Abstract
Introduction
Measurement of early subsidence of uncemented femoral stems can be used to evaluate the likelihood of long term stem component loosening and therefore clinical failure.
Our aim was to evaluate the factors associated with subsidence in collared and uncollared versions of the Corail femoral stem.
Methods
121 hips in 113 consecutive patients were studied, operated on by two surgeons in our hospital differing in their choice of Corail stem. This gave two groups of patients with 66 hips having collared stems and 55 hips having uncollared. We recorded patients’ age, sex, ASA grade and BMI. Radiographs post-operatively at day 1, 6 weeks and 1 year were evaluated measuring subsidence, angulation, signs of stability and fixation, and canal fill ratio at the metaphysis and diaphysisafter correcting for magnification errors by calibration using femoral head size.
Results
Clinically significant subsidence (>3 mm) occurred in 7.6% of collared and 10.9% of uncollared stems, all within 6–8 weeks, but did not reach statistical significance (p = 0.345). Revision for symptomatic loosening was required in 1 patient in each group (1.5% collared versus 1.8% uncollared).
Discussion
Early subsidence of Corail femoral stem should alert surgeons to closer patient follow-up as the rate of early revision is 18% in stems with >3 mm of subsidence. However, the presence of a collar does not seem to be protective.
Keywords: Femoral stems, Corail stem, Uncemented
1. Introduction
The data from National Joint Registry (NJR) of England and Wales shows that the Corail is the most common uncemented femoral stem used in primary total hip arthroplasty, with a recorded increase in its usage from 15% in 2003 to just under 50% in 2011.1 Corail femoral stems are manufactured in two designs; the collared and the collarless. Each design is available in two further subsets. The collared stems are available as standard and lateralised neck segment stems. The collarless stems are available as standard and high offset neck segment stems.2, 3 The Corail implant is made of forged titanium alloy (TiAl6V4). The proximal part of the stem is trapezoid in cross section, which flares in the sagittal and coronal plane to resist axial and torsional stresses providing initial stability in metaphyseal area. The distal part of the stem is quadrangular in cross section, which provides rotational stability in the absence of cortical contact. The whole stem is coated with 150 mm thick layer of hydroxyapatite (HA), which not only helps to prevent the release of metal ions, but also helps to provide maximum osteointegration at the bone–implant interface and prevents the interposition of the fibrous membrane around the distal portion of the stem.2
The differences in the short- and long-term durability of the two available designs of Corail stems are controversial. One potential limitation of any uncemented femoral stem is the risk of early subsidence or migration leading to loosening and implant failure.4, 5, 6, 7 Berend reported that the early subsidence of femoral stem was associated with higher revision rate.4 However, Krismer et al. reported an increased incidence of early subsidence but better subsequent stability and good long-term results.8 However, there is still a lack of sufficient evidence outlining the factors responsible for early subsidence in uncemented Corail femoral stems.8, 9, 10 Our study aimed at another attempt to identify the factors responsible for early subsidence of the Corail femoral stems and to assess if the differences in the stem designs were responsible for this subsidence.
2. Patients and methods
Between August 2007 and February 2010, 135 uncemented total hip replacements were performed using the Corail femoral stems and Pinnacle acetabular component (Corail; DePuy Orthopaedics Inc., Warsaw, IN) in 126 patients by two surgeons (IC and APW) in a district general hospital in the UK. One of these surgeons (IC) used the collarless stems, while the other surgeon (APW) used the collared stems for all his patients. We reviewed the outcome of these patients retrospectively. All consecutive primary total hip replacements performed for osteoarthritis, rheumatoid arthritis, avascular necrosis and dysplastic hips using the above implants were included. As a routine, plain radiographs were obtained at first postoperative day, as well as at 6–8 weeks and 1 year follow up. All primary hip replacements performed for fractured neck of femurs and all revision hip replacements were excluded from the study. Patients who lost to follow up were also excluded. The study was approved by the Biomedical Research Ethics Sub-Committee (BREC), University of Warwick, as a service evaluation for subsidence rate for alternative designs of the Corail femoral stems.
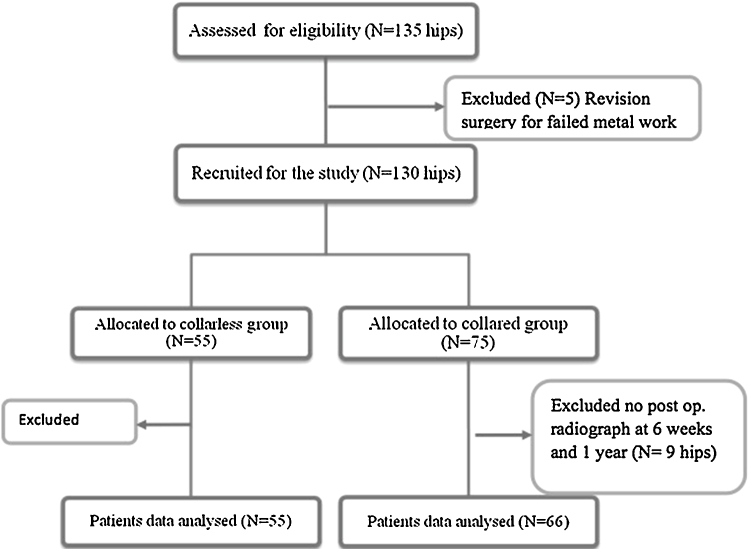
Fourteen hip replacements (13 patients) were further excluded from the study. Five of these were excluded because they had conversion of failed internal fixation for previous hip fractures to total hip replacements, and nine were excluded due to incomplete radiographic follow up at 6–8 weeks or 1 year stages. The remaining 121 hip replacements (113 patients) were considered valid for the study. Fifty-five hip replacements (51 patients) were allocated to the collarless group, and 66 hip replacements (62 patients) were allocated to the collared group. There was no loss to follow up in these patients (Fig. 1).
Fig. 1.
Flow diagram of recruitment of patients.
Radiographic assessment was done on anteroposterior (AP) radiographs obtained at the afore-mentioned follow up intervals and included the degree of subsidence or early migration, angulation, signs of loosening and associated implant complications. Subsidence of the femoral stems was measured comparing the radiographs at the first day after surgery with the radiographs taken at the mean of 1 year using the following technique (Fig. 2):
-
1.
The magnification error (ME) for both the films was minimised. It was measured by a straight line drawn from the centre of the head to the margin of the head, and then dividing the measured value with the actual size of the head used (28 or 36 mm).
-
2.
The distance from the centre of the head to the tip of the stem or the most prominent point of the lesser trochanter (LT), and then divided it by the magnification error.
-
3.
The distance from the tip of greater trochanter (GT) to the shoulder of the stem and then divided it by the magnification error.
-
4.
Calcar height (CH), which is the distance from the most prominent aspect of the medial part of the femoral neck to the tip of the lesser trochanter, divided by the magnification error.
-
5.
Valgus or varus angulation of the stem.
-
6.
The canal-fill ratio at the distal (diaphyseal) and the middle (metaphyseal) third of the stem, measured only on the radiographs at the first day postoperatively.
Fig. 2.
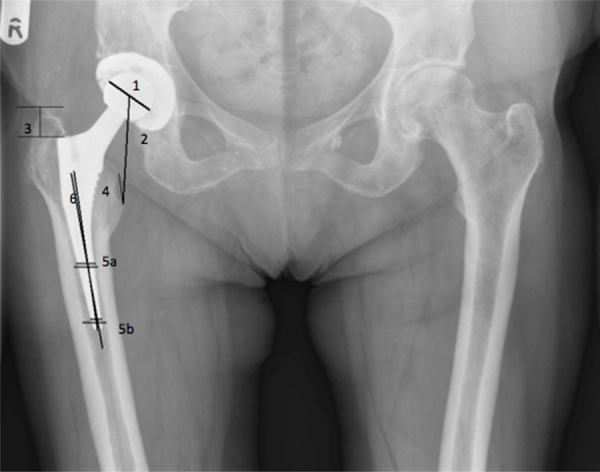
Subsidence measurement. (1) Centre of head for magnification error (ME), (2) centre of head to tip of lesser trochanter (LT), (3) tip of greater trochanter to shoulder of stem (GT), (4) calcar height (CH), (5) canal fill ratio, (5a) middle 1/3, (5b) lower 1/3, (6) varus or valgus angulation.
After obtaining all the required measurements, final calculations were performed. The original measurements were dichotomised, using a distance of 3 mm as the cut off; a value of ≥3 mm was considered to exceed the effects of magnification error, measurement error and observer error. If there was a significant subsidence of 3 mm or more, or stem angulations of 3° or more, then radiographs taken at 6 weeks postoperatively were also reviewed to check for any signs of early subsidence using the same method.
Other signs of stability and fixation were assessed, including new endosteal bone formation (spots of welds), radiolucent lines around the prosthesis in all Gruen zones and pedestal formation.11 Radiolucent lines were considered significant if they were greater than 2 mm; using 7 Gruen zones classification system.12 Other factors that may have contributed to subsidence were evaluated including body mass index (BMI), age, gender, weight bearing status and co-morbidity status (ASA grade).
To test for a difference in the three measurements between the two prostheses on the transformed continuous scale, an ANOVA model was used, with type of prosthesis as the factor and sex, age, BMI, middle-third fill ratio, lower-third fill ratio and ASA score as covariates. For the dichotomised data, a logistic regression model was used to estimate odds ratios, again with type of prosthesis as the factor and with the same covariates. Statistical significance was set at p ≤ 0.05.
3. Results
In both groups, there were comparable distribution of gender; age, BMI, prosthetic size, and prosthetic metaphyseal and diaphyseal fill ratios (Table 1). Combining the two groups, 9% hip replacements (11/121) showed radiographic evidence of subsidence at 1-year follow up. Majority of the subsidence was found to have occurred within the first 6–8 weeks in both groups. 7.6% (5/66) implants in the collared group and 10.9% (6/55) implants in the collarless group showed subsidence within the 6–8 weeks. After this stage, 2 patients had further subsidence of implants and underwent revision at 13 months for the collared stem and 36 months for the collarless stem after primary surgery. No further subsidence was seen in the remaining subsided implants in both groups (Table 1, Table 5).
Table 1.
Baseline data in the two groups.
| Collared group | Collarless group | |
|---|---|---|
| No of patients | 62 | 51 |
| No of hip replacements | 66 | 55 |
| Male | 25 | 26 |
| Female | 38 | 28 |
| Mean age (years) | 68.3 (40–88) | 66 (38–77) |
| Subsidence (3–5 mm) | 4 (6%) | 3 (5.5%) |
| Subsidence (5–10 mm) | 0 | 1 (1.8%) |
| Subsidence (>10 mm) | 1 (1.5%) | 2 (3.6%) |
| Mean stem size | 11 (8–15) | 11.5 (8–18) |
| Stem angulation >3° | 2 | 1 |
| Signs of loosening | 4 | 3 |
| Mean stem size (range) | 11.0 (8.0–15.0) | 11.5(8.0–18.0) |
| Mean BMI (SD) | 27.79 (4.54) | 28.23 (3.59) |
| Mean fill ratio middle third (SD) | 0.78 (0.12) | 0.83 (0.08) |
| Mean fill ratio lower third (SD) | 0.69 (0.10) | 0.72 (0.10) |
| Median ASA grade (IQR) | 2 (2, 3) | 2 (2, 2) |
SD, standard deviation; IQR, interquartile range.
Table 5.
Complications in both groups.
| Complication | Collared group Number (%) |
Collarless group Number (%) |
|---|---|---|
| Surgical site infection | 4 (6%) | 1 (1.8%) |
| Cellulitis | 1 (1.5%) | 1 (1.8%) |
| DVT | 2 (3%) | 2 (3.6%) |
| PE | 0 | 0 |
| Cup revision | 1 (1.5%) | 1 (1.8%) |
| Stem revision | 1 (1.5%) | 1(1.8%) |
| Dislocation | 0 | 0 |
| Iatrogenic fracture | 1 (1.5%) | 0 |
Clinical factors evaluated for subsidence correlation included patient age, BMI, ASA grade, weight bearing status and implant size. In the collared group, an increased BMI was related to increased early subsidence rate. A mean BMI of 27.7 in the subsidence group compared to 28.2 in the non-subsidence group was noticed. This suggested that high BMI might be associated with subsidence, even in the collared implants, because forces up to 3 times body weight are transmitted across the hip joint during mobilisation.13 There were a 13% greater metaphyseal canal-fill ratio and a 9% greater diaphyseal canal-fill ratio in the non-subsidence compared to subsidence group. Therefore a combination of high BMI and low canal-fill ratio may be predictive of clinically significant subsidence on the immediate postoperative radiographs. This may help to identify the patients who require cautious postoperative follow up to pick up early subsidence. In the collarless group there was no clinically significant correlation between BMI, gender, weight bearing status or implant size. However, it was noticed that the patients in the subsidence group were, on an average, 5 years younger and had a mode ASA of 1 compared to mode ASA of 2 in the non-subsistence group. This may suggest that in younger and more active patients, a collared implant, with the extra proximal support to block further migration, may be beneficial. Postoperative complications in both groups are described in Table 5.
All three measurements exhibited a marked positive skew and heterogeneity of variance across the prosthesis groups. A reciprocal transformation was therefore applied to normalise the data and stabilise the variances. On all three measurements, more movement had occurred in the collarless group. These differences (on the transformed data) were significant for the greater trochanter line (p < 0.001) and the calcar height (p = 0.035), but not for the lesser trochanter line (p = 0.236) (Table 2).
Table 2.
Outcome data.
| Measurement | Collared group |
Collarless group |
||
|---|---|---|---|---|
| Mean (SD) | Median (IQR) | Mean (SD) | Median (IQR) | |
| Greater trochanter line | 0.71 (0.90) | 0.30 (0.10, 0.90) | 1.62 (2.06) | 1.20 (0.50, 1.85) |
| Lesser trochanter line | 0.88 (0.88) | 0.50 (0.30, 1.40) | 1.56 (2.06) | 0.80 (0.30, 2.00) |
| Calcar height | 0.99 (1.01) | 0.80 (0.30, 1.50) | 1.33 (0.96) | 1.10 (0.70, 1.95) |
SD, standard deviation; IQR, interquartile range.
The analysis of the patients in whom a movement of 3 mm or more had occurred is shown in Table 3. The results of the logistic regression analysis on the dichotomised data are shown in Table 4. Compared to the collared group, the odds of a 3 mm movement in the collarless group were 2.16 times more with reference to both the greater trochanter line and the lesser trochanter line, and 1.48 times more with reference to the calcar height. However, none of these odds ratios was found significant. The comparative analysis of subsidence group and non-subsidence group is described in detail in Table 6.
Table 3.
Patients in whom a movement of 3 mm or more had occurred.
| Measurement | Collared group Number (%) |
Collarless group Number (%) |
|---|---|---|
| Greater trochanter line | 4 (6) | 6 (11) |
| Lesser trochanter line | 4 (6) | 6 (11) |
| Calcar height | 3 (5) | 3 (6) |
Table 4.
Logistic regression analysis.
| Predictor | Greater/lesser trochanter line# |
Calcar height |
||
|---|---|---|---|---|
| Odds ratio (95% CI) | p value | Odds ratio (95% CI) | p value | |
| Prosthesis (0 = collared, 1 = collarless) | 2.16 (0.44, 10.64) | 0.345 | 1.48 (0.22, 10.00) | 0.689 |
| Nagelkerke pseudo-R2 for model | 0.298 | 0.222 | ||
CI, confidence interval.
Logistic regression analysis.
Table 6.
Comparative analysis of subsidence and non-subsidence groups with both collarless and collared implants.
| Collard group |
Collarless group |
|||
|---|---|---|---|---|
| Non-subsidence Mean (range) |
Subsidence Mean (range) |
Non-subsidence Mean (range) |
Subsidence Mean (range) |
|
| Canal fill ratio (middle-third) | 78% (48–95%) | 65% (48–81%) | 83% (66–95%) | 79% (66–89%) |
| Canal fill ratio (lower-third) | 69% (46–85%) | 60% (40–84%) | 72% (53–92%) | 74% (60–83%) |
| Stem size | 11 (8–15) | 10 (9–12) | 11 (8–15) | 12 (8–18) |
| BMI (kg/m2) | 27.8 (19–40) | 29.4 (23–35) | 28.3 (21–36) | 27.5 (24–34) |
| ASA grade | 2 (1–3) | 2 (2) | 2 (1–3) | 1.3 (1–2) |
| Age | 67.4 (40–88) | 68.8 (55–83) | 66.6 (38–77) | 61.6 (38–77) |
| Male | 39 | 4 | 22 | 3 |
| Female | 20 | 1 | 27 | 3 |
4. Discussion
The Corail femoral implant has shown 96.3% survival at 23 years.2 The implant stability is considered to be due to multiple factors including impaction bone grafting, implant insertion techniques, osteoinductive properties of hydroxyapatite and metaphyseal fit design of the prosthesis. Early subsidence of implants has been reported but the cause remains unclear.3, 5, 8, 9, 10 The initial subsidence may relate to an inadequate cancellous bone impaction intraoperatively. As the patient begins to weight-bear, the hoop stresses transmitted from the implant to the bone, compact the implant further, which leads to subsidence until the mechanical stability is achieved. Most of the osteointegration of the implant typically takes 4–12 weeks but may take up to 3 years.14, 15 The degree of micromotion at the bone–implant interface determines the quality of this biological stability. Micromotion of less than 20 mm is believed to result in osteointegration, whereas micromotion of 150 mm or more is considered to lead to less stable fibrous tissue formation at the bone–implant interface.16, 17, 18 Therefore, first 3 months after surgery are important to achieve successful osteointegration and mechanical stability resulting in minimal movement or subsidence.
The available NJR data for Corail implants provides the combined results for both collared and collarless implants. Therefore it is difficult to ascertain the superiority of one implant design over the other in the short- and long-term.1 The use of a collarless implant allows even loading through the entire surface area of the stem, maximising bony support and force transmission, whereas a collared implant has greater initial preferential proximal stem loading, and thus less force transmission distally, which may negatively impact on distal osteointegration and may allow early implant loosening.2
The correlation between the extent of subsidence visible on plain radiographs and its clinical significance remains unclear. The available literature suggests that as little as 1.5–3 mm radiographic subsidence may prove be clinically significant.3, 6, 16 However the measurement of the extent of subsidence varies, which may lead to inaccurate assessment of the data and difficulty in comparing the available studies. It is generally agreed that less than 1.5 mm subsidence is acceptable, and up to 2 mm is considered within the limits of error for radiographic assessment.6, 16 Campbell et al. reported the results of the collarless implants used in 30 patients.5 Their results showed subsidence of 0.23–3.71 mm at a mean of 2 years follow up. Majority of the subsidence was reported to occur within the first 6 months after surgery (mean 0.5 mm) and less than 0.3 mm further subsistence was seen between 6 and 24 months. This was not found to be clinically significant and no patient required revision surgery, supporting the findings from some other studies that less than 3 mm subsistence is not considered clinically significant.3, 19, 20 The amount of subsidence was greater in our series, but the methods of radiographic assessment of subsidence were different between the two series, making further comparison difficult.
Sudhahar et al. evaluated both the designs of Corail implants.3 In their series, among 39 collarless stems, 28% (11/39) stems showed subsidence of more than 3 mm, which is greater than seen in our series. Two of their patients among this group required revision surgery. Among their collared stems, 7% (3/43) showed subsidence of more than 3 mm. In addition, 5 other collared stems showed an initial subsistence of 1–3 mm, however, this was not found clinically significant. In this group, no implant required revision. Our results were comparable to this series.
In our series, there was proportionally more clinically significant subsidence in the collarless stems compared to the collared stems (10.9% vs. 7.6% respectively). Furthermore, on all three measurements, more movement of the stems was found to have occurred in the collarless group. These differences were significant for the subsidence at the greater trochanter line (p < 0.001) and the calcar height (p = 0.035), but not for the lesser trochanter line (p = 0.236), which demonstrates that the collar prevents further migration once the collar has engaged against the femoral neck cut. However, logistic regression analysis on all implants with greater than 3 mm subsistence in both groups suggested no advantage of the collared implants over the collarless implants.
In the collared group, among those implants which did not show subsidence, there were a 13% greater metaphyseal canal-fill ratio and a 9% greater diaphyseal canal-fill ratio compared to those, which did subside. Being a proximal metaphyseal loading stem, the better proximal medullary fit leads to a greater early mechanical fit, which leads to less distal migration and stable biological osteointegration. This was supported by the fact that in our series, none of the non-subsidence group required revision. Four out of the five collared stems, which showed subsidence initially, did not show any further distal migration once the collar had rested upon the neck cut. In the collarless group, the metaphyseal canal fill ratio was greater in the non-subsidence group by 4% and less at the diaphysis by 2%. In this group, the stems with a better metaphyseal fit did not subside to clinically significant levels and achieved stable biological osteointegration and none of these stems required revision. This indicates that stems, which had clinically significant subsidence, had a greater distal bone impaction providing better implant stability. However, the absence of early proximal metaphyseal stability and poor fibrous osteointegration may have contributed to stems loosening in this group.
4.1. Study limitations
Our study was a retrospective study, therefore the variables could not be controlled, however consecutive data collection was used to minimise selection bias. Radiographs had magnification error, which was calculated prior to taking measurements. All the measurements were performed by the same person, leading to the possibility of intra- and inter-observer errors. Due to being a retrospective study, a standard method of taking the radiographs, with scaling balls, could not be used, which if used, could have minimised the rotational difference between subsequent radiographs enabling more accurate measurements. No clinical scoring system was used to assess the hip function before or after surgery, which could have enabled better correlation between degree of subsidence and functional outcome. However, this study was a service evaluation, and contains sufficient data to construct a power calculation to devise a randomised controlled trail to compare radiological and clinical outcomes related to subsistence of the collared and the collarless uncemented implants. The other strong points of our study include comparable number of patients in both groups, strict exclusion criteria and standardised statistical analysis.
5. Conclusion
In our series, the majority of radiographic subsidence was seen within the first 6–8 weeks after surgery, followed by minimum subsidence for the subsequent 10 months suggesting progressive biological stability and osteointegration. The collarless stems showed significant radiological subsidence (>3 mm) compared to the collared stems, suggesting that the presence of the collar contributed in the prevention of further subsidence once the collar rested upon the femoral neck cut. However, based on the outcomes, we did not find any statistically significant advantage of the collared stems compared to the collarless stems despite reduced subsidence rates. Reduced proximal fill ratios on the immediate postoperative radiographs were found to be predictive of possible subsequent subsidence, and may suggest cautious postoperative follow up, especially in patients with increased BMI. Younger and more active patients with collarless implants had an increased incidence of subsidence, suggesting that they may benefit from collared implants. However, further randomised controlled trials are required to identify the clinical and radiological factors associated with subsidence in these two types of implants.
Conflicts of interest
The authors have none to declare.
Acknowledgments
I am sincerely grateful to Dr Juul Achten (University of Warwick) for her support in completing the project. I thank Mr Moores and Mr Majeed for their advice on the final manuscript.
References
- 1.National Joint Registry for England and Wales (NJR). 9th National Joint Registry Annual Clinical Report 2011. Available from: http://www.njrcentre.org.uk/NjrCentre/Portals/0/Documents/England/Reports/9th_annual_report/NJR 9th Annual Report 2012.pdf.
- 2.Vidalain J.P. Twenty-year results of the cementless Corail stem. Int Orthop. 2011;35(2):189–194. doi: 10.1007/s00264-010-1117-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sudhahar T.A., Morapudi S., Barnes K. Evaluation of subsidence between collarless and collared Corail femoral cementless total hip replacement. J Orthop. 2009;6(2):e3. [Google Scholar]
- 4.Berend M.E. Cemented femoral fixation: a historical footnote. Orthopedics. 2006;29(9):791–792. doi: 10.3928/01477447-20060901-03. [DOI] [PubMed] [Google Scholar]
- 5.Campbell D., Mercer G., Nilsson K.G., Wells V., Field J.R., Callary S.A. Early migration characteristics of a hydroxyapatite-coated femoral stem: an RSA study. Int Orthop. 2011;35(4):483–488. doi: 10.1007/s00264-009-0913-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kärrholm J., Borssén B., Löwenhielm G., Snorrason F. Does early micromotion of femoral stem prostheses matter? 4–7-year stereoradiographic follow-up of 84 cemented prostheses. J Bone Jt Surg Br. 1994;76(6):912–917. [PubMed] [Google Scholar]
- 7.Kärrholm J., Herberts P., Hultmark P., Malchau H., Nivbrant B., Thanner J. Radiostereometry of hip prostheses. Review of methodology and clinical results. Clin Orthop Relat Res. 1997;(344):94–110. [PubMed] [Google Scholar]
- 8.Krismer M., Biedermann R., Stöckl B., Fischer M., Bauer R., Haid C. The prediction of failure of the stem in THR by measurement of early migration using EBRA-FCA. Einzel-Bild-Roentgen-Analyse-femoral component analysis. J Bone Jt Surg Br. 1999;81(2):273–280. doi: 10.1302/0301-620x.81b2.8840. [DOI] [PubMed] [Google Scholar]
- 9.Ström H., Mallmin H., Milbrink J., Petrén-Mallmin M., Nivbrant B., Kolstad K. The cone hip stem: a prospective study of 13 patients followed for 5 years with RSA. Acta Orthop Scand. 2003;74(5):525–530. doi: 10.1080/00016470310017901. [DOI] [PubMed] [Google Scholar]
- 10.Ström H., Nilsson O., Milbrink J., Mallmin H., Larsson S. Early migration pattern of the uncemented CLS stem in total hip arthroplasties. Clin Orthop Relat Res. 2007;454:127–132. doi: 10.1097/01.blo.0000238785.98606.9d. [DOI] [PubMed] [Google Scholar]
- 11.Engh C.A., Massin P., Suthers K.E. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990;(257):107–128. [PubMed] [Google Scholar]
- 12.Gruen T.A., McNeice G.M., Amstutz H.C. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;(141):17–27. [PubMed] [Google Scholar]
- 13.Barrett D. Butterworth Heinemann; Oxford: 1994. Essential Basic Sciences for Orthopaedics. [Google Scholar]
- 14.Albrektsson T., Brånemark P.I., Hansson H.A., Lindström J. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981;52(2):155–170. doi: 10.3109/17453678108991776. [DOI] [PubMed] [Google Scholar]
- 15.Galante J., Rostoker W., Lueck R., Ray R.D. Sintered fiber metal composites as a basis for attachment of implants to bone. J Bone Jt Surg Am. 1971;53(1):101–114. [PubMed] [Google Scholar]
- 16.Engh C.A., O’Connor D., Jasty M., McGovern T.F., Bobyn J.D., Harris W.H. Quantification of implant micromotion, strain shielding, and bone resorption with porous-coated anatomic medullary locking femoral prostheses. Clin Orthop Relat Res. 1992;(285):13–29. [PubMed] [Google Scholar]
- 17.Jasty M., Bragdon C., Burke D., O’Connor D., Lowenstein J., Harris W.H. In vivo skeletal responses to porous-surfaced implants subjected to small induced motions. J Bone Jt Surg Am. 1997;79(5):707–714. doi: 10.2106/00004623-199705000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Pilliar R.M., Lee J.M., Maniatopoulos C. Observations on the effect of movement on bone ingrowth into porous-surfaced implants. Clin Orthop Relat Res. 1986;(208):108–113. [PubMed] [Google Scholar]
- 19.Butt A.J., Weeks G., Curtin W., Kaar K. Early experience with uncemented primary total hip arthroplasty using Corail stems and Duraloc cups. J Bone Jt Surg Br. 2005;87-B(III):269. [Google Scholar]
- 20.Khatib Y.S.O., Mendes D.G., Said M. Corail stem for total hip arthroplasty: 11 years of imaging follow-up. J Bone Jt Surg Br. 2002;84-B(III):301. [Google Scholar]