Abstract
Background
Traffic noise can induce stress reactions that have effects on the cardiovascular system. The exposure–risk relationship between aircraft, road, and rail traffic noise and myocardial infarction is currently unknown.
Method
19 632 patients from the Rhine-Main region of Germany who were diagnosed with myocardial infarction in the years 2006–2010 were compared with 834 734 control subjects. The assignment of persons to groups was performed on the basis of billing and prescription data from three statutory health insurance carriers. The exposure of all insurees to aircraft, road, and rail traffic noise in 2005 was determined from their residence addresses. As estimators of risk, odds ratios (OR) were calculated by logistic regression analysis, with adjustment for age, sex, regional social status variables, and individual social status (if available). The evaluation was performed on the basis of the continuous 24-hour noise level and the categorized noise level (in 5 decibel classes).
Results
The linear model revealed a statistically significant risk increase due to road noise (2.8% per 10 dB rise, 95% confidence interval [1.2; 4.5]) and railroad noise (2.3% per 10 dB rise [0.5; 4.2]), but not airplane noise. Airplane noise levels of 60 dB and above were associated with a higher risk of myocardial infarction (OR 1.42 [0.62; 3.25]). This higher risk is statistically significant if the analysis is restricted to patients who had died of myocardial infarction by 2014/2015 (OR 2.70 [1.08; 6.74]. In this subgroup, the risk estimators for all three types of traffic noise were of comparable magnitude (3.2% to 3.9% per 10 dB rise in noise level).
Conclusion
In this study, a substantial proportion of the population was exposed to traffic noise levels that were associated with an albeit small increase in the risk of myocardial infarction. These findings underscore the importance of effective traffic noise prevention.
Traffic noise can trigger complex psychological and physiological stress reactions. In terms of the effects of traffic noise on the cardiovascular system, activation of the sympathetic nervous system is regarded as the chief mechanism, along with activation of the hypothalamus–pituitary–adrenal axis (1). The World Health Organization (WHO) estimates that in the western part of Europe at least 1 million disability-adjusted life years (DALYs) are lost due to diseases induced by traffic noise (2). “Disability-adjusted life years” means the total number of life years lost due to premature death and life years spent with a disease-related disability; severe disability is weighted more heavily in the calculation than mild disability.
Several studies have investigated the relationship between traffic noise and cardiovascular disease. In a recently published systematic review with meta-analysis, Vienneau and colleagues (3) analyzed three studies of the relationship between aircraft noise and ischemic heart disease including myocardial infarction (4– 6). In their results, they calculated a pooled relative risk of 1.06 (95% confidence interval [95% CI]: [1.04–1.08]) per 10 dB Lden aircraft or road traffic noise. “Lden” is the term used to refer to the weighted day–evening–night sound level, where 5 dB is added to the evening noise and 10 dB to the night-time noise. In the systematic review by Vienneau et al. (3), different average sound level indicators were converted to the Lden: for example, 1.5 dB were added to the 24-hour continuous noise level in order to estimate the Lden.
By comparison, very little is known about the effects of rail traffic noise. In a Swedish study, Eriksson and colleagues found a statistically insignificant correlation between rail traffic noise and a self-reported diagnosis of coronary heart disease (7).
At present the exact nature of the exposure–risk relationship between aircraft, road, and rail traffic noise and defined cardiovascular diseases such as myocardial infarction (MI) remains obscure. The case–control study presented here should help filling this gap. The full scientific report is available on the internet (8).
Method
Full details of the methods used are given in eBox 1.
eBox 1. Methods.
-
Study area and study population:
The study area consisted of the administrative district of Darmstadt, the cities of Mainz and Worms, and the rural districts of Mainz-Bingen and Alzey-Worms (Figure). The study population included all persons aged over 40 insured with one of the three large statutory health insurers in the study area (n = 1 026 670; corresponding to about 23% of the over 40-year-olds in the study area).
-
Noise exposure in the study area:
The engineering firm Möhler und Partner Ingenieure AG provided address-specific external noise levels data (relating to streets with house numbers) for aircraft noise (based on radar tracks of individual flights) and road and rail traffic noise in the study area (for details see [9]). The reference year for noise exposure chosen was 2005. Traffic noise levels were calculated in accordance with current regulations (10–12). To aid interpretation of the traffic noise levels, Table 1 gives some examples of sound sources together with their respective noise levels in decibels (dB).
-
Linking the diagnostic data to the noise data:
Participating insurers delivered pseudonymized claims and prescription data to the evaluation center in Dresden (study IDs were added, but no names or addresses were supplied). From this information, cases of myocardial infarction and control cases without myocardial infarction were selected. The following information was transferred, separately for each reporting year from 2005 to 2010: key data of the insured person, diagnostic data (ICD-10; divided into outpatient and inpatient care), and prescription data according to the anatomic therapeutic chemical (ATC) classification code. Noise data were linked to the address data of the insured persons by an external trust center at the Leibniz Institute for Prevention Research and Epidemiology BIPS in the case of two insurers and in the case of the third insurer by the insurer’s own linkage department. Noise data were successfully linked to address data for 95.5% of the study population (n = 907 736). The addresses were then replaced by the study IDs and passed on to the evaluation center in Dresden, where the diagnostic data and noise data were merged.
-
Myocardial infarction cases (n = 19 632):
In order to best assess incident cases and facilitate the exclusion of prevalent cases in this secondary-data-based study, patients were included as cases only if they had an acute myocardial infarction (MI) (ICD-10: I21; Table 2) coded during the reporting period of 2006 to 2010—that is, after the measured noise exposure (13). A diagnosis-free period of at least four consecutive quarterly periods before the MI event was required; however, this requirement cannot exclude the possibility of an infarction event occurring prior to the observed time period.
-
Control subjects (n = 834 734):
Control subjects were drawn from the pool of all insured persons (including family members insured on their policy). The study control subjects consisted of all insured persons without a diagnosis of MI (including a confirmed outpatient diagnosis) during the relevant reporting period of 2005 to 2010, who were at least 40 years old in 2010 or in the year in which their insurance ceased, and who were insured for at least four consecutive quarterly periods during the entire reporting period.
-
Statistical analysis:
Logistic regression analysis was used to calculate odds ratios (OR) with 95% confidence intervals (95% CI) as effect estimates of the relative disease risks. In the analysis of the categorized noise levels (5 dB classes), people exposed to a 24-hour continuous noise level <40 dB were assigned to the reference category; for aircraft noise, people exposed to a 24-hour continuous noise level <40 dB and a night-time maximum ≥ 50 dB were removed from the reference category and analyzed in a category of their own. Overall, 89.4% of people included in the study were exposed to road traffic noise higher than the reference category, 46.4% to rail traffic noise higher than the reference category, and 90.1% to aircraft noise higher than the reference category. In another analysis, only people who had not been exposed to any traffic noise ≥ 40 dB were placed in the reference category. In addition, the continuous noise levels were included as a linear term in the logistic regression analyses. A subgroup analysis included only the patients with MI (diagnosed 2006–2010) who had died by 2014/2015 (irrespective of cause of death). The vital status of MI patients was checked by the health insurers, but no causes of death could be ascertained. The date on which vital status data were collected varied between the insurers (between February 2014 for insurer #1 and January 2015 for insurer #3). The different modes of traffic noise were always assessed in separate models. In an additional analysis, the three different modes of traffic noise were included together in a single logistic regression model.
-
Confounding factors:
Age (as a third-degree polynomial), sex, and social status were included as confounders in the statistical analysis. Cases were included in the analysis with their age at the time of the MI diagnosis. The median year of diagnosis of the MI patients was 2008, so control subjects were included in the analysis according to their age in 2008, but had to be at least 40 years old at the end of the observation period (2010). Because of data protection, we had only birth years, not exact birth dates. People were taken to be at least 40 years old in 2010 if their birth year was 1970 or earlier. For both cases and controls, the (city or rural district-related) SGB-II rate (percentage of persons under the age of 65 years receiving social welfare payments; SGB, German Social Code, Sozialgesetzbuch) was included in the logistic regression model as an aggregate social status variable. Where the five-character occupation code was available, additional adjustment was made for the individual’s education (available for 29.4% of the study population) and occupational classification according to Blossfeld (14) (available for 32.4%); missing values were included in the regression model as a separate category. A subanalysis included only persons whose individual social status (individual educational level and/or occupation) was known.
Study area and study population
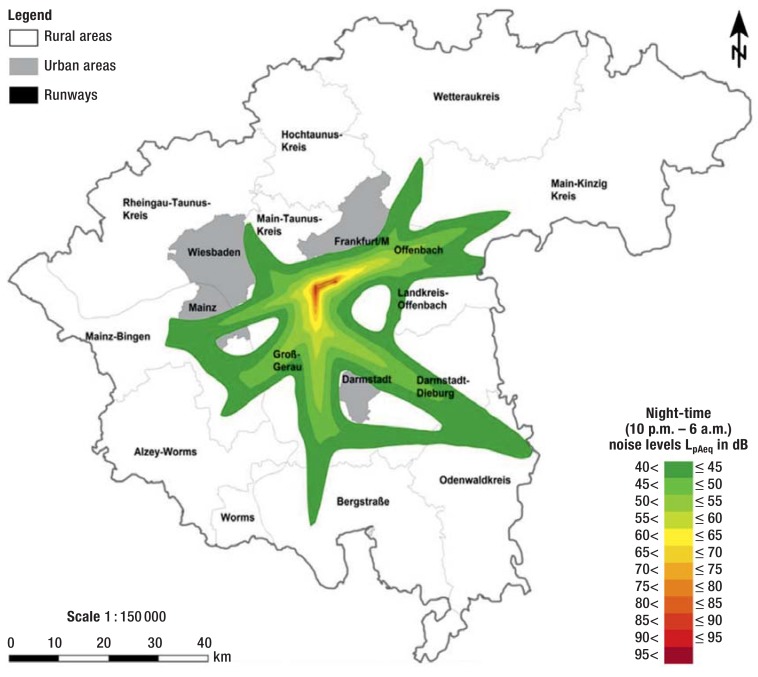
The study area consisted of the administrative district of Darmstadt, the cities of Mainz and Worms, and the rural districts of Mainz-Bingen and Alzey-Worms (Figure). The study population consisted of all persons over the age of 40 who were insured with one of three large state health insurers in the study area (n = 1 026 670).
Figure.
Aircraft noise in the hours between 10 p.m. and 6 a.m. in 2005
Study area in the case–control study based on secondary data (gray outline), showing examples of continuous noise level contours for night-time aircraft noise exposure during 2005 (adapted from [8]); areas in which the night-time (10 p.m. to 6 a.m.) mean level LpAeq of aircraft noise was below 40 dB are shown in white.
pAeq, energy-equivalent continuous noise level; Kreis, district
Noise exposure in the study area
The engineering company Möhler und Partner Ingenieure AG provided address-specific external noise level data for aircraft, road, and rail traffic noise in the study area for 2005 (9). Traffic noise levels were calculated in accordance with current German regulations (10– 12). Further details on traffic noise calculation are given in eBox 2. To aid interpretation of the traffic noise levels, Table 1 gives some examples of sound sources together with their respective noise levels in decibels (dB).
eBox 2. Calculation of traffic noise levels.
Aircraft noise levels were calculated according to appendix 2 of the first regulations for data collection and the calculation procedure for the determination of noise control zones, directions for calculating noise control zones (1. Verordnung über die Datenerfassung und das Berechnungsverfahren für die Festsetzung von Lärmschutzbereichen, Anleitung zur Berechnung von Lärmschutzbereichen) (98), using radar tracks of the individual flights. The noise emissions from road and rail traffic were determined using the 34th set of regulations for implementation of the Federal Emissions Control Act (Bundes-Immissionsschutzgesetz) (10, 11). For this case -control study based on secondary data, the 24-hour continuous noise level (LpAeq,24h) together with the mean noise levels for the night-time hours (10 p.m. to 6 a.m.) and the corresponding day-time hours (6 a.m. to 10 p.m.) were made available separately for the three different modes of traffic noise (external noise level, loudest façade) for the reference year 2005. For aircraft noise, other night-time periods were also available (11 p.m. to 5 a.m., 11 p.m. to 7 a.m., individual hours between 10 p.m. and 8 a.m.). In addition, the maximum sound pressure level (LpAmax) was known (this is used to describe the noise level reached or exceeded by six flights during the night hours between 10 p.m. and 6 a.m.).
Table 1. Examples of sources of noise and their sound levels in decibels (dB)*.
| Noise | Loudness |
|---|---|
| Quiet ticking of a clock; steady light rain; whispering | 30 dB |
| Whispering close-up; quiet residential street | 40 dB |
| Conversational speech | 50 dB |
| Conversational speech 1 m away | 60 dB |
| Loud conversation; shouting; car 10 m away | 70 dB |
| Street noise with a lot of traffic | 80 dB |
| Loud factory | 90 dB |
| Car honking 7 m away | 100 dB |
*Sound pressure is given on a logarithmic scale in decibels (dB); the threshold of hearing is at 0 dB. A 10 dB change in sound pressure level is roughly equivalent to doubling or halving of the subjectively perceived sound volume. The amount of energy transported with the sound varies with the sound pressure level. The energy-equivalent continuous sound level (LpAeq) underlying the study presented here has been chosen such that—regarded as a constant sound pressure level—it would transport the same energy content. The continuous sound level serves to give the burden of noise for a defined period of time—in the analysis underlying the present study, 24 hours. If a noise emission lasts for only a tenth of the time, the mean continuous sound level goes down by 10 dB; if the noise emission lasts for only one-hundredth of the time, the mean continuous sound level goes down by 20 dB. In this way, for example, a 24-hour continuous sound level of 50 dB can result from a 24-hour noise emission of 50 dB or from a noise emission of 70 dB lasting about 15 minutes. Adapted from http://www.bmub.bund.de/themen/luft-laerm-ver kehr/laermschutz/laermschutz-im-ueberblick/was-ist-laerm/
Linking the diagnostic data to the noise data
Participating insurers delivered pseudonymized billing information to the evaluation center in Dresden, and this information was used for the selection of cases with MI and control cases without MI. Linking of the noise data to the address data of the insured persons was carried out by an external trust center. Noise data were successfully linked to address data for 95.5% of the insured persons (n = 907 736).
Myocardial infarction cases (n = 19 632)
In order best assess incident cases and facilitate the exclusion of prevalent cases in this study based on secondary data, patients were included as cases only if they had an acute MI (ICD-10: I21; Table 2) coded during the reporting period of 2006 to 2010—that is, after the measured exposure (13).
Table 2. Definition of myocardial infarction.
| ICD-10 Classification | Myocardial infarction* |
|---|---|
| I21.-: Acute myocardial infarction | 1 × inpatient discharge diagnosis or secondary diagnosis I21.- |
| 1× outpatient confirmed diagnosis I21.- (“g”) and death during the same quarter as the diagnosis or the following quarter |
*The presence of either of the two criteria sufficed to define a myocardial infarction
Controls (n = 834 734)
The study control subjects consisted of all insured persons without a diagnosis of MI (including a confirmed outpatient diagnosis) during the relevant reporting period of 2005 to 2010, who were at least 40 years old in 2010 or in the year in which their insurance ceased, and who were insured for at least four consecutive 3-month periods (quarterly insurance periods) during the entire reporting period.
Statistical analysis
Logistic regression analysis was used to calculate odds ratios (OR) with 95% confidence intervals as effect estimates of the relative disease risks. In the analysis of categorized noise levels (5 dB categories), people exposed to a 24-hour continuous noise level <40 dB were assigned to the reference category; for aircraft noise, people exposed to a 24-hour continuous noise level <40 dB and a night-time maximum ≥ 50 dB were removed from the reference category and analyzed in a category of their own. In another analysis, only people who had not been exposed to any traffic noise ≥ 40 dB were placed in the reference category. In addition, the continuous noise levels were included as a linear term in the logistic regression analyses.
A subgroup analysis included only patients with MI (diagnosed 2006–2010) who had died by 2014/2015 (irrespective of cause of death). The different modes of traffic noise were always assessed in separate models. In an additional analysis, the three different modes of traffic noise were included together in one logistic regression model.
Confounding factors
Age, sex, and social status were included as confounding variables in the statistical analysis. For all cases and controls, the (city or rural district-related) SGB-II rate (percentage of population under the age of 65 years receiving social welfare payments; SGB, German Social Code, Sozialgesetzbuch) was included in the logistic regression model as an aggregate social status variable. Where the five-character occupation code was available, additional adjustment was made for the individual’s education (available for 29.4% of the study population) and occupational classification according to Blossfeld (14) (available for 32.4%). A subanalysis included only persons whose individual social status (individual educational level and/or occupation) was known.
Results
eTable 1 lists the characteristics of cases and controls. The population-related higher incidence of MI in men is reflected in the fact that 56.5% of the MI patients are male, compared with only 43.4% of the control subjects. Patients with a diagnosis of MI (median age 74 years, interquartile range 65 to 82 years) are, as would be expected, on average older than control subjects (median age 60 years, interquartile range 48 to 72 years). Of the MI patients whose occupation is known, 23% had graduated from university or finished high school, versus 17% of control subjects. Regional SGB-II rates are similar for MI patients and control subjects.
eTable 1. Characteristics of myocardial infarction cases and control subjects.
| Cases | Controls | |||
|---|---|---|---|---|
| n | % | n | % | |
| Total | 19632 | 100.0 | 834734 | 100.0 |
| Sex | ||||
| Male | 11088 | 56.5 | 362665 | 43.4 |
| Female | 8544 | 43.5 | 472069 | 56.3 |
| Age (years) | ||||
| 35 –<45 | 306 | 1.6 | 131344 | 15.7 |
| 45 –<50 | 566 | 2.9 | 98758 | 11.8 |
| 50 –<55 | 921 | 4.7 | 88834 | 10.6 |
| 55 –<60 | 1282 | 6.5 | 88073 | 10.6 |
| 60 –<65 | 1522 | 7.8 | 79161 | 9.5 |
| 65 –<70 | 2331 | 11.9 | 93737 | 11.2 |
| 70 –<75 | 2908 | 14.8 | 89291 | 10.7 |
| 75 –<80 | 3065 | 15.6 | 63744 | 7.6 |
| 80 –<85 | 3128 | 15.9 | 51144 | 6.1 |
| ≥ 85 | 3603 | 18.4 | 50648 | 6.1 |
| Participating insurers | ||||
| Insurer 1 | 12999 | 66.2 | 525698 | 63.0 |
| Insurer 2 | 1620 | 8.3 | 61562 | 7.4 |
| Insurer 3 | 5013 | 25.5 | 247474 | 29.6 |
| Educational status | ||||
| Elementary/general school without vocational qualification | 733 | 3.7 | 66016 | 7.9 |
| Elementary/general school with vocational qualification | 1351 | 6.9 | 141006 | 16.9 |
| High school without vocational qualification | 109 | 0.6 | 4425 | 0.5 |
| High school with vocational qualification | 247 | 1.3 | 14220 | 1.7 |
| Technical college | 196 | 1.0 | 10662 | 1.3 |
| University | 76 | 0.4 | 11762 | 1.4 |
| Educational status unknown. No details available. | 16920 | 86.2 | 586643 | 70.3 |
| Occupational classification (Blossfeld) | ||||
| Farming | 28 | 0.1 | 3043 | 0.4 |
| Unskilled manual work | 394 | 2.0 | 35647 | 4.3 |
| Skilled manual work | 370 | 1.9 | 33672 | 4.0 |
| Technician | 65 | 0.3 | 5300 | 0.6 |
| Engineer | 20 | 0.1 | 2285 | 0.3 |
| Unskilled service jobs | 695 | 3.5 | 62572 | 7.5 |
| Skilled service jobs | 67 | 0.3 | 11937 | 1.4 |
| Semiprofessional | 79 | 0.4 | 20185 | 2.4 |
| Professional | 14 | 0.1 | 2259 | 0.3 |
| Unqualified office worker in business or administration | 172 | 0.9 | 25030 | 3.0 |
| Qualified office worker in business or administration | 414 | 2.1 | 59454 | 7.1 |
| Manager | 49 | 0.2 | 5715 | 0.2 |
| Other | 70 | 0.4 | 7682 | 0.9 |
| No information about occupation | 17195 | 87.6 | 559953 | 67.1 |
| Regional SGB-II rate (quintiles)* | ||||
| ≤ 6.7% | 6472 | 33.0 | 277988 | 33.3 |
| >6.7 – ≤ 7.5% | 3041 | 15.5 | 135782 | 16.3 |
| >7.5 – ≤ 8.7% | 2789 | 14.2 | 92052 | 11.0 |
| >8.7 – ≤ 12.7% | 5406 | 27.5 | 246977 | 29.6 |
| >12.7% | 1924 | 9.8 | 81935 | 9.8 |
*Division of SGB-II rate into quintiles: in dividing the probands into quintiles, we always tried to ensure that each quintile contained 20% of the probands. However, because of the frequent repetition of SBG-II rates, the final distribution was uneven
Relationship between aircraft noise and MI
Up to an aircraft noise level of 55 dB, the effect sizes are around 1 (Table 3). The odds ratio (OR) rises to 1.42 (95% CI: [0.62; 3.25]) in the highest noise level category of >60 dB, but does not achieve statistical significance because of small case numbers. For people exposed to a night-time maximum noise level of over 50 dB with a 24-hour continuous noise level of <40 dB, the OR is 1.05 (95% CI: [0.98; 1.11]). If the 24-hour continuous noise level is included in the logistic regression model as a continuous variable, no statistically significant risk estimates are found.
Table 3. Traffic noise (LpAeq,24h, LpAeq,night) and incident myocardial infarction.
| Aircraft noise | Road traffic noise | Rail traffic noise | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Exposure | Cases | Controls | OR | 95% CI | Cases | Controls | OR | 95% CI | Cases | Controls | OR | 95% CI |
| 24h continuous noise level | ||||||||||||
| <40 db, max. <50 db | 7885 | 328815 | 1.00 | – | 2167 | 88177 | 1.00 | – | 10725 | 446965 | 1.00 | – |
| <40 db, max. ≥ 50 db | 1346 | 52825 | 1.05 | [0.98; 1.11] | ||||||||
| ≥ 40 – <45 db | 5839 | 249666 | 1.01 | [0.97; 1.05] | 4308 | 177419 | 1.02 | [0.96; 1.07] | 2445 | 104139 | 1.04 | [0.99; 1.09] |
| ≥ 45 – <50 db | 3029 | 134464 | 1.00 | [0.95; 1.05] | 4627 | 200544 | 0.99 | [0.94; 1.05] | 2966 | 132524 | 1.00 | [0.96; 1.05] |
| ≥ 50 –<55 db | 1151 | 52923 | 0.97 | [0.91; 1.04] | 3340 | 148430 | 1.01 | [0.96; 1.07] | 2115 | 91861 | 1.05 | [1.00; 1.10] |
| ≥ 55 – <60 db | 376 | 15845 | 1.06 | [0.95; 1.18] | 2171 | 91493 | 1.05 | [0.99; 1.11] | 823 | 36040 | 1.04 | [0.97; 1.12] |
| ≥ 60–<65 db | 6 | 196 | 1.42 | [0.62; 3.25] | 1637 | 68672 | 1.09 | [1.02; 1.16] | 340 | 13783 | 1.10 | [0.98; 1.23] |
| ≥ 65 – <70 db | – | – | – | – | 1069 | 46715 | 1.06 | [0.98; 1.15] | 138 | 5962 | 1.14 | [0.96; 1.36] |
| ≥ 70 dB | – | – | – | – | 313 | 13284 | 1.13 | [1.00; 1.27] | 80 | 3460 | 1.16 | [0.93; 1.46] |
| Continuous (pro 10 dB) | 0.993 | [0.966; 1.020] | 1.028 | [1.012; 1.045] | 1.023 | [1.005; 1.042] | ||||||
| p = 0.606 | p = 0.001 | p= 0.014 | ||||||||||
| Night hours 10 p.m. to 6 a.m. | ||||||||||||
| <40 db, max. <50 db | 9073 | 380331 | 1.00 | – | 8139 | 337086 | 1.00 | – | 10703 | 443563 | 1.00 | – |
| <40 db, max. ≥ 50 db | 5211 | 222319 | 1.00 | [0.96; 1.03] | ||||||||
| ≥ 40 – <45 db | 3319 | 140511 | 0.99 | [0.95; 1.04] | 3879 | 169775 | 1.00 | [0.96; 1.04] | 2392 | 102929 | 1.01 | [0.96; 1.06] |
| ≥ 45 – <50 db | 1382 | 65738 | 0.95 | [0.89; 1.01] | 2999 | 131960 | 1.00 | [0.96; 1.05] | 2832 | 127897 | 1.00 | [0.96; 1.05] |
| ≥ 50 – <55 db | 623 | 24693 | 1.07 | [0.98; 1.17] | 2302 | 95548 | 1.07 | [1.02; 1.12] | 2190 | 94192 | 1.04 | [0.99; 1.09] |
| ≥ 55 – <60 db | 24 | 1142 | 0.99 | [0.66; 1.49] | 1557 | 67195 | 1.07 | [1.01; 1.13] | 916 | 40916 | 1.02 | [0.95; 1.10] |
| ≥ 60 dB | 0 | 0 | – | – | 756 | 33170 | 1.07 | [0.99; 1.15] | 599 | 25237 | 1.10 | [1.01; 1.20] |
| Night hours 11 p.m. to 5a.m. | ||||||||||||
| <40 db, max. <50 db | 9114 | 382121 | 1.00 | – | ||||||||
| <40 db, max. ≥ 50 db | 6025 | 257513 | 0.99 | [0.96; 1.03] | ||||||||
| ≥ 40 – <45 db | 2848 | 123392 | 0.99 | [0.95; 1.03] | ||||||||
| ≥ 45 – <50 db | 1256 | 55504 | 0.98 | [0.92; 1.05] | ||||||||
| ≥ 50 – <55 db | 381 | 15955 | 1.05 | [0.94; 1.17] | ||||||||
| ≥ 55 – <60 db | 8 | 249 | 1.50 | [0.73; 3.07] | ||||||||
| ≥ 60 dB | 0 | 0 | – | – | ||||||||
OR: odds ratio, adjusted for age, sex, education, and occupation (from occupation code), SGB-II rate(quintile); LpAeq.24h: unweighted 24h-continuous noise level; LpAeq.night: average sound level indicator for the night hours 10 p.m. to 6 a.m. and 11 p.m. to 5 a.m.; 95% CI: 95% confidence interval
In all night-time periods the effect sizes are around 1 in the noise level categories up to <50 dB. In higher noise level categories, the increases in risk are not significant. If individual hours are analyzed, a statistically significantly increased risk of MI is shown only for the time between 5.00 and 6.00 a.m. with an aircraft noise level between 55 and <60 dB (OR: 1.25; 95% CI: [1.05; 1.48]); the corresponding OR for the time between 6.00 and 7.00 a.m. is of borderline statistical significance (OR: 1.12; 95% CI: [1.00; 1.25]). Analysis of the night-time maximum noise level shows a non-significantly increased risk of MI for noise between 70 and 80 dB OR: 1.07; 95% CI: [0.96; 1.19]).
Relationship between road traffic noise and MI
Increased risk estimates can be seen starting from a road traffic noise level of 55 dB: the OR reaches statistical significance at a noise level between 60 dB and <65 dB (OR: 1.09; 95% CI: [1.02; 1.16]); the highest OR of 1.13 (95% CI: [1.00; 1.27]) is found with a 24-hour continuous noise level ≥ 70 dB. When the 24-hour continuous noise level is included as a continuous variable in the logistic regression model, a statistically significant risk increase of 2.8% per 10 dB road traffic noise is seen. Looking at the night-time hours between 10 p.m. and 6 a.m., the risk of MI increases when road traffic noise increases above 50 dB (statistically significant in some cases).
Relationship between rail traffic and MI
For rail traffic, in the 50 to <55 dB category there is a statistically borderline significantly raised OR of 1.05 (95% CI: [1.00; 1.10]); in the 55 to <60 dB category the OR is 1.04 (95% CI: [0.97; 1.12]); while in the highest sound level category, 70 dB and upwards, the OR is 1.16 (95% CI: [0.93; 1.46]). When the 24-hour continuous noise level is included as a continuous variable in the logistic regression model, a statistically significant risk increase of 2.3% is seen per 10 dB increase in rail traffic noise. Considering the night-time hours from 10 p.m. to 6 a.m, the ORs begin to rise notably at noise levels of ≥ 60 dB (OR: 1.10; 95% CI: [1.01; 1.20]).
Esimated risks of fatal MI related to traffic noise
In the interval between their first diagnosis (2006 to 2010) and the selection of insurees to be invited by the insurers to take part in a supplementary survey (2014/2015), about 53% of the MI patients died. If only these cases are included in the analysis (eTable 2), a statistically significant OR of 2.70 (95% CI: [1.08; 6.74]) for aircraft noise with a 24-hour continuous noise level of ≥ 60 dB is observed. In all analyses, higher risk estimates are given for all three modes of traffic noise when the case group is restricted to MI patients who died than when all MI patients are included: thus, in the linear model a risk increase of 3.2% (95% CI: [–5.6; 7.1]) is seen per 10 dB increase in the level of aircraft noise, an increase of 3.9% (95% CI: [1.6; 6.3]) per 10 dB increase in the level of road traffic noise, and an increase of 3.8% (95% CI: 1.2; 6.4]) per 10 dB increase in the level of rail traffic noise.
eTable 2. Traffic noise (LpAeq,24h, LpAeq,night) and fatal myocardial infarction*.
| Aircraft noise | Road traffic noise | Rail traffic noise | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Exposure | Cases | Controls | OR | 95% CI | Cases | Controls | OR | 95% CI | Cases | Controls | OR | 95% CI |
| 24-h continuous noise level | ||||||||||||
| <40 db, max. <50 db | 4021 | 328815 | 1.00 | – | 1160 | 88177 | 1.00 | – | 5638 | 446965 | 1.00 | – |
| <40 db, max. ≥ 50 db | 703 | 52825 | 1.07 | [0.98; 1.16] | ||||||||
| ≥40 – <45 db | 3121 | 249666 | 1.06 | [1.01; 1.12] | 2257 | 177419 | 1.01 | [0.94; 1.08] | 1264 | 104139 | 1.04 | [0.97; 1.10] |
| ≥45 – <50 db | 1649 | 134464 | 1.08 | [1.01; 1.15] | 2433 | 200544 | 0.99 | [0.92; 1.07] | 1566 | 132524 | 1.01 | [0.96; 1.07] |
| ≥50 –<55 db | 605 | 52923 | 1.03 | [0.94; 1.12] | 1708 | 148430 | 1.00 | [0.92; 1.08] | 1093 | 91861 | 1.06 | [0.99; 1.13] |
| ≥ 55 – <60 db | 198 | 15845 | 1.09 | [0.94; 1.27] | 1146 | 91493 | 1.05 | [0.97; 1.14] | 427 | 36040 | 1.05 | [0.95; 1.16] |
| ≥ 60–<65 db | 5 | 196 | 2.70 | [1.08; 6.74] | 875 | 68672 | 1.13 | [1.03; 1.24] | 206 | 13783 | 1.26 | [1.10; 1.46] |
| ≥ 65 – <70 db | 0 | – | 563 | 46.715 | 1.09 | [0.98; 1.21] | 68 | 5962 | 1.14 | [0.89; 1.45] | ||
| ≥ 70 dB | 0 | – | – | 160 | 13284 | 1.12 | [0.95; 1.33] | 40 | 3460 | 1.21 | [0.88; 1.66] | |
| Continuous (pro 10 dB) | 1.032 | [0.944; 1.071] | 1.039 | [1.016; 1.063] | 1.038 | [1.012; 1.064] | ||||||
| p=0.097 | p=0.001 | p= 0.004 | ||||||||||
| Night hours 10 p.m. to 6 a.m. | ||||||||||||
| <40 db, max. <50 db | 4637 | 380331 | 1.00 | – | 4314 | 337086 | 1.00 | – | 5639 | 443563 | 1.00 | – |
| <40 db, max. ≥ 50 db | 2773 | 222319 | 1.04 | [0.98; 1.09] | ||||||||
| ≥ 40 – <45 db | 1813 | 140511 | 1.07 | [1.01; 1.13] | 1976 | 169775 | 0.97 | [0.92; 1.03] | 1231 | 102929 | 0.99 | [0.93; 1.06] |
| ≥ 45 – <50 db | 717 | 65738 | 1.00 | [0.92; 1.08] | 1583 | 131960 | 1.01 | [0.95; 1.07] | 1461 | 127897 | 0.99 | [0.93; 1.06] |
| ≥ 50 – <55 db | 348 | 24693 | 1.14 | [1.01; 1.28] | 1222 | 95548 | 1.09 | [1.02; 1.16] | 1176 | 94192 | 1.07 | [1.00; 1.14] |
| ≥ 55 – <60 db | 14 | 1142 | 1.24 | [0.73; 2.13] | 819 | 67195 | 1.09 | [1.01; 1.18] | 452 | 40916 | 0.99 | [0.89; 1.09] |
| ≥ 60 dB | 0 | 0 | – | – | 388 | 33170 | 1.07 | [0.96; 1.19] | 343 | 25237 | 1.23 | [1.10; 1.37] |
| Night hours 11 p.m. to 5 a.m. | ||||||||||||
| <40 db, max. <50 db | 4649 | 382121 | 1.00 | – | ||||||||
| <40 db, max. ≥ 50 db | 3244 | 257513 | 1.04 | [0.99; 1.09] | ||||||||
| ≥ 40 – <45 db | 1538 | 123392 | 1.06 | [1.00; 1.13] | ||||||||
| ≥ 45 – <50 db | 661 | 55504 | 1.02 | [0.94; 1.11] | ||||||||
| ≥ 50 – <55 db | 203 | 15955 | 1.10 | [0.95; 1.27] | ||||||||
| ≥ 55 – <60 db | 7 | 249 | 2.80 | [1.29; 6.07] | ||||||||
| ≥ 60 dB | 0 | 0 | – | – | ||||||||
*Probands were assigned to the fatalities group irrespective of their actual cause of death. Depending on the insurer, deaths that occurred up to at least February 2014 or up to January 2015 at the latest were included.OR: odds ratio, adjusted for age, sex, education, and occupation (from occupation code), SGB-II rate (quintiles); L pAeq.24h : unweighted 24-h continuous noise level; L pAeq.night : average sound level indicator for the night hours 10 p.m. to 6 a.m. and 11 p.m. to 5 a.m.; 95% CI: 95% confidence interval
Restricting the reference category to people without noise exposure ≥ 40 dB
If the reference category consists only of people exposed to traffic noise no higher than 40 dB (eTable 3), this leads to some increase in estimated risk in the individual noise categories. In the analyses where traffic noise is included as a continuous variable with the reference category restricted to people without noise exposure ≥ 40 dB, a slight rise in OR per 10 dB rail traffic noise is seen (from 2.3% without this restriction on the reference category to 3.2%). The increase is smaller in relation to road traffic noise (from 2.8% to 3.3%), while for aircraft noise the continuous model shows no change in OR.
eTable 3. Traffic noise (LpAeq,24h) and incident myocardial infarction; reference category contains only people with continuous noise exposure <40 dB.
| Aircraft noise | Road traffic noise | Rail traffic noise | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Exposure | Cases | Controls | OR | 95% CI | Cases | Controls | OR | 95% CI | Cases | Controls | OR | 95% CI |
| 24-h continuous noise level | ||||||||||||
| <40db traffic noise | 1136 | 47180 | 1.00 | –- | 1136 | 47180 | 1.00 | – | 1136 | 47180 | 1.00 | – |
| <40db. max. ≥ 50db aircraft noise, | 1346 | 52825 | 1.09 | [1.00; 1.18] | ||||||||
| <40db, at least one other source of traffic noise ≥ 40db | 5839 | 249666 | 1.05 | [0.98; 1.12] | 1031 | 40997 | 1.06 | [0.97; 1.15] | 9589 | 399785 | 1.04 | [0.97; 1.10] |
| ≥ 40 – <45 db | 5839 | 249666 | 1.05 | [0.98; 1.12] | 4308 | 177419 | 1.04 | [0.98; 1.12] | 2445 | 104139 | 1.07 | [1.00; 1.15] |
| ≥ 45 – <50 db | 3029 | 134464 | 1.04 | [0.97; 1.12] | 4627 | 200544 | 1.02 | [0.96; 1.09] | 2966 | 132524 | 1.04 | [0.96; 1.11] |
| ≥ 50 –<55 db | 1151 | 52923 | 1.01 | [0.93; 1.10] | 3340 | 148430 | 1.04 | [0.97; 1.11] | 2115 | 91861 | 1.08 | [1.01; 1.17] |
| ≥ 55 – <60 db | 376 | 15845 | 1.10 | [0.98; 1.12] | 2171 | 91493 | 1.08 | [1.00; 1.16] | 823 | 36040 | 1.07 | [0.98; 1.18] |
| ≥ 60–<65 db | 6 | 196 | 1.48 | [0.65; 3.39] | 1637 | 68672 | 1.12 | [1.03; 1.21] | 340 | 13783 | 1.14 | [1.00; 1.29] |
| ≥ 65 – <70 db | – | – | – | – | 1069 | 46715 | 1.09 | [1.00; 1.19] | 138 | 5962 | 1.18 | [0.99; 1.46] |
| ≥ 70 dB | – | – | – | – | 313 | 13284 | 1.16 | [1.02; 1.32] | 80 | 3460 | 1.20 | [0.95; 1.51] |
| Continuous (per 10 dB). People with at least one other source of traffic noise ≥40 dB are excluded | 0.991 | [0.958; 1.026] | 1.033 | [1.015; 1.051] | 1.032 | [1.004; 1.061] | ||||||
| p = 0.615 | p <0.001 | p = 0.027 | ||||||||||
OR: odds ratio, adjusted for age, sex, education, and occupation (from occupation code), SGB-II rate (quintiles); LpAeq.24h: unweighted 24-h continuous noise level; 95% CI: 95% confidence interval
Restricting the analysis to people of known individual social status
If only those people whose individual social status is known are included in the analysis, this subanalysis tends to show a rise in estimated risk for all three modes of traffic noise (eTable 4).
eTable 4. Traffic noise (LpAeq,24h) and incident myocardial infarction, only people of known individual social status (16.1% of MI patients, 36.6% of controls).
| Aircraft noise | Road traffic noise | Rail traffic noise | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Exposure | Cases | Controls | OR | 95% CI | Cases | Controls | OR | 95% CI | Cases | Controls | OR | 95% CI |
| 24-h continuous noise level | ||||||||||||
| <40 db, max. <50 db | 1217 | 117384 | 1.00 | – | 288 | 31585 | 1.00 | – | 1633 | 163631 | 1.00 | – |
| <40 db, max. ≥ 50 db | 213 | 19 400 | 1.08 | [0.93; 1.25] | ||||||||
| ≥ 40 – <45 db | 939 | 92981 | 0.99 | [0.90; 1.08] | 659 | 64074 | 1.12 | [0.97; 1.29] | 418 | 38427 | 1.12 | [1.00; 1.25] |
| ≥ 45 – <50 db | 527 | 49526 | 1.04 | [0.93; 1.17] | 741 | 73146 | 1.12 | [0.98; 1.29] | 522 | 48030 | 1.13 | [1.02; 1.25] |
| ≥ 50 –<55 db | 207 | 19922 | 1.02 | [0.87; 1.19] | 588 | 55025 | 1.18 | [1.02; 1.37] | 359 | 33606 | 1.10 | [0.98; 1.24] |
| ≥ 55 – <60 db | 63 | 5874 | 1.05 | [0.81; 1.37] | 367 | 33433 | 1.21 | [1.03; 1.42] | 149 | 12969 | 1.21 | [1.02; 1.43] |
| ≥ 60–<65 db | 1 | 83 | 1.28 | [0.18; 9.35] | 280 | 25621 | 1.21 | [1.02; 1.43] | 48 | 4944 | 1.01 | [0.75; 1.35] |
| ≥ 65 – <70 db | – | – | – | – | 191 | 17336 | 1.19 | [0.99; 1.44] | 21 | 2244 | 0.99 | [0.64; 1.53] |
| ≥ 70 dB | – | – | – | – | 53 | 4950 | 1.20 | [0.89; 1.62] | 17 | 1319 | 1.40 | [0.86; 2.27] |
| Continuous (per 10 dB) | 1.017 | [0.952–1.087] | 1.050 | [1.009; 1.093] | 1.061 | [1.016; 1.109] | ||||||
| p = 0.618 | p = 0.017 | p = 0.008 | ||||||||||
MI: myocardial infarction; OR: odds ratio, adjusted for age, sex, education, and occupation (from occupation code), SGB-II rate (quintiles); LpAeq.24h: unweighted 24-h continuous noise level; 95% CI: 95% confidence interval
Age-stratified analysis
If persons under 65 years of age and those aged 65 and over are regarded separately, no uniform effect is shown: in the younger people, the estimated risks for road traffic noise are slightly higher, while for the older people the estimated risks for aircraft noise are slightly higher (but without statistical significance) (eTable 5).
eTable 5. Traffic noise (LpAeq,24h) and incident myocardial infarction, stratified by age.
| Aircraft noise | Road traffic noise | Rail traffic noise | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Exposure | Cases | Controls | OR | 95% CI | Cases | Controls | OR | 95% CI | Cases | Controls | OR | 95% CI |
| Only people below age 65 (4597 cases, 486170 controls), 24-h continuous noise level | ||||||||||||
| <40 db, max. <50 db | 1776 | 183842 | 1.00 | – | 424 | 48157 | 1.00 | – | 2372 | 253636 | 1.00 | – |
| <40 db, max. ≥ 50 db | 295 | 30576 | 0.99 | [0.87; 1.12] | ||||||||
| ≥ 40 – <45 db | 1385 | 147684 | 0.95 | [0.88; 1.02] | 918 | 99191 | 1.06 | [0.94; 1.19] | 592 | 62208 | 1.02 | [0.93; 1.11] |
| ≥ 45 – <50 db | 767 | 81706 | 0.94 | [0.86; 1.03] | 1060 | 115.374 | 1.05 | [0.94; 1.18] | 751 | 79242 | 1.02 | [0.94; 1.11] |
| ≥ 50 –<55 db | 281 | 32484 | 0.87 | [0.76; 1.00] | 871 | 89070 | 1.11 | [0.99; 1.25] | 526 | 55305 | 1.02 | [0.93; 1.13] |
| ≥ 55 – <60 db | 92 | 9756 | 0.99 | [0.80; 1.24] | 527 | 54340 | 1.10 | [0.97; 1.26] | 218 | 21503 | 1.09 | [0.95; 1.26] |
| ≥ 60–<65 db | 1 | 122 | 0.84 | [0.12; 6.07] | 412 | 42188 | 1.11 | [0.97; 1.27] | 76 | 8252 | 0.99 | [0.78; 1.24] |
| ≥ 65 – <70 db | – | – | – | – | 289 | 29332 | 1.10 | [0.95; 1.28] | 35 | 3828 | 0.99 | [0.71; 1.39] |
| ≥ 70 dB | – | – | – | – | 96 | 8518 | 1.28 | [1.02; 1.60] | 27 | 2196 | 1.37 | [0.93; 2.02] |
| Continuous (per 10 dB) | 0.961 | 0.910; 1.016] | 1.040 | [1.006; 1.075] | 1.019 | [0.983; 1.057] | ||||||
| p = 0.160 | p = 0.020 | p = 0.301 | ||||||||||
| Only people aged 65 or over (15035 cases,. 348564 controls), 24-h continuous noise level | ||||||||||||
| <40 db, max. <50 db | 6109 | 144973 | 1.00 | – | 1743 | 40020 | 1.00 | – | 8353 | 193329 | 1.00 | – |
| <40 db, max. ≥ 50 db | 1051 | 22249 | 1.06 | [0.99; 1.14] | ||||||||
| ≥ 40 – <45 db | 4454 | 101982 | 1.03 | [0.99; 1.07] | 3390 | 78228 | 1.01 | 0.95; 1.07 | 1853 | 41931 | 1.04 | [0.99; 1.10] |
| ≥ 45 – <50 db | 2262 | 52758 | 1.02 | [0.96; 1.07] | 3567 | 85170 | 0.98 | 0.92; 1.04 | 2215 | 53282 | 0.99 | [0.94; 1.04] |
| ≥ 50 –<55 db | 870 | 20439 | 1.01 | [0.94; 1.09] | 2469 | 59360 | 0.98 | 0.92; 1.04 | 1589 | 36556 | 1.05 | [1.00; 1.11] |
| ≥ 55 – <60 db | 284 | 6089 | 1.09 | [0.96; 1.24] | 1644 | 37153 | 1.03 | 0.96; 1.11 | 605 | 14537 | 1.02 | [0.93; 1.11] |
| ≥ 60–<65 db | 5 | 74 | 1.72 | [0.69; 4.28] | 1225 | 26484 | 1.08 | 1.00; 1.17 | 264 | 5531 | 1.13 | [0.99; 1.28] |
| ≥ 65 – <70 db | – | – | – | – | 780 | 17383 | 1.04 | 0.96; 1.14 | 103 | 2134 | 1.19 | [0.98; 1.46] |
| ≥ 70 dB | – | – | – | – | 217 | 4766 | 1.07 | 0.92; 1.23 | 53 | 1264 | 1.06 | [0.81; 1.40] |
| Continuous (pro 10 dB) | 1.006 | [0.975; 1.038] | 1.021 | 1.002; 1.041 | 1.021 | [1.000; 1.043] | ||||||
| p = 0.712 | p = 0.030 | p = 0.051 | ||||||||||
OR: odds ratio, adjusted for age, sex, education, and occupation (from occupation code), SGB-II rate (quintiles); LpAeq.24h: unweighted 24-h continuous noise level; 95% CI: 95% confidence interval
Simultaneous inclusion of all three modes of traffic noise in the logistic regression model
For each of the three modes of traffic noise, the estimated risks for MI do not change much after adjustment for the other two modes of noise: the linear model continues to show no statistically significant change of risk for aircraft noise, while for road and rail traffic noise statistically significant risk increases of 2.8% and 2.5% per 10 dB are found, respectively.
Discussion
The results of this case–control study based on secondary data, suggest a relationship between exposure to traffic noise and the occurrence of a myocardial infarction. The risk indicators tend to be more pronounced for road and rail traffic noise than for aircraft noise. If the case group is restricted to MI patients who died, the extent of the increase in risk per 10 dB rise in noise level is similar across the three modes of traffic noise.
A limitation of the subanalysis of cases of MI with fatal outcome is that the cause of death could not be identified from the data provided by the insurers. A methodological strength of this case–control study is that it takes account of newly occurring inpatient and outpatient diagnoses of MI with fatal outcome. However, because of the relatively short pre-observation period, it cannot be ruled out that a previous infarction event had occurred at some time in the past, especially for diagnoses in the earlier years. An estimate of the validity of this case–control study is provided in eBox 3.
eBox 3. Assessment of external validity of the case–control study.
The participation of three large health insurers meant that around 23% of the population over the age of 40 living in the study area was included in this case–control study based on secondary data. It may be safely assumed that if any particular traffic noise exposure leads to manifest disease in people insured with one insurer, its effect on those insured with another will be no different. Morever, despite considerable differences in the social structure of the participating insurers, insurer-specific subgroup analysis showed similar estimated risks of myocardial infarction. This supports the external validity of the results.
If only persons whose individual social status is known are included in the analysis (36% of the study population), the estimated risks rise for all three modes of traffic noise. This result suggests that the traffic-noise-related increases in risk cannot be explained by insufficient accounting for social status as a confounding factor. The insurers’ data include no information about lifestyle- and occupation-related risk factors. However, for the case group of patients with heart failure, bias due to unknown or residual confounding was largely ruled out in an additional in-depth survey of about 8500 insured persons (8).
The acoustic input data in this study are of high quality and take account of a variety of different mean and maximum noise level indicators. Even with 24-hour continuous noise levels <40 dB, many people were found who were briefly exposed to night-time aircraft noise events that were much louder than this. These night-time aircraft noise events can also be linked with health effects, particularly those relating to disturbed sleep. The examination of people exposed to maximum night-time noise levels of ≥ 50 dB as a separate exposure group helps to assess this possible etiological pathway.
The findings of our case–control study based on secondary data essentially agree with other published results. However, there are not many other studies investigating different sources of traffic noise within in the same study. In their systematic review of ischemic heart disease, Vienneau and colleagues showed a 6% increase in risk per 10 dB aircraft noise and a 4% increase in risk per 10 dB road traffic noise (start level: 50 dB Lden corresponding to a 24-hour continuous noise level of about 48.5 dB) (3). We calculated risks of slightly below 4% per 10 dB traffic noise (start level: 24-hour continuous noise level of 35 dB) for a fatal MI, and in some cases much lower risks for a newly diagnosed MI. Unlike our study, Vienneau et al. did not find a higher risk of fatal as compared to nonfatal ischemic heart disease (3). However, these authors included the entire group of all patients with ischemic heart disease in their systematic review – whereas MI as investigated in our study is only a subgroup of all ischemic heart disease, although one that carries relatively high mortality.
No direct comparison is possible between our results and those achieved by Greiser and Greiser for the area around the Cologne Bonn Airport: these latter authors included two interaction terms in their evaluation model, both of which included aircraft noise (15, 16). In that sense the main effects of the aircraft noise cannot be directly derived from their study. We did not consider any interaction terms in our models, because additional stratified analyses did not indicate any substantial effect modification due to age.
Summary
Our case–control study allows, for the first time, direct comparison of MI risk estimates for aircraft and road and rail traffic noises on the basis of a very large data set from health insurers. For all three modes of traffic noise investigated, relationships were found with a diagnosis of MI, although the association tends to be more pronounced for road and rail traffic noise than for aircraft noise. It is possible that the continuous noise level is less well suited to represent aircraft-noise-related MI risks than it is to represent health risks related to, in particular, road traffic noise.
It must also be taken into consideration that comparatively few persons in this study were exposed to aircraft noise ≥ 55 dB (1.9% of controls for aircraft noise compared with 26.4% for road traffic noise and 7.1% for rail traffic noise). With aircraft noise, unlike road and rail traffic noise, a continuous noise level above 65 dB did not occur. This means that the marked increase in risk associated with (very) high road and rail traffic noise levels can of course not be seen in relation to aircraft noise, and estimates of the exposure–risk relationship for aircraft noise are altogether more uncertain. The comparably high estimated risks for all three modes of traffic noise in the subgroup of those who died—well above the respective estimated risks in the study population as a whole—suggest that traffic noise may affect not just the onset, but also the course of a MI. In our opinion, this is an area requiring more research.
A large proportion of the population is exposed to levels of traffic noise that our case–control study indicates to be associated with increased—if only slightly increased—risks of MI. For this reason, effective control of traffic noise is a matter of great importance.
Key Messages.
The present analysis of the NORAH case–control study, which was based on secondary data, investigated the risks of myocardial infarction related to traffic noise, using a data set of 1 026 658 over-40-year-olds insured with three health insurers in the Rhine–Main region of Germany.
For the first time, it has been possible to compare directly the estimated risks for road and rail traffic and aircraft noise. For all three modes of traffic noise investigated, relationships with a diagnosis of myocardial infarction were found.
The relationship between myocardial infarction and 24-hour continuous noise level tended to be stronger for road and rail traffic noise than for aircraft noise. The continuous noise level may be of limited use in representing the risks of myocardial infarction related to aircraft noise.
The fact that estimated risks for all three modes of traffic noise in the subgroup of those who died were all similarly high—well above the respective estimated risks in the study population as a whole—suggests that traffic noise may affect not just the onset, but also the course of a myocardial infarction.
Because of the frequency of exposure to traffic noise at the population level as well as the frequency of myocardial infarctions, even small increases in risk are important.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
We are grateful to Dr. Eva Haufe and Prof. Dr. Jochen Schmitt, MPH, for their collaboration in the design of this study. We are especially grateful to Peter Ihle of the PMV Research Group (PMV-Forschungsgruppe) and Ursel Prote of the Leibniz Institute for Prevention Research and Epidemiology (BIPS) and to the participating insurance providers. Warmest thanks also go to Prof. Dr. Wolfgang Hoffmann, MPH, and all other members of the scientific advisory group for their constructive support and commitment.
Decisions of Ethics Committees and Data Protection Officers
The statement by the Ethics Committee of the Faculty of Medicine at the University of Dresden (reference number: EK328102012; 21 February 2013 and 22 April 2014) was taken into account in carrying out this study. The study design was also submitted to the Federal Commissioner for Data Protection and Freedom of Information (reference number: III-320/010#0011; response dated 11 June 2012) and to the Data Protection Officers of the participating federal states of Hessen (reference number: 43.60-we; response dated 13 March 2012; amendment notification 7 February 2014) and Rhineland-Pfalz (reference number: 6.08.22.002; response dated 7 May 2012; amendment notification 4 February 2014). These authorities confirm that this research project complies with data protection regulations.
Financial support
This study was financially supported by the Gemeinnützige Umwelthaus GmbH (Environment & Community Center) in Kelsterbach.
References
- 1.Kraus U, Schneider A, Breitner S, et al. Individual daytime noise exposure during routine activities and heart rate variability in adults: a repeated measures study. Environ Health Perspect. 2013;121:607–612. doi: 10.1289/ehp.1205606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO. www.euro.who.int/__data/assets/pdf_file/0008/136466/e94888.pdf. Bonn: WHO European Centre for Environment and Health; 2010. Burden of disease from environmental noise: quantification of healthy life years lost in Europe. (last accessed on 12 October 2015) [Google Scholar]
- 3.Vienneau D, Schindler C, Perez L, Probst-Hensch N, Röösli M. The relationship between transportation noise exposure and ischemic heart disease: A meta-analysis. Environ Res. 2015;138:372–380. doi: 10.1016/j.envres.2015.02.023. [DOI] [PubMed] [Google Scholar]
- 4.Huss A, Spoerri A, Egger M, Röösli M. Aircraft noise, air pollution, and mortality from myocardial infarction. Epidemiology. 2010;21:829–836. doi: 10.1097/EDE.0b013e3181f4e634. [DOI] [PubMed] [Google Scholar]
- 5.Hansell A, Blangiardo M, Fortunato L, Floud S, et al. Aircraft noise and cardiovascular disease near Heathrow airport in London: small area study. BMJ. 2013;347 doi: 10.1136/bmj.f5432. [DOI] [PubMed] [Google Scholar]
- 6.Correia AW, Peters JL, Levy JI, Melly S, Dominici F. Residential exposure to aircraft noise and hospital admissions for cardiovascular diseases: multi-airport retrospective study. BMJ. 2013;347 doi: 10.1136/bmj.f5561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eriksson C, Nilsson ME, Willers SM, Gidhagen L, Bellander T, Pershagen G. Traffic noise and cardiovascular health in Sweden: the roadside study. Noise and Health. 2012;14:140–147. doi: 10.4103/1463-1741.99864. [DOI] [PubMed] [Google Scholar]
- 8.Seidler A, Wagner M, Schubert M, Dröge P, Hegewald J. Sekundärdatenbasierte Fallkontrollstudie mit vertiefender Befragung. NORAH (Noise-related annoyance, cognition and health). Verkehrslärmwirkungen im Flughafenumfeld. Endbericht, Band 6. 2015. www.laermstudie.de/fileadmin/files/Laermstudie/Krankheitsrisiken_Wiss_Ergebnisbericht.pdf. (last accessed on 5 March 2016) [Google Scholar]
- 9.Möhler U, Liepert M, Mühlbacher M, et al. Erfassung der Verkehrsgeräuschexposition. Dokumentation zur Berechnung der akustischen Daten in NORAH. NORAH (Noise-related annoyance, cognition and health): Verkehrslärmwirkungen im Flughafenumfeld. Endbericht, Band 2. 2015. www.laermstudie.de/fileadmin/files/Laermstudie/Akustik_Wiss_Ergebnisbericht.pdf. (last accessed on 5 March 2016) [Google Scholar]
- 10.Bundesregierung. Erste Verordnung über die Datenerfassung und das Berechnungsverfahren für die Festsetzung von Lärmschutzbereichen vom 27. Dezember 2008 (1. FlugLSV). Anlage 2: Anleitung zur Berechnung von Lärmschutzbereichen (AzB) Bundesanzeiger. 2008;195a [Google Scholar]
- 11.Bundesregierung. Verordnung zur Durchführung des Bundes-Immissionsschutzgesetzes (Verordnung über die Lärmkartierung) vom 6. März 2006 (34. BImSchV (2006). Anlage 2: Vorläufige Berechnungsmethode für den Umgebungslärm an Schienenwegen (VBUSch) vom 22. Mai 2006. Bundesanzeiger 2006a. 154a [Google Scholar]
- 12.Bundesregierung. Verordnung zur Durchführung des Bundes-Immissionsschutzgesetzes (Verordnung über die Lärmkartierung) vom 6. März 2006 (34. BImSchV (2006). Anlage 3: Vorläufige Berechnungsmethode für den Umgebungslärm an Straßen (VBUS) vom 22. Mai 2006. Bundesanzeiger 2006b. 154a [Google Scholar]
- 13.Schubert I, Ihle P, Köster I. Interne Validierung von Diagnosen in GKV-Routinedaten: Konzeption mit Beispielen und Falldefinition. Das Gesundheitswesen. 2010;72:316–322. doi: 10.1055/s-0030-1249688. [DOI] [PubMed] [Google Scholar]
- 14.Blossfeld HP. Frankfurt: Campus; 1985. Bildungsexpansion und Berufschancen. [Google Scholar]
- 15.Greiser E, Greiser C. Risikofaktor nächtlicher Fluglärm: Abschlussbericht über eine Fall-Kontroll-Studie zu kardiovaskulären und psychischen Erkrankungen im Umfeld des Flughafens Köln-Bonn. Umweltbundesamt 2010a. www.umweltbundesamt.de/sites/default/files/medien/461/publikationen/3774.pdf. (last accessed on 12 October 2015) [Google Scholar]
- 16.Greiser E, Greiser C. Risikofaktor nächtlicher Fluglärm: Abschlussbericht über eine Fall-Kontroll-Studie zu kardiovaskulären und psychischen Erkrankungen im Umfeld des Flughafens Köln-Bonn. Anlagenband: Umweltbundesamt 2010b. www.umweltbundesamt.de/sites/default/files/medien/461/publikationen/3775.pdf. (last accessed on 12 October 2015) [Google Scholar]