Abstract
Metastases to proximal femur are common and surgery is often suggested to prevent fractures; otherwise it is necessary in cases where this has already occurred. Adjuvant radiotherapy is necessary to reduce the risk of local progression. Nevertheless, the success or failure of radiation therapy treatments depends upon the accuracy in which target identification is correct and dose prescription is fulfilled. Unfortunately, the use of titanium nails consistently limits radiation dose; indeed, the presence of ferromagnetic artifacts interferes with target identification.
We present the technique for implant a new carbon fiber nail useful to reduce the ferromagnetic artifacts which allows a better adjuvant radiotherapy.
Keywords: Artifacts, Osteolysis, Pathologic fracture, Proximal femur metastases, Radiotherapy, Tumor
1. Introduction
Proximal femur is one of the most common sites of metastasis secondary to the spine and pelvis.1
Within the proximal femur about half of the lesions are located in the neck, 20% in the pertrochanteric region and 30% in the subtrochanteric region.2 These types of lesions often compromise quality of life due to consistent and severe pain endured which can subsequently evolve into pathological fractures.
Even though the main approach used toward patients with metastatic disease is systemic therapy, surgery is often suggested to prevent fractures, particularly in cases where this has already occurred.3
When the proximal femur is the only site of metastasis, wide resection and prosthesis replacement are the most reasonable choices, regardless whether the primitive histotype is favorable.4
Intramedullary nailing treatment is indicated in patients with multiple metastases, in the following conditions: when prognosis is considered unfavorable, when it is important to avoid constraining the patient to the bed, permitting weight bearing and preventing local and general complications.
This surgery is intralesional and has just a biomechanical aim; it does not decrease the tumor mass, otherwise the associated bleeding and growth factors release could increase its progression. Thus adjuvant radiotherapy is vital in reducing the risk of local progression making previous surgery useless and in reducing the risk of nail breakage otherwise happening with consistent probability.5
Unfortunately, the use of titanium nails in the canal and femoral neck leads artifacts during radiation imaging and therapy. The presence of a high-Z material in an irradiated patient results in reducing radiation through the inhomogeneity as well as local perturbations known as interface effects. Thus, imaging results are affected by ferromagnetic artifacts and dose calculation is rendered inaccurate.6 The success or failure of radiation therapy treatments depends upon the accuracy in which target identification is correct and dose prescription is fulfilled. The presence of cold spot of the prescription dose could result in under-treating the disease with major risk of progression. In addition, there will obviously be significant benefits also in defining the state of the disease detectable in CT imaging follow-up of treated patients.
Carbon fiber nails are characterized by a low artifacts level so that radiotherapists can administer a more effective dose with less risks for the patient.7, 8 Unfortunately, until now, its use was limited by the absence of the nailing system with cephalic screw. To the best of our knowledge, this is the first nail which allows neck screws. The technique here presented emphasizes the use of radiopaque markers.
2. Methods
The technique is similar to traditional nailing; nevertheless, some differences have to be taken into account. Because of its radiolucency, it would not have been possible to see the nail during the insertion if radiopaque markers had not been present in its structure. Under X-ray intensifier control, it is possible to identify the nail proximal end, the lag screw–nail interface marker, the longitudinal marker and the distal hole marker.
The patient is placed in the supine position onto a fracture table, the affected limb is stretched out with dedicated support; traction is necessary in case a pathological fracture is present or there is an increased of it occurring during surgery. The contralateral hip is flexed and abducted.
After setting the operative field, an 8 cm incision is performed in the lateral hip, about 5 cm proximally to the apex of the great trochanter. After splitting fascia lata longitudinally, a sharp cannulated intruder is used to open the medullary canal (Fig. 1a); its stylet is then removed and a K-wire is inserted (Fig. 1b).
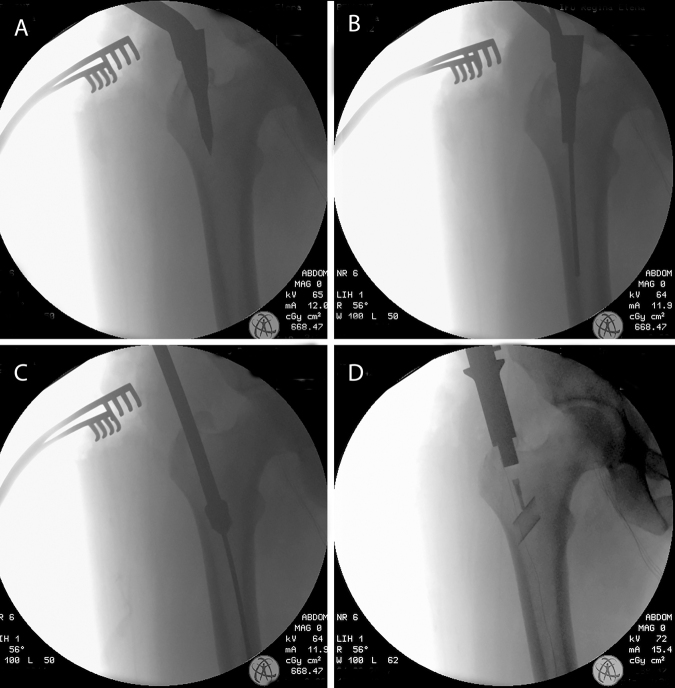
Fig. 1.
Intraoperative X-ray intensifier imaging showing the medullary canal opening (A), the K-wire inserted as guide inside after stylet removal (B), the canal reaming (C) and the nail being inserted inside the canal until the lag-screw marker is in right position (D).
In this specific case, a 48-year-old lady was affected by a metastasis from lung cancer with a partial involvement of the greater trochanter and the neck of the right femur.
The canal is then reamed until a diameter of 13 mm for a length of a little more than 200 mm and 19 mm in the proximal part, typically 2 mm more than the diameter of the nail (length 200 mm, proximal diameter 17 mm, medium-distal diameter 11 mm) (Fig. 1c). The nail is inserted, using the dedicated handle, into the canal until the lag-screw marker is in the right position aiming the inferior aspect of the femoral neck (Fig. 1d). A K-wire is drilled through the lateral cortex until the femoral head and left inside (Fig. 2a) to act as guide to the successive reaming (Fig. 2b) and lag-screw insertion (Fig. 2c); the K-wire is then removed and the tip screw tightened to lock the cephalic one.
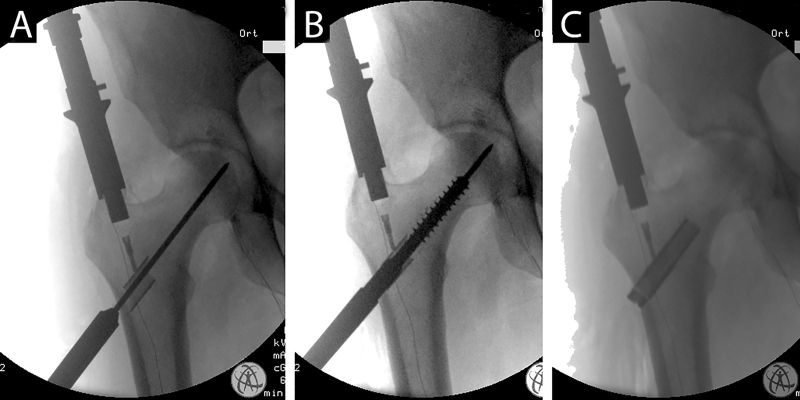
Fig. 2.
Intraoperative X-ray intensifier imaging showing the K-wire insertion along the femoral neck (A), the successive reaming (b) and the nail positioned at the right level with the cephalic lag-screw inserted and visible just in the proximal part (C).
A 1 cm skin incision is successively performed in the lateral thigh, corresponding to the distal guide hole of the nail handle. A K-wire is drilled through the first and the second cortexes and used to measure and hypothesize the screw length. After removing the K-wire, a partially threaded distal screw is inserted verifying in AP a lateral view, the correct positioning through the distal hole of the nail based on its distal markers (Fig. 3a and b). The nail handle is removed and the access is stitched up after abundant irrigation (Fig. 3c). The AP post-operative X-ray evidenced a good positioning of the nail (Fig. 4).
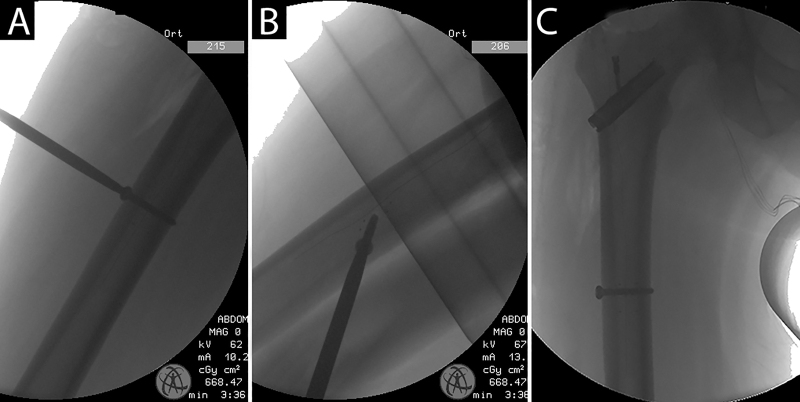
Fig. 3.
Intraoperative X-ray intensifier imaging showing the AP and LL check to verify the correct insertion of the distal screw; the nail handle is then removed (C).
Fig. 4.

AP postoperative X-ray showing the correct placement of the nail.
The patient underwent adjuvant radiotherapy after 1 month when the wounds were healed; a partial weight bearing with crutches was allowed after 1 week and a total weight bearing allowed after 4 months from RT. The patient died for disease progression after 13 months from surgery.
3. Results
The technique allows an easy stabilization of impending femoral fracture and already occurred fractures. The lower level of artifacts allows a safer RT.
4. Discussion
Intramedullary nailing is a well consolidated and effective technique in treating long bone metastasis because its efficacy allows a precocious weight bearing, technically easier for the surgeon and less invasive for the patient that it is able to continue systemic therapy for sometime.
Traditional nails are made out of titanium alloy which assures an easy insertion technique because of its radiopacity but at the same time this material renders successive therapeutic protocol more problematic as the carbon electron density blinds CT which is used to enhance the radiation field during adjuvant therapy but also during the follow-up to detect disease progression. Also MRI imaging is deeply influenced by the presence of titanium and steel instruments.9
Due to its intrinsic characteristic, carbon fiber stabilizations are ideal in treating oncological patients. Indeed, they assure more effective adjuvant therapy with a lower risk of local recurrence but they also allow to detect local recurrences or progression more easily at CT and MRI performed during the follow-up.
Moreover, carbon fiber implants have a modulus elasticity similar to that of the cortical bone one more than titanium and stainless steel implants as well as higher fatigue and bending strength.
Taking into account this important characteristic and considering that a more efficient RRT should assure a faster bone resistance recovery, carbon fiber nails should assure even al longer reliability than traditional titanium nail; nevertheless prospective randomized studies are advocated to verify a theoretic insight. By the way, the implant survival looks already sufficient for metastatic patients considering their low survival.
Carbon fiber nails were already available but their use was quite limited in treating humerus and diaphysial femoral osteolysis.10 Indeed, the availability of nails to insert the cephalic screws facilitates extending indications to proximal femur lesion where metastases are more frequent.
Prospective randomized studies are advocate to verify the hardware survival and the effectiveness of RT, when applied in patient treated with carbon nail, in reducing tumor local progression rate and in facilitating bone consolidation.
The operative technique for radiolucent nails is similar to the technique used for traditional instrumentation; nevertheless more attention has to be paid during the distal screw insertion. Markers are important when confirming the correct distal locking.
Long nails are nonetheless advocated for permitting more appropriate treatment for metastatic patients.
Conflicts of interest
The authors have none to declare.
Acknowledgements
We thank Christina M. Walter and Marta Merlino for the precious English revision. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Hage W.D., Aboulafia A.J., Aboulafia D.M. Incidence, location, and diagnostic evaluation of metastatic bone disease. Orthop Clin N Am. 2000;31(4):515–528. doi: 10.1016/s0030-5898(05)70171-1. [DOI] [PubMed] [Google Scholar]
- 2.Sim F.H. Metastatic bone disease of the pelvis and femur. Instr Course Lect. 1992;41:317–327. [PubMed] [Google Scholar]
- 3.Jacofsky D.J., Haidukewych G.J. Management of pathologic fractures of the proximal femur: state of the art. J Orthop Trauma. 2004;18(7):459–469. doi: 10.1097/00005131-200408000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Camnasio F., Scotti C., Peretti G.M., Fontana F., Fraschini G. Prosthetic joint replacement for long bone metastases: analysis of 154 cases. Arch Orthop Trauma Surg. 2008;128(8):787–793. doi: 10.1007/s00402-007-0464-y. [DOI] [PubMed] [Google Scholar]
- 5.Townsend P.W., Smalley S.R., Cozad S.C., Rosenthal H.G., Hassanein R.E. Role of postoperative radiation therapy after stabilization of fractures caused by metastatic disease. Int J Radiat Oncol Biol Phys. 1995;31(1):43–49. doi: 10.1016/0360-3016(94)E0310-G. [DOI] [PubMed] [Google Scholar]
- 6.Stoll P., Wächter R., Hodapp N., Schilli W. Radiation and osteosynthesis. Dosimetry on an irradiation phantom. J Craniomaxillofac Surg. 1990;18(8):361–366. doi: 10.1016/s1010-5182(05)80057-5. [DOI] [PubMed] [Google Scholar]
- 7.Xin-ye N., Xiao-bin T., Chang-ran G., Da C. The prospect of carbon fiber implants in radiotherapy. J Appl Clin Med Phys. 2012;13(4):38218. doi: 10.1120/jacmp.v13i4.3821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zimel M.N., Hwang S., Riedel E.R., Healey J.H. Carbon fiber intramedullary nails reduce artifact in postoperative advanced imaging. Skelet Radiol. 2015;44(9):1317–1325. doi: 10.1007/s00256-015-2158-9. [DOI] [PubMed] [Google Scholar]
- 9.Buckwalter K.A., Lin C., Ford J.M. Managing postoperative artifacts on computed tomography and magnetic resonance imaging. Semin Musculoskelet Radiol. 2011;15(4):309–319. doi: 10.1055/s-0031-1286013. [DOI] [PubMed] [Google Scholar]
- 10.Collis P.N., Clegg T.E., Seligson D. The invisible nail: a technique report of treatment of a pathological humerus fracture with a radiolucent intramedullary nail. Injury. 2011;42(4):424–426. doi: 10.1016/j.injury.2010.10.012. [DOI] [PubMed] [Google Scholar]