Abstract
Introduction
Appendiceal mucocele is a relatively rare condition characterized by progressive dilation of the appendix caused by intra-luminal accumulation of mucoid substance. Its incidence is 0.07 – 0,63% of all appendectomies performed.
Case report
We report the case of a 70-year-old man who came to our observation with gravative pain in right lower abdominal region. A computed tomography abdominal scan revealed a cystic/tubular structure like an appendicular mass with wall enhancement but without calcifications suggestive of a mucocele. Into peritoneal cavity we found profuse mucinous material with a 1,5 cm size parietal nodule. We also identified a free perforation of the cecum with consensual spillage of gelatinous material mimicking a pseudomyxoma peritonei. We decided to perform a right hemicolectomy with excision of peritoneal lesion.
Discussion
The controversy in the pathologic terminology can give rise to a clinical dilemma in terms of the management and follow-up plans. For mucosal hyperplasia and cystadenoma simple appendectomy is curative. Only in case of large base of implantation it may be necessary the resection of the ileum and caecum or right hemicolectomy. In case of mucinous cystoadenocarcinoma authors perform a right hemicolectomy.
Conclusion
Appendiceal mucinous neoplasms are different pathological entities. The correct surgical management depends on size and location of lesion. A preoperative diagnosis is obviously needed in order to perform the correct treatment. CT abdominal scan is the better diagnostic tool, but different authors show their inability to reach a preoperative diagnosis in the larger majority of cases.
Keywords: Appendiceal mucocele, Appendiceal mucinous neoplasms, Mucocele, Laparoscopic appendectomy, Laparoscopy, Laparoscopic surgery
Introduction
Appendiceal mucocele is a relatively rare condition. Its incidence is 0.07–0.63% of all appendectomies performed (1). It is more frequent in females with a ratio of 4:1 versus men. Appendiceal mucocele represents a progressive appendix dilation caused by intraluminal accumulation of mucoid substance, as it may be a malignant or a benign process. On the basis of histopathological characteristics we identify: appendiceal adenomas, benign pathology treated by appendectomy alone; low-grade appendiceal mucinous neoplasm with low risk of recurrence; low-grade appendiceal mucinous neoplasm with high risk of recurrence; mucinous adenocarcinoma (2). The clinical presentation is very unspecific, it can remain asymptomatic for a long time or can occur with acute abdominal pain, usually in the right iliac fossa, possibly associated with the presence of a palpable mass. The major complication is represented by pseudomyxoma peritonei, characterized by the collection of intra-abdominal mucus and repetitive lesions on peritoneal surface. Surgical treatment depends on the dimensions and histology of the mucinous neoplasm, as well as the clinical presentation. Appendectomy is considered to be sufficient in case of mucous hyperplasia or cystadenoma with an intact appendiceal base, as no long-term follow-up is required in this case. In case of cystadenoma with positive borders – base affection, cecum resection is necessary. If there are data for cystadenocarcinoma with or without lymph nodes colonization, right hemicolectomy with thorough lymph node dissection must be performed. Long term follow-up is obligatory for these patients.
Case report
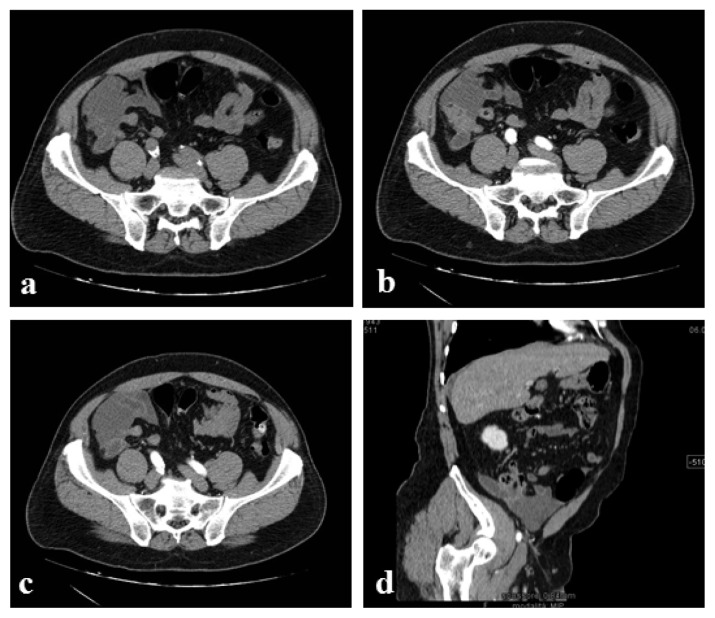
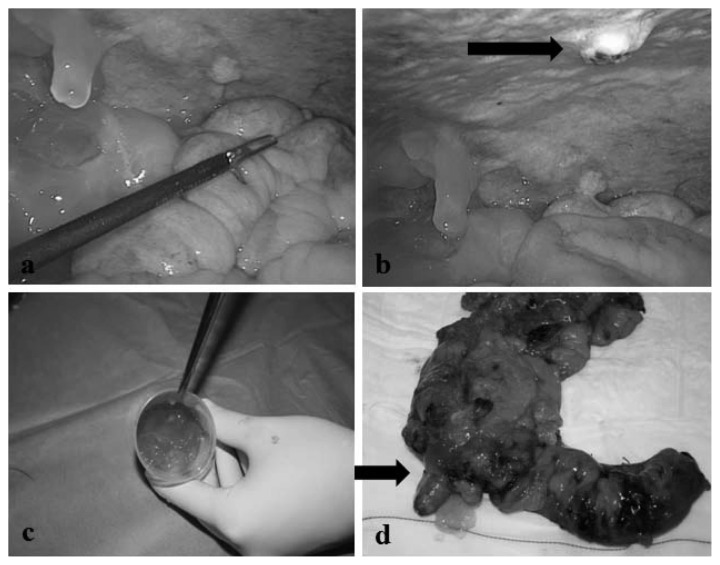
We report the case of a 70-year-old man with history of colonic diverticulosis, who came to our observation with gravative pain in right lower abdominal region. On examination his abdomen was tenderness in right iliac fossa. Bowel sounds were present. Blood tests: Hb 14.9 g/dl, WBC 5,100 without leucocytosis. Computed tomography (CT) abdominal scan revealed a cystic/tubular structure like an appendicular mass with wall enhancement but without calcifications suggestive of a mucocele with no involvement of the surrounding tissues. CT showed also hypodense material consistent with mucine in the peritoneal cavity (Figure 1). These reports encouraged us to carry out an exploratory diagnostic laparoscopy in emergency setting (3–5). After general anesthesia the patient was placed in dorsal lithotomy position (6, 7). We used Veress needle (8) to induce pneumoperitoneum positioning a 10-mm trocars in left para-umbilical region for the camera and other two 5-mm trocars in left flank and in sovrapubic region (9). Into peritoneal cavity we found profuse mucinous material with a 1,5 cm size parietal nodule. The appendix appeared remarkably increased in size (10 × 2 cm in diameter), with thickened walls and with a large base of implantation. We also identified a free perforation of the cecum with consensual spillage of gelatinous material mimicking a pseudomyxoma peritonei (Figure 2). There were no macroscopic lesion on liver surface. On the basis of detection of intraoperative peritoneal lesion, presence of mucoid material and large cecal perforation we decided to convert to the open surgery to perform a right hemicolectomy with excision of peritoneal lesion. Operative time was 135 min and blood loss was no significant. Patient began food intake in first POD with regular postoperative course. The histopathology reported a low-grade appendiceal mucinous neoplasm with high risk of recurrence. 17 isolated lymph nodes presented reactive hyperplasia and peritoneal nodule showed no neoplastic colonization.
Fig. 1.
a) non contrast-enhanced axial CT showed cecal appendix filled with hypodense material; b–c) contrast-enhanced axial CT: presence of lesion of the cecal wall on the side of the appendix with contrast-enhanced wall. Coexisted periappendicular and pericecal hypodense material; d) multiplanar reformatted contrast-enhanced CT showed cecal appendix completely repleted with hypodense material consistent with mucine. The same patient with small amount of perihepatic fluid.
Fig. 2.
a) intraoperative laparoscopic finding with diffuse gelatinous material mimicking a pseudomixoma peritonei; b) presence of peritoneal lesion; c) mucoid material; d) resected right colon, cecum perforation and appendix with a large base of implantation.
Discussion
For many authors the term “mucocele” should be abandoned in favour of a more specific pathological entity (10). In our opinion, the term should be retained for some reasons: it is deeply used in literature and it is a simple descriptive term, which enables the surgeon or radiologist to report on a particular lesion before any pathological characterization. Pathologically the condition may be classified into neoplastic and nonneoplastic variants. The neoplastic lesions include: mucosal hyperplasia, cystadenoma and cystadenocarcinoma (11). For mucosal hyperplasia and cystadenoma simple appendectomy is curative. Only in case of large base of implantation it may be necessary the resection of ileum and caecum or right hemicolectomy. On the other hand, mucinous cystoadenocarcinoma is characterized by the presence of stromal invasion by malignant glands and/or the presence of mucus and mucus secreting cells in the peritoneal cavity. In these cases the authors perform a right hemicolectomy. Recently some authors identified mucinous neoplasm with low risk of recurrence and mucinous neoplasm with high risk of recurrence. This controversy in the pathologic terminology can give rise to a clinical dilemma in terms of the management and follow-up plans (12). The most common clinical presentation of appendiceal mucinous neoplasm is pain in the right region of the lower abdomen simulating acute appendicitis (13). In other cases we find abdominal mass, bowel perforation with intraperitoneal free air, weight loss or bowel obstruction. A preoperative diagnosis is obviously needed in order to perform the correct treatment. CT abdominal scan is the better diagnostic tool (14–16), but different authors show their inability to reach a preoperative diagnosis in the larger majority of cases (17). From EAES Guidelines we know that patients with symptoms and diagnostic findings suggestive of acute appendicitis should undergo diagnostic laparoscopy (18, 19). When we suspect an appendiceal mucinous neoplasm we should use laparoscopy prudently because laparoscopic appendectomy for appendiceal mucocele, in some cases, has been followed by wide dissemination of mucinous implants on the peritoneal surface several months later (20). The presence of periappendiceal mucoid material does not always mean malignancy, as it has been seen with hyperplasia and cystadenoma. While surgery is the only known potentially curative treatment, currently, there is no consensus regarding the optimal management. The size and location of the tumour, presence of mucus collections, involvement of lymph nodes and the final histology are the determining factors for correct surgical resection (21). Our surgery is aligned with the above mentioned lines. For laparoscopic surgery no solid proof exists with or against its safety.
Conclusion
Appendiceal mucinous neoplasms are different pathological entities. The correct surgical management depends on size and location of lesion. The majority of paper that we found in literature are case reports. The laparoscopic approach in the treatment of mucocele has been adopted for a small number of patients. In our case CT abdominal scan showed a cecal appendix completly repleted with hypodense material consistent with mucine. We performed an exploratory laparoscopy and than we converted to open surgery to avoid peritoneal surface dissemination. In any case the correct management of these patients depends on intraoperative findings and histology.
References
- 1.Agarwala N, Liu CY. Laparoscopic appendectomy. J Am Assoc Gynecol Laparosc. 2003 May;10(2):166–8. doi: 10.1016/s1074-3804(05)60292-7. [DOI] [PubMed] [Google Scholar]
- 2.Rabie ME, Al Shraim M, Al Skaini MS, Alqahtani S, El Hakeem I, Al Qahtani AS, Malatani T, Hummadi A. Mucus containing cystic lesions of the appendix: the unresolved issues. Int J Surg Oncol. 2015;2015:139461. doi: 10.1155/2015/139461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Agrusa A, Romano G, De Vita G, Frazzetta G, Chianetta D, Di Buono G, Gulotta G. Adrenal gunshot wound: Laparoscopic approach. Report of a case. Int J Surg Case Rep. 2014;5(2):70–2. doi: 10.1016/j.ijscr.2013.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agrusa A, Frazzetta G, Chianetta D, Di Giovanni S, Gulotta L, Di Buono G, Sorce V, Romano G, Gulotta G. “Relaparoscopic” management of surgical complications: The experience of an Emergency Center. Surg Endosc. 2015 Oct 21; doi: 10.1007/s00464-015-4558-2. [DOI] [PubMed] [Google Scholar]
- 5.Agrusa A, Romano G, Frazzetta G, Chianetta D, Sorce V, Di Buono G, Gulotta G. Role and outcomes of laparoscopic cholecystectomy in the elderly. Int J Surg. 2014;12(Suppl 2):S37–9. doi: 10.1016/j.ijsu.2014.08.385. [DOI] [PubMed] [Google Scholar]
- 6.Novo G, Corrado E, Tortorici E, Novo A, Agrusa A, Saladino V, Marturana I, Lentini R, Ferrandes M, Visconti C, Massenti F, D’Arienzo M, Vitale F, Gulotta G, Novo S. Cardiac risk stratification in elective non-cardiac surgery: role of NT-proBNP. Int Angiol. 2011 Jun;30(3):242–6. [PubMed] [Google Scholar]
- 7.Agrusa A, Romano G, Lo Re G, Di Buono G, Vernuccio F, Galfano MC, Midiri F, Gulotta G. Hemoperitoneum following mild blunt abdominal trauma: first presentation of Crohn’s disease. Acta Medica Mediterranea. 2014;30(2):315–318. [Google Scholar]
- 8.Agrusa A, Di Buono G, Chianetta D, Sorce V, Citarrella R, Galia M, Vernuccio L, Romano G, Gulotta G. Three-dimensional (3D) versus two-dimensional (2D) laparoscopic adrenalectomy: A case-control study. Int J Surg. 2016 Apr;28(Suppl 1):S114–7. doi: 10.1016/j.ijsu.2015.12.055. [DOI] [PubMed] [Google Scholar]
- 9.Agrusa A, Romano G, Di Buono G, Frazzetta G, Chianetta D, Sorce V, Billone V, Cucinella G, Gulotta G. Acute appendicitis and endometriosis: Retrospective analysis in emergency setting. Giornale Italiano di Ostetricia e Ginecologia. 2013;35(6):728–732. [Google Scholar]
- 10.Rymer B, Forsythe RO, Husada G. Mucocoele and mucinous tumours of the appendix: review of the literature. Int J Surg. 2015 Jun;18:132–5. doi: 10.1016/j.ijsu.2015.04.052. [DOI] [PubMed] [Google Scholar]
- 11.Qizilbash AH. Mucoceles of the appendix. Their relationship to hyperplastic polyps, mucinous cystadenomas, and cystadenocarcinomas. Arch Pathol. 1975 Oct;99(10):548–55. [PubMed] [Google Scholar]
- 12.Pai RK, Beck AH, Norton JA, Longacre TA. Appendiceal mucinous neoplasms: clinicopathologic study of 116 cases with analysis of factors predicting recurrence. Am J Surg Pathol. 2009 Oct;33(10):1425–39. doi: 10.1097/PAS.0b013e3181af6067. [DOI] [PubMed] [Google Scholar]
- 13.Lai CW, Yue CT, Chen JH. Mucinous cystadenocarcinoma of the appendix mimics acute appendicitis. Clin Gastroenterol Hepatol. 2013 Feb;11(2):e11. doi: 10.1016/j.cgh.2012.05.023. [DOI] [PubMed] [Google Scholar]
- 14.Romano G, Agrusa A, Frazzetta G, De Vita G, Chianetta D, Di Buono G, Amato G, Gulotta G. Laparoscopic drainage of liver abscess: case report and literature review. G Chir. 2013 May-Jun;34(5–6):180–2. doi: 10.11138/gchir/2013.34.5.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Agrusa A, Romano G, Frazzetta G, Chianetta D, Sorce V, Di Buono G, Gulotta G. Laparoscopic adrenalectomy for large adrenal masses: single team experience. Int J Surg. 2014;12(Suppl 1):S72–4. doi: 10.1016/j.ijsu.2014.05.050. [DOI] [PubMed] [Google Scholar]
- 16.Romano G, Agrusa A, Chianetta D, Frazzetta G, Sorce V, Di Buono G, Gulotta G. Laparoscopic management of adrenal tumors: a four-year experience in a single-center. Minerva Chirurgica. 2014;69(2 Suppl 1):125–129. [Google Scholar]
- 17.Madwed D, Mindelzun R, Jeffrey RB., Jr Mucocele of the appendix: imaging findings. AJR Am J Roentgenol. 1992 Jul;159(1):69–72. doi: 10.2214/ajr.159.1.1609724. [DOI] [PubMed] [Google Scholar]
- 18.Agresta F, Ansaloni L, Baiocchi GL, Bergamini C, Campanile FC, Carlucci M, et al. Laparoscopic approach to acute abdomen from the Consensus Development Conference of the Società Italiana di Chirurgia Endoscopica e nuove tecnologie (SICE), Associazione Chirurghi Ospedalieri Italiani (ACOI), Società Italiana di Chirurgia (SIC), Società Italiana di Chirurgia d’Urgenza e del Trauma (SICUT), Società Italiana di Chirurgia nell’Ospedalità Privata (SICOP), and the European Association for Endoscopic Surgery (EAES) Surg Endosc. 2012 Aug;26(8):2134–64. doi: 10.1007/s00464-012-2331-3. [DOI] [PubMed] [Google Scholar]
- 19.Agrusa A, Romano G, Di Buono G, Dafnomili A, Gulotta G. Laparoscopic approach in abdominal emergencies: a 5-year experience at a single center. G Chir. 2012 Nov-Dec;33(11–12):400–3. [PubMed] [Google Scholar]
- 20.Cartanese C, Petitti T, Ferrozzi L. Laparoscopic resection of an incidental appendiceal mucocele: is it correct. Case report. Ann Ital Chir. 2012 Jul-Aug;83(4):359–62. [PubMed] [Google Scholar]
- 21.Karakaya K, Barut F, Emre AU, Ucan HB, Cakmak GK, Irkorucu O, Tascilar O, Ustundag Y, Comert M. Appendiceal mucocele: case reports and review of current literature. World J Gastroenterol. 2008 Apr 14;14(14):2280–3. doi: 10.3748/wjg.14.2280. [DOI] [PMC free article] [PubMed] [Google Scholar]