Abstract
Background: Delivering specialty care remotely directly into people's homes can enhance access for and improve the healthcare of individuals with chronic conditions. However, evidence supporting this approach is limited. Materials and Methods: Connect.Parkinson is a randomized comparative effectiveness study that compares usual care of individuals with Parkinson's disease in the community with usual care augmented by virtual house calls with a Parkinson's disease specialist from 1 of 18 centers nationally. Individuals in the intervention arm receive four virtual visits from a Parkinson's disease specialist over 1 year via secure, Web-based videoconferencing directly into their homes. All study activities, including recruitment, enrollment, and assessments, are conducted remotely. Here we report on interest, feasibility, and barriers to enrollment in this ongoing study. Results: During recruitment, 11,734 individuals visited the study's Web site, and 927 unique individuals submitted electronic interest forms. Two hundred ten individuals from 18 states enrolled in the study from March 2014 to June 2015, and 195 were randomized. Most participants were white (96%) and college educated (73%). Of the randomized participants, 73% had seen a Parkinson's disease specialist within the previous year. Conclusions: Among individuals with Parkinson's disease, national interest in receiving remote specialty care directly into the home is high. Remote enrollment in this care model is feasible but is likely affected by differential access to the Internet.
Key words: : chronic conditions, home healthcare, Parkinson's disease, randomized controlled trial, specialists, telemedicine, videoconferencing, access to care
Introduction
Chronic medical conditions affect over 140 million Americans, account for 85% of healthcare expenditures,1 and are now the leading causes of disability and death globally.2,3 Access to care for individuals affected by chronic conditions is limited by distance, disability, the distribution of doctors, and other socioeconomic factors. Telemedicine has the potential to reach these individuals directly in their homes. Virtual house calls using simple, secure videoconferencing could represent the next-generation house call.
Although many studies have evaluated telemedicine for chronic conditions, few have examined videoconferencing, and even fewer have examined videoconferencing into the home. A 2012 review by Wootton4 found 141 randomized controlled trials of telemedicine interventions for chronic conditions. However, most studies evaluated remote, generally asynchronous (e.g., text messages) monitoring or telephone support. Ten evaluated videoconferencing, but most were conducted in clinics. A subsequent literature search5 found only six randomized controlled studies evaluating video visits directly into the home. With the exception of one multicenter spinal cord injury study,6 most studies have been single center, short, and small. Despite this limited evidence base, interest in virtual house calls is rising rapidly for many conditions.7–10
Parkinson's disease is a prototypical chronic condition. Its incidence increases with age,11 and its burden will double over the next generation.12 Individuals have Parkinson's disease for approximately 14–16 years after diagnosis,13,14 and it leads to progressive disability, cognitive impairment, limited mobility,15 and impaired driving ability.16 Parkinson's disease also burdens caregivers,17 frequently requires institutional care,18–20 generates high healthcare costs,21,22 and benefits from specialty care.23–26 However, over 40% of Medicare beneficiaries with Parkinson's disease do not receive care from a neurologist within the first 4 years after diagnosis,26 and those who do not have worse health outcomes, including a 22% increased risk of death within 6 years.26
Because many motor features (e.g., tremor, bradykinesia, gait changes) are assessed visually27 and many nonmotor aspects (e.g., depression) are assessed by history, Parkinson's disease is well suited to remote assessment. Initial telemedicine applications began over 20 years ago28 and have increased since then.29 A 6-month randomized pilot study of 20 individuals demonstrated that video visits into the home were feasible, could produce comparable outcomes to traditional in-person care, and saved patients and their caregivers 3 hours of time and 100 miles of travel per visit.24 However, national, large-scale studies of virtual house calls are lacking for Parkinson's disease and other chronic conditions. To that end, we are conducting such a multicenter study and here report baseline data, as well as interest, feasibility, and barriers to enrollment.
Materials and Methods
Trial Design
We are conducting a 12-month, multicenter national randomized comparative effectiveness study (Connect.Parkinson) comparing usual care in the community to usual care augmented by four virtual house calls from a remote Parkinson's disease specialist into participants' homes. The protocol details have been previously published.5 The study was designed to enroll 200 individuals with Parkinson's disease and their care partners and has four specific aims: (1) to demonstrate the feasibility of using virtual house calls to deliver specialty care into the homes of individuals with Parkinson's disease who have limited access to care; (2) to show that such an approach can improve participants' quality of life; (3) to establish that telemedicine can enhance the quality of care received by participants; and (4) to demonstrate that this remote approach to care can save time, reduce travel, and decrease caregiver burden. The study was approved by the institutional review boards of the University of Rochester (coordinating center) and of the participating sites.
Participants
Eligible study participants are individuals with clinically diagnosed Parkinson's disease who have access to a nonpublic, Internet-enabled device with the capacity for videoconferencing and who are physically located in a state where a participating site investigator is licensed to practice medicine. Care partners, whose participation is optional, are family members or friends who provide regular, unpaid assistance with daily activities.
Recruitment and Enrollment
Recruitment for the study began in February 2014 and included efforts directed at patients and physicians. Based on previous research,26 we identified counties in states where we had licensed specialists and where a majority of Medicare beneficiaries with Parkinson's disease do not currently see a neurologist. We targeted those counties using Google AdWords keyed to searches related to Parkinson's disease and through phone, mail, e-mail, and personal contacts to support groups and primary care providers. We also reached out to the Parkinson's community more broadly, announcing the study through electronic communications from the National Parkinson Foundation, a patient social networking site (PatientsLikeMe), and a posting in Fox Trial Finder (Michael J. Fox Foundation).
Interested participants were directed to a 1-page Web site (http://connect.parkinson.org/) where individuals could complete an online form to register interest in participating in the study. In addition, interested individuals could contact the National Parkinson Foundation PD Helpline (800.4PD.INFO). The study team at the coordinating center then contacted interested individuals by phone to assess eligibility and begin the enrollment process. We initially prioritized enrollment of individuals who either came from an underserved region or were not seeing a neurologist.
Intervention
All participants received an e-mail link to secure, Health Insurance Portability and Accountability Act–compliant virtual visit software from SBR Health (Cambridge, MA) that embeds videoconferencing software from Vidyo (Hackensack, NJ) and is hosted by ID Solutions (Indianapolis, IN). Participants who did not have a Web camera received one (Creative Labs Live! Cam Chat HD camera; Creative Technology Ltd., Singapore) by mail. A study coordinator performed a test connection with participants prior to study visits and provided technical support by phone. No in-person support was provided.
All participants receive a baseline and end of study virtual visit with an independent rater. Those in the intervention arm are scheduled to receive four virtual visits over 1 year from a Parkinson's disease specialist. The exact content of each visit is determined by the clinician and patient but generally consists of a history, Parkinson's disease–focused examination,23 addressing the patient's questions or concerns, and providing recommendations. Previous studies have demonstrated the reliability of remote clinical evaluation for Parkinson's disease in comparison with that of personal care.23,30 Due to state law differences on prescribing medications remotely,31 these recommendations, including medication changes (if indicated), are then mailed to the patient and the patient's local providers, who were notified at the study's outset of their patient's study participation, for implementation. Those randomized to their usual care in the community receive one video visit with a Parkinson's disease specialist after the 12-month visit with the independent rater.
Outcomes
The primary outcomes are feasibility, defined as the percentage of telemedicine participants who complete at least one telemedicine visit and the overall percentage of completed telemedicine visits, and efficacy, as measured by the change in the Parkinson's Disease Questionnaire 39, a widely used Parkinson's disease–specific quality of life measure.32 Secondary outcomes include quality of care as measured by the change in the Patient Assessment of Chronic Illness Care,33 time and travel savings, and change in caregiver burden as measured by the Multidimensional Caregiver Strain Index.34
Sample Size
The sample size of 200 participants was selected to ensure adequate power of at least 80% to detect a moderate effect size on the quality of life measure, allowing for a 20% dropout rate.
Results
Enrollment
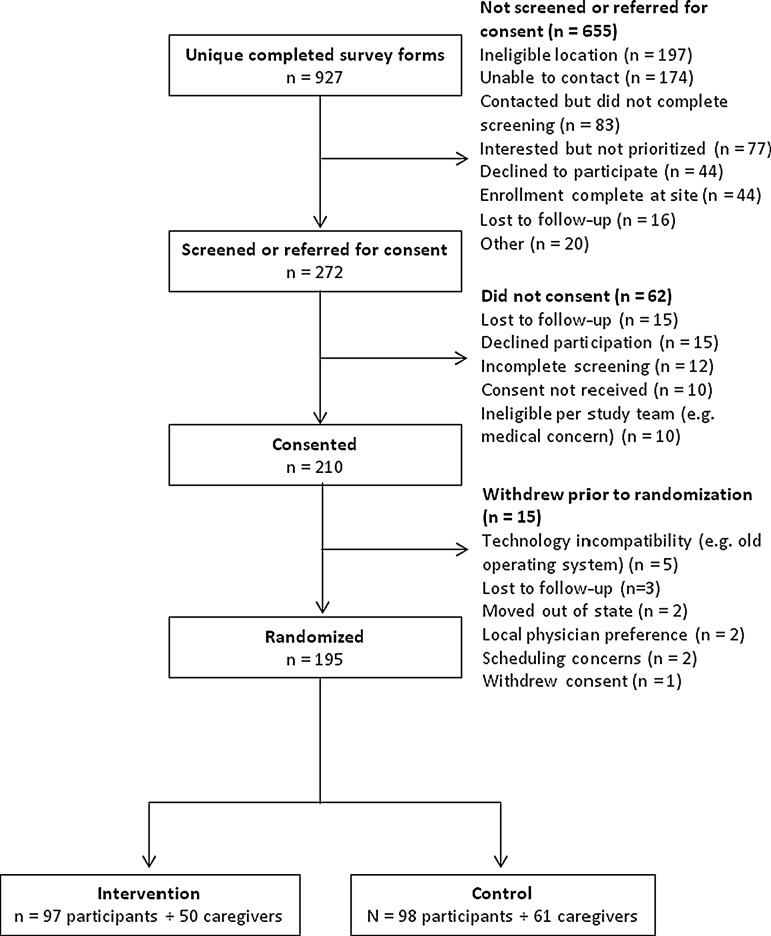
From February 1, 2014 to August 25, 2015, 11,734 individuals from 50 states and 80 countries visited the 1-page study Web site. Of these, 1,704 (15%) clicked through to the study interest form, and 927 (8%) completed it (Fig. 1). Most forms (79%) came from individuals in eligible states. Because initial interest was high, individuals who were not seeing a Parkinson's disease specialist were prioritized to the exclusion of others (n = 77), and 44 were excluded because enrollment was complete in their state's site. Ultimately, 272 individuals were referred to 18 research sites for consent, 210 enrolled in the study, and 195 were randomized. As shown in Table 1, most participants learned about the study from the National Parkinson Foundation Web site (n = 339), PatientsLikeMe (n = 204), and Fox Trial Finder (n = 132).
Fig. 1.
Flowchart of study participants.
Table 1.
Referral Sources of Interested Participants
| NUMBER OF REFERRAL RESPONSES (N = 1,058)a | |
|---|---|
| National Parkinson Foundation Web site | 339 (36.6%) |
| PatientsLikeMe | 204 (22.0%) |
| Michael J. Fox Foundation's Fox Trial Finder | 132 (14.2%) |
| 93 (10.0%) | |
| Parkinson's disease support group | 67 (7.2%) |
| Referral by friend or family | 43 (4.6%) |
| National Parkinson Foundation print media | 37 (4.0%) |
| Google advertisement | 18 (1.9%) |
| ClinicalTrials.gov | 18 (1.9%) |
| Other healthcare provider | 12 (1.3%) |
| Other social networking site | 9 (1.0%) |
| Primary care provider | 3 (0.3%) |
| 2 (0.2%) | |
| Other | 81 (8.7%) |
The 927 participants provided 1,058 referral sources. Because participants could indicate multiple referral sources, percentages add up to more than 100%.
Study Population
Table 2 summarizes the baseline characteristics of the study population that underwent randomization. Fifteen individuals withdrew prior to randomization, which occurred after a baseline visit with an independent rater. The most common reasons for withdrawal were technological incompatibility (e.g., old operating system) and losses to follow-up (Fig. 1). The characteristics of those who withdrew (data not shown) were similar to those who were randomized. Most study participants are white (96%) and college educated (73%), with a mean age of 66 years and average Parkinson's disease duration of 8 years. At baseline, their mean Parkinson's disease–specific quality of life scores are relatively low, indicating mild perceived impairment. Participants' mean scores on the Patient Assessment of Chronic Illness Care are comparable to what has been observed in other chronic disease populations. Of our participants, 96% use the Internet or e-mail at home, and 54% have used their computer to participate in a video call. In the 12 months prior to enrollment, only 3% had not seen either a general neurologist or a Parkinson's disease specialist. However, 55% of participants come from a U.S. county in which fewer than 55% of Medicare beneficiaries with Parkinson's disease receive neurological care. Participants travel on average 52 miles each way to receive Parkinson's disease care.
Table 2.
Baseline Characteristics of Randomized Study Participants
| ALL RANDOMIZED PARTICIPANTS (N = 195) | |
|---|---|
| Women [n (%)] | 91 (46.7) |
| Age (years) as of screening | 66.4 (8.1) |
| Bachelor's degree or higher education [n (%)] | 143 (73.3) |
| Ethnicity [n (%)] | |
| Hispanic/Latino | 3 (1.5) |
| Not Hispanic/Latino | 183 (93.9) |
| Prefer not to answer/unknown | 9 (4.6) |
| Race [n (%)] | |
| White | 187 (95.9) |
| Other | 3 (1.5) |
| Did not answer/unknown | 5 (2.6) |
| Presently married [n (%)] | 151 (77.4) |
| Participants who use the Internet or e-mail at home [n (%)] | 187 (95.9) |
| Participants who have ever used the Internet to look for health or medical information online [n (%)] | 189 (96.9) |
| Participants who have ever used their desktop or laptop computer to participate in a video call or video chat [n (%)] | 105 (53.8) |
| Parkinson's disease duration (years) (n = 185) | 8.0 (5.6) |
| Movement Disorder Society Unified Parkinson's Disease Rating Scale | |
| Part 1A (scale of 0–24)a | 4.6 (3.8) |
| Part 1B (scale of 0–28)a | 10.3 (4.4) |
| Part 2 (n = 194) (scale of 0–52)a | 14.7 (7.6) |
| Part 3 (scale of 0–64)a,b | 28.9 (10.0) |
| Part 4 (n = 194) (scale of 0–24)a | 4.5 (4.8) |
| Montreal Cognitive Assessment Score (scale of 0–30)c | 26.2 (2.8) |
| Parkinson's Disease Questionnaire 39 total score (n = 177) (scale of 0–100)a | 25.4 (13.9) |
| EuroQol 5D (scale of 0–1)c | 0.8 (0.1) |
| Geriatric Depression Scale 15 (n = 190) (scale of 0–15)a | 4.1 (3.2) |
| Patient Assessment of Chronic Illness Care composite score (n = 182) (scale of 1–5)c | 2.4 (0.9) |
| Participants who have seen a general neurologist for Parkinson's disease in the last 12 months [n (%)] | 85 (43.6) |
| Participants who have seen a Parkinson's disease specialist for their Parkinson's disease in the last 12 months [n (%)] | 143 (73.3) |
Data are mean (standard deviation) unless otherwise noted. The number of responses is 195 unless otherwise noted.
Higher scores indicate greater disability.
Excludes “rigidity” and “postural stability” fields.
Lower scores indicate greater disability/dissatisfaction.
Table 3 summarizes the baseline characteristics of the participating caregivers. Like the participants with Parkinson's disease, most are white (79%) and college educated (55%).
Table 3.
Baseline Characteristics of the Participating Care Partners of Randomized Participants
| CARE PARTNERS OF RANDOMIZED PARTICIPANTS (N = 111) | |
|---|---|
| Women [n (%)] | 67 (60.4) |
| Age (years) | 64.6 (9.2) |
| Bachelor's degree or higher education [n (%)] | 61 (55) |
| Ethnicity [n (%)] | |
| Hispanic/Latino | 1 (0.9) |
| Not Hispanic/Latino | 92 (82.9) |
| Prefer not to answer/unknown | 18 (16.2) |
| Race [n (%)] | |
| White | 88 (79.3) |
| Other | 7 (6.3) |
| Prefer not to answer/unknown | 16 (14.4) |
| Relationship to participant [n (%)] | |
| Spouse/partner | 73 (65.8) |
| Child/grandchild | 4 (3.6) |
| Other family | 1 (0.9) |
| Friend | 1 (0.9) |
| No response | 32 (28.8) |
| Multidimensional Caregiver Strain Index Score (n = 80) (scale of 0–26)a | 11.6 (9.5) |
Data are mean (standard deviation) values unless otherwise noted.
Higher scores indicate higher amounts of strain for caregiver.
Remote Assessments
At baseline, 177 (91%) of the 195 randomized individuals completed all 39 questions of the Parkinson's Disease Questionnaire 39. Of those who did not, 11 failed to complete one question, 5 failed to complete two questions, and 1 failed to complete three questions. Similarly, 180 (92%) provided responses to all questions of the Patient Assessment of Chronic Illness Care. Among care partners, 111 were randomized with the participants, and 72% answered all questions of the Multidimensional Caregiver Strain Index.
Discussion
Interest and enrollment in this national randomized controlled trial of virtual house calls suggest that latent demand for this care model is high and that remote recruitment and enrollment may be feasible. However, although the study reached those in geographically underserved areas, it did not reach those who are not seeing a specialist.
Over 10,000 individuals from all over the world visited the 1-page study Web site, and almost 1,000 individuals with Parkinson's disease expressed interest in participating in this study. This large latent demand for virtual visits, which initially surpassed our capacity to respond in a timely manner, is consistent with the experience of Kaiser Permanente of Northern California35 and the Department of Veterans Affairs,36 which have experienced large and rapid adoption of their various virtual visit models.
The principal driver of this interest may be convenience,25,37 as most study participants are currently seeing a neurologist. For older individuals who generally live in suburban and rural areas, have limited mobility, impaired driving ability, and overburdened caregivers, receiving convenient, patient-centered care may be critical.
Enrollment also demonstrated the feasibility of entirely remote participation in research studies, at least through the initial phase. Nationwide recruitment, consent, enrollment, and completion of assessments were all completed by individuals with Parkinson's disease and their care partners without the need or potential benefit of an in-person encounter. Other clinical studies that have used remote approaches to evaluate therapeutics have demonstrated the feasibility of such an approach.38–43 That said, contacting many individuals was difficult because of telephone blocking services, absence of a prior relationship, and incomplete information provided. The inclusion of data checks to identify any missing responses would likely have reduced inadvertent omissions in sometimes lengthy forms and surveys.
Recruitment and enrollment in this study demonstrated the ability to address geographic but not socioeconomic barriers to care. Over half of the study participants come from counties with limited access to neurological care. Importantly, despite efforts to reach those who are not receiving care from a neurologist, the vast majority of study participants are seeing a neurologist. The characteristics of those with Parkinson's disease with the least access to care—older, rural dwelling, women, for example26—are very similar to the characteristics seen in those with the least access to the Internet and broadband.44,45 Although broadband access is increasing,46,47 recruitment and enrollment in this study were likely affected by the Digital Divide48—the difference in information between those who have access to the Internet and those who do not.49 Internet access among individuals with chronic conditions is less than that of those without chronic conditions (72% versus 89%).50,51 Participants in this study demonstrate higher usage of the Internet (96%) than the general population of adults (87%) and much higher usage than adults 65 years of age or older (57%).52 The impact of the well-connected nature of this study population remains to be determined. Beyond increasing access to the Internet, future efforts will have to develop alternative approaches that likely rely on in-person contact,53 such as outreach to local support groups and community leaders, to reach the most underserved.
Beyond the Digital Divide, the study encountered additional barriers that slowed enrollment. Despite great interest, enrollment in the study took 13 months, principally due to the need for review and approval of the protocol by each site's institutional review board. The limitations of local institutional review board review in multicenter studies,54–56 as well as the benefits of central institutional review boards, have been well documented.57–61 The other principal source of delay was the requirement for hand-signed consent forms, which could be addressed by adopting the electronic signatures that are increasingly used in clinical trials.38
Beyond this study, virtual house calls face additional policy barriers, especially licensure and reimbursement. Because state medical licensing boards generally require that a physician be licensed in the state where the patient is physically located when services are rendered, we had to exclude nearly 200 individuals from participation simply because they lived in the “wrong” state. The Federation of State Medical Boards recently drafted a framework for an Interstate Medical Licensure Compact to enable expedited licensure in multiple states;62 however, the speed at which such change will occur is questioned.63 Last year, Congress reintroduced the TELE-MED Act, which would enable Medicare providers, like those in the Department of Veterans Affairs, who are licensed in one state to provide telemedicine services to Medicare beneficiaries in a different state.64,65
The second major barrier is reimbursement. Fueled by state parity laws,66,67 private insurers are increasingly reimbursing for telemedicine services, but Medicare is lagging. In 2012, Medicare spent approximately $5 million on telemedicine-related expenditures,68 which was less than 0.001% of its total expenditures.69 Moreover, Medicare provides no coverage of virtual house calls70 and continues to incent institutional care over community-based care.71 In organizations where licensure and reimbursement barriers have been addressed (e.g., Kaiser Permanente, the Department of Veterans Affairs), adoption of virtual visits has been rapid and welcomed.
In addition to difficulty enrolling a diverse population, this study has several limitations. The first is that it is almost exclusively focused on delivering care from a single specialist to an individual with a single chronic condition. Multidisciplinary care72 delivered remotely could offer potentially greater benefits. For example, remote delivery of speech therapy73 has already been found to be clinically valid and reliable in Parkinson's disease. Individuals with Parkinson's disease may suffer from multiple comorbidities that require personalized solutions,74 some of which could be delivered remotely by other providers. In addition, almost all study participants had no preexisting relationship with the clinician whom they are seeing remotely. Combining in-person and virtual visits, especially after a diagnosis has been made, may provide additional benefits. Because of variation in state laws and policies,31 the recommendations of the remote specialists in this study are communicated to the local clinician and participant for implementation. Although this may replicate some practices, more direct involvement of the remote specialist could enable more rapid and likely implementation of recommendations. Finally, although this study does not include a cost-effectiveness analysis, more frequent neurologist visits are associated with lower healthcare expenses due to a reduction in Parkinson's disease–related hospitalizations.75
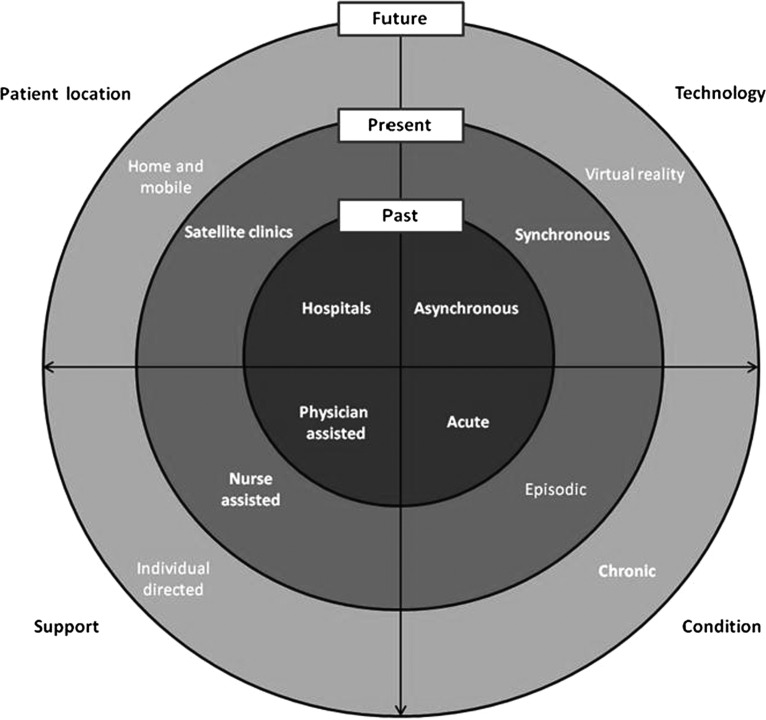
Overall, virtual house calls use technology to drive synchronous delivery of care directly to patients with lifelong conditions in their homes (Fig. 2). Such a model stands in contrast to the current institutional-based care that relies on colocation of a patient and clinician(s), generally in urban centers. Fueled by increasingly inexpensive and available technology, the next generation house call may deliver and increase access to patient-centered care for those with chronic conditions. Hopefully, this study will elucidate the benefits and limitations of this approach.
Fig. 2.
Expanding model of telemedicine care.
Acknowledgments
This research is supported by an award (AD-12-11-4701) from the Patient-Centered Outcomes Research Institute, and the National Parkinson Foundation is collaborating in the conduct of the study. Software used in the study is provided and supported by SBR Health (Cambridge, MA), Vidyo (Hackensack, NJ), and ID Solutions (Indianapolis, IN). The project described in this publication was supported by the University of Rochester CTSA award number UL1 TR000042 from the National Center for Advancing Translational Sciences of the National Institutes of Health. We would also like to thank Dr. David Brailer (Health Evolution Partners), Dr. Robert Kolodner (ViTel Net), Dr. Ruth Schneider (University of Rochester Medical Center), Ms. Kathryn Duderstadt (Struthers Parkinson's Center), Ms. Silvia Vargas-Parra (University of Miami), and Ms. Catherine Wielinski (Struthers Parkinson's Center) for their contributions to the study.
Disclosure Statement
E.R.D. has filed for a patent related to neurology and telemedicine, is an unpaid adviser to SBR Health and Vidyo, and serves on the Medical Advisory Board of and has stock options in Grand Rounds. K.M.B. has filed for a patent related to neurology and telemedicine. The remaining authors declare no conflicts of interest exist.
References
- 1.Anderson G. Chronic care: Making the case for ongoing care. Princeton, NJ: Robert Wood Johnson Foundation, 2010. [Google Scholar]
- 2.Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2095–2128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2163–2196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wootton R. Twenty years of telemedicine in chronic disease management—An evidence synthesis. J Telemed Telecare 2012;18:211–220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Achey MA, Beck CA, Beran DB, et al. Virtual house calls for Parkinson disease (Connect.Parkinson): Study protocol for a randomized, controlled trial. Trials 2014;15:465. [DOI] [PMC free article] [PubMed]
- 6.Dallolio L, Menarini M, China S, et al. Functional and clinical outcomes of telemedicine in patients with spinal cord injury. Arch Phys Med Rehabil 2008;89:2332–2341 [DOI] [PubMed] [Google Scholar]
- 7.Daschle T, Dorsey ER. The return of the house call. Ann Intern Med 2015;162:587–588 [DOI] [PubMed] [Google Scholar]
- 8.Lapowsky I. Video is about to become the way we all visit the doctor. Wired. Available at www.wired.com/2015/04/united-healthcare-telemedicine/ (last accessed August24, 2015)
- 9.Pinsker B. Online doctor visits are set to surge. Time, Inc. Available at http://time.com/money/3994614/online-doctor-visit-increase/ (last accessed August24, 2015)
- 10.Terry K. Physicians and telehealth: Is it time to embrace virtual visits? Medical Economics. Available at http://medicaleconomics.modernmedicine.com/medical-economics/news/physicians-and-telehealth-it-time-embrace-virtual-visits?page=full (last accessed August24, 2015) [PubMed]
- 11.Van Den Eeden SK, Tanner CM, Bernstein AL, et al. Incidence of Parkinson's disease: Variation by age, gender, and race/ethnicity. Am J Epidemiol 2003;157:1015–1022 [DOI] [PubMed] [Google Scholar]
- 12.Dorsey ER, Constantinescu R, Thompson JP, et al. Projected number of people with Parkinson disease in the most populous nations, 2005 through 2030. Neurology 2007;68:384–386 [DOI] [PubMed] [Google Scholar]
- 13.Macleod AD, Taylor KS, Counsell CE. Mortality in Parkinson's disease: A systematic review and meta-analysis. Mov Disord 2014;29:1615–1622 [DOI] [PubMed] [Google Scholar]
- 14.Buter TC, van den Hout A, Matthews FE, Larsen JP, Brayne C, Aarsland D. Dementia and survival in Parkinson disease: A 12-year population study. Neurology 2008;70:1017–1022 [DOI] [PubMed] [Google Scholar]
- 15.Evans JR, Mason SL, Williams-Gray CH, et al. The natural history of treated Parkinson's disease in an incident, community based cohort. J Neurol Neurosurg Psychiatry 2011;82:1112–1118 [DOI] [PubMed] [Google Scholar]
- 16.Crizzle AM, Classen S, Uc EY. Parkinson disease and driving: An evidence-based review. Neurology 2012;79:2067–2074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schrag A, Hovris A, Morley D, Quinn N, Jahanshahi M. Caregiver-burden in Parkinson's disease is closely associated with psychiatric symptoms, falls, and disability. Parkinsonism Relat Disord 2006;12:35–41 [DOI] [PubMed] [Google Scholar]
- 18.Safarpour D, Thibault DP, DeSanto CL, et al. Nursing home and end-of-life care in Parkinson disease. Neurology 2015;85:413–419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goetz CG, Stebbins GT. Risk factors for nursing home placement in advanced Parkinson's disease. Neurology 1993;43:2227–2229 [DOI] [PubMed] [Google Scholar]
- 20.Aarsland D, Larsen JP, Tandberg E, Laake K. Predictors of nursing home placement in Parkinson's disease: A population-based, prospective study. J Am Geriatr Soc 2000;48:938–942 [DOI] [PubMed] [Google Scholar]
- 21.Noyes K, Liu H, Li Y, Holloway R, Dick AW. Economic burden associated with Parkinson's disease on elderly Medicare beneficiaries. Mov Disord 2006;21:362–372 [DOI] [PubMed] [Google Scholar]
- 22.Kowal SL, Dall TM, Chakrabarti R, Storm MV, Jain A. The current and projected economic burden of Parkinson's disease in the United States. Mov Disord 2013;28:311–318 [DOI] [PubMed] [Google Scholar]
- 23.Dorsey ER, Deuel LM, Voss TS, et al. Increasing access to specialty care: A pilot, randomized controlled trial of telemedicine for Parkinson's disease. Mov Disord 2010;25:1652–1659 [DOI] [PubMed] [Google Scholar]
- 24.Dorsey ER, Venkataraman V, Grana MJ, et al. Randomized controlled clinical trial of “virtual house calls” for Parkinson disease. JAMA Neurol 2013;70:565–570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Venkataraman V, Donohue SJ, Biglan KM, Wicks P, Dorsey ER. Virtual visits for Parkinson disease: A case series. Neurol Clin Pract 2014;4:146–152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Willis AW, Schootman M, Evanoff BA, Perlmutter JS, Racette BA. Neurologist care in Parkinson disease: A utilization, outcomes, and survival study. Neurology 2011;77:851–857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Parkinson J. An essay on the shaking palsy. 1817. J Neuropsychiatry Clin Neurosci 2002;14:223–236; discussion 222. [DOI] [PubMed] [Google Scholar]
- 28.Hubble JP, Pahwa R, Michalek DK, Thomas C, Koller WC. Interactive video conferencing: A means of providing interim care to Parkinson's disease patients. Mov Disord 1993;8:380–382 [DOI] [PubMed] [Google Scholar]
- 29.Achey M, Aldred JL, Aljehani N, et al. The past, present, and future of telemedicine for Parkinson's disease. Mov Disord 2014;29:871–883 [DOI] [PubMed] [Google Scholar]
- 30.Cubo E, Gabriel-Galan JM, Martinez JS, et al. Comparison of office-based versus home Web-based clinical assessments for Parkinson's disease. Mov Disord 2012;27:308–311 [DOI] [PubMed] [Google Scholar]
- 31.Center for Connected Health Policy. State laws and reimbursement policies. Available at http://cchpca.org/state-laws-and-reimbursement-policies (last accessed August24, 2015)
- 32.Peto V, Jenkinson C, Fitzpatrick R. PDQ-39: A review of the development, validation and application of a Parkinson's disease quality of life questionnaire and its associated measures. J Neurol 1998;245(Suppl 1):S10–S14 [DOI] [PubMed] [Google Scholar]
- 33.Glasgow RE, Wagner EH, Schaefer J, Mahoney LD, Reid RJ, Greene SM. Development and validation of the Patient Assessment of Chronic Illness Care (PACIC). Med Care 2005;43:436–444 [DOI] [PubMed] [Google Scholar]
- 34.Stull D. The Multidimensional Caregiver Strain Index (MCSI). Its measurement and structure. J Clin Geropsychol 1996;2:175–196 [Google Scholar]
- 35.Pearl R. Kaiser Permanente Northern California: Current experiences with internet, mobile, and video technologies. Health Aff (Millwood) 2014;33:251–257 [DOI] [PubMed] [Google Scholar]
- 36.Darkins A, Ryan P, Kobb R, et al. Care Coordination/Home Telehealth: The systematic implementation of health informatics, home telehealth, and disease management to support the care of veteran patients with chronic conditions. Telemed J E Health 2008;14:1118–1126 [DOI] [PubMed] [Google Scholar]
- 37.Polinski JM, Barker T, Gagliano N, Sussman A, Brennan TA, Shrank WH. Patients' satisfaction with and preference for telehealth visits. J Gen Intern Med 2015. August 13 [Epub ahead of print]. doi: 10.1007/s11606-015-3489-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Orri M, Lipset CH, Jacobs BP, Costello AJ, Cummings SR. Web-based trial to evaluate the efficacy and safety of tolterodine ER 4 mg in participants with overactive bladder: REMOTE trial. Contemp Clin Trials 2014;38:190–197 [DOI] [PubMed] [Google Scholar]
- 39.Eilenberg KL, Hoover AM, Rutherford ML, Melfi CA, Segal S. From informed consent through database lock: An interactive clinical trial conducted using the Internet. Drug Inf J 2004;38:239–251 [Google Scholar]
- 40.Jacobs BP, Bent S, Tice JA, Blackwell T, Cummings SR. An internet-based randomized, placebo-controlled trial of kava and valerian for anxiety and insomnia. Medicine (Baltimore) 2005;84:197–207 [DOI] [PubMed] [Google Scholar]
- 41.McAlindon T. Why are clinical trials of glucosamine no longer uniformly positive? Rheum Dis Clin North Am 2003;29:789–801 [DOI] [PubMed] [Google Scholar]
- 42.Wicks P, Vaughan TE, Massagli MP, Heywood J. Accelerated clinical discovery using self-reported patient data collected online and a patient-matching algorithm. Nat Biotechnol 2011;29:411–414 [DOI] [PubMed] [Google Scholar]
- 43.Brenes GA, Danhauer SC, Lyles MF, Hogan PE, Miller ME. Telephone-delivered cognitive behavioral therapy and telephone-delivered nondirective supportive therapy for rural older adults with generalized anxiety disorder: A randomized clinical trial. JAMA Psychiatry 2015;72:1012–1020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Smith A. Older adults and technology use. Pew Research Center. 2014. Available at www.pewinternet.org/2014/04/03/older-adults-and-technology-use/ (last accessed August24, 2015)
- 45.Rainie L. The state of digial divides (video & slides). Pew Research Center. 2013. Available at www.pewinternet.org/2013/11/05/the-state-of-digital-divides-video-slides/ (last accessed August24, 2015)
- 46.Pew Research Center. Broadband technology fact sheet. Available at www.pewinternet.org/fact-sheets/broadband-technology-fact-sheet/ (last accessed August24, 2015)
- 47.Pew Research Center. Internet use over time. Available at www.pewinternet.org/data-trend/internet-use/internet-use-over-time/ (last accessed August24, 2015)
- 48.Norris P. Digital divide: Civic engagement, information poverty, and the Internet worldwide. New York: Cambridge University Press, 2001 [Google Scholar]
- 49.Internet World Stats: Usage and Population Statistics. The Digital Divide, ICT, and broadband Internet. Available at www.internetworldstats.com/links10.htm (last accessed August24, 2015)
- 50.Fox S, Purcell K. Chronic disease and the internet. Pew Research Center. Available at www.pewinternet.org/2010/03/24/chronic-disease-and-the-internet/ (last accessed August24, 2015)
- 51.Fox S, Duggan M. The diagnosis difference. Pew Research Center. Available at www.pewinternet.org/2013/11/26/the-diagnosis-difference/ (last accessed August24, 2015)
- 52.Pew Research Center. Internet user demographics. Available at www.pewinternet.org/data-trend/internet-use/latest-stats/ (last accessed August24, 2015)
- 53.Wallerstein NB, Duran B. Using community-based participatory research to address health disparities. Health Promot Pract 2006;7:312–323 [DOI] [PubMed] [Google Scholar]
- 54.Finch SA, Barkin SL, Wasserman RC, Dhepyasuwan N, Slora EJ, Sege RD. Effects of local institutional review board review on participation in national practice-based research network studies. Arch Pediatr Adolesc Med 2009;163:1130–1134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ravina B, Deuel L, Siderowf A, Dorsey ER. Local institutional review board (IRB) review of a multicenter trial: Local costs without local context. Ann Neurol 2010;67:258–260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.McWilliams R, Hoover-Fong J, Hamosh A, Beck S, Beaty T, Cutting G. Problematic variation in local institutional review of a multicenter genetic epidemiology study. JAMA 2003;290:360–366 [DOI] [PubMed] [Google Scholar]
- 57.Flynn KE, Hahn CL, Kramer JM, et al. Using central IRBs for multicenter clinical trials in the United States. PloS One 2013;8:e54999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wagner TH, Murray C, Goldberg J, Adler JM, Abrams J. Costs and benefits of the National Cancer Institute central institutional review board. J Clin Oncol 2010;28:662–666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Menikoff J. OHRP correspondence. U.S. Department of Health and Human Services. 2010. Available at www.hhs.gov/ohrp/policy/Correspondence/mcdeavitt20100430letter.html (last accessed August24, 2015)
- 60.US Food and Drug Administration. Guidance for industry. Using a centralized IRB review process in multicenter clinical trials. 2006. Available at www.fda.gov/cber/gdlns/irbclintrial.pdf (last accessed August24, 2015)
- 61.Human subjects research protections: Enhancing protections for research subjects and reducing burden, delay, and ambiguity for investigators. Biotechnol Law Rep 2011;30:707–727 [Google Scholar]
- 62.Federation of State Medical Boards. Medical boards explore licensure compact. 2013. Available at www.fsmb.org/policy/advocacy-policy/interstate-model-proposed-medical-lic (last accessed August24, 2015)
- 63.Robeznieks A. Interstate medical license compact becoming a reality. Modern Healthcare. 2015. Available at www.modernhealthcare.com/article/20150520/NEWS/150519873 (last accessed August24, 2015)
- 64.S. 1778: TELE-MED Act of 2015. 2015. Available at https://www.govtrack.us/congress/bills/114/s1778 (last accessed August24, 2015)
- 65.Text of the TELE-MED Act of 2015. 2015. Available at https://www.govtrack.us/congress/bills/114/hr3081/text (last accessed August24, 2015)
- 66.Weinstein RS, Lopez AM, Joseph BA, et al. Telemedicine, telehealth, and mobile health applications that work: Opportunities and barriers. Am J Med 2014;127:183–187 [DOI] [PubMed] [Google Scholar]
- 67.American Telemedicine Association. State telemedicine gaps analysis. Available at www.americantelemed.org/policy/state-policy-resource-center#.VdumdflVhBd (last accessed August24, 2015)
- 68.Neufeld JD, Doarn CR. Telemedicine spending by Medicare: A snapshot from 2012. Telemed J E Health 2015;21:686–693 [DOI] [PubMed] [Google Scholar]
- 69.Henry J. Kaiser Family Foundation. Medicare as a share of the Federal Budget, 2012. 2013. Available at http://kff.org/medicare/slide/medicare-as-a-share-of-the-federal-budget-2012/ (last accessed August24, 2015)
- 70.U.S. Department of Health and Human Services. Telehealth services. Rural health fact sheet series. Available at https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/telehealthsrvcsfctsht.pdf (last accessed August24, 2015)
- 71.Dorsey ER, George BP, Leff B, Willis AW. The coming crisis: Obtaining care for the growing burden of neurodegenerative conditions. Neurology 2013;80:1989–1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bloem BR, de Vries NM, Ebersbach G. Nonpharmacological treatments for patients with Parkinson's disease. Mov Disord 2015;30:1504–1520 [DOI] [PubMed] [Google Scholar]
- 73.Constantinescu G, Theodoros D, Russell T, Ward E, Wilson S, Wootton R. Treating disordered speech and voice in Parkinson's disease online: A randomized controlled non-inferiority trial. Int J Lang Commun Disord 2011;46:1–16 [DOI] [PubMed] [Google Scholar]
- 74.Tinetti ME, Fried TR, Boyd CM. Designing health care for the most common chronic condition—Multimorbidity. JAMA 2012;307:2493–2494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Willis AW, Schootman M, Tran R, et al. Neurologist-associated reduction in PD-related hospitalizations and health care expenditures. Neurology 2012;79:1774–1780 [DOI] [PMC free article] [PubMed] [Google Scholar]