Abstract
Objective
This study examined the direct and the buffering effects of social support on longer-term global psychological distress among parents coping with pediatric cancer. In both sets of analyses we examined whether these effects depended on the dimension of social support provided (i.e., satisfaction with support versus size of support network).
Method
Participants were 102 parents of pediatric cancer patients. At study entry, parents reported their trait anxiety, depression, and two dimensions of their social support network (satisfaction with support and size of support network). Parents subsequently reported their psychological distress in 3- and 9-month follow-up assessments.
Results
Parents’ satisfaction with support had a direct effect on longer-term psychological distress; satisfaction was negatively associated with distress at both follow-ups. In contrast, size of support network buffered (moderated) the impact of trait anxiety and depression on later distress. Parents with smaller support networks and higher levels of trait anxiety and depression at baseline had higher levels of psychological distress at both follow-ups; for parents with larger support networks, there was no relationship.
Conclusion
Social support can attenuate psychological distress in parents coping with pediatric cancer; however, the nature of the effect depends on the dimension of support. Whereas, interventions that focus on increasing satisfaction with social support may benefit all parents, at-risk parents will likely benefit from interventions that ensure they have an adequate number of support resources.
Keywords: parents, pediatric, cancer, oncology, social support, psychological distress
Background
According to the American Cancer Society, an estimated 10,450 children under the age of 15 will be diagnosed with cancer in the United States in 2014 [1]. Fortunately the treatment of pediatric cancer is often successful, and deaths from pediatric cancer are declining [1]. However, coping with the diagnosis and treatment of pediatric cancer can have profound negative psychosocial effects on children and their parents over time (for reviews, see [2, 3]). In this study, we focus on the longer-term1 psychological distress of parents of pediatric cancer patients.
Frequent treatments, hospital stays, side effects, and the fear of relapse can all contribute to psychological distress for parents [4]. After a diagnosis of pediatric cancer, many parents report symptoms of distress including anger, anxiety, depression, and PTSD [4-6]. These symptoms of distress can persist up to five years post-diagnosis [7, 8]. However, there is variability in parents’ level of psychological distress such that not all parents experience the same negative psychological effects over time [9]. According to human ecology theories (e.g., Bronfenbrenner [10]), people's environment or social context at the time of life stressors plays an important role in their response to these stressors. This broad theory suggests that environmental or social resources may mitigate the psychological distress associated with the experience of having a child with cancer for some parents. This study provides empirical evidence that supports this prediction.
Social support is one environmental factor that has the potential to reduce parents’ psychological distress. Social support is the verbal and nonverbal communication that helps manage uncertainty about a situation, the self, others, or an interpersonal relationship and provides benefit by enhancing perceptions of personal control [11]. Extensive research supports the positive impact of social support in reducing stress, facilitating positive coping, and improving health and medical outcomes [12].
According to Cohen and Wills [13], social support can have psychological benefits in two ways. First, support can provide direct protective effects such that higher levels of social support offset the negative impact of stressful events for all people. Second, social support may have an indirect (moderating) effect such that social support “buffers” or reduces the negative effects of stressful events primarily for people who are at risk for experiencing such stress [13-15]. There has been substantial support for both direct protective effects (e.g., [16, 17]) and buffering effects (e.g., [18-20]) of social support. To understand which effect is more likely to occur in a given context, it is important to consider the nature of social support provided. Sarason and colleagues [21] and others (e.g., [13]) argue there are two related but distinct dimensions to social support. The first is the extent to which a person feels satisfied with the social support provided; the second is the size of one's network or the number of people the person believes is available to provide support. Cohen and Wills [13] proposed that the effects of social support (i.e., direct versus buffering) may depend on whether one is considering satisfaction with or size of a person's social support network.
Social support may be particularly relevant for parents of pediatric cancer patients. Parents of children not only experience secondary stress (i.e., caring for their children), but also parents of pediatric patients experience greater stress than parents of healthy children [22, 23] and parents of children with other childhood medical challenges (e.g., [24]). Previous research also shows social support to be a valuable and beneficial resource for these parents (e.g., [2, 25, 26]. Higher levels of social support have been associated with more positive outcomes in parents (including more resilience and less anxiety, fewer symptoms of PTSD, and less psychological distress [22, 23, 25, 27-29]). Some research has also shown that the amount of support was a key factor. For example, in studies of the families of long-term cancer survivors, Kazak et al. [23] and Barakat et al. [22] found the size of social support networks of parent(s) was negatively associated with symptoms of psychological distress (e.g., anxiety, worry, traumatic stress). However, there is little clarity in these studies about whether the effects of social support are direct or involve buffering. A literature search located only one study of parents of pediatric cancer patients that directly tested the buffering effects of social support. Rini et al. [30] examined whether social support from friends/family moderated the impact of low spousal support in mothers of children undergoing hematopoietic stem cell transplantation. Results showed that mothers with low spousal support and high friend/family support had better psychological functioning, which provides support for the buffering effects of social support. However, neither Rini et al. nor any other study we could find examined the nuances of both dimensions of social support proposed by Sarason et al. (i.e., satisfaction with social support versus size of network) and whether they might differentially influence the effect of social support (direct versus buffering) on distress in parents of pediatric cancer patients.
The present study extends prior research on the benefits of social support during stressful events, in general and specifically, among parents of cancer patients in several ways. First, as already noted, no one has systematically examined both direct and buffering effects of social support on longer-term psychological distress among parents coping with pediatric cancer. In the present study, we examined both effects. Second, we examined whether parents’ negative affect and levels of social support early in treatment interacted to influence their subsequent longer-term global psychological distress. This provided a means to specifically test the buffering hypothesis. Third, in contrast to most prior studies, we separately examined the impact of satisfaction with social support and size of social support networks among parents. As noted [13, 21], these two dimensions of social support are thought to function independently from each other, and therefore it is critical to understand which dimension of support might provide the most benefit to the parents. Cohen and Wills [13] specifically proposed that satisfaction is typically associated with direct effects of social support, while size of network is associated with the buffering effects of social support (i.e., higher satisfaction versus more sources). In this study, we directly tested this proposal.
The study had two research aims. The first aim was to investigate the direct effects of social support on parents’ distress. We examined: (a) whether parents with higher levels of social support experience lower levels of longer-term global psychological distress, and (b) whether this relationship was true for both satisfaction with support and size of support networks. The second aim was to investigate the buffering (or indirect) effects of each dimension of social support. We separately examined satisfaction with support and size of support network as moderators of the relationship between parents’ negative affect and longer-term distress.
Method
Overview
The present study is part of a larger, on-going longitudinal parent study that began in 2009 at two children's hospitals in the United States. The study protocol was reviewed and approved by Institutional Review Boards at both study sites. The primary aim of the parent study is to identify personal, interpersonal, and environmental factors that mitigate the psychosocial impact of pediatric cancer and, specifically, cancer-related treatment procedures on the families of pediatric cancer patients. There are three phases of data collection: (1) baseline assessment – adult primary caregivers (“parents”) complete questionnaires about themselves and their children at study entry; (2) treatment assessments – at the time of children's treatment-related procedures (port starts, bone marrow aspirations, or lumbar punctures), parents’ self-report their cognition and affect; ratings of child distress and cooperation during procedures are made by parents, nurses, children, and independent observers of the treatment procedures. Data from the treatment assessments are not presented in this study; (3) first follow-up assessment – approximately three months after the last treatment assessment, parents complete a set of questionnaires about themselves and their children; (4) second follow-up assessment – approximately 9 months after the last treatment assessment, parents complete a second set of questionnaires about themselves and their children.
Recruitment Procedures
Families were eligible if (a) the child was between 3 and 12 years old; (b) parent and child were able to speak and the parent could read English; (c) the child had been diagnosed with cancer within the last 18 months and was receiving port starts, lumbar punctures, and/or bone marrow aspirations as part of treatment, and (d) for the present study, parents had completed the baseline and first and second follow-up assessments. Following HIPAA guidelines, clinical staff identified eligible children and initially approached families about their interest in the study. Research staff met with interested parents and obtained informed consent, and when appropriate, verbal assent from children. Parents received $15 gift cards for the initial assessment and each video-recorded treatment procedure and $20 gift cards for each of the follow-ups. Children received $10 gift cards for each of these data collection points. Approximately 87% of parents and children approached agreed to participate.
Participants
The current study sample consisted of 102 parents of children with pediatric cancer. Parent and child demographic characteristics are shown in Table 1. The majority of children were diagnosed with Acute Lymphoblastic Leukemia (83.3%), followed by Wilm's Tumors (4.9%), Non-Hodgkin's Lymphoma (2%), other lymphomas (2%), astrocytoma (2%), and other cancers (e.g., Ewing's sarcoma, osteosarcoma, unspecified; 5.8%). At study entry, all children had started cancer treatment (mean time in treatment=3.42 months, SD=3.42; median=2.23). Parents completed the baseline assessment at study entry.
Table 1.
Parent and Child Demographics and Clinical Characteristics (N=102 families)
| Parents | Children | |
|---|---|---|
| Age: mean (SD) | 34.71 (7.19) | 6.44 (3.13) |
| Gender (%) | ||
| Female | 85 (83%) | 43 (42%) |
| Male | 17 (17%) | 59 (58%) |
| Ethnicity (%) | ||
| Caucasian | 74 (72%) | 73 (71%) |
| African American | 18 (18%) | 18 (18%) |
| Bi-racial | 0 | 5 (5%) |
| Hispanic/Latino | 7 (7%) | 5 (5%) |
| American Indian/Alaska | 2 (2%) | 0 |
| Other | 1 (1%) | 1 (1%) |
| Household income | ||
| <$20,000 | 33% | |
| $20,000-$59,999 | 24% | |
| $60,000-$100,000 | 32% | |
| >$100,000 | 11% | |
| Employment status | ||
| Unemployed | 57% | |
| Part-time | 17% | |
| Full-time | 26% | |
| Education | ||
| Less than high school diploma | 13% | |
| High school diploma | 20% | |
| Some college | 41% | |
| College degree or higher | 26% | |
At the first follow-up assessment, average amount of time in treatment (i.e., prior treatment plus treatment during study) was 10.01 months (SD=3.99); average time from the baseline assessment was 6.57 months (SD=1.93; range=3.65-13.17). At the second follow-up assessment, average amount of time children had been in treatment was 17.00 months (SD=4.42); average time from the baseline assessment was 13.49 months (SD=2.47; range=10.02-21.65).
Study Assessments
Baseline Assessment
The baseline assessment consisted of questions about parent and child demographic and children's medical history (e.g., time in treatment, type of cancer, procedures experienced), environmental resources, and personal attributes. The focus of the present study is on measures of social support and negative affect.
Social Support
The Brief Measure of Social Support (SSQ; [31]) was used to assess social support in six areas (e.g., providing dependable help, showing concern). For each area, parents reported the number of people who provide this type of support to them and then used a six-point Likert scale (1=very disappointed to 6=very satisfied) to rate their satisfaction with each type of support (mean satisfaction=5.45, SD=0.82). The number of people who provided social support to parents ranged from 0 to 9 (mean=4.00, SD=2.32). Following Sarason et al, responses were combined across the six areas separately for satisfaction and size of network (i.e., number) to yield total scores for each dimension of social support. In the present study, coefficient alphas for satisfaction with support and size of network were .91 and .95, respectively. Satisfaction with support and size of network were positively correlated (r=.37; p<.01). Previous research shows that the SSQ correlates well with other measures of social support and predicts adjustment to negative life experiences [31].
Negative Affect
The 20-item trait anxiety subscale of the State Trait Anxiety Inventory for Adults [32] is used to assess anxiety as an stable personal attribute. Extensive research supports the measure's construct validity [33]. Items are rated on a four-point Likert scale (1=almost never to 4=almost always) and summed to create a total trait anxiety score (mean=37.64, SD=9.46). The 20-item Center for Epidemiologic Studies – Depression Scale [34], a widely used and validated measure of depressive symptoms, was used to assess parent depression. Items were rated on a four-point Likert scale (0=rarely/none of the time to 3=most/all of the time) and summed to create a total depression score (mean=15.48, SD=10.02). Coefficient alphas for the two scales were .89 and .88, respectively.
Follow-Up Assessments
At each of the two follow-up assessments, parents completed the Brief Symptom Inventory-18 (BSI-18; [35]), which contains subscales for psychiatric symptoms of anxiety, depression, and somatization (i.e., physical symptoms with no identifiable physical cause); these subscales are typically combined into a single measure of global psychological distress and transformed into T scores (mean=49.77; SD=9.40, range=39.54-81.63). Prior research supports the scale's construct and convergent validity (e.g., [36, 37]). Coefficient alphas in this study were >.85 for each of the three subscales at both follow-up assessments. Coefficient alphas for the global (i.e., total) psychological distress scores were .93 for the first follow-up and .94 for the second follow-up.
Data Preparation and Analysis
Values for sporadic missing data (<1% of all items) were imputed using substitution of sample mean. Data were inspected for outliers; none were identified. Statistical analyses were done using the IBM Statistical Package for the Social Sciences, Release 22.0. All variables were analyzed as continuous variables. Partial correlations were used address the direct effect of each dimension of social support on global distress (Aim 1). Hayes’ [38] PROCESS Model 1 SPSS macro was used to test whether either dimension of social support (satisfaction or size) moderated (i.e., buffered) the relationship between baseline trait anxiety and depression and global psychological distress (Aim 2). If a regression analysis showed a significant interaction involving either dimension of social support (i.e., satisfaction or size) and trait anxiety or depression, following standard procedures (see [38], pp. 234-239) we then compared the slopes of the relationships between anxiety/depression and global distress for parents (using ±1 standard deviation from the sample mean on the social support measure).
The results for the three BSI symptom subscales (i.e., anxiety, depression, somatization) closely paralleled the global distress scores. Therefore, in the interest of brevity, we only report outcomes for the global distress scores in the analyses below. Further, parents’ global distress at the first and second follow-up assessments was highly correlated (r=.78, p<.001), and the results for each outcome were essentially identical. Therefore, we only report outcomes of analyses for the second follow-up assessment.2
Results
Parent Gender Differences
We found no differences between female and male parents with respect to their own or their child's demographic or child medical characteristics, amount of time spent with the child during procedures, or on any of the assessments (ps>.05). As there were no significant gender differences, and there were only 17 fathers in the sample, male and female parents were included in the same analyses.
Direct Effects of Social Support (Aim 1)
The first aim examined whether the two different dimensions of social support (i.e., satisfaction with support and size of support network) directly influenced parents’ longer-term global psychological distress. Prior to addressing this question, we conducted a preliminary analysis to examine the correlations between parents’ baseline trait anxiety and depression and satisfaction with social support and size of support network. Three of the four correlations were significant: satisfaction with social support: ranx=−.36 and rdep=−.37, ps<.001; size of social support network: ranx=−.12, p>.05 and rdep=−.26, p<.01). Thus, we conducted partial correlations that controlled for parents’ baseline trait anxiety and depression in analyzing the direct effects of social support on global psychological distress.
Partial correlations showed that parents’ satisfaction with social support had a direct negative effect on global distress at follow-up (r=−.33, p<.01). In contrast, size of parents’ social support network was not significantly correlated with global distress at follow-up (p>.05). Thus, results showed that, after controlling for baseline anxiety and depression, only satisfaction with support had a direct effect on parents’ longer-term global distress.
Buffering Effects of Social Support (Aim 2)
The second aim examined the buffering effects of each dimension of social support (i.e., satisfaction and size) on the relationship between parents’ baseline negative affect and subsequent global distress. Prior to addressing this question, we conducted a preliminary analysis of the correlations between parents’ baseline negative affect and their longer-term global psychological distress. We found that baseline trait anxiety and depression were both positively and significantly correlated with global psychological distress at follow-up (ranx=.52 and rdep=.60, ps<.001).
To examine the buffering effects of social support, satisfaction with support and size of network were independently tested as moderators in two regression models (i.e., anxiety predicting global distress at follow-up and depression predicting global distress at follow-up). There were no significant interactions when satisfaction with social support was the moderator variable in the model (ps>.05). However, we did find significant interactions when size of support network was included as the moderator. These effects are discussed below.
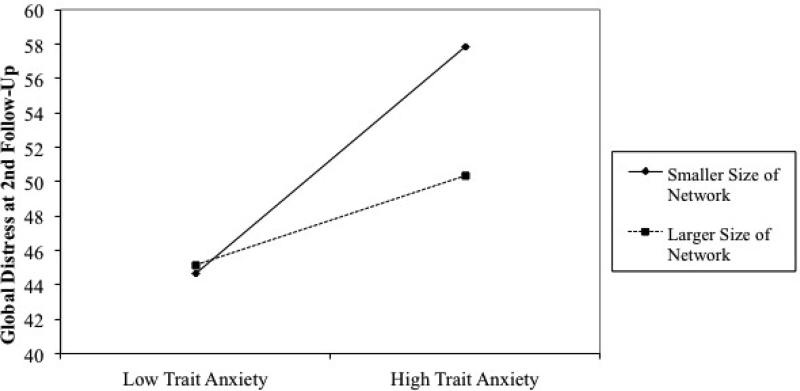
There was a significant main effect for trait anxiety; higher levels of trait anxiety were associated with higher levels of global distress (t=4.96, p<.001). However, there was also a significant interaction (binter=−.09, se=.04; ΔR2=.04, F(1,97)=5.60, p<.05), indicating that the slopes differed significantly from each other. Figure 1 shows the regression slopes for parents 1 SD above and 1 SD below the sample mean for size of support network. Both slopes are significant and positive: parents with smaller support networks (1 SD below the mean) (conditional effect=.70, se=.12, t=5.88, p<.001) and parents with larger support networks (1 SD above the mean) (conditional effect=.27, se=.13, t=2.15, p<.05). However, as shown by the relative size of the conditional effects, the relationship between parents’ baseline anxiety and global distress at follow-up was significantly stronger for parents with smaller support networks.
Figure 1.
Buffering Effects of Size of Social Support Network on the Relationship between Parent Trait Anxiety and Global Distress at Second Follow-Up
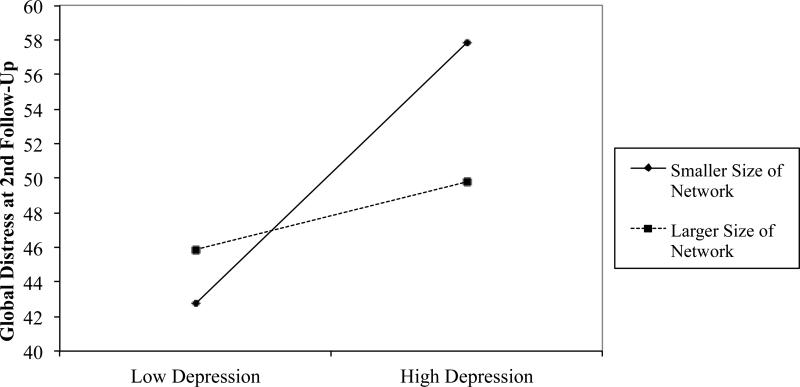
There was a significant main effect for depression; higher levels of depressive symptoms were associated with higher levels of global distress (t=6.61, p<.001). However, there was also a significant interaction (binter=−.12, se=.04; ΔR2=.07, F(1,97)=10.95, p<.01), again indicating the slopes differed significantly from each other. Figure 2 shows the regression slopes for parents 1 SD above and 1 SD below the sample mean for size of support network. Among parents with smaller support networks (1 SD below the mean), depression at baseline was significantly and positively associated with global distress at follow-up (conditional effect=.76, se=.10, t=7.76, p<.001). Among parents with larger support networks (1 SD above the mean), there was no significant relationship between baseline depressive and global distress at follow-up (conditional effect=.20, se=.13, t=1.50, p>.05).
Figure 2.
Buffering Effects of Size of Social Support Network on the Relationship between Parent Depression and Global Distress at Second Follow-Up
Conclusions
The underlying assumption of the present study (and other research we have conducted) is that pediatric cancer is a psychosocial stressor for children and their parents. In previous work, we have found that some intrapersonal resources mitigate the psychosocial impact of the experience of pediatric cancer (e.g., [5]). The present study examines the impact of environmental factors – specifically, social support – on parents’ psychological distress. While previous research generally concludes that social support is a valuable resource for parents of children with cancer [2, 25, 26], it has not identified the paths (i.e., indirect versus direct) through which social support might mitigate distress. Previous research has also not considered whether there are nuanced effects of social support such that satisfaction with support and size of support networks have distinct effects on parents’ psychological distress. Thus, the present study examined the direct and indirect effects of both satisfaction with support and size of support network. Understanding the mechanisms by which social support influences distress has the potential to increase the effectiveness and benefits of social support interventions designed to decrease parent distress associated with pediatric cancer (e.g., [26]. Our study yielded several potentially important findings that might benefit these interventions.
Consistent with theories of social support [13, 21], we found that satisfaction with support and size of support network have different pathways of influence for parents of children with cancer. Parents’ satisfaction with support showed a direct relationship with parents’ global distress up to almost 18 months later. That is, all parents seemed to benefit from having support with which they were satisfied. In contrast, the size of parents’ network was unrelated to their longer-term distress. That is, simply having more sources of support did not significantly reduce longer-term distress for parents. The experience of pediatric cancer can create financial, practical, and emotional burden for families [2, 3, 39, 40], and as such, it is possible that having larger networks and more sources of support is not as important for parents as is knowing they can count on a few key support resources when they most need them (e.g., picking up other children, being available to listen, cutting the grass).
In contrast, whereas satisfaction with support provided direct but not buffering benefits, we found substantial evidence of buffering effects for size of network. The size of parents’ support network moderated the relationship between trait anxiety and depression at baseline and longer-term global psychological distress. In other words, more anxious and/or depressed parents with larger social networks experienced substantially less longer-term global distress than did more anxious and/or depressed parents with smaller social networks. One possible explanation for the buffering effects of network size is that parents who are predisposed to negative affect may feel easily overwhelmed by the numerous challenges of their child's cancer. As such, the belief that they have many sources of support to help (e.g., if my sister can't help me, my friend or next-door neighbor or co-worker can) may reduce their level of distress.
Obviously, these explanations about the underlying mechanisms of social support are speculative and require further testing. Nevertheless, our findings strongly support the conclusion that satisfaction with social support and size of support network differentially affect the longer-term psychological distress experienced by parents of pediatric cancer patients.
In summary, social support reduces global psychological distress among parents of pediatric cancer patients, but these effects are more nuanced than suggested by the prior literature [25-28, 30]. Whereas satisfaction with social support appears to directly benefit for all parents, the size of support networks appears to have primary benefit for parents with higher levels of negative affect. Parents with more trait anxiety and depression are more likely to experience global distress over time than parents with lower trait anxiety and/or depression unless they perceive having relatively more sources of support (i.e., larger social support networks).
Limitations
Although these results represent important findings about the different pathways through which social support benefits parents of pediatric cancer patients, the study is not without limitations. First, social support was assessed only at study entry. This information allows us to examine the longer-term effects of parents’ satisfaction with support and size of support network early in their child's cancer experience. However, previous research has shown that social support diminishes over time during a child's time in treatment [28, 41]. Thus, it is possible that changes in satisfaction with support or number of support sources over time could also impact the course of parents’ distress. Future research studying changes in support over time might shed light on the dynamic effect of social support on parents’ psychological adjustment during their child's cancer treatment. Second, parents provided self-reports of their negative affect, social support, and global distress, thus introducing possible bias due to common method variance [42]. At the same time, we are interested in parents’ “lived” experience, and therefore, self-reports are a suitable method of capturing parents’ perceived distress. Third, although the sample's demographic (e.g., child gender and race, mothers as primary parent) and medical characteristics (e.g., diagnosis of ALL) are fairly typical of children with pediatric cancer, the sample size and distribution of such characteristics did not permit us to consider whether factors such as gender/race, sex of the parent, or diagnosis might moderate the nature of the relationships between social support and distress. Future studies would likely benefit from examining the effects of social support in more heterogeneous and diverse samples.
Implications
With these limitations in mind, the results have important clinical implications. First, satisfaction with social support seems to have a uniform direct benefit for parents of pediatric cancer patients regardless of initial levels of negative affect. Thus, interventions that focusing on increasing parents’ satisfaction with support early in treatment can be effective for all parents. Second, it is possible to identify and intervene with parents who may be most at risk for longer-term psychological difficulties. Specifically, those parents who report higher levels of trait anxiety and/or depression and limited sources of social support early in their child's treatment may derive added benefit from interventions to ensure they have a multitude of support resources. These interventions could help parents identify sources of support to increase the size of networks as well as potentially build supportive connections with other parents in the same situation to reduce psychological distress over time.
In summary, the experience of pediatric cancer is a well-established psychosocial stressor for parents [2, 3], and social support can reduce distress in parents coping with pediatric cancer. However, the benefits of social support in reducing distress among parents caring for their children depend on the dimension of support. Identifying and providing services to those most in need of psychosocial intervention is a critical goal, especially for institutions with limited resources. Knowing which interventions provide the most benefit to which parents can maximize the efforts of medical staff and resources available within the clinic environment.
Acknowledgments
This work is part of a larger investigation of parents’ influence on child coping with cancer treatment and was supported by the National Cancer Institute at the National Institutes of Health (NCI#1R01CA138981; PI: L. Penner) and The Herrick Foundation (PI: L. Penner).
Footnotes
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
“Longer-term” refers to distress in the 1-2 years after the start of treatment and is used to differentiate from short-term distress at the time of diagnosis and long-term distress experienced by parents of survivors.
Results using the individual BSI subscales and the BSI global psychological distress score at the first follow-up assessment are available from the first author on request.
Portions of this research were presented at the 11th Annual Meeting of the American Psycho-Oncology Society, Tampa, FL.
References (references in red have been added)
- 1.American Cancer Society Cancer Facts & Figures Special Section: Cancer in Children and Adolescents. 2014 [Google Scholar]
- 2.Gibbins J, Steinhardt K, Beinart H. A Systematic Review of Qualitative Studies Exploring the Experience of Parents Whose Child Is Diagnosed and Treated for Cancer. Journal of Pediatric Oncology Nursing. 2012;29(5):253–271. doi: 10.1177/1043454212452791. [DOI] [PubMed] [Google Scholar]
- 3.Long KA, Marsland AL. Family adjustment to childhood cancer: A systematic review. Clinical child and family psychology review. 2011;14(1):57–88. doi: 10.1007/s10567-010-0082-z. [DOI] [PubMed] [Google Scholar]
- 4.Sloper P. Predictors of distress in parents of children with cancer: a prospective study. J Pediatr Psychol. 2000;25(2):79–91. doi: 10.1093/jpepsy/25.2.79. [DOI] [PubMed] [Google Scholar]
- 5.Harper FWK, et al. Longitudinal Study of Parent Caregiver Self-Efficacy and Parent Stress Reactions with Pediatric Cancer Treatment Procedures. Psycho-Oncology. 2012;22(7):593–613. doi: 10.1002/pon.3199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lindahl Norberg A, Boman KK. Parent distress in childhood cancer: A comparative evaluation of posttraumatic stress symptoms, depression and anxiety. Acta Oncologica. 2008;47(2):267–274. doi: 10.1080/02841860701558773. [DOI] [PubMed] [Google Scholar]
- 7.Vrijmoet-Wiersma CJ, et al. Assessment of parental psychological stress in pediatric cancer: A review. Journal of Pediatric Psychology. 2008;33(7):694–706. doi: 10.1093/jpepsy/jsn007. [DOI] [PubMed] [Google Scholar]
- 8.Norberg AL, Boman KK. Mothers and fathers of children with cancer: loss of control during treatment and posttraumatic stress at later follow-up. Psycho-Oncology. 2013;22(2):324–329. doi: 10.1002/pon.2091. [DOI] [PubMed] [Google Scholar]
- 9.Gudmundsdottir E, Schirren M, Boman KK. Psychological resilience and long-term distress in Swedish and Icelandic parents’ adjustment to childhood cancer. Acta Oncologica. 2010;50(3):373–380. doi: 10.3109/0284186X.2010.489572. [DOI] [PubMed] [Google Scholar]
- 10.Bronfenbrenner U. The ecology of human development:experiments by nature and design. Harvard University Press; 1979. [Google Scholar]
- 11.Albrecht TL, Adelman MB. Communicating social support. Sage Publications, Inc.; 1987. [Google Scholar]
- 12.Albrecht TL, Goldsmith DJ. Social support, social networks, and health. In: Thompson TL, et al., editors. Handbook of health communication. Erlbaum; Hillsdale, NJ.: 2003. pp. 263–284. [Google Scholar]
- 13.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychological bulletin. 1985;98(2):310. [PubMed] [Google Scholar]
- 14.Thoits PA. Conceptual, methodological, and theoretical problems in studying social support as a buffer against life stress. Journal of Health and Social behavior. 1982:145–159. [PubMed] [Google Scholar]
- 15.Cohen S, et al. Measuring the functional components of social support. Social support: Theory, research and applications. Springer. 1985:73–94. [Google Scholar]
- 16.Mezuk B, Diez Roux AV, Seeman T. Evaluating the buffering vs. direct effects hypotheses of emotional social support on inflammatory markers: the multi-ethnic study of atherosclerosis. Brain, behavior, and immunity. 2010;24(8):1294–1300. doi: 10.1016/j.bbi.2010.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Penninx BW, et al. Direct and buffer effects of social support and personal coping resources in individuals with arthritis. Social science & medicine. 1997;44(3):393–402. doi: 10.1016/s0277-9536(96)00156-6. [DOI] [PubMed] [Google Scholar]
- 18.Thoits PA. Stress and health major findings and policy implications. Journal of Health and Social Behavior. 2010;51(1 suppl):S41–S53. doi: 10.1177/0022146510383499. [DOI] [PubMed] [Google Scholar]
- 19.Umberson D, Montez JK. Social relationships and health A flashpoint for health policy. Journal of Health and Social Behavior. 2010;51(1 suppl):S54–S66. doi: 10.1177/0022146510383501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bruce M. A systematic and conceptual review of posttraumatic stress in childhood cancer survivors and their parents. Clinical psychology review. 2006;26(3):233–256. doi: 10.1016/j.cpr.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 21.Sarason IG, et al. Assessing social support: the social support questionnaire. Journal of personality and social psychology. 1983;44(1):127. [Google Scholar]
- 22.Barakat LP, et al. Families Surviving Childhood Cancer: A Comparison of Posttraumatic Stress Symptoms with Families of Healthy Children. Journal of Pediatric Psychology. 1997;22(6):843–859. doi: 10.1093/jpepsy/22.6.843. [DOI] [PubMed] [Google Scholar]
- 23.Kazak AE, et al. Posttraumatic stress, family functioning, and social support in survivors of childhood leukemia and their mothers and fathers. Journal of Consulting and Clinical Psychology. 1997;65(1):120–129. doi: 10.1037//0022-006x.65.1.120. [DOI] [PubMed] [Google Scholar]
- 24.Hung JW, Wu YH, Yeh CH. Comparing stress levels of parents of children with cancer and parents of children with physical disabilities. Psycho-Oncology. 2004;13(12):898–903. doi: 10.1002/pon.868. [DOI] [PubMed] [Google Scholar]
- 25.Manne SL, Duhamel K, Redd WH. Association of psychological vulnerability factors to post-traumatic stress symptomatology in mothers of pediatric cancer survivors. Psycho-Oncology. 2000;9(5):372–384. doi: 10.1002/1099-1611(200009/10)9:5<372::aid-pon471>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 26.Marsland AL, et al. A Pilot Trial of a Stress Management Intervention for Primary Caregivers of Children Newly Diagnosed With Cancer: Preliminary Evidence That Perceived Social Support Moderates the Psychosocial Benefit of Intervention. Journal of Pediatric Psychology. 2013;38(4):449–461. doi: 10.1093/jpepsy/jss173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Norberg AL, Lindblad F, Boman KK. Support-seeking, perceived support, and anxiety in mothers and fathers after children's cancer treatment. Psycho-Oncology. 2006;15(4):335–343. doi: 10.1002/pon.960. [DOI] [PubMed] [Google Scholar]
- 28.Wijnberg-Williams BJ, et al. Psychological distress and the impact of social support on fathers and mothers of pediatric cancer patients: Long-term prospective results. Journal of Pediatric Psychology. 2006;31(8):785–792. doi: 10.1093/jpepsy/jsj087. [DOI] [PubMed] [Google Scholar]
- 29.Rosenberg AR, et al. Resilience and psychosocial outcomes in parents of children with cancer. Pediatric blood & cancer. 2014;61(3):552–557. doi: 10.1002/pbc.24854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rini C, et al. Social support from family and friends as a buffer of low spousal support among mothers of critically ill children: A multilevel modeling approach. Health psychology. 2008;27(5):593. doi: 10.1037/0278-6133.27.5.593. [DOI] [PubMed] [Google Scholar]
- 31.Sarason IG, et al. A brief measure of social support: Practical and theoretical implications. Journal of social and personal relationships. 1987;4(4):497–510. [Google Scholar]
- 32.Spielberger C. State Trait Anxiety Inventory for Adults. Mind Garden; Redwood, CA: 1977. [Google Scholar]
- 33.Spielberger C, et al. Measuring anxiety and anger with the State-Trait Anxiety Inventory (STAI) and the State-Trait Anger Expression Inventory (STAXI) In: Marush M, editor. The use of psychological testing for treatment planning and outcomes assessment. Lawrence Erlbaum Associates; Mahwah, NJ.: 1999. pp. 993–1021. [Google Scholar]
- 34.Radloff LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied psychological measurement. 1977;1(3):385–401. [Google Scholar]
- 35.Derogatis LR, Savitz KL. The SCL–90–R and Brief Symptom Inventory (BSI) in primary care. 2000 [Google Scholar]
- 36.Zabora J, et al. A new psychosocial screening instrument for use with cancer patients. Psychosomatics. 2001;42(3):241–246. doi: 10.1176/appi.psy.42.3.241. [DOI] [PubMed] [Google Scholar]
- 37.Prelow HM, et al. A preliminary investigation of the validity and reliability of the Brief-Symptom Inventory-18 in economically disadvantaged Latina American mothers. Journal of Community Psychology. 2005;33(2):139–155. [Google Scholar]
- 38.Hayes A. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach (Guilford, New York) 2013 [Google Scholar]
- 39.Dahlquist LM, et al. Parents of children newly diagnosed with cancer: anxiety, coping, and marital distress. Journal of pediatric psychology. 1993;18(3):365–376. doi: 10.1093/jpepsy/18.3.365. [DOI] [PubMed] [Google Scholar]
- 40.Frank NC, et al. Predictors of affective responses of mothers and fathers of children with cancer. Psycho-Oncology. 2001;10(4):293–304. doi: 10.1002/pon.526. [DOI] [PubMed] [Google Scholar]
- 41.Hoekstra-Weebers JE, et al. Psychological adaptation and social support of parents of pediatric cancer patients: A prospective longitudinal study. Journal of pediatric psychology. 2001;26(4):225–235. doi: 10.1093/jpepsy/26.4.225. [DOI] [PubMed] [Google Scholar]
- 42.Doty DH. Common Methods Bias: Does Common Methods Variance Really Bias Results? Organizational research methods. 1998;1(4):374–406. [Google Scholar]