Abstract
Background
Prescription opioid use disorder and overdose have risen substantially in the U.S. Primary care physicians are critical to many ongoing and proposed efforts to address the prescription opioid epidemic. Yet, little is known about their attitudes and beliefs surrounding this issue. This study aimed to determine primary care physicians’ perceptions of the seriousness of the problem, its causes, groups responsible for addressing it, attitudes toward individuals with prescription opioid use disorder, beliefs about the effectiveness of addiction treatments, and support for various policies.
Methods
We conducted a national web-based survey in 2014 among 1,010 primary care physicians. We gauged responses to attitude and belief items on 7-point Likert scales. We examined the proportion agreeing with each statement, and whether responses differed among physicians prescribing higher and lower volumes of opioids.
Results
Respondents largely attributed the causes of prescription opioid use disorder to individual-oriented factors and certain physician-oriented factors, and believed that individuals with prescription opioid use disorder and physicians were primarily responsible for addressing the problem. Negative attitudes toward people with prescription opioid use disorder were prevalent, but a majority believed that treatment could be effective. There was majority support for all measured policies, with the highest levels of support for policies to monitor prescribing among patients potentially at risk for an opioid use disorder and to improve physician education and training.
Conclusions
Given strong endorsement of recommended policies, physician support could be leveraged to advance efforts to curb prescription opioid use disorder and overdose.
Keywords: Analgesics, opioids, opioid-related disorders, substance-related disorders, physicians, primary care
1. INTRODUCTION
During the last fifteen years, the substantial rise in sales and prescribing of opioid medications has correlated with increases in prescription opioid use disorder (OUD) and opioid overdose mortality rates (Kolodny et al., 2015). While the percentage of U.S. adults reporting nonmedical prescription opioid use declined during the period 2003–2013, the prevalence of prescription OUD and opioid overdose mortality rates rose (Han et al., 2015). The prescription opioid crisis also has contributed to a growing heroin problem, with the heroin overdose mortality rate climbing sharply in recent years (National Center for Health Statistics, 2015; Rudd et al., 2014). Problematic prescription opioid use is associated with greater susceptibility to heroin use (Cicero et al., 2014; Compton et al., 2016).
In the 1990s, the marketing of opioids for moderate to severe chronic non-cancer pain and an enhanced focus on improving pain treatment contributed to the upsurge in opioid prescribing (Kolodny et al., 2015; Zee, 2009). This marketing also minimized the addictive risks of these medications (Zee, 2009). Among all medical specialties, primary care physicians (PCPs) account for the largest volume of prescriptions for opioid medications (Chen et al., 2015; Volkow et al., 2011). Between 2007 and 2012, the opioid-prescribing rate grew at above-average rates among family practice, general practice and internal medicine specialties (Levy et al., 2015).
PCPs are critical to many ongoing and proposed efforts to prevent inappropriate prescribing and to detect prescription OUD and intervene to reduce morbidity and mortality (Alexander et al., 2015; Dowell et al., 2016). Altering opioid prescribing guidelines, enhancing training on pain management and addiction detection and treatment in medical school, residency and continuing medical education curricula, and increasing use of prescription drug monitoring programs (PDMPs) are all actions that directly affect physicians or require their engagement.
Recent survey research among physicians has focused largely on issues most relevant to clinical practice, including knowledge, attitudes, and concerns surrounding pain management, tamper-resistant medications, and using opioids to treat chronic non-cancer pain (Hwang et al., 2015a, 2015b; Jamison et al., 2014; Macerollo et al., 2014; Turk et al., 2014; Wolfert et al., 2010). Hwang and colleagues’ 2014 survey of PCPs found that more than half of respondents felt that prescription drug abuse was a major problem (Hwang et al., 2015b). Hwang and colleagues also examined provider perspectives on factors contributing to problematic prescription opioid use, knowledge of how these medications are misused, and support for clinical interventions involving physicians and regulatory interventions including restrictions on pharmaceutical companies’ marketing practices (Hwang et al., 2015a, 2015b).
However, no study to-date has examined physician perspectives on who is responsible for addressing the problem, their attitudes toward people with prescription OUD, and their support for a broad range of proposed policies. In fact, we are aware of only one study that has examined these issues among the broader U.S. non-physician public, which offers an opportunity to compare physician attitudes on this topic to the general population (Barry et al., 2016). Understanding the role physicians see themselves as playing in addressing the crisis and how they feel about the affected population and potential policy responses have important implications for identifying viable solutions.
In order to fill these gaps in prior research, we conducted a survey among PCPs in the U.S. to assess attitudes surrounding the prescription opioid epidemic. We examined a wide array of causal attributions for prescription OUD and assessed which groups PCPs view as responsible for addressing the problem, and the extent to which physicians view themselves as responsible relative to other stakeholders. In addition, we measured PCPs’ beliefs about individuals with prescription OUD and perceptions of the effectiveness of addiction treatment. We also measured physicians’ support for 19 policies endorsed by expert bodies and governmental entities (American Medical Association, 2013; Centers for Disease Control and Prevention, 2013; Office of National Drug Control Policy, 2013; Trust for America’s Health, 2013). Finally, we sought to characterize differences in attitudes among the subgroup of PCPs prescribing higher quantities of opioid medications, given their closer interaction with patients potentially at risk of prescription OUD (Edlund et al., 2014).
2. MATERIAL AND METHODS
2.1 Data collection
From July 11 – 21, 2014, we conducted a web-based survey among a random sample of physicians practicing in internal medicine, family practice and pediatrics. We contracted with a survey research firm, which has developed a national panel of approximately 90,000 physicians in the U.S. using the American Medical Association (AMA) Physician Masterfile to recruit panelists (GfK KnowledgeNetworks, 2015). Panelists opt-in and receive financial incentives to participate in surveys. Other researchers have conducted surveys using this panel to gain insight into U.S. physician opinions and attitudes on various health issues (Gilkey et al., 2015a, 2015b; Maurer and Harris, 2014). Among the 3,495 panelists sampled to participate in this survey, 1,023 completed or screened out of the survey, resulting in a survey completion rate of 29.2 percent. In addition to eleven who screened out, we also dropped two respondents who took three minutes or less to complete the survey, resulting in a final sample size of 1,010.
2.2 Survey design
Prior to asking questions specific to prescription opioids, we asked respondents to indicate the degree to which they felt 12 different health issues were serious problems (measured on 5-point Likert scales) using an item adapted from other survey research to assess issue salience among the public (Barry et al., 2016; Mendes, 2012; Thompson et al., 2013). We asked about health issues including prescription OUD, unhealthy alcohol use, and illegal drug use, as well as chronic illnesses including heart disease and diabetes. Throughout the survey, we used the terminology “prescription pain medication” accompanied by a short definition and the opportunity to view a list of these medications. (See Supplementary Material A1.)
We asked respondents about their medical careers and practices, including: highest medical degree, year of medical school graduation, setting in which they worked most often, practice size, professional activity (patient care, research, teaching or administration), and the state in which they practiced. To gain a sense of physicians’ prescribing patterns, we asked respondents how often they prescribed opioids in a typical month, and the most frequent indication for prescribing these medications (mostly to treat acute pain, chronic pain or a combination). We also asked respondents to indicate, on 7-point Likert scales (strongly disagree to strongly agree), whether opioid medications are an effective treatment option for managing non-cancer acute pain or non-cancer chronic pain. In addition, we asked whether respondents had ever prescribed buprenorphine or naltrexone to treat OUD and measured, on 7-point Likert scales (very uncomfortable to very comfortable), respondents’ comfort screening patients for substance use and mental disorders.
To understand better how PCPs viewed the problem, we asked respondents about the causes of prescription OUD, which groups are responsible for addressing the problem, beliefs about individuals with prescription OUD, perceptions of treatment effectiveness, and support for different types of policies to address the prescription opioid epidemic. We randomized the order of the question modules and the order of questions within each module in order to mitigate the influence of earlier questions on responses to later questions. Specifically, we asked respondents about the degree to which they agreed with twenty different potential explanations for prescription OUD, measuring agreement on a 7-point Likert scale (strongly disagree to strongly agree). Causal explanations included individual-oriented causes (e.g., some people do not understand how easy it is to become addicted), physician-oriented causes (e.g., doctors often put patients on too high doses), pharmaceutical industry-oriented causes (e.g., pharmaceutical companies promote these medications without adequate knowledge of their safety and effectiveness), and other causes related to health insurance companies, law enforcement and pharmacies (Barry et al., 2016).
We asked respondents to rate the level of responsibility of various groups for addressing the prescription opioid epidemic, including: individuals with prescription OUD, physicians, pharmaceutical companies, health insurance companies, law enforcement, pharmacies and pharmacists, and government. We measured these responses on 7-point scales with 1 indicating hardly any responsibility and 7 a great deal of responsibility for addressing the problem.
Respondents reported on how they viewed persons with prescription OUD, using a variety of questions adapted from other survey research on social stigma (Barry et al., 2014; Link et al., 2004; McGinty et al., 2015; Pescosolido et al., 2010), including concepts like social distance from the target group, perceived dangerousness, and acceptance of discrimination. Specifically, we asked respondents to indicate the degree to which they were willing to have a person with prescription OUD start working closely with them on the job or marry into their family as measures of desire for social distance (an aspect of stigma); their agreement with the statement that people with prescription OUD are more dangerous than the general population; and the extent to which they agreed that employers should be allowed to deny employment, and landlords to deny housing, to a person with prescription OUD. Finally, using questions adapted from other surveys to assess perceptions of treatment effectiveness (Barry et al., 2014; Pescosolido et al., 2010), respondents reported on the extent to which they believed that effective treatment options are available to help people with prescription OUD and that most people with prescription OUD can, with treatment, get well and return to productive lives. We measured all items on 7-point Likert scales.
We asked respondents to indicate whether they opposed or favored 19 different policies to address prescription OUD. These included policies that focused on individuals with prescription OUD (e.g., increasing government spending to improve treatment for prescription OUD), physicians (e.g., requiring doctors to complete a physical exam on a patient before recommending prescription opioids), pharmaceutical companies (e.g., requiring better labeling of prescription opioids), other health system-related issues (e.g., increasing oversight of clinics that employ doctors who write a large number of opioid prescriptions), among others. We selected policies endorsed by various expert bodies including Trust for America’s Health (Trust for America’s Health, 2013) the Centers for Disease Control and Prevention (Centers for Disease Control and Prevention, 2013) the Office of National Drug Control and Prevention (Office of National Drug Control Policy, 2013), and the American Medical Association.(American Medical Association, 2013)
2.3 Analytic Approach
We calculated the proportion of respondents who endorsed each statement by dichotomizing the Likert scale responses. We coded responses 5–7 on the 7-point Likert scales as one (indicating endorsement/agreement) and coded responses 1–4 as zero. We selected five as the point of dichotomization because it is the rating level above the neutral point (4) on the 7-point Likert scale. In addition, we used chi square tests to examine whether responses differed among physicians who reported prescribing higher and lower volumes of prescription opioids. We categorized respondents as higher-volume prescribers if they reported prescribing opioid medications more than 20 times in a typical month and lower-volume prescribers as prescribing opioids 20 times or less in a typical month. We also conducted a sensitivity analysis comparing respondents prescribing opioids more than 30 times in a month to the remaining respondents. We analyzed these data using Stata 12® (StataCorp, 2011). The [blinded for review] internal review board approved this study as exempt.
3. RESULTS
3.1 Respondent characteristics
Table 1 displays information on respondent characteristics and their clinical practices. Ninety percent of respondents had doctor of medicine degrees with the remaining 10% holding doctor of osteopathy degrees. Respondents were fairly evenly distributed across the three specialties: family practice (35%), internal medicine (32%), and pediatrics (33%). The majority of respondents (78%) reported prescribing opioids 20 times or less in a typical month. Among those who reported prescribing these medications, only 10% reported prescribing opioids mostly to treat chronic pain whereas nearly half (48%) prescribed these medications mostly to treat acute pain and 42% for a combination of acute and chronic pain. Most (85%) respondents thought opioids were an effective treatment for managing acute non-cancer pain; greater than half (56%) thought opioids were effective treatment options for chronic non-cancer pain. Sixty-two percent of respondents reported feeling comfortable screening patients for substance use disorders and 13% reported having prescribed medication for opioid addiction (e.g., buprenorphine, naltrexone).
Table 1. Primary care physician characteristics, clinical practices and attitudes, 2014.
| Proportion of respondents | N Total = 1,010 |
|
|---|---|---|
| Respondent characteristics | ||
| Highest medical degree | ||
| Doctor of Medicine (MD) | 89.5 | 904 |
| Doctor of Osteopathy (DO) or other a | 10.5 | 106 |
| Specialty | ||
| Family practice | 34.7 | 351 |
| Internal medicine | 32.2 | 325 |
| Pediatrics | 33.1 | 334 |
| Year graduated medical school | ||
| 1979 or earlier | 18.9 | 191 |
| 1980–1989 | 39.0 | 394 |
| 1990–1999 | 33.6 | 339 |
| 2000 or later | 8.5 | 86 |
| Gender | ||
| Male | 72.3 | 730 |
| Female | 27.7 | 280 |
| Practice setting (where respondent works most often) | ||
| Private solo or group practice | 82.1 | 818 |
| Hospital setting (e.g., ED, outpatient department) b | 6.0 | 60 |
| Community health center | 4.5 | 45 |
| Other (e.g., HMO, institutional setting, gov’t or free clinic) c | 7.4 | 74 |
| Number of physicians associated with practice | ||
| 1 physician | 19.2 | 194 |
| 2–3 physicians | 25.2 | 254 |
| 4–10 physicians | 32.7 | 330 |
| 11–50 physicians | 15.0 | 151 |
| 51 or more physicians | 8.0 | 81 |
| Professional activity | ||
| Patient care | 98.8 | 998 |
| Other (e.g., research, teaching, administration) | 1.2 | 12 |
| Region of practice | ||
| Northeast | 25.8 | 261 |
| Midwest | 21.0 | 212 |
| South | 36.5 | 369 |
| West | 16.6 | 168 |
| Clinical practices and attitudes | ||
| Frequency of prescribing opioid medications in typical month | ||
| Never prescribes opioid medications | 13.6 | 137 |
| 1–20 times/month | 64.5 | 651 |
| 21 times/month or more | 22.0 | 222 |
| Reason for prescribing opioid medications (N=868) | ||
| Mostly to treat acute pain | 48.0 | 419 |
| Mostly to treat chronic pain | 9.9 | 86 |
| A combination of both | 42.1 | 368 |
| Agrees that prescription opioids are an effective treatment option for managing non-cancer acute pain d | 85.2 | 860 |
| Agrees that prescription opioids are an effective treatment option for managing non-cancer chronic pain | 55.6 | 562 |
| Has ever prescribed buprenorphine/suboxone/Subutex or naltrexone to treat opioid addiction | 13.1 | 132 |
| Comfortable screening patients for mental health disorders | 76.0 | 767 |
| Comfortable screening patients for substance use disorders | 62.1 | 627 |
Other included 3 respondents, one of whom identified self as doctor of osteopathic medicine in the text field, one whom identified self as an internist and one whom provided no additional information.
This category included respondents identifying hospital emergency department (ED), hospital outpatient department, city hospital, and hospital inpatient (not further defined) as the location in which they work most often.
This category included respondents identifying free standing clinic, institutional settings (e.g., school infirmary, nursing home, prison), non-federal government clinic (e.g., state, county, city, maternal and child health), industrial outpatient facility, family planning clinic, federal government operated clinic (e.g., VA, military, etc.) and health maintenance organization or other prepaid practices (e.g., Kaiser Permanente).
Agreement with statement was measured on 7-point Likert scale with 7 indicating strongly agree with statement. Responses 5–7 were coded 1 to indicate general agreement with statement.
3.2 Respondent attitudes and beliefs
Seventy-two percent of respondents felt that prescription OUD was a very or extremely serious problem facing the U.S. (see Supplementary Material B2). However, in comparison to the other 12 health issues queried, prescription OUD ranked in the middle, below major chronic illnesses like obesity, heart disease, smoking and tobacco use, but above unhealthy alcohol use and motor vehicle crashes.
Table 2 shows respondents’ beliefs about the causes of the prescription OUD. Substantial majorities of respondents agreed with all of the individual-oriented causal explanations. Large majorities also agreed that it was too easy to obtain multiple prescriptions from different doctors (85%) and that doctors often keep patients on prescription opioids for too long (73%). Approximately half of respondents endorsed causal attributions related to the pharmaceutical industry, such as inadequate explanation of the risks of addiction on medication labels (54%) and promotion of these medications without adequate knowledge of their safety and effectiveness (46%). We identified several statistically significant but small differences in causal attributions comparing respondents with different prescribing practices. More lower-volume prescribers than higher-volume prescribers thought that it was too easy for patients to obtain multiple prescriptions from different doctors (87% vs. 77%, p-value<0.01), and that doctors often keep patients on prescription opioids for too long (75% vs. 68%, p-value=0.04).
Table 2.
Beliefs about the causes of prescription opioid use disorder among higher- and lower- volume prescribing primary care physicians, 2014
| Proportion of respondents who agree with statementa (95% CI) |
|||
|---|---|---|---|
| All respondents N=1,010 |
Lower volume prescribersb N=788 |
Higher volume prescribersc N=222 |
|
| Individual-oriented causes | |||
| Some people do not understand how easy it is to become addicted to prescription pain medication | 89.6 (87.7, 91.5) |
90.2 (88.2, 92.3) |
87.4 (83.0, 91.8) |
| Some people are self-medicating untreated pain | 88.7 (86.8, 90.7) |
88.7 (86.5, 90.9) |
88.7 (84.5, 92.9) |
| Some people are given prescription pain medications by friends or family members | 87.5 (85.5, 89.6) |
86.5 (84.1, 88.9) |
91.0 (87.2, 94.8) |
| Some people have a family history that makes them more likely to abuse prescription pain medications | 82.5 (80.1, 84.8) |
82.9 (80.2, 85.5) |
81.1 (75.9, 86.3) |
| Some people do not store prescription pain medications safely in their homes, making these drugs easy for others to take | 75.7 (73.1, 78.4) |
74.9 (71.8, 77.9) |
78.8 (73.4, 84.2) |
| Some people lack self-discipline to use prescription pain medications without becoming addicted | 74.4 (71.7, 77.1) |
73.2 (70.1, 76.3) |
78.4 (72.9, 83.8) |
| Some people do not dispose prescription pain medications when they are no longer needed, making these drugs easy for others to take | 69.2 (66.4, 72.1) |
69.4 (66.2, 72.6) |
68.5 (62.3, 74.6) |
| Physician-oriented causes | |||
| Too easy to get multiple pain medication prescriptions from different doctors | 84.9 (82.6, 87.1) |
87.1 (84.7, 89.4) |
77.0** (71.5, 82.6) |
| Doctors often keep patients on prescription pain medications for too long | 73.1 (70.3, 75.8) |
74.6 (71.6, 77.7) |
67.6* (61.4, 73.8) |
| Doctors don’t get enough training about how to prescribe prescription pain medications | 66.0 (63.1, 69.0) |
66.5 (63.2, 69.8) |
64.4 (58.1, 70.8) |
| Doctors often write prescriptions for pain medications without properly examining patient to assess need | 61.1 (58.1, 64.1) |
62.6 (59.2, 65.9) |
55.9 (49.3, 62.4) |
| Doctors often put patients on prescription pain medications at too high doses | 49.2 (46.1, 52.3) |
49.5 (46.0, 53.0) |
48.2 (41.6, 54.8) |
| Some doctors exchange prescription pain medications for money | 39.2 (36.2, 42.2) |
40.5 (37.0, 43.9) |
34.7 (28.4, 41.0) |
| Pharmaceutical industry-oriented causes | |||
| Pharmaceutical companies do not adequately explaining the risks of addiction on medication labels | 54.5 (51.4, 57.5) |
55.1 (51.6, 58.6) |
52.3 (45.6, 58.9) |
| Pharmaceutical companies promote prescription pain medications without adequate knowledge of safety and effectiveness | 45.9 (42.9, 49.0) |
46.7 (43.2, 50.2) |
43.2 (36.7, 49.8) |
| There has been inadequate research on safety and effectiveness of prescription pain medications | 44.6 (41.5, 47.6) |
44.2 (40.6, 47.6) |
45.9 (39.3, 52.6) |
| Other causes | |||
| Too easy to get multiple prescription pain medications from different pharmacies | 79.4 (76.9, 81.9) |
81.0 (78.2, 83.7) |
73.9* (68.0, 79.7) |
| Health insurance companies more likely to pay for prescription pain medications than other treatments like PT or acupuncture | 74.1 (71.4, 76.8) |
74.2 (71.2, 77.3) |
73.4 (67.6, 79.3) |
| Drug dealers face too little risk for illegally selling prescription pain medications | 73.3 (70.5, 76.0) |
73.1 (70.1, 76.2) |
73.9 (68.0, 79.7) |
| Law enforcement doesn’t focus enough on arresting drug dealers who illegally sell prescription pain medications | 59.5 (56.5, 62.5) |
59.5 (56.1, 63.0) |
59.5 (53.0, 66.0) |
Respondents who selected 5–7 on the 7-point Likert scale (7 indicating “strongly agree” with statement) were coded as generally agreeing with the statement about the cause of prescription opioid abuse in the U.S. Respondents who selected 1–4 on the 7-point Likert scale (1 indicating “strongly disagree” with statement) were coded as disagreeing or being neutral about the statement.
Respondents were identified as low volume prescribers if they reported prescribing opioid medications 20 times or less in a typical month.
Respondents were identified as high volume prescribers if they reported prescribing opioid medications more than 20 times in a typical month.
p-value<0.01
p-value<0.05
Chi square tests were used to assess whether proportions differed significantly between high and low volume prescribers.
Most (89%) respondents attributed responsibility for the problem to individuals with prescription OUD (see Figure 1). Although the second largest proportion (83%) attributed responsibility for addressing the problem to doctors, this proportion was statistically significantly lower (p-value<0.01) than the proportion attributing responsibility to individuals with prescription OUD.
Figure 1.
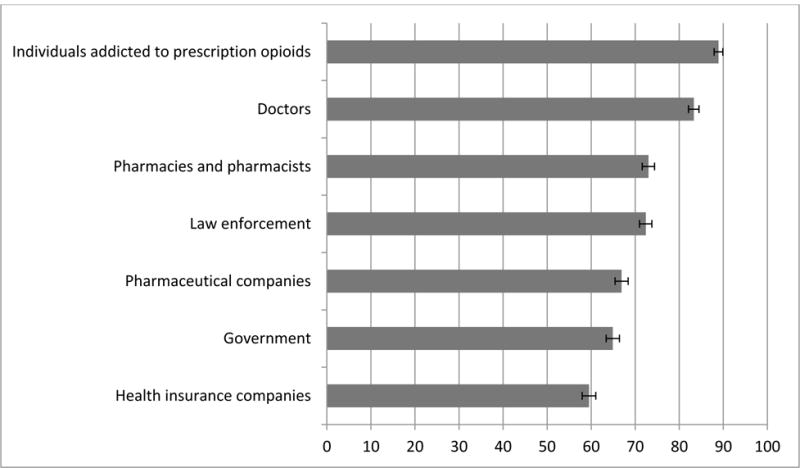
Proportion of primary care physicians who view group as responsible for addressing the problem, 2014
Respondents who selected 5–7 on the 7-point Likert scale (7 indicating group had “a great deal” of responsibility for addressing the problem of prescription opioid abuse in the U.S.) were coded as generally viewing the group as responsible for addressing the problem.
Table 3 displays respondents’ beliefs about individuals with prescription OUD, and perceptions of the effectiveness of available treatments for opioid addiction. Respondents reported high levels of desire for social distance: large majorities were unwilling to have a person with prescription OUD marry into the family (79%) or to work closely with the respondent on the job (77%). More than half (66%) viewed people with prescription OUD as more dangerous than the general population. The majority of respondents, however, believed that most people with a prescription OUD can get well with treatment (69%) and that effective treatment options are available to help people with OUD (58%).
Table 3.
Beliefs about persons with prescription opioid use disorder (OUD) and perceptions of treatment effectiveness among primary care physicians, 2014
| Proportion of respondents who endorse statementa (95% CI) |
|
|---|---|
| Beliefs about population | |
| Unwilling to have a person with an addiction to prescription pain medication marry into family | 79.3 (76.8, 81.8) |
| Unwilling to have a person with an addiction to prescription pain medication start working closely with respondent on the job | 76.6 (74.0, 79.2) |
| People addicted to prescription pain medication are more dangerous than the general population | 66.4 (63.5, 69.4) |
| Employers should be allowed to deny employment to a person addicted to prescription pain medication | 64.1 (61.1, 67.0) |
| Landlords should be allowed to deny housing to a person addicted to prescription pain medication | 37.5 (34.5, 40.5) |
| Perceptions of effectiveness of opioid addiction treatment options | |
| Most people addicted to prescription pain medication can, with treatment, get well and return to productive lives | 69.2 (66.4, 72.1) |
| Effective treatment options are available to help people who are addicted to prescription pain medication | 57.8 (54.8, 60.9) |
Respondents who selected 5–7 on the 7-point Likert scale were coded as generally endorsing the statement.
Table 4 displays support for different types of policies to reduce prescription OUD. Virtually all respondents supported identification verification requirements at pharmacies (96%), establishing PDMPs in all states (92%), and requiring medical schools and residency programs to provide training on addiction detection and treatment (91%) and chronic pain treatment (90%). Among all policies, respondents expressed the lowest level of support for providing naloxone to friends and family members of people using opioid medications; even so, slightly more than half of respondents (53%) supported this policy.
Table 4.
Support for policies to reduce prescription opioid use disorder among higher and lower volume prescribing primary care physicians, 2014
| Proportion of respondents who favor policy a (95% CI) |
|||
|---|---|---|---|
| All respondents N=1,010 |
Low volume prescribersb N=788 |
High volume prescribersc N=222 |
|
| Requiring pharmacies to verify patient identification before giving out prescription pain medication | 96.3 (95.2, 97.5) |
96.6 (95.3, 97.8) |
95.5 (92.7, 98.2) |
| Establishing prescription drug monitoring programs (PDMPs) in all states | 91.6 (89.9, 93.3) |
92.3 (90.4, 94.1) |
89.2 (85.1, 93.3) |
| Requiring medical schools and physician residency programs to provide training for physicians in how to detect and treat addiction to prescription pain medication | 91.4 (89.7, 93.1) |
92.0 (90.1, 93.9) |
89.2 (85.1, 93.3) |
| Requiring medical schools and physician residency programs to train physicians to treat chronic pain | 90.2 (88.4, 92.0) |
90.1 (88.0, 92.2) |
90.5 (86.7, 94.4) |
| Requiring individuals enrolled in Medicaid programs who are suspected of abusing prescription pain medication to use a single physician prescriber and single pharmacy | 88.4 (86.4, 90.4) |
87.6 (85.3, 89.9) |
91.4 (87.7, 95.2) |
| Integrating PDMPs into current electronic medical record systems | 87.2 (85.2, 89.3) |
88.6 (86.4, 90.8) |
82.4* (77.4, 87.5) |
| Arresting and prosecuting people who obtain multiple prescriptions for pain medication at the same time from different doctors | 84.3 (82.0, 86.5) |
84.8 (82.3, 87.3) |
82.4 (77.4, 87.5) |
| Requiring doctors to complete a physical exam on a patient before recommending prescription pain medication | 84.3 (82.0, 86.5) |
85.5 (83.1, 88.0) |
79.7* (74.4, 85.1) |
| Increasing oversight of clinics that employ doctors who write a very large number of prescriptions for pain medication | 83.5 (81.2, 85.8) |
86.5 (84.2, 88.9) |
72.5** (66.6, 78.4) |
| Requiring pharmaceutical companies to include prominent labels with instructions about how to properly dispose of unused prescription pain medications | 81.8 (79.4, 84.2) |
82.1 (79.5, 84.8) |
80.6 (75.4, 85.9) |
| Developing new guidelines to encourage physicians to consider alternates for prescription pain medication, such as physical therapy or acupuncture, for treating chronic pain | 81.2 (78.8, 83.6) |
82.6 (80.0, 85.3) |
76.1* (70.5, 81.8) |
| Requiring doctors to check and record patient histories in these databases when prescribing prescription pain medication | 76.0 (73.4, 78.7) |
77.3 (74.3, 80.2) |
71.6 (65.6, 77.6) |
| Expanding Medicaid insurance benefits for low income families to require coverage for treatment of substance abuse problems, including addiction to prescription pain medications | 71.7 (68.9, 74.5) |
70.8 (67.6, 74.0) |
74.8 (69.0, 80.5) |
| Increasing government spending to improve treatment of substance abuse problems, including addiction to prescription pain medications | 69.6 (66.8, 72.4) |
69.9 (66.7, 73.1) |
68.5 (62.3, 74.6) |
| Requiring pharmaceutical companies to fund more studies on the safety and effectiveness of prescription pain medications to treat chronic pain | 66.7 (63.8, 69.6) |
67.4 (64.1, 70.7) |
64.4 (58.1, 70.8) |
| Passing laws to protect people from criminal charges for drug crimes if they seek medical help for themselves or others experiencing a prescription pain medication overdose | 66.4 (63.5, 69.4) |
65.7 (62.4, 69.1) |
68.9 (62.8, 75.1) |
| Requiring doctors to complete continuing medical education in order to prescribe narcotic pain medications | 64.2 (61.2, 67.1) |
65.9 (62.5, 69.2) |
58.1* (51.6, 64.6) |
| Arresting and prosecuting doctors who provide prescriptions for pain medication without an appropriate indication | 63.0 (60.0, 66.0) |
65.6 (62.3, 68.9) |
53.6** (47.0, 60.2) |
| Providing naloxone, a medication that can quickly help a person experiencing a life-threatening drug overdose, to friends and family members of people using prescription pain medication | 52.6 (49.5, 55.7) |
51.9 (48.4, 55.4) |
55.0 (48.4, 61.6) |
Respondents who selected 5–7 on the 7-point Likert scale were coded as generally favoring the policy.
Respondents were identified as low volume prescribers if they reported prescribing opioid medications 20 times or less in a typical month.
Respondents were identified as high volume prescribers if they reported prescribing opioid medications more than 20 times in a typical month.
p-value<0.01
p-value<0.05
Chi square tests were used to assess whether proportions differed significantly between high and low volume prescribers.
While there was widespread support for most of the policies among both higher- and lower-volume prescribers, higher-volume providers expressed somewhat lower support for several policies targeting physician practices, including: the integration of PDMPs into current electronic medical records (82% of high volume prescribers vs. 89% of low volume prescribers, p-value=0.02); requiring doctors to complete a physical exam before prescribing opioids to a patient (80% vs. 86%, p-value=0.04); increasing oversight of clinics employing doctors who write a large number of opioid prescriptions (73% vs. 87%, p-value<0.01); developing new guidelines to encourage alternative methods of treating chronic pain (76% vs. 83%, p-value=0.03); requiring doctors to complete continuing medical education to prescribe opioids (58% vs. 66%, p-value=0.03); and arresting and prosecuting doctors who provide these medications without appropriate indication (54% vs. 66%, p-value<0.01).
3.3 Study limitations
This study has several limitations. First, the extent to which our findings can be generalized to PCPs nationwide may be limited. Although we sampled from a large national panel of U.S. physicians, the completion rate was relatively low (29%), a common challenge in physician surveys (Flanigan et al., 2008). Given this limitation, our sample may differ in some respects from the broader population of PCPs practicing in the U.S. Secondly, pediatricians made up about a third of our sample, although they are less likely to prescribe opioids than other PCPs (Volkow et al., 2011). To address this concern, we conducted a sensitivity analysis excluding pediatricians. Nevertheless, understanding pediatrician attitudes as well is important given recent FDA approval of OxyContin for pediatric patients (Food and Drug Administration, 2015). A third limitation involves our inability to account for patient panel size in constructing our measure of higher versus lower volume prescribers, which may not be a precise measure. Future research should explore further how prescribing behavior is related to attitudes surrounding the causes of and policy responses to prescription OUD. Fourth, use of terms like abuse and addiction in the survey questions may have influenced responses to items assessing stigma toward this population. Although prescription OUD is the clinical diagnosis in the Diagnostic and Statistical Manual of Mental Disorders 5th edition (American Psychiatric Association, 2013), we used terms most likely to be familiar to PCPs, who generally have minimal training in substance use disorder detection and treatment.
4. DISCUSSION
Primary care physicians largely attributed prescription OUD to individual factors, but many also recognized the roles of both physicians and other sectors of the health care system in contributing to the problem. Respondents held individuals with prescription OUD and physicians as primarily responsible for addressing this issue. Negative attitudes toward people with prescription OUD were prevalent and perceptions of treatment effectiveness were not as high as might be expected given evidence of the clinical effectiveness of several treatments for opioid addiction (Fiellin et al., 2014, 2001; Mattick et al., 2014, 2009; Schwartz et al., 2013). The most commonly endorsed solutions among physicians were those that monitored or restricted prescribing opioids among potentially at-risk patients and improved physician training and education on treatment of pain and prescription OUD.
Our finding that slightly more than half of physicians identified prescription opioids as an effective treatment option for managing non-cancer chronic pain and reported using these medications to treat chronic pain raises concerns. Evidence of benefit of long-term opioid treatment for chronic pain is lacking ; in contrast, numerous observational studies suggest substantial harms associated with long-term opioid use (Chou et al., 2015; LeResche et al., 2015). In March 2016, the CDC released guidelines for PCPs for prescribing opioids for chronic non-cancer pain (Dowell et al., 2016). These guidelines recommended non-pharmacologic and non-opioid therapies for chronic pain for most patients (Dowell et al., 2016). Future research should assess whether attitudes among PCPs regarding opioid prescribing have changed following the release of these guidelines.
Physicians expressed the highest levels of endorsement of individual-oriented causes of prescription OUD. Although majorities of respondents endorsed several physician-oriented causes as well, endorsement levels were generally lower than endorsement of the individual-oriented causal attributions. Of note, only about half of respondents endorsed pharmaceutical industry-oriented causes, despite the significant role that the industry played in changing opioid prescribing practices in the 1990s, findings of criminal wrongdoing, and Senate investigations into the role of the industry in patient advocacy groups and medical societies (U.S. Senate Committee on Finance, 2012; Zee, 2009). These patterns suggest physicians may be unaware of these events or place greater emphasis on individual over structural factors in understanding this problem.
In general, lower- and higher-volume prescribers viewed the causes of the problem similarly. However, for several physician-oriented causes, endorsement was significantly lower among higher-volume prescribers than among lower-volume prescribers. A sensitivity analysis using a higher threshold to identify higher-volume prescribers (prescribing opioid medications more than 30 times per month) produced qualitatively similar results. The differences in causal beliefs among these groups are relatively small in magnitude. However, in combination with significant differences in support for several proposed policies targeting physicians (e.g., increasing oversight over physicians prescribing large numbers of opioids), these patterns suggest that higher-volume prescribers may be less amenable to efforts to alter physicians’ opioid prescribing practices perhaps because they view physician-related causes as less important contributors to the opioid epidemic. Future research might examine what strategies are most effective in changing attitudes and opioid prescribing practices among physicians, particularly the subgroup that prescribes higher volumes of opioid medications.
A larger proportion of respondents viewed physicians as holding responsibility for addressing the prescription opioid problem compared to other entities, like the government, health insurance companies and pharmaceutical companies. However, the largest proportion identified individuals with prescription OUD as responsible, likely reflecting a perception of prescription OUD as attributable to controllable factors resolvable through individual initiative and exercise of self-control (Weiner, 2006). At the same time, physicians clearly see their profession as playing an important role in addressing the problem.
We found that larger proportions of physicians in our survey expressed negative attitudes toward people with prescription OUD than has the general public, according to a nationally representative survey conducted on this topic in early 2014 (Barry et al, 2016; Kennedy-Hendricks et al, Under Review). Although research in this area is limited, prior work suggests that provider stigma toward patients with substance use disorders may result in lower quality care, poorer outcomes, and reduced connection to treatment services (Van Boekel et al., 2013). Lack of knowledge of effective treatment options for prescription opioid addiction may be one factor contributing to negative perceptions. More research is needed to identify effective strategies to reduce stigma among health care providers toward individuals with OUD (Livingston et al., 2012) and to assess whether improved education on evidence-based treatments for OUD reduces stigma.
In terms of policy support, respondents generally favored solutions that allowed for better identification and stricter monitoring of patients prescribed opioids, as well as improved medical training. The former category included policies such as PDMPs and their integration into current electronic medical record systems, verification of patient identification at pharmacies, programs that require Medicaid enrollees suspected of problematic use to have a single prescriber and pharmacy, and arresting and prosecuting patients obtaining opioid prescriptions from multiple doctors. However, physicians also expressed substantial support for improving education and training for clinicians in both addiction and chronic pain treatment. Although support was lower for harm reduction approaches, such as broader distribution of naloxone to family and friends of those prescribed opioids and immunity laws that protect people seeking help for an overdose from being charged with drug crimes, a larger proportion of physicians expressed support for naloxone distribution than has the general public, among which only 40 percent expressed support (Barry et al., 2016). A recent CDC report on overdose prevention programs involving naloxone found that the large majority of opioid overdose reversals using naloxone were heroin overdoses rather than prescription opioid overdoses despite the fact that these medications account for a larger proportion of drug overdose deaths than heroin (Wheeler et al., 2015). Research has found several messaging strategies to be effective in increasing public support for expanding naloxone distribution (Bachhuber et al., 2015) but the persuasive power of these messages has not been tested among physicians.
While contributing to our understanding of PCP attitudes and beliefs surrounding the prescription opioid epidemic, this study also raises additional questions. Understanding how attitudes vary among PCPs from different geographic regions of practice and with varying years of experience and levels of comfort treating patients with OUD would be informative to the development of interventions targeting PCPs. Future studies should evaluate the effectiveness of communication strategies designed to alter opioid prescribing practices, reduce provider stigma, and increase support for promising policy interventions to address prescription OUD. Research is also needed to assess how physician advocacy may be leveraged more effectively to advance evidence-based policy interventions.
Given that physicians expressed strong support for a number of policies recommended by expert bodies, their substantial political influence as a constituency (Morone and Ehlke, 2013) might be effectively leveraged toward advancing public health efforts to curb the opioid crisis. Such widespread support might be particularly useful in efforts to enhance training and education to improve physician capacity to respond to prescription OUD and chronic pain.
Supplementary Material
Highlights.
Respondents strongly supported requiring training on addiction and pain treatment.
Respondents expressed strong support for programs to monitor at-risk opioid users.
Negative attitudes toward people with prescription opioid addiction were prevalent.
The majority thought that addiction treatment options were effective and available.
Acknowledgments
Role of Funding Source
This research was supported by a grant from the National Institute for Drug Abuse (NIDA R01 DA026414) and an unrestricted research grant from AIG, Inc. (114061). The funders had no role in the study design, analysis, interpretation, or preparation of this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
Contributors
A Kennedy-Hendricks, SH Busch, EE McGinty, MA Bachhuber, J Niederdeppe, SE Gollust, DW Webster, DA Fiellin, and CL Barry all conceived the study, designed the survey, contributed to the analysis of the data, interpreted the results, critically reviewed the manuscript and approved the final version as submitted. AKH drafted the manuscript.
Conflict of Interest
Dr. Fiellin has received honoraria from Pinney Associates for serving on an external advisory board monitoring the diversion and abuse of buprenorphine. The other authors have no conflicts of interest to declare.
References
- Alexander CG, Frattaroli S, Gielen AC. The Prescription Opioid Epidemic: An Evidence-Based Approach. The Johns Hopkins University School of Public Health; Baltimore, MD: 2015. [Google Scholar]
- American Medical Association (AMA) Issue Brief: Rx Drug Abuse And Diversion. Washington, DC: 2013. [Google Scholar]
- American Psychiatric Association. Diagnostic And Statistical Manual Of Mental Disorders. 5th. Washington, DC: 2013. [Google Scholar]
- Bachhuber MA, McGinty EE, Kennedy-Hendricks A, Niederdeppe J, Barry CL. Messaging to increase public support for naloxone distribution policies in the United States: results from a randomized survey experiment. PLoS One. 2015;10:e0130050. doi: 10.1371/journal.pone.0130050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry C, Kennedy-Hendricks A, Gollust S, Niederdeppe J, Webster D, McGinty B. Understanding Americans’ views on opioid pain reliever abuse. Addiction. 2016;111:85–93. doi: 10.1111/add.13077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry CL, McGinty EE, Pescosolido BA, Goldman HH. Stigma, discrimination, treatment effectiveness, and policy: public views about drug addiction and mental illness. Psychiatr Serv. 2014;65:1269–1272. doi: 10.1176/appi.ps.201400140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Policy impact: prescription painkiller overdoses [WWW Document] CDC Natl Cent Inj Prev Control. 2013 URL http://www.cdc.gov/HomeandRecreationalSafety/pdf/PolicyImpact-PrescriptionPainkillerOD.pdf (accessed 4.1.15)
- Chen JH, Humphreys K, Shah NH, Lembke A. Distribution of opioids by different types of Medicare prescribers. JAMA Intern Med. 2015;176:259–261. doi: 10.1001/jamainternmed.2015.6662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou R, Turner J, Devine E, Hansen R, Sullivan S, Blazine I, Dana T, Bougatsos C, Devo R. The effectiveness and risks of long-term opioid therapy for chronic pain: a systematic review for a National Institutes of Health Pathways to Prevention Workshop. Ann Intern Med. 2015;162:276–86. doi: 10.7326/M14-2559. [DOI] [PubMed] [Google Scholar]
- Cicero TJ, Ellis MS, Surratt HL, Kurtz SP. The changing face of heroin use in the United States. JAMA Psychiatry. 2014;71:821–6. doi: 10.1001/jamapsychiatry.2014.366. [DOI] [PubMed] [Google Scholar]
- Compton WM, Jones CM, Baldwin GT. Relationship between nonmedical prescription-opioid use and heroin use. N Engl J Med. 2016;374:154–63. doi: 10.1056/NEJMra1508490. [DOI] [PubMed] [Google Scholar]
- Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain - United States, 2016. MMWR Recomm Rep. 2016;65:1–49. doi: 10.15585/mmwr.rr6501e1. [DOI] [PubMed] [Google Scholar]
- Edlund M, Martin B, Russo J, DeVries A, Braden J, Sullivan M. The role of opioid prescription in incident opioid abuse and dependence among individuals with chronic noncancer pain: the role of opioid prescription. Clin J Pain. 2014;30:557–64. doi: 10.1097/AJP.0000000000000021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiellin DA, O’Connor P, Chawarski M, Pakes J, Pantalon M, Schottenfeld R. Methadone maintenance in primary care: a randomized controlled trial. JAMA. 2001;286:1724–31. doi: 10.1001/jama.286.14.1724. [DOI] [PubMed] [Google Scholar]
- Fiellin DA, Schottenfeld R, Cutter C, Moore B, Barry D, O’Connor P. Primary care-based buprenorphine taper vs maintenance therapy for prescription opioid dependence: a randomized clinical trial. JAMA Intern Med. 2014;174:1947–54. doi: 10.1001/jamainternmed.2014.5302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flanigan T, McFarlane E, Cook S. Conducting survey research among physicians and other medical professionals: a review of current literature. ASA Proc Sect Surv Res Methods. 2008:4136–47. [Google Scholar]
- Food and Drug Administration (FDA) Pediatric pain management options [WWW Document] Cent Drug Eval Res Conversation FDA website. 2015 URL http://www.fda.gov/drugs/newsevents/ucm456973.htm (accessed 11.20.15)
- GfK KnowledgeNetworks. Physicians Consulting Network (PCN(R)) [WWW Document] GfK website. 2015 URL http://www.knowledgenetworks.com/resources/pcn.html (accessed 7.15.15)
- Gilkey MB, Malo TL, Shah PD, Hall ME, Brewer NT. Quality of physician communication about human papillomavirus vaccine: findings from a national survey. Cancer Epidemiol Biomarkers Prev. 2015;24:1673–1679. doi: 10.1158/1055-9965.EPI-15-0326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilkey MB, Moss JL, Coyne-Beasley T, Hall ME, Shaw PD, Brewer NT. Physician communication about adolescent vaccination: how is human papillomavirus vaccine different? Prev Med. 2015;77:181–185. doi: 10.1016/j.ypmed.2015.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han B, Compton WM, Jones CM, Cai R. Nonmedical prescription opioid use and use disorders among adults aged 18 through 64 years in the United States, 2003–2013. JAMA. 2015;314:1468–1478. doi: 10.1001/jama.2015.11859. [DOI] [PubMed] [Google Scholar]
- Hwang CS, Turner LW, Kruszewski SP, Kolodny A, Alexander GC. Primary care physicians’ knowledge and attitudes regarding prescription opioid abuse and diversion. Clin J Pain. 2015a;1 doi: 10.1097/AJP.0000000000000268. [DOI] [PubMed] [Google Scholar]
- Hwang CS, Turner LW, Kruszewski SP, Kolodny A, Alexander GC. Prescription drug abuse: a national survey of primary care physicians. JAMA Intern Med. 2015b;175:302–204. doi: 10.1001/jamainternmed.2014.6403. Author. [DOI] [PubMed] [Google Scholar]
- Jamison R, Sheehan K, Scanlan E, Matthews M, Ross E. Beliefs and attitudes about opioid prescribing and chronic pain management: survey of primary care providers. J Opioid Manag. 2014;10:375–82. doi: 10.5055/jom.2014.0234. [DOI] [PubMed] [Google Scholar]
- Kennedy-Hendricks A, McGinty EE, Gollust S, Chisolm M, Ensminger M, Barry CL. How is social stigma toward individuals with prescription opioid use disorder associated with public support for punitive and public health-oriented policies? Paper currently under review. doi: 10.1176/appi.ps.201600056. [DOI] [PubMed] [Google Scholar]
- Kolodny A, Courtwright DT, Hwang CS, Kreiner P, Eadie JL, Clark TW, Alexander GC. The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annu Rev Public Health. 2015;36:1–25. doi: 10.1146/annurev-publhealth-031914-122957. [DOI] [PubMed] [Google Scholar]
- LeResche L, Saunders K, Dublin S, Thielke S, Merrill JO, Shortreed SM, Campbell C, Von Korff MR. Sex and age differences in global pain status among patients using opioids long term for chronic noncancer pain. J Women’s Health. 2015;24:629–635. doi: 10.1089/jwh.2015.5222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy B, Paulozzi L, Mack K a, Jones CM. Trends in opioid analgesic–prescribing rates by specialty, U.S., 2007–2012. Am J Prev Med. 2015:1–5. doi: 10.1016/j.amepre.2015.02.020. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, Yang LH, Phelan JC, Collins PY. Measuring mental illness stigma. Schizophr Bull. 2004;30:511–541. doi: 10.1093/oxfordjournals.schbul.a007098. [DOI] [PubMed] [Google Scholar]
- Livingston JD, Milne T, Fang ML, Amari E. The effectiveness of interventions for reducing stigma related to substance use disorders: a systematic review. Addiction. 2012;107:39–50. doi: 10.1111/j.1360-0443.2011.03601.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macerollo A, Mack D, Oza R, Bennett I, Wallace L. Academic family medicine physicians’ confidence and comfort with opioid analgesic prescribing for patients with chronic nonmalignant pain. J Opioid Manage. 2014;10:255–61. doi: 10.5055/jom.2014.0213. [DOI] [PubMed] [Google Scholar]
- Mattick R, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev. 2014:CD002207. doi: 10.1002/14651858.CD002207.pub4. [DOI] [PubMed] [Google Scholar]
- Mattick R, Breen C, Kimber J, Davoli M. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst Rev. 2009:CD002209. doi: 10.1002/14651858.CD002209.pub2. [DOI] [PubMed] [Google Scholar]
- Maurer J, Harris KM. Issuance of patient reminders for influenza vaccination by US-based primary care physicians during the first year of universal influenza vaccination recommendations. Am J Public Health. 2014;104:e60–2. doi: 10.2105/AJPH.2014.301888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinty EE, Goldman HH, Pescosolido B, Barry CL. Portraying mental illness and drug addiction as treatable health conditions: effects of a randomized experiment on stigma and discrimination. Soc Sci Med. 2015;126:73–85. doi: 10.1016/j.socscimed.2014.12.010. [DOI] [PubMed] [Google Scholar]
- Mendes E. Americans’ concerns about obesity soar, surpass smoking. Gallup News 2012 [Google Scholar]
- Morone JA, Ehlke D. Health Politics and Policy. 5th. Cengage Learning; Stamford, CT: 2013. [Google Scholar]
- National Center for Health Statistics. Number and age-adjusted rates of drug-poisoning deaths involving opioid analgesics and heroin: United States, 2000–2014. 2015 [ http://www.cdc.gov/nchs/data/health_policy/AADR_drug_poisoning_involving_OA_Heroin_US_2000–2014.pdf (accessed 7.1.16)
- Office of National Drug Control Policy (ONDCP) 2013 National Drug Control Strategy (NDCS) 2013 URL http://www.whitehouse.gov/ondcp/national-drug-control-strategy (accessed 4.1.15)
- Pescosolido B, Martin J, Long J, Medina T, Phelan J, Link B. A disease like any other? A decade of change in public reactions to schizophrenia, depression, and alcohol dependence. Am J Psychiatry. 2010;167:1321–1330. doi: 10.1176/appi.ajp.2010.09121743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd RA, Paulozzi LJ, Bauer MJ, Burleson RW, Carlson RE, Dao D, Davis JW, Dudek J, Eichler BA, Fernandes JC. Increases in Heroin Overdose Deaths — 28 States, 2010 to 2012. MMWR. 2014;63:849–854. [PMC free article] [PubMed] [Google Scholar]
- Schwartz RP, Gryczynsi J, O’Grady KE, Sharfstein JM, Warren G, Olsen Y, Mitchell SG, Jaffe JH. Opioid agonist treatments and heroin overdose deaths in Baltimore, Maryland, 1995–2009. Am J Public Health. 2013;103:917–922. doi: 10.2105/AJPH.2012.301049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp, editor. StataCorp. Stata Statistical Software: Release 12. College Station, TX: 2011. [Google Scholar]
- The U.S. Senate Committee on Finance. Baucus, Grassley seek answers about opioid manufacturers’ ties to medical groups. Press Release; 2012. URL http://www.finance.senate.gov/newsroom/chairman/release/?id=021c94cd-b93e-4e4e-bcf4-7f4b9fae0047 (accessed 8.7.15) [Google Scholar]
- Thompson T, Benz J, Agiesta J, Brewer KH, Bye L. Obesity in the United States: Public perceptions. The Associated Press - NORC Center for Public Research; Washington, DC: 2013. [Google Scholar]
- Trust for America’s Health. Prescription Drug Abuse: Strategies To Stop The Epidemic, 2013. Trust For America’s Health Report; Washington, DC: 2013. [Google Scholar]
- Turk D, Dansie E, Wilson H, Moskovitz B, Kim M. Physicians’ beliefs and likelihood of prescribing opioid tamper-resistant formulations for chronic noncancer pain patients. Pain Med. 2014;15:625–36. doi: 10.1111/pme.12352. [DOI] [PubMed] [Google Scholar]
- Van Boekel LC, Brouwers EPM, Van Weeghel J, Garretsen HFL. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: dystematic review. Drug Alcohol Depend. 2013;131:23–35. doi: 10.1016/j.drugalcdep.2013.02.018. [DOI] [PubMed] [Google Scholar]
- Volkow ND, McLellan TA, Cotto JH, Karithanom M, Weiss SRB. Characteristics of opioid prescriptions in 2009. JAMA. 2011;305:1299–1301. doi: 10.1001/jama.2011.401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner B. Social Motivation, Justice, And Themoral Emotions: An Attributional Approach. Lawrence Erlbaum; Mahwah, NJ: 2006. [Google Scholar]
- Wheeler E, Jones TS, Gilbert MK, Davidson PJ. Opioid overdose prevention programs providing naloxone to laypersons – United States, 2014. MMWR. 2015;64:631–635. [PMC free article] [PubMed] [Google Scholar]
- Wolfert MZ, Gilson AM, Dahl JL, Cleary JF. Opioid analgesics for pain control: Wisconsin physicians’ knowledge, beliefs, attitudes, and prescribing practices. Pain Med. 2010;11:425–434. doi: 10.1111/j.1526-4637.2009.00761.x. [DOI] [PubMed] [Google Scholar]
- Van Zee A. The promotion and marketing of OxyContin: commercial triump, public health tragedy. Am J Public Health. 2009;99:221–227. doi: 10.2105/AJPH.2007.131714. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


