Abstract
Background: For more than two decades, national career development programs (CDPs) have addressed underrepresentation of women faculty in academic medicine through career and leadership curricula. We evaluated CDP participation impact on retention.
Methods: We used Association of American Medical Colleges data to compare 3268 women attending CDPs from 1988 to 2008 with 17,834 women and 40,319 men nonparticipant faculty similar to CDP participants in degree, academic rank, first year of appointment in rank, and home institution. Measuring from first year in rank to departure from last position held or December 2009 (study end date), we used Kaplan–Meier curves; Cox survival analysis adjusted for age, degree, tenure, and department; and 10-year rates to compare retention.
Results: CDP participants were significantly less likely to leave academic medicine than their peers for up to 8 years after appointment as Assistant and Associate Professors. Full Professor participants were significantly less likely to leave than non-CDP women. Men left less often than non-CDP women at every rank. Participants attending more than one CDP left less often than those attending one, but results varied by rank. Patterns of switching institutions after 10 years varied by rank; CDP participants switched significantly less often than men at Assistant and Associate Professor levels and significantly less often than non-CDP women among Assistant Professors. Full Professors switched at equal rates.
Conclusion: National CDPs appear to offer retention advantage to women faculty, with implications for faculty performance and capacity building within academic medicine. Intervals of retention advantage for CDP participants suggest vulnerable periods for intervention.
Introduction
High-performing organizations, including academic health centers (AHCs), must recruit and retain skilled professionals. At AHCs, estimated costs for recruiting and training new faculty range from 1.5 times a first-year salary1 to up to $900,000.2–4 Thus, faculty are important economic as well as intellectual assets to AHCs,5 and their departure results in substantial costs.6–8 Individual faculty who depart before realizing their full potential lose the time already spent building careers, often after many years training for clinical practice or research careers.9 For institutions, departures of faculty create gaps in leadership, mentoring, knowledge of system-specific effectiveness and technology, and experience with the evolving field of healthcare and academic medicine at large. Institutions lose the productivity of departed faculty, with added burden for those remaining until replacements are fully integrated, and bear the costs for recruiting and training replacements.7 Considerable cost may also be incurred to retain individuals being recruited by other institutions. From a financial and workforce perspective, faculty departures represent a loss of institutional investment and potential productivity and are unsustainable long term.8
Departure rates from academic medicine are high. Among faculty entering academic medicine in the United States between 1981 and 1997, 37% of men and 43% of women left within 10 years.6 Higher rates were reported for Assistant Professors: 43% of men and 45% of women. Rates vary by specialty, from 23% for emergency medicine to 37% for obstetrics and gynecology.10 Reports of faculty intention to leave academic medicine range from 8.6% within 2 years10 to 42% within 5 years,11 with career dissatisfaction reported as the motivation to leave ranging from 21%12 to 40%,11 dramatically higher than motivation for personal and family issues (5%) and retirement (2%).12 Although reasons may differ by gender, these reports of dissatisfaction and departure present a large potential loss for the U.S. health system and society,5 with particular implications for women's recruitment into senior ranks.13
As academic medicine is increasingly challenged with constrained resources, programs and policies that foster faculty retention grow in importance.14 Mounting evidence that organizational innovation and financial health are linked to greater diversity in staff and leadership15 underscores the need for practices that support a diverse faculty. Reporting on three national career development programs (CDPs) for women faculty designed to address these issues and sponsored for more than two decades by the Association of American Medical Colleges (AAMC) and Drexel University College of Medicine (DUCOM), we focus on retention among women faculty. The 4-day AAMC Early and Mid-Career Women Faculty Professional Development programs (EWIM and MWIM, respectively) aim to inspire and provide academic career skills for early and midcareer faculty. The yearlong Hedwig van Ameringen Executive Leadership in Academic Medicine (ELAM®) program at DUCOM aims to build capacity for individuals and institutions for leadership16 and increase the number of women faculty in leadership.17 We used AAMC data about faculty appointments, collected since 1966 from accredited U.S. medical schools, to test our hypothesis that women faculty CDP participants would remain longer in academic medicine than nonparticipating women and men faculty at the same career stage. The overarching research questions posed were whether CDP participation was associated with retention in academic medicine and whether the association varied by academic rank.
Materials and Methods
Participants
We linked faculty from attendance lists from CDPs held between May 1, 1988, and December 31, 2008, to the AAMC Faculty Roster (FR) database18 and identified 4575 women for analysis. In brief, the FR is a continuously updated database with more than 130,000 active and 230,000 inactive faculty identified by social security numbers and institutional identification numbers. We excluded those without a faculty appointment at a Liaison Committee on Medical Education (LCME)-accredited institution at the time of CDP participation (n = 1247), men (n = 18), individuals without reported sex (n = 4), and those with unknown rank, primary appointment, appointment dates, or degree (n = 38). The resulting group of 3268 women participated in CDPs 420 times in the ELAM program and 3249 times in the AAMC programs; 359 (11%) attended more than one CDP.
For comparison with CDP participants, we included two faculty groups: women nonparticipants (i.e., women who did not participate in any CDPs, “non-CDP”) who comprise a pool of faculty eligible for CDP participation and men who represent a natural group from which to contrast the experience of women faculty. Both comparisons were selected to be as closely comparable in career stage and organizational environment as possible to CDP participants. Specifically, we formed cohorts for analysis by rank of CDP participants and non-CDP women and men faculty from the same institutions (indicated by a unique institutional ID), with the same degree types (i.e., MD, PhD, or MD/PhD), who were appointed in the same year at the same academic rank (i.e., Assistant, Associate, and Full Professors) as those held by the CDP participant when she participated in the CDP (CDP index rank). Women who participated in CDPs were not included as comparisons if they ever participated in CDPs.
The study protocol was approved by the University of Texas MD Anderson (DR09-0396) and the University of New Mexico (HRRC 09-556) Institutional Review Boards, the latter of which served as the IRB of record at the Drexel University College of Medicine (IRB 00000696, FWA 00005917).
Retention analyses
We assessed the impact of CDP participation on retention in academic medicine overall and by academic rank. Retention time for each individual was calculated in years from first year of appointment in the CDP index rank to either last date of follow-up by AAMC (December 31, 2009) or date of last departure from academic medicine, indicated by a specific end date for the most recently held faculty position. For women participating in more than one CDP, we assessed retention from the academic rank held at the first CDP attended.
To compare retention unadjusted for other factors that influence retention overall and at a specific time point after appointment in rank (10 years), we used Kaplan–Meier survival curves and the log-rank test and adapted a method used by AAMC researchers6 to calculate 10-year retention rates. We calculated 10-year rates for those remaining at the same institution, switching institutions, and departing from academic medicine altogether. To calculate 10-year rates, we included participants in CDPs from 1989 to 1999 (n = 1376) in comparison to men and women from the same period. We evaluated rate differences in two comparisons: first, for groups remaining in and departing from academic medicine after 10 years, and second, for groups remaining at the same institution and switching institutions after 10 years. For faculty remaining, switching, and departing after 10 years for each comparison group, we present histograms of counts and percentages by rank to allow comparison of absolute numbers by group. Statistical significance was declared if p-values were less than 0.05 or if 95% confidence intervals (CI) did not overlap 1.0.
To adjust for potential confounders (i.e., age, tenure track status, degree type, and department type), we used Cox proportional hazards models to estimate the likelihood of departure from academic medicine for CDP participants relative to same career-stage men or women faculty. Tenure track status, coded by AAMC as “tenured,” “not tenured, but on eligible tenure track,” “not tenured and not on eligible tenure track,” or “tenure not available,” was grouped for analysis as “tenured or tenure-track,” “non-tenure track,” and “tenure not available”; degree type was coded as “MD,” “MD/PhD,” and “PhD”; and department type was coded as “clinical,” “basic science,” or others. For each model by rank, we first tested the appropriateness of the proportional hazard (PH) assumption that the ratio of the hazard functions was constant between the groups. We then constructed models to estimate hazard ratios (HRs) and their 95% CIs. HR values below 1.0 indicated lower likelihood (i.e., longer retention) of leaving academic medicine for CDP participants, and values above 1.0 indicated their greater likelihood of departure. In analyses for which the PH assumption was met, HRs were assumed to be constant and relevant for all periods. In analyses for which the PH assumption was not met, we extended Cox models to accommodate changes in hazards over time by including time covariates (t and t2) to test interactions with CDP participation, calculating HRs and their 95% CIs for each year of retention in rank, up to 40 years. Models were adjusted for age given the independent relationship between older age and likelihood of retirement.
We also conducted a sensitivity analysis using propensity score analysis to assess possible bias from differences between the comparison groups. We assembled two one-to-one data sets of CDP participants and same career-stage comparison faculty with similar propensity scores. The scores were calculated based on having the same home institutions, first year of appointment in rank at CDP participation, age, degree type, department type, and tenure track status. Using these data sets, we then reran Cox proportional hazards models. For these models, the baseline hazard function was allowed to vary across data sets to produce valid estimates.19
Results
Demographic description
Overall, 3268 women participating 3669 times in CDPs between 1988 and 2008 were included with 17,834 non-CDP women and 40,319 men in cohorts organized by academic rank (Table 1). Just more than a third of all faculty were tenured or on the tenure track (36.7%, 19,341 of 52,629), and the majority were in clinical departments (94.5%, 61,265 of 64,859). CDP participants held more PhD or MD/PhD degrees and were younger than both men and non-CDP women peers at every rank. Median times spent in rank for Assistant, Associate, and Full Professors, respectively, were 8, 10, and 11 years. As expected based on programmatic focus, the majority of AAMC EWIM participants were Assistant Professors, whereas the majority of AAMC MWIM, WIM, and ELAM participants were Associate and Full Professors (Supplementary Data; Supplementary Data are available online at www.liebertpub.com/jwh).
Table 1.
Career Demographic Characteristics of CDP Participants and Non-CDP Peer Comparisons by Rank and Gender
| Non-CDP faculty | |||
|---|---|---|---|
| Characteristic | CDP faculty (N = 3268) | Women (N = 18,642)a | Men (N = 43,189)a |
| Assistant Professors, n | 1802 | 15,533 | 30,579 |
| Degree,bn (%) | |||
| MD | 1481 (82) | 14,034 (90) | 28,157 (92) |
| PhD | 219 (12) | 1336 (9) | 1846 (6) |
| MD/PhD | 102 (6) | 163 (1) | 576 (2) |
| Mean age in years (SD)b | 35.2 (4.3) | 37.9 (7.1) | 37.0 (6.2) |
| Median follow-up in years (10th, 90th percentile range) | 10 (4, 20) | 7 (2, 16) | 8 (2, 18) |
| Associate Professors, n | 1000 | 2617 | 9685 |
| Degree,bn (%) | |||
| MD | 771 (77) | 2223 (85) | 8675 (90) |
| PhD | 171 (17) | 355 (14) | 828 (9) |
| MD/PhD | 58 (6) | 39 (1) | 182 (2) |
| Mean age in years (SD)b | 41.1 (5.2) | 43.2 (6.7) | 43.7 (6.4) |
| Median follow-up in years (10th, 90th percentile range) | 12 (4, 21) | 8 (2, 18) | 10 (3, 19) |
| Full Professors, n | 466 | 492 | 2925 |
| Degree,c,dn (%) | |||
| MD | 273 (59) | 309 (63) | 2236 (76) |
| PhD | 161 (35) | 169 (34) | 627 (21) |
| MD/PhD | 32 (7) | 14 (3) | 62 (2) |
| Mean age in years (SD)b | 44.7 (5.3) | 48.5 (7.6) | 49.0 (7.2) |
| Median follow-up in years (10th, 90th percentile range) | 13 (5, 22) | 9 (3, 18) | 11 (4, 20) |
Some non-CDP individuals were selected as comparisons for analysis in more than one academic rank, which accounts for the difference between the number of non-CDP women and men listed in Table 1 and the total numbers reported in the “Results” section.
Z-statistic p < 0.001 comparing degrees or age of CDP participants to both non-CDP women and men.
Z-statistic p = 0.09 comparing degrees of CDP participants and non-CDP women.
Z-statistic p < 0.001 comparing degrees of CDP participants and men.
CDP, career development program.
Descriptive retention analysis using Kaplan–Meier method and log-rank test
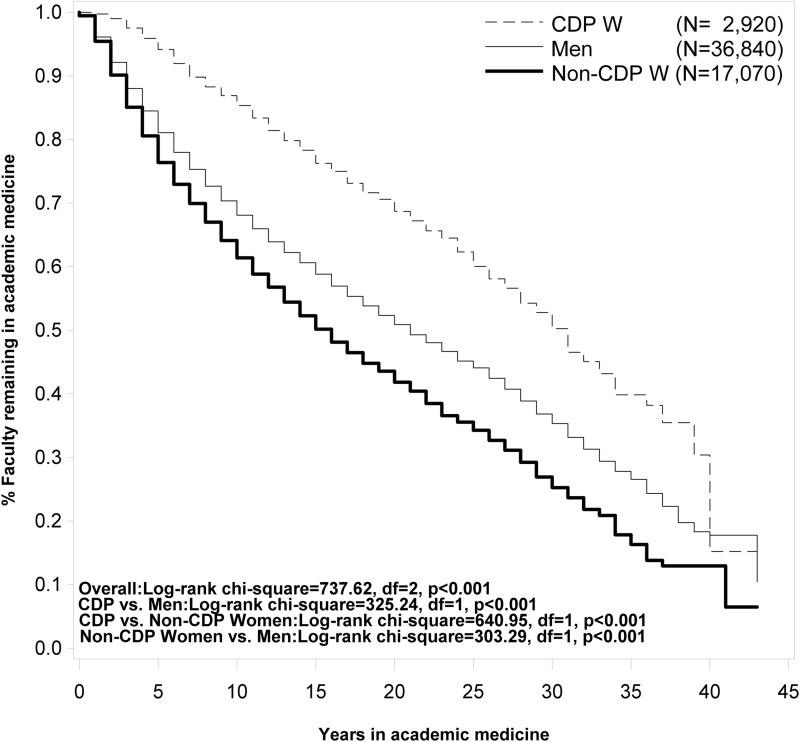
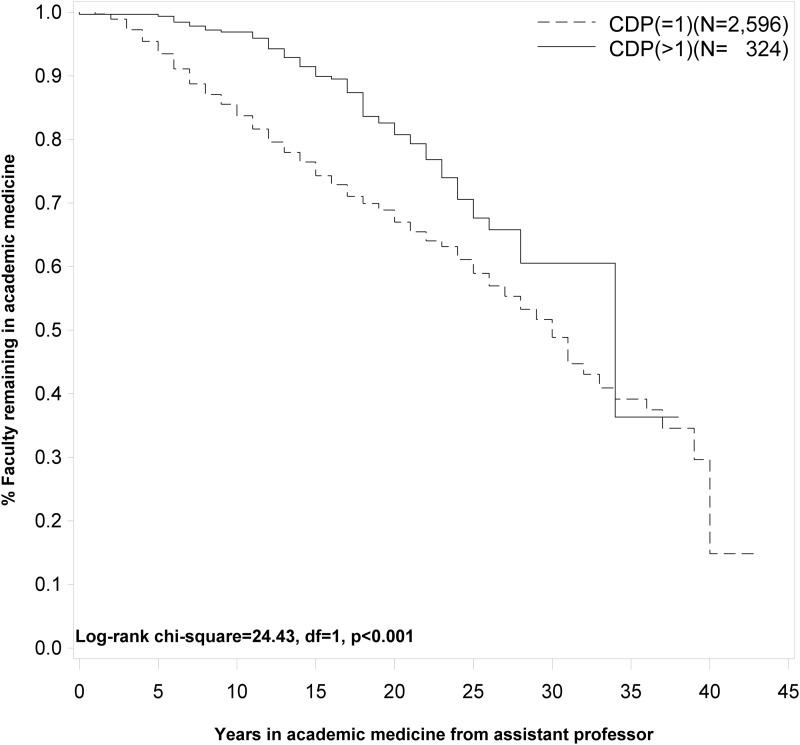
Overall, CDP participants remained in academic medicine significantly longer than same career-stage non-CDP women and men (Fig. 1). Within each academic rank, CDP participants had significantly longer retention than their peer counterparts (Supplementary Fig. S1; Supplementary Data are available online at www.liebertpub.com/jwh). The type of CDP (i.e., AAMC vs. ELAM) was not associated with retention for Associate and Full Professors (Supplementary Fig. S2; log-rank chi-square = 0.0069, df = 1, p = 0.93; log-rank chi-square = 1.1562, df = 1, p = 0.28, respectively). Men also remained significantly longer than non-CDP women overall and by rank. Participation in more than one CDP was associated with longer retention than that in one CDP (Fig. 2), with a mean interval of 5.3 years (SD = 3.35) between CDP. By rank, the finding was significant among Assistant Professors only (by rank; Supplementary Fig. S3).
FIG. 1.
Retention from first year of appointment as Assistant Professor for CDP participants and faculty peer comparisons. CDP, career development program.
FIG. 2.
Retention from first year of appointment as Assistant Professor for CDP participants by number of CDP attended.
Multivariable retention analyses using extended Cox model survival approach
Results from multivariable Cox model analyses adjusted for age were similar to those fully adjusted for age, tenure status, degree, and department type, which are presented in this study (Table 2). CDP women were less likely to leave academic medicine and significantly so at every academic rank than same career-stage women and men, except in comparisons between CDP women and men Full Professors. Women Full Professors at time of CDP participation had equal likelihood of leaving academic medicine as men peers. However, among Full Professors, both CDP participants and men in separate models were significantly less likely to leave academic medicine than non-CDP women (32% and 28%, respectively).
Table 2.
Hazard Ratios and 95% Confidence Intervals of Adjusted Models Comparing Likelihood of Departure from Academic Medicine of CDP Participants, Men, and Non-CDP Women
| HR (95% CI; year in academic rank)a | ||
|---|---|---|
| Age adjusted | Fully adjustedb | |
| Assistant Professors | ||
| CDP versus non-CDP women | 0.84 (0.73, 0.97; 13) | 0.85 (0.74, 0.98; 13) |
| CDP versus men | 0.84 (0.75, 0.95; 9) | 0.92 (0.86, 0.97; 9) |
| Men versus non-CDP women | 0.85 (0.74, 0.99; 20) | 0.86 (0.74, 0.99; 20) |
| Associate Professors | ||
| CDP versus non-CDP women | 0.73 (0.60, 0.90; 9) | 0.76 (0.64, 0.93; 9) |
| CDP versus men | 0.84 (0.66, 0.92; 8) | 0.88 (0.81, 0.96; 8) |
| Men versus non-CDP women | 0.81 (0.68, 0.96; 17) | 0.82 (0.69, 0.98; 17) |
| Full Professors | ||
| CDP versus non-CDP women | 0.64 (0.47, 0.87) | 0.68 (0.50, 0.92) |
| CDP versus men | 0.84 (0.68, 1.05) | 0.93 (0.84, 1.05) |
| Men versus non-CDP women | 0.70 (0.57, 0.85) | 0.72 (0.59, 0.88) |
All models for Assistant and Associate Professors were adjusted for t and t2 because the assumption of proportional hazards was not met, indicating changes in HRs over time. Therefore, the HRs presented in the table for these models are for the highest year for which HRs were statistically significant. Models for Full Professors met the assumption for proportional hazards; therefore, the HRs presented in the table for these models are relevant for all years.
Fully adjusted models were also adjusted for age, tenure track status, and department type.
CI, confidence interval; HR, hazard ratio.
Among Assistant and Associate Professors, the hazard proportionality assumption was not met; thus, HRs were statistically significant only for specific intervals that indicate lower likelihood of leaving academic medicine (Table 3). Assistant Professor CDP participants were significantly less likely to leave academic medicine in their first 9 years following initial appointment compared with men. CDP participants were also significantly less likely to leave in their first 13 years of appointment compared with non-CDP women. Among Assistant Professors, men were significantly less likely to leave academic medicine for 20 years after appointment in rank than non-CDP women. Once promoted to Associate Professor, CDP participants were significantly less likely to leave academic medicine in the subsequent 8 years compared to same career-stage men and for the next 9 years compared to non-CDP women. Among Associate Professors, men were significantly less likely to leave for 17 years after appointment than non-CDP women (Supplementary Table S3 and Supplementary Fig. S4).
Table 3.
Intervals of Longer Retention in Academic Medicine by Groups Compared and Academic Rank
| Intervals of significantly longer retention in years since initial appointment in academic rank | |||
|---|---|---|---|
| Academic rank | For CDP participants compared to men | For CDP participants compared to non-CDP women | For men compared to non-CDP women |
| Assistant Professor | 0–9, ≥23 | 0–13, ≥22 | 0–20 |
| Associate Professor | 0–9 | 0–10 | 6–18 |
| Full Professor | No significant difference | All years | All years |
In Cox model analyses using the propensity score data set, we confirmed that CDP participants were significantly less likely to leave academic medicine than men and women peers for all ranks, except in comparison with men among Full Professors (Supplementary Table S4).
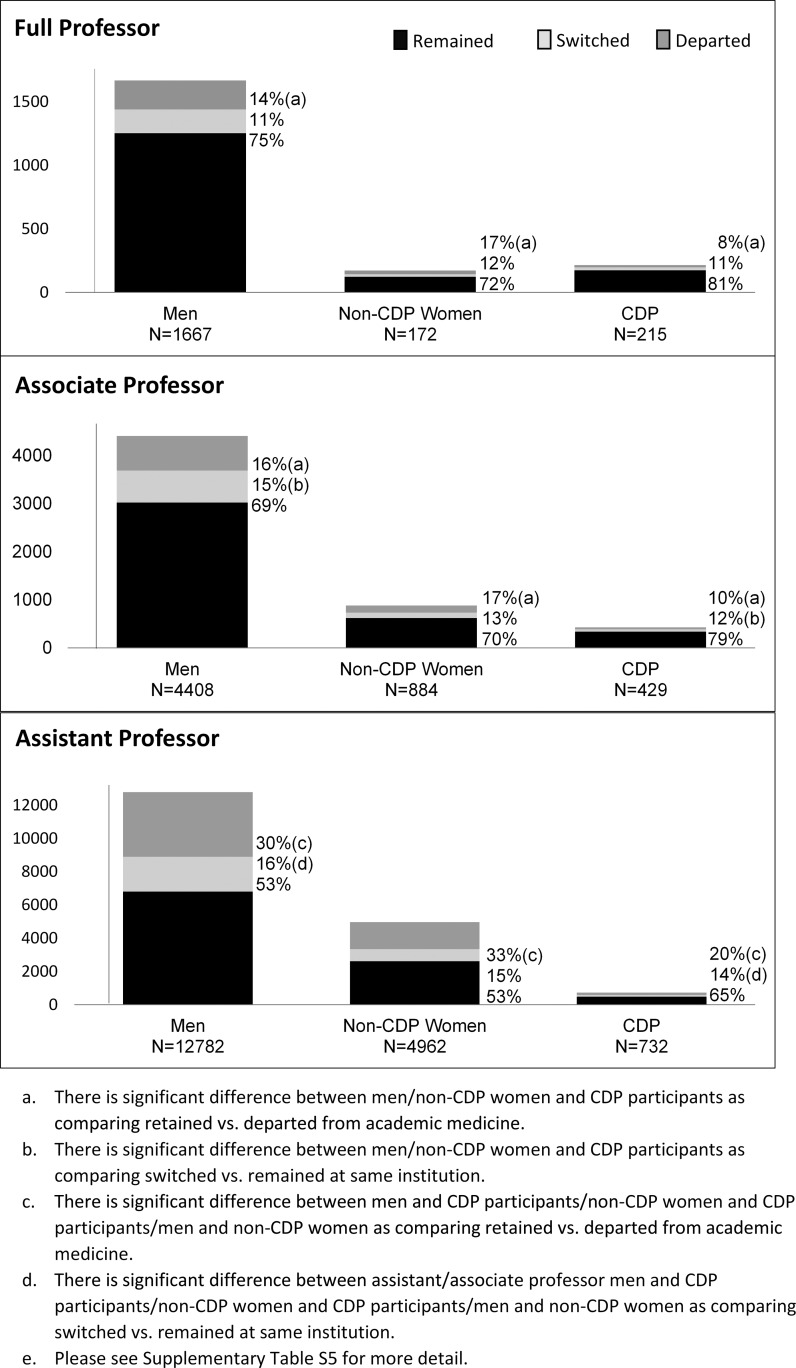
Ten-Year departure rates from academic medicine and index institutions
We found that overall, and at each rank, significantly fewer CDP participants left academic medicine after 10 years than their counterparts (Fig. 3 and Supplementary Table S5). Switching institutions within academic medicine varied by rank and gender. CDP participants switched institutions significantly less often than men at Assistant and Associate Professor ranks. CDP participants also switched institutions less often than non-CDP women at all ranks but significantly so only among Assistant Professors. Men switched institutions slightly less often than non-CDP women at Assistant and Associate Professor ranks, although with borderline significance. No differences in switching institutions were significant among Full Professors.
FIG. 3.
Number and proportion of faculty who at 10 years had departed academic medicine (dark grey), had switched institutions (light grey), or remained at the same institutions (black) by academic rank for women participating in CDPs from 1989 to 1999 in comparison with men and women faculty.
Discussion
Our analyses of three national CDPs for women faculty in academic medicine revealed a compelling association of longer retention for CDP participants in comparison with both women and men faculty peers. This relationship sits within the context of steady attrition for all groups over time and across rank. The strength of the association suggests that CDP participation benefits women at all ranks compared with non-CDP women faculty. A potential ceiling effect for CDP impact is suggested by the statistical equivalence in comparison to men, notably as men left academic medicine less often than non-CDP women at every rank.
That retention of CDP Assistant and Associate Professors significantly exceeded that of same career-stage men is noteworthy given the general experience of women in academic medicine. In a nationally representative sample of medical colleges, Pololi et al.20 reported that women faculty had a lower sense of gender equity and belonging and were less convinced than men that their institutions were family friendly, successfully addressing diversity, and shared their values—three major issues that influence retention. Women in that study reported professional engagement and leadership aspirations equal to men, suggesting greater impact of these factors on women's departure from academic medicine. Our findings are meaningful as they show that CDP participants gained advantage within a system that traditionally benefits men.17,21
The higher retention associated with specific intervals of CDP participants at early career ranks has several positive implications. First, intervening to reduce early career attrition has the potential to build numbers and diversity in the AHC workforce. This is especially important for Assistant Professors at or before appointment to the Associate Professor rank when the greatest loss of faculty is reported.6,22 Second, the mechanism by which such program participation might influence the staying power of junior faculty, both men and women, and others underrepresented in academic medicine, should be considered. These results add to evidence that CDPs can help faculty remain engaged in academic medicine.23,24 Increasing engagement, by creating a better fit between an individual faculty member and his or her job, which can be improved through CDPs, even participation in multiple professional development programs can increase intention to stay at one's institution.25 Third, specific intervals of longer likelihood of retention associated with CDP participation suggest that the first decades following initial appointment as Assistant Professor and first promotion as Associate Professor are critical periods for retention that can be enhanced with professional development participation.26–28
The loss of each faculty member is costly for individual AHCs, even if faculty remain elsewhere within academic medicine.7 A recent report found that intent to switch institutions was correlated with a perception of “far too much/too much” time/effort spent in a given mission area.25 Both intent and actual switching institutions were greater for junior faculty.6,25 Thus, our finding that Assistant Professor CDP participants switched institutions significantly less often than their peers has important implications. One AHC reported that average annual costs related to medicine and surgery faculty turnover exceeded $400,000 per person per department, and subspecialist replacement exceeded $500,000.9 Another study calculated faculty turnover, including 9% physician turnover, cost 5.8% of the annual operating budget, with physician recruitment comprising 67% of total annual hiring costs.7 Institutional investment in recruitment, especially for those with large start-up packages, has been estimated to take up to 10 years to amortize.29 These reports indicate the substantial, both calculable and intangible, costs related to recruitment and turnover in academic medicine.9,30
Our findings suggest that some costs may be avoidable with a modest investment of faculty time and organizational support to attend CDPs. That said, individuals switching institutions may do so for promotion to higher level ranks or leadership opportunities, as observed for ELAM alumni who relocated geographically.31 When opportunities are infrequently available locally, ambitious and talented faculty may have to leave their home institutions to pursue professional opportunities elsewhere that are more fulfilling and personally satisfying even at the cost of moving themselves and their families.
Although our findings are related to programs attended by women, the program content is largely generalizable; it is reasonable, given that we compared participants to same career-stage counterparts, to expect that all faculty would benefit with such professional development,23 a meaningful point given the large numbers of men who leave academic medicine as well as the marked attrition from every faculty rank over time. Similarly, we anticipate that internal CDPs can provide benefit. Clear differences exist between internal and national programs, and comparability of benefits obtained with those from national programs remains unknown.23,32,33
Our results document increased retention for CDP participants but do not answer the question why this occurs. Survey and interview data from the same CDP population show that participants identified skill building and career guidance from the experience.34 Others have reported that such skill building influences retention in academic medicine.35,36 The critical skills gained may include strengthening personal assertiveness, increasing self-efficacy, enhancing career aspiration,16,34,37 and increasing awareness of resources for career development. Moreover, institutional visibility from selection for CDPs explicitly endorses the value of the individual both to the woman herself and to those following her academic and leadership potential, consistent with frames of reference described by scholars of women's career development.17,38
The conceptual model used to construct this research hypothesized that CDPs play a crucial role in mitigating the tensions of competing organizational and individual demands for women faculty and in developing their capacity to contribute to their organizations.39 The current study shows that at a minimum, CDPs support retention, a requirement for continuing career productivity. As an individual strategy, participation appears to increase the probability of building a career undisrupted by changes in institutions. As an institutional strategy, supporting CDP participation shows a willingness to invest in individual success, which may contribute to retention of selected individuals at a specific institution, as we observed, particularly among Assistant Professors, and in academic medicine generally. Indeed, recognizing institutions for such sponsorship may produce benefit beyond the sponsorship itself. Thus, programs such as CDPs, coupled with changing the structure of the workplace to achieve a critical mass of women leaders,40–42 can promote permanent change in the diversity of the academic medical faculty workforce and leadership.
This work has several strengths. One is the accrual over time of a large number of participants trained in multiple disciplines in these high-quality national programs. The consistency and magnitude of the robust association of CDP participation with longer retention in academic medicine are striking in spite of different program lengths (i.e., 4 days and 1 year), different ranks, different comparison groups, and across CDPs. Another major strength was the use of the comprehensive AAMC FR Data Set, including data from individual faculty and medical schools in the United States.
A major limitation is that an observational study cannot definitively establish the causal role of CDP participation in long-term retention in academic medicine. We also did not have information about factors that influence career longevity in academic medicine (e.g., publishing productivity, grant funding success, honors and awards, and participation in other career development training programs) and so were unable to adjust for such potential confounders. For these reasons, to reduce the possible influence of individual or institutional selection as much as possible given the data available to us, we constructed our analytic cohorts to include faculty most comparable to CDP participants in their home institutions, academic ranks at CDP participation, and year of appointment in those ranks and adjusted for age, tenure track status, degree type, and department type. Thus, although the possible influence of selection must be considered, and because it is debatable whether the value of findings based on archival data outweighs the infeasibility and ethical considerations of conducting long-term randomized experiments to overcome selection bias, these findings can be useful to institutions deciding whether to send their faculty to such programs given that we report many meaningful benefits to CDP participants.34 Thus, such analyses of programs that track the careers of women faculty can inform development of interventions to influence retention and promotion.
Conclusions
Our analysis suggests that in spite of steady attrition of faculty at all ranks from academic medicine,43 women faculty participating in CDPs were less likely to leave academic medicine than their men and women faculty peers. Our work provides information for both faculty members and their institutions, leading to possible strategies to promote retention in academic medicine careers. Increasing research is finding that much can be gained if talented women and other underrepresented individuals are retained longer in their careers in professional organizations, academia, and academic medicine.44 They can be promoted to higher ranks, serve as role models, mentors, and expert teachers, and be appointed as leaders, helping diversify leadership and increase organizational effectiveness and financial return.15 Retention is the necessary underpinning to produce a diverse faculty with potential for leadership; such leaders can then provide the critical mass of diverse perspectives for organizational change in structure and culture necessary for AHCs to thrive in the current arena.45 For these reasons, our findings have serious implications for workplace performance through the mutually complementary agendas of advancing gender equity, strengthening academic career development, reducing the multiple costs of departure and turnover, and increasing organizational effectiveness.46,47
Supplementary Material
Acknowledgments
The authors would like to thank Drs. Kevin Grigsby, Hershel Alexander, Stephanie Wragg (formerly at AAMC), and Elizabeth Coakley of the Association of American Medical Colleges; Katherine Gleason and Aleya Lyn (formerly at Drexel University College of Medicine); Chin Seto at University of New Mexico; and Yue-Ming Chen, Lerong Li, and Chih-Chieh Wu (formerly at MD Anderson) at University of Texas MD Anderson Cancer Center for their support of the project. We would also like to thank the individuals who served on our project's Advisory Committee: Drs. Jasit Ahluwalia, Carol Aschenbrener, Lorris Betz, Molly Carnes, Carmen R. Green, Sharon McDade, Lois Nora, and Diane Wara. This work was supported by grant funding from NICHD (R01 HD064655) for RFA-GM-09-012 “Research on Causal Factors and Interventions that Promote and Support the Careers of Women in Biomedical and Behavioral Science and Engineering.”
Author Disclosure Statement
Drs. D.H., S.C., P.S.M., and D.M. have participated as faculty leaders in the AAMC career development programs for women; Drs. D.H. and D.M. have participated as fellows in the Drexel University College of Medicine career development program; Drs. P.S.M. and D.M. are leaders of the Drexel University College of Medicine Career Development Program; Dr. D.M. was an AAMC staff member and responsible for the leadership of the AAMC career development programs for women; and Drs. S.C. and D.H. were participants in the AAMC WIM programs.
References
- 1.Wenger D. Conducting a cost-benefit analysis of faculty development programs. Acad Phys Sci 2003:6–7 [Google Scholar]
- 2.Bickel J, Brown AJ. Generation X: Implications for faculty recruitment and development in academic health centers. Acad Med 2005;80:205–210 [DOI] [PubMed] [Google Scholar]
- 3.Demmy TL, Kivlahan C, Stone TT, Teague L, Sapienza P. Physicians' perceptions of institutional and leadership factors influencing their job satisfaction at one academic medical center. Acad Med 2002;77:1235–1240 [DOI] [PubMed] [Google Scholar]
- 4.Bachrach D. Retain or replace: The true costs of unintended faculty departures and how to minimize them. Acd Phys Sci 2005;2 [Google Scholar]
- 5.Chapman AB, Guay-Woodford LM. Nurturing passion in a time of academic climate change: The modern-day challenge of junior faculty development. Clin J Am Soc Nephrol 2008;3:1878–1883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alexander H, Lang J. The long-term retention and attrition of US medical school faculty. AAMC Anal Brief 2008;8:1–2 [Google Scholar]
- 7.Waldman JD, Kelly F, Aurora S, Smith HL. The shocking cost of turnover in health care. Health Care Manage Rev 2004;29:2–7 [DOI] [PubMed] [Google Scholar]
- 8.Allen DG. Retaining talent: A guide to analyzing and managing employee turnover. Alexandria, VA: SHRM Foundation, 2008 [Google Scholar]
- 9.Schloss EP, Flanagan DM, Culler CL, Wright AL. Some hidden costs of faculty turnover in clinical departments in one academic medical center. Acad Med 2009;84:32–36 [DOI] [PubMed] [Google Scholar]
- 10.Corrice A, Fox S, Bunton SA. Retention of full-time clinical MD faculty at US medical schools. In: Analysis in Brief. Washington, DC: Association of American Medical College; 2011;11:1–2 [Google Scholar]
- 11.Lowenstein SR, Fernandez G, Crane LA. Medical school faculty discontent: Prevalence and predictors of intent to leave academic careers. BMC Med Educ 2007;7:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pololi LH, Krupat E, Civian JT, Ash AS, Brennan RT. Why are a quarter of faculty considering leaving academic medicine? A study of their perceptions of institutional culture and intentions to leave at 26 representative US medical schools. Acad Med 2012;87:859–869 [DOI] [PubMed] [Google Scholar]
- 13.Association of American Medical Colleges (2008): The long-term retention and attrition of U.S. Medical School Faculty. Available at: www.aamc.org/download/67968/data/aibvol8no4.pdf (accessed February25, 2014)
- 14.Steinert Y, Naismith L, Mann K. Faculty development initiatives designed to promote leadership in medical education. A BEME systematic review: BEME Guide No. 19. Med Teach 2012;34:483–503 [DOI] [PubMed] [Google Scholar]
- 15.Catalyst. The bottom line: Connecting corporate performance and gender diversity. Catalyst 2004
- 16.Morahan PS, Dannels SA, Yamagata H, et al. . Evaluating a leadership program: A comparative, longitudinal study to assess the impact of the Executive Leadership in Academic Medicine (ELAM) Program for Women. Acad Med 2008;83:488–495 [DOI] [PubMed] [Google Scholar]
- 17.Morahan PS, Gleason KA, Richman RC, Dannels S, McDade SA. Advancing women faculty to senior leadership in US academic health centers: Fifteen years of history in the making. NASPA J Women Higher Educ 2010;3:140–165 [Google Scholar]
- 18.Hayes N, Introna LD. Cultural values, plagiarism, and fairness: When plagiarism gets in the way of learning. Ethics Behav 2005;15:213–231 [Google Scholar]
- 19.Faries DE, Leon AC, Haro JM, Obenchain RL. Analysis of observational health care data using SAS. Cary, NC: SAS Institute, 2010 [Google Scholar]
- 20.Pololi LH, Civian JT, Brennan RT, Dottolo AL, Krupat E. Experiencing the culture of academic medicine: Gender matters, a national study. J Gen Internl Med 2013;28:201–207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bickel J, Wara D, Atkinson BF, et al. . Increasing women's leadership in academic medicine: Report of the AAMC Project Implementation Committee. Acad Med 2002;77:1043–1061 [DOI] [PubMed] [Google Scholar]
- 22.Liu CQ, Morrison E. U.S. Medical school full-time faculty attrition. Anal Brief 2014;14:1–2 [Google Scholar]
- 23.Ries A, Wingard D, Morgan C, Farrell E, Letter S, Reznik V. Retention of junior faculty in academic medicine at the University of California, San Diego. Acad Med 2009;84:37–41 [DOI] [PubMed] [Google Scholar]
- 24.Speck RM, Sammel MD, Troxel AB, et al. . Factors impacting the departure rates of female and male junior medical school faculty: Evidence from a longitudinal analysis. J Womens Health 2012;21:1059–1065 [DOI] [PubMed] [Google Scholar]
- 25.Pollart SM, Novielli KD, Brubaker L, et al. . Time well spent: The association between time and effort allocation and intent to leave among clinical faculty. Acad Med 2015;90:365–371 [DOI] [PubMed] [Google Scholar]
- 26.Speck RM, Sammel M, Troxel AB, Cappola AR, et al. . Factors impacting the departure rates of female and male junior medical school faculty: Evidence from a longitudinal analysis. J Womens Health (Larchmt) 2012;21:1059–1065 [DOI] [PubMed] [Google Scholar]
- 27.Satiani B, Williams T, Brod H, Way DP, Ellison EC. A review of trends in attrition rates for surgical faculty: A case for a sustainable retention strategy to cope with demographic and economic realities. J Am Coll Surg 2013;216:944–953 [DOI] [PubMed] [Google Scholar]
- 28.Bucklin BA, Valley M, Welch C, Tran ZV, Lowenstein SR. Predictors of early faculty attrition at one Academic Medical Center. BMC Med Educ 2014;14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Joiner KA. A strategy for allocating central funds to support new faculty recruitment. Acad Med 2005;80:218–224 [DOI] [PubMed] [Google Scholar]
- 30.Dorsey ER, Van Wuyckhuyse BC, Beck CA, Passalacqua WP, Guzick DS. Economics of new faculty hires in basic science. Acad Med 2009;84:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McLean MR, Morahan P, Dannels SA, McDade SA. Geographic mobility advances careers: Study of the Executive Leadership in Academic Medicine (ELAM) program for women. Acad Med 2013;88:1700–1706 [DOI] [PubMed] [Google Scholar]
- 32.Morahan PS, Kasperbauer D, McDade SA, et al. . Training future leaders of academic medicine: Internal programs at three academic health centers. Acad Med 1998;73:1159–1168 [DOI] [PubMed] [Google Scholar]
- 33.Wingard DL, Garman KA, Reznik V. Facilitating faculty success: Outcomes and cost benefit of the UCSD National Center of Leadership in Academic Medicine. Acad Med 2004;79:S9–S11 [DOI] [PubMed] [Google Scholar]
- 34.Helitzer DL, Newbill SL, Morahan PS, et al. . Perceptions of skill development of participants in three national career development programs for women faculty in academic medicine. Acad Med 2014;89:896–903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Levine RB, Lin F, Kern DE, Wright SM, Carrese J. Stories from early-career women physicians who have left academic medicine: A qualitative study at a single institution. Acad Med 2011;86:752–758 [DOI] [PubMed] [Google Scholar]
- 36.Bucklin BA, Valley M, Welch C, Tran ZV, Lowenstein SR. Predictors of early faculty attrition at one Academic Medical Center. BMC Med Educ 2014;14:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sloma-Williams L, McDade SA, Richman RC, et al. . The role of self-efficacy in developing women leaders. Women in academic leadership: Professional strategies, personal choices. Sterling, VA: Stylus, 2009:50–73 [Google Scholar]
- 38.Meyerson DE, Fletcher JK. A modest manifesto for shattering the glass ceiling. Harv Bus Rev 2000;78:126–136 [Google Scholar]
- 39.Magrane D, Helitzer D, Morahan P, et al. . Systems of career influences: A conceptual model for evaluating the professional development of women in academic medicine. J Womens Health 2012;21:1244–1251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Soe L, Yakura EK. What's wrong with the pipeline? Assumptions about gender and culture in IT work. Women's Studies 2008;37:176–201 [Google Scholar]
- 41.Donaldson EL, Emes CG. The challenge for women academics: Reaching a critical mass in research, teaching, and service. Can J Higher Educ 2000;30:33–55 [Google Scholar]
- 42.De Wet CB. Reaching critical mass: Women in faculty and administrative roles. Forum on Public Policy Online: ERIC, 2010 [Google Scholar]
- 43.Liu C, Morrison E. U.S. Medical school full-time faculty attrition. Anal Brief 2014;14:1–2 [Google Scholar]
- 44.Ehrenberg RG, Jakubson GH, Martin ML, Main JB, Eisenberg T. Do trustees and administrators matter? Diversifying the faculty across gender lines. Cambridge, MA: National Bureau of Economic Research, 2009 [Google Scholar]
- 45.Morahan P, Bickel J. Capitalizing on women's intellectual capital in the professions. Acad Med 2002;77:110–112 [DOI] [PubMed] [Google Scholar]
- 46.Ely RJ, Scully MA, Foldy E. Reader in gender, work and organization. New York, NY: Oxford, 2003 [Google Scholar]
- 47.Rapoport R, Bailyn L, Fletcher J, Pruitt B. Beyond work-family balance: Advancing gender equity and workplace performance. San Francisco, CA: Jossey-Bass, 2002 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.