
OR (95% CI) | P-value | |
|---|---|---|---|---|---|---|---|
| P-value | I2 (%) | ||||||
| Febrile neutropenia | 4 | 14/328 | 9/330 | 0.72 | 0 | 1.59 (0.68–3.73) | 0.28 |
| Neutropenia | 7 | 162/558 | 119/566 | 0.004 | 68 | 1.54 (0.91–2.61) | 0.11 |
| Thrombosis | 5 | 34/439 | 9/447 | 0.58 | 0 | 3.8 (1.86–7.79) | 0.0003 |
| Fatigue | 7 | 83/558 | 60/566 | 0.66 | 0 | 1.55 (1.05–2.27) | 0.03 |
| Nausea | 6 | 42/447 | 34/450 | 0.56 | 0 | 1.31 (0.78–2.21) | 0.31 |
| Diarrhea | 7 | 65/558 | 39/566 | 0.28 | 20 | 2.1 (1.29–3.41) | 0.003 |
| Peripheral neuropathy | 7 | 71/558 | 65/566 | 0.51 | 0 | 1.13 (0.78–1.63) | 0.53 |
| Hypertension | 6 | 56/495 | 51/504 | 0.69 | 0 | 1.15 (0.75–1.75) | 0.52 |
Abbreviations: BEV, bevacizumab; OR, odds ratio; CI, confidence interval.
Sensitivity analysis
Sensitivity analysis was independently performed by excluding the study12 with low scores (2 points), and the exclusion of the study did not change the results.
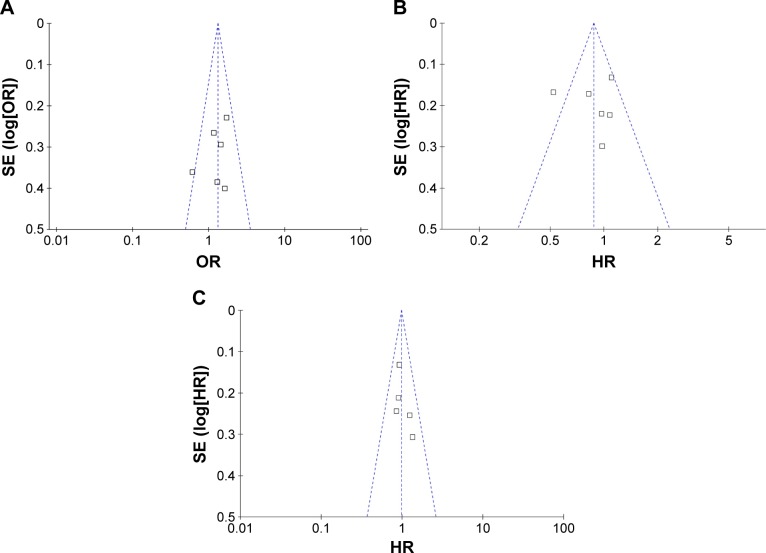
Publication bias
Based on funnel plots for the analysis of visual acuity, no obvious evidence of publication bias was found for ORR, PFS, and OS (Figure 5A–C).
Figure 5.
Funnel plot analysis of potential publication bias for all eligible studies.
Abbreviations: SE, standard error; OR, odds ratio; HR, hazard ratio.
Discussion
Recently, most clinical trials of the first-line treatment for Her-2-negative LR/MBC focus on BEV-based doublet regimens.19–21 It was well demonstrated that the combined therapy of BEV and taxane was significantly associated with improved PFS and ORR relative to BEV or taxane therapy alone or other BEV-based doublet therapy.8,22–24 In 2008, BEV was approved by the FDA for the first-line treatment of Her-2-negative LR/MBC in combination with taxane. However, the lack of OS benefit led to controversy about the therapeutic indication.25
Some Phase II/III trials attempted to improve clinical outcomes by adding an agent, such as a cytotoxic or biologic drug, to the BEV/taxane regimens for the treatment of Her-2-negative patients with LR/MBC in the first-line setting. Although some trials achieved positive results in terms of PFS and ORR, others reached opposite conclusions. For a more comprehensive analysis on the efficacy and safety of adding an agent to the BEV/taxane regimens for managing Her-2-negative LR/MBC, the systematic assessment was performed. Our pooled analysis indicated that the addition of neither a cytotoxic nor a biologic drug to the BEV/taxane treatment regimens could significantly prolong the OS and PFS (HR =0.98, 95% CI: 0.82–1.16, P=0.78; HR =0.87, 95% CI: 0.68–1.13, P=0.31, respectively) except for achieving a clinically significant advantage toward improved tumor remission rate (OR =1.31, 95% CI: 1.03–1.67, P=0.03), which is consistent with the conclusion elicited by Makhoul et al.26 However, the toxicity effect was predictable and manageable.
The subset analyses of adding a cytotoxic agent yielded similar results to that of the pooled analysis. Of the included three studies that were designed to receive the addition of a cytotoxic agent, one study reported by Lam et al14 showed that adding capecitabine to the BEV/paclitaxel regimen significantly improved ORR and response duration in Her2-negative patients with LR/MBC. While another two studies reported by Brufsky et al13 and Lück et al,15 demonstrated that the addition of neither capecitabine nor gemcitabine, respectively, was associated with a statistically significant improvement in clinical outcomes. The precise reasons for the discrepancy are unclear and possible explanations may include the following. 1) The duration of treatment was not long enough due to unfavorable safety profile of triplet regimens containing docetaxel or the number of patients in subgroups was too small to obtain a statistically significant result. For example, the study by Lück et al15 was prematurely closed after the preplanned interim analysis due to an unfavorable risk–benefit profile in some patients treated with the three-drug regimen containing docetaxel, which was consistent with that of the trial reported by Carbognin et al27 in which the addition of docetaxel significantly increased hematologic toxicities regardless of the chemotherapy backbone. 2) There could have been patient or drug selection issues, or no drug–drug interaction was evident in patients with hormone-positive disease. In the trial reported by Brufsky et al,13 a subset analysis showed that the triplet regimen significantly improved ORR relative to the doublet regimen (62.2% vs 45.1%; P=0.040) in patients with age <65 years and numerically prolonged the median OS in patients with triple-negative disease (21.8 months vs 15.3 months; P=0.097) although the statistical difference was not significant. Moreover, it should also be noted that the clinical outcomes of BEV/paclitaxel-based triplet regimens perhaps could be improved by substituting nanoparticle albumin-bound-paclitaxel (nab-P) for paclitaxel, which is partially supported by some Phase II/III trials28,29 that demonstrated reduced toxicities and superior efficacy of nab-P-contained treatment regimens relative to paclitaxel-contained regimens in female patients with breast cancer. Thus, in the presence of BEV, gemcitabine or capecitabine in combination with a different paclitaxel formulation may yield a favorably clinical outcome in Her-2-negative patients with LR/MBC. However, this hypothesis needs to be tested in further multicenter randomized trials.
Likewise, the addition of a biologic agent, including everolimus, trebananib, or onartuzumab, did not improve clinical efficacy of the BEV/paclitaxel regimen as the first-line treatment for Her2-negative patients with LR/MBC, except a treatment efficacy was inconclusive owing to the addition of sunitinib exhibiting an unacceptably high level of drug-related toxicities leading to the termination of the trial reported by Mayer et al.12 These results contrast with the demonstrated positive outcomes of adding everolimus to either hormonal or Her2-targeted therapy for pretreated patients with LR/MBC in clinical trials.30,31 The possible reasons are as follows. 1) Everolimus, a rapamycin derivative, selectively inhibits the mammalian target of rapamycin, which is a serine/threonine kinase playing a central role in cell metabolism, proliferation, differentiation, and angio-genesis via PI3K-dependent signaling pathways.32 In some estrogen receptor (ER)-positive tumors that are resistant to hormonal treatments, inhibition of the PI3K pathways results in increased expression of ER on the cell surface, providing a possible mechanism for reversal of the hormone-refractory status.33,34 In the trial reported by Yardley et al,18 the majority of patients were ER positive and untreated with hormonal therapy for LR/MBC. The lack of concurrent hormonal therapy may have allowed ongoing signaling to transmit through the ER pathway and compromised the impact of PI3K pathway inhibition. 2) Onartuzumab, a recombinant humanized anti-MET monoclonal antibody, selectively blocks MET-dependent signaling which is associated with the upregulation of VEGF expression.35,36 While in the trial reported by Diéras et al,16 the question of a positive treatment efficacy of the addition of onartuzumab in Her-2-negative patients with LR/MBC could not be answered owing to the low proportion of patients (12%) with MET-positive tumors. 3) Potential dose deficiency of trebananib, an investigational peptide-Fc fusion protein that could block the interaction of angiopoietin-1 and -2 with the Tie2 receptor, was possibly responsible for no significant difference in the improvement of clinical efficacy. For example, the addition of trebananib was weekly used with a dose of 10 mg/kg in the inclusion trial reported by Diéras et al,17 which was lower than that reported by the Phase III TRINOVA-1 study37 in which the treatment with a 15 mg/kg of trebananib every week plus weekly paclitaxel resulted in a significant improvement in PFS compared with placebo plus paclitaxel (HR =0.66, 95% CI: 0.57–0.77, P<0.0001). In a Phase I study (ClinicalTrials.gov, NCT00807859), trebananib is being investigated at doses up to 30 mg/kg every week in combination with chemotherapeutic drugs in the treatment of patients with LR/MBC. In addition, it should be noted that along with targeted therapies being increasingly used in clinical practice, anatomical imaging- or positron emission tomography–computed tomography-based evaluation criteria, including Choi, morphology, attenuation, size, and structure (MASS) and European association for the study of the liver (EASL), and PET response criteria in solid tumors (PERCIST), were designed to evaluate the therapeutic efficacy of targeted drugs in solid tumors. While in this meta-analysis, all inclusion trials adopted Response Evaluation Criteria in Solid Tumors (RECIST), which was traditionally used to evaluate clinical efficacy of chemotherapeutic drugs, to perform tumor assessment. Choi et al38 and Crabb et al39 reported that a statistically significant difference could be concluded from targeted therapy for solid tumors when clinical efficacy was assessed with anatomical or functional imaging-based evaluation criteria rather than traditional RECIST criteria.
In clinical trials, the efficacy and safety of a treatment regimen are equally important to patients. Under the premise that BEV plus taxane significantly improves ORR and PFS, treatment benefit and risk of adding an agent to the BEV/taxane regimens determine its fate. In the included trials, the fact that triplet regimens were associated with certain severe toxicities should not be ignored, and these events should be reasonably analyzed to avoid their occurrence. Our meta-analysis indicated that severe neutropenia, severe febrile neutropenia, nausea, hypertension, and peripheral neuropathy (≥grade 3) were infrequent and occurred at similar rates in both doublet and triplet regimens. Venous or arterial thromboembolic events, fatigue, and diarrhea (all $grade 3) were significantly more common in triplet regimens, but these adverse events are controllable and reversible in clinical practice.
Several strengths and limitations should also be considered when interpreting our results. First, a major strength of our study is that all the available data were obtained from recent RCTs and most of the studies were well performed and high in quality. Second, data analysis in all included seven trials was on the basis of ITT. Thus, we have enhanced a statistical power to provide reliable effect estimates. Although our meta-analysis represents a complete summary of the efficacy of adding a cytotoxic or biologic agent to the BEV/taxane regimens for Her2-negative patients with LR/MBC, it also serves to note the potential limitations. First, we were not able to do a subgroup analysis by age and hormonal-receptor status because of the lack of sufficient data, although all trials involved patients with age <65 years and hormonal-receptor negative tumors. Second, the triplet regimens varied widely between included trials and this may have influenced the results. Third, the sample size is relatively small. Further research with a large sample size is necessary to confirm these findings.
Conclusion
This analysis indicates that adding an agent to BEV/taxane treatment regimens does not confer a clinically meaningful improvement in PFS and OS except for significantly improving ORR in Her-2-negative patients with LR/MBC. However, its side effects are predictable and manageable. With the recommendations for drug selection and more selected populations of patients, adding an agent to the BEV/taxane regimens could be a preferable option as the first-line therapy for Her-2-negative patients with LR/MBC. Consequently, a multicenter randomized study with a large sample size and selected populations, such as patients with triple-negative disease or age <65 years, is needed in the future to better understand the role of BEV/taxane-based triplet regimens in the first-line treatment for patients with LR/MBC.
Acknowledgments
The authors thank the researchers whose studies were involved in this meta-analysis and provided useful data to us.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Gavilá J, Lopez-Tarruella S, Saura C, et al. SEOM clinical guidelines in metastatic breast cancer 2015. Clin Transl Oncol. 2015;17(12):946–955. doi: 10.1007/s12094-015-1476-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gasparini G. Biological and clinical role of angiogenesis in breast cancer. Breast Cancer Res Treat. 1995;36(2):103–107. doi: 10.1007/BF00666032. [DOI] [PubMed] [Google Scholar]
- 3.Liu F, You X, Wang Y, et al. The oncoprotein HBXIP enhances angio-genesis and growth of breast cancer through modulating FGF8 and VEGF. Carcinogenesis. 2014;35(5):1144–1153. doi: 10.1093/carcin/bgu021. [DOI] [PubMed] [Google Scholar]
- 4.Fisher CM, Schefter TE. Profile of bevacizumab and its potential in the treatment of cervical cancer. Onco Targets Ther. 2015;8:3425–3431. doi: 10.2147/OTT.S73251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Manso L, Moreno F, Márquez R, et al. Use of bevacizumab as a first-line treatment for metastatic breast cancer. Curr Oncol. 2015;22(2):e51–e60. doi: 10.3747/co.22.2210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ng SS, Figg WD, Sparreboom A. Taxane-mediated antiangiogenesis in vitro: influence of formulation vehicles and binding proteins. Cancer Res. 2004;64(3):821–824. doi: 10.1158/0008-5472.can-03-3391. [DOI] [PubMed] [Google Scholar]
- 7.Gray R, Bhattacharya S, Bowden C, Miller K, Comis RL. Independent review of E2100: a phase III trial of bevacizumab plus paclitaxel versus paclitaxel in women with metastatic breast cancer. J Clin Oncol. 2009;27(30):4966–4972. doi: 10.1200/JCO.2008.21.6630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miles DW, Chan A, Dirix LY, et al. Phase III study of bevacizumab plus docetaxel compared with placebo plus docetaxel for the first-line treatment of human epidermal growth factor receptor 2-negative metastatic breast cancer. J Clin Oncol. 2010;28(20):3239–3247. doi: 10.1200/JCO.2008.21.6457. [DOI] [PubMed] [Google Scholar]
- 9.Pivot X, Schneeweiss A, Verma S, et al. Efficacy and safety of bevacizumab in combination with docetaxel for the first-line treatment of elderly patients with locally recurrent or metastatic breast cancer: results from AVADO. Eur J Cancer. 2011;47(16):2387–2395. doi: 10.1016/j.ejca.2011.06.018. [DOI] [PubMed] [Google Scholar]
- 10.Jadad AR, Moher D, Klassen TP. Guides for reading and interpreting systematic reviews: II. How did the authors find the studies and assess their quality? Arch Pediatr Adolesc Med. 1998;152(8):812–817. doi: 10.1001/archpedi.152.8.812. [DOI] [PubMed] [Google Scholar]
- 11.Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med. 1998;17(24):2815–2834. doi: 10.1002/(sici)1097-0258(19981230)17:24<2815::aid-sim110>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 12.Mayer EL, Dhakil S, Patel T, et al. SABRE-B: an evaluation of paclitaxel and bevacizumab with or without sunitinib as first-line treatment of metastatic breast cancer. Ann Oncol. 2010;21(12):2370–2376. doi: 10.1093/annonc/mdq260. [DOI] [PubMed] [Google Scholar]
- 13.Brufsky A, Hoelzer K, Beck T, et al. A randomized phase II study of paclitaxel and bevacizumab with and without gemcitabine as first-line treatment for metastatic breast cancer. Clin Breast Cancer. 2011;11(4):211–220. doi: 10.1016/j.clbc.2011.03.019. [DOI] [PubMed] [Google Scholar]
- 14.Lam SW, de Groot SM, Honkoop AH, et al. Dutch Breast Cancer Research Group Paclitaxel and bevacizumab with or without capecitabine as first-line treatment for HER2-negative locally recurrent or metastatic breast cancer: a multicentre, open-label, randomized phase 2 trial. Eur J Cancer. 2014;50(18):3077–3088. doi: 10.1016/j.ejca.2014.10.008. [DOI] [PubMed] [Google Scholar]
- 15.Lück HJ, Lübbe K, Reinisch M, et al. Phase III study on efficacy of taxanes plus bevacizumab with or without capecitabine as first-line chemotherapy in metastatic breast cancer. Breast Cancer Res Treat. 2015;149(1):141–149. doi: 10.1007/s10549-014-3217-y. [DOI] [PubMed] [Google Scholar]
- 16.Diéras V, Campone M, Yardley DA, et al. Randomized, phase II, placebo-controlled trial of onartuzumab and/or bevacizumab in combination with weekly paclitaxel in patients with metastatic triple-negative breast cancer. Ann Oncol. 2015;26(9):1904–1910. doi: 10.1093/annonc/mdv263. [DOI] [PubMed] [Google Scholar]
- 17.Diéras V, Wildiers H, Jassem J, et al. Trebananib (AMG 386) plus weekly paclitaxel with or without bevacizumab as first-line therapy for HER2-negative locally recurrent or metastatic breast cancer: a phase 2 randomized study. Breast. 2015;24(3):182–190. doi: 10.1016/j.breast.2014.11.003. [DOI] [PubMed] [Google Scholar]
- 18.Yardley DA, Bosserman LD, O’Shaughnessy JA, et al. Paclitaxel, bevacizumab, and everolimus/placebo as first-line treatment for patients with metastatic HER2-negative breast cancer: a randomized placebo-controlled phase II trial of the Sarah Cannon Research Institute. Breast Cancer Res Treat. 2015;154(1):89–97. doi: 10.1007/s10549-015-3599-5. [DOI] [PubMed] [Google Scholar]
- 19.Sengupta S, Rojas R, Mahadevan A, Kasper E, Jeyapalan S. CPT-11/bevacizumab for the treatment of refractory brain metastases in patients with HER2-neu-positive breast cancer. Oxf Med Case Reports. 2015;2015(4):254–257. doi: 10.1093/omcr/omv010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li Q, Yan H, Zhao P, Yang Y, Cao B. Efficacy and safety of bevacizumab combined with chemotherapy for managing metastatic breast cancer: a meta-analysis of randomized controlled trials. Sci Rep. 2015;5:15746. doi: 10.1038/srep15746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cunningham D, Lang I, Marcuello E, et al. Bevacizumab plus capecitabine versus capecitabine alone in elderly patients with previously untreated metastatic colorectal cancer (AVEX): an open-label, randomised phase 3 trial. Lancet Oncol. 2013;14(11):1077–1085. doi: 10.1016/S1470-2045(13)70154-2. [DOI] [PubMed] [Google Scholar]
- 22.Lang I, Brodowicz T, Ryvo L, et al. Bevacizumab plus paclitaxel versus bevacizumab plus capecitabine as first-line treatment for HER2-negative metastatic breast cancer: interim efficacy results of the randomised, open-label, non-inferiority, phase 3 TURANDOT trial. Lancet Oncol. 2013;14(2):125–133. doi: 10.1016/S1470-2045(12)70566-1. [DOI] [PubMed] [Google Scholar]
- 23.von Minckwitz G, Puglisi F, Cortes J, et al. Bevacizumab plus chemotherapy versus chemotherapy alone as second-line treatment for patients with HER2-negative locally recurrent or metastatic breast cancer after first-line treatment with bevacizumab plus chemotherapy (TANIA): an open-label, randomised phase 3 trial. Lancet Oncol. 2014;15(11):1269–1278. doi: 10.1016/S1470-2045(14)70439-5. [DOI] [PubMed] [Google Scholar]
- 24.Wang X, Huang C, Li M, Gu Y, Cui Y, Li Y. The efficacy of bevacizumab plus paclitaxel as first-line treatment for HER2-negative metastatic breast cancer: a meta-analysis of randomized controlled trials. Tumour Biol. 2014;35(5):4841–4848. doi: 10.1007/s13277-014-1635-4. [DOI] [PubMed] [Google Scholar]
- 25.Fralick M, Ray M, Fung C, Booth CM, Mallick R, Clemons MJ. Bevacizumab for advanced breast cancer: hope, hype, and hundreds of headlines. Oncologist. 2013;18(11):1174–1179. doi: 10.1634/theoncologist.2013-0160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Makhoul I, Klimberg VS, Korourian S, et al. Combined neoadjuvant chemotherapy with bevacizumab improves pathologic complete response in patients with hormone receptor negative operable or locally advanced breast cancer. Am J Clin Oncol. 2015;38(1):74–79. doi: 10.1097/COC.0b013e31828940c3. [DOI] [PubMed] [Google Scholar]
- 27.Carbognin L, Sperduti I, Nortilli R, et al. Balancing activity and tolerability of neoadjuvant paclitaxel- and docetaxel-based chemotherapy for HER2-positive early stage breast cancer: sensitivity analysis of randomized trials. Cancer Treat Rev. 2015;41(3):262–270. doi: 10.1016/j.ctrv.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 28.Lobo C, Lopes G, Baez O, et al. Final results of a phase II study of nab-paclitaxel, bevacizumab, and gemcitabine as first-line therapy for patients with HER2-negative metastatic breast cancer. Breast Cancer Res Treat. 2010;123(2):427–435. doi: 10.1007/s10549-010-1002-0. [DOI] [PubMed] [Google Scholar]
- 29.Gradishar WJ, Tjulandin S, Davidson N, et al. Phase III trial of nano-particle albumin-bound paclitaxel compared with polyethylated castor oil-based paclitaxel in women with breast cancer. J Clin Oncol. 2005;23(31):7794–7803. doi: 10.1200/JCO.2005.04.937. [DOI] [PubMed] [Google Scholar]
- 30.André F, O’Regan R, Ozguroglu M, et al. Everolimus for women with trastuzumab-resistant, HER2-positive, advanced breast cancer (BOLERO-3): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet Oncol. 2014;15(6):580–591. doi: 10.1016/S1470-2045(14)70138-X. [DOI] [PubMed] [Google Scholar]
- 31.Yardley DA, Noguchi S, Pritchard KI, et al. Everolimus plus exemestane in postmenopausal patients with HR(+) breast cancer: BOLERO-2 final progression-free survival analysis. Adv Ther. 2013;30(10):870–884. doi: 10.1007/s12325-013-0060-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Albanell J, Dalmases A, Rovira A, Rojo F. mTOR signalling in human cancer. Clin Transl Oncol. 2007;9(8):484–493. doi: 10.1007/s12094-007-0092-6. [DOI] [PubMed] [Google Scholar]
- 33.de Graffenried LA, Friedrichs WE, Russell DH, et al. Inhibition of mTOR activity restores tamoxifen response in breast cancer cells with aberrant Akt Activity. Clin Cancer Res. 2004;10(23):8059–8067. doi: 10.1158/1078-0432.CCR-04-0035. [DOI] [PubMed] [Google Scholar]
- 34.Creighton CJ, Fu X, Hennessy BT, et al. Proteomic and transcriptomic profiling reveals a link between the PI3K pathway and lower estrogen-receptor (ER) levels and activity in ER+ breast cancer. Breast Cancer Res. 2010;12(3):R40. doi: 10.1186/bcr2594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nakade J, Takeuchi S, Nakagawa T, et al. Triple inhibition of EGFR, Met, and VEGF suppresses regrowth of HGF-triggered, erlotinib-resistant lung cancer harboring an EGFR mutation. J Thorac Oncol. 2014;9(6):775–783. doi: 10.1097/JTO.0000000000000170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Matsumura A, Kubota T, Taiyoh H, et al. HGF regulates VEGF expression via the c-Met receptor downstream pathways, PI3K/Akt, MAPK and STAT3, in CT26 murine cells. Int J Oncol. 2013;42(2):535–542. doi: 10.3892/ijo.2012.1728. [DOI] [PubMed] [Google Scholar]
- 37.Monk BJ, Poveda A, Vergote I, et al. Anti-angiopoietin therapy with trebananib for recurrent ovarian cancer (TRINOVA-1): a randomised, multicentre, double-blind, placebo-controlled phase 3 trial. Lancet Oncol. 2014;15(8):799–808. doi: 10.1016/S1470-2045(14)70244-X. [DOI] [PubMed] [Google Scholar]
- 38.Choi H, Charnsangavej C, Faria SC, et al. Correlation of computed tomography and positron emission tomography in patients with metastatic gastrointestinal stromal tumor treated at a single institution with imatinib mesylate: proposal of new computed tomography response criteria. J Clin Oncol. 2007;25(13):1753–1759. doi: 10.1200/JCO.2006.07.3049. [DOI] [PubMed] [Google Scholar]
- 39.Crabb SJ, Patsios D, Sauerbrei E, et al. Tumor cavitation: impact on objective response evaluation in trials of angiogenesis inhibitors in non-small-cell lung cancer. J Clin Oncol. 2009;27(3):404–410. doi: 10.1200/JCO.2008.16.2545. [DOI] [PubMed] [Google Scholar]