Abstract
Background
While screening for colorectal cancer (CRC) is a widely accepted concept nationally and screening rates are increasing, there are differences in screening rates between states and within states.
Methods
In an effort to increase screening rates and ensure equal access based on race/ethnicity, the New York City Department of Health and Mental Hygiene formed a coalition of stakeholders in 2003, with the primary focus on colonoscopy, to develop and implement strategies across the city to achieve this goal.
Results
From a screening colonoscopy rate of only 42% in 2003, these concerted efforts contributed to achieving a screening rate of 62% by 2007, and almost 70% in 2014, with the elimination of racial and ethnic disparities.
Conclusions
We provide details of how this program was successfully conceived, implemented and sustained in the large urban population of NYC. We hope that by sharing the many elements involved and the lessons that we learned, other communities may adapt our experiences to their own environments so that CRC screening rates can be maximized.
Keywords: colorectal cancer, colorectal cancer screening, screening colonoscopy, colorectal cancer prevention
Precis
A strong partnership between the NYC Department of Health and Mental Hygiene and an actively engaged community and academic coalition successfully raised colorectal screening colonoscopy rates from 42% to 69% and eliminated ethnic disparities.
Introduction
Screening for colorectal cancer (CRC) is today a widely accepted intervention, because of its demonstrated effectiveness for reducing incidence and mortality. National rates for CRC screening test use increased from 54% in 2002 to 65% in 20121, and efforts are in place by over 250 public, private, and non-profit organizations to increase CRC screening to 80% by 20182.
Colonoscopy as a screening modality was first introduced into clinical guidelines in 19973, 4, and became a covered benefit for Medicare beneficiaries at average risk in 2001. Shortly thereafter (2003), Dr. Thomas Frieden, then Commissioner of the New York City Department of Health and Mental Hygiene (NYC DOHMH), made CRC screening colonoscopy a top priority for NYC. His reasoning was: over 1,500 men and women were dying of CRC each year in NYC; scientific studies had demonstrated that CRC deaths can be prevented by screening; approximately 60% of at-risk New Yorkers were not being screened; and, his belief that NYC had the medical and financial resources to implement a colonoscopy screening program to dramatically reduce CRC mortality.5 Dr. Frieden’s concept was supported by Dr. Benjamin Chu, then head of the NYC Health and Hospitals Corporation (HHC) which is charged with providing care regardless of ability to pay. An Advisory Committee was formed; the main charge was to assess the potential contribution of colonoscopy to NYC’s CRC prevention efforts. From this, the Citywide Colon Cancer Control Coalition (“C5 Coalition”) was launched as a program to increase CRC screening for all New Yorkers age 50 and older, with strong endorsements coming from the top health care leadership in the city.
This paper provides details of how C5 was conceived and how it successfully implemented screening colonoscopy over time. As a result, screening colonoscopy rates in NYC increased from 42% in 2003 (well below the national average of 52%) to 62% in 20076 a rate that was not reached nationally until 20121. As of 2012, the NYC screening colonoscopy rate increased 64% from baseline, translating into an additional 833,000 individuals screened7. Moreover, during this period, screening colonoscopy rates among Hispanics, for example, increased from 38% to 70%, considerably higher than the national rate that reached only 48% by 20121. It is hoped that by understanding the many elements involved, other communities, especially in large urban settings may adapt some of the lessons learned to their own environments to increase CRC screening rates with the ultimate goal of reducing the incidence and mortality of CRC.
Creation of a DOHMH Advisory Committee
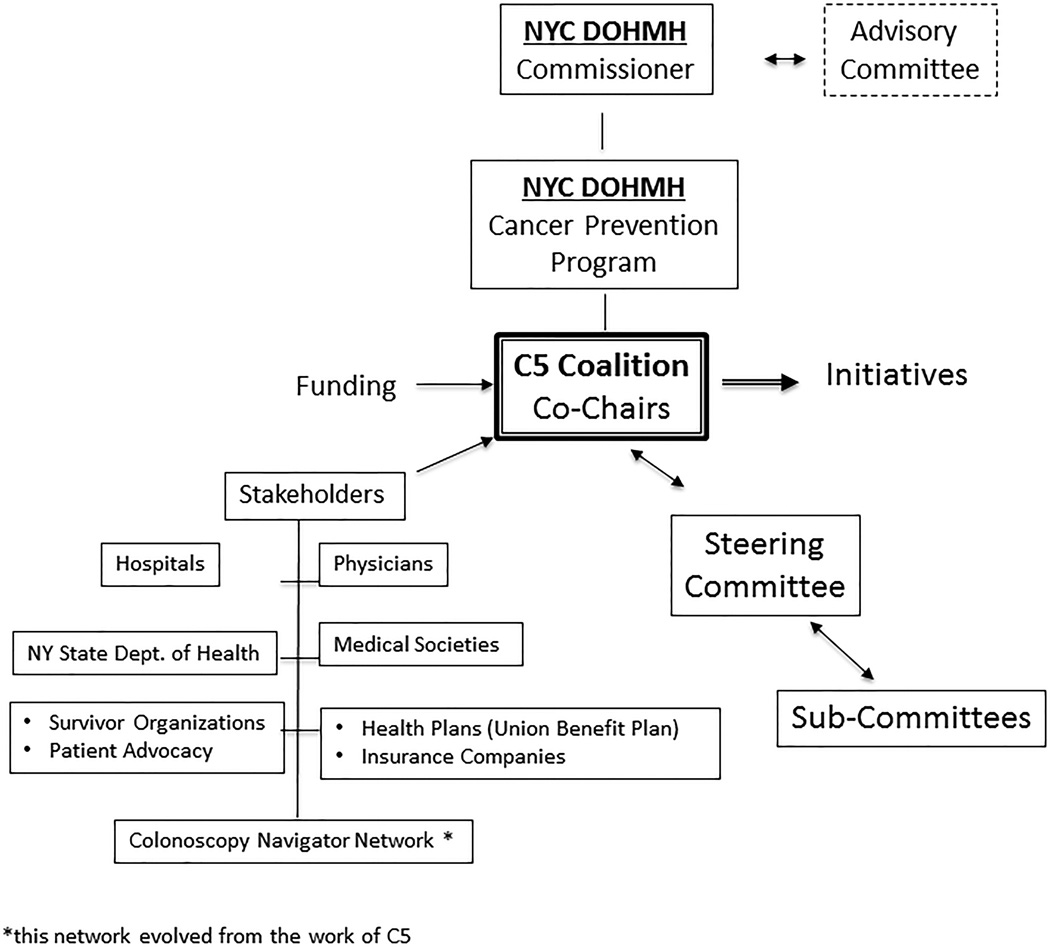
An Advisory Committee, co-chaired by Drs. Harold Freeman and Sidney Winawer, was formed in 2002 to consider whether or not colonoscopy should be regarded as the preferred screening approach in NYC (Figure 1). The Advisory Committee reviewed available evidence related to screening reported in several guidelines3, 8–11, additional relevant papers3, 8, 11–13 and met with DOHMH cancer prevention professionals. Screening guidelines and their rationale were specifically tailored to the NYC health care environment, which included considerations of capacity, reimbursement and expected compliance by providers and the public. The following guidelines were adopted:
Men and women age 50 years of age and older should undergo colonoscopy every 10 years.
Annual fecal occult blood testing is recommended for individuals who are unable or unwilling to have a colonoscopy.
People at high risk for colorectal cancer should begin screening with colonoscopy at age 40 or earlier.
Figure 1.
C5 Structure.
Colonoscopy was recommended as the preferred test because: it examines the entire colon; it is relatively safe; polyps can be detected and removed to prevent cancer; and biopsies can be taken of suspicious lesions. Fecal occult blood testing (FOBT) was recommended as an alternative but considered less optimal because it is less sensitive and its impact on CRC morbidity and mortality requires annual testing over many years. It is thus programmatically more difficult to implement and monitor, compared with a single colonoscopy every 10 years3, 4. A simple message encouraging one screening test was also considered to be more effective than a menu of options as recommended in most guidelines. DOHMH conducted a capacity study which confirmed that NYC’s healthcare system had sufficient resources to screen its ‘at risk’ population by colonoscopy5.
Launching of the C5 Coalition
In March 2003, a presentation was made by the Advisory Committee to a roundtable of healthcare providers, DOHMH staff, and stakeholders. The group agreed that there should be a coalition (C5) consisting of a broad representation of stakeholders in the community. The following mission statement was formulated:
“The mission of the C5 Coalition is to partner with the NYC DOHMH to increase awareness and screening for colorectal cancer and adenomatous polyps in NYC men and women in order to reduce the incidence and mortality of this highly prevalent and preventable disease.”
From the onset, DOHMH and the Advisory Committee sought to establish clear goals:
Increase colonoscopy screening rates for all New Yorkers age 50 or older and define targeted screening goals
Eliminate racial and ethnic screening disparities
A number of sub-committees were formed. Table 1 lists the current and past sub-committees of C5. With its mission and goals delineated, several central questions were raised as DOHMH began to expand the membership of the Advisory Committee into a broader coalition of stakeholders (Table 2). Who were the key individuals and groups that would be critical to demonstrate the City’s commitment to the new screening policy? What resources (access to networks, to intellectual capital, and to financial support) could be mobilized to expand the reach and capacity of DOHMH? Which institutions and individuals would be critical for implementing initiatives, and who could provide a range of feedback evaluating the program and focus?
Table 1.
C5 Committees
| Committee | Responsibilities |
|---|---|
| CURRENT | |
| Steering Committee |
|
| Screening Guidelines |
|
| Summit Planning |
|
| Communications |
|
| Colonoscopy Quality/Benchmarking |
|
| Community Health Centers |
|
| PAST | |
| Direct Endoscopy Referral System (DERS) |
|
| “Plateau” Committee |
|
| Health Care Access |
|
| Ambassador Program |
|
Table 2.
C5 Stakeholders
| Type of Participant | C5 Partners |
|---|---|
| Physicians |
|
| Hospitals and other Health Care Organizations |
|
| Insurers with extensive NYC membership |
|
| Professional Organizations |
|
| Health Departments |
|
| Advocacy Groups |
|
| Survivor Organizations |
|
| Patient Navigators |
|
Initiatives to Achieve Goals
Central to C5 efforts was an ongoing effort to engage all sectors in the awareness of the importance of CRC prevention and early detection through screening continually based on existing data. For example, in 2002, DOHMH launched the Community Health Survey (CHS), an annual, digitally-assisted, telephone survey of 10,000 randomly selected adults 18 and older to understand the health status of New Yorkers. Data from these annual surveys provided crucial information to track critical outcomes such as a detailed demographic profile of who reported having a colonoscopy, and assessed progress against goals and targets including eliminating gender and racial disparities.
Annual C5 Summit
The C5 Steering Committee, charged with overseeing all operations of C5, sought to engage as many stakeholders as possible in the development of C5 goals. An annual Summit was implemented to think critically as a unified community about C5 program initiatives. The Summit (http://c5nyc.org/) became an important venue for presenting updates of C5 activities and obtaining critical feedback. Since the first Summit (November 2003), participation has grown to well over 200 attendees in 2014, many from around the country.
Public Education
Public education campaigns supported through DOHMH funding with some support from New York State (NYS) were targeted both at the general public and at specific underserved communities with low screening rates. These included recruiting celebrity spokespeople for radio and poster campaigns in the subway, on bus shelters, and throughout HHC hospitals; palm card distribution in check cashing offices; and extensive radio campaigns on selected ethnic radio stations. These campaigns were initially in English and Spanish. In addition, several NYC Health Bulletins encouraging colonoscopy screening were made available in other languages (i.e., Russian, Mandarin, and Cantonese) and widely distributed by DOHMH.
Professional Education
Ongoing publications and outreach to health care providers about the need for colorectal cancer screening with the single message of colonoscopy screening every 10 years were implemented by DOHMH. Multiple postings in the City Health Information newsletter (e.g., June 2002, volume 27 (supplement 1); April 2009, volume 28 (supplement 2)) were sent to over 10,000 providers.
DOHMH “Detailing Initiative”
A public health detailing program was initiated to promote the use of preventive services among primary care providers in NYC areas with a high incidence of CRC morbidity and mortality. Modeled after successful “detailing” strategies used by the pharmaceutical industry, trained DOHMH representatives delivered evidence-based messages and materials and provided brief, targeted messages to primary care offices and distributed “action kits” for providers and patients. Specific to CRC screening, representatives conducted approximately 640 site visits and 3940 one-on-one contacts during 2004, 2005 and 2008 to encourage adherence to NYC’s screening guidelines, and to promote colonoscopy screening referrals. Sites were located primarily in neighborhoods with either poor screening uptake, high poverty and/or large immigrant populations. The initial results from 2004 showed a significant increase from 26% to 42% in the proportion of providers who reported colonoscopy as their primary screening method14. When the campaign was repeated in 2008, that proportion increased from 82% to 93%. Moreover, the proportion of offices with systems in place to promote colon cancer screening increased significantly from 52% to 62%15.
Patient Navigator Programs
Patient navigation, first described by Dr. Harold Freeman, involves the use of trained staff within the health care setting to help patients obtain necessary medical care16. While originally used within minority populations to ensure timely resolution of abnormal screening test findings, participating institutions in C5 adapted patient navigation to screen for CRC. The DOHMH secured significant foundation support from the New York Community Trust to develop a proof of concept that navigation could be successfully used to help patients complete a colonoscopy and also reduce the no-show rate. The navigator program has now been implemented in all 11 public hospitals and in 12 voluntary hospitals throughout NYC. In addition, an extensive training program was developed, and is on-line for public access, including a one-week orientation and on-going seminars for navigators17. Further, the DOHMH developed an extensive database that permitted navigators to track their referred patients so that outcomes could be reported, and gaps in service addressed.
The business case for the CRC screening patient navigation program has been demonstrated18–20. For example, in a stakeholder hospital, C5 participants demonstrated that lay individuals (those over age 50 who have had their own colonoscopy) can be readily trained to serve effectively as peer patient navigators21. Modeling studies have demonstrated that navigating primarily African-American and Latino populations of low socioeconomic status from this same hospital is cost-effective22. This demonstration led to the development of additional training materials (including a focus on cultural issues) and a manual. The navigator program has been a consistent focus of C5, and on-going evaluation and updates on the use and value of navigation has encouraged robust support of the program.
Direct Referral Initiative
Direct endoscopic referral (DERS) was developed to help streamline the colonoscopy referral process, including the elimination of the need for medically eligible patients to have a consultation prior to colonoscopy. DERS forms23 were developed by DOHMH in consultation with C5 members to encourage their use by primary care health professionals. Many hospitals in NYC have moved to a DERS system with some using the online form (www.nyc.gov/html/doh/downloads/pdf/cancer/cancer-colon-ders.pdf).
NYC Colonoscopy Quality Initiative
As NYC’s screening rates continued to increase, it became apparent to DOHMH that it was necessary also to focus on ensuring the quality of the colonoscopies and that high quality exams be delivered in all screening settings in NYC. A working committee was formed to delineate the specifics of a Quality Initiative for NYC. This committee included stakeholders critical to such a program: several insurers, New York Society for Gastrointestinal Endoscopy (NYSGE), hospital based, ambulatory care, and office based gastroenterologists (GI), DOHMH and NYS DOH.
In response to national data showing the impact of colonoscopy quality metrics on the rate of interval cancers, the national GI professional associations undertook important quality tracking initiatives24. The American College of Gastroenterology and American Society of Gastrointestinal Endoscopy joined together in 2009 and launched the GI Quality Improvement Consortium, Ltd (GIQuIC). This national GI endoscopy data repository allows for storage of endoscopy quality measures for GI endoscopists and is provided through downloads from their respective endowriters. After the C5 Quality sub-committee proposed a partnership with GIQuIC24, NYC sites were added to that database, and DOHMH developed tailored benchmarking reports for its participating gastroenterologists.
In 2011, the NYC Colonoscopy Quality Benchmarking Group (CQBG) was created with support from the CDC and the NYS DOH and led by the DOHMH in partnership with C5 and NYSGE. The campaign recruited hospitals, private practices and ambulatory surgery centers. Practice sites participated voluntarily. Over a 3-year period, more than 230 gastroenterologists were recruited. DOHMH provides sites with de-identified quarterly benchmarking reports tracking evidence-based quality measures, which allows for comparison of endoscopist performance within and between sites.
Targeted programs to address inequalities
Since the inception of NYC’s CRC screening campaign a decade ago, the elimination of inequalities has been a core goal. Strategies were data driven, with annual analysis of the DOHMH Community Health Survey to identify and monitor screening inequalities for a range of subgroups. As certain inequalities were eliminated, others persisted or emerged, and strategies evolved to respond. We highlight here a few initiatives that illustrate how these strategies developed and evolved.
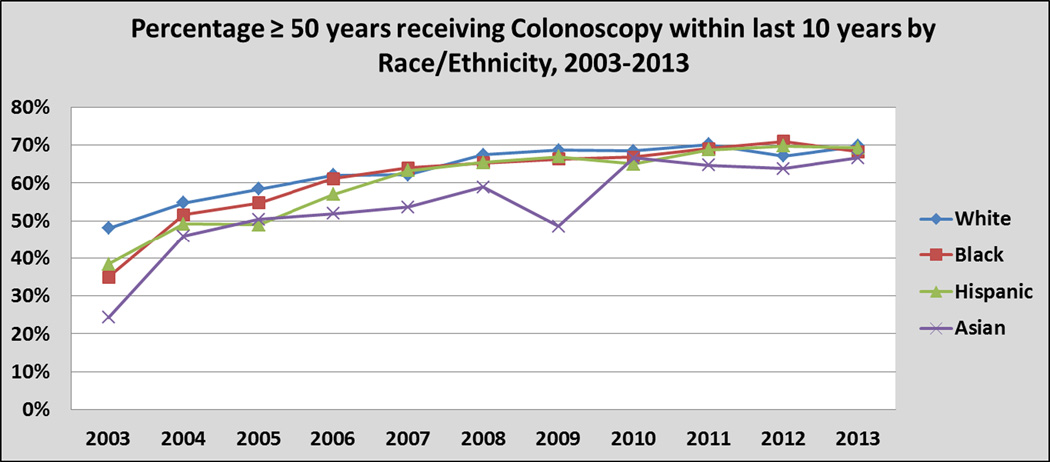
Although in 2003 significant gaps existed between the screening rates for black, white, Asian and Hispanic New Yorkers who had timely screening by colonoscopy7, by 2007, the screening gaps between blacks, whites and Hispanics were eliminated, with the gap for Asian New Yorkers closing in 2010 (Figure 2)7. An extensive outreach campaign at NYC’s public hospital system, HHC, which serves 1.3 million patients annually, the majority of whom are black, Hispanic and Asian, contributed significantly to the elimination of racial and ethnic disparities. Today all these groups are screened on par7.
Figure 2.
Percentage of NYC individuals ≥ 50 years old who received colonoscopy within the last 10 years by race/ethnicity; 2003-2013. Source: New York City Community Health Survey
Targeting the Russian and Chinese Speaking Communities
As racial and ethnic disparities were eliminated, others inequalities were identified. Utilizing the NYC Community Health Survey 2010 data, DOHMH analyzed screening trends geographically, mapping neighborhoods and their screening rates. The analysis revealed significant screening disparities based upon ‘language spoken at home.’ Specifically, in 2009, the screening rates for the Russian and Chinese speaking community were significantly lower than those for English or Spanish speaking New Yorkers25. Overlaying the geographic and demographic data, neighborhoods were identified that had both low CRC screening rates and a high concentration of Russian and Chinese speakers. Culturally and linguistically tailored interventions were then designed and implemented in those neighborhoods, including an aggressive media campaign with posters and text tested by focus groups, ethnic radio and newspaper campaigns, and provider education.
Leveraging Endoscopy Centers to Provide Free Colonoscopy Screening
A recently launched DOHMH project, the ‘Community Cares Project’, grew out of a recommendation from the newly formed C5 Community Health Center Sub-committee (CHC). The ‘Community Cares Project’ focuses on NYC’s uninsured, a subgroup screened at a rate significantly lower than those who are insured26. In this project, free-standing endoscopy centers provide free colonoscopy screenings to uninsured patients referred by CHCs. The project leveraged a NYS ‘charity care’ requirement27 for certain endoscopy centers, and harnessed the desire and dedication of providers to give back to their community. On the CHC side of the equation, the project aligned with an enhanced focus on CRC screening, as CRC screening rates became a reportable metric for Federally Qualified Health Centers in 2012.28 In its pilot year, two participating endoscopy centers performed over 500 screening colonoscopies on uninsured patients referred from five CHCs29. Thus far in year two, an additional 10 sites have joined, including seven new endoscopy centers. Additionally, quality improvement strategies are being developed and tested in the CHCs.
Funding for C5 Initiatives
Most of C5’s work was made possible by a willingness among the many constituents of the NYC health care community to be active participants and to work synergistically. NYC DOHMH, NY State and the CDC all provided significant public support, as well as additional private support numerous foundations. Physicians and hospital systems redoubled their efforts to increase screening colonoscopy by whatever means and resources worked in their local environment. Several insurance companies developed outreach initiatives to their members along with registries to identify unscreened patients for their physicians. Community based organizations focused their resources on CRC prevention. Several centers redesigned their endoscopy units to create greater efficiency and implement direct referral systems. Individual hospitals assumed leadership roles. For example, the Mount Sinai Medical Center launched innovative and carefully studied patient navigation programs funded by the National Cancer Institute20, 21, 30 and Columbia Presbyterian Hospital developed an efficient DERS program23. An important amount of the resources needed to support these efforts was generated by the organizations themselves, and not through an infusion of public funding.
The American Cancer Society (ACS) developed and managed an important citywide initiative to provide screening colonoscopy to uninsured and underinsured New Yorkers. Launched in 2004, the ACS Colonoscopy Screening Program for the Uninsured was funded by the NYC Council and has provided over 20,000 free screening colonoscopies to uninsured New Yorkers to date. ACS Advocacy staff conducted intensive annual campaigns to secure uninterrupted funding from the NYC Council for this key program. Further, in 2004, ACS also led the effort to obtain voluntary agreement from most NYS Commercial Health Plans to reimburse for CRC screening with colonoscopy.
“Lessons Learned” From the C5 Experience
The implementation and evolution of C5 may offer some generalizable principles and approaches that could help guide the development of similar coalitions in other communities. Like the proposed Cascade model in which screening guidelines are driven by available resources as well as medical evidence31, communities seeking to develop a C5-like organization must build it using their unique resources. The following lessons are distilled from the NYC experience:
Identify High Level Champions and Encourage Distributed Leadership: NYC’s effort was spearheaded by the Commissioner of the NYC DOHMH with very strong support from the President of HHC. The initial Advisory Panel included leading international experts on CRC screening. This core group of very high level, public and private sector experts was joined by leadership from multiple sectors which sustained the growth of C5 and NYC’s screening initiatives.
Engage a convening entity: DOHMH was the convening entity and continues to provide significant, sustained resources to anchor C5.
Define and revise goals: Goals were defined at the inception of the initiative and were continually revised based upon emerging data and trends. NYC’s dual goal of both increasing screening city-wide and eliminating screening inequalities informed and drove all strategies. A laser-like, sustained focus on screening inequalities has been essential.
Be data-driven: Various data sources were used to track progress and gaps in care that informed new strategies. These included NYC’s Community Health Survey, Uniform Data System (UDS), NYS Quality Assurance Reporting Requirements (QARR), GIQuIC, NYS Cancer Registry, and the DOHMH Colonoscopy Navigator Database.
-
Identify trends and create synergies: Emerging healthcare system trends were identified to create synergies that promoted NYC’s goals.
NYC’s initial focus on colonoscopy screening was a policy decision that was based on the inclusion of colonoscopy as a screening option in national guidelines and the decision of payers to provide reimbursement.
Patient navigation has now been demonstrated to be integral to the success of screening colonoscopy programs.
Colonoscopy quality – after identifying that there was a need for quality improvement, NYC leveraged the work of the national GI associations, including its partnership with GIQuIC.
NYS public health law provision requiring free-standing endoscopy centers (ambulatory surgical centers) to perform services for the medically underserved was utilized to screen the uninsured.
Leadership continuously identified strategies to take advantage of incentives embedded in the evolving models for payment system reform, such as Patient Centered Medical Homes, Accountable Care Organizations, Pay for Performance.
Healthcare Effectiveness Data and Information Set (HEDIS) and QARR quality measures included colonoscopy screening.
Establish an Organizational Structure: The organizational structure (with sub-committees and working groups) was program-driven and flexible, and supported evolving goals. In addition, the structure was a vehicle to engage stakeholders’ participation, report progress and receive alerts to new challenges, and sustain commitment.
Engage Multi-Sector Stakeholders: Multi-sector stakeholders (Table 2) who were invested in achieving the goals, such as provider systems, health plans, and advocacy and community based organizations, were recruited to C5.
-
NYC-specific assets: The success of C5 clearly has depended in part on infrastructure features that are specific to NYC.
NYC’s safety net healthcare system - Without this far reaching high quality healthcare system serving NYC’s underserved communities, the elimination of racial and ethnic disparities would not have been possible
NYC Council funding of colonoscopies for underinsured adults, along with significant ACS operational support.
NYS’s Emergency Medicaid Program – if a CRC is detected by screening, this program provides coverage for CRC treatment, regardless of insurance or whether an individual is undocumented. Given NYC’s extensive and essential undocumented population, this benefit has been vital.
The high concentration of gastroenterologists that provide significant capacity for colonoscopy screening helped make this possible.
Strong health department provides sustained, significant support.
Extensive voluntary hospital systems, with strong academic commitment and which value physician engagement and research
-
Challenges:
Efforts to sustain active engagement and support from the primary care provider community have met with uneven success. The enduring competing priorities facing primary care providers present challenges to achieving high rates of cancer screening, including CRC screening.
There remains a lack of adequate resources to screen the uninsured. Despite innovative, significant local programs, and NYS’s Cancer Services Program, the screening gap for the uninsured remains significant. While the Affordable Care Act has helped lower the number of NYC’s uninsured, this legislation does not provide coverage to the undocumented community.
Data are needed regarding the outcome of those who are found to have CRC or advanced adenomas with respect to the continuum of care.
While a business case has been developed for endoscopy-based patient navigation18, 20 no corresponding sustainable model has yet been developed for primary care.
Efforts to include navigators as a sustainable resource have failed, requiring independent funding of these programs.
There is a continual need for securing current and new resources in a climate of dwindling resources.
Increases in CRC screening rates have leveled off. Underlying factors need to be studied in order to reassess strategies.
The preference for colonoscopy provides a strong, clear, unified message. However, for systems such as Community Health Centers that may implement fecal occult-blood based programs, C5 has so far provided less support.
Conclusions
The dramatic increase in NYC screening colonoscopy rates among average-risk men and women from 42% (2003) to 62% (2012) and now at 69% (2013) were advanced by this series of sequential steps. Foremost was that CRC screening was made a top priority by both the NYC Commissioner of Health and the President of NYC HHC. Second, a mission statement and clear goals were established. Third, a citywide coalition was organized, a broad range of stakeholders were engaged, and a structure was established. Fourth, many programs were developed and adapted to increase screening in all NYC communities and to eliminate inequalities. Fifth, program strategies and goals evolved as new needs were defined. Finally, metrics were put in place to monitor progress and provide positive feedback to all stakeholders.
Our goal in describing the history of the program is to provide a description of the multiple elements of NYC’s Colonoscopy Screening Initiative, its evolution, and the important role of the DOHMH/C5 partnership. We have learned that this needs to be a dynamic process that is flexible as new concepts of CRC prevention evolve (e.g., chemopreventive agents, new technology such as new screening tests with high sensitivity for CRC and advanced adenomas, new genetic evidence) and the health care landscape changes which will have further impact on resources and sustainability. The impact that increased screening might have on the incidence and mortality of CRC in NYC, especially as it relates to current disparities, will be the subject of a future report. We anticipate that these developments will have an impact nationally and will influence future directions of the DOHMH/C5 program locally in NYC. Hopefully, this will result in significant reduction in the incidence and mortality of CRC.
Acknowledgments
Funding Source: This publication was supported in part by the Cooperative Agreement Grant No. CDC Grant 1U38DP004969-01 from the Centers for Disease Control and Prevention. Its contents are solely the responsibility of the authors and do not necessarily reflect the official views of the Centers for Disease Control and Prevention.
Any financial disclosures: Dr. Itzkowitz receives consulting fees and research support from Exact Sciences Corporation. Dr. Winawer receives consulting fees from Exact Sciences Corporation and Applied Proteomics, Inc. Dr. Schnoll-Susman receives consulting fees from Covidian and CdX Diagnositics.
Contributor Information
Steven H. Itzkowitz, Professor of Medicine and Oncological Sciences, Icahn School of Medicine at Mount Sinai, One Gustave Levy Place, Box 1069, New York, NY 10029, (T) 212-241-0333, (F) 646-537-8647, Steven.Itzkowitz@mountsinai.org.
Sidney Winawer, Paul Sherlock Chair in Medicine, Gastroenterology and Nutrition Service, Department of Medicine, Memorial Sloan-Kettering Cancer Center, Professor of Medicine, Weill Cornell Medical College, Cornell University, 1275 York Avenue, New York, NY 10065, (T) 212-639-7678, (F) 212-639-2766, winawers@MSKCC.ORG.
Marian Krauskopf, Former Director, Cancer Prevention and Control Program, New York City Department of Health and Mental Hygiene, 12 W. 96th Street, New York, NY 10025, (T) 212-864-1598, (F) 212-864-1598, Mskrauskopf@gmail.com.
Mari Carlesimo, Senior Director, Cancer Prevention Program, New York City Department of Health and Mental Hygiene, Director, C5 Coalition, 42-09 28th Street, 12th floor, Long Island City, NY 11101, (T) 347-396-4375, (F) 347-396-4920, mcarlesimo@health.nyc.com.
Felice Schnoll-Sussman, Associate Professor Clinical Medicine, Weill Cornell Medical Center, 1315 York Avenue, New York, NY 10012, (T) 212-746-4014, (F) 212-746-5845, fhs2001@med.cornell.edu.
Katy Huang, Citywide Colon Cancer Control Coalition Program Manager, New York City Department of Health and Mental Hygiene, Cancer Prevention and Control Program, 42-09 28th Street, 11th Floor, Unit 12-50, Long Island City, NY 11101, (T) 347-396-4291, (F) 347-396-4920, khuang@health.nyc.gov.
Thomas Weber, Professor of Surgery, State University of New York Health Sciences Center, Brooklyn, New York, Chief of Surgery, VA Brooklyn Medical Center, Suite 112, 800 Poly Place, Brooklyn, NY 11209, (T) 718-630-3706.
Lina Jandorf, Professor of Oncological Sciences, Icahn School of Medicine at Mount Sinai, One Gustave Levy Place, Box 1130, New York, NY 10029, (T) 212-659-5506, (F) 212-849-2566.
References
- 1.Centers for Disease Control and Prevention. Vital signs: colorectal cancer screening test use-United States, 2012. Morbidity and Mortality Weekly Report. 2013;62:881. [PMC free article] [PubMed] [Google Scholar]
- 2.National Colorectal Cancer Roundtable. [accessed Apr 17, 2015];80% by 2018 fact sheet. Available from URL: http://nccrt.org/wp-content/uploads/80-by-2018-FACT-SHEET.FINAL_.pdf.
- 3.Winawer SJ, Fletcher RH, Miller L. Colorectal cancer screening: Clinical guidelines and rationale. Gastroenterology. 1997;112:594–642. doi: 10.1053/gast.1997.v112.agast970594. [DOI] [PubMed] [Google Scholar]
- 4.Byers T, Levin B, Rothenberger D, Dodd GD, Smith RA. American Cancer Society guidelines for screening and surveillance for early detection of colorectal polyps and cancer: update 1997. CA-Cancer J. Clin. 1997;47:154–160. doi: 10.3322/canjclin.47.3.154. [DOI] [PubMed] [Google Scholar]
- 5.Leng JC, Thorpe LE, Feldman GE, Thomas PA, Frieden TR. The volume and capacity of colonoscopy procedures performed at New York City hospitals in 2002. Prev Chronic Dis. 2005;2:A09. [PMC free article] [PubMed] [Google Scholar]
- 6.Richards CA, Kerker BD, Thorpe L, et al. Increased screening colonoscopy rates and reduced racial disparities in the New York Citywide campaign: an urban model. Am J Gastroenterol. 2011;106:1880–1886. doi: 10.1038/ajg.2011.191. [DOI] [PubMed] [Google Scholar]
- 7.New York City Department of Health and Mental Hygiene. Community Health Survey 2003–2012. http://www.nyc.gov/html/doh/html/data/chs-data.shtml. Updated 2014.
- 8.Smith RA, von Eschenbach AC, Wender R, et al. American cancer society guidelines for the early detection of cancer: Update of early detection guidelines for prostate, colorectal, and endometrial cancers: Also: Update 2001—testing for early lung cancer detection. CA Cancer J Clin. 2001;51:38–75. doi: 10.3322/canjclin.51.1.38. [DOI] [PubMed] [Google Scholar]
- 9.Lieberman D, Rex D, Winawer S, Giardiello F, Johnson D, Levin T. United States Multi-Society Task Force on Colorectal Cancer. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2012;143:844–857. doi: 10.1053/j.gastro.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 10.Levin B, Lieberman DA, McFarland B, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: A joint guideline from the American cancer society, the US multi-society task force on colorectal cancer, and the American college of radiology. CA Cancer J Clin. 2008;58:130–160. doi: 10.3322/CA.2007.0018. [DOI] [PubMed] [Google Scholar]
- 11.U.S. Preventive Services Task Force. Screening for colorectal cancer: Recommendation and rationale. Ann Intern Med. 2002;137:129–131. doi: 10.7326/0003-4819-137-2-200207160-00014. [DOI] [PubMed] [Google Scholar]
- 12.Sonnenberg A, Delco F, Inadomi JM. Cost-effectiveness of colonoscopy in screening for colorectal cancer. Ann Intern Med. 2000;133:573–584. doi: 10.7326/0003-4819-133-8-200010170-00007. [DOI] [PubMed] [Google Scholar]
- 13.Winawer SJ, Zauber AG, Ho MN, et al. Prevention of colorectal cancer by colonoscopic polypectomy. N Engl J Med. 1993;329(27):1977–1981. doi: 10.1056/NEJM199312303292701. [DOI] [PubMed] [Google Scholar]
- 14.Larson K, Levy J, Rome MG, Matte TD, Silver LD, Frieden TR. Public health detailing: a strategy to improve the delivery of clinical preventive services in New York City. Public Health Rep. 2006;121(3):228–234. doi: 10.1177/003335490612100302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dresser MG, Short L, Wedemeyer L, et al. Public health detailing of primary care providers: New York City's experience, 2003–2010. Am J Prev Med. 2012;42:S122–S134. doi: 10.1016/j.amepre.2012.03.014. [DOI] [PubMed] [Google Scholar]
- 16.Freeman HP, Muth B, Kerner J. Expanding access to cancer screening and clinical follow-up among the medically underserved. Cancer Pract. 1995;3(1):19. [PubMed] [Google Scholar]
- 17.New York City Department of Health and Mental Hygiene. [accessed Apr 17, 2015];Colonoscopy patient navigator program orientation manual. Available from URL: http://www.nyc.gov/html/doh/downloads/pdf/cancer/orientation.pdf.
- 18.Elkin EB, Shapiro E, Snow JG, Zauber AG, Krauskopf MS. The economic impact of a patient navigator program to increase screening colonoscopy. Cancer. 2012;118:5982–5988. doi: 10.1002/cncr.27595. [DOI] [PubMed] [Google Scholar]
- 19.Chen LA, Santos S, Jandorf L, et al. A program to enhance completion of screening colonoscopy among urban minorities. Clinical Gastroenterology and Hepatology. 2008;6:443–450. doi: 10.1016/j.cgh.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 20.Jandorf L, Stossel LM, Cooperman JL, et al. Cost analysis of a patient navigation system to increase screening colonoscopy adherence among urban minorities. Cancer. 2013;119:612–620. doi: 10.1002/cncr.27759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sly JR, Edwards T, Shelton RC, Jandorf L. Identifying barriers to colonoscopy screening for nonadherent African American participants in a patient navigation intervention. Health Educ Behav. 2013;40:449–457. doi: 10.1177/1090198112459514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ladabaum U, Mannalithara A, Jandorf L, Itzkowitz S. Cost-effectiveness of patient navigation to increase adherence with screening colonoscopy among minority individual. Cancer. 2015;121:1088–1097. doi: 10.1002/cncr.29162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lebwohl B, Neugut AI, Stavsky E, et al. Effect of a patient navigator program on the volume and quality of colonoscopy. J Clin Gastroenterol. 2011;45:e47–e53. doi: 10.1097/MCG.0b013e3181f595c3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pike IM, Vicari J. Incorporating quality measurement and improvement into a gastroenterology practice. Am J Gastroenterol. 2010;105:252–254. doi: 10.1038/ajg.2009.475. [DOI] [PubMed] [Google Scholar]
- 25.New York City Department of Health and Mental Hygiene. [accessed Apr 17, 2015];Community health survey 2007. Available from URL: http://www.nyc.gov/html/doh/html/data/chs-data.shtml.
- 26.New York City Department of Health and Mental Hygiene. [accessed on Nov 24, 2014];Community health survey data 2007–2012. Available from URL: http://www.nyc.gov/html/doh/html/data/chs-data.shtml.
- 27.New York State Department of Health. [accessed Apr 17, 2015];Public health law. Available from URL: http://www.nyc.gov/html/doh/html/data/survey.shtml.
- 28.Health Resources and Services Administration. [accessed Nov 24, 2014];Unified data system, 2012. Available from URL: http://datawarehouse.hrsa.gov.
- 29.Lewis B, Henick A. [accessed Apr 17, 2015];How we leveled the CRC screening playing field. Available from URL: http://www.gastro.org/journals-publications/agaperspectives/octobernovember2014/how-we-leveled-the-crc-screening-playing-field.
- 30.Ladabaum U, Ferrandez A, Lanas A. Cost-effectiveness of colorectal cancer screening in high-risk spanish patients: Use of a validated model to inform public policy. Cancer Epidemiol Biomarkers Prev. 2010;19:2765–2776. doi: 10.1158/1055-9965.EPI-10-0530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Winawer SJ, Krabshuis J, Lambert R, O'Brien M, Fried M World Gastroenterology Organization Guidelines Committee. Cascade colorectal cancer screening guidelines: A global conceptual model. J Clin Gastroenterol. 2011;45:297–300. doi: 10.1097/MCG.0b013e3182098e07. [DOI] [PubMed] [Google Scholar]