Abstract
Children with autism have heightened risk of developing oral health problems. Interventions targeting at-home oral hygiene habits may be the most effective means of improving oral hygiene outcomes in this population. This randomized control trial examined the effectiveness of a 3-week video-modeling brushing intervention delivered to patients over the internet. Eighteen children with autism were assigned to an Intervention or Control video condition. Links to videos were delivered via email twice daily. Blind clinical examiners provided plaque index ratings at baseline, midpoint, and endpoint. Results show oral hygiene improvements in both groups, with larger effect sizes in the Intervention condition. The findings provide preliminary support for the use of internet-based interventions to improve oral hygiene for children with autism.
Keywords: Oral hygiene, Intervention, Internet
Introduction
Individuals with autism spectrum disorder (ASD) exhibit a range of behavioral symptoms (American Psychiatric Association 2013). In addition, those with autism may have an array of concomitant medical issues, including problems with oral health. Studies have demonstrated that children with ASD exhibit habits that put them at high risk for developing caries (i.e., tooth decay or cavities) due to their classification as having special needs; in addition, those with ASD may have further risk factors specific to their disorder (American Academy of Pediatric Dentistry 2013; Jaber 2011; Klein and Nowak 1999; Marshall et al. 2010). Some of these factors may include poor hygiene, detrimental oral behaviors, medication-induced xerostomia, concurrent medical diagnoses, low cognitive abilities, poor dietary habits, gastric reflux, a preference for soft or sweet foods, use of sweets for behavior modification, and a need for help with tooth-brushing and other general fine-motor tasks. Due to the heterogeneity of symptom presentation in those with an ASD diagnosis, an individual child may exhibit a unique combination of these risk factors that impact his or her oral health.
Despite agreement that individuals with autism display many traits that increase their risk for developing dental decay, the reported caries rate in individuals with ASD is inconsistent. Some studies report high caries rate, as expected in a population with high risk habits (American Academy of Pediatric Dentistry 2013; Jaber 2011; Marshall et al. 2010), whereas others indicate that though individuals with ASD have many high caries risk factors, they actually have a low rate of caries (Loo et al. 2008).
Children with ASD are also at significant risk for developing dental disease that can be difficult to manage in the dental clinic. Children with autism tend to be extremely dependent on routine, and activities outside of their routine, such as a dental appointment, can cause significant stress on the child and dental office staff (Stein et al. 2012). Furthermore, children with ASD often have communicative impairments. Because behavior management techniques most often employed by dental practitioners rely on verbal communication, such strategies may not be as effective for this population (Loo et al. 2008; Weil and Inglehart 2012). In addition, many children with ASD are sensitive to sensory stimuli like bright lights, sounds, sensations, and odors; dental treatment may consequently be much more distressing for patients with ASD than typical patients (Cuvo et al. 2010; Friedlander et al. 2006).
Although children with ASD display many high caries risk behaviors, regular preventive care through improving oral hygiene may be the best way to reduce caries risk in this population. It is worth noting that there are many possible reasons why oral hygiene, more clearly defined as the practice of maintaining the cleanliness of the mouth and teeth on a regular basis, may be impaired in children with autism, including oppositional behaviors and aggression. However, the present intervention was designed to provide information about proper brushing techniques in an effort to improve oral health outcomes. Although many high-risk behaviors are only present in a small proportion of individuals with ASD, poor oral hygiene seems to be fairly common among these individuals and difficulty with home care can be explained by many of the same reasons that complicate treatment at the dentist's office (Capozza and Bimstein 2012; Jaber 2011; Stein et al. 2012; Weil and Inglehart 2012). However, because daily oral care is much less invasive and cost-effective, targeting interventions toward general oral hygiene may be a more effective route than clinic-based approaches.
There are many important considerations when designing oral hygiene interventions for children with ASD. First, information about the importance of good brushing habits and proper technique should be framed in a way that is interesting and accessible to this population and their caregivers. Interventions should be designed in a way that makes them realistic for families to access and adopt. In essence, they should be cost-effective, and parents should be able to employ the intervention frequently enough to impact behavior. One promising approach is through video-modeling delivered to caregivers and individuals over the internet.
Video modeling is one method that has been shown to effectively deliver information to children with ASD (Cardon 2012; Wang et al. 2011). It requires a child to watch a video clip of a target behavior and subsequently perform the viewed behavior, and it is most effective as an intervention for functional skills and imitation (Cardon and Wilcox 2011). Video modeling minimizes distractions and presents information using a medium that children with ASD are already comfortable with and interested in watching, and using video-modeled educational information is easily accessible by families.
There is a great need for effective interventions designed to improve oral hygiene in the home for children with ASD, and electronically delivered video-modeled social stories may offer one promising approach. This study is the first step toward developing an easily accessible, evidence-based, digital dental education program for individuals with autism and their caregivers.
Methods
This study was approved by the Yale University Human Investigation Committee and Pediatric Protocol Committee and registered at Clinicaltrials.gov. It was completed through collaboration between the Yale-New Haven Hospital (YNHH) Pediatric Dentistry and the Yale Child Study Center.
The YNHH Pediatric Dental clinic was responsible for patient recruitment, clinical examinations, and dental-related questions from participants. The Yale Child Study Center was responsible for technology management and any other questions the participants had during the course of the intervention. The YNHH Pediatric Dentistry team was blind to group assignment throughout the study.
Participants
Eighteen children between the ages of 5 and 14 years who had been identified in the YNHH Pediatric Dental clinic medical system as having autism were recruited to participate in this study. Parents also confirmed that the child had a current Individualized Education Program (IEP) specific to autism (See Table 1 for characterization). Access to Internet and email at home were required to participate. In addition, participants had to be patients on record at YNHH Pediatric Dental clinic, as well as have reliable transportation to and from the clinic. Eleven children (Intervention n = 6; Control n = 5) dropped out of the study by Time 3.
Table 1.
Sample characterization (means and standard deviations)
| Measure | Control | Experimental |
|---|---|---|
| N | 9 | 9 |
| Males:females | 4:5 | 6:3 |
| Age | 8.89 (1.76) | 8.78 (1.64) |
| Total videos | 8.33 (12.79) | 15.56 (16.00) |
| SRS-2 | 73.00 (16.32) | 82.11 (7.17) |
Participants were identified within the existing patient population at the Yale-New Haven Hospital Pediatric Dentistry clinic. The parents of potential participants were contacted by phone or at their child's routine clinical exam. If participants qualified, three appointment times for clinical exams were then scheduled. At the first clinic visit, written and verbal information about the study was given to parents. If the parents and child decided to participate, parents signed a consent form and children signed an assent form. If the parent and clinical examiner concluded that the child was unable to give consent, the assent form was omitted and only parental consent was used.
Intervention
This study was designed to assess the effectiveness and feasibility this program as a 3-week intervention, as well as to gauge parent interest in incorporating it into the child's home routine. At enrollment, participants were randomly assigned to receive a control video or intervention video for the duration of the study. Both videos were 1 min and 6 s long. Qualtrics online survey software was used to deliver video content by email at 5:30 AM and 4:30 PM each day for 3 weeks beginning the morning following the first clinical visit. At the conclusion of the video, participants were asked to complete a two-question survey asking if the participant watched the video and whether the child brushed his or her teeth after watching. After the first 3 weeks, participants were given a YouTube link to the video and told they were free to continue to watch the video if they chose. After 6 weeks, participants were given access to both videos and informed of their group assignment.
The intervention video modeled proper brushing technique with narration and closed captioning, allowing multiple ways to understand the message and potentially improving its effectiveness (Kokina and Kern 2010). It began with a title screen and an audio prompt signaling the start of the video (“Time to brush!”). From there, a 10-year-old female applied toothpaste to a toothbrush and began to brush her teeth. The video illustrates brushing each quadrant and ends with the subject brushing her anterior teeth. A male voice narrated the video with written captions for each quadrant (“Start with the toothpaste. Brush here for 30 s! Next, brush here for 30 s! Okay, now brush here for 30 s! Don't forget to brush the bottom teeth for 30 s! Brush the front teeth! Now it's your turn.”). The control video content consisted of moving, colorful fractal images generated by Electric Sheep (http://www.electric sheep.org/) set to original electronic, instrumental background music. It was designed to not be immediately obvious to parents that it was a control video, given what they knew about the study's hypotheses. Both videos were edited to be the same length.
Evaluations
At the initial visit, parents completed a Social Responsiveness Scale-Second Edition to confirm ASD diagnosis in the sample beyond the information provided by the IEP (SRS-2; Constantino and Gruber 2002). Caregivers also completed a short survey evaluating the child's oral hygiene practices at all three clinical visits. These surveys were rated on a 5-point Likert scale and included questions such as “How would you rate your child's oral hygiene at this time?” and “How often are teeth being brushed each day?” This survey also contained an open-ended section for parents or participants to provide any comments or feedback.
At each visit, clinical dental evaluators who were blinded to group assignment completed a plaque index to determine hygiene. A modified version of the plaque index described by Podshadley and Haley (1968) was used. One posterior and one anterior tooth in each arch were evaluated for the presence of plaque (#8, 14, 24, and #30). If permanent posterior teeth were not present, the most posterior primary tooth was used (#J or T). Each tooth was divided into five sections, and each section was identified as positive or negative for plaque. Quantity and quality of plaque were not evaluated; if any plaque was detected, the section was considered positive.
Six weeks after each participant's start date, a final hygiene survey was emailed to evaluate if the video was still being used and if any changes in oral hygiene were noted.
Results
Independent-sample t tests indicated that the two groups did not differ in age or SRS-2 scores. There was great variability in the number of videos watched over the course of the intervention, but this showed no difference between groups (Table 1). In addition, at Time 1, Mann–Whitney U tests on responses to the oral hygiene surveys indicated that the two groups were similar in all survey questions, including how their parents rated their oral hygiene, how many times per day their teeth were being brushed, and how motivated they were to brush (all p's > .05). Results at all time points are presented in Table 2.
Table 2.
Survey results means (choice endorsed)
| Time 1 |
Time 2 |
Time 3 |
||||
|---|---|---|---|---|---|---|
| Control | Exp | Control | Exp | Control | Exp | |
| How would you rate the severity of your child's autism? | 2.1 (Moderate) | 2.3 (Moderate) | 2.5 (Moderate-severe) | 2.4 (Moderate) | 2.2 (Moderate) | 2.5 (Moderate-severe) |
| How would you describe your child's sensitivity to sensory stimulation (touch, texture, light, taste)? | 2.9 (Fairly sensitive) | 3.0 (Fairly sensitive) | 2.6 (Fairly sensitive) | 2.8 (Fairly sensitive) | 2.3 (A little sensitive) | 3.0 (Fairly sensitive) |
| How often do you use visual supports (such as picture books, social stories, visual schedules) to help manage your child's behavior? | 2.6 (Every day) | 2.8 (Every day) | 2.0 (Occasionally) | 1.3 (Rarely) | 2.6 (Every day) | 3.0 (Every day) |
| How well can your child follow single-step instructions (e.g., “go get your backpack.”)? | 3.1 (Easily) | 2.9 (Easily) | 2.6 (Easily) | 2.4 (With difficulty) | 2.8 (Easily) | 2.5 (With difficulty-easily) |
| How well can your child follow multi-step instructions (e.g., “go put on your shoes and get your backpack.”)? | 2.0 (With difficulty) | 2.0 (With difficulty) | 2.2 (With difficulty) | 2.3 (With difficulty) | 2.2 (With difficulty) | 2.0 (With difficulty) |
| How would you rate your child's oral hygiene at this time? | 2.4 (Fair) | 2.0 (Fair) | 3.2 (Good) | 2.0 (Fair) | 3.2 (Good) | 1.8 (Fair) |
| Who initiates brushing each time? | 3.0 (Child must be reminded to brush) | 2.4 (Child must be convinced to brush) | 3.2 (Child must be reminded to brush) | 2.2 (Child must be convinced to brush) | 3.0 (Child must be reminded to brush) | 2.3 (Child must be convinced to brush) |
| How often are teeth being brushed each day? | 1.6 (2 times) | 1.7 (2 times) | 2.0 (2 times) | 2.0 (2 times) | 2.0 (2 times) | 2.0 (2 times) |
| How is oral hygiene completed? | 1.9 (Equally caregiver and child) | 2.3 (Equally caregiver and child) | 3.0 (Mostly by caregiver) | 2.0 (Equally caregiver and child) | 2.0 (Equally caregiver and child) | 2.3 (Equally caregiver and child) |
| How would you describe a typical visit to the dentist? | 1.9 (Neutral) | 2.3 (Neutral) | 2.0 (Neutral) | 3.0 (Difficult) | 1.6 (Neutral) | 2.8 (Difficult) |
| How motivated is your child to brush at this point? | 2.2 (Motivated) | 1.7 (Motivated) | 1.8 (Motivated) | 1.8 (Motivated) | 1.8 (Motivated) | 2.3 (Motivated) |
| How often is the video being watched before brushing? | N/A | N/A | 3.0 (Most of the time) | 3.0 (Most of the time) | 3.0 (Most of the time) | 2.8 (Most of the time) |
| How likely are you to continue using the video when the study ends? | N/A | N/A | 3.0 (Fairly likely) | 3.0 (Fairly likely) | 1.8 (Unsure) | 3.5 (Fairly likely-very likely) |
| If you are no longer using the video why has it been stopped? | N/A | N/A | 0.0 (Other) | 2.0 (Too difficult to access) | 2.3 (Too difficult to access) | 2.5 (Too difficult to access-does not help) |
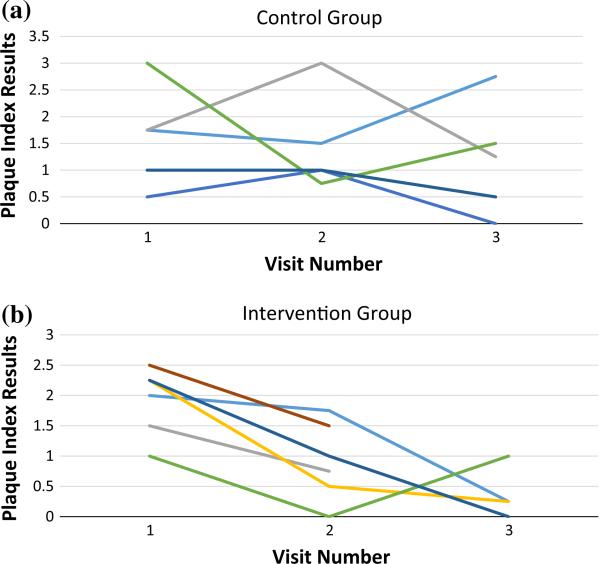
We used a linear mixed model approach with random subject intercepts to assess improvements in dental hygiene by group as measured by plaque index results over time. Results showed that children's oral hygiene improved in both groups [F(2, 22.27) = 5.92, p < .01]. No Group × Time interaction was detected (p = .28); however, an examination of effect sizes and mean-level changes suggested greater improvements in oral hygiene in the treatment group (Fig. 1; Table 3). At Time 1, plaque index results for both groups were similar [MC = 1.75 (.83), ME = 1.78(.62); Cohen's d = 0.04]. However, greater differences emerged by Time 3 [MC = 1.2(1.05), ME = .38(.43); d = 1.02].
Fig. 1.
Plot of plaque index results over time for individuals in the a Control, and b Intervention group
Table 3.
Plaque index scores (means and standard deviations)
| Group | Time 1 | Time 2 | Time 3 |
|---|---|---|---|
| Control | 1.75 (.83) | 1.45 (.91) | 1.20 (1.05) |
| Intervention | 1.78 (.62) | .92 (.65) | .38 (.43) |
| Cohen's d | 0.4 | 0.67 | 1.02 |
Due to the high attrition rate, we did not conduct any tests for differences in survey results over time. Overall the experimental group indicated that they were between “Fairly likely” and “Very likely” to continue using the video intervention. In addition to survey results, parent reporting and patient interaction at clinical exam showed that the intervention video made a positive impression on many participants. For example, one participant's mother indicated that her son had started reciting the prompts in the video as he watched his two older sisters brush their teeth and encouraged them to brush their teeth as outlined in the video. Another parent reported that their son requested the intervention video in the morning and before bed during a period of 2 days in which they were unable to access it, suggesting that it reinforced the routine of good oral hygiene.
In another case, parents reported that the control video had helped with brushing as well. Routinely sitting and focusing on the video allowed their child time to prepare for the act of brushing, resulting in more successfully completed brushing sessions.
Many patients’ behavior in the clinic improved over the course of the three clinical visits, as well. Most participants became more comfortable in the clinic at each visit, as reported by their dental provider. For example, three children who were unable to take intraoral radiographs before the study were able to at their third visit. One of these children was also able to sit for fillings, a procedure that previously had to be completed under general anesthesia in the operating room. These anecdotal improvements suggest further areas of promise and exploration within this field of study.
Discussion
This study was designed as a pilot for an intervention strategy designed to improve teeth brushing in children with autism. Results indicate that hygiene marginally improved in both the intervention and control groups. Although this improvement was not statistically significant, likely due to the small sample size, these findings are promising. Consistently decreasing plaque scores in the experimental group over the course of the intervention, coupled with parent reports of intervention success, suggests that this is a likely candidate for future intervention efforts.
Improved overall oral hygiene was likely due to twice-daily emails sent to both groups that reminded participants to watch the assigned video and to brush their teeth. The frequency of these reminders may have encouraged good oral hygiene practices regardless of the video content, making oral hygiene a higher priority in general and an established piece of the daily routine. Parent- and dentist-reports also indicated that the intervention had a noticeably positive effect on patients’ oral hygiene experience.
Although these results are encouraging, this study has a few notable limitations. Most importantly, the small sample size made it difficult to draw any definitive conclusions about the efficacy of the intervention video. This was due in large part to a high attrition rate caused by difficulties parents had getting to the dental clinic on a frequent basis. It is worth noting that this study was conducted in a dental clinic that primarily serves low income, Medicaid patients. Reliable transportation to and from the clinic as well as lack of access to technology exacerbated the attrition rate in this study. In addition, this population was exclusively characterized by SRS-2 scores and IEPs, suggesting uncontrolled variance in the diagnostic instruments and diagnoses in our sample. Although this is an important limitation to note, it is also reflective of the realities of many low-income children on the spectrum (Mandell et al. 2007). Future work will explore the effect of this intervention in larger and more diverse samples and include more comprehensive characterization assessments. Finally, this study had no way of documenting how frequently a child viewed each emailed video once the page was opened, leaving no way to control for potentially repetitive patterns of viewing. Future deployments will better document the number of plays so that this can be explored as well.
Future interventions could also incorporate other targets such as behavioral issues, social skills, or dental skills into a short, personalized story as well as provide additional behavioral supports. (Kokina and Kern 2010). It is likely that other techniques may be needed in addition to video modeling to address the particular difficulties with daily brushing experienced in this group.
Despite these limitations, this work demonstrates that many children with autism are able to brush their teeth effectively with the proper supports. This study also suggests that video modeling paired with email reminders can be a powerful means of providing information and resources to members of the autism community.
Acknowledgments
The authors thank Michael Perlmutter, for his expert video editing, and for N.P., for starring in the intervention video used in this study. We thank the children and their families for contributing to this research.
Funding This work benefited from funding by NIH awards K01 MH104739, R21 MH103550; the NSF Expedition in Socially Assistive Robotics #1139078; IES EDIES13C0046 I+II; the FAR Fund; the Nancy Taylor Foundation for Chronic Diseases, and the Hilibrand Family Foundation.
Footnotes
Author Contributions BP, FV, and FS conceptualized the study. BP, CW, LF, and FS designed the protocol. BP oversaw dental clinical study components and recruitment with aid from KD & DK. CW, LF, and FS designed and oversaw internet, digital, and questionnaire administration. KP designed the behavioral clinical battery. CW, FS, and MM conducted statistical analyses and with BP interpreted the findings. BP, CW, and FS drafted the manuscript, and all authors contributed to manuscript editing.
Compliance with Ethical Standards
Conflict of interest Ben Popple is owner of White Oak Pediatric Dentistry, PC. Frederick Shic has received research funding from Janssen and Roche. All other authors declare that they have no conflicts of interest.
Ethical Standards All procedures performed were in accordance with the ethical standards of the institutional review board.
Informed Consent Informed consent was obtained from an authorized representative (parent or guardian) for all participants in the study.
Human and Animal Rights This article does not contain any studies with animals performed by any of the authors.
References
- American Academy of Pediatric Dentistry Guideline on caries-risk assessment and management for infants, children, and adolescents. Pediatric Dentistry. 2013;35(5):E157–E164. [PubMed] [Google Scholar]
- American Psychiatric Association The diagnostic and statistical manual of mental disorders: DSM 5. bookpointUS. 2013 Retrieved from http://books.google.com/books?hl=en&lr=&id=_VzzAgAAQBAJ&oi=fnd&pg=PT2&dq=Diagnostic?and?statistical?manual?of?mental?disorders?(5th?ed.)&ots=oTXnrbMYXo&sig=HquBZDOR4lMNcsH8qAzS4KvXqro.
- Capozza LE, Bimstein E. Preferences of parents of children with autism spectrum disorders concerning oral health and dental treatment. Pediatric Dentistry. 2012;34(7):480–484. [PubMed] [Google Scholar]
- Cardon TA. Teaching caregivers to implement video modeling imitation training via iPad for their children with autism. Research in Autism Spectrum Disorders. 2012;6(4):1389–1400. doi:10.1016/j.rasd.2012.06.002. [Google Scholar]
- Cardon TA, Wilcox MJ. Promoting imitation in young children with autism: A comparison of reciprocal imitation training and video modeling. Journal of Autism and Developmental Disorders. 2011;41(5):654–666. doi: 10.1007/s10803-010-1086-8. [DOI] [PubMed] [Google Scholar]
- Constantino JN, Gruber CP. The social responsiveness scale. Los Angeles: Western Psychological Services. 2002 Retrieved from http://www.giuntios.it/it/catalogo/SR011.
- Cuvo AJ, Godard A, Huckfeldt R, DeMattei R. Training children with autism spectrum disorders to be compliant with an oral assessment. Research in Autism Spectrum Disorders. 2010;4(4):681–696. doi:10.1016/j.rasd.2010.01.007. [Google Scholar]
- Friedlander AH, Yagiela JA, Paterno VI, Mahler ME. The neuropathology medical management and dental implications of autism. The Journal of the American Dental Association. 2006;137(11):1517–1527. doi: 10.14219/jada.archive.2006.0086. doi:10.14219/jada.archive.2006.0086. [DOI] [PubMed] [Google Scholar]
- Jaber MA. Dental caries experience, oral health status and treatment needs of dental patients with autism. Journal of Applied Oral Science. 2011;19(3):212–217. doi: 10.1590/S1678-77572011000300006. doi:10.1590/S1678-77572011000300006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein U, Nowak AJ. Characteristics of patients with autistic disorder (AD) presenting for dental treatment: A survey and chart review. Special Care in Dentistry. 1999;19(5):200–207. doi: 10.1111/j.1754-4505.1999.tb01386.x. doi:10.1111/j.1754-4505.1999.tb01386.x. [DOI] [PubMed] [Google Scholar]
- Kokina A, Kern L. Social story™ interventions for students with autism spectrum disorders: A meta-analysis. Journal of Autism and Developmental Disorders. 2010;40(7):812–826. doi: 10.1007/s10803-009-0931-0. doi:10.1007/s10803-009-0931-0. [DOI] [PubMed] [Google Scholar]
- Loo CY, Graham RM, Hughes CV. The caries experience and behavior of dental patients with autism spectrum disorder. The Journal of the American Dental Association. 2008;139(11):1518–1524. doi: 10.14219/jada.archive.2008.0078. doi:10.14219/jada.archive.2008.0078. [DOI] [PubMed] [Google Scholar]
- Mandell DS, Ittenbach RF, Levy SE, Pinto-Martin JA. Disparities in diagnoses received prior to a diagnosis of autism spectrum disorder. Journal of Autism and Developmental Disorders. 2007;37(9):1795–1802. doi: 10.1007/s10803-006-0314-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall J, Sheller B, Mancl L. Caries-risk assessment and caries status of children with autism. Pediatric Dentistry. 2010;32(1):69–75. [PubMed] [Google Scholar]
- Podshadley AG, Haley JV. A method for evaluating oral hygiene performance. Public Health Reports. 1968;83(3):259. [PMC free article] [PubMed] [Google Scholar]
- Stein LI, Polido JC, Najera SOL, Cermak SA. Oral care experiences and challenges in children with autism spectrum disorders. Pediatric Dentistry. 2012;34(5):387–391. [PubMed] [Google Scholar]
- Wang S-Y, Cui Y, Parrila R. Examining the effectiveness of peer-mediated and video-modeling social skills interventions for children with autism spectrum disorders: A meta-analysis in single-case research using HLM. Research in Autism Spectrum Disorders. 2011;5(1):562–569. doi:10.1016/j.rasd.2010.06.023. [Google Scholar]
- Weil TN, Inglehart MR. Three- to 21-year-old patients with autism spectrum disorders: Parents’ perceptions of severity of symptoms, oral health, and oral health-related behavior. Pediatric Dentistry. 2012;34(7):473–479. [PubMed] [Google Scholar]