Abstract
The European Hematology Association (EHA) Roadmap for European Hematology Research highlights major achievements in diagnosis and treatment of blood disorders and identifies the greatest unmet clinical and scientific needs in those areas to enable better funded, more focused European hematology research. Initiated by the EHA, around 300 experts contributed to the consensus document, which will help European policy makers, research funders, research organizations, researchers, and patient groups make better informed decisions on hematology research. It also aims to raise public awareness of the burden of blood disorders on European society, which purely in economic terms is estimated at €23 billion per year, a level of cost that is not matched in current European hematology research funding. In recent decades, hematology research has improved our fundamental understanding of the biology of blood disorders, and has improved diagnostics and treatments, sometimes in revolutionary ways. This progress highlights the potential of focused basic research programs such as this EHA Roadmap.
The EHA Roadmap identifies nine ‘sections’ in hematology: normal hematopoiesis, malignant lymphoid and myeloid diseases, anemias and related diseases, platelet disorders, blood coagulation and hemostatic disorders, transfusion medicine, infections in hematology, and hematopoietic stem cell transplantation. These sections span 60 smaller groups of diseases or disorders.
The EHA Roadmap identifies priorities and needs across the field of hematology, including those to develop targeted therapies based on genomic profiling and chemical biology, to eradicate minimal residual malignant disease, and to develop cellular immunotherapies, combination treatments, gene therapies, hematopoietic stem cell treatments, and treatments that are better tolerated by elderly patients.
Introduction
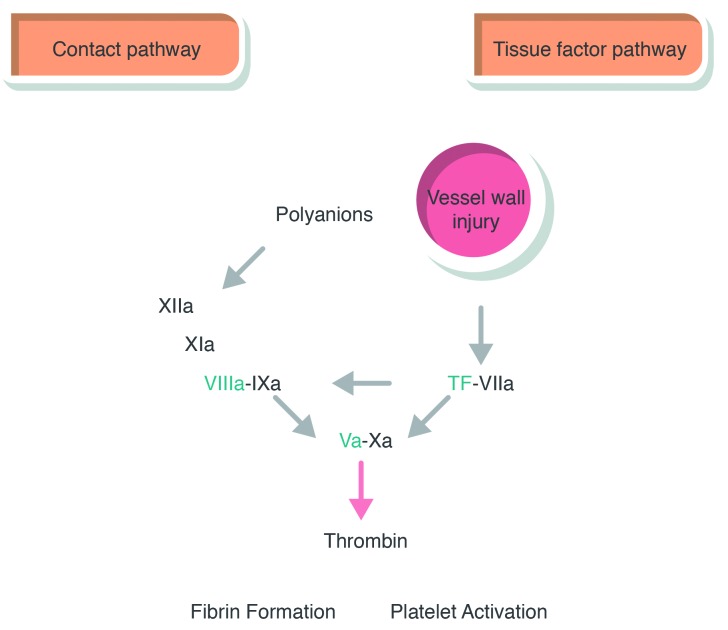
Blood can be described as one of the human body’s largest organs. It is essentially a liquid tissue containing many different types of specialized cells needed for the normal functioning of the human body. When one or more of these cell types do not perform well, a wide variety of blood disorders can result, ranging from blood cancers and coagulation and platelet disorders to very common diseases such as anemia.
Hematology is the medical discipline concerned with diagnosing and treating all of these diseases.
In the European Union (EU) alone, an estimated 80 million people are currently affected with blood disorders.
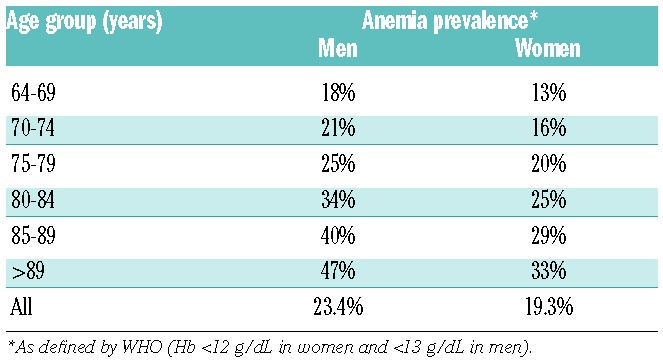
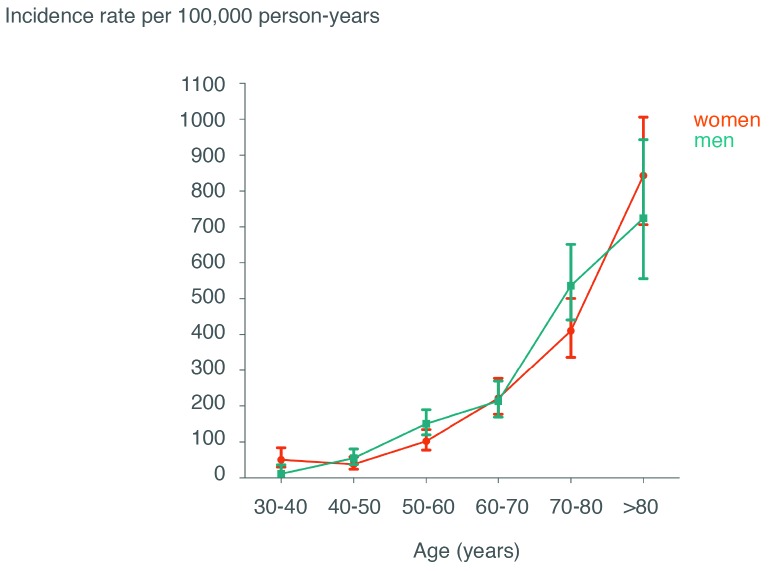
Various types of anemia affect more than 50 million children and adults in the World Health Organization’s European region.1 Blood cancers, some of which mainly affect young people, contribute strongly to premature cancer-related mortality and lost productivity in Europe.2 Among cancers, blood cancers [leukemia, Hodgkin and non-Hodgkin lymphomas (HLs and NHLs), and multiple myeloma] together rank third after lung cancer and colorectal cancer in terms of age-adjusted mortality in the European Economic Area.3
Inherited blood diseases, such as thalassemia, sickle cell disease, and glucose-6-phosphate dehydrogenase deficiency, also affect millions of people and cause substantial morbidity and mortality. Rarer forms of congenital blood disorders represent an immense burden on those affected. Many infectious diseases affect various types of blood or blood-forming cells, causing widespread diseases such as malaria and HIV/AIDS.
In recent decades, enormous progress has been made in terms of diagnosis and treatment of these diseases. Unfortunately, many blood disorders remain incurable. Approximately 115,000 patients die each year.4
Blood disorders have immense economic consequences as well. The combined societal cost of hematologic diseases for the EU, Norway, Iceland, and Switzerland has been estimated at €23 billion per year.
At a European level, current public spending on hematology research does not match this vast medical need. Of the €6.1 billion that the European Union allocated to health research under its 7th Framework Programme (2007–2013), only 2.2% (€137 million) was granted to hematology research. That amounts to less than 0.1% of the societal cost of blood disorders in Europe over that same period.
Milestones in hematology and the contribution from Europe
Research in hematology has fundamentally improved our understanding of the biology of hematologic diseases and resulted in many innovative discoveries. Many of these discoveries are powerful examples of how carefully designed basic research can lead to new approaches that block or interact with key pathways in diseased cells, resulting in very impressive anti-tumor effects. European hematologists have pioneered important inventions and played leading roles in developing, for example, curative approaches for patients with malignant diseases, such as lymphomas and leukemias,5,6 which often affect young patients.
Key milestones included the characterization of hemoglobin (Hb),7 induced pluripotent stem cells (iPSCs),8 and somatic driver mutations.9 The discovery of the Philadelphia chromosome and the subsequent identification of the BCR-ABL1 tyrosine kinase and its role in chronic myeloid leukemia (CML)10 led to the successful development of potentially curative targeted treatment in this form of blood cancer.11 This was an unprecedented rate of success and it occurred in a malignancy that previously could only be treated by allogeneic transplant in a very select number of patients. Acute promyelocytic leukemia became one of the first malignancies that could be cured without conventional chemotherapy.12
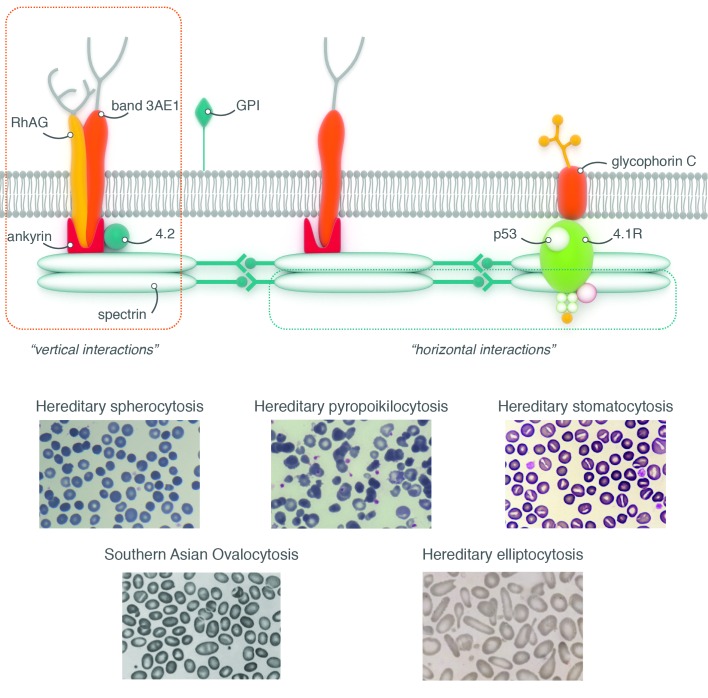
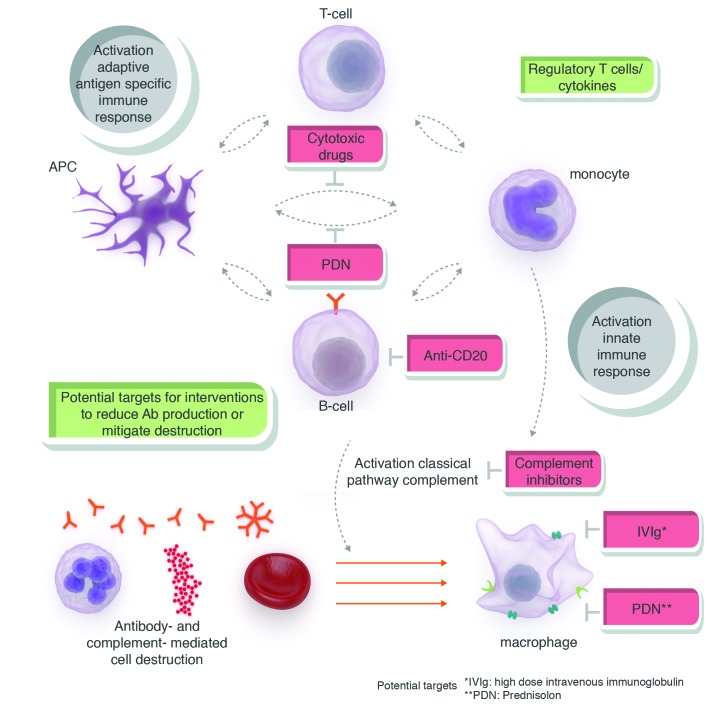
Another key development in hematology was that of a wide range of monoclonal antibodies following the original invention by Köhler and Milstein in the UK.13 Humanized or fully human monoclonal antibodies are now used in hematology for both diagnostic and therapeutic purposes. The clinical breakthrough was a humanized monoclonal antibody targeting the CD20 antigen on B-cell lymphoma.14 Today, monoclonal antibodies or antibody-based conjugates are used successfully in most malignant lymphomas and leukemias. They can, however, also be effective in nonmalignant blood disorders such as paroxysmal nocturnal hemoglobinuria (PNH), a rare acquired clonal stem cell defect leading to increased fragility of hematopoietic cells and hemolytic anemia (HA), thrombosis, and bone marrow failure (BMF). Prognosis of patients with severe PNH used to be less than five years, but changed radically with the advent of an anti-complement monoclonal antibody that counteracts membrane fragility.15 Today, PNH patients treated with this antibody have a normal life expectancy.
Severe hemophilia represents another story of unprecedented success. Patients used to be confined to wheelchairs or face the specter of death because of untreatable hemorrhage or blood-born infections such as HIV/AIDS. Today, new recombinant substitutive therapy is completely safe and effective in long-term prophylaxis. Hematology expects to further improve in this area, with innovative factor VIII or IX molecules that have increased activity and prolonged half-life.
Gene therapy is becoming a reality for more and more blood diseases, while treatment of malignant and nonmalignant hematologic diseases is impossible without blood transfusions and blood-derived medicinal products. “Haemovigilance”, a European initiative that provides a surveillance registry of serious unwanted transfusion effects, is now up and running in most EU member states.
European research policy
Governments, politicians and other policy makers carry the responsibility for making well informed decisions on regulation and funding priorities for health research and medicinal product development. The research community has a responsibility in providing policy makers with the kind of information and evidence that they need to make those informed decisions.
With respect to research funding, the authors feel that hematology was underfunded in the EU’s 7th Framework Programme. The current Framework Programme (Horizon 2020) was spared major budget cuts, but raising the relative level of funding for hematology research needs to be improved.
With respect to regulation, a key issue on the table is the EU’s new regulation on clinical trials on medicinal products for human use, which will come into effect in 2016. Over the past years, the number of clinical trials in Europe has decreased. These trials are key to medical research. European research groups have been instrumental in setting up multicenter clinical trials to test important new products. However, the new regulation has the potential of making future trials in Europe too expensive and too complex to carry out, especially in terms of academic research, and, therefore, may lead to a further decrease in clinical trials. A drop in the number of trials and the number of participants would harm the interests of European patients and damage Europe’s knowledge infrastructure and future economy.
The European Hematology Association Roadmap
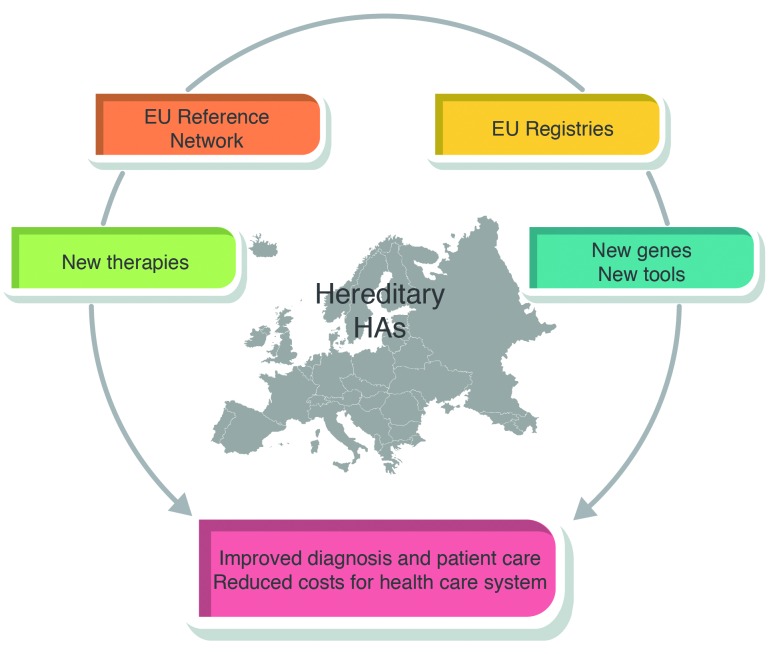
In 2014, at its 19th Annual Congress in Milan, Italy, the European Hematology Association (EHA), Europe’s largest non-profit membership organization in the field of hematology, decided to launch a Roadmap project. One of its goals was to better inform European policy makers and other stakeholders about the urgent needs and priorities of patients with blood diseases and the field of hematology. Another goal was to help the European hematology research community in harnessing resources by bringing basic researchers, clinical trial networks and patient advocates together in comprehensive study groups. A European consensus on medical and research priorities will also promote excellence and collaboration between academics and the pharmaceutical industry.
The EHA Roadmap Task Force included EHA board members and other top experts from all fields of hematology. Hundreds of hematologists, clinical trial groups, drug makers, national hematology societies, patient representatives and others were invited to provide input and advice. Many contributed to the drafting of the document and the various stages of review.
This Roadmap is the outcome of this project. It identifies the greatest unmet needs in hematology research and clinical science, describing: 1) state-of-the-art hematologic research; 2) the most urgent research priorities; and 3) the anticipated impact this research could have.
The EHA Roadmap Task Force identified nine major ‘sections’ in hematology: normal hematopoiesis, malignant lymphoid and myeloid diseases, anemias and related diseases, platelet disorders, blood coagulation and hemostatic disorders, transfusion medicine, infections in hematology, and hematopoietic stem cell transplantation (HSCT). For each section, the Roadmap Task Force appointed one or two editors. Together, the Roadmap Task Force and section editors drafted and reviewed a more detailed framework of 60 ‘subsections’ of groups of diseases and conditions. Section editors selected experts from their various fields to contribute as subsection editors or authors. Each section and subsection adapted the same basic format.
Draft texts and figures were discussed by the Roadmap Task Force and section editors during three meetings between October 2014 and March 2015. Sections were then reviewed by the Roadmap Task Force, the EHA board, and a selection of experts. The final draft was sent for consultation to stakeholders such as national hematology societies, patients’ organizations, hematology trial groups, and other European organizations in, for example, overlapping disease areas. All comments were discussed and integrated before submission of the manuscript to Haematologica.
In all, around 300 European hematologists and top experts helped to create the Roadmap.
At the request of the EHA board, the University of Oxford simultaneously carried out a study into the societal burden and cost of blood disorders in Europe. Outcomes from their analysis also informed various parts of this Roadmap.
Some dominating topics and unmet needs can be recognized in nearly all of the nine EHA Roadmap sections. They include:
developing novel targeted therapies based on genomic profiling and chemical biology;
unleashing the power of cellular immunotherapy;
eradicating minimal residual disease (MRD) in hematologic malignancies;
creating smarter combination treatments;
developing better tolerated treatments for blood disorders with a special emphasis on elderly patients;
using gene therapy to tackle blood disorders;
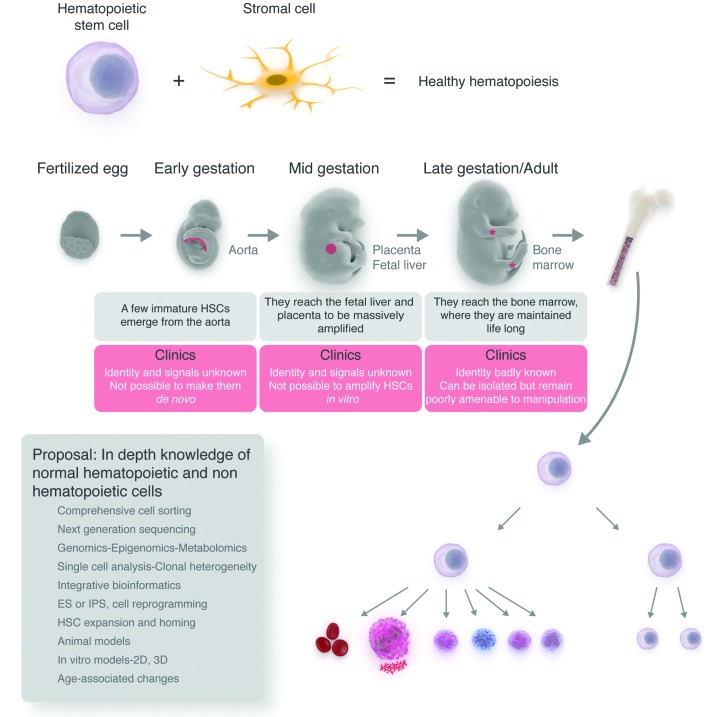
maximizing the clinical application of hematopoietic stem cells (HSCs) for transfusion, immunomodulation, and repair.
Taken together, this EHA Roadmap highlights major past achievements in the diagnostics and treatment of blood disorders, identifies unmet clinical and scientific needs in those same areas, and will enable better funded and more focused European hematology research.
The EHA will pro-actively bring this Roadmap to the attention of all stakeholders involved in hematology, and calls upon those stakeholders to do the same.