Abstract
Background: Previous studies have shown race/ethnicity, particularly African American and/or Hispanic status, to be a predictor of overweight/obese status in children. However, these studies have failed to adjust for low socioeconomic status (SES). This study assessed whether race/ethnicity remained an independent predictor of childhood obesity when accounting for variations in SES (low-income) among communities in Massachusetts.
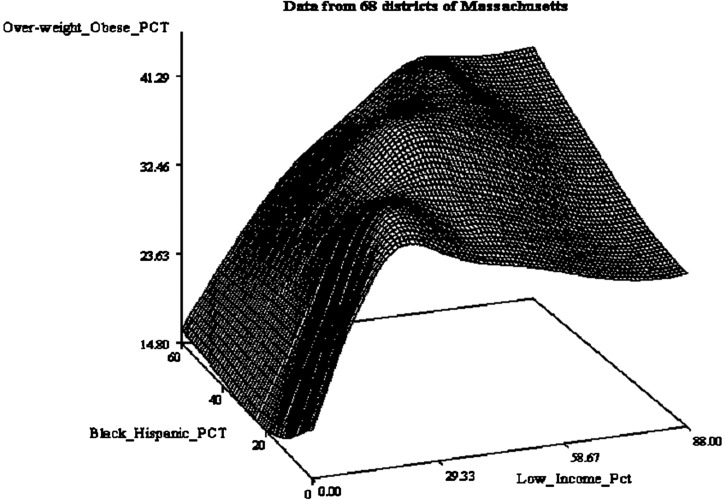
Methods: This study was based on 2009 summarized data from 68 Massachusetts school districts with 111,799 students in grades 1, 4, 7, and 10. We studied the relationship between the rate of overweight/obese students (mean = 0.32; range = 0.10–0.46), the rate of African American and Hispanic students (mean = 0.17; range = 0.00–0.90), and the rate of low-income students (mean = 0.27; range = 0.02–0.87) in two and three dimensions. The main effect of the race/ethnicity rate, the low-income rate, and their interaction on the overweight and obese rate was investigated by multiple regression modeling.
Results: Low-income was highly associated with overweight/obese status (p < 0.0001), whereas the effect of race/ethnicity (p = 0.27) and its interaction (p = 0.23) with low-income were not statistically significant. For every 1% increase in low-income, there was a 1.17% increase in overweight/obese status. This pattern was observed across all African American and Hispanic rates in the communities studied.
Conclusions: Overweight/obese status was highly prevalent among Massachusetts students, varying from 10% to 46% across communities. Although there were higher rates of overweight/obese status among African American and Hispanic students, the relationship disappeared when controlling for family income. Our findings suggest low SES plays a more significant role in the nation's childhood obesity epidemic than race/ethnicity.
Introduction
Obesity rates in both adults and children in the United States have steadily risen over the past few decades.1–6 In 2009–2010, the prevalence of obesity (BMI ≥95th percentile) was 18.4% in 12- to 19-year-olds. Increasingly, data suggest that obesity in childhood is associated with a high likelihood of obesity in adulthood.6,7 If an individual is overweight in adolescence, there is a 70%chance that they will remain overweight or obese as an adult.8 This association between childhood and adult obesity brings with it an accumulated multitude of medical conditions, including hypertension, diabetes, sleep apnea, hyperlipidemia, and a higher incidence of stroke, myocardial infarction, some types of cancer, kidney disease, and death.2,7,9–13
Perhaps even more concerning, whereas obesity prevalence increased by 10% for all US children, obesity increased by 23–33% for children in low-education, low-income, and higher-unemployment households in 2003–2007.14 Moreover, low-income families are less likely to realize that their child is overweight or believe that they should interfere with the child's eating and activity behaviors.15 Low-income communities face a host of barriers to improving health statuses.16,17
Efforts to understand the underpinnings of childhood obesity have been increasingly successful in identifying associated factors that appear to substantially correlate with childhood obesity.12 A number of reports have shown that race/ethnicity is highly correlated with rates of childhood obesity.1–3,9 In 2009–2010, 23.7% of African Americans ages 12–19 were obese, compared to only 16.1% of whites in the respective age group.3 African American and Hispanic children also have been shown to have higher rates of obesity-related risk factors, such as hyperlipidemia, lower high-density lipoprotein, and higher fasting glucose.1,2,18 In addition, studies have suggested that African Americans, on average, eat more fast food and have poorer dietary habits in childhood/adolescence than Caucasians.1 This is likely owing to the nature of food availability in predominantly lower-income African American neighborhoods.17 Similar observations have been made concerning physical activity behaviors.19
This study showed that lower household income was strongly correlated with a higher incidence of childhood obesity in Massachusetts.20 However, it is unclear whether race/ethnicity or income status are risk factors for obesity when the other variable is controlled. This report explores this interaction between community income, race/ethnicity, and the community incidence of childhood obesity among 68 Massachusetts school districts and 111,799 students in grades 1, 4, 7, and 10 collected in the 2009 calendar year.
Methods
The Massachusetts Department of Public Health began mandated screening of BMI among students enrolled in public schools in 2011. However, in 2010, school nurses submitted 2009 data from 80 school districts for all students enrolled in grades 1, 4, 7, and 10. Measured height and weight were used to calculate BMI for all 80 school districts. Data were submitted to the Massachusetts Department of Public Health's state-wide database. To correlate community rates of childhood obesity with lower-income status, the percentage of students who were overweight or obese was compared with the percentage of students in each district who were eligible for free/reduced-price lunch, received transitional aid, or were eligible for food stamps. These data were also obtained from the Department of Public Health, which monitors and records the use of such programs within each community. Overweight/obese status was calculated based on sex-specific CDC growth charts. A student was considered overweight if he or she had a BMI greater than or equal to the 85th percentile, but less than the 95th percentile. A student was considered obese if he or she had a BMI greater than or equal to the 95th percentile. Race/ethnicity frequency reporting was available in 68 of 80 school districts at the community level, and the study compared the percentage of African American and Hispanic students to all others in each community. Each community was defined by the school district. The percentage of all students categorized as overweight/obese was calculated for the entire state population.
Statistical Analysis
Initial two- and three-dimensional graphical exploration was conducted to examine the relationship between the rate of overweight/obese students, the rate of low-income students, and the rate of African American/Hispanic students. A multiple regression analysis was used to examine the effect of low-income and African American/Hispanic proportion, as well as their interaction, on overweight/obese rates. Owing to the observed exponential relationship between low-income percentages and overweight/obese percentages in the two-dimensional plot, log transformation of low-income percentage was used in the regression model. The regression modeling and analysis were conducted in JMP (version 10.0) statistical software and the Statistical Analysis System (version 9.3; SAS Institute Inc., Cary, NC). A Fourier plot was created to illustrate these relationships where each school district is represented as a single point on a three-dimensional grid.
Results
BMI data were available for 111,799 students (100% of students in the reporting districts) from grades 1, 4, 7, and 10 in 68 of the 80 school districts in Massachusetts. Race/ethnicity and low-income status were obtained on a community level for these same 68 districts. The percentage of overweight/obese among Massachusetts children across 68 school districts ranged from a low of 9.6% to a high of 42.8%. The percentage of low-income status among Massachusetts school districts varied from 2.4% to as high as 69.5%. Mean prevalence by district of overweight or obese was 32% (95% confidence interval [CI], 10–46). Mean prevalence of African American/Hispanic status was 17% (95% CI, 0–90). Mean prevalence of low-income status was 27% (95% CI, 2–87). These are shown in Table 1. As shown by multiple regression modeling, districts' low-income status was strongly associated with overweight/obese status (p < 0.0001) (see Table 2). For every 1 percentage point increase in low-income designation (i.e., the proportion of children who have low-income status), there was a corresponding 1.17 percentage point increase in overweight/obese prevalence across the 68 districts when controlling for race/ethnicity. Race/ethnicity (African American/Hispanic status) was not significantly correlated, when controlling for income, with the mean prevalence of overweight/obese in the school districts. The relationship between these three variables is illustrated in the Fourier transformation three-dimensional plot in Figure 1.
Table 1.
Obesity, Race, and SES Prevalence across 68 School Districts
| Mean prevalence (%) | Range (%) | |
|---|---|---|
| Overweight/obese | 32 | 10–46 |
| African American or Hispanic | 17 | 0–90 |
| Low income | 27 | 2–87 |
SES, socioeconomic status.
Table 2.
Regression Result
| Estimated parameter | Standard error | t | p value | |
|---|---|---|---|---|
| Intercept, β0 | 13.7 | 2.2 | 6.2 | <0.0001 |
| Log low-income percentage | 6.3 | 0.87 | 7.3 | <0.0001 |
| African American/Hispanic percentage | 0.013 | 0.038 | 0.36 | 0.7 |
Regression model: Overweight-obese PCT = β0 + β1*Log (low-income PCT) + β2*African American-Hispanic PCT + Error. The R-square is 0.63.
Figure 1.
Percent of overweight and obese versus percent of low-income versus percent of African American and Hispanic. PCT/Pct, percent.
Discussion
The battle to curb childhood obesity is critically tied to studies that can enunciate its underpinnings and national, state, community, neighborhood, and household efforts to change modifiable risks that enable positive health change for each and every child.2,16,19,20 This study showed the independent relationship of community income status and rates of overweight/obese status in 68 school districts representing a majority of the school districts in Massachusetts. Importantly, it was illustrated that race/ethnicity in communities may not be a significant correlate with overweight/obese status once the community's income is considered. Whereas this study was representative of Massachusetts only, future studies may expose similar trends in other populations. This is important because it helps focus more critically on actionable targets for change, which include a host of factors unique to each household, neighborhood, community, and region.
Previous studies have illustrated the magnitude of effect that household income appears to have on the rates of childhood obesity.21–24 Similarly, a large number of reports have suggested that Mexican American and non-Hispanic black children are especially vulnerable with prevalence of obesity in excess of 20%.3 Increasingly, investigators have shown that these differences are largely attributable to inequities in the physical and social environment in which children are raised.25–27 For example, this study reported that childhood obesity rates in two neighboring communities varied by nearly a factor of two, and that the lower-income community (with higher ethnic/racial diversity) could be characterized comparatively for its remarkable lack of full-service grocery stores, exercise facilities, and recreational programs and parks. As expected, children in the lower-income community reported substantially less physical activity, poorer nutritional food consumption, more consumption of fried food and sugary beverages, and much more time watching television or playing video games.28 Similarly, Galvaz and colleagues reported that block by block neighborhood physical activity resources had a substantial impact on actual hours of weekly physical activity among children living in Harlem.29 Other studies have also reported that lower-income communities have reduced access to supermarkets and places to exercise, but that these same communities have numerous convenience stores and fast food chains, which, taken together, promote poor nutrition and little or no physical activity.30–35
How much of the apparent correlation between childhood obesity and racial/ethnic disparity can then be explained by household sociodemographic and economic characteristics, including low socioeconomics, food availability, and physical activity resources? In this study, the apparent correlation between race/ethnicity and childhood obesity was nullified when considering community socioeconomic status (SES). Powell and colleagues showed that up to three quarters of the apparent relationship between race/ethnicity and childhood obesity is removed when one considers these alternative explanations.36 Rossen also recently reported that after adjusting for individual-level SES and neighborhood deprivation (and their interaction), 74% of the apparent differences in childhood obesity between non-Hispanic black and non-Hispanic white children disappeared.37 That study represented a national survey of 18,369 children using the National Health and Nutrition Examination Survey (NHANES) database and offers confirmatory evidence that childhood obesity has far more to do with resources than it does the color of a child's skin or his or her ethnic origin.37
The roadmap for attacking childhood obesity starts with understanding these relationships between resources and childhood health. Solutions will only be effective if they create sustainable improvement in the child's knowledge about health, create ready access to higher nutritional value foods and beverages, offer enjoyable and safe avenues and time for physical activity, discourage unhealthy choice when it comes to food/beverage intake, and discourage unhealthy excess sedentary activities.38,39 Ultimately, bottom-up neighborhood, school, and community engagement and education, and top-down legislative actions that will encourage healthier choices for adults and their children, is needed to battle this nation-wide health crisis.40,41
A previous study showed that local interventions using a middle-school–based health curriculum (Project Healthy Schools) can result in substantial improvements in self-reported health behaviors and physiological measures, such as serum total cholesterol, low-density lipoprotein, and triglyceride levels, within 4 months of the program's initiation.42 This program, now introduced in 55 Michigan middle schools, is but one example of how a bottom-up, grassroots effort can begin to change the tide of this overwhelming national health issue. The benefits of Project Healthy Schools appear to be especially favorable in lower-income communities.20
This study has both limitations and strengths. The major limitation is that whereas the information on BMI was gathered from 111,799 unique children, the information on race/ethnicity and SES represented state-reported community estimates for each of the 68 school districts that were studied. Though one can only assume that household income and race/ethnicity strongly correlate with community means, the data are not household-to-household comparisons, but rather a community comparison. This bias would likely weaken—not strengthen—correlations, but it must be acknowledged. The strength of this study comes from the fact that it represents 111,799 students representing a majority (85.0%) of all school districts in Massachusetts. Given that these findings mirror findings from other states as well as national samples, there is confidence in their veracity.
Conclusions
In conclusion, lower household resources appear to have a much greater impact on childhood obesity rates in this cohort of Massachusetts students than race and ethnicity. Future research in additional states is warranted to build the wealth of knowledge on this topic and assist in the development of effective interventions to reduce childhood obesity in communities with varying income levels.
Acknowledgments
Project Healthy Schools' wellness efforts have been generously supported throughout the past 10 years by a number of health systems, foundations, and individuals, including the University of Michigan Health System, the Thompson Foundation, the Hewlett Foundation, the Mardigian Foundation, the Memorial Healthcare Foundation, the William Beaumont Health System Foundation, the Ann Arbor Area Community Foundation, the Allen Foundation, AstraZeneca Healthcare Foundation, the D. Dan and Betty Kahn Foundation, DeRoy Testamentary Foundation, Blue Cross Blue Shield of Michigan, Mr. and Mrs. Richard Sarns, Ms. Eleanor Gimon, Mrs. Peter Corriveau, Mrs. Byron Gerson, Mr. and Mrs. Edward Blanch, Dr. Thomas Varbedian, Mr. and Mrs. William Whelan, Mr. and Mrs. Jack Edman, Dr. and Mrs. William Heisel, Mr. Brian Campbell, Mr. Fahi Nona, Mr. Ralph Boehnke, and several anonymous donors.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Hurt RT, Kulisek C, Buchanan LA, et al. The obesity epidemic: Challenges, health initiatives, and implications for gastroenterologists. Gastroenterol Hepatol 2010;6:780–792 [PMC free article] [PubMed] [Google Scholar]
- 2.Caprio S, Daniels SR, Drewnowski A, et al. Influence of race, ethnicity, and culture on childhood obesity: Implications for prevention and treatment. Obesity 2008;16:2566–2577 [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA 2012;307:483–490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA 2010;303:242–249 [DOI] [PubMed] [Google Scholar]
- 5.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA 2008;299:2401–2405 [DOI] [PubMed] [Google Scholar]
- 6.Whitaker RC, Wright JA, Pepe MS, et al. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med 1997;337:869–873 [DOI] [PubMed] [Google Scholar]
- 7.Dietz WH. Childhood weight affects adult morbidity and mortality. J Nutr 1998;128(2 Suppl):411S–414S [DOI] [PubMed] [Google Scholar]
- 8.Freedman DS, Khan LK, Serdula MK, et al. The relation of childhood BMI to adult adiposity: The Bogalusa Heart Study. Pediatrics 2005;115:22–27 [DOI] [PubMed] [Google Scholar]
- 9.Freedman DS, Mei Z, Srinivasan SR, et al. (2007) Cardiovascular risk factors and excess adiposity among overweight children and adolescents: The Bogalusa Heart Study. J Pediatr 2007;150:12–17 [DOI] [PubMed] [Google Scholar]
- 10.Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA 2006;295:1549–1555 [DOI] [PubMed] [Google Scholar]
- 11.Jolliffe D. Extent of overweight among US children and adolescents from 1971 to 2000. Int J Obes Relat Metab Disord 2003;28:4–9 [DOI] [PubMed] [Google Scholar]
- 12.Dietz WH. Overweight in childhood and adolescence. N Engl J Med 2004;350:855–857 [DOI] [PubMed] [Google Scholar]
- 13.Tirosh A, Shai I, Afek A, et al. Adolescent BMI trajectory and risk of diabetes versus coronary disease. N Engl J Med 2011;364:1315–1325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Singh GK, Siahpush M, Kogan MD. Rising social inequalities in US childhood obesity, 2003–2007. Ann Epidemiol 2010;20:40–52 [DOI] [PubMed] [Google Scholar]
- 15.Hansen AR, Duncan DT, Tarasenko YN, et al. Generational shift in parental perceptions of overweight among school-aged children. Pediatrics 2014;134:481–488 [DOI] [PubMed] [Google Scholar]
- 16.DeVoe JE, Baez A, Angier H, et al. Insurance + access ≠ health care: Typology of barriers to health care access for low-income families. Ann Fam Med 2007;5:511–518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Powell LM, Slater S, Mirtcheva D, et al. Food store availability and neighborhood characteristics in the United States. Prev Med 2007;44:189–195 [DOI] [PubMed] [Google Scholar]
- 18.Batey LS, Goff DC, Jr., Tortolero SR, et al. Summary measures of the insulin resistance syndrome are adverse among Mexican-American versus non-Hispanic white children: The Corpus Christi Child Heart Study. Circulation 1997;96:4319–4325 [DOI] [PubMed] [Google Scholar]
- 19.Gordon-Larsen P, McMurray RG, Popkin BM. Determinants of adolescent physical activity and inactivity patterns. Pediatrics. 2000;105:e83. [DOI] [PubMed] [Google Scholar]
- 20.Eagle TF, Sheetz A, Gurm R, et al. Understanding childhood obesity in America: linkages between household income, community resources, and children's behaviors. Am Heart J 2012;163:836–843 [DOI] [PubMed] [Google Scholar]
- 21.Ogden CL, Lamb MM, Carroll MD, et al. Obesity and socioeconomic status in children and adolescents: United States, 2005–2008. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics: Hyattsville, MD, 2010 [Google Scholar]
- 22.Wang Y, Monteiro C, Popkin BM. Trends of obesity and underweight in older children and adolescents in the United States, Brazil, China, and Russia. Am J Clin Nutr 2002;75:971–977 [DOI] [PubMed] [Google Scholar]
- 23.Wang Z, Patterson CM, Hills AP. Association between overweight or obesity and household income and parental body mass index in Australian youth: Analysis of the Australian National Nutrition Survey, 1995. Asia Pac J Clin Nutr 2002;11:200–205 [DOI] [PubMed] [Google Scholar]
- 24.Gable S, Lutz S. Household, parent, and child contributions to childhood obesity. Fam Relat 2000;49:293–300 [Google Scholar]
- 25.Yancey AK, Kumanyika SK. Bridging the gap: Understanding the structure of social inequities in childhood obesity. Am J Prev Med 2007;33(4 Suppl):S172–S174 [DOI] [PubMed] [Google Scholar]
- 26.White K, Borrell LN. Racial/ethnic residential segregation: Framing the context of health risk and health disparities. Health Place 2011;17:438–448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Finch BK, Phuong Do D, Heron M, et al. Neighborhood effects on health: Concentrated advantage and disadvantage. Health Place 2010;16:1058–1060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jackson EA, Eagle T, Leidal A, et al. Childhood obesity: A comparison of health habits of middle-school students from two communities. Clin Epidemiol 2009;1:133–139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Galvez MP, McGovern K, Knuff C, et al. Associations between neighborhood resources and physical activity in inner-city minority children. Acad Pediatr 2013;13:20–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gordon-Larsen P, Nelson MC, Page P, et al. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics 2006;117:417–424 [DOI] [PubMed] [Google Scholar]
- 31.Larson NI, Story MT, Nelson MC. Neighborhood environments: Disparities in access to healthy foods in the US. Am J Prev Med 2009;36:74–81 [DOI] [PubMed] [Google Scholar]
- 32.Lovasi GS, Hutson MA, Guerra M, et al. Built environments and obesity in disadvantaged populations. Epidemiol Rev 2009;31:7–20 [DOI] [PubMed] [Google Scholar]
- 33.Papas MA, Alberg AJ, Ewing R, et al. The built environment and obesity. Epidemiol Rev 2007;29:129–143 [DOI] [PubMed] [Google Scholar]
- 34.Sallis JF, Glanz K. The role of built environments in physical activity, eating, and obesity in childhood. Future Child 2006;16:89–108 [DOI] [PubMed] [Google Scholar]
- 35.Slater SJ, Ewing R, Powell LM, et al. The association between community physical activity settings and youth physical activity, obesity, and body mass index. J Adolesc Health 2010;47:496–503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Powell LM, Slater SJ, Chaloupka FJ. The relationship between community physical activity settings and race, ethnicity and socioeconomic status. Evidence Based Prev Med 2004;1:135–144 [Google Scholar]
- 37.Rossen LM. Neighbourhood economic deprivation explains racial/ethnic disparities in overweight and obesity among children and adolescents in the USA. J Epidemiol Commun Health 2014;68:123–129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sarrafzadegan N, Rabiei K, Wong F, et al. The sustainability of interventions of a community-based trial on children and adolescents' healthy lifestyle. ARYA Atheroscler 2014;10:107–117 [PMC free article] [PubMed] [Google Scholar]
- 39.Cotts T, Goldberg C, Davis LP, et al. A school-based health education program can improve cholesterol values for middle school students. Pediatr Cardiol 2008;29:940–945 [DOI] [PubMed] [Google Scholar]
- 40.Borys JM, Le Bodo Y, Jebb SA, et al. EPODE approach for childhood obesity prevention: Methods, progress and international development. Obes Rev 2012;13:299–315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Oen G, Stormark KM. (2013) Participatory action research in the implementing process of evidence-based intervention to prevent childhood obesity: project design of the “Healthy Future” study. J Obes 2013;2013:437206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cotts TB, Durussel-Weston JE, Goldberg CS, et al. Project healthy schools: A school based health education program to prevent childhood obesity. AGRO Food Industry Hi Tech 2007;18:32–34 [Google Scholar]