Abstract
Background
New Delhi metallo-beta-lactamase-1(NDM-1) is a novel type of metallo-beta-lactamase (MBL) which inactivates all β-lactam antibiotics except aztreonam. Enterobacteriaceae expressing NDM-1 have been identified worldwide. The aim of this study was to detect MBLs in carbapenem-resistant K. pneumoniae isolates obtained from patients hospitalized in one of the university hospitals in Isfahan, Iran.
Methods
Of the 112 isolates obtained from various clinical samples, 49 were selected for carbapenemase detection based on their reduced susceptibility to imipenem or meropenem according to the disc diffusion method. These isolates were screened for carbapenemase and MBL production using the Modified Hodge Test (MHT) and Epsilometer test (E-test) MBL strips. Polymerase chain reaction was performed on all 49 isolates using specific primers to detect genes encoding IMP (active on imipenem), VIM (Verona integron-encoded metallo-β-lactamase), SPM-1 (Sao Paulo metallo-β-lactamase) and NDM-1.
Results
Among 49 carbapenem-resistant isolates, 32 (65.3 %) were positive for MHT and 6 (12.2 %) were found positive for blaNDM-1. Other MBL genes were not detected.
Conclusion
This is the second report on the detection of blaNDM-1 in Iran since it was first reported by Shahcheraghi and colleagues in 2012. This study indicated that resistance to carbapenems and isolation of bacteria producing NDM-1 is increasing. Therefore, the rapid detection of isolates expressing NDM-1 is essential to control their spread. Hippokratia 2015; 19 (3): 205-209.
Keywords: New Delhi metallo-beta-lactamase-1, Klebsiella pneumoniae, carbapenem, Modified Hodge test, Epsilometer test
Introduction
Klebsiella pneumoniae is an important nosocomial pathogen causing urinary tract, respiratory tract, and bloodstream infections1. It is the second most common cause of nosocomial Gram-negative bacteremia after Escherichia coli (E. coli). As an opportunistic pathogen, Klebsiella spp. often affects immunocompromised individuals receiving treatment for other severe underlying diseases, such as diabetes mellitus and chronic pulmonary obstruction2. Beta-lactam antibiotics are widely used to treat infections caused by Gram-negative pathogens. However, the efficacy of these drugs is reduced considerably due to the appearance of extended-spectrum beta-lactamases (ESBLs) and the consequent emergence of multi-drug resistant (MDRs) strains3. Carbapenems are the most important therapeutic agents used to treat infections caused by MDR Gram-negative bacteria. However, their efficacy is threatened by the emergence of resistant isolates4,5. Carbapenemases represent a heterogeneous group of beta-lactamases from various molecular classes (A, B and D).The emergence of acquired metallo-beta-lactamases (MBLs) among major Gram-negative pathogens has clinical and epidemiological implications and causes particular concern worldwide6. MBLs have been reported in many geographic areas. The most common acquired MBLs include IMP (active on imipenem), VIM (Verona integron-encoded metallo-β-lactamase), SPM (Sao Paulo metallo-β-lactamase), GIM (German imipenemase), SIM (Seoul imipenemase), and NDM-1 (New Delhi metallo-beta-lactamase-1) enzymes7,8. New Delhi Metallo-beta-lactamase was first reported in K. pneumoniae and E .coli isolated from a Swedish 59-year-old patient from India that was previously admitted to a hospital in New Delhi7.
MBL genes are located within a variety of integron structures. Horizontal transfer of integrons carrying MBL genes that is associated with plasmids or transposons between bacteria, plays an important role in the occurrence of resistance to beta-lactam antibiotics in the community and hospitals3,8. Because of poor treatment and increased mortality rate related to the infections caused by these organisms, the early detection of MBL-producing organisms for infection control purposes and the prevention of nosocomial outbreaks is very important.
The aim of the present study was to determine the presence of MBL genes among carbapenem-resistant K. pneumoniae isolates obtained from hospitalized patients in a university hospital in Isfahan, Iran.
Methods
Clinical isolates
One hundred twelve K. pneumoniae isolates were collected from various clinical specimens including: urine (n =46), tracheal aspirate (n =21), bronchoalveolar-lavage (BAL) fluid (n =10), wound (n =10), abscess (n =7), cerebrospinal fluid (n =3), sputum (n =2), catheter (n =2), and eye (n =1) between March 2012 and March 2013 from hospitalized patients at the main university hospital of Isfahan, Iran. The specimens were identified by standard laboratory methods and API20E system (BioMerieux, Marcy l’Etoile, France). Isolates were then preserved at -80˚C in Brain-heart infusion (BHI) broth containing 20% glycerol.
Antimicrobial susceptibility testing
The antibiotic susceptibility of isolates was determined using the disc diffusion technique (Kirby-Bauer) on Muller-Hinton agar plates. Results were interpreted according to the guidelines of the Clinical and Laboratory Standards Institute (CLSI), January 20129. The antibiotic discs used in this study were amikacin (30 µg), gentamicin (10 µg), ciprofloxacin (5 µg), levofloxacin (5 µg), ceftazidime (30 µg), cefepime (30 µg), piperacillin (100 µg), piperacillin/tazobactam (110 µg) and aztreonam (30 µg) (Mast Group Limited, Merseyside, UK). E. coli ATCC® 25922™ was used as the quality control for antimicrobial susceptibility test. The minimum inhibitory concentrations (MICs) of imipenem were determined using E-test strips (Liofilchem, Roseto degli Abruzzi, Italy) for imipenem and meropenem resistant isolates.
Phenotypic detection of MBLs
All imipenem and meropenem-resistant isolates were examined for MBL production using the Modified Hodge test (MHT) and Epsilometer test (E-test) MBL strips. The MHT was carried out according to CLSI guidelines using a 10μg disc of ertapenem on Muller–Hinton agar plates. Following overnight incubation, the presence of a “cloverleaf shaped” inhibition zone was interpreted as a positive result10. E. coli ATCC® 25922™ was used as the carbapenem-susceptible strain. The detection of MBLs was carried out using E-tests according to the manufacturer’s instructions (Liofilchem, Roseto degli Abruzzi, Italy). The E-test MBL strips contained imipenem (4 to 256 µg/ml) and imipenem (1 to 64 µg/ml)-EDTA combinations. A three-fold or greater reduction in imipenem MIC in the presence of EDTA was interpreted as the positive result. Furthermore, the presence of a “phantom” zone between the two gradient sections or a deformation of the imipenem ellipses was considered as a marker of MBL production11. Pseudomonas aeruginosa ATCC® 27853™ strain was used as a negative control.
Polymerase chain reaction (PCR) amplification and DNA sequencing
Genomic DNA was extracted using the DNA Extraction Kit (Sinaclon, Iran) according to the manufacturer’s directions. All carbapenem-resistant isolates were screened by standard PCR using specific primers for MBL genes (Table 1). Standard strains for blaVIM, blaIMP, and blaSPM genes were provided by the Pasteur Institute of Iran. PCR fragments were sequenced at Macrogen Inc. (Seoul, Korea). The sequences were then confirmed using the NCBI web site (http://www.ncbi.nlm.nih.gov/).
Table 1. Forward (F) and Reverse (R) primer pairs used for the detection of metallo-beta-lactamases (MBLs) in K. pneumoniae isolates.
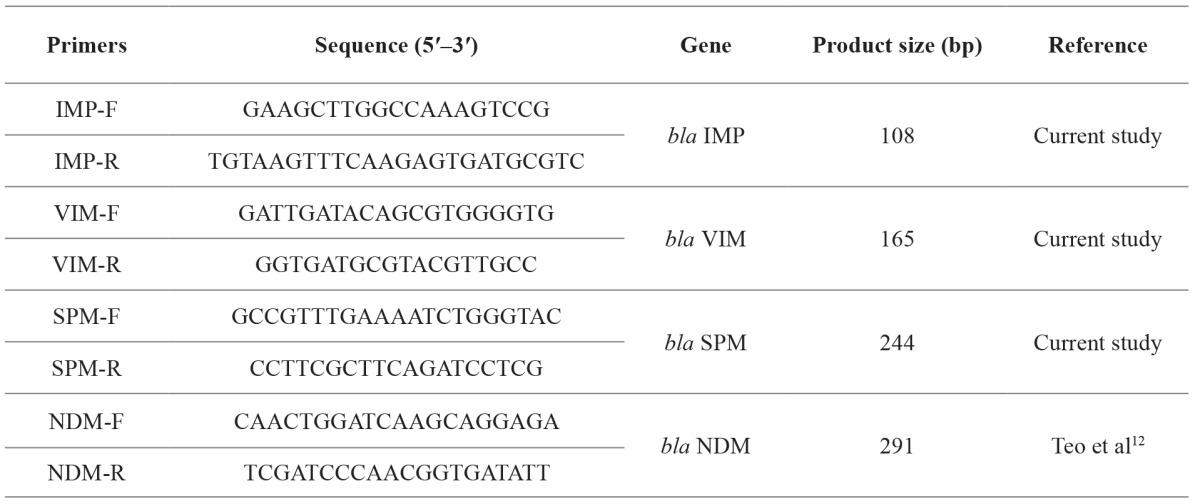
bp: basepairs, F: Forward primer pairs, R: Reverse primer pairs.
Ethics Statement
The Ethics Committee of the Faculty of Medical School, Isfahan University of Medical Sciences approved the study (no 290284), and the author group collected written informed consent from the patients.
Results
Antimicrobial susceptibility test
The antimicrobial susceptibility results for all 112 isolates are summarized in Table 2. In total, 80.3 % (n =90) of the isolates were resistant to 3 or more antibiotics of different classes and were determined as multidrug resistant (MDR). High-level resistance to piperacillin, ceftazidime and ciprofloxacin was observed in 88.4 % (n =99), 83 % (n =93) and 63.4 % (n =71) of the isolates respectively.
Table 2. Antimicrobial susceptibility results. In this study, high-level resistance to piperacillin, ceftazidime and ciprofloxacin was observed. Also, from 112 K. pneumoniae isolates, 49 isolates were resistant to imipenem and meropenem.
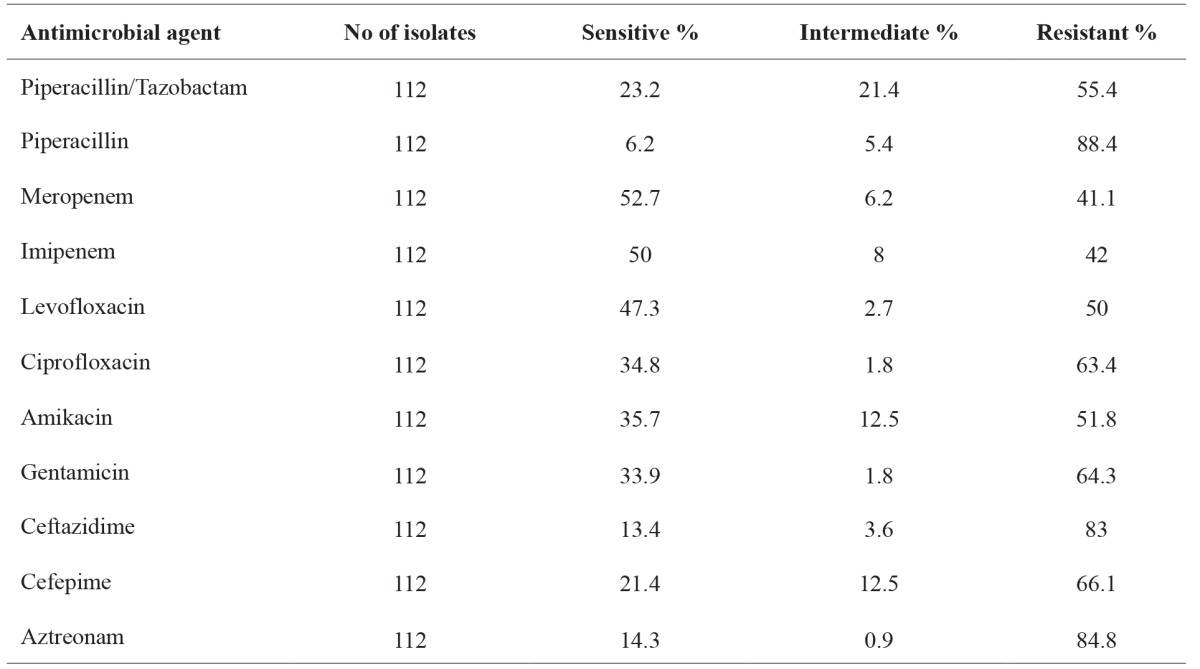
Susceptibility of selected antimicrobials was obtained using the disc diffusion technique on Muller-Hinton agar plates and were interpreted according to the guidelines of the Clinical and Laboratory Standards Institute (CLSI), January 2012. No: number.
From 112 K. pneumoniae isolates, a total number of 49 isolates were screened for carbapenemase production based on their reduced sensitivity to imipenem and meropenem.
MBL detection
From 49 carbapenem-resistant isolates, MHT indicated that 65.3% (32/49) of the isolates were carbapenemase-producers. Moreover, E-test MBL strips demonstrated that 10.2% (5/49) of the isolates were MBL-producers.
PCR screening for MBL-encoding genes and sequencing
PCR using specific primers for VIM, IMP, SPM and NDM-1 genes was performed on all the IMP-resistant isolates. A 291 bp fragment representing blaNDM-1 gene was amplified in 12.2% (n =6) of the isolates, including all those that were positive by the E-test MBL strips. Therefore, there was no false positive result for E-test MBL strips. However, there was one MBL-positive isolate that was negative for the E-test MBL strips. Alignment of the blaNDM-1 PCR fragment sequence with other blaNDM-1 sequences displayed on the GenBank database revealed a 97-100% similarity. We submitted two nucleotide sequences of blaNDM-1 gene, determined in this study, to the GenBank nucleotide sequence database under the accession numbers of KF734093 and KF734094. The characteristics of the MBL positive isolates are summarized in Table 3.
Table 3. Characteristics of metallo-beta-lactamase-producing isolates. From 49 carbapenem-resistant isolates, 6 isolates were positive for New Delhi metallo-beta-lactamase-1 (blaNDM-1).
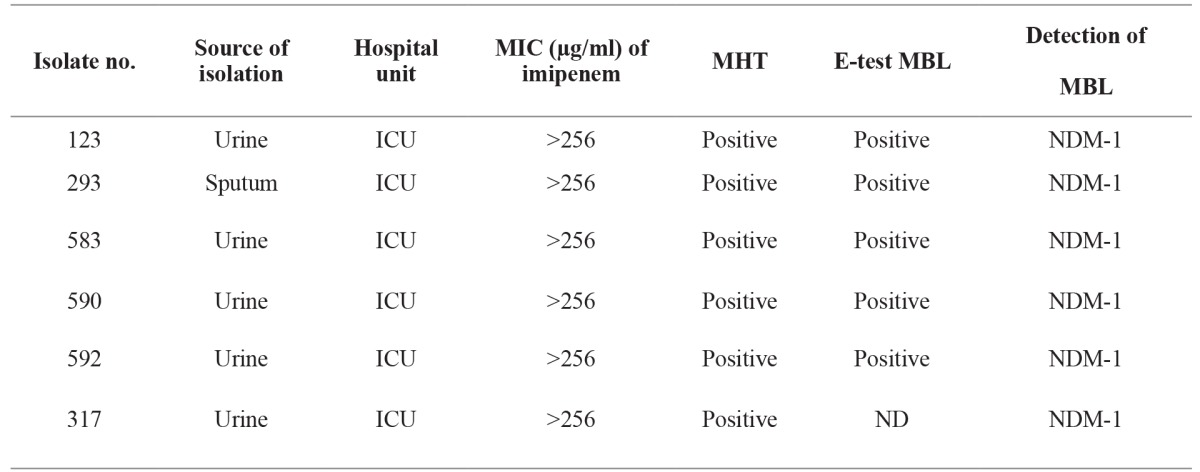
ND: non determinable, MBL: Metallo-Beta-Lactamase, MHT: modified Hodge test, E-test: Epsilometer test, MIC: minimal inhibitory concentrations; ICU, intensive care unit.
Discussion
The current emergence of carbapenemase-producing bacteria represents a major threat to the clinical application of all beta-lactam antibiotics6. The clinical significance of bacteria possessing an MBL gene is their ability to hydrolyze β-lactams.
MBL genes are also often associated with aminoglycoside resistant genes, and thus, these bacteria are often co-resistant to aminoglycosides, further compromising therapeutic regimes13,14.
In recent years, detection of MBLs and other antibiotic resistance genes among Gram-negative bacilli has been reported worldwide. The presence of MBL genes on mobile genetic elements, such as integrons and plasmids helps their widespread dissemination and is a serious concern in nosocomial infection control15,16.
Nowadays, K. pneumoniae is recognized as an important reservoir for a variety of resistance determinants including β-lactamases, such as KPC (K. pneumoniae carbapenemase) and metallo-β-lactamases VIM, IMP, and NDM17. In this study, PCR results demonstrated that 6 out of 49 (12%) carbapenem-resistant isolates expressed the New Delhi metallo-beta-lactamase, five of which were also positive by the MHT and E-test MBL strips. This is the second report on the detection of NDM-1 in Iran. It was first reported by Shahcheraghi et al in 2012 during a study on Enterobacteriaceae family isolates collected from five hospitals in Tehran. Shahcheraghi et al detected a K. pneumoniae isolate carrying blaNDM-118. The data obtained in this study indicate that the results of MBL detection using phenotypic tests and PCR correspond to the findings of other studies, such as Ikonomidis, Kassis-Chikhani, Psichogiou, Roy and Nordmann19-23. Previous studies showed that the sensitivity of MBL-producing isolates to carbapenems varied from intermediate to resistant. However, all the isolates in this study that expressed blaNDM-1 were completely resistant to imipenem and meropenem with MICs >256 for imipenem.
NDM-1 is an Ambler class B beta-lactamase that confers resistance to all β-lactams except aztreonam. In this study, isolates harboring NDM-1 were resistant to all tested antibiotics, including aztreonam. This may probably indicate the simultaneous presence of other antibiotic resistance mechanisms in these isolates. The NDM-1-encoding gene can spread from one strain of bacteria to another by horizontal gene transfer and moreover, plasmids possessing the bla NDM gene often carry other resistance genes including: ESBLs and 16SrRNA methylase genes (armA, rmtA, rmtB, rmtC, rmtD, rmtE, rmtFand npmA), conferring resistance to all β-lactams and aminoglycosides. Therefore, the early detection of NDM-1 producing bacteria causing clinical infections and/or colonization is essential to prevent their spread24-26. Some studies have suggested the use of tigecycline and colistin as the only available options for the treatment of infections caused by MBL- or KPC-producing Gram-negative bacilli. However, reports of the emergence of colistin and tigecycline-resistant isolates and also unfavorable pharmacokinetics and toxic side-effects of these antibiotics, may limit their use18. Recently, FIM-1 (Florence Imipenemase), a new type of acquired MBL was detected in a multidrug-resistant P. aeruginosa clinical isolate in Florence, Italy. This novel MBL enzyme has 40% amino acid similarity to the NDM enzyme27.
The isolation of NDM-1 expressing strains in Iran is still very rare. However, it is expected that the number of such isolations will increase in the near future. Therefore, the early detection of NDM-1 expressing bacteria using molecular methods could be a useful control strategy. Moreover, it is necessary that antibiotics should be applied appropriately to prevent the emergence and spread of MDR bacterial strains in hospitals and the community.
Conflict of interest
All authors report no conflicts of interest relevant to this article.
Acknowledgment
We would like to appreciate the Pasteur Institute of Iran for providing the standard strains.
References
- 1.Brisse S, Fevre C, Passet V, Issenhuth-Jeanjean S, Tournebize R, Diancourt L, et al. Virulent clones of Klebsiella pneumoniae: identification and evolutionary scenario based on genomic and phenotypic characterization. PLoS ONE. 2009;4:e4982. doi: 10.1371/journal.pone.0004982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Silva N, Igrejas G, Poeta P. High-throughput genomic technology in research of virulence and antimicrobial resistance in microorganisms causing nosocomial infections. JIOMICS. 2014;4:44–56. [Google Scholar]
- 3.Davies J, Davies D. Origins and Evolution of Antibiotic Resistance. Microbiol Mol Biol Rev. 2010;74:417–433. doi: 10.1128/MMBR.00016-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zagorianou A, Sianou E, Iosifidis E, Dimou V, Protonotariou E, Miyakis S, et al. Microbiological and molecular characteristics of carbapenemase-producing Klebsiella pneumoniae endemic in a tertiary Greek hospital during 2004-2010. Euro Surveill. 2012;17:pii=20088. [PubMed] [Google Scholar]
- 5.Enwuru NV, Enwuru CA, Ogbonnia SO, Adepoju-Bello AA. Metallo-β-Lactamase Production by Escherichia Coli and Klebsiella Species Isolated from Hospital and Community Subjects in Lagos, Nigeria. Nat Sci. 2011;9:1–5. [Google Scholar]
- 6.Cornaglia G, Akova M, Amicosante G, Cantón R, Cauda R, Docquier JD, et al. Metallo-beta-lactamases as emerging resistance determinants in Gram-negative pathogens: open issues. Int J Antimicrob Agents. 2007;29:380–388. doi: 10.1016/j.ijantimicag.2006.10.008. [DOI] [PubMed] [Google Scholar]
- 7.Poirel L, Revathi G, Bernabeu S, Nordmann P. Detection of NDM-1-Producing Klebsiella pneumoniae in Kenya. Antimicrob Agents Chemother. 2011;55:934–936. doi: 10.1128/AAC.01247-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Queenan AM, Bush K. Carbapenemases: the versatile beta-Lactamases. Clin Microbiol Rev. 2007;20:440–458. doi: 10.1128/CMR.00001-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.CLSI Performance Standards for Antimicrobial Susceptibility Testing; Twenty-Second Informational Supplement. CLSI document M100-S22. Wayne, PA: Clinical and Laboratory Standards Institute. 2012 [Google Scholar]
- 10.Anderson KF, Lonsway DR, Rasheed JK, Biddle J, Jensen B, McDougal LK, et al. Evaluation of methods to identify the Klebsiella pneumoniae carbapenemase in Enterobacteriaceae. J Clin Microbiol. 2007;45:2723–2725. doi: 10.1128/JCM.00015-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walsh TR, Bolmstrom A, Qwarnstrom A, Gales A. Evaluation of a new Etest for detecting metallo-beta-lactamases in routine clinical testing. J Clin Microbiol. 2002;40:2755–2759. doi: 10.1128/JCM.40.8.2755-2759.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Teo J, Ngan G, Balm M, Jureen R, Krishnan P, Lin R. Molecular characterization of NDM-1 producing Enterobacteriaceae isolates in Singapore hospitals. Western Pac Surveill Response J. 2012;3:19–24. doi: 10.5365/WPSAR.2011.2.4.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Walsh TR, Toleman MA, Poirel L, Nordmann P. Metallo-beta-lactamases: the quiet before the storm? Clin Microbiol Rev. 2005;18:306–325. doi: 10.1128/CMR.18.2.306-325.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walsh TR. The emergence and implications of metallo-beta-lactamases in Gram-negative bacteria. Clin Microbiol Infect. 2005;11:2–9. doi: 10.1111/j.1469-0691.2005.01264.x. [DOI] [PubMed] [Google Scholar]
- 15.Palzkill T. Metallo-beta-lactamase structure and function. Ann N Y Acad Sci. 2013;1277:91–104. doi: 10.1111/j.1749-6632.2012.06796.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mohamed NM, Raafat D. Phenotypic and Genotypic Detection of Metallo-beta-lactamases in Imipenem-resistant Acinetobacter baumannii Isolated from a Tertiary Hospital in Alexandria, Egypt. Res J Microbiol. 2011;6:750–760. [Google Scholar]
- 17.Meletis G, Tzampaz E, Protonotariou E, Sofianou D. Emergence of Klebsiella pneumoniae carrying bla(VIM) and bla(KPC) genes. Hippokratia. 2010;14:139–140. [PMC free article] [PubMed] [Google Scholar]
- 18.Shahcheraghi F, Nobari S, Rahmati Ghezelgeh F, Nasiri S, Owlia P, Nikbin VS, et al. First report of New Delhi metallo-beta-lactamase-1-producing Klebsiella pneumoniae in Iran. Microb Drug Resist. 2013;19:30–36. doi: 10.1089/mdr.2012.0078. [DOI] [PubMed] [Google Scholar]
- 19.Ikonomidis A, Tokatlidou D, Kristo I, Sofianou D, Tsakris A, Mantzana P, et al. Outbreaks in distinct regions due to a single Klebsiella pneumoniae clone carrying a bla VIM-1 metallo-{beta}-lactamase gene. J Clin Microbiol. 2005;43:5344–5347. doi: 10.1128/JCM.43.10.5344-5347.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kassis-Chikhani N, Decre D, Gautier V, Burghoffer B, Saliba F, Mathieu D, et al. First outbreak of multidrug-resistant Klebsiella pneumoniae carrying blaVIM-1 and blaSHV-5 in a French university hospital. J Antimicrob Chemother. 2006;57:142–145. doi: 10.1093/jac/dki389. [DOI] [PubMed] [Google Scholar]
- 21.Psichogiou M, Tassios PT, Avlamis A, Stefanou I, Kosmidis C, Platsouka E, et al. Ongoing epidemic of blaVIM-1-positive Klebsiella pneumoniae in Athens, Greece: a prospective survey. J Antimicrob Chemother. 2008;61:59–63. doi: 10.1093/jac/dkm443. [DOI] [PubMed] [Google Scholar]
- 22.Roy S, Viswanathan R, Singh AK, Das P, Basu S. Sepsis in neonates due to imipenem-resistant Klebsiella pneumoniae producing NDM-1 in India. J Antimicrob Chemother. 2011;66:1411–1413. doi: 10.1093/jac/dkr068. [DOI] [PubMed] [Google Scholar]
- 23.Nordmann P, Poirel L, Carrer A, Toleman MA, Walsh TR. How to detect NDM-1 producers. J Clin Microbiol. 2011;49:718–721. doi: 10.1128/JCM.01773-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rasheed JK, Kitchel B, Zhu W, Anderson KF, Clark NC, Ferraro MJ, et al. New Delhi metallo-beta-lactamase-producing Enterobacteriaceae, United States. Emerg Infect Dis. 2013;19:870–878. doi: 10.3201/eid1906.121515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee CS, Vasoo S, Hu F, Patel R, Doi Y. Klebsiella pneumoniae ST147 coproducing NDM-7 carbapenemase and RmtF 16S rRNA methyltransferase in Minnesota. J Clin Microbiol. 2014;52:4109–4110. doi: 10.1128/JCM.01404-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kumarasamy KK, Toleman MA, Walsh TR, Bagaria J, Butt F, Balakrishnan R, et al. Emergence of a new antibiotic resistance mechanism in India, Pakistan, and the UK: a molecular, biological, and epidemiological study. Lancet Infect Dis. 2010;10:597–602. doi: 10.1016/S1473-3099(10)70143-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pollini S, Maradei S, Pecile P, Olivo G, Luzzaro F, Docquier JD, et al. FIM-1, a new acquired metallo-β-Lactamase from a Pseudomonas aeruginosa clinical isolate from Italy. Antimicrob Agents Chemother. 2013;57:410–416. doi: 10.1128/AAC.01953-12. [DOI] [PMC free article] [PubMed] [Google Scholar]


