Abstract
Background
Current control policies for intestinal parasitosis focuses on soil-transmitted helminths, being ineffective against Giardia intestinalis, a highly prevalent protozoon that impacts children’s nutritional status in developing countries. The objective of this study was to explore spatial and molecular epidemiology of Giardia intestinalis in children of Amerindian descent in the Brazilian Amazon.
Methodology/Principal Findings
A cross sectional survey was performed in the Brazilian Amazon with 433 children aged 1 to 14 years. Fecal samples were processed through parasitological techniques and molecular characterization. Prevalence of G. intestinalis infection was 16.9% (73/433), reaching 22.2% (35/158) among children aged 2–5 years, and a wide distribution throughout the city with some hot spots. Positivity-rate was similar among children living in distinct socioeconomic strata (48/280 [17.1%] and 19/116 [16.4%] below and above the poverty line, respectively). Sequencing of the β-giardin gene revealed 52.2% (n = 12) of assemblage A and 47.8% (n = 11) of assemblage B with high haplotype diversity for the latter. The isolates clustered into two well-supported G. intestinalis clades. A total of 38 haplotypes were obtained, with the following subassemblages distribution: 5.3% (n = 2) AII, 26.3% (n = 10) AIII, 7.9% (n = 3) BIII, and 60.5% (n = 23) new B genotypes not previously described.
Conclusions/Significance
Giardia intestinalis infection presents a high prevalence rate among Amerindian descended children living in Santa Isabel do Rio Negro/Amazon. The wide distribution observed in a small city suggests the presence of multiple sources of infection, which could be related to environmental contamination with feces, possibly of human and animal origin, highlighting the need of improving sanitation, safe water supply and access to diagnosis and adequate treatment of infections.
Introduction
Among the intestinal parasites, Giardia intestinalis stands out for its high frequency in different socioenvironmental scenarios and its prevalence in both developed and developing countries [1–5]. G. intestinalis presents high levels of genetic diversity, which have been classified into eight assemblages (A-H). Parasites isolated from humans belong to the globally distributed assemblages A and B, which also have other animals as hosts, being potentially zoonotic [6]. Genotypes C and D have been described in domestic and wild canines, genotype E in domestic ruminants and pigs, F in cats, G in mice and rats and H in seals [7].
Infections with G. intestinalis occur after the ingestion of cysts in contaminated water, directly from person to person by fecal-oral contamination or, occasionally, from food [7]. Low-income populations residing in environments with poor household sanitation level and without safe water supply are more vulnerable to water and excreta-related diseases. Contaminated central water supplies can be the source of community-wide outbreaks or spreading of G. intestinalis [4]. Giardiasis prevalence ranges to 20–30% in developing countries and 2–7% in developed countries, being, in the latter, frequently related with day care center disease and public pools outbreaks, and also to travel-associated diarrhea [4,8].
Although G. intestinalis is an important cause of diarrhea, most infections have chronic and asymptomatic character [9]. The pathogenicity of G. intestinalis includes apoptosis of enterocytes, epithelial cell damage, and consequent malabsorption [10]. Importantly, G. intestinalis infection has been shown to impact the nutritional status of children, with the potential of seriously compromising their physical development [11–15].
While control policies for intestinal parasitoses have been successful against soil-transmitted helminths, these same policies are ineffective against protozoan parasites as the treatment for the diseases they cause requires different drugs and more complex ministration schedules [16–18]. Here we assessed the prevalence, spatial distribution and molecular epidemiology of G. intestinalis infection in children of Amerindian descent that live in a remote municipality in the Brazilian Amazon.
Materials and Methods
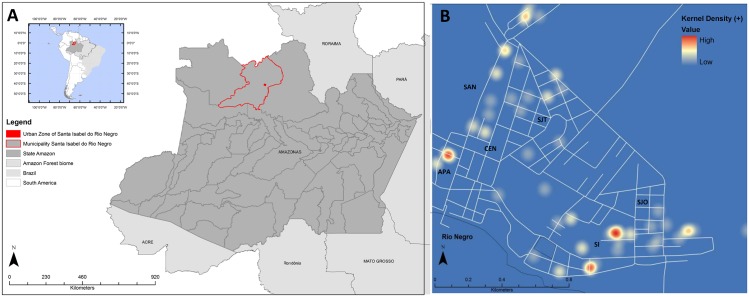
This study was a cross-sectional survey performed in 433 children from Santa Isabel do Rio Negro in 2011 (Fig 1A). This small city in Brazilian Amazon was occupied mainly by Amerindians, descendent from the Tukano and Aruak speaking societies. Although the overall population of this area was approximately 18,000 people, this study was conducted in the urban area, comprised of approximately 5,000 inhabitants, distributed among six districts: Aparecida (APA), Centro (CEN), Santa Inês (SI), São José Operário (SJO), São Judas Tadeu (SJT), and Santana (SAN). All children included in our study were at maximum 14 years old. None of them presented with diarrhea during the study. Containers without preservatives were distributed for stool samples collection, and parasitological tests were performed using ether sedimentation technique [19]
Fig 1.
A: Map of the study area in the Brazilian Amazon. B: Hotspot map of Giardia intestinalis cases in Santa Isabel do Rio Negro-AM, Brazil, in 2011, generated using the kernel method. Districts: APA- Aparecida; SAN- Santana; CEN- Centro; SJT- São Judas Tadeu; SI- Santa Inês; SJO- São José Operário. The maps were made with data provided by OpenStreetMap available under the Open Database License (https://www.openstreetmap.org/copyright).
Georeferencing was performed with a Global Position System in the SAD-69 geodetic datum. Spatial data were analyzed in a GIS platform using ArcGis 9.3® software (Environmental Systems Research Institute, Redlands, CA-USA). Maps were generated using the kernel density estimation method, and only first order effects were evaluated. The maps were made using data provided by OpenStreetMap® available under the Open Database License (https://www.openstreetmap.org/copyright).
DNA was extracted, in a field laboratory, only from parasitologicaly confirmed G. intestinalis-positive stool samples using the ZR Fungal/Bacterial DNA kit (ZymoResearch, Irvine-USA). For the amplification of the 753-bp β-giardin (βG) gene fragment we utilized the G7-G759 primers, as described by Cacciò et al. [20]. Products were purified using the Illustra-GFX kit (GE Healthcare, Pittsburgh, PA-USA) and sequenced with the ABI-BigDye Terminator kit (Applied Biosystems, Foster City, CA-USA) using ABI 3730 (Applied Biosystems) automated sequencer. In addition, sequences that presented double peaks were cloned using pGEM® T-Easy (Promega, Madison, WI-USA). Briefly, the inserts were amplified by PCR using the M13 primer and sequenced [21]. We used the Bioedit-7.1 and Mega-6.0 in order to edit and align the sequences.
Bayesian and maximum-likelihood phylogenetic trees based on 657-bp βG sequences were inferred with BEAST-1.8 and PhyML-3.0, respectively. The Akaike and Bayesian Information Criteria of jMODELTEST-2 were used to elect Tamura-Nei with four gamma categories as the best-fit evolutionary model for the dataset. Eighteen orthologous sequences representing the diversity of G. intestinalis (six of the eight known assemblages) were retrieved from GenBank and added to the analyses. Genealogies were reconstructed with Network-4.6 (Fluxus-Engineering, Inc.) using the median-joining method with maximum-parsimony post-processing.
Ethics Statement
This study was approved by the Evandro Chagas Research Institute Committee for Ethics on Research of FIOCRUZ (0011.0.009.000–3). The parent or legal guardian of all children included in this study provided written informed consent on their behalf.
Results and Discussion
The prevalence of G. intestinalis infection was 16.9% (73/433). Infection was more frequent among children aged 2–5 years old and among males (Table 1). In addition, giardiasis was observed in distinct income strata with similar frequencies.
Table 1. Distribution of Giardia intestinalis infection according to sociodemographic characteristics in Santa Isabel do Rio Negro-AM, Brazil, 2011.
| Characteristic | Number of Giardia intestinalis positive / examined subjects (% positive) | p-valuea |
|---|---|---|
| Locality | ||
| Aparecida | 7/47 (14.9%) | 0.026 |
| Centro | 3/20 (15.0%) | |
| Santana | 18/104 (17.3%) | |
| Santa Ines | 25/87 (28.7%) | |
| São José Operário | 11/104 (10.6%) | |
| São Judas Tadeu | 9/71 (12.7%) | |
| Sex | ||
| Female | 29/208 (14.0%) | 0.157 |
| Male | 44/225 (19.6%) | |
| Age (years) | ||
| 0–1 | 10/60 (16.7%) | 0.164 |
| 2–5 | 35/158 (22.2%) | |
| 6–11 | 25/192 (13.0%) | |
| 12–14 | 3/17 (17.6%) | |
| Unknown | 0/6 (0%) | |
| Income per capita per month (USD) USD 1 = BRL 4 | ||
| Below the poverty line (≤ 38.5) | 48/280 (17.1%) | 0.854 |
| Above the poverty line (> 38.5 and ≤ 330) | 19/116 (16.4%) | |
| Unknown | 6/37 (16.2%) |
aFisher exact test.
SI presented a significantly higher G. intestinalis positivity rate than the other districts (Table 1). A similar trend was observed with the kernel analysis that identified infection hotspots in the APA and SI districts (Fig 1B).
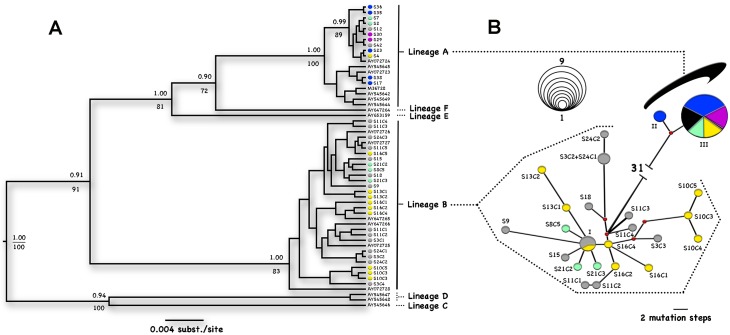
Since the extraction was performed in a field laboratory, it was possible to obtain DNA from 50/73 (68.5%) positive stool samples. From these, 23 (46.0%) were good-quality sequences (fragment of 657-bp). The isolates clustered into two well-supported G. intestinalis clades (Fig 2A). The assemblage frequencies were 52.2% (n = 12) for A and 47.8% (n = 11) for B. While assemblage A sequences obtained did not contain double-peaks, most assemblage B sequences did (n = 7), and were thus cloned. Up to five different haplotypes could be retrieved from a single sample in five clones analyzed.
Fig 2. Evolutionary relationships of Giardia intestinalis.
Each locality is represented by a different color. (A) Phylogenetic consensus tree of the 56 βG clone sequences. Posterior probabilities (Bayesian reconstruction) >0.9 and bootstrap values (ML tree) >70 are shown above and below the nodes, respectively. GenBank accession numbers for samples sequenced in other studies are shown in the terminal branches. (B) Median-joining network with maximum-parsimony post-processing. Each circle represents a unique haplotype; nodes represent median vectors. The size of each node is proportional to the number of sequences that shared the same haplotype (see scale) and the branch size is proportional to the number of mutational steps. For improved graphic resolution, the distance between assemblages A and B is not proportional (31 mutational steps). Color key: Blue—APA; Yellow- SAN; Red- CEN; Purple- SJT; Gray- SI; Green- SJO. Sample IDs: I—S11C5, S16C5 and S24C3; II—S17 and S38; and III—S4, S7, S12, S23, S29, S30, S35, S36 and S42. The other IDs concord with Table 2.
G. intestinalis assemblages A and B are widely distributed in the studied region (Fig 2B). Assemblage A exhibited low haplotype diversity, with two haplotypes separated from each other by two mutation steps. One haplotype of assemblage A was observed in five of the six districts, and the other one only in APA. On the other hand, assemblage B exhibited high haplotype diversity (Hd = 0.85), with 22 different haplotypes separated by 1–10 mutation steps. These were present in four districts and only one haplotype was shared between two localities, APA and SI.
A total of 38 haplotypes were obtained, with the following subassemblages distribution: 5.3% (n = 2) AII, 26.3% (n = 10) AIII, 7.9% (n = 3) BIII, and 60.5% (n = 23) new B genotypes not previously described (Table 2). Two distinct epidemiological scenarios were observed. While children living in the same house were infected by the same assemblage, surprisingly children in one house were infected by distinct assemblages (AIII and new B haplotypes).
Table 2. Molecular characterization of isolates from Santa Isabel do Rio Negro, Amazonas, Brazil.
| Community | Sample ID | Assemblage | Subassemblage | GenBank accession number |
|---|---|---|---|---|
| Aparecida | S17 | A | AII | KU504725 |
| Aparecida | S23 | A | AIII | KU504729 |
| Aparecida | S35 | A | AIII | KU504735 |
| Aparecida | S36 | A | AIII | KU504736 |
| Aparecida | S38 | A | AII | KU504737 |
| Centro | S8 | B | New | KU504707 |
| Santa Inês | S3C1 | B | New | KU504702 |
| Santa Inês | S3C2 | B | New | KU504703 |
| Santa Inês | S3C3 | B | New | KU504704 |
| Santa Inês | S9 | B | New | KU504708 |
| Santa Inês | S11C1 | B | New | KU504712 |
| Santa Inês | S11C2 | B | New | KU504713 |
| Santa Inês | S11C3 | B | New | KU504714 |
| Santa Inês | S11C4 | B | New | KU504715 |
| Santa Inês | S11C5 | B | BIII | KU504716 |
| Santa Inês | S12 | A | AIII | KU504717 |
| Santa Inês | S15 | B | New | KU504720 |
| Santa Inês | S18 | B | New | KU504726 |
| Santa Inês | S24C1 | B | New | KU504730 |
| Santa Inês | S24C2 | B | New | KU504731 |
| Santa Inês | S24C3 | B | BIII | KU504732 |
| Santa Inês | S42 | A | AIII | KU504738 |
| São José Operário | S2 | A | AIII | KU504701 |
| São José Operário | S7 | A | AIII | KU504706 |
| São José Operário | S21C2 | B | New | KU504727 |
| São José Operário | S21C3 | B | New | KU504728 |
| São Judas Tadeu | S29 | A | AIII | KU504733 |
| São Judas Tadeu | S30 | A | AIII | KU504734 |
| Santana | S4 | A | AIII | KU504705 |
| Santana | S10C3 | B | New | KU504709 |
| Santana | S10C4 | B | New | KU504710 |
| Santana | S10C5 | B | New | KU504711 |
| Santana | S13C1 | B | New | KU504718 |
| Santana | S13C2 | B | New | KU504719 |
| Santana | S16C1 | B | New | KU504721 |
| Santana | S16C2 | B | New | KU504722 |
| Santana | S16C4 | B | New | KU504723 |
| Santana | S16C5 | B | BIII | KU504724 |
G. intestinalis infection was distributed throughout the city, with some hotspots of higher frequency. Interestingly, G. intestinalis positivity is not associated with income stratum. The wide distribution observed in a small city suggests the presence of multiple sources of infection, which could be related to environmental contamination with feces, possibly of human and animal origin [22]. Many houses do not have access to potable water, being served by two sources: “black water”, which is drawn from the Rio Negro and chlorinated in a plant, and “white water”, which is taken up in wells. The vast majority of homes do not have septic tanks or latrines and the disposal of feces is done directly in the river. This practice may facilitate the spread of different haplotypes of G. intestinalis. The observed hotspots on the margins of the Rio Negro suggest that people who live closer to the river are at greater risk of becoming infected.
The high genetic divergence between A and B (5.5–6.3%) supports previous proposal for their separation in two taxa, G. intestinalis and Giardia enterica [23, 24]. Assemblage A haplotypes detected in the present study are identical to European strains [20], evidencing their low genetic divergence. In contrast, assemblage B haplotypes were highly diverse, being possible to observe up to five different clones in a single sample. Previous genome sequencing analysis evidenced a 10-fold difference in heterozygosity levels between assemblages A and B [24], but the reasons for such difference are still unknown and deserves further investigation.
The Amazon region is the largest drainage basin in the world and harbors one-fifth of the fresh water reserves on the planet. Paradoxically, the living conditions of many people who inhabit this basin are substandard, favoring the transmission of fecal-oral diseases such as giardiasis. It has been proposed that the routine water treatment practices usually employ concentrations of chlorine able to inactivate only bacterial and viral pathogens, but not Giardia cysts [25–26]. Thus, adequate control of giardiasis, particularly in Amazon region requires the improvement of drinking water quality and reduction of environmental contamination with feces [27]. Despite the high prevalence of giardiasis and its health impact worldwide, large-scale interventions—as those implemented for STH control—are lacking in developing countries. In this context, enteric protozoa infections emerge as neglected conditions in the STH control era [18].
Acknowledgments
We thank the Master’s degree students in Tropical Medicine (Daniel C. Portela Camara, Amanda C. de Souza, Angélica T. de L. Barbosa, Andrea M. de A. Cabral, Carlos Vinicio C. Guacho, Daiana de J. Hardoim, Fábio B. dos Santos, Leonardo S. de Assunção, Manoela H. da Silva, Moyra M. Portilho, and Vanessa A. Marques) from Fiocruz for essential assistance in field work and the administrative staff of Santa Isabel do Rio Negro for lodging the research team. This work was supported by the Oswaldo Cruz Foundation (Fiocruz) and the Brazilian Federal Agency for Support and Evaluation of Graduate Education (CAPES)/ Brazilian Ministry of Education and Ministry of Social Development, in the context of the CAPES-Fiocruz-Brazil without Poverty Plan. This work was performed at the Laboratory of Epidemiology and Molecular Systematics, Oswaldo Cruz Institute, Oswaldo Cruz Foundation, Rio de Janeiro.
Data Availability
All relevant data are within the paper.
Funding Statement
This work was supported by the Oswaldo Cruz Foundation (Fiocruz) and the Brazilian Federal Agency for Support and Evaluation of Graduate Education (CAPES)/ Brazilian Ministry of Education and Ministry of Social Development, in the context of the CAPES-Fiocruz-Brazil without Poverty Plan.
References
- 1.Ehsan AM, Geurden T, Casaert S, Parvin SM, Islam TM, Ahmed UM, et al. Assessment of zoonotic transmission of Giardia and Cryptosporidium between cattle and humans in rural villages in Bangladesh. PLoS One. 2015;10(2):e0118239 10.1371/journal.pone.0118239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barry MA, Weatherhead JE, Hotez PJ, Woc-Colburn L. Childhood parasitic infections endemic to the United States. Pediatr Clin North Am. 2013;60(2):471–85. 10.1016/j.pcl.2012.12.011 [DOI] [PubMed] [Google Scholar]
- 3.Jenkins EJ, Castrodale LJ, de Rosemond SJ, Dixon BR, Elmore SA, Gesy KM, et al. Tradition and transition: parasitic zoonoses of people and animals in Alaska, northern Canada, and Greenland. Adv Parasitol. 2013;82:33–204. 10.1016/B978-0-12-407706-5.00002-2 [DOI] [PubMed] [Google Scholar]
- 4.Fletcher SM, Stark D, Harkness J, Ellis J. Enteric protozoa in the developed world: a public health perspective. Clin Microbiol Rev. 2012;25(3):420–49. 10.1128/CMR.05038-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.David ÉB, Guimarães S, de Oliveira AP, Goulart de Oliveira-Sequeira TC, Nogueira Bittencourt G, Moraes Nardi AR, et al. Molecular characterization of intestinal protozoa in two poor communities in the State of São Paulo, Brazil. Parasit Vectors. 2015;15(8):103 10.1186/s13071-015-0714-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cacciò SM, Sprong H. Giardia duodenalis: genetic recombination and its implications for taxonomy and molecular epidemiology. Exp Parasitol. 2010;124(1): 107–112. 10.1016/j.exppara.2009.02.007 [DOI] [PubMed] [Google Scholar]
- 7.Feng Y, Xiao L. Zoonotic potential and molecular epidemiology of Giardia species and giardiasis. Clin Microbiol Rev. 2011;24(1):110–40. 10.1128/CMR.00033-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garbossa G, Pía Buyayisqui M, Geffner L, López Arias L, de la Fournière S, Haedo AS, et al. Social and environmental health determinants and their relationship with parasitic diseases in asymptomatic children from a shantytown in Buenos Aires, Argentina. Pathog Glob Health. 2013;107(3):141–52. 10.1179/2047773213Y.0000000087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kotloff KL, Nataro JP, Blackwelder WC, Nasrin D, Farag TH, Panchalingam S, et al. Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the Global Enteric Multicenter Study, GEMS): a prospective, case-control study. Lancet. 2013;382:209–222. 10.1016/S0140-6736(13)60844-2 [DOI] [PubMed] [Google Scholar]
- 10.Luther A, Bartelt LA, Sartor RB. Advances in understanding Giardia: determinants and mechanisms of chronic sequelae. F1000Prime Rep. 2015;7:62 10.12703/P7-62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carvalho-Costa FA, Gonçalves AQ, Lassance SL, Silva Neto LM, Salmazo CA, Bóia MN. Giardia lamblia and other intestinal parasitic infections and their relationships with nutritional status in children in Brazilian Amazon. Rev Inst Med Trop São Paulo. 2007;49(3):147–153. [DOI] [PubMed] [Google Scholar]
- 12.Ignatius R, Gahutu JB, Klotz C, Steininger C, Shyirambere C, Lyng M, et al. High prevalence of Giardia duodenalis Assemblage B infection and association with underweight in Rwandan children. PLoS Negl Trop Dis. 2012;6(6):e1677 10.1371/journal.pntd.0001677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nematian J, Gholamrezanezhad A, Nematian E. Giardiasis and other intestinal parasitic infections in relation to anthropometric indicators of malnutrition: a large, population-based survey of schoolchildren in Tehran. Ann Trop Med Parasitol. 2008;102(3):209–214. 10.1179/136485908X267876 [DOI] [PubMed] [Google Scholar]
- 14.Quihui L, Morales GG, Méndez RO, Leyva JG, Esparza J, Valencia ME. Could giardiasis be a risk factor for low zinc status in schoolchildren from northwestern Mexico? A cross-sectional study with longitudinal follow-up. BMC Public Health. 2010;10:85 10.1186/1471-2458-10-85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Verhagen LM, Incani RN, Franco CR, Ugarte A, Cadenas Y, Sierra Ruiz CI, et al. High malnutrition rate in Venezuelan Yanomami compared to Warao Amerindians and Creoles: significant associations with intestinal parasites and anemia. PLoS One. 2013;8:e77581 10.1371/journal.pone.0077581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ferreira FS, Baptista-Fernandes T, Oliveira D, Rodrigues R, Neves E, Lima A, et al. Giardia duodenalis and soil-transmitted helminths infections in children in São Tomé and Príncipe: do we think Giardia when addressing parasite control? J Trop Pediatr. 2015;61(2):106–112. 10.1093/tropej/fmu078 [DOI] [PubMed] [Google Scholar]
- 17.Macchioni F, Segundo H, Gabrielli S, Totino V, Gonzales PR, Salazar E, et al. Dramatic decrease in prevalence of soil-transmitted helminths and new insights into intestinal protozoa in children living in the Chaco region, Bolivia. Am J Trop Med Hyg. 2015;92(4):794–796. 10.4269/ajtmh.14-0039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Turkeltaub JA, McCarty TR 3rd, Hotez PJ. The intestinal protozoa: emerging impact on global health and development. Curr Opin Gastroenterol. 2015;31(1):38–44. 10.1097/MOG.0000000000000135 [DOI] [PubMed] [Google Scholar]
- 19.Ritchie LS. An ether sedimentation technique for routine stool examination. Bull U S Army Med Depart 1948;8:326. [PubMed] [Google Scholar]
- 20.Cacciò S, De Giacomo M, Pozio E. Sequence analysis of the β-giardin gene and development of a polymerase chain reaction-restriction fragment length polymorphism assay to genotype Giardia duodenalis cysts from human faecal samples. Int J Parasitol. 2002;32(8):1023–1030. [DOI] [PubMed] [Google Scholar]
- 21.Messing J. M13 cloning vehicles. Their contribution to DNA sequencing. Methods Mol Biol. 1993;23:9–22. [DOI] [PubMed] [Google Scholar]
- 22.Durigan M, Abreu AG, Zuccenhi MI, Franco RM, de Souza AP. Genetic diversity of Giardia duodenalis: multilocus genotyping reveals zoonotic pottial between clinical and environmental sources in a metropolitan region of Brazil. PLoS One. 2014; 9(12):e115489 10.1371/journal.pone.0115489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Monis PT, Caccio SM, Thompson RC. Variation in Giardia: towards a taxonomic revision of the genus. Trends Parasitol. 2009;25(2):93–100. 10.1016/j.pt.2008.11.006 [DOI] [PubMed] [Google Scholar]
- 24.Adam RD, Dahlstrom EW, Martens CA, Bruno DP, Barbian KD, Ricklefs SM, et al. Genome sequencing of Giardia lamblia genotypes A2 and B isolates (DH and GS) and comparative analysis with the genomes of genotypes A1 and E (WB and Pig). Genome Biol Evol. 2013;5(12):2498–511. 10.1093/gbe/evt197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nygard K, Schimmer B, Søbstad Ø, Walde A, Tveit I, Langeland N, Hausken T, Aavitsland P. A large community outbreak of waterborne giardiasis-delayed detection in a non-endemic urban area. BMC Public Health. 2006;6:141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Triviño-Valencia J, Lora F, Zuluaga JD, Gomez-Marin JE. Detection by PCR of pathogenic protozoa in raw and drinkable water samples in Colombia. Parasitol Res. 2016;115(5):1789–97. 10.1007/s00436-016-4917-5 [DOI] [PubMed] [Google Scholar]
- 27.Robertson LJ, Lim YAL. Waterborne and Environmentally-Borne Giardiasis In: Luján HD, Svärd S. Giardia: A model organism. Springer Wien, New York; 2011. pp. 29–61. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.