Introduction
The incidence of swallowing disorders (dysphagia) in the pediatric population is increasing at least in part because of the improved survival of children with medically complex conditions and histories of prematurity and low birth weight [1-4]. Oropharyngeal dysphagia is defined as difficulty swallowing caused by one or more underlying conditions that may involve any or all phases of swallowing [5]. In turn, infants and young children with dysphagia are at increased risk for aspiration-induced lung injury, nutritional compromise and stressful mealtime interactions. Various investigative imaging modalities are considered in diagnostic algorithms given the broad range of potential underlying etiologies, dysphagic presentations, and their associated consequences [6-8].
Two common diagnostic procedures are the upper gastrointestinal (UGI) series and videofluoroscopic swallow study (VFSS). The UGI series, which includes an esophagram, primarily focuses on the evaluation of upper gastrointestinal tract anatomy. The American College of Radiology and Society for Pediatric Radiology (ACR-SPR) has established a set of practice parameters for the performance of the UGI series that includes fluoroscopic screening of swallow function as a basic component of the UGI series [9]. In adherence with practice mandates to keep radiation exposure “as low as reasonably achievable” (ALARA), these examinations are typically performed at reduced fluoroscopic pulse rates [10, 11]. Although radiation exposure is decreased by the use of lower pulse rates, the detection of contrast entering the airway has been underestimated with rates less than 30 frames per second (fps) [10-12]. In contrast, the VFSS, is performed at 30 fps. It is the current the gold standard for the detection of swallowing impairments that may result in aspiration and development of appropriate treatment recommendations[8]. Health care providers are faced with clinical decision-making that calls upon incorporating information from varying evaluation modalities, including the presence or absence of aspiration on UGI series. Whether findings of aspiration on UGI are generalizable to clinical decision-making about aspiration with oral intake are unclear. Such information may be used to guide clinical management and the initiation of other referrals, particularly when aspiration with oral feeding is a concern. Our aims were to evaluate (1) whether findings of aspiration on the UGI series are predictive of aspiration on VFSS and (2) the impact of swallowing screening during UGI on radiation exposure.
Materials and Methods
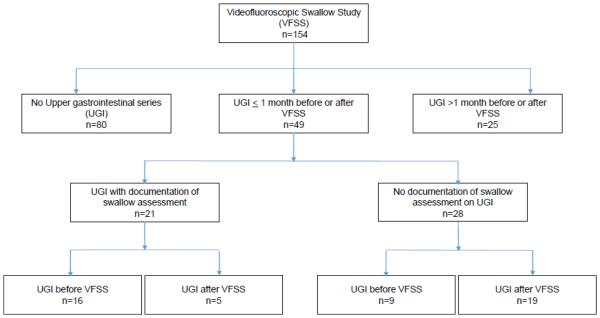
The present study is part of a larger prospective investigation that is focused on the standardization of the acquisition and interpretation of VFSS images in bottle-fed children with dysphagic concerns on the basis of history and/or clinical presentation. The protocol for this study was approved by the Institutional Review Board of the participating institution. For this investigation, a retrospective review was extracted from the database of all the 154 children who were bottle-fed (mean age 6.8 months, range 0.3–34.3 months), participated in the primary study, and who underwent a VFSS between March 2012 and December 2014. Data were extracted from the 49 patients (mean age 4.7 months; range 0.4–30.3 months) identified as having an UGI series performed within 1 month before or after the VFSS (Fig. 1).
Figure 1. Flowchart of VFSS and UGI series in the study population.
VFSS - Videofluoroscopic Swallow Study
UGI - Upper gastrointestinal series
VFSS studies were completed to evaluate children presenting with airway compromise or feeding difficulties suspicious for oropharyngeal dysfunction. Two speech-language pathologists (SLPs), with 8 and 25 years of experience with instrumental assessments in infants and young children, conducted and interpreted VFSS examinations. Children were positioned in their typical or best positions for bottle-feeding. They were seated in a dedicated fluoroscopy chair and imaged in the lateral plane. A standardized preparation of thin liquid barium (Varibar® 40% w/v ratio of barium sulfate concentration) was used for all VFSS examinations. The barium contrast was room temperature and administered by nipples and bottles that were supplied by radiology or brought from home, and adapted according to the clinical characteristics of the individual child. Outside the scope of this investigation, SLPs proceeded with clinically indicated compensatory strategies (e.g., bolus or utensil modifications, or positional changes) to optimize airway protection and bolus clearance. All examinations were performed with pediatric radiologists. Imaging focused on addressing each child’s clinical questions and management needs, while limiting radiation exposure. Consequently, the number of swallows imaged per child varied. All examinations used continuous fluoroscopy at a rate of 30 fps and digitized images of VFSS examinations were recorded and stored on the KayPENTEX Digital Swallowing Workstation Model 7245C. Upon completion of VFSS examinations, the participating SLP and senior radiology resident in conjunction with one fellowship trained pediatric radiologist reviewed images for evidence of swallowing dysfunction and the presence of aspiration as determined by consensus.
UGI series were performed for a variety of clinical indications, including vomiting with possible intestinal midgut malrotation, trachea-esophageal fistula, and pre-operative examinations to evaluate anatomy prior to planned gastrostomy tube placement [13]. All UGI examinations were performed by pediatric radiologists or supervised radiology residents or pediatric radiology fellows. They were completed using pulsed fluoroscopy at a rate of 3 fps and with the same thin liquid barium sulfate suspension (Varibar® 40% w/v ratio of barium sulfate concentration) that was used for VFSS examinations. The protocol at our institution includes a lateral view of the nasopharynx and larynx on digital fluoroscopy for the duration of 3-5 swallows during bottle feeding. Children were typically evaluated in the decubitus position.
Two radiologists blinded to the clinical characteristics of the children extracted and coded data from the final written reports of VFSS and UGI examinations. Decisions were made by consensus and coded according to whether the report included documentation of swallow function and if so, the presence or absence of aspiration. Cumulative radiation dose (CD), an estimation of skin dose, and radiation dose area product (DAP), an indicator of whole body dose, were recorded for each VFSS and UGI series.
Continuous measures (e.g., age, CD, and DAP) were not normally distributed and were summarized and compared using non-parametric statistics, i.e., medians, ranges, and Wilcoxon rank-sum tests. Categorical measures were summarized using counts and percentages, and compared using Fisher’s exact tests. Exact binomial confidence intervals (CIs) were calculated for sensitivity and specificity. Analyses were performed using SAS version 9.3 (SAS Institute, Inc., Cary, NC) and Stata/IC 12.1 (College Station, TX). All tests were two-sided and statistical significance was set at p<0.05.
Results
Demographic characteristics were comparable for children with and without documentation of swallowing on UGI (Table 1). Of the 49 patients who had both examinations, swallowing was documented in only 21 (43%) of the final UGI reports. As shown in Table 1, although CD was significantly higher for UGI with documentation of swallowing, DAP was not significantly higher for UGI with documentation of swallowing compared to without documentation of swallowing.
Table 1.
Demographic and radiologic characteristics by documentation of swallowing function on UGI for bottle-fed children (n = 49) with UGI performed within 1 month of VFSS
| Swallowing Function on UGI | |||
|---|---|---|---|
|
|
|||
| Documented (n=21) |
Not Documented (n=28) |
P valuea | |
| Demographic Characteristics | |||
| Male sex, N (%) | 14 (67) | 18 (64) | 0.99 |
| Gestational age, weeks | 38 (34-41) | 38 (23-40) | 0.87 |
| Chronologic Age at VFSS, months | 1.9 (0.4-17.5) | 3 (0.4-34.3) | 0.16 |
| Corrected age, months | 1.8 (0.0-17.8) | 2.5 (−1.0-34.3) | 0.23 |
| Inpatient, N (%) | 13 (62) | 24 (86) | 0.09 |
| Radiologic Details | |||
| UGI before VFSS, N (%) | 16 (76) | 9 (32) | 0.004 |
| UGI: | |||
| Cumulative radiation dose, mGy | 0.33 (0.05-0.96) | 0.21 (0.00-0.59) | 0.02 |
| Dose area product, μGycm2 | 4.11 (0.28-11.03) | 3.02 (0.24-9.37) | 0.09 |
| VFSS:b | |||
| Cumulative radiation dose, mGy | 1.42 (0.64-3.57) | 1.58 (0.57-3.51) | 0.63 |
| Dose area product, μGycm2 | 6.77 (3.03-31.92) | 9.75 (2.56-23.24) | 0.39 |
Abbreviations: mGy, milliGray; μGycm2, microGray centimeter squared; UGI, upper gastrointestinal series; VFSS, Videofluoroscopic Swallow Study Results presented are median (range) unless otherwise specified
P values are from Fisher’s exact tests or Wilcoxon rank-sum tests
Data are missing for one patient in the documented and 3 patients in the not documented group.
Using the VFSS as the gold standard, the calculated sensitivity for aspiration documented on UGI was 31% (4/13; 95% CI=9-61%) and specificity was 100% (8/8; 95% CI=63-100%). The positive predictive value was 100% (4/4; 95% CI=40-100%) and negative predictive value was 47% (8/17; 95% CI=23-72%).
Discussion
This is the first investigation, to our knowledge, that reports on the concordance between detection of aspiration on UGI series and VFSS, and the impact on radiation exposure associated with the imaging of swallowing function during an UGI series. Each study is performed to evaluate specific aspects of the digestive tract. While the UGI primarily evaluates the anatomy of the upper gastrointestinal tract, the VFSS focuses on oropharyngeal function for management decision-making. Although aspiration can be detected during either examination, neither the VFSS nor UGI is completed for the sole purpose of determining the presence or absence of aspiration. Our findings demonstrate that the UGI series performed at 3 fps has a high specificity and positive predictive value but a relatively low sensitivity for detection of aspiration. Given that children with dysphagic concerns frequently undergo both diagnostic procedures, this information may help guide clinical decision-making.
All of our patients with documentation of aspiration on UGI series had aspiration on thin liquid during VFSS. In contrast, 53% of our children without aspiration on UGI aspirated on VFSS. Consequently, although findings of aspiration on UGI are diagnostic and should prompt the need for further work up that may include a VFSS, the absence of aspiration on UGI series is not reassuring in symptomatic children. Consistent with the work of Vazquez, negative UGI findings in symptomatic children with suspected oropharyngeal dysphagia should prompt feeding/swallowing evaluations, including VFSS [13]. Multiple factors may contribute to the low sensitivity of UGI series for the detection of aspiration. UGI series guidelines recommend imaging a total of 3-5 swallows using pulsed fluoroscopy, which may not capture intermittent episodes of aspiration or changes in performance over time [9, 12]. In addition, UGI procedures are not set up to capture the typical range of oropharyngeal function during meals because of patient positioning, the administration of only a liquid contrast, and movement of the fluoroscope away from the oropharyngeal structures to capture bolus passage through the esophagus. In comparison, VFSS are performed with continuous fluoroscopy, imaging remains focused on the pharynx and upper esophageal sphincter, and efforts are made to simulate a “typical” oral feeding [8, 12]. Importantly, VFSS images provide information on the swallowing function and identify the physiologic reasons for the aspiration, which are essential to the development of management plans [13, 14].
Consequently, when clinical decision-making is dependent upon the increased risk of thin liquid aspiration in medically fragile infants and those with underlying lung disease, documentation of aspiration on UGI may provide the information needed for patient care. That said, even in the setting of liquid aspiration on UGI, the utility of VFSS should be considered to objectively define swallowing impairments and to guide diagnostic and management decision-making.
The updated ACR-SPR practice guidelines for the performance of contrast UGI examinations of infants and children include an assessment of swallowing in the lateral view, especially if the patient has a history or symptoms suggesting swallowing dysfunction [9]. We were surprised that more than half of the UGI did not document whether swallowing function was imaged. It is possible that the timing of UGI series relative to the VFSS influenced decisions about the safety and utility of imaging of swallowing function. UGI performed after VFSS may not have screened pharyngeal swallowing because of safety concerns or documentation of aspiration on a previous VFSS. We found a statistically significant increase in radiation exposure on UGI when swallowing function was documented; however, the clinical significance of this finding is not clear because of inherent variability found in recorded data from fluoroscopy equipment. Patient dose calculation and display on pediatric fluoroscopy equipment can vary as much as ±15 % for skin dose (1 mGy) and ± 20 % for DAP (0.1 µGy cm2) [15]. Additionally, we are unable to calculate comparable data for any patients who may have had their swallows imaged without documentation of swallowing. Although reasons for that lack of documentation are not clear, it is possible that performing radiologists did not document swallowing because they were aware of limitations associated with the reduced pulse rates and patient positioning. Additionally, the most recent ACR-SPR practice guidelines were published shortly after our subjects were examined [9]. Nonetheless, the potential impact on radiation exposure underscores the importance of documenting whether swallowing function was assessed or reasons for not imaging swallows during UGI.
Primary limitations of this study are related to factors associated with the retrospective nature of UGI data capture and a small sample derived from a single setting. Another limitation is related to the potential impact of the time interval and changes in patient status between the two imaging studies. We attempted to limit the likelihood of influences related to changes in medical and developmental status by excluding data from studies completed with greater than a 1-month interval. Despite the potential of remaining intervening influences, our experience suggests that clinicians are frequently asked to interpret the potential relevance of data acquired over time. Although lower frame rates reduce radiation exposure, frame rates below 30 fps may fail to capture contrast entering the airway and therefore underestimate the presence of swallowing dysfunction [12, 16]. As such, the 3 fps rate used during UGI may have compromised the detection of contrast entering the airway. In contrast to our findings, it is possible that an UGI series may show evidence of aspiration that is not detected during the same patient’s VFSS. Intermittent aspiration may not be captured during either examination and procedural variations may differentially impact airway protection. Further research is needed to determine the best means of identifying and quantifying oropharyngeal dysphagia for meaningful management and with the lowest dosage of radiation exposure.
Conclusion
In summary, aspiration on UGI series is highly predictive of thin liquid aspiration on VFSS. In comparison to VFSS, it is not sensitive for detection of aspiration. Imaging of swallows during an UGI series may have an appreciable increase on radiation exposure, therefore documentation of swallowing in the final report is important. Documentation of whether swallowing function is assessed is critical to the clinical care of patients. This information may facilitate further evaluation of high risk children, including VFSS for the objective identification of the type and extent of the underlying swallowing impairments.
Acknowledgements
The authors wish to thank the families for partaking in this project. We are also grateful for the contributions of Jennifer Wright, RN and Jeannine Hoch, MA, CCC-SLP in the Department of Pediatrics and Mahadevappa Mahesh MD, PhD, Chief Physicist in the Department of Radiology at Johns Hopkins Medical Institutions. Portions of the preliminary data were presented at the 7th Annual Meeting of the Society for Pediatric Radiology in May 2014. (“Should Routine UGIs Include Screening for Swallowing Dysfunction?” 57th Annual Meeting of the Society for Pediatric Radiology. Washington, DC.) This work was partially supported by the National Institutes of Health Grants NIDCD 5R01DC011290-05 (ML-G and BM-H). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Funding: This study was funded by NIH/NIDCD (1R01DC011290)
Footnotes
Conflict of Interest: Authors Kathryn A. Carson, Renee Flax-Goldenberg, Maureen Lefton-Greif, Bonnie Martin-Harris and Jeanne M. Pinto have received research grant funding from NIH/NIDCD.
Contributor Information
Renee Flax-Goldenberg, Division of Pediatric Radiology, The Russell H. Morgan Department of Radiology and Radiological Science, The Johns Hopkins University School of Medicine, Sheikh Zayed Tower, Room 4174, 1800 Orleans Street, Baltimore, MD 21287, USA
Kopal S. Kulkarni, The Russell H. Morgan Department of Radiology and Radiological Science, The Johns Hopkins Hospital, 601 N. Caroline Street, Room 4210, Baltimore, MD 21287, USA
Kathryn A. Carson, Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health, Welch Center for Prevention, Epidemiology and Clinical Research, 2024 East Monument Street, Suite 2-500, Baltimore, MD 21287, USA
Jeanne M. Pinto, Eudowood Division of Pediatric Respiratory Sciences, Department of Pediatrics, The Johns Hopkins University School of Medicine, David M. Rubenstein Building, Suite 3070, 200 North Wolfe Street, Baltimore, MD 21287, USA
Bonnie Martin-Harris, Department of Otolaryngology Head and Neck Surgery, College of Medicine, Medical University of South Carolina, 135 Rutledge Avenue, MSC 550, Charleston, SC 29425, USA, Evelyn Trammell Institute for Voice and Swallowing, Medical university of South Carolina, Charleston, SC 29425, USA, Ralph H. Johnson Veterans Affairs Medical Center, Charleston, SC 29425, USA.
Maureen A. Lefton-Greif, Eudowood Division of Pediatric Respiratory Sciences, Department of Pediatrics, The Johns Hopkins University School of Medicine, David M. Rubenstein Building, Suite 3017, 200 North Wolfe Street, Baltimore, MD 21287, USA, Department of Otolaryngology-Head and Neck Surgery, The Johns Hopkins University School of Medicine, Baltimore, MD 21287, USA, Department of Physical Medicine and Rehabilitation, The Johns Hopkins University School of Medicine, Baltimore, MD 21287, USA.
Reference List
- 1.Buie VC, Owings MF, DeFrances CJ, Golosinskiy A. National Hospital Discharge Survey: 2006 summary. National Center for Health Statistics. Vital Health Stat. 2010;13(168) [PubMed] [Google Scholar]
- 2.Newman LA, Keckley C, Petersen MC, Hamner A. Swallowing function and medical diagnoses in infants suspected of Dysphagia. Pediatrics. 2001;108(6):E106. doi: 10.1542/peds.108.6.e106. [DOI] [PubMed] [Google Scholar]
- 3.Ancel PY, Livinec F, Larroque B, Marret S, Arnaud C, Pierrat V, Dehan M, N'Guyen S, Escande B, Burguet A, Thiriez G, Picaud JC, Andre M, Breart G, Kaminski M. Cerebral palsy among very preterm children in relation to gestational age and neonatal ultrasound abnormalities: the EPIPAGE cohort study. Pediatrics. 2006;117(3):828–835. doi: 10.1542/peds.2005-0091. [DOI] [PubMed] [Google Scholar]
- 4.Burklow KA, Phelps AN, Schultz JR, McConnell K, Rudolph C. Classifying complex pediatric feeding disorders. J Pediatr Gastroenterol Nutr. 1998;27(2):143–147. doi: 10.1097/00005176-199808000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Donner MW. Editoral. Dysphagia. 1986;1(1):1–2. [Google Scholar]
- 6.Loughlin GM, Lefton-Greif MA. Dysfunctional swallowing and respiratory disease in children. Adv Pediatr. 1994;41:135–162. [PubMed] [Google Scholar]
- 7.Cleveland RH, Kushner DC, Schwartz AN. Gastroesophageal reflux in children: Results of a standardized fluoroscopic approach. American Journal of Roentgenology. 1983;141:53–56. doi: 10.2214/ajr.141.1.53. [DOI] [PubMed] [Google Scholar]
- 8.Arvedson JC, Lefton-Greif MA. Pediatric Videofluoroscopic Swallow Studies: A Professional Manual with Caregiver Handouts. Communication Skill Builders; San Antonio: 1998. [Google Scholar]
- 9.National Guideline Clearinghouse NGC . ACR-SPR practice guideline for the performance of contrast esophagrams and upper gastrointestinal examinations in infants and children. American College of Radiology (ACR): Agency for Healthcare Research and Quality (AHRQ); 2015. [Google Scholar]
- 10.Strauss KJ. ALARA in Pediatric Fluoroscopy. J Am Coll Radiol. 2007;4(12):931–933. doi: 10.1016/j.jacr.2007.08.023. [DOI] [PubMed] [Google Scholar]
- 11.Strauss KJ, Kaste SC. ALARA in pediatric interventional and fluoroscopic imaging: striving to keep radiation doses as low as possible during fluoroscopy of pediatric patients--a white paper executive summary. J Am Coll Radiol. 2006;3(9):686–688. doi: 10.1016/j.jacr.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 12.Cohen MD. Can we use pulsed fluoroscopy to decrease the radiation dose during video fluoroscopic feeding studies in children? Clin Radiol. 2009;64(1):70–73. doi: 10.1016/j.crad.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 13.Vazquez JL, Buonomo C. Feeding difficulties in the first days of life: findings on upper gastrointestinal series and the role of the videofluoroscopic swallowing study. Pediatr Radiol. 1999;29(12):894–896. doi: 10.1007/s002470050719. [DOI] [PubMed] [Google Scholar]
- 14.Logemann JA. Manual for the Videofluorographic Study of Swallowing. Pro-Ed; Austin, TX: 1993. [Google Scholar]
- 15. PhilipsEasyDiagnost Eleva Manual. Ver. 4.0. Hamburg Germany: 2010; Section: 18.1.8.
- 16.Dodds WJ, Stewart ET, Logemann JA. Physiology and radiology of the normal oral and pharyngeal phases of swallowing. American Journal of Roentgenology. 1990;154(5):953–963. doi: 10.2214/ajr.154.5.2108569. [DOI] [PubMed] [Google Scholar]