Abstract
Purpose
To evaluate the incidence and pathologic correlation of thin-section computed tomography (TSCT) findings in smoking-related interstitial fibrosis (SRIF) with pulmonary emphysema.
Patients and methods
Our study included 172 consecutive patients who underwent TSCT and subsequent lobectomy. TSCT findings including clustered cysts with visible walls (CCVW) and ground-glass attenuation with/without reticulation (GGAR) were evaluated and compared in nonsmokers and smokers and among lung locations. TSCT findings, especially CCVW, were also compared with histological findings using lobectomy specimens.
Results
The incidence of CCVW and GGAR was significantly higher in smokers than in nonsmokers (34.1% and 40.7%, respectively, vs 2.0% and 12.2%). CCVW and GGAR were frequently found in the lower and peripheral zones. Histologically, CCVW corresponded more often with SRIF with emphysema than usual interstitial pneumonia (UIP, 63.3% vs 30%). CCVW of irregular size and shape were seen in 19 of 20 SRIF with emphysema and in seven of nine UIP-manifested areas with similar round cysts. A less-involved subpleural parenchyma was observed more frequently in SRIF with emphysema.
Conclusion
SRIF with emphysema is a more frequent pathological finding than UIP in patients with CCVW on TSCT. The irregular size and shape of CCVW and a less-involved subpleural parenchyma may be a clue suggesting the presence of SRIF with emphysema.
Keywords: pulmonary emphysema, smoking, usual interstitial pneumonia, honeycombing, smoking-related interstitial fibrosis, airspace enlargement with fibrosis
Introduction
Cigarette smoking is a risk factor for various interstitial lung diseases (ILD) and pulmonary emphysema. While smoking is strongly implicated in the development of respiratory bronchiolitis (RB)-associated interstitial lung disease (RB-ILD), desquamative interstitial pneumonia (DIP), and pulmonary Langerhans cell histiocytosis,1–8 some cigarette smokers present with idiopathic pulmonary fibrosis9 and nonspecific interstitial pneumonia (NSIP).10 Although pulmonary emphysema or ILD tend to predominate, the coexistence of diffuse fibrosing interstitial pneumonia and pulmonary emphysema, known as combined pulmonary fibrosis and emphysema syndrome,11,12 has been proposed as a distinct clinical entity. Localized or nonspecific fibrosis accompanied by emphysematous changes is also a frequent pathological finding in smokers.13,14 Although these pathological changes appear to be similar, they are known by different names, ie, airspace enlargement with fibrosis (AEF),15 clinically occult interstitial fibrosis or smoking-related interstitial fibrosis (SRIF),16,17 RB-ILD with fibrosis,18 respiratory bronchiolitis with fibrosis (RBF),19 subclinical ILD,20 and interstitial lung abnormalities.21 Although these forms of fibrosis were suggested to represent pathological conditions different from diffuse fibrosing interstitial pneumonia,13,16,17 the incidence and features of these fibroses detected by thin-section computed tomography (TSCT) and the precise correlation between TSCT findings and their pathology remain to be elucidated, especially when such fibrosis coexists with pulmonary emphysema.
On TSCT images, the coexistence of fibrotic changes and pulmonary emphysema in the same lung area may result in similar clustered cysts that mimic honeycombing. This poses diagnostic problems. In fact, the degree of interobserver agreement in the assessment of honeycombing on CT images was only moderate due to the presence of mimicking lesions, including superimposed pulmonary emphysema.22 Because honeycombing is a key finding in the diagnosis of usual interstitial pneumonia (UIP) patterns on TSCT images,23 to improve the accuracy of CT diagnoses, additional studies are needed to clarify the difference in the TSCT appearance of true and mimicked honeycombing.
Based on our hypothesis that both true and mimicked honeycombing manifest similar clustered cysts on TSCT images, we regarded all clustered cysts as a single group designated as clustered cysts with visible walls (CCVW) in the first CT analysis that evaluated the incidence and location of CT findings of reported smoking-related ILD. Then, using lobectomy specimens of the same patients, we correlated each abnormal CT finding with observed pathological findings, especially focusing on the pathological basis of CCVW.
Patients and methods
Patients
This retrospective study was approved by our institutional review board of Shiga University of Medical Science, which approved the collection and use of the materials, patient informed consent was waived. A review of the thoracic surgery records identified 192 consecutive patients who had undergone lobectomy at our institution. After excluding 20 patients, because lobectomy specimens were unavailable or inappropriate for histological analysis, the final study population comprised 172 patients (120 men and 52 women) with lung nodules who had undergone TSCT and subsequent lobectomy between April 1, 2007, and June 30, 2009. The 172 patients, 123 smokers and 49 nonsmokers, ranging in age from 40 years to 86 years (mean 67.7 years), were divided into three groups: 49 patients (group 1, 28.5%) were nonsmokers, 58 (group 2, 33.7%) were moderate smokers (<50 packs/year), and 65 (group 3, 37.8%) were heavy smokers (>50 packs/year). All underwent pulmonary function tests <2 weeks before lobectomy. The vital capacity was 115.3%±14.8% in group 1, 106.7%±14.6% in group 2, and 104.0%±20.5% in group 3; their forced expiratory volume in 1 second was 76.0%±8.3%, 72.4%±9.7%, and 68.6%±11.6%, respectively. The histological diagnosis of the nodules was lung cancer in 162 patients (94.2%), metastases in four (2.3%), benign tumor in four (2.3%), and inflammatory nodules in two patients (1.2%).
CT scanning protocols
All patients underwent scanning on one of three MDCT scanners. The scan parameters on the SOMATOM Sensation Cardiac instrument (Siemens, Erlangen, Germany) were 0.75×16 mm collimation, 0.37 second gantry rotation time, 120 kV tube voltage, 100 effective mAs, and 0.85 beam pitch. On the Aquilion 16 and the Aquilion ONE (Toshiba, Tokyo, Japan) they were 1.0 ×16 mm collimation, 0.5-second gantry rotation time, 120 kV tube voltage, 150 mA tube current, 0.688 beam pitch; and 0.5×64 mm collimation, 0.5-second gantry rotation time, 120 kV tube voltage, 200 mA tube current, and 0.641 beam pitch, respectively. All CT examinations were performed with the patient in the supine position at full inspiration. CT images were reconstructed with a high-spatial frequency algorithm at a section thickness of 1 mm.
CT evaluation
Two radiologists with 30 years and 12 years of experience, respectively, evaluated contiguous 1 mm-thick CT images of the whole lung independently and then by consensus. All images were reviewed on a workstation at lung window settings (width 1,500 HU and level −650 HU). The CT images were randomized, and the reviewers were blinded to clinical information and histological diagnoses. The presence or absence of TSCT findings suggestive of smoking-related pulmonary emphysema and ILD was recorded for each lobe. The left lingula was regarded as an independent lobe in this study. The reviewers looked for a simple low attenuation area (LAA) without visible walls, CCVW, ground-glass attenuation with/without reticulation (GGAR), and diffuse ill-defined centrilobular nodules (DICN). CCVW included all multiple cystic changes with shared walls irrespective of the cyst size and shape and of the wall thickness. GGAR with dependent distribution or affecting <5% of any lobe was not regarded as abnormal.21 TSCT findings within lobes were recorded as peripheral, central, or diffuse. About one-third of the outer lung zone from the chest wall or diaphragm was regarded as peripheral.
The incidence of each TSCT finding in the three patient groups was compared using both case-based and lobe-based analyses. It was also compared among the upper, middle, and lower lobes in each group as was the distribution of TSCT findings among the lung zones.
Pathological evaluation
We prepared two to five sections from each of the 172 lobectomy specimens for histological analysis. They were stained with hematoxylin and eosin and elastic van Gieson stains and evaluated independently by two pathologists with 17 years and 3 years of experience, respectively. Masson’s trichrome staining was added when it was needed to show fibroblastic foci. Disagreements were resolved by consensus. The readers evaluated all histological sections from the same lobe and recorded the pathological patterns as normal, emphysema, UIP, NSIP, DIP, organizing pneumonia, RB, and SRIF. The criteria for a diagnosis of UIP, NSIP, DIP, organizing pneumonia, and RB were based on the International Consensus Classification.24 As there is no consensus on the nomenclature for the smoking-related localized form of interstitial fibrosis, we used the term “SRIF” to describe the pathological pattern showing paucicellular, frequently hyalinized interstitial fibrosis.15–17 Other histological diagnoses were recorded as “other”. When more than one pathological pattern was identified, all were recorded for that specimen.
Correlation between CT and pathological findings
All patterns identified on TSCT images of the 172 lobes were compared with all pathological patterns. However, as it was difficult to correlate histological sections exactly with the same lung area on TSCT images, all observed histological patterns were recorded and described as representing the resected lobe. In addition, in 30 lobes including CCVW, TSCT findings of CCVW were further evaluated with respect to irregularities in the cyst size and shape and the presence or absence of a less-involved subpleural parenchyma. In this analysis, irregularity of CCVW was judged positive when clustered cysts included multiple large cysts >10 mm in diameter or cysts whose wall was destroyed, resulting in irregular cystic fusion. Then, CCVW were divided into three categories as only areas of CCVW with similar size and shape, only areas of CCVW with irregular size and shape, and coexisting areas of CCVW with both similar and irregular types and compared with pathological patterns.
Statistical analysis
Interobserver agreement on the TSCT findings was assessed by kappa analysis. The incidence of specific TSCT findings in the three patient groups and among lung lobes or zones was evaluated using the chi-square test. A P-value of <0.05 was considered to indicate a significant difference. Statistical analysis was done using IBM SPSS Statistics 20 (IBM Corporation, Armonk, NY, USA).
Results
CT evaluation
Interobserver agreement for each TSCT finding was good. The kappa coefficients for LAA, CCVW, GGAR, and DICN were 0.699, 0.795, 0.713, and 0.605, respectively.
The incidence of each TSCT finding was assessed by both case-based and lobe-based analyses. As shown in Table 1 and Figure 1, the incidence of LAA, CCVW, and GGAR was significantly higher in smokers than in nonsmokers in both case-based and lobe-based analyses. By lobe-based analysis, heavy smokers manifested a significantly higher incidence of CCVW and GGAR than moderate smokers. By lobe-based but not case-based analysis, the incidence of DICN was significantly higher in smokers than nonsmokers.
Table 1.
Incidence of thin-section CT findings in nonsmokers and smokers (172 cases and 1,032 lobes)
| CT finding | Nonsmokers | Mild/moderate smokers | Heavy smokers | All smokers |
|---|---|---|---|---|
| LAA | ||||
| Case | 6.1% (3/49) | 58.6% (34/58) | 83.1% (54/65) | 71.5% (88/123) |
| Lobe | 2.4% (7/294) | 35.1% (122/348) | 59.7% (233/390) | 48.1% (355/738) |
| CCVW | ||||
| Case | 2.0% (1/49) | 27.6% (16/58) | 40.0% (26/65) | 34.1% (42/123) |
| Lobe | 0.7% (2/294) | 11.5% (40/348) | 23.3% (91/390) | 17.8% (131/738) |
| GGAR | ||||
| Case | 12.2% (6/49) | 37.9% (22/58) | 43.1% (28/65) | 40.7% (50/123) |
| Lobe | 6.8% (20/294) | 16.4% (57/348) | 23.8% (93/390) | 20.3% (150/738) |
| DICN | ||||
| Case | 4.1% (2/49) | 6.9% (4/58) | 9.2% (6/65) | 8.1% (10/123) |
| Lobe | 3.1% (9/294) | 5.7% (20/348) | 6.9% (27/390) | 6.4% (47/738) |
Abbreviations: CT, computed tomography; LAA, low attenuation area; CCVW, clustered cysts with visible walls; GGAR, ground-glass attenuation with/without reticulation; DICN, diffuse ill-defined centrilobular nodules.
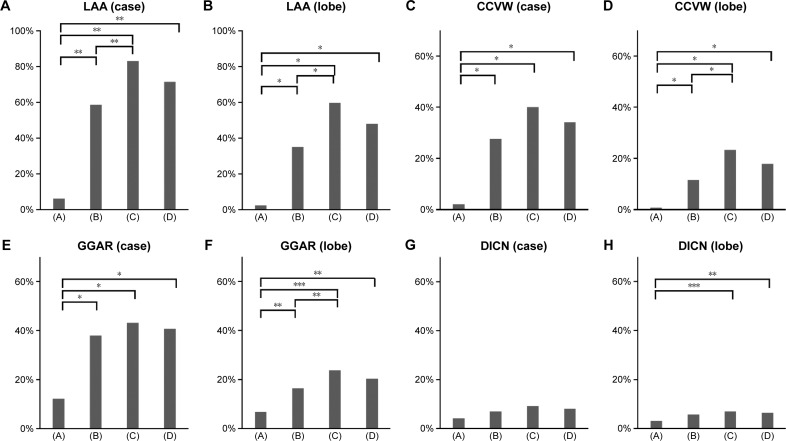
Figure 1.
Incidence of thin-section computed tomography findings in nonsmokers and smokers (172 cases and 1,032 lobes).
Notes: Incidence of LAA in cases (A), LAA in lobes (B), CCVW in cases (C), CCVW in lobes (D), GGAR in cases (E), GGAR in lobes (F), DICN in cases (G), DICN in lobes (H). The incidence of LAA, CCVW, and GGAR was significantly higher in smokers than in nonsmokers in both case-based and lobe-based analyses. By lobe-based analysis, heavy smokers manifested a significantly higher incidence of CCVW and GGAR than moderate smokers. By lobe-based but not case-based analysis, the incidence of DICN was significantly higher in smokers than nonsmokers. (A) Nonsmokers, (B) mild/moderate smokers, (C) heavy smokers, and (D) all smokers. *P<0.001, **P<0.005, ***P<0.05.
Abbreviations: LAA, low attenuation area; CCVW, clustered cysts with visible walls; GGAR, ground-glass attenuation with/without reticulation; DICN, diffuse ill-defined centrilobular nodules.
GGAR only, CCVW with or without GGAR, or DICN was seen in 66 (53.7%) of the 123 smokers. CCVW lesions were accompanied by GGAR in 99 (75.6%) of 131 lobes of smokers.
As shown in Table 2 and Figure 2, CCVW and GGAR were observed primarily in the lower lobes and in the peripheral zone (P<0.001), whereas LAA showed an upper lobe predominance and DICN was present diffusely in most cases.
Table 2.
Incidence of thin-section CT findings among lobes and zones
| Upper | Middle | Lower | Peripheral | Central | Diffuse | |
|---|---|---|---|---|---|---|
| LAA | 48.8% (168/344) | 22.4% (77/344) | 34.0% (117/344) | 19.6% (71/362) | 33.1% (120/362) | 47.2% (171/362) |
| CCVW | 10.5% (36/344) | 7.6% (26/344) | 20.6% (71/344) | 75.2% (100/133) | 6.0% (8/133) | 18.8% (25/133) |
| GGAR | 9.8% (34/344) | 11.6% (40/344) | 27.9% (96/344) | 79.4% (135/170) | 0.6% (1/170) | 20.0% (34/170) |
| DICN | 7.0% (24/344) | 4.7% (16/344) | 4.7% (16/344) | 0.0% (0/56) | 3.6% (2/56) | 96.4% (54/56) |
Abbreviations: CT, computed tomography; LAA, low attenuation area; CCVW, clustered cysts with visible walls; GGAR, ground-glass attenuation with/without reticulation; DICN, diffuse ill-defined centrilobular nodules.
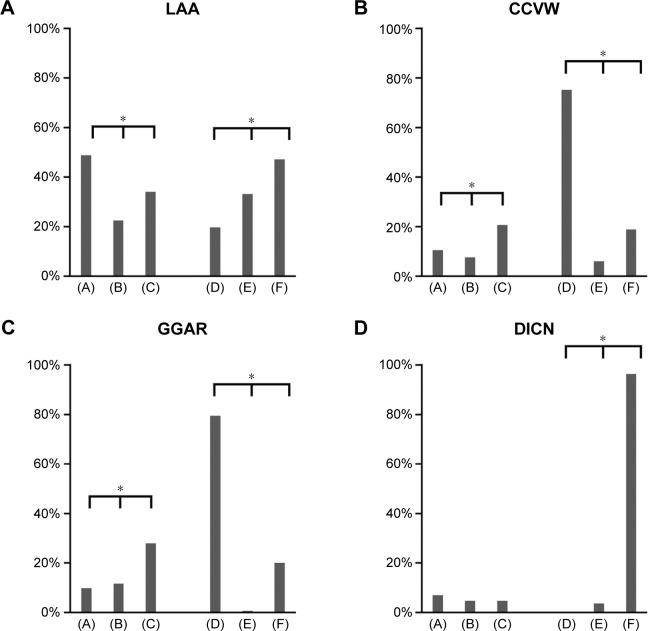
Figure 2.
Incidence of thin-section computed tomography findings among lobes and zones.
Notes: Incidence of LAA (A), CCVW (B), GGAR (C), DICN (D) among lobes and zones. CCVW and GGAR were observed primarily in the lower lobes and in the peripheral zone, whereas LAA showed an upper lobe predominance and DICN was present diffusely in most cases. (A) Upper; (B) middle; (C) lower; (D) peripheral; (E) central; and (F) diffuse. *P<0.001.
Abbreviations: LAA, low attenuation area; CCVW, clustered cysts with visible walls; GGAR, ground-glass attenuation with/without reticulation; DICN, diffuse ill-defined centrilobular nodules.
CT-pathologic correlation in lobectomy specimens
The correlation between TSCT and histological findings in the 172 lobes is summarized in Table 3. Of the 172 patients, TSCT findings were normal in 79 patients, LAA was observed only in 37 patients, DICN in 11 patients, GGAR in 15 patients, and CCVW in 30 patients. Of the 79 normal lobes on CT, only 44 (55.7%) were diagnosed as normal histologically; among the other 35 normal-appearing lobes, histology revealed pulmonary emphysema in 12 patients, non-UIP/fibrosis in 19 patients, UIP in one patient, and other diseases in three patients. Of the 37 lobes with only LAA on CT, 22 (59.5%) revealed SRIF or RB in addition to emphysema. The histological findings on most DICN cases were SRIF and/or RB combined with emphysema. GGAR mainly corresponded to SRIF with or without emphysema (11/15, 73.3%) although some UIP lesions coexisted in two of 15 lobes (13.3%). Among 30 lobes with CCVW, there were 19 (63.3%) with SRIF with or without emphysema and RB; nine (30%) showed UIP combined with or without emphysema and SRIF.
Table 3.
Correlation of thin-section CT findings with histological findings in 172 resected lobes
| Histological findings | Thin-section CT findings
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Normal (79) | LAA (37) | DICN (11) | GGAR (12) | GGAR + LAA (3) | CCVW + LAA (9) | CCVW + GGAR (7) | CCVW + LAA + GGAR (14) | CCVW (all) (30) | |
| Normal (48) | 44 | 3 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Em (26) | 12 | 11 | 1 | 1 | 0 | 1 | 0 | 0 | 1 |
| SRIF (5) | 1 | 0 | 1 | 2 | 0 | 1 | 0 | 0 | 1 |
| SRIF + Em (58) | 9 | 18 | 5 | 6 | 3 | 5 | 3 | 9 | 17 |
| SRIF + RB (1) | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| SRIF + Em + RB (4) | 1 | 2 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| RB (6) | 4 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| RB + Em (5) | 3 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| UIP (1) | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| UIP + Em (2) | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 |
| UIP + Em + SRIF (9) | 0 | 0 | 0 | 2 | 0 | 1 | 2 | 4 | 7 |
| UIP + Em + SRIF + RB (1) | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Others (6) | 3 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 1 |
Note: The numbers in parentheses correspond to the number of total cases for each row.
Abbreviations: CT, computed tomography; DICN, diffuse ill-defined centrilobular nodules; LAA, low attenuation area; GGAR, ground-glass attenuation with/without reticulation; CCVW, clustered cysts with visible walls; Em, emphysema; SRIF, smoking-related interstitial fibrosis; RB, respiratory bronchiolitis; UIP, usual interstitial pneumonia.
Additional evaluation of CCVW
The correlation of additional TSCT and histological findings in 30 resected lobes with CCVW is shown in Table 4. The 30 lobes included nine upper lobes, one middle lobe, and 20 lower lobes. Only areas of CCVW with irregular size and shape were observed in 19 of 20 (95%) lobes with SRIF with or without emphysema and RB (Figures 3 and 4) and in two of nine (22%) with UIP combined with or without emphysema and SRIF. Relative sparing of the subpleural parenchyma was seen more frequently in lobes with SRIF with or without emphysema and RB (11/20, 55%) than in lobes with UIP combined with or without emphysema and SRIF (1/9, 11.1%; Figures 4 and S1). Among nine lobes with UIP combined with or without emphysema and SRIF, three showed only areas of CCVW of similar size and shape (Figure 5). Coexisting areas of CCVW of similar and irregular size and shape were seen in four lobes (Figures 6 and 7).
Table 4.
Correlation of additional thin-section CT findings of CCVW with histological findings in 30 resected lobes
| Histological findings | Additional morphological findings
|
||||
|---|---|---|---|---|---|
| Only areas of CCVW with similar size and shape | Coexisting areas of CCVW with both similar and irregular types | Only areas of CCVW with irregular size and shape | Presence of less-involved subpleural parenchymal change
|
||
| (+) | (−) | ||||
| Em (1) | 1 | 1 | |||
| SRIF (1) | 1 | 1 | |||
| SRIF + Em (17) | 1 | 16 | 9 | 8 | |
| SRIF + Em + RB (1) | 1 | 1 | |||
| UIP (1) | 1 | 1 | |||
| UIP + Em (1) | 1 | 1 | |||
| UIP + Em + SRIF (7) | 2 | 3 | 2 | 7 | |
| Others (ACIF + Em) (1) | 1 | 1 | |||
| Total (30) | 4 | 4 | 22 | 12 | 18 |
Note: The numbers in parentheses correspond to the number of total cases for each row.
Abbreviations: CT, computed tomography; CCVW, clustered cysts with visible walls; Em, emphysema; SRIF, smoking-related interstitial fibrosis; RB, respiratory bronchiolitis; UIP, usual interstitial pneumonia; ACIF, airway-centered idiopathic fibrosis.
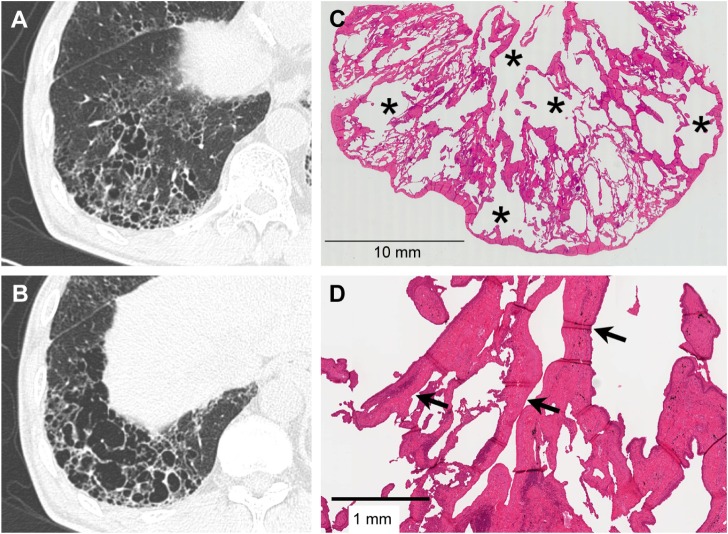
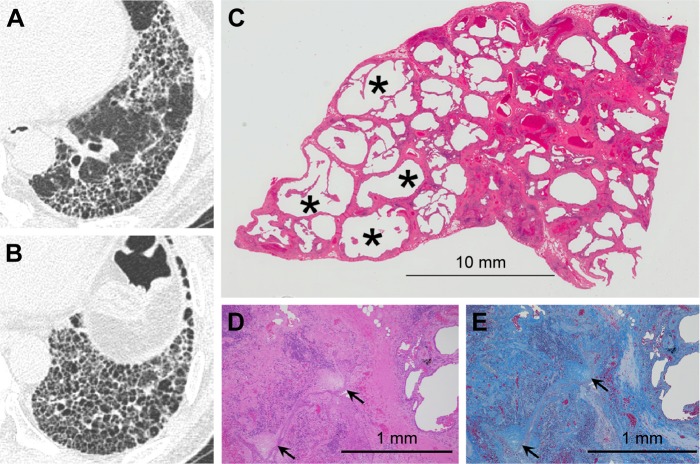
Figure 3.
Severe SRIF with emphysema pattern on thin-section CT images and histological findings.
Notes: (A and B) Thin-section CT images showing clustered cysts of markedly irregular size and shape accompanied by ground-glass attenuation with reticular structures in the surrounding area. (C) Low-power photograph of a histological section (hematoxylin–eosin stain) reveals irregularly shaped emphysematous spaces (asterisk) with collagenous fibrotic walls. Many of the walls are truncated. Patchy fibrosis is observed in the intervening lung parenchyma and corresponds to ground-glass attenuation with reticular structures on thin-section CT. Irregular cysts with thickened walls tend to be present a little apart from the pleura with less-involved subpleural lung parenchyma. (D) On this high-power photograph of a histological section, fibrosis consists of hyalinized paucicellular fibrosis (arrow) corresponding to SRIF.
Abbreviations: SRIF, smoking-related interstitial fibrosis; CT, computed tomography.
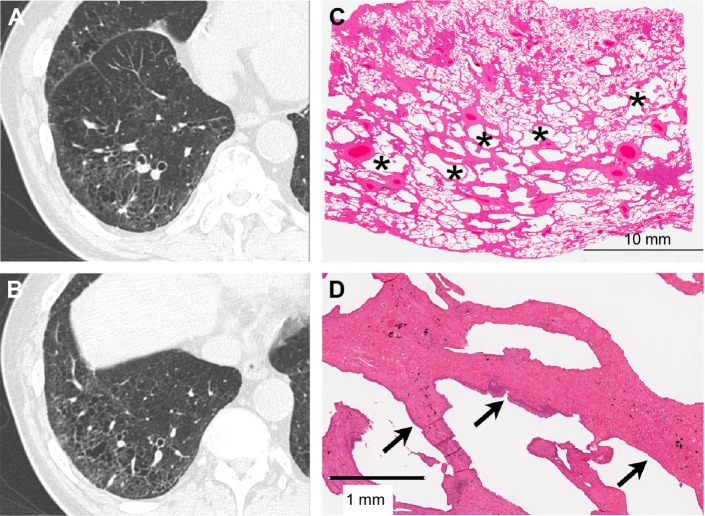
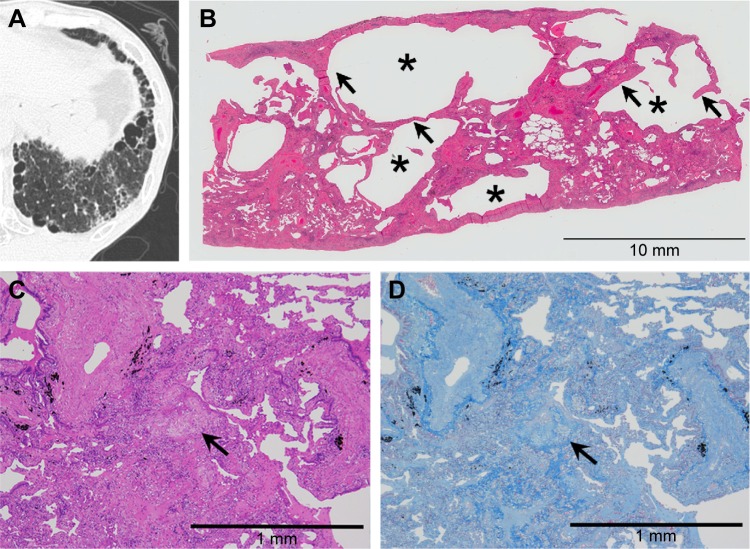
Figure 4.
Mild SRIF with emphysema pattern on thin-section CT images and histological findings.
Notes: (A and B) Thin-section CT images showing clustered cysts with visible walls in the peripheral zone with less involvement of the subpleural parenchyma. The size and shape of the cysts vary. Note ground-glass attenuation with reticular or branching structures in the surrounding area. (C) This low-power photograph of the histological section (hematoxylin–eosin stain) reveals irregularly shaped emphysematous spaces (asterisk) with thickened fibrotic walls corresponding to clustered cysts with visible walls on the thin-section CT image. There is patchy fibrosis at peribronchiolar and subpleural sites corresponding to ground-glass attenuation with reticular or branching structures in the surrounding area. Irregular cysts with thickened walls are present apart from the pleura with less-involved subpleural lung parenchyma. (D) On this high-power photograph of a histological section, fibrosis of this pattern consists of hyalinized paucicellular fibrosis (arrow) or SRIF.
Abbreviations: SRIF, smoking-related interstitial fibrosis; CT, computed tomography.
Figure 5.
UIP pattern on thin-section CT images and histological findings.
Notes: (A and B) Thin-section CT images showing clustered cysts of similar size and shape. Note surrounding ground-glass attenuation with reticular opacity. (C) This low-power photograph of the histological section (hematoxylin–eosin stain) reveals macroscopic honeycombing (asterisk) corresponding to honeycombing on thin-section CT images and patchy fibrosis with architectural distortion and microscopic honeycombing reflecting ground-glass attenuation with reticular opacity. (D) Note dense fibrosis and fibroblastic foci (arrow) on high-power photographs of the histological section. (E) Masson’s trichrome stain reveals architecture destruction with scattered fibroblastic foci (arrow).
Abbreviations: UIP, usual interstitial pneumonia; CT, computed tomography.
Figure 6.
Combined SRIF and UIP patterns on thin-section CT images and histological findings.
Notes: (A) Thin-section CT images showing foci of clustered cysts of irregular size and shape and surrounding ground-glass attenuation with reticular or branching structures. (B) This low-power photograph of the histological section (hematoxylin–eosin stain) reveals areas with irregularly shaped emphysematous spaces (asterisk) and hyalinized fibrotic walls (arrow). (C) High-power photograph of a histological section. Note dense fibrosis and fibroblastic foci (arrow) in the same histological specimen. (D) Masson’s trichrome stain reveals architecture destruction with irregularly distributed dense fibrosis. The fibroblastic focus (arrow) is seen inside the fibrosis.
Abbreviations: SRIF, smoking-related interstitial fibrosis; UIP, usual interstitial pneumonia; CT, computed tomography.
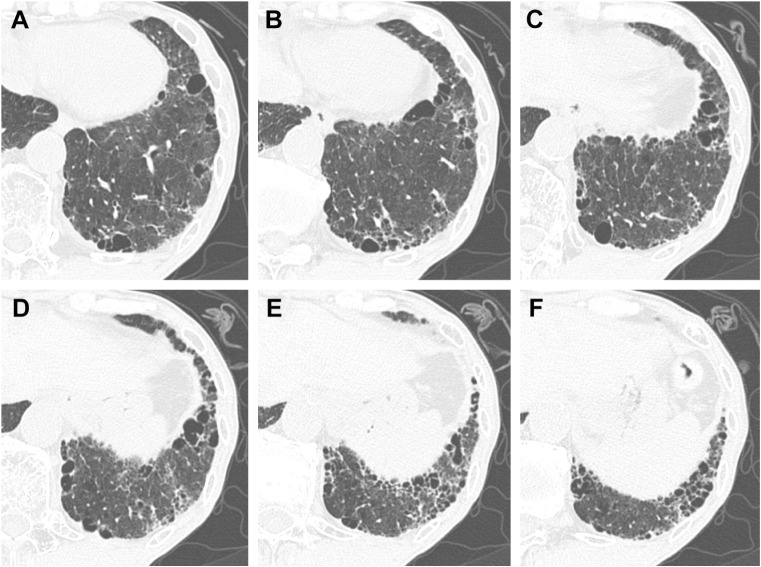
Figure 7.
Combined SRIF and UIP patterns on thin-section CT images.
Notes: (A–F) Thin-section CT images showing foci of clustered cysts of irregular size and shape and clustered cysts with similar size and shape accompanied by ground-glass attenuation and reticular or branching structures.
Abbreviations: SRIF, smoking-related interstitial fibrosis; UIP, usual interstitial pneumonia; CT, computed tomography.
Discussion
Although various interstitial lung abnormalities have been reported to be smoking-related, it is not clear how often these lesions are seen on TSCT scans of smokers. We observed GGAR only, CCVW with/without GGAR, or DICN in 66 (53.7%) of our 123 smokers. This incidence of interstitial changes is much higher than was reported by Washko et al,21 who found interstitial lung abnormalities including nondependent ground glass or reticular abnormalities, diffuse centrilobular nodularity, nonemphysematous cysts, honeycombing, and traction bronchiectasis in 8% of smokers included in their COPD gene study. In a lung cancer screening trial,25 UIP was seen in 0.3%, other chronic interstitial pneumonia in 3.8%, RB in 15.7%, and an indeterminate CT pattern in 3% of 692 smokers. The discrepancy between ours and earlier findings may be attributable to differences in the study populations; all of our study subjects underwent lobectomy primarily due to lung cancer. Kawabata et al15 observed AEF and UIP in 27.6% and 37.8% of 587 lobectomy specimens from smokers, and Katzenstein et al16 identified SRIF in 60% of their lobectomy specimens. These findings suggest that interstitial lung lesions are found more frequently in smokers with lung cancer than in other smokers and may also suggest that for early detection of lung cancer, smokers with subclinical interstitial abnormalities must be followed more closely than smokers without them. The special attention we paid to mild or localized interstitial changes on 1 mm-thick CT images may be another reason why their incidence was higher in our study than that in earlier studies.
Among the interstitial lung abnormalities related to smoking, a localized form of fibrosis or SRIF has been reported to be a relatively common histological finding. We identified SRIF in 78 (45.3%) of 172 resected lobes. Different names have been given to this histological finding, eg, AEF,15 clinically occult interstitial fibrosis or SRIF,16,17 RB-ILD with fibrosis,18 and RBF.19 However, the reported histological features seem to be similar and include foci of alveolar septal fibrosis distributed subpleurally and centrilobularly that are composed of distinct hyalinized collagen deposits without fibroblastic foci. Additionally, as was reported earlier, SRIF was not only a single finding but also frequently combined with pulmonary emphysema and RB. Therefore, AEF can be regarded as SRIF with pulmonary emphysema, and RBF seems to be almost equal to SRIF with RB. AEF might be a more appropriate term than SRIF with pulmonary emphysema to describe a single condition that is composed of emphysematous changes and thickened walls with collagenous fibrosis.
Although SRIF was demonstrated as GGAR, CCVW, or DICN on TSCT images, it must be noted that CT findings were normal in many of our patients with histological findings of SRIF. Similarly, only some patients with a histological diagnosis of pulmonary emphysema showed LAA on TSCT. When the degree of SRIF or pulmonary emphysema exceeded the resolution level of the CT image, these pathological changes could be detected on TSCT images and the combination of SRIF and pulmonary emphysema in the same lung area would appear as CCVW mimicking honeycombing. Regarding the location of SRIF with pulmonary emphysema, Reddy et al19 reported that RBF was seen predominantly in the upper lobes. However, they analyzed histological sections from five biopsy and two lobectomy specimens from only upper lobes so that the incidence of RBF in lower lobes remains unknown. We found that CCVW was identified more often in the lower lobes and in the peripheral zone than in the upper lobes and central zone, and SRIF with pulmonary emphysema was demonstrated more frequently than UIP in the histological analysis of CCVW. Therefore, it is more likely that while SRIF can arise anywhere in the lung, it is encountered more often in the lower lobes.
These results complicate the diagnosis of interstitial pneumonia because honeycombing, defined as clustered cystic airspaces characterized by well-defined walls,26,27 is the most important TSCT finding for the diagnosis of idiopathic pulmonary fibrosis.23 Although this seems to be a clear definition, the identification of honeycombing on CT scans is subjective, and observer agreement was only moderate even among experienced chest radiologists due to the presence of traction bronchiectasis, large cysts, and superimposed pulmonary emphysema.21 For a more accurate CT diagnosis, SRIF with pulmonary emphysema must be distinguished from honeycombing. In this respect, Watanabe et al28 recently reported that the maximum cyst wall thickness of multiple thin-walled cysts was significantly thinner than that of honeycombing. Although we felt the similar tendency regarding wall thickness, the accurate measurement of wall thickness of clustered cysts seems to be difficult practically due to limitation of special resolution of CT. In fact, we had a difficulty in separating thin from thick wall of clustered cysts so that we did not include wall thickness in detailed evaluation of clustered cysts in this study.
To elucidate the difference between SRIF with pulmonary emphysema and honeycombing, we evaluated TSCT images in more detail and compared additional TSCT findings with histological findings in 30 lobes with CCVW. TSCT analysis revealed that CCVW of markedly irregular size and shape was seen more often in specimens with only SRIF with pulmonary emphysema than with UIP lesions. On the other hand, round cysts of relatively similar size were present more often in specimens with UIP lesions than with only SRIF with pulmonary emphysema. The subpleural parenchyma was relatively less involved only in cases with SRIF with pulmonary emphysema. Therefore, a markedly irregular size and shape and relatively less involvement of the subpleural parenchyma may be useful findings suggesting the presence of SRIF with pulmonary emphysema when CCVW are seen on TSCT.
On the other hand, we document that the coexistence of UIP and SRIF with pulmonary emphysema was not a rare finding; this renders their differentiation difficult. But many of our patients with UIP lesions harbored predominantly round cysts of relatively similar size or manifested a regional mixture of areas with round and relatively similar size in addition to areas with clustered cysts of irregular size and shape. This suggests that UIP lesions basically show round cysts of relatively similar size, while in SRIF with pulmonary emphysema the cyst size and shape tend to be irregular. Therefore, when both CCVW of round and similar size and CCVW of irregular shape and size are seen on TSCT, the coexistence of UIP lesions and SRIF with pulmonary emphysema is possible.
The coexistence of UIP and SRIF raises the possibility that they reflect different phases of the same pathological process. However, in 68 of our lobectomy specimens, only SRIF was present with no UIP lesions anywhere and the degree of SRIF varied from mild to severe. Therefore, it seems unlikely that SRIF is the end stage of continuously progressive fibrotic changes such as UIP or NSIP. Rather, it would be reasonable to consider that SRIF is an independent pathological condition different from UIP.
Our study has some limitations. First, as it was retrospective we cannot rule out that selection bias affected the incidence of specific TSCT findings. Second, the number of patients with CCVW was small, and further study is necessary to elucidate the difference between honeycombing and SRIF with pulmonary emphysema. Third, the pathological findings in our lobectomy specimens could not be correlated with the exact same lung area on TSCT. Therefore, especially in patients with combined UIP and SRIF lesions, there is a possibility of location errors in correlating CT finding with pathological findings. However, an approximate correlation that takes into account the cystic shape and size would provide reasonable results regarding the pathological basis of CT findings. Fourth, we did not compare sequential changes in lobes with honeycombing and SRIF. To confirm clinical differences, additional studies must be performed to ascertain whether these changes are different in UIP and SRIF and whether and how they affect the prognosis.
Conclusion
CCVW are a relatively frequent TSCT finding in smokers, and SRIF with pulmonary emphysema rather than UIP is the predominant pathological pattern. TSCT findings such as marked irregularity in the cystic size and shape and less involvement of the subpleural parenchyma may be more suggestive of SRIF with pulmonary emphysema than honeycombing. Sequential changes in SRIF with pulmonary emphysema and honeycombing must be investigated to elucidate their clinical significance in smokers with interstitial lung abnormalities.
Supplementary material
High-power photograph of a normal lung.
Notes: The parenchyma of normal lung shows little fibrotic change compared with SRIF. The architectural destruction and emphysematous change are absent in normal lung.
Abbreviation: SRIF, smoking-related interstitial fibrosis.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Desai SR, Ryan SM, Colby TV. Smoking-related interstitial lung diseases: histopathological and imaging perspectives. Clin Radiol. 2003;58(4):259–268. doi: 10.1016/s0009-9260(02)00525-1. [DOI] [PubMed] [Google Scholar]
- 2.Selman M. The spectrum of smoking-related interstitial lung disorders. The never-ending story of smoke and disease. Chest. 2003;124(4):1185–1186. doi: 10.1378/chest.124.4.1185. [DOI] [PubMed] [Google Scholar]
- 3.Rao RN, Goodman LR, Tomashedski JF. Smoking-related interstitial lung disease. Ann Diagn Pathol. 2008;12(6):445–457. doi: 10.1016/j.anndiagpath.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 4.Moon J, du Bois RM, Colby TV, Hansell DM, Nicholson AG. Clinical significance of respiratory bronchiolitis on open lung biopsy and its relationship to smoking related interstitial lung disease. Thorax. 1999;54(11):1009–1014. doi: 10.1136/thx.54.11.1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heyneman LE, Ward S, Lynch DA, Remy-Jardin M, Johkoh T, Müller NL. Respiratory bronchiolitis, respiratory bronchiolitis-associated interstitial lung disease, and desquamative interstitial pneumonia: different entities or part of the spectrum of the same disease process? AJR Am J Roentgenol. 1999;173(6):1617–1622. doi: 10.2214/ajr.173.6.10584810. [DOI] [PubMed] [Google Scholar]
- 6.Ryu JH, Colby TV, Hartman TE, Vassallo R. Smoking-related interstitial lung diseases: a concise review. Eur Respir J. 2001;17(1):122–132. doi: 10.1183/09031936.01.17101220. [DOI] [PubMed] [Google Scholar]
- 7.Hidalgo A, Franquet T, Gimenez A, Bordes R, Pineda R, Madrid M. Smoking-related interstitial lung diseases: radiologic-pathologic correlation. Eur Radiol. 2006;16(11):2463–2470. doi: 10.1007/s00330-006-0340-0. [DOI] [PubMed] [Google Scholar]
- 8.Attili AK, Kazerooni EA, Gross BH, Flaherty KR, Myers JL, Martinez FJ. Smoking-related interstitial lung disease: radiologic-clinical-pathologic correlation. Radiographics. 2008;28(5):1383–1398. doi: 10.1148/rg.285075223. [DOI] [PubMed] [Google Scholar]
- 9.Baumgartner KB, Samet JM, Stidley CA, Colby TV, Waldron JA. Cigarette smoking: a risk factor for idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 1997;155(1):242–248. doi: 10.1164/ajrccm.155.1.9001319. [DOI] [PubMed] [Google Scholar]
- 10.Marten K, Milne D, Antoniou KM, et al. Non-specific interstitial pneumonia in cigarette smokers: a CT study. Eur Radiol. 2009;19(7):1679–1685. doi: 10.1007/s00330-009-1308-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cottin V, Nunes H, Brillet P-Y, et al. Groupe d’Etude et de Recherche sur les Maladies Orphelines Pulmonaires (GERM O P) Combined pulmonary fibrosis and emphysema: a distinct underrecognized entity. Eur Respir J. 2005;26(4):586–593. doi: 10.1183/09031936.05.00021005. [DOI] [PubMed] [Google Scholar]
- 12.Jankowich MD, Rounds SI. Combined pulmonary fibrosis and emphysema syndrome. A review. Chest. 2012;141(1):222–231. doi: 10.1378/chest.11-1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wright JL, Tazelaar HD, Churg A. Fibrosis with emphysema. Histopathology. 2010;58(4):517–524. doi: 10.1111/j.1365-2559.2010.03648.x. [DOI] [PubMed] [Google Scholar]
- 14.King TE. Smoking and subclinical interstitial lung disease. N Engl J Med. 2011;364(10):968–970. doi: 10.1056/NEJMe1013966. [DOI] [PubMed] [Google Scholar]
- 15.Kawabata Y, Hoshi E, Murai K, et al. Smoking-related changes in the background lung of specimens resected for lung cancer: a semiquantitative study with correlation to postoperative course. Histopathology. 2008;53(6):707–714. doi: 10.1111/j.1365-2559.2008.03183.x. [DOI] [PubMed] [Google Scholar]
- 16.Katzenstein AL, Mukhopadhyay S, Zanardi C, Dexter E. Clinically occult interstitial fibrosis in smokers: classification and significance of a surprisingly common finding in lobectomy specimens. Hum Pathol. 2010;41(3):316–325. doi: 10.1016/j.humpath.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 17.Katzenstein AL. Smoking-related interstitial fibrosis (SRIF), pathogenesis and treatment of usual interstitial pneumonia (UIP), and transbronchial biopsy in UIP. Mod Pathol. 2012;25(suppl 1):S68–S78. doi: 10.1038/modpathol.2011.154. [DOI] [PubMed] [Google Scholar]
- 18.Yousem SA. Respiratory bronchiolitis-associated interstitial lung disease with fibrosis is a lesion distinct from fibrotic nonspecific interstitial pneumonia: a proposal. Mod Pathol. 2006;19(11):1474–1479. doi: 10.1038/modpathol.3800671. [DOI] [PubMed] [Google Scholar]
- 19.Reddy TL, Mayo J, Churg A. Respiratory bronchiolitis with fibrosis. High-resolution computed tomography findings and correlation with pathology. Ann Am Thorac Soc. 2013;10(6):590–601. doi: 10.1513/AnnalsATS.201304-088OC. [DOI] [PubMed] [Google Scholar]
- 20.Lederer DJ, Enright PL, Kawut SM, et al. Cigarette smoking is associated with subclinical parenchymal lung disease. The multi-ethnic study of atherosclerosis (MESA)-lung study. Am J Respir Crit Care Med. 2009;180(5):407–414. doi: 10.1164/rccm.200812-1966OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Washko GR, Hunninghake GM, Fernandez IE, et al. COPDGene Investigators Lung volumes and emphysema in smokers with interstitial lung abnormalities. N Engl J Med. 2011;364(10):897–906. doi: 10.1056/NEJMoa1007285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Watadani T, Sakai F, Johkoh T, et al. Interobserver variability in the CT assessment of honeycombing in the lungs. Radiology. 2013;266(3):936–944. doi: 10.1148/radiol.12112516. [DOI] [PubMed] [Google Scholar]
- 23.Raghu G, Collard HR, Egan JJ, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183(6):788–824. doi: 10.1164/rccm.2009-040GL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.American Thoracic Society American Thoracic Society/European Respiratory Society international multidisciplinary consensus classification of the idiopathic interstitial pneumonia. Am J Respir Crit Care Med. 2002;165:277–304. doi: 10.1164/ajrccm.165.2.ats01. [DOI] [PubMed] [Google Scholar]
- 25.Sverzellati N, Guerci L, Randi G, et al. Interstitial lung diseases in a lung cancer screening trial. Eur Respir J. 2011;38(2):392–400. doi: 10.1183/09031936.00201809. [DOI] [PubMed] [Google Scholar]
- 26.Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J. Fleischner society: glossary of terms for thoracic imaging. Radiology. 2008;246(3):697–722. doi: 10.1148/radiol.2462070712. [DOI] [PubMed] [Google Scholar]
- 27.Arakawa H, Honma K. Honeycomb lung: history and current concepts. AJR Am J Roentgenol. 2011;196(4):773–782. doi: 10.2214/AJR.10.4873. [DOI] [PubMed] [Google Scholar]
- 28.Watanabe Y, Kawabata Y, Kanauchi T, et al. Multiple, thin-walled cysts are one of the HRCT features of airspace enlargement with fibrosis. Eur J Radiol. 2015;84(5):986–992. doi: 10.1016/j.ejrad.2015.01.015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
High-power photograph of a normal lung.
Notes: The parenchyma of normal lung shows little fibrotic change compared with SRIF. The architectural destruction and emphysematous change are absent in normal lung.
Abbreviation: SRIF, smoking-related interstitial fibrosis.