Abstract
Although care coordination is a popular intervention, there is no standard method of delivery. Also little is known about who most benefits or characteristics that predict the amount of care coordination needed, especially with chronically ill older adults. The purpose of this study was to identify types and amount of nurse care coordination interventions provided to 231 chronically ill older adults who participated in a 12-month home care medication management program in the Midwestern. For each participant, the nurse care coordinator spent an average of 134 minutes/month providing in-person home care, 48 minutes/month of travel, and 18 minutes/month of indirect care occurring outside the home visit. This accounted for 67.2%, 23.8%, and 9.0% of nursing time respectively for home visits, travel, and indirect care. Four of 11 nursing interventions focused on medication management were provided to all participants. Seven of the 11 main interventions were individualized according to each person’s special needs. Wide variations were observed in time provided with in-person home care and communications with multiple stakeholders. Study findings indicate the importance of individualizing interventions and the variability in the amount of nursing time needed to provide care coordination to chronically ill older adults.
Keywords: elderly, care coordination, electronic health records, standardized nursing terminology
Given that chronically ill older adults are the major consumers of health care dollars, development of systems that provide support in the management of the complex health care needs is critical.1 The current health care system, however, fails to meet the needs of most chronically ill older adults. Care is often provided in a confusing and complicated maze that provides minimal support and multiple barriers to the persons most vulnerable to expensive preventable health events.2 The inefficiencies of the United States health care system are not only costly, but can lead to poor quality care,3,4 demanding new models of care in the current era of healthcare reform.
Major areas of inefficiencies are fragmentation of care, incomplete follow up, duplication of diagnostic testing, dangerous polypharmacy, and conflicting plans of care. Care coordination was identified by the Institute of Medicine5 as one of eight national priority areas for health care quality improvement and disparities elimination. In a paper commissioned by the Agency for Healthcare Research and Quality, care coordination was defined as “the deliberate organization of patient care activities between two or more participants (including the patient) involved in a patient’s care to facilitate the appropriate delivery of health care services. Organizing care involves marshaling of personnel and other resources needed to carry out all required patient care activities, and is often managed by the exchange of information among participants responsible (page v)”.6
While care coordination is a popular intervention, especially for older adults with multiple chronic conditions to ensure the quality of care across the care continuum, limited evidence is available as to what constitutes care coordination of chronically ill community-dwelling older adults and what factors influence the dose of care coordination needed for the intervention to be effective. As health information technology (HIT) advances, it becomes possible to enhance our understanding of care coordination activities using data generated from electronic health records (EHRs).7 Accordingly, this study was designed to examine nurse care coordination interventions delivered to chronically ill older adults in their home and the time allocated for care coordination interventions.
Literature Review
While there is growing evidence of the effectiveness of care coordination programs in improving patient outcomes and reducing costs,8–11 care coordination and case management are often used interchangeably in the literature. Further, care coordination is delivered in a wide variety of approaches in different settings, with different providers, and with different clinical populations.12 These variations make it difficult to understand what components of care coordination are essential to ensure the success of the program. Three basic configurations of care coordination programs include: (a) transitional care, patients are first engaged in the hospital and followed for 4–12 weeks post hospitalization, usually by advance practice nurses (APNs)10, 13,14 or Registered Nurses (RNs) directed by APNs,9 (b) self-management education via the Chronic Care Model,15,16 and (c) coordinated care interventions provided by nurses (mostly via telephone) who monitor patients with chronic conditions at high risk for hospitalization and facilitate communication among the primary care provider, family, and patient.8,17–19
Common elements of care coordination interventions include initial comprehensive assessment, development of a plan of care, monitoring, and revising the plan as required.20,21 In addition, other areas identified as common targets of intervention are medication adherence and facilitating support services.22 Disease management programs usually have a care coordination component with specific protocols related to the disease focus. Although previous research supported that the majority of the care coordination interventions occur in person-to-person encounters with the patient, a factor found to be more effective with complex patients,23 the amount and type of interventions provided with care coordination are yet to be examined.
Home Care Medication Management Program (HCMM)
The parent study for this analysis was a randomized controlled trial that tested the use of nurse care coordination and technology in participants discharged from home health care with problems in medication management.8 Medicare patients were eligible to participate if they were age 60 or older and not terminally ill at the time of enrollment.11 Care coordination was delivered by a study team directed by an APN with RN nurse care coordinators, using study protocol related to medication management and care plans based on each participant’s care needs. Participants were visited at least every two weeks over the study period to fill their pill organizer or medication dispensing machine, and assess their health care needs and self-management abilities. Based on this assessment, the care coordinators further provided nursing interventions, including ongoing assessments, care plans and evaluation, and communications with various stakeholders involved in patient care.
The program functioned independently from the local home health agencies in an urban area of a large Midwestern city.8 All interventions provided by the nurse care coordinators were documented using a structured visit note and unstructured (narrative) communication logs via an EHR system (CareFacts® Version 2)24 used by only the nurses in the HCMM study. In addition, nurses recorded time spent in home visits and indirect care activities (e.g., communication) using a paper-based activity log that was entered manually into a Microsoft Access database by study personnel. All the EHR data and activity logs were the data source for this secondary study.
Specific Aim
In this secondary analysis, we aimed to answer the following questions:
What specific nursing interventions were provided by the nurse care coordinator over 12 months of care coordination services?
How much nursing time was required for nursing care coordination of community-dwelling older adults?
Was there an association between time spent for in-person home visits and the amount of indirect nursing care occurring outside the home visit?
Methods
Participants
This study used secondary data collected regarding nurse care coordinator activity in the EHR from the parent study.8 To achieve the purpose of this study, only study participants who received care coordination interventions for at least one quarter (3 months) were included in this secondary analysis, yielding a total of 231 chronically ill older adults.
Measures
Participant characteristics
Four demographic factors were included in this study; age (years), sex (male/female), race (black/white), and living arrangement (living alone/living with someone). Also included were factors related to the participants’ health such as comorbidities, medication regimen complexity, and the baseline health status measures of depression, cognition, functional status, and quality of life. Comorbidities included the presence/absence of the ten most frequently occurring Centers for Medicare and Medicaid Servcies (CMS) chronic conditions – atrial fibrillation, chronic kidney disease (CKD), chronic obstructive pulmonary disease (COPD), dementia, depression, diabetes, heart failure (HF), ischemic heart disease, osteoporosis, and stroke.25
The complexity of medication regimen was assessed using the Medication Complex Index (MCI) measuring the number of medications, number of doses/day, directions required, and mechanical actions required for administration.26,27 Although there is no upper limit, Maddigan et al.27 reported a range of an MCI score from 1 to 103. A higher MCI score indicates a more complex medication regimen. It is noted that the study participants used either a home medication dispensing system (or MD.2) or a simple pillbox (or Mediplanner) for medication management, which was randomly allocated as part of the HCMM study protocol.
The severity of depression was measured using the Geriatric Depression Scale (GDS) whose total score ranges from 0 to 15.28 A GDS score of 5 or greater indicates mild (5–8), moderate (9–11) or severe (12–15) depression, meaning lower GDS scores present less depressed mood. The Mini-Mental State Examination (MMSE) was the instrument used to assess level of cognitive impairment (range: 0~30).29,30 The Physical Performance Test (PPT) involving 7 specific tasks was used to examine each subject’s functional status (range: 0~28).31 Quality of life was assessed using the SF-36 Physical Component Scale (PCS) and Mental Component Scale (MCS) whose score ranges from 0 to 100.32 The higher the score of MMSE, PPT, and SF-36, the better the health status of individuals. Lastly, the occurrence of hospitalization over the one-year study period was coded as a simple yes/no, rather than frequency.
Nurse care coordination interventions
Nursing care provided during the home visit was documented using the EHR system (CareFacts® Version 5).24 Nurse care coordinators usually documented care delivered in the home visit during the home visit. The software employed a standard structure for Visit Notes where the nurses recorded patient problems, nursing interventions, and visit time (minutes). Visit Notes were coded using the Omaha System organized in a simple hierarchical structure with 42 client problems and 76 interventions.33 The Omaha System is recognized as an interface nursing terminology for clinical use by the American Nurses Association34 and has been utilized in documentation of care – nursing assessment, intervention, and outcome evaluation – in electronic records.35,36
There were also a small portion of short free-text notes attached to the visit note. A total of 645 narrative notes were manually reviewed by the authors and assigned a corresponding Omaha System nursing intervention code if a semantic match existed. Two authors independently coded the nurses’ free-text data using the Omaha System. The level of agreement between the two investigators was computed using Cohen’s Kappa37 (κ = .269, p < .001). Any disagreement among the authors was discussed until 100% agreement was achieved. This final agreement served as for the basis of developing machine-aided coding rules applied to Communication Logs below.
Communication logs embedded in the EHR were used to record nurses’ communication and documentation activities (or indirect care) that were provided to coordinate health care of the older adults outside the home visit. Each communication log consisted of a subject, short text notes, contact person(s), and the means of a communication (e.g., phone, e-mail) used by the care coordinator. It is noted that the nurse care coordinators recorded their time spent in indirect care separate from the visit notes using a paper-based activity log.
Due to the nature of unstructured free-text data hindering the quantification of nursing activities in the communication logs, rules were developed to classify and code nursing activities using the Omaha System interventions. Two authors selected 550 free-text indirect care log entries and mapped each to an Omaha System intervention code based on keywords identified in each communication log. For example, a communication log included a statement such as “INR [international normalized ratio] was 1.6, adjust coumadin to 4 mg on Monday and Thursday, 2mg the other days.” Or “Call to [physician’s name] office that INR 4.8, hold warfarin today and they will call later with further instructions.” The authors coded these statements with the Omaha System “case management of laboratory findings” and “case management of medication coordination.”
In order to extract keywords from the Communication Logs, we applied a range of techniques to transform unstructured narrative text data into a useful format for analyses. MetaMap, which is a natural language processing tool developed by the National Library of Medicine (NLM), was used to process and map the text data to standardized concepts available in the NLM Unified Medial Language System (UMLS) methathesaurus.38 The UMLS methathesaurus encompasses more than nine million distinct concept names provided by more than 150 health and nursing terminologies or classification systems.39 We then developed procedural rules for machine-aided classification of concepts or text in the communication logs. Using the procedural rules developed through our coding activities, we further mapped these coded communication logs to the Omaha System nursing intervention codes. When comparing coding results, overall the level of agreement between the Omaha System coding performed by the authors and coding performed by machine was a recall of 0.94, a precision of 0.95, an accuracy of 0.83, and an F-measure of 0.94, indicating good performance of the machine classification.40
Average nurse time
Direct time was measured by summing nurses’ time spent for in-person home visits per participant, excluding travel time. Indirect time was computed by summing nurses’ time spent for communications and documentation per participant, which was separated from nurses’ time required for study coordination. Due to the variation in the length of study participation, the average nursing time required for each individual per month was then calculated by dividing the sum of direct and indirect nursing time by the length (months) of stay in the original study.
Data analysis
All the study variables were summarized using descriptive statistics. The association between direct and indirect care time was examined using regression analysis while controlling for participant characteristics including age, race, living arrangement, medication regimen complexity, comorbidities, baseline health status, and occurrence of hospital admission. All analyses were conducted using the IBM SPSS statistical package (version 22). Approval for this study was obtained from the Institutional Review Boards of Arizona State University, University of California Davis, and University of Wisconsin-Milwaukee.
Results
Participants’ characteristics
Nurse care coordination interventions delivered to a total of 231 older adults was examined in this secondary analysis. As shown in Table 1, the majority of the study participants were female (69.3%) and white (81.4%) with a mean age of 79.5 years (range: 60–98). Approximately 50% lived alone with the most prevalent chronic condition of diabetes (40.3%) followed by depression (25.1%). Almost half of the participants (47%; n=109) presented more than one CMS chronic condition. A wide variation in the complexity of medication regimen was observed according to MCI scores ranging from 7 to 141 (median: 34).
Table 1.
Characteristics of the Study Participants (n=231)
| Characteristics: Categorical Variables | n | % | |
|---|---|---|---|
| Sex | Female | 160 | 69.3 |
| Race/Ethnicity | White | 188 | 81.4 |
| Black | 43 | 18.6 | |
| Living Status | Living alone | 111 | 48.1 |
| Comorbidities: CMS Chronic conditions | Diabetes | 93 | 40.3 |
| Depression | 58 | 25.1 | |
| Chronic obstructive pulmonary disease (COPD) | 35 | 15.2 | |
| Dementia | 35 | 15.2 | |
| Ischemic heart disease | 30 | 13.0 | |
| Atrial fibrillation | 29 | 12.6 | |
| Chronic kidney disease (CKD) | 26 | 11.3 | |
| Stroke | 18 | 7.8 | |
| Heart Failure (HF) | 14 | 6.1 | |
| Osteoporosis | 13 | 5.6 | |
| Length of stay in the care coordination program | 1 quarter | 14 | 6.1 |
| 2 quarters | 13 | 5.6 | |
| 3 quarters | 8 | 3.5 | |
| 4 quarters | 196 | 84.8 | |
| Characteristics: Continuous Variables | Mean | SD | |
| Age | Years | 79.5 | 7.7 |
| MCI | Medication complexity index (MCI) score | 40.2 | 23.2 |
| Baseline health status | Geriatric depression scale (GDS) score | 4.3 | 3.3 |
| Mini-mental state exam (MMSE) score | 25.3 | 3.5 | |
| Physical performance test (PPT) score | 14.6 | 5.0 | |
| SF-36 physical component scale (PCS) score | 34.1 | 9.5 | |
| SF-36 mental component scale (MCS) score | 49.1 | 12.3 | |
SD = standard deviation
When examining the baseline health status measurements, a cut-off point of GDS score28 of 5 identified 41.1% (n=95) of the study participants with mild to severe depression (mean GDS score: 4.3 ± 3.3, range: 0–15). Forty-two percent (n=98) of the study participants showed either mild or moderate cognitive impairment according to the cut-off point of MMSE score30 of below 26. With regard to functional status, half (n=116) of the study participants presented less than 16 points of PPT score (range: 1–23), indicating they were most likely dependent and homebound at baseline. The mean score of the SF-36 PCS was 34.1 ± 9.5 (range: 9.4–60.7) while the mean score of SF-36 MCS was 49.1 ± 12.3 (range: 11.9–74.6). Approximately half of the participants (45%; n=104) were hospitalized at least one time after the enrollment in the original study.
Types of nursing care
A total of 7,628 home visit records and 10,916 communication logs were created using the EHR system over the one year study period for the 231 program participants. The mean number of home visits was 33.0 ± 9.9, ranging from 11 to 68. The mean number of communications (indirect care) was 47.3 ± 48.6, ranging from 0 to 253. These wide variations in home visits and communication occurrence were observed due, in part, to variations in length of stay in care coordination services.
Nurse care coordination interventions
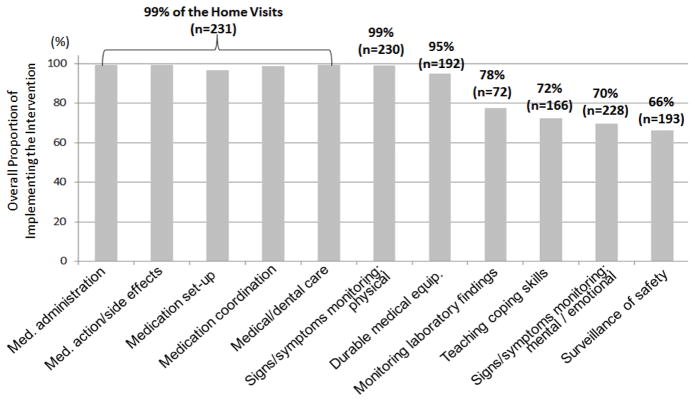
Over the one year study period, 11 nursing interventions were most frequently implemented. Of those, four nursing interventions (based on the Omaha System intervention classification) were performed at every visit for all the study participants, including (a) medication set-up, (b) medication administration, (c) medication action/side effects monitoring, and (d) coordination of medications as these interventions were part of the original study protocol (Figure 1). In addition to the study protocol interventions, coordination of medical/dental care (i.e., coordination of patient assessment and treatment provided by physicians, dentists, and their staff.) and physical signs/symptoms monitoring occurred in every visit for all the participants. These two interventions were individualized to the older adult and associated with physical problems in circulation (86.1%; n=199), pain (55.4%; n=128), respiration (43.7%; n=101), urinary function (32.0%; n=74), digestion and hydration (27.7%; n=64), bowel function (25.5%; n=59), and neuro-musculo-skeletal function (21.6%; n=50) in the nurses’ documentation.
Figure 1.
Overall Proportion of Implementing Direct Care Interventions in the Home Visits
(Note: Each intervention was documented using the Omaha System in the EHR.)
Although additional non-study protocol interventions were implemented frequently, the number of study participants who required these interventions varied according to individual needs. While the interventions of case management for the use of durable medical equipment occurred in the majority of participants (83.1%; n=192), this intervention was most often delivered to the participants who used a home medication dispensing system (97% of the home visits in 115 participants). Likewise case management for laboratory findings was an intervention provided to individuals with diabetes and individuals receiving anticoagulation therapy. In addition, the majority of participants required interventions of psychological signs and symptoms monitoring (98.7%; n=228), prevention of injury (83.5%; n=193), and teaching/counseling about self-management of chronic illness (i.e., coping skills) (71.9%; n=166). These interventions were implemented more than two third of the home visits (Figure 1).
Indirect care interventions
The patterns of indirect care were examined using nurses’ documentation in communication logs. Of 10,916 indirect care communications (involving a total of 47,147 minutes spent by the nurse care coordinator), 43.2 percent of communications occurred on the same date as a home visit (2,845 visits or 37.3% of the visits) while 56.8 percent of communications occurred separately from a visit day.
The majority of communications (94.0%) were performed via phone (including case conference and voice mail) while the rest of communications were done using other mediums such as fax, e-mail/mail, and in-person meetings with other providers outside the home visit. The recipients of nurse care coordinators’ communications included primary care physicians (21.6%), pharmacists (20.5%), patients (20.1%), caregivers (8.3%), community agencies (5.7%) and others (16.9%), such as durable medical equipment suppliers, laboratory facilities, and hospitals.
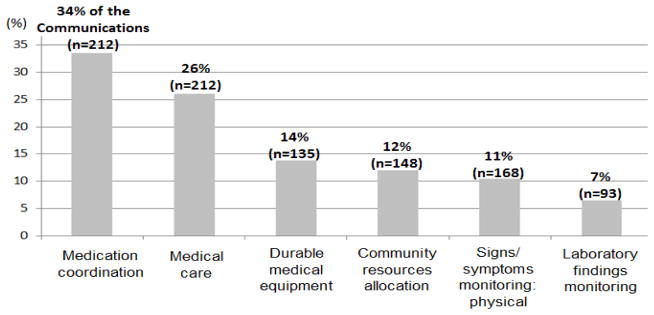
The most frequently occurring communications were associated with six nursing interventions (Figure 2), which encompassed 85% of all indirect care communications. Those interventions were (a) medication coordination/ordering (34%) including refills and new medication screening using the First DataBank® drug database and Beers criteria,41 (b) medical care scheduling and hospital coordination (26%), (c) monitoring of the medical durable equipment such as the home medication dispensing device (14%), (d) community resources allocation (such as obtaining homecare and meals-on-wheels services) (12%), (e) monitoring of physical signs and symptoms (11%), and (f) monitoring of laboratory results (7%). In fact, all these activities were interrelated and often sequentially occurred over a few days. For example, when the nurse care coordinator detected abnormal laboratory findings (e.g., international normalized ratio or INR value), s/he contacted the primary care physician to discuss dose change in the medication (e.g., coumadin), obtained a new prescription of the medication, and contacted and/or visited the participant regarding the new dose of the medication.
Figure 2.
Overall Proportion of Implementing Indirect Care Interventions
(Note: Each intervention was recoded using the Omaha System by applying machine-aided procedural rules against Communication Logs.)
Amount of nursing care
On average, 47.0 ± 9.1 minutes were spent for direct care in addition to 16.6 ± 5.5 travel time (minutes) per visit. The monthly mean number of visits per participant was 2.8 ± 0.8 (range: 1.2–5.7), resulting in the monthly mean direct care (or home visit) time of 134.3 ± 46.4 minutes (range: 51.6–314.9) and the monthly mean traveling time of 47.7 ± 22.2 minutes (range: 10.2–157.1). In addition, the monthly mean number of communications by the nurse care coordinator was 4.2 ± 4.2 per participant (rang: 0–20.0), which yielded a mean indirect time of 18.0 ± 17.8 minutes/month per participant (range: 0–133.1). In sum, the nurse care coordinator allocated 67.2%, 23.8%, and 9.0% of their time for home visits, travel and indirect care respectively by month.
Association between the amount of direct and indirect care time
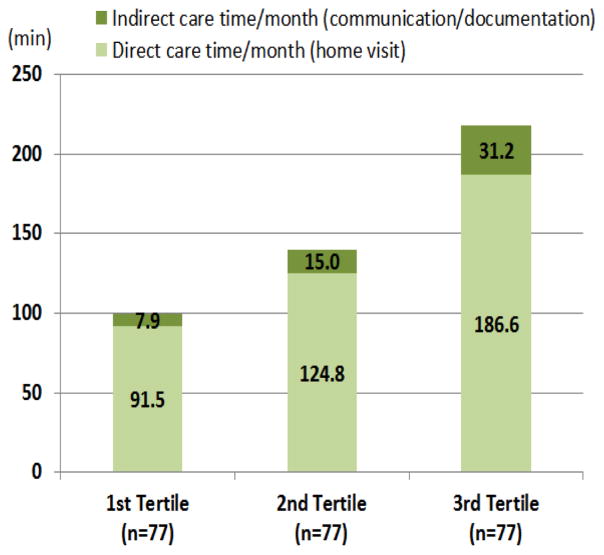
When controlling participant characteristics (age, race, living arrangement, medication regimen complexity, comorbidities, baseline health status, and occurrence of hospital admission), regression analysis presented a significant relationship between direct and indirect care time (p < .001). This means when participants required more home visits, they also needed more indirect care outside the home visits. Clearly, when the participants were evenly divided into three parts according to an ordered distribution of the total care time (i.e., the sum of direct and indirect care time), one third of the study participants who were included in the third group (n=77) required the most nurse time on average (Figure 3). Both direct and indirect time (3.6 hours/month) spent for the third group was two times higher as compared to the nurse time spent for the first group (1.7 hours/month).
Figure 3.
A summary of the Nurse Time Spent for Care Coordination by Group
(Note: Each tertile contains one third of the study participants divided evenly according to an ordered distribution of the nurse time.)
Discussion
Nurse care coordination interventions delivered to community-dwelling older adults with chronic conditions were examined in this study. As a follow-up to a larger study, this secondary data analysis focused on identifying types and amount of direct and indirect nursing interventions provided by nurse care coordinators. Overall the participants were visited three times per month by the nurse care coordinator, resulting in more than three hours of home visits (direct care), travel, and communications (indirect care outside the home visit) per person. As the target of the original study was care coordination and home medication management, the nurse care coordinator focused on medication set-up, administration, and coordination in addition to monitoring side-effects of medications administered in every visit. Frequent nursing interventions included medical/dental care coordination and physical signs/symptoms monitoring as the nurse care coordinator completed comprehensive assessment with every home visit.
However, a wide variation in the types and amount of direct and indirect care was identified in this study. This resulted from person-centered care since each individual had different needs in relation to their chronic illness and suboptimal physical/mental functioning. As presented in the baseline health measures, more than 40% of the participants were living alone, cognitively impaired, depressed, and/or had physical limitations, which in part, contributed to their inability to independently manage medications at home. Accordingly, nurses provided additional interventions, such as case management for the use of durable medical equipment, monitoring of laboratory results, teaching/counseling about self-management of chronic conditions, and monitoring of emotional/psychological symptoms. This finding suggests that individuals with complex healthcare needs benefit most from nurse care coordinators who provide individualized, patient-centered care, which is consistent with a recent qualitative study presenting collective experience of 11 community-based nurse care coordinators across the country.42
The Affordable Care and Health Information Technology for Economic and Clinical Health (HITECH) Acts include the provision of patient-centered care, a critical component within Health Care Homes.43 In this context, our finding illuminates that patient-centered care coordination is not limited to in-person encounters. In other words, this study identified that individualized care was needed not only during the home visit but also outside the home visit as the chronically ill older adults unexpectedly experienced short supply of prescribed medications, new or worsening signs/symptoms, adverse effects of medications, functional decline, hospital admissions, medical equipment dysfunction, and/or abnormal changes in laboratory values. Accordingly, the nurse care coordinators contacted various stakeholders to coordinate medication ordering/refills, medical care including office visit scheduling and hospital admission/discharge, as well as community services (e.g., homecare, meals-on-wheels services). All these indirect nursing interventions often involved not only physicians and pharmacists but also patients and care givers as they were the primary actors in self-management of chronic conditions. Further, a set of nursing activities occurred together to complete care coordination over a few days suggests a need for clustering serial nursing activities to enhance our understanding of the care coordination interventions. Overall these findings underscore the complex and dynamic processes of self-management of chronic illness conceptualized in the Individual and Family Self-management Theory.44 In fact, beyond the HCMM program, similar circumstances could happen in the community, demanding additional care managers’ time during homecare episodes.
Understanding the importance of both direct and indirect care conducted by professional nurses in care coordination is necessary for planning and budgeting such services. When examining the proportion of total care time per month, 88% and 12% of nurses’ time were allocated for direct and indirect care respectively. It is not surprising that individuals who needed more home visits also demanded more indirect care outside the home visit considering the complex healthcare needs of the chronically ill older adults. When total care time (i.e., sum of direct and indirect care time) was divided into three groups (Figure 3), direct and indirect care time spent in the highest tertile was two times greater than nursing time spent in the lowest tertile, indicating further investigation is needed to identify what caused this large variation. While it is difficult to estimate the appropriate amount of indirect time in care coordination due to limited evidence in the literature, a local workflow analysis of care coordination in Australia illustrates that indirect care time (allocated for administration, consultation, planning, service development, etc.) accounts for substantial amount of care coordinators’ time in the community.45
It is well known that administrative or billing data sets are limited to describing the number and costs of a home visit provided. The richness of nursing documentation collected through the HCMM study provided a means for disentangling the types and amount of nurse care coordination interventions, as these specific activities were often obscure and underreported in the literature. Moreover, coordinating medications and medical care, as well as other community resources are difficult to capture in intensity measures, as these types of indirect care are conducted outside the actual home visit. The standardized nursing terminology adopted in this study (i.e., Omaha System) was conducive in quantifying patterns of nursing interventions provided over the one year of care coordination services as demonstrated in previous studies.46–49
The nurse care coordination interventions examined in this study were provided to older adults who were discharged from home care as no longer eligible for the current Medicare Home Health program. Although it was not possible to compute how much time was required for each nursing intervention, it is apparent that the nurse care coordinator is the one professional who provided interventions across health care and social service delivery settings and providers (i.e., physician, pharmacist, social worker). More importantly, results of the primary study demonstrated that the nurse care coordinator played a significant role in improving patient outcomes (including improved cognition, physical function, and quality of life, as well as reduced depression),8 and reducing monthly costs to the Medicare program.11 This cost effective results indicate that the size of a nurse care coordinator’s caseload based on the complexity of the older adult should be considered if care coordination is to be successful. It is noted that because this was a research study, the nurse’s time in documentation for reimbursement was not included, as would be the case for nurses who provided Medicare Home Health (e.g., documentation of CMS Outcome and Assessment Information Set (OASIS) and Medicare Form 485, Home Health Certification and Plan of Care). Data collected for research evaluation was gathered by research staff and not by the nurses who provided the nurse care coordination.
Our analysis has limitations in that the study dataset was constructed based on EHR data of both structured and unstructured free text data. The study findings resulted from clinicians’ documentation that may not capture all activities and nursing time spent during and outside the home visit. Along with the lack of control of the quality and accuracy of EHR documentation, automated coding of text data with the Omaha System could potentially create systematic bias in computing indirect care components. Though the authors made every effort to overcome these limitations inherent in using EHR data through human validation, the interpretation of these findings requires caution. Understanding that care coordination was associated with a wide variation of interventions and total nursing time, however, suggests further research about how individualized care was associated with the amount of nurse time, who the best candidates for nursing care coordination might be, and how to both standardize and tailor nursing care coordination interventions to achieve best outcomes with limited resources in communities.
Conclusion
To our knowledge, there was little research explaining what specific nursing interventions constitute nurse care coordination provided to chronically ill community-dwelling older adults. We focused on older adults post home health care who were identified as having problems in medication management, a pervasive problem in chronically ill older adults. Patterns of implemented nursing interventions were detected with a wide variation in the types and amount of interventions, indicating there might be subgroups of patients requiring different intensity of nursing care. The number of communications involving various stakeholders also demonstrated the complexity of care coordination needs of older adults, especially in coordination of medications, medical care and community resources. While further research is warranted, our analysis reaffirms that there is a need for individualizing nurse care coordination for chronically ill older adults across the care continuum.
Acknowledgments
This work was supported by the National Institute of Nursing Research, National Institutes of Health (Grant 1R03NR012802 – TK, KM & AC; 5R01NR008911 – KM).
References
- 1.Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. 2002 Nov 11;162(20):2269–2276. doi: 10.1001/archinte.162.20.2269. [DOI] [PubMed] [Google Scholar]
- 2.Bodenheimer T. Coordinating care--a perilous journey through the health care system. N Engl J Med. 2008 Mar 6;358(10):1064–1071. doi: 10.1056/NEJMhpr0706165. [DOI] [PubMed] [Google Scholar]
- 3.Schoen C, Osborn R, How SK, Doty MM, Peugh J. In chronic condition: experiences of patients with complex health care needs, in eight countries, 2008. Health Aff (Millwood) 2009 Jan-Feb;28(1):w1–16. doi: 10.1377/hlthaff.28.1.w1. [DOI] [PubMed] [Google Scholar]
- 4.Schoen C, Osborn R, Squires D, Doty M, Pierson R, Applebaum S. New 2011 survey of patients with complex care needs in eleven countries finds that care is often poorly coordinated. Health Aff (Millwood) 2011 Dec;30(12):2437–2448. doi: 10.1377/hlthaff.2011.0923. [DOI] [PubMed] [Google Scholar]
- 5.Institute of Medicine. Future Directions for the National Healthcare Quality and Disparities Reports. Washington, DC: National Academy Press; 2010. [PubMed] [Google Scholar]
- 6.McDonald KM, Sundaram V, Bravata D, Lewis R, Lin N, Kraft S, McKinnon M, Paguntalan H, Owens DK. Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies Technical Review 9. Vol. 7. Rockville, MD: Agency for Healthcare Research and Quality; 2007. Care Coordination. [PubMed] [Google Scholar]
- 7.Bauer AM, Thielke SM, Katon W, Unutzer J, Arean P. Aligning health information technologies with effective service delivery models to improve chronic disease care. Prev Med. 2014 Sep;66:167–172. doi: 10.1016/j.ypmed.2014.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marek KD, Stetzer F, Ryan PA, et al. Nurse care coordination and technology effects on health status of frail older adults via enhanced self-management of medication: randomized clinical trial to test efficacy. Nurs Res. 2013 Jul-Aug;62(4):269–278. doi: 10.1097/NNR.0b013e318298aa55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006 Sep 25;166(17):1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 10.Baldwin KM, Black D, Hammond S. Developing a rural transitional care community case management program using clinical nurse specialists. Clin Nurse Spec. 2014 May-Jun;28(3):147–155. doi: 10.1097/NUR.0000000000000044. [DOI] [PubMed] [Google Scholar]
- 11.Marek KD, Stetzer F, Adams SJ, Bub LD, Schlidt A, Colorafi KJ. Cost analysis of a home-based nurse care coordination program. J Am Geriatr Soc. 2014 Dec;62(12):2369–2376. doi: 10.1111/jgs.13162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lamb G. Care Coordination: The Game Changer – How Nursing Is Revolutionizing Quality Care. Silver Spring, MD: American Nurses Association; 2014. [Google Scholar]
- 13.Englander H, Michaels L, Chan B, Kansagara D. The care transitions innovation (C-TraIn) for socioeconomically disadvantaged adults: results of a cluster randomized controlled trial. J Gen Intern Med. 2014 Nov;29(11):1460–1467. doi: 10.1007/s11606-014-2903-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Naylor MD, Brooten DA, Campbell RL, Maislin G, McCauley KM, Schwartz JS. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J Am Geriatr Soc. 2004 May;52(5):675–684. doi: 10.1111/j.1532-5415.2004.52202.x. [DOI] [PubMed] [Google Scholar]
- 15.Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the Chronic Care Model in the new millennium. Health Aff (Millwood) 2009 Jan-Feb;28(1):75–85. doi: 10.1377/hlthaff.28.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Aff (Millwood) 2001 Nov-Dec;20(6):64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- 17.Brown R, Peikes D, Chen A, Schore J. 15-site randomized trial of coordinated care in Medicare FFS. Health Care Financ Rev. 2008 Fall;30(1):5–25. [PMC free article] [PubMed] [Google Scholar]
- 18.Brown R. Strategies for Reining in Medicare Spending through Delivery System Reforms: Assessing the Evidence and Opportunities. Menlo Park, CA: The Henry J. Kaiser Family Foundation; 2009. [Google Scholar]
- 19.Rantz M, Popejoy LL, Galambos C, et al. The continued success of registered nurse care coordination in a state evaluation of aging in place in senior housing. Nurs Outlook. 2014 Jul-Aug;62(4):237–246. doi: 10.1016/j.outlook.2014.02.005. [DOI] [PubMed] [Google Scholar]
- 20.Chen A, Brown R, Archibald N, Aliotta S, Fox PD. Best Practices in Coordinated Care. Princeton, NJ: Mathematica Policy Research; 2000. [Google Scholar]
- 21.McDonald KM, Schultz E, Albin L, Pineda N, Lonhart J, Sundaram V, Smith-Spangler C, Brustrom J, Malcolm E. Care Coordination Measures Atlas. Rockville, MD: Agency for Healthcare Research and Quality; 2011. [Google Scholar]
- 22.Brown R. A Report Commissioned by the National Coalition on Care Coordination (N3C) Princeton, NJ: Mathematica Policy Research; 2009. The Promise of Care Coordination: Models that Decrease Hospitalizations and Improve Outcomes for Medicare Beneficiaries with Chronic Illnesses. [Google Scholar]
- 23.Bodenhimer TS, Berry-Millett R. Care Management of Patients with Complex Health Care Needs. Princeton, NJ: The Robert Wood Johnson Foundation; 2009. [Google Scholar]
- 24.CareFacts™. [Accessed July 22, 2015];CareFacts Information Systems. 2012 Available at http://www.carefacts.com/
- 25.Centers for Medicare and Medicaid Services. [Accessed July 22, 2015];CMS chronic condition data warehouse condition categories. Available at http://www.ccwdata.org/cs/groups/public/documents/document/ccw_conditioncategories.pdf.
- 26.Conn VS, Taylor SG, Kelley S. Medication regimen complexity and adherence among older adults. Image J Nurs Sch. 1991 Winter;23(4):231–235. doi: 10.1111/j.1547-5069.1991.tb00677.x. [DOI] [PubMed] [Google Scholar]
- 27.Maddigan SL, Farris KB, Keating N, Wiens CA, Johnson JA. Predictors of older adults’ capacity for medication management in a self-medication program: a retrospective chart review. J Aging Health. 2003 May;15(2):332–352. doi: 10.1177/0898264303251893. [DOI] [PubMed] [Google Scholar]
- 28.Sheikh JA, Yesavage JA. Geriatric depression scale (GDS): Recent evidence and development of a shorter version. In: Brink TL, editor. Clinical Gerontology: A Guide to Assessment and Intervention. New York: The Howarth Press, Inc; 1986. pp. 165–173. [Google Scholar]
- 29.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975 Nov;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 30.Kukull WA, Larson EB, Teri L, Bowen J, McCormick W, Pfanschmidt ML. The Mini-Mental State Examination score and the clinical diagnosis of dementia. J Clin Epidemiol. 1994 Sep;47(9):1061–1067. doi: 10.1016/0895-4356(94)90122-8. [DOI] [PubMed] [Google Scholar]
- 31.Reuben DB, Siu AL. An objective measure of physical function of elderly outpatients. The Physical Performance Test. J Am Geriatr Soc. 1990 Oct;38(10):1105–1112. doi: 10.1111/j.1532-5415.1990.tb01373.x. [DOI] [PubMed] [Google Scholar]
- 32.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992 Jun;30(6):473–483. [PubMed] [Google Scholar]
- 33.Martin KS. The Omaha System: A Key to Practice, Documentation, and Information Management. 2. Omaha, NE: Health Connections Press; 2005. [Google Scholar]
- 34.American Nurses Association. [Accessed July 22, 2015];ANA Recognized Terminologies and Data Element Sets. 2006 Available at http://www.nursingworld.org/npii/terminologies.htm.
- 35.Martin KS, Monsen KA, Bowles KH. The Omaha system and meaningful use: applications for practice, education, and research. Comput Inform Nurs. 2011 Jan-Feb;29(1):52–58. doi: 10.1097/NCN.0b013e3181f9ddc6. [DOI] [PubMed] [Google Scholar]
- 36.Westra BL, Solomon D, Ashley DM. Use of the Omaha System data to validate Medicare required outcomes in home care. J Healthc Inf Manag. 2006 Summer;20(3):88–94. [PubMed] [Google Scholar]
- 37.Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20:37–46. [Google Scholar]
- 38.Aronson AR, Lang FM. An overview of MetaMap: historical perspective and recent advances. J Am Med Inform Assoc. 2010 May-Jun;17(3):229–236. doi: 10.1136/jamia.2009.002733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.UMLS Reference Manual. Bethesda, MD: National Library of Medicine; 2009. [Accessed July 22, 2015]. Available at http://www.ncbi.nlm.nih.gov/books/NBK9676/ [Google Scholar]
- 40.Powers DMW. Evaluation: From precision, recall and F-measure to ROC, informedness, markedness & correlation. J Mach Lear Tech. 2011;2(1):37–63. [Google Scholar]
- 41.Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR, Beers MH. Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Arch Intern Med. 2003 Dec 8–22;163(22):2716–2724. doi: 10.1001/archinte.163.22.2716. [DOI] [PubMed] [Google Scholar]
- 42.Vanderboom CE, Thackeray NL, Rhudy LM. Key factors in patient-centered care coordination in ambulatory care: nurse care coordinators’ perspectives. Appl Nurs Res. 2015 Feb;28(1):18–24. doi: 10.1016/j.apnr.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 43.Jackson GL, Powers BJ, Chatterjee R, Bettger JP, Kemper AR, Hasselblad V, Dolor RJ, Irvine RJ, Heidenfelder BL, Kendrick AS, Gray R, Williams JW. The patient-centered medical home: A systematic review. Ann Intern Med. 2013 Feb;158(3):69–178. doi: 10.7326/0003-4819-158-3-201302050-00579. [DOI] [PubMed] [Google Scholar]
- 44.Ryan P, Sawin KJ. The Individual and Family Self-Management Theory: background and perspectives on context, process, and outcomes. Nurs Outlook. 2009;57(4):217–225. doi: 10.1016/j.outlook.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Heslop L, Power R, Cranwell K. Building workforce capacity for complex care coordination: a function analysis of workflow activity. Hum Resour Health. 2014;12:52. doi: 10.1186/1478-4491-12-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Westra BL, Oancea C, Savik K, Marek KD. The feasibility of integrating the Omaha system data across home care agencies and vendors. Comput Inform Nurs. 2010 May-Jun;28(3):162–171. doi: 10.1097/NCN.0b013e3181d7812c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Monsen KA, Fitzsimmons LL, Lescenski BA, Lytton AB, Schwichtenberg LD, Martin KS. A public health nursing informatics data-and-practice quality project. Comput Inform Nurs. 2006 May-Jun;24(3):152–158. doi: 10.1097/00024665-200605000-00012. [DOI] [PubMed] [Google Scholar]
- 48.Monsen KA, Fulkerson JA, Lytton AB, Taft LL, Schwichtenberg LD, Martin KS. Comparing maternal child health problems and outcomes across public health nursing agencies. Matern Child Health J. 2010 May;14(3):412–421. doi: 10.1007/s10995-009-0479-9. [DOI] [PubMed] [Google Scholar]
- 49.Popejoy LL, Khalilia MA, Popescu M, et al. Quantifying care coordination using natural language processing and domain-specific ontology. J Am Med Inform Assoc. 2015 Apr;22(e1):e93–103. doi: 10.1136/amiajnl-2014-002702. [DOI] [PMC free article] [PubMed] [Google Scholar]