Abstract
Introduction
Given the burden of road traffic injuries (RTIs) in South Africa, economic evaluations of prevention interventions are necessary for informing and prioritising public health planning and policy with regard to road safety.
Methods
In view of the dearth of RTI cost analysis, and in order to understand the extent to which RTI-related costs in South Africa compare with those in other low- and middle-income countries (LMICs), we reviewed published economic evaluations of RTI-related prevention in LMICs.
Results
Thirteen articles were identified, including cost-of-illness and cost-effectiveness studies. Although RTI-related risk factors in South Africa are well described, costing studies are limited. There is minimal information, most of which is not recent, with nothing at all on societal costs. Cost-effective interventions for RTIs in LMICs include bicycle and motorcycle helmet enforcement, traffic enforcement, and the construction of speed bumps.
Discussion
Policy recommendations from studies conducted in LMICs suggest a number of cost-effective interventions for consideration in South Africa. They include speed bumps for pedestrian safety, strategically positioned speed cameras, traffic enforcement such as the monitoring of seatbelt use, and breathalyzer interventions. However, interventions introduced in South Africa will need to be based either on South African cost-effectiveness data or on findings adapted from similar middle-income country settings.
Keywords: economic evaluation, cost-effectiveness analysis, injury, accidents, South Africa, low- and middle-income countries
Introduction
The Decade of Action for Road Safety 2011–2020, which is now at the halfway mark, began with goals to improve road and vehicle safety and increase the legislation and enforcement of the use of helmets, seatbelts, and child restraints; drink driving laws; and speed limits (1). Globally, efforts are underway to study these interventions, not only in terms of road traffic injuries (RTIs) and related deaths, but also their costs and cost-effectiveness. This is particularly relevant to low- and middle-income countries (LMICs) with constrained resources.
In South Africa, RTIs are a leading cause of injury-related deaths, accounting for 27 deaths per 100,000 people compared to the global average of 10 deaths per 100,000 (2). South Africa's injury-related mortality rate is higher than the aggregate death rate for the World Health Organization (WHO) African Region and nearly twice the global average. In 2012, RTIs in South Africa accounted for USD10.5 billion of health services expenditure, or 3% of gross domestic product (GDP) (3).
South Africa's RTI risk factors are well described by Statistics South Africa, the Road Transport Management Corporation, and the National Injury Mortality Surveillance System. These include lack of pedestrian safety measures, alcohol misuse, aggressive driving, and limited seatbelt use (4–6). Sixty percent of fatal RTIs are due to the influence of alcohol (4). Speeding is a factor in 30–50% of road traffic crashes (7). Concurrently, seatbelt use in South Africa is estimated to be 50%, at best, for front seat occupants, and 8% for rear-seated passengers (2). Seatbelt use is proportionally lower in lower-income areas within South Africa (8).
In 2008, the National Road Traffic Act introduced a number of safety requirements to address the risk factors outlined in Table 1, (9). However, over the last 8 years, implementing these legislative initiatives has been limited (10). In the absence of enforced legislation and targeted interventions, the costs of RTIs in South Africa are mounting, comprising more than 1.5 times South Africa's GDP per capita (4). Not only is this expenditure high compared to other LMICs, but it approaches the 3.8% of GDP allocated to all government public health spending in South Africa (11).
Table 1.
Road traffic injury (RTI) safety requirements introduced in South Africa's National Road Traffic Act, 2008
| RTI safety requirement |
| Cyclists wear helmets. |
| Child restraints are enforced. |
| Child pedestrian reflective clothing is evaluated. |
| Roadside alcohol testing is instituted. |
| Seatbelts must be functional. |
| Minibus taxis must provide seatbelts for drivers and at least one passenger. |
Source: South African Department of Transport, 2008.
The aim of this study is three-fold. First, describe sources of information and the full extent to which RTI-related costing data are available in South Africa. Second, describe the extent to which RTI-related costing data are available in other LMICs through a review of the literature. Third, use these findings to suggest potential cost-effective RTI prevention interventions for South Africa.
RTI data collection systems in South Africa
South African RTI-related data are collected by two independent organizations: the National Injury Mortality Surveillance System (NIMSS) and National Department of Transportation (NDOT). In 2008, NIMSS collected data from 39 mortuaries in seven of South Africa's nine provinces (5). The data are biased towards urban areas because the data from the rural mortuaries are concentrated in only one province. The data do not include costs.
The NDOT is the main source of RTI-related data, having published three reports to date (12–14). The first report, published in 2000, classified RTIs as fatal, severe, or minor from 1998 data collected by the Road Accident Fund (RAF) (12). The RAF is a statutory body that provides compulsory insurance to South African road users. In 2002, the NDOT published its second report: a cost of RTI survey based on 363 household interviews (13). The third report, published in 2004, analysed data from the RAF (14). The 2000 and 2004 publications reported the exact number and distribution of RTI fatalities; an additional study described the national costs associated with RTIs by referencing the 2000 report as its primary data source (15). In an effort to avoid duplication, we report only findings from the 2000 report that used 1998 data, emphasizing that South African costing studies are based on data that is now nearly 20 years old.
Costs of RTIs in South Africa
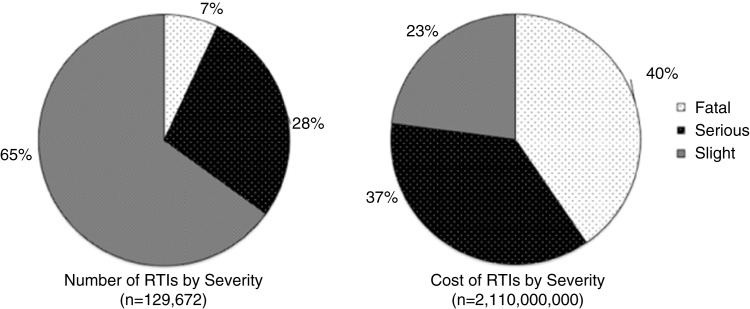
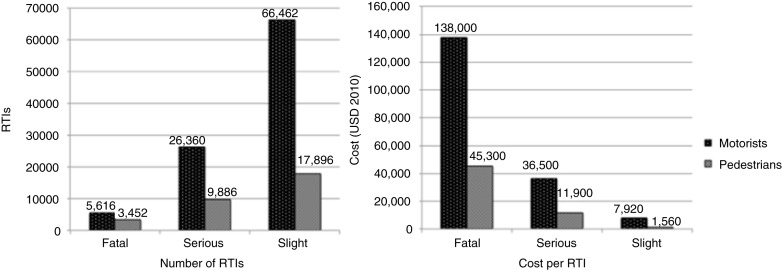
In 1998, there were 129,672 RTIs that cost more than USD 1.57 billion, or USD 2.1 billion, when converted to 2010 values, although the type of costs included in this estimate is not stated (12). Seven percent of these RTIs were fatal and accounted for 40% of the total costs; slight injuries accounted for 65% of RTIs but only 23% of costs (Fig. 1) (12). In contrast, pedestrian injuries accounted for 24% of all RTI-related injuries, but only 13% of total costs. Fatal and severe pedestrian injury costs were much lower than similar motorist expenditures (Fig. 2) (12). The NDOT did not define ‘serious’ and ‘slight’ injuries, limiting the ability to generalize findings to other studies.
Fig. 1.
The total number and total costs of road traffic injuries (RTIs) in South Africa in 1998. Source: Department of Transport, South Africa (12).
Fig. 2.
The total number and total costs of road traffic injuries (RTIs) in South Africa in 1998, by severity and status (costs reported in USD 2010). Source: Department of Transport, South Africa (12).
In 2009, alcohol-related RTIs in South Africa resulted in USD 940.6 million in damage to motor vehicles (16). Only one study has looked at cost-effectiveness with regard to seatbelts and RTIs: Harris and Olukoga showed that if seatbelt usage increased in urban areas by an additional 16% from a baseline rate of 32%, RTIs could decrease by 9.5% (17). Assuming linearity, this translates to a savings of USD 2.72 million in a single South African province (17). With the exception of this study, cost analyses of RTI prevention interventions are absent in South Africa.
There are many ways to describe the costs of RTIs. However, in our review of the data, we found that the published studies described above often did not define the types of costs that were included. The cost of health care includes much more than the upfront hospital bills. Costs can be categorized into three groups: provider costs defined as the organizing and operating costs of health sector; patient costs defined as the costs borne by the patients and their families; and societal costs or costs borne externally to the health sector and the patient (18). These important cost distinctions are not made in the current South African published literature.
As such, it is difficult to compare the costs between studies and even understand the economic magnitude of RTI in South Africa. Moreover, our review of the South African literature of the RTI cost data available over the last two decades found that, arguably, one of the most important categories of costs-effectiveness – cost analysis – is lacking (19). In view of the dearth of RTI cost-analysis data and to understand the extent to which RTI-related costs in South Africa compare to costs in other LMICs, we reviewed published economic evaluations of RTI-related prevention in LMICs.
Methods
Six databases, including PubMed/Medline (20), Embase (21), the Cochrane Library (22), EconLit (23), Econbase (24), and the National Health Service Economic Evaluation Database (25), were searched to identify articles containing information on the costs associated with RTIs in LMICs. Searches were not limited by year or language. Citations and reference lists were reviewed to further identify relevant studies (26). Our search terms are provided in Appendix.
All citations were imported into an electronic database (Refworks®, Proquest, Bethesda, MD) and two reviewers independently assessed the identified studies. Titles and abstracts were screened for initial exclusion. Articles were excluded if they were not relevant to LMICs and RTIs, and did not discuss economic evaluations. Review articles, commentaries, and editorials were excluded. The full texts of articles were then obtained and reviewed using the same exclusion criteria. Studies were included if they described an economic evaluation of RTIs in a LMIC. Information was extracted using a standardized data form and tabulated in Microsoft Excel® for the following categories: study aim, setting, sample population, type of economic evaluation, methods, data sources, and findings.
As part of a descriptive analysis of the data, studies were grouped according to the type of economic evaluation that best reflected their aim, design, and methods. They included partial and full economic evaluations. Partial evaluations included studies that examined either the costs of the output (RTIs) or input (prevention interventions), but not both (18). For the purposes of this review, these studies were classified as either cost-of-injury or cost-of-prevention studies. Cost-of-injury studies categorized costs as medical costs, costs associated with loss of productivity, and total costs (27, 28). Loss of productivity was attributed to absence from work and premature death (29). Cost-of-prevention studies described the costs associated with purchasing an RTI-related safety device or implementing a prevention intervention.
Full economic evaluation studies, which include cost-effectiveness analyses (CEAs), cost-benefit analyses (CBAs), and cost-utility analyses (CUAs), compare the relative costs and outcomes of two or more interventions. CEAs report costs as a ratio: the denominator is a gain in health, such as a year of life, and the numerator is the cost associated with that health gain. CBAs report costs in terms of willingness to pay (WTP) for injury prevention tools. CUAs, a variant of CEA, report consequences in terms of preference-based measures of health, such as quality-adjusted life years (QALYs) (18).
Results
Our review identified 13 articles that met inclusion criteria (Fig. 3). In one article, four CEAs were performed using baseline data from four different studies (30). For the purposes of this review, we present these analyses separately, giving a total of 16 economic evaluation studies (Table 2).
Fig. 3.
Search strategy flowchart.
Table 2.
Published studies that describe economic evaluations of road traffic injuries (RTIs) in low- and middle-income countries (costs reported in USD 2010)
| Author, Year | Country | WHO region | Intervention/study aim | Study setting | Study sample | Methods and data source | Findings |
|---|---|---|---|---|---|---|---|
| Cost of injury | |||||||
| Al-Masaeid, 1998 (31) | Jordan | EMRO | Estimate the cost of RTIs. | National level | 15,375 RTIs | Cost of RTIs from police, insurance, and hospital data | Mean RTI cost per injured person: $4,200 |
| Hijar, 2004 (32) | Mexico | AMRO | Analyses the impact of RTIs on demand for hospital emergency services. | 4 urban hospitals | 233 RTIs | Cost of RTI from patient interviews | Pedestrians had higher health care costs and 80% paid out of pocket, compared to 45% of drivers and passengers |
| Anh, 2005 (33) | Vietnam | SEARO | Estimate the cost of RTIs. | National Level | 26,925 RTIs | Cost of RTI from police, court, and insurance data | Mean RTI cost per injured person: $8,770 |
| Riewpaiboon 2008 (34) | Thailand | SEARO | Estimate the cost of RTIs. | District hospital | 200 RTIs | Cost of RTI from hospital records | Mean RTI cost per injured person: $2,980 |
| Riewpaiboon 2008 (35) | Thailand | SEARO | Develop a drug cost model for RTI patients. | Urban hospital | 3,723 RTIs | Cost of RTI described in a drug cost model | Mean predicted RTI drug cost per injured person: $21 |
| Li, 2011 (36) | China | WPRO | Estimate the cost of bicycle injuries. | Urban city | 550 bicycle-related injuries | Cost of bicycle injuries from hospital records and government data | Mean bicycle-related injury costs per injured person: $4,330. Total productivity loss: $136 million (10.9% GDP) |
| Parkinson, 2014 (37) | South Africa | AFRO | Estimate the cost of RTIs. | District hospital | 100 RTIs | Cost of RTI from hospital records | Mean RTI cost per injured person: $6,610 |
| Cost of RTI prevention | |||||||
| Bishai, 2003 (38) | Uganda, Pakistan | AFRO, EMRO | Assess the effectiveness of road safety investments. | National level | Model | Analysis of road safety expenditures data | National cost per capita on road safety Pakistan: $0.09; Uganda: $0.12 |
| Hendrie, 2004 (39) | Albania, China, Philippines Thailand, Venezuela, Vietnam | EURO, WPRO, SEARO AMRO |
Compare the affordability of safety devices. | Urban settings | Retail stores and internet vendors | Affordability defined as hours needed to work to afford safety device | Mean cost and number of factory hours needed to work to pay for safety devices: Car seat: $102; 30.9 h Booster seat: $98.7; 36.7 h Motorcycle helmet: $15.7; 4.1 h |
| Cost-benefit analysis | |||||||
| Pham, 2008 (40) | Vietnam | WPRO | Estimate WTP for motorcycle helmets. | Urban city | 414 households | Households’ WTP | A $3.99 government subsidy resulted in a 99% WTP for a motorcycle helmet |
| Cost-utility analysis | |||||||
| Tsauo, 1999 (41) | Taiwan | WPRO | Estimate the costs and effectiveness of motorcycle helmet enforcement. | Urban city | 99 RTIs with head injury | QAST (42, 43) | Motorcycle helmet enforcement could decrease RTI-related head injuries by 1,300, or 6,240 QALYs gained |
| Cost-effectiveness analysis | |||||||
| Bishai, 2006 (30) | China | WPRO | Estimate the costs and effectiveness of bicycle helmet enforcement. | Provincial level | Model | CEA modelling using data from Li, 199744 | Bicycle helmet enforcement could decrease RTI-related head injuries by 85% or $131 per DALY averted |
| Bishai, 2006 (30) | China | WPRO | Estimate the costs and effectiveness of motorcycle helmet enforcement. | National Level | Model | CEA modelling using data from Zhang, 2004 (45) and Ichikawa, 2003 (46) | Motorcycle helmet enforcement could decrease RTI-related head injuries by 41% or $572 per DALY averted |
| Bishai, 2006 (30) | Brazil | AMRO | Estimate the costs and effectiveness of traffic enforcement. | WHO regions | Model | CEA modelling using data from Poli de Figueiredo, 2001 (47) | Traffic enforcement could decrease RTI-related deaths by 25% or $78.4 per DALY averted |
| Bishai, 2006 (30) | Ghana | AFRO | Estimate the costs and effectiveness of speed bumps. | National level | Model | CEA modelling using data from Afukaar, 2003 (48) | Speed bumps could decrease RTI-related deaths by 10% or $10.9 per DALY averted |
| Bishai, 2008 (49) | Uganda | AFRO | Estimate the costs and effectiveness of traffic enforcement. | Urban city | 10 police stations | ARIMA and Poisson regression | Traffic enforcement could decrease RTI-related deaths by 17% or $669 per death averted |
| Chisholm, 2008 (50) | All countries | All regions | Estimate the costs and effectiveness of multiple RTI interventions. | All WHO regions | Model | CEA modelling | DALYs saved range from 415 to 425,093 or $1,380–$5,400 per DALY averted |
ARIMA: autoregressive integrated moving average; CEA: cost-effectiveness analysis; DALYs: disability-adjusted life years; QALYs: quality-adjusted life years; QAST: quality-adjusted survival time WTP: willingness to pay.
Of the six cost-of-injury studies, four described the average RTI costs per injured person in terms of total, medical, and loss of productivity costs (Table 3) (31, 33, 34, 36). Total costs ranged between USD 2,980 and USD 8,770. The majority of costs were due to loss of productivity (63–96% of total costs). Medical treatment accounted for 1–14% of total costs. South Africa's cost estimates were crudely two to four times higher than costs reported from Jordan, Thailand, Vietnam, and China. These comparisons should, however, be cautiously considered; each study reported different cost standards and included varying cost components, data sources, study sample populations, dates, and settings. Additionally, these four studies were conducted in four different countries and three different regions, with differing medical care costs and GDPs per capita, further limiting cost comparisons, although the use of international dollars can enhance comparability.
Table 3.
Estimates of costs of road traffic and bicycle injuries per injured person (costs reported in USD 2010)
| Injury | Country | Year data were collected | Injured persons in study (n) | Medical costs | Loss of productivity costs | Total costs |
|---|---|---|---|---|---|---|
| Road traffic injuries | South Africa (12) | 1998 | 80,622 | $990 | $5,486 | $16,200a |
| Jordan (31) | 1996 | 15,927 | $473 | $1,630 | $4,200b | |
| Thailand (34) | 2004 | 200 | $93 | $2,860 | $2,980c | |
| Vietnam (33) | 2004 | 26,925 | $1,260 | $3,810 | $8,770d | |
| South Africa (37) | 2014 | 100 | $6,610 | N/A | N/A | |
| Bicycle injuries | China (36) | 2004 | 36,705 | $58 | $3,760 | $4,330e |
Total costs include medical, loss of productivity, property damage (including vehicle damage, damage to goods carried, and damage to fixed property), pain and suffering, insurance administrative, legal, policy and promotion, and towing costs.
Total costs include medical, loss of productivity (output), temporary losses, community and family loses, and pain and suffering.
Total costs include: medical costs, loss of productivity, property damage (including vehicle damage, damage to goods, and damage to fixed property), pain and suffering, insurance administrative costs, legal costs, and funeral costs.
Total costs include medical costs and loss of productivity costs.
Total costs include total medical costs and loss of productivity.
In addition to the cost of injury, our review highlighted studies that described the cost of RTI prevention projects. Two studies described the national costs per capita invested in RTI prevention in Uganda and Pakistan and the mean cost of safety restraints in four WHO regions (38, 39). However, without a complete understanding of the context in which the data were collected, the results must be interpreted cautiously. Only two studies, both from Vietnam, explored this in the context of motorcycle helmets (40, 41). Although these studies present interesting findings regarding the acceptance of motorcycle helmet usage among the study participants, we note that the application and use of these methods in other regions are limited in the published literature.
Table 4 presents findings from CEA models regarding RTI prevention interventions in terms of the cost per disability-adjusted life years (DALYs) averted. Many of these analyses are highlighted in the second edition of Disease Control Priorities in Developing Countries (30, 49–51). These interventions include bicycle and motorcycle helmet usage, traffic enforcement, and the construction of speed bumps. Findings suggest that at USD 10.9 per DALY averted, speed bumps may be one of the most cost-effective interventions, followed by seatbelt usage and bicycle helmet enforcement at USD 101 and USD 131 per DALY averted, respectively (17, 30). Traffic enforcement, according to three different models, ranged from USD 78.4 to USD 1,860 per DALY averted (30, 49, 50).
Table 4.
Annualized costs and DALYs averted of road traffic injury (RTI) prevention interventions
| Intervention | Author, year | Study or model location | Cost per DALY averted |
|---|---|---|---|
| Traffic enforcement | Bishai, 2006 (30) | All WHO regions | $78.4 |
| Bishai, 2008 (49) | Uganda | $96 | |
| Speed bumps | Bishai, 2006 (30) | Ghana | $10.9 |
| Speed limit enforcement via mobile cameras | Chisholm, 2008 (50) | AfroE | $77,200 |
| Bicycle helmet enforcement | Bishai, 2006 (30) | China | $131 |
| Chisholm, 2008 (50) | AfroE | $51,400 | |
| Motorcycle helmet enforcement | Bishai, 2006 (30) | China | $572 |
| Chisholm, 2008 (50) | AfroE | $8,680 | |
| Seatbelt usage | Harris, 2005 (17) | South Africa | $28.70 |
| Chisholm, 2008 (50) | AfroE | $22,400 | |
| Drink driving laws and enforcement via breath-testing | Chisholm, 2008 (50) | AfroE | $51,300 |
Discussion
Costing implications for South Africa
In the South African context of a quadruple burden of disease, RTIs place a significant burden on a society and health care system already faced with competing priorities. In addition to the growing burden of injuries, South Africa must contend with the ongoing HIV and tuberculosis epidemics, the exploding burden of obesity-related non-communicable diseases, and an unfinished agenda to address maternal and child mortality (2). Evidence-based studies are needed to show the costs and affordability of effective interventions, particularly how they relate to South Africa's major RTI risk factors: lack of pedestrian safety measures, alcohol misuse, aggressive driving, and limited seatbelt use. Policymakers are more likely to act if they understand the financial implications, especially for budgets already under pressure. Full economic evaluations, such as CEAs, are appropriate tools to achieve this: they describe the health benefits gained, and also the costs saved.
From the literature review, and as outlined in Table 5, the only full economic evaluation conducted in South Africa relates to seatbelt usage. Moreover, the societal costs associated with RTIs were not included in any of the reviewed studies. In South Africa, there is no practical methodology in place to value the household costs of injury-related illness. Due to high unemployment rates, the use of average salaries may not be a good measure, particularly in rural areas where unemployment is highest. Although there are methods that can be used to value these household costs, and it is possible to use more than one method with sensitivity analysis, methodological development is needed to include broader societal costs in economic evaluations of RTIs in South Africa.
Table 5.
Summary of availability of road traffic injury (RTI) cost-effectiveness studies
| Are cost-effectiveness studies available? | ||
|---|---|---|
|
|
||
| RTI intervention | In LMICs | In South Africa |
| Traffic enforcement | Yes | No |
| Speed bumps | Yes | No |
| Alcohol misuse | Yes | No |
| Bicycle helmet enforcement | Yes | No |
| Motorcycle helmet enforcement | Yes | No |
| Seatbelt usage | Yes | Yes |
LMICs: low- and middle-income countries.
We propose that South African surveillance systems already in place to collect demographic RTI data, such as the NIMSS and NDOT, could expand their scope of work to include provider, patient, and societal costing data. This could enhance not only our understanding of the costs associated with RTIs, but also allow policy makers to use such data as evidence to invest in RTI prevention. Recently published economic evaluation guidelines, such as the Consolidated Health Economic Evaluation Reporting Standards, offer methods to conduct and report economic evaluations (52). These resources would allow South Africa to move forward to improve data collection and, ultimately, health resource allocation.
Context-specific evidence for RTI risk factors is critical for informing and implementing targeted interventions. In South Africa, we know that major RTI risk factors are aggressive driving, lack of pedestrian safety measures, limited seatbelt use, and alcohol misuse. As such, some of the ‘best buys’ from other LMICs might be applicable in South Africa. For example, at USD 10.9 per DALY averted, speed bumps may be one of the most cost-effective interventions, followed by seatbelt usage and bicycle helmet enforcement at USD 101 and USD 131 per DALY averted, respectively (17, 30). Economies of scale could also be considered for the roadside enforcement of traffic codes, which may only incur incremental costs for monitoring seatbelt use (53). With regard to drinking-and-driving campaigns, interventions that require breathalyzers might be expensive but effective (50). Weighing the costs of legislating, regulating, and enforcing the regional trade of alcohol against the costs of lost lives and productivity from alcohol-related RTIs could be a comparison to use the point of departure for performing an economic analysis (54, 55).
A key aspect of the Decade of Action for Road Safety 2011–2020 is to support research that will provide data not only in terms of road traffic deaths and injuries but also in terms of costs (56). Thus far, the majority of the evidence focused on the cost-effectiveness of injury prevention has taken place in HICs in which less than 10% of the global burden of traffic injury occurs (57–60).
Strong political will, capacity enhancement, and cultural applicability are fundamental to addressing road injuries. Including many actors, such as business and government, could be transformative. Preventing road crashes will be shaped by factors largely outside the health system, as explicitly acknowledged by the WHO Marmot Commission on Social Determinants of Health (61). The South African National Planning Commission, an expert multi-sector panel, has emphasized RTI prevention as a priority for South Africa by 2030 (62). Context-specific data on the cost-effectiveness of prevention of RTIs in South Africa is essential, but this alone will not prevent injuries.
Conclusion
Road safety is a growing public health issue in South Africa. Economic evaluations of road safety interventions are needed to understand the cost of RTIs and inform policy makers about choices between competing spending priorities.
Appendix: Key terms formatted for PubMed
(‘Road traffic injury’[All Fields] OR ‘road traffic injuries’[All Fields]) AND (“cost-benefit analysis”[MeSH Terms] OR ‘cost effectiveness’[All Fields] OR ‘cost analysis’[All Fields]) AND (“Cote d'Ivoire”[All Fields] OR “eritrea”[MeSH Terms] OR (“eritrea”[MeSH Terms] OR “eritrea”[All Fields]) OR “ethiopia”[MeSH Terms] OR (“ethiopia”[MeSH Terms] OR “ethiopia”[All Fields]) OR “gambia”[MeSH Terms] OR (“gambia”[MeSH Terms] OR “gambia”[All Fields]) OR “ghana”[MeSH Terms] OR (“ghana”[MeSH Terms] OR “ghana”[All Fields]) OR “guinea”[MeSH Terms] OR (“guinea”[MeSH Terms] OR “guinea”[All Fields]) OR “guinea-bissau”[MeSH Terms] OR (“guinea-bissau”[MeSH Terms] OR “guinea-bissau”[All Fields] OR (“guinea”[All Fields] AND “bissau”[All Fields]) OR “guinea bissau”[All Fields]) OR “haiti”[MeSH Terms] OR (“haiti”[MeSH Terms] OR “haiti”[All Fields]) OR “india”[MeSH Terms] OR (“india”[MeSH Terms] OR “india”[All Fields]) OR “kenya”[MeSH Terms] OR (“kenya”[MeSH Terms] OR “kenya”[All Fields]) OR Democratic[All Fields] AND (“korea”[All Fields] OR “korea”[MeSH Terms]) OR “Kyrgyz Republic”[All Fields] OR “Lao PDR”[All Fields] OR “lesotho”[MeSH Terms] OR (“lesotho”[MeSH Terms] OR “lesotho”[All Fields]) OR “liberia”[MeSH Terms] OR (“liberia”[MeSH Terms] OR “liberia”[All Fields]) OR “madagascar”[MeSH Terms] OR (“madagascar”[MeSH Terms] OR “madagascar”[All Fields]) OR “malawi”[MeSH Terms] OR (“malawi”[MeSH Terms] OR “malawi”[All Fields]) OR “mali”[MeSH Terms] OR (“mali”[MeSH Terms] OR “mali”[All Fields]) OR “mauritania”[MeSH Terms] OR (“mauritania”[MeSH Terms] OR “mauritania”[All Fields]) OR “moldova”[MeSH Terms] OR (“moldova”[MeSH Terms] OR “moldova”[All Fields]) OR “mongolia”[MeSH Terms] OR (“mongolia”[MeSH Terms] OR “mongolia”[All Fields]) OR “mozambique”[MeSH Terms] OR (“mozambique”[MeSH Terms] OR “mozambique”[All Fields]) OR “myanmar”[MeSH Terms] OR (“myanmar”[MeSH Terms] OR “myanmar”[All Fields]) OR “nepal”[MeSH Terms] OR (“nepal”[MeSH Terms] OR “nepal”[All Fields]) OR “nicaragua”[MeSH Terms] OR (“nicaragua”[MeSH Terms] OR “nicaragua”[All Fields]) OR “niger”[MeSH Terms] OR (“niger”[MeSH Terms] OR “niger”[All Fields]) OR “nigeria”[MeSH Terms] OR (“nigeria”[MeSH Terms] OR “nigeria”[All Fields]) OR “North Korea”[All Fields] OR “DPRK”[All Fields] OR “pakistan”[MeSH Terms] OR (“pakistan”[MeSH Terms] OR “pakistan”[All Fields]) OR “Papua New Guinea”[All Fields] OR “rwanda”[MeSH Terms] OR (“rwanda”[MeSH Terms] OR “rwanda”[All Fields]) OR “Sao Tome and Principe”[All Fields] OR “senegal”[MeSH Terms] OR (“senegal”[MeSH Terms] OR “senegal”[All Fields]) OR “Sierra Leone”[All Fields] OR “Solomon Islands”[All Fields] OR “somalia”[MeSH Terms] OR (“somalia”[MeSH Terms] OR “somalia”[All Fields]) OR “sudan”[MeSH Terms] OR (“sudan”[MeSH Terms] OR “sudan”[All Fields]) OR “tajikistan”[MeSH Terms] OR (“tajikistan”[MeSH Terms] OR “tajikistan”[All Fields]) OR “tanzania”[MeSH Terms] OR (“tanzania”[MeSH Terms] OR “tanzania”[All Fields]) OR “east timor”[All Fields] OR “east timor”[MeSH Terms] OR (“east timor”[MeSH Terms] OR (“east”[All Fields] AND “timor”[All Fields]) OR “east timor”[All Fields] OR (“timor”[All Fields] AND “leste”[All Fields]) OR “timor leste”[All Fields]) OR “togo”[MeSH Terms] OR (“togo”[MeSH Terms] OR “togo”[All Fields]) OR “uganda”[MeSH Terms] OR (“uganda”[MeSH Terms] OR “uganda”[All Fields]) OR “uzbekistan”[MeSH Terms] OR (“uzbekistan”[MeSH Terms] OR “uzbekistan”[All Fields]) OR “vietnam”[MeSH Terms] OR (“vietnam”[MeSH Terms] OR “vietnam”[All Fields]) OR “yemen”[MeSH Terms] OR (“yemen”[MeSH Terms] OR “yemen”[All Fields]) OR “Republic of Yemen”[All Fields] OR “democratic republic of the congo”[All Fields] OR “democratic republic of the congo”[MeSH Terms] OR (“democratic republic of the congo”[MeSH Terms] OR (“democratic”[All Fields] AND “republic”[All Fields] AND “congo”[All Fields]) OR “democratic republic of the congo”[All Fields] OR “zaire”[All Fields]) OR “zambia”[MeSH Terms] OR (“zambia”[MeSH Terms] OR “zambia”[All Fields]) OR “zimbabwe”[MeSH Terms] OR (“zimbabwe”[MeSH Terms] OR “zimbabwe”[All Fields]) OR “albania”[MeSH Terms] OR (“albania”[MeSH Terms] OR “albania”[All Fields]) OR “algeria”[MeSH Terms] OR (“algeria”[MeSH Terms] OR “algeria”[All Fields]) OR “angola”[MeSH Terms] OR (“angola”[MeSH Terms] OR “angola”[All Fields]) OR “armenia”[MeSH Terms] OR (“armenia”[MeSH Terms] OR “armenia”[All Fields]) OR “azerbaijan”[MeSH Terms] OR (“azerbaijan”[MeSH Terms] OR “azerbaijan”[All Fields]) OR “byelarus”[MeSH Terms] OR (“byelarus”[MeSH Terms] OR “byelarus”[All Fields] OR “belarus”[All Fields]) OR “bolivia”[MeSH Terms] OR (“bolivia”[MeSH Terms] OR “bolivia”[All Fields]) OR “Bosnia and Herzegovina”[All Fields] OR “brazil”[MeSH Terms] OR (“brazil”[MeSH Terms] OR “brazil”[All Fields]) OR “bulgaria”[MeSH Terms] OR (“bulgaria”[MeSH Terms] OR “bulgaria”[All Fields]) OR “Cape Verde”[All Fields] OR “china”[MeSH Terms] OR (“china”[MeSH Terms] OR “china”[All Fields]) OR “colombia”[MeSH Terms] OR (“colombia”[MeSH Terms] OR “colombia”[All Fields]) OR “cuba”[MeSH Terms] OR (“cuba”[MeSH Terms] OR “cuba”[All Fields]) OR “djibouti”[MeSH Terms] OR (“djibouti”[MeSH Terms] OR “djibouti”[All Fields]) OR “Dominican Republic”[All Fields] OR “ecuador”[MeSH Terms] OR (“ecuador”[MeSH Terms] OR “ecuador”[All Fields]) OR “egypt”[MeSH Terms] OR (“egypt”[MeSH Terms] OR “egypt”[All Fields]) OR “Arab Republic of Egypt”[All Fields] OR “El Salvador”[All Fields] OR “fiji”[MeSH Terms] OR (“fiji”[MeSH Terms] OR “fiji”[All Fields]) OR “georgia republic”[MeSH Terms] OR “georgia”[tiab] OR “georgia (republic)”[MeSH Terms] OR “guatemala”[MeSH Terms] OR (“guatemala”[MeSH Terms] OR “guatemala”[All Fields]) OR “guyana”[MeSH Terms] OR (“guyana”[MeSH Terms] OR “guyana”[All Fields]) OR “honduras”[MeSH Terms] OR (“honduras”[MeSH Terms] OR “honduras”[All Fields]) OR “indonesia”[MeSH Terms] OR (“indonesia”[MeSH Terms] OR “indonesia”[All Fields]) OR “iran”[MeSH Terms] OR (“iran”[MeSH Terms] OR “iran”[All Fields]) OR “Islamic Republic of Iran”[All Fields] OR “iraq”[MeSH Terms] OR (“iraq”[MeSH Terms] OR “iraq”[All Fields]) OR “jamaica”[MeSH Terms] OR (“jamaica”[MeSH Terms] OR “jamaica”[All Fields]) OR “jordan”[MeSH Terms] OR (“jordan”[MeSH Terms] OR “jordan”[All Fields]) OR “kazakhstan”[MeSH Terms] OR (“kazakhstan”[MeSH Terms] OR “kazakhstan”[All Fields]) OR “micronesia”[All Fields] OR “micronesia”[MeSH Terms] OR (“micronesia”[MeSH Terms] OR “micronesia”[All Fields] OR “kiribati”[All Fields]) OR “macedonia republic”[MeSH Terms] OR (“macedonia (republic)”[MeSH Terms] OR (“macedonia”[All Fields] AND “(republic)”[All Fields]) OR “macedonia (republic)”[All Fields] OR “macedonia”[All Fields]) OR “FYR of Macedonia”[All Fields] OR “Former Yugoslav Republic of Macedonia”[All Fields] OR “indian ocean islands”[All Fields] OR “indian ocean islands”[MeSH Terms] OR (“indian ocean islands”[MeSH Terms] OR (“indian”[All Fields] AND “ocean”[All Fields] AND “islands”[All Fields]) OR “indian ocean islands”[All Fields] OR “maldives”[All Fields]) OR “Marshall Islands”[All Fields] OR “micronesia”[MeSH Terms] OR (“micronesia”[MeSH Terms] OR “micronesia”[All Fields]) OR “Federated States of Micronesia”[All Fields] OR “morocco”[MeSH Terms] OR (“morocco”[MeSH Terms] OR “morocco”[All Fields]) OR “namibia”[MeSH Terms] OR (“namibia”[MeSH Terms] OR “namibia”[All Fields]) OR “paraguay”[MeSH Terms] OR (“paraguay”[MeSH Terms] OR “paraguay”[All Fields]) OR “peru”[MeSH Terms] OR (“peru”[MeSH Terms] OR “peru”[All Fields]) OR “philippines”[MeSH Terms] OR (“philippines”[MeSH Terms] OR “philippines”[All Fields]) OR “romania”[MeSH Terms] OR (“romania”[MeSH Terms] OR “romania”[All Fields]) OR “samoa”[MeSH Terms] OR (“samoa”[MeSH Terms] OR “samoa”[All Fields]) OR “Serbia and Montenegro”[All Fields] OR “Sri Lanka”[All Fields] OR “suriname”[MeSH Terms] OR (“suriname”[MeSH Terms] OR “suriname”[All Fields]) OR “swaziland”[MeSH Terms] OR (“swaziland”[MeSH Terms] OR “swaziland”[All Fields]) OR “Syrian Arab Republic”[All Fields] OR “syria”[MeSH Terms] OR (“syria”[MeSH Terms] OR “syria”[All Fields]) OR “thailand”[MeSH Terms] OR (“thailand”[MeSH Terms] OR “thailand”[All Fields]) OR “tonga”[MeSH Terms] OR (“tonga”[MeSH Terms] OR “tonga”[All Fields]) OR “tunisia”[MeSH Terms] OR (“tunisia”[MeSH Terms] OR “tunisia”[All Fields]) OR “turkmenistan”[MeSH Terms] OR (“turkmenistan”[MeSH Terms] OR “turkmenistan”[All Fields]) OR “ukraine”[MeSH Terms] OR (“ukraine”[MeSH Terms] OR “ukraine”[All Fields]) OR “vanuatu”[MeSH Terms] OR (“vanuatu”[MeSH Terms] OR “vanuatu”[All Fields]) OR “West Bank and Gaza”[All Fields] OR “American Samoa”[All Fields] OR “Antigua and Barbuda”[All Fields] OR “argentina”[MeSH Terms] OR (“argentina”[MeSH Terms] OR “argentina”[All Fields]) OR “barbados”[MeSH Terms] OR (“barbados”[MeSH Terms] OR “barbados”[All Fields]) OR “belize”[MeSH Terms] OR (“belize”[MeSH Terms] OR “belize”[All Fields]) OR “botswana”[MeSH Terms] OR (“botswana”[MeSH Terms] OR “botswana”[All Fields]) OR “chile”[MeSH Terms] OR (“chile”[MeSH Terms] OR “chile”[All Fields]) OR “Costa Rica”[All Fields] OR “croatia”[MeSH Terms] OR (“croatia”[MeSH Terms] OR “croatia”[All Fields]) OR “Czech Republic”[All Fields] OR “dominica”[MeSH Terms] OR (“dominica”[MeSH Terms] OR “dominica”[All Fields]) OR “Equatorial Guinea”[All Fields] OR “estonia”[MeSH Terms] OR (“estonia”[MeSH Terms] OR “estonia”[All Fields]) OR “gabon”[MeSH Terms] OR (“gabon”[MeSH Terms] OR “gabon”[All Fields]) OR “grenada”[MeSH Terms] OR (“grenada”[MeSH Terms] OR “grenada”[All Fields]) OR “hungary”[MeSH Terms] OR (“hungary”[MeSH Terms] OR “hungary”[All Fields]) OR “latvia”[MeSH Terms] OR (“latvia”[MeSH Terms] OR “latvia”[All Fields]) OR “lebanon”[MeSH Terms] OR (“lebanon”[MeSH Terms] OR “lebanon”[All Fields]) OR “libya”[MeSH Terms] OR (“libya”[MeSH Terms] OR “libya”[All Fields]) OR “lithuania”[MeSH Terms] OR (“lithuania”[MeSH Terms] OR “lithuania”[All Fields]) OR “malaysia”[MeSH Terms] OR (“malaysia”[MeSH Terms] OR “malaysia”[All Fields]) OR “mauritius”[MeSH Terms] OR (“mauritius”[MeSH Terms] OR “mauritius”[All Fields]) OR “comoros”[All Fields] OR “comoros”[MeSH Terms] OR (“comoros”[MeSH Terms] OR “comoros”[All Fields] OR “mayotte”[All Fields]) OR “mexico”[MeSH Terms] OR (“mexico”[MeSH Terms] OR “mexico”[All Fields]) OR “Northern Mariana Islands”[All Fields] OR “oman”[MeSH Terms] OR (“oman”[MeSH Terms] OR “oman”[All Fields]) OR “palau”[MeSH Terms] OR (“palau”[MeSH Terms] OR “palau”[All Fields]) OR “panama”[MeSH Terms] OR (“panama”[MeSH Terms] OR “panama”[All Fields]) OR “poland”[MeSH Terms] OR (“poland”[MeSH Terms] OR “poland”[All Fields]) OR “Russian Federation”[All Fields] OR “seychelles”[MeSH Terms] OR (“seychelles”[MeSH Terms] OR “seychelles”[All Fields]) OR “Slovak Republic”[All Fields] OR “South Africa”[All Fields] OR “St. Kitts and Nevis”[All Fields] OR “St. Lucia”[All Fields] OR “St. Vincent and the Grenadines”[All Fields] OR “Trinidad and Tobago”[All Fields] OR “turkey”[MeSH Terms] OR (“turkey”[MeSH Terms] OR “turkey”[All Fields]) OR “uruguay”[MeSH Terms] OR (“uruguay”[MeSH Terms] OR “uruguay”[All Fields]) OR “venezuela”[MeSH Terms] OR (“venezuela”[MeSH Terms] OR “venezuela”[All Fields]) OR “developing countries”[All Fields] OR “less developed countries”[All Fields] OR “third-world countries”[All Fields] OR “under-developed countries”[All Fields] OR “poOR countries”[All Fields] OR “less developed countries”[All Fields] OR “under developed countries”[All Fields] OR “less developed nations”[All Fields] OR “third world nations”[All Fields] OR “under developed nations”[All Fields] OR “developing nations”[All Fields] OR “poOR nations”[All Fields] OR “poor economies”[All Fields] OR “developing economies”[All Fields] OR “less developed economies”[All Fields] OR “myanmar”[MeSH Terms] OR (“myanmar”[MeSH Terms] OR “myanmar”[All Fields] OR “burma”[All Fields]) OR “Czechoslovakia”[All Fields] OR “Democratic Republic of Congo”[All Fields] OR “French Guiana”[All Fields] OR “East Timor”[All Fields] OR “laos”[MeSH Terms] OR (“laos”[MeSH Terms] OR “laos”[All Fields]) OR “North Korea”[All Fields] OR “Ivory Coast”[All Fields] OR “Republic of Georgia”[All Fields] OR “Republic of Yemen”[All Fields] OR “Republic of Zaire”[All Fields] OR “slovakia”[MeSH Terms] OR (“slovakia”[MeSH Terms] OR “slovakia”[All Fields]) OR “Soviet Union”[All Fields] OR “suriname”[MeSH Terms] OR (“suriname”[MeSH Terms] OR “suriname”[All Fields] OR “surinam”[All Fields]) OR “ussr”[MeSH Terms] OR (“ussr”[MeSH Terms] OR “ussr”[All Fields]) OR “samoa”[MeSH Terms] OR (“samoa”[MeSH Terms] OR “samoa”[All Fields]) OR “yugoslavia”[MeSH Terms] OR (“yugoslavia”[MeSH Terms] OR “yugoslavia”[All Fields]) OR “democratic republic of the congo”[MeSH Terms] OR (“democratic republic of the congo”[MeSH Terms] OR (“democratic”[All Fields] AND “republic”[All Fields] AND “congo”[All Fields]) OR “democratic republic of the congo”[All Fields] OR “zaire”[All Fields]) OR “asia”[MeSH Terms] OR (“asia”[MeSH Terms] OR “asia”[All Fields]) OR “West Indies”[All Fields] OR “polynesia”[MeSH Terms] OR (“polynesia”[MeSH Terms] OR “polynesia”[All Fields]) OR “micronesia”[MeSH Terms] OR (“micronesia”[MeSH Terms] OR “micronesia”[All Fields]) OR “Middle East”[All Fields] OR “africa”[MeSH Terms] OR (“africa”[MeSH Terms] OR “africa”[All Fields]) OR “Latin America”[All Fields] OR “Central America”[All Fields] OR “South America”[All Fields] OR (“west indies”[MeSH Terms] OR (“west”[All Fields] AND “indies”[All Fields]) OR “west indies”[All Fields]) OR “west indies”[MeSH Terms] OR “caribbean region”[MeSH Terms] OR (“west indies”[MeSH Terms] OR (“west”[All Fields] AND “indies”[All Fields]) OR “west indies”[All Fields] OR “caribbean”[All Fields] OR “caribbean region”[MeSH Terms] OR (“caribbean”[All Fields] AND “region”[All Fields]) OR “caribbean region”[All Fields]) OR “caribbean region”[MeSH Terms] OR Hispanola[All Fields] OR “Southeast Asia”[All Fields] OR “Sub-Saharan Africa”[All Fields] OR “Eastern Europe”[All Fields] OR Balkans[All Fields]) NOT (“new mexico”[MeSH Terms]) OR “new mexico”[All Fields] “Developing Countries”[MeSH Terms] OR “Developing Country” [All Fields] OR “Developing Countries” [All Fields] OR “Low Resource Setting” [All Fields] OR “Low Resource Settings” [All Fields])
Authors' contributions
Study conception and design: HKHW, AAH, KJH Acquisition of data: HKHW, NB, KJH Analysis and interpretation of data: HKHW, NB, MB, KJH Drafting of manuscript: HKHW Critical revision: KJH, AAH.
Conflict of interest and funding
The study was funded by the Bill & Melinda Gates Foundation, Seattle, USA, and by the Fogarty International Center at NIH. The study was undertaken under the auspices of PRICELESS SA (Priority Cost Effective Lessons for Systems Strengthening – South Africa) www.pricelesssa.ac.za.
Paper context
Context-specific information on the cost-effectiveness of RTI prevention strategies in South Africa is essential for road safety advocacy. The current published literature describing the costs of RTIs in South Africa do not define the full scope of the costs incurred, and there are no cost-effectiveness analyses on interventions apart from seatbelt use. Surveillance systems should consider introducing data on costs, especially societal costs. This information can be used to better inform choices and trade-offs between competing spending priorities.
References
- 1.Krug E. Decade of Action for Road Safety 2011–2020. Injury. 2012;43:6–7. doi: 10.1016/j.injury.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Geneva, Switzerland: World Health Organization; 2009. Global status report on road safety: time for action. [Google Scholar]
- 3.Letsoalo CP. Pretoria, South Africa: Road Traffic Management Corporation; 2012. State of the road safety report. [Google Scholar]
- 4.Road Traffic Management Corporation. Johannesburg, South Africa: Road Traffic Management Corporation; 2009. Road Traffic report for the calendar year 2009. [Google Scholar]
- 5.South Africa Medical Research Council. The National Injury Mortality Surveillance System. Available from: https://www.mrc.ac.za/crime/nimss.htn [cited 15 January 2016]
- 6.Statistics South Africa. Pretoria, South Africa: Statistics South Africa; 2009. Road traffic accident deaths in South Africa, 2001–2006: evidence from death notification. [Google Scholar]
- 7.Sukai A, Seedat M, Jordaan E, Jackson D. A city-level study of aggressive road behaviors: magnitude, predictors, and implications for traffic safety. S Afr J Psychol. 2005;35:244–69. [Google Scholar]
- 8.Van Hoving DJ, Sinclair M, Wallis LA. Patterns of seatbelt use in different socioeconomic communities in the Cape Town Metropole, South Africa. S Afr Med J. 2013;103:628–31. doi: 10.7196/samj.7126. [DOI] [PubMed] [Google Scholar]
- 9.Department of Transport. Pretoria, South Africa: Department of Transport; 2008. National Road Traffic Act, 1996 (Act No. 93 of 1996) Amendement of the national road traffic regulations. [Google Scholar]
- 10. Wallis LA. Trauma care in South Africa – a call to arms. S Afr Med J. 2011;101:171. doi: 10.7196/samj.4802. [DOI] [PubMed] [Google Scholar]
- 11.Pretoria, South Africa: Republic of South Africa; Republic of South Africa National Treasury (2012). Budget review 2012. [Google Scholar]
- 12.Schutte IC. Pretoria, South Africa: Republic of South Africa; 2000. An estimate of the unit cost of road traffic collisions in South Africa for 1998. Report No. CR-2000/4. [Google Scholar]
- 13.de Beer EJH, van Niekerk EC, Vermaak L. Pretoria, South Africa: CTDFID; 2002. Updating crash costing methodology in developing countries: pilot study in South Africa. Report No. CR-2001. [Google Scholar]
- 14.de Beer EJH, van Niekerk EC. Pretoria, South Africa: National Department of Transportation; 2004. The estimation of unit costs of road traffic accidents in South Africa. Report No. CR-2004/6. [Google Scholar]
- 15.Olukoga A. Cost analysis of road traffic crashes in South Africa. Inj Control Saf Promot. 2004;11:59–62. doi: 10.1076/icsp.11.1.59.26304. [DOI] [PubMed] [Google Scholar]
- 16.Truen S, Ramkolowan Y, Corrigall J, Matzopoulos R. Pretoria, South Africa: Department of Trade and Industry; 2011. Baseline study of the liquor industry including the impact of the National Liquor Act 59 of 2003. [Google Scholar]
- 17.Harris GT, Olukoga IA. A cost benefit analysis of an enhanced seat belt enforcement program in South Africa. Inj Prev. 2005;11:102–5. doi: 10.1136/ip.2004.007179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Drummond MF, Sculpher MJ, Torrance GW, O'Brien BJ, Stoddart JL. Oxford: Oxford University Press; 2005. Methods for the economic evaluation of health care programmes. [Google Scholar]
- 19.Rutstein SE, Price JT, Rosenberg NE, Rennie SM, Biddle AK, Miller WC. Hidden costs: the ethics of cost-effectiveness analyses for health interventions in resource-limited settings. Global Public Health. 2016:1–13 [Epub ahead of print]. doi: 10.1080/17441692.2016.1178319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. PubMed. Available from: http://www.ncbi.nlm.nih.gov/pubmed [cited 21 January 2016]
- 21.Embase. Elsevier Inc. Available from: http://www.embase.com/ [cited 25 January 2016]
- 22.The Cochrane Library. Available from: http://www.cochrane.org [cited 23 January 2016]
- 23.EconLit. Available from: https://www.aeaweb.org/econlit/ [cited 25 January 2016]
- 24.Econbase. Eldis. Available from: http://www.eldis.org/go/home&id=1648&type=Organisation [cited 25 January 2016]
- 25.National Health Service Economic Evaluation Database. Elsevier, Inc. Available from: http://www.elsevier.com/homepage/sae/econworld/menu [cited 26 January 2016]
- 26.Littell JH, Corcoran J, Pillai VK. New York: Oxford University Press; 2008. Systematic reviews and meta-analysis. [Google Scholar]
- 27.Rice DP. Cost of illness studies: what is good about them? Inj Prev. 2000;6:177–9. doi: 10.1136/ip.6.3.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hendrie D, Miller TR. Assessing the burden of injuries: competing measures. Inj Contr Saf Promot. 2004;11:193–9. doi: 10.1080/156609704/233/289689. [DOI] [PubMed] [Google Scholar]
- 29.Kobelt G. 2nd ed. London: Office of Health Economics; 2002. Health economics: an introduction to economic evaluation. [Google Scholar]
- 30.Bishai DM, Hyder AA. Modeling the cost effectiveness of injury interventions in lower and middle income countries: opportunities and challenges. Cost Eff Resour Alloc. 2006;4:2. doi: 10.1186/1478-7547-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.al-Masaeid HR, al-Mashakbeh AA, Qudah AM. Economic costs of traffic accidents in Jordan. Accid Anal Prev. 1999;31:347–57. doi: 10.1016/s0001-4575(98)00068-2. [DOI] [PubMed] [Google Scholar]
- 32.Hijar M, Arredondo A, Carrillo C, Solorzano L. Road traffic injuries in an urban area in Mexico. An epidemiological and cost analysis. Accid Anal Prev. 2004;36:37–42. doi: 10.1016/s0001-4575(02)00112-4. [DOI] [PubMed] [Google Scholar]
- 33.Anh TT, Anh TT, Doa NX. The cost of road traffic accident in Vietnam. Proc Eastern Asia Soc Transp Stud. 2005;5:1923–33. [Google Scholar]
- 34.Riewpaiboon A, Piyauthakit P, Chaikledkaew U. Economic burden of road traffic injuries: a micro-costing approach. Southeast Asian J Trop Med Public Health. 2008;39:1139–49. [PubMed] [Google Scholar]
- 35.Riewpaiboon A, Piyauthakit P, Srijariya W, Chaikledkaew U. A drug cost model for injuries due to road traffic accidents. Pharm Pract. 2008;6:9–14. doi: 10.4321/s1886-36552008000100002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li YH, Rahim Y, De-Ding Z. A study on bicycle-related injuries and their costs in Shanghai, China. J Environ Health. 2011;73:22–8. [PubMed] [Google Scholar]
- 37.Parkinson F, Kent SJ, Aldous C, Oosthuizen G, Clarke D. The hospital cost of road traffic accidents at a South African Regional Trauma Centre: a micro-costing study. Injury. 2014;45:342–5. doi: 10.1016/j.injury.2013.04.007. [DOI] [PubMed] [Google Scholar]
- 38.Bishai D, Hyder AA, Ghaffar A, Morrow RH, Kobusingye O. Rates of public investment for road safety in developing countries: case studies of Uganda and Pakistan. Health Policy Plan. 2003;18:232–5. doi: 10.1093/heapol/czg028. [DOI] [PubMed] [Google Scholar]
- 39.Hendrie D, Miller TR, Orlando M, Spicer RS, Taft C, Consunji R, et al. Child and family safety device affordability by country income level: an 18 country comparison. Inj Prev. 2004;10:338–43. doi: 10.1136/ip.2004.005652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pham KH, Le Thi QX, Petrie DJ, Adams J, Doran CM. Households’ willingness to pay for a motorcycle helmet in Hanoi, Vietnam. Appl Health Econ Health Policy. 2008;6:137–44. doi: 10.1007/BF03256128. [DOI] [PubMed] [Google Scholar]
- 41.Tsauo JY, Hwang JS, Chiu WT, Hung CC, Wang JD. Estimation of expected utility gained from the helmet law in Taiwan by quality-adjusted survival time. Accid Anal Prev. 1999;31:253–63. doi: 10.1016/s0001-4575(98)00078-5. [DOI] [PubMed] [Google Scholar]
- 42.Rosser R, Cottee M, Rabin R, Selai C. Index of health-related quality of Life. In: Hopkins A, editor. Measures of quality of life. London: Royal College of Physicians of London; 1992. pp. 81–89. [Google Scholar]
- 43.Hwang JS, Tsauo JY, Wang JD. Estimation of expected quality adjusted survival by cross-sectional survey. Stat Med. 1996;15:93–102. doi: 10.1002/(SICI)1097-0258(19960115)15:1<93::AID-SIM155>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 44.Li G, Baker SP. Injuries to bicyclists in Wuhan, People's Republic of China. Am J Public Health. 1997;87:1049–52. doi: 10.2105/ajph.87.6.1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang J, Norton R, Tang KC, Lo SK, Jiatong Z, Wenkui G. Motorcycle ownership and injury in China. Inj Control Saf Promot. 2004;11:159–63. doi: 10.1080/156609704/233/289643. [DOI] [PubMed] [Google Scholar]
- 46.Ichikawa M, Chadbunchachai W, Marui E. Effect of the helmet act for motorcyclists in Thailand. Accid Anal Prev. 2003;35:183–9. doi: 10.1016/s0001-4575(01)00102-6. [DOI] [PubMed] [Google Scholar]
- 47.Poli de Figueiredo LF, Rasslan S, Bruscagin V, Cruz R, Rocha e Silva M. Increases in fines and driver licence withdrawal have effectively reduced immediate deaths from trauma on Brazilian roads: first-year report on the new traffic code. Injury. 2001;32:91–4. doi: 10.1016/s0020-1383(00)00172-8. [DOI] [PubMed] [Google Scholar]
- 48.Afukaar FK, Antwi P, Ofosu-Amaah S. Pattern of road traffic injuries in Ghana: implications for control. Inj Contr Saf Promot. 2003;10:69–76. doi: 10.1076/icsp.10.1.69.14107. [DOI] [PubMed] [Google Scholar]
- 49.Bishai D, Asiimwe B, Abbas S, Hyder AA, Bazeyo W. Cost-effectiveness of traffic enforcement: case study from Uganda. Inj Prev. 2008;14:223–7. doi: 10.1136/ip.2008.018341. [DOI] [PubMed] [Google Scholar]
- 50.Chisholm D, Naci H. Geneva, Switzerland: World Health Organization; 2008. Road Traffic Injury prevention: an assessment of risk exposure and intervention cost-effectiveness in different world regions. [Google Scholar]
- 51.Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, et al. 2nd ed. Washington, DC: The World Bank; 2006. Disease control priorities in developing countries. [PubMed] [Google Scholar]
- 52.Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. Value Health. 2013;16:e1–5. doi: 10.1016/j.jval.2013.02.010. [DOI] [PubMed] [Google Scholar]
- 53.Chisholm D, Naci H, Hyder AA, Tran NT, Peden M. Cost effectiveness of strategies to combat road traffic injuries in sub-Saharan Africa and South East Asia: mathematical modelling study. BMJ. 2012;344:e612. doi: 10.1136/bmj.e612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Garrib A, Herbst AJ, Hosegood V, Newell ML. Injury mortality in rural South Africa 2000–2007: rates and associated factors. Trop Med Int Health. 2011;16:439–46. doi: 10.1111/j.1365-3156.2011.02730.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Matzopoulos R, Myers JE, Jobanputra R. Road traffic injury: prioritising interventions. S Afr Med J. 2008;98:692–6. [PubMed] [Google Scholar]
- 56.World Health Organization. Geneva, Switzerland: World Health Organization; 2011. Global plan for the Decade of Action for Road Safety 2011–2020. [Google Scholar]
- 57.Waters HR, Hyder AA, Phillips TL. Economic evaluation of interventions to reduce road traffic injuries – a review of the literature with applications to low and middle-income countries. Asia Pac J Public Health. 2004;16:23–31. doi: 10.1177/101053950401600105. [DOI] [PubMed] [Google Scholar]
- 58.Dinh-Zarr TB, Sleet DA, Shults RA, Zaza S, Elder RW, Nichols JL, et al. Reviews of evidence regarding interventions to increase the use of safety belts. Am J Prev Med. 2001;21(4 Suppl):48–65. doi: 10.1016/s0749-3797(01)00378-6. [DOI] [PubMed] [Google Scholar]
- 59.Nilsen P, Hudson D, Lindqvist K. Economic analysis of injury prevention – applying results and methodologies from cost-of-injury studies. Int J Inj Contr Saf Promot. 2006;13:7–13. doi: 10.1080/17457300500167651. [DOI] [PubMed] [Google Scholar]
- 60.Gyllensvard H. Cost-effectiveness of injury prevention – a systematic review of municipality based interventions. Cost Eff Resour Alloc. 2010;8:17. doi: 10.1186/1478-7547-8-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Commission on Social Determinants of Health. Geneva, Switzerland: World Health Organization; 2008. Closing the gap in a generation: health equity through action on the social determinants of health. [DOI] [PubMed] [Google Scholar]
- 62.National Planning Commission. Pretoria, South Africa: National Planning Commission; 2010. National Planning Commission diagnostic overview. [Google Scholar]