Abstract
BACKGROUND
Schools are a key setting for childhood obesity interventions yet nurses are not often included in delivering these interventions. The objective of this systematic review and meta-analysis was to examine school-based interventions involving nurses in a role beyond anthropometric measurement for effect on change in body measures.
METHODS
We performed a systematic review and meta-analysis of these papers.
RESULTS
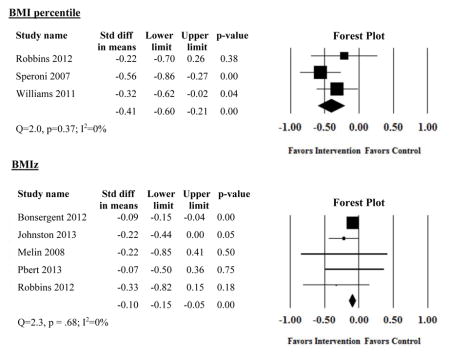
The literature search produced 2412 articles. Eleven met inclusion criteria for the systematic review (4 RCT, 7 quasi-experimental) and 8 for the meta-analysis. None have been included in prior meta-analyses. Four studies restricted eligibility to overweight and/or obese children; 7 included all children regardless of body weight. Random effects meta-analytic models represent data from 6050 (BMI), 5863 (BMIz), and 416 (BMI percentile) children respectively. Pooled analyses demonstrated statistically significant decreases in BMI (6 studies: −0.48 [95% CI −0.84, −0.12]; I2=91.2%, Q=68.1), BMIz (5 studies: −0.10 [95% CI: −0.15, −0.05]; I2=0, Q=2.3), and BMI percentile (3 studies: −0.41 [95% CI: −0.60, −0.21]; I2=0, Q=2.0).
CONCLUSIONS
These findings are similar to those of other meta-analyses of school-based interventions and suggest that school nurses can play a key role in implementing sustainable, effective school-based obesity interventions.
Keywords: childhood obesity, nurses, schools, meta-analysis
Childhood obesity affects 16.9% of children in the United States (US), with an additional 14.9% being overweight1 with children from racial minority groups and low-income households disproportionately affected.1,2 Childhood obesity is associated with morbidity, premature mortality,3 and obesity in adulthood.4,5 As a result, decreasing childhood obesity is a national6 and global7 priority.
In their recent report, Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation, the Institute of Medicine recommended that schools be a focal point of the fight against obesity.8 There is a growing body of research on school-based obesity interventions; however, findings are conflicting, with some demonstrating effectiveness9–12 and others finding that school-based interventions are not effective.13–16
One potential means of implementing effective school based interventions is to involve school nurses. School nurses may be well-suited to fight childhood obesity because of their ongoing connection with students and families, continual presence in schools, and cost-free accessibility to students.17–19 In addition, school nursing services are cost-beneficial.20 School nurses may provide a means of sustainability for an obesity intervention. Whereas many school-based obesity interventions may terminate when the research team completes their study, school nurses remain present in schools and available to work with children.
Previous systematic reviews and meta-analyses of school-based obesity interventions have not examined school nurse involvement. Therefore, the purpose of this study was to examine the efficacy of school-based obesity interventions that involve nurses.
METHODS
Eligibility Criteria
Studies of interest included school-based interventions to prevent or treat childhood obesity. Studies were included if they: (1) were of quasi-experimental or experimental design; (2) reported body weight or body mass index (BMI/BMIz/BMI percentile) as an outcome measure: (3) were conducted in a primary, middle, or high school setting; (4) involved nurses in the conduct of the study in a role beyond anthropometric measurement; (5) were published in a peer-reviewed journal; and (6) were written in the English language. Exclusion criteria were: (1) cross-sectional or cohort design; (2) no report of body weight or body mass index as an outcome measure; (3) conducted only in pre-school, day care, or university setting; (4) involvement of nurses in a role of anthropometric measurement only; (5) not published in a peer-review journal; and (6) published only in a language other than English. Neither year of publication and nor duration of follow-up was restricted. We included interventions implemented by registered nurses as their scope of practice is concordant with that of school nurses. However, studies reporting interventions delivered solely by student nurses or advanced practice nurses (nurse practitioners or clinical nurse specialists) were excluded, as their scope of practice differs significantly from that of registered nurses and school nurses.
Information Sources and Search
The research team developed a comprehensive search strategy in consultation with a research librarian (Appendix A). To ensure broad capture, search terms included BMI, overweight, obesity, adiposity, weight, schools, children, adolescents, teenagers, students, and nursing. Terms were searched in the title, abstract, and text. The search was performed within the Cumulative Index of Nursing and Allied Health Literature (CINAHL), Medline, PsychInfo, Proquest, and Education Resources Information Center (ERIC) databases in June 2014 and updated in March 2015. Search limitations were placed on source (peer-reviewed journals only) and language (English only). Reference lists of resulting studies were searched to ensure identification of any missed articles.
Study Selection
After search completion, title and abstracts were screened for eligibility criteria using Covidence,21 a software program designed to support the systematic review process. Each study was screened based on inclusion/exclusion criteria with the reason for decision entered into Covidence by one researcher. At each level of screening (title screen, abstract screen, full text screen), references were filtered into groups (included or excluded). Any uncertainty regarding study inclusion was resolved through discussion among the research team.
Data Extraction and Data Items
One researcher read each full-text article and extracted data into an Excel template that included details of study design, study location, study type (obesity prevention or obesity treatment), sample size and characteristics, intervention components, dose, and duration, methods of outcome measurement, and anthropometric outcomes and the time point of measurement.
Quantitative Synthesis
Studies that reported body measure change (BMI, BMIz, or BMI percentile) and a measure of variance (standard deviation, standard error) or p-value were eligible for inclusion in the meta-analysis. When sufficient data for effect size calculation were not provided in the manuscript, study authors were contacted for additional information. Effect sizes were calculated and pooled using Comprehensive Meta-analysis version 3.22 Effect sizes were combined using the inverse variance weighted method in a random effects model.23 For effect size calculations, a pre/post correlation of anthropometric measures was assumed to be 0.90, based on published reports,24 with sensitivity analyses conducted with a range of 0.80 to 0.99. When outcomes at different time points were reported, results from the longest follow-up were used. Heterogeneity of each model was assessed using Cochran’s Q and I-squared tests. Where heterogeneity was present, subgroup and sensitivity analyses were conducted to explore potential sources of heterogeneity and assess robustness of the point estimate. To assess publication bias, we conducted a failsafe N test and visually inspected funnel plots.23
Risk of Bias
Risk of bias was assessed using The Checklist for Measuring Quality, developed by Downs and Black.25 This 27 item checklist assesses 5 aspects of a study: reporting (10 items); external validity (3 items); bias (7 items); confounding (6 items); and power analysis (1 item). Each item is scored as 0 or 1 (with the exception of item 5, which addresses distribution of confounders between groups of participants and can receive a score between 0 and 2) resulting in a total quality index score ranging between 0 and 28 with a higher score indicating higher study quality. The tool is a reliable and valid measure that can be applied to quasi-experimental and experimental healthcare intervention studies.25 Two reviewers independently appraised each study. Following evaluation completion, ratings were compared with discrepancies discussed until consensus was achieved.
RESULTS
Study Selection
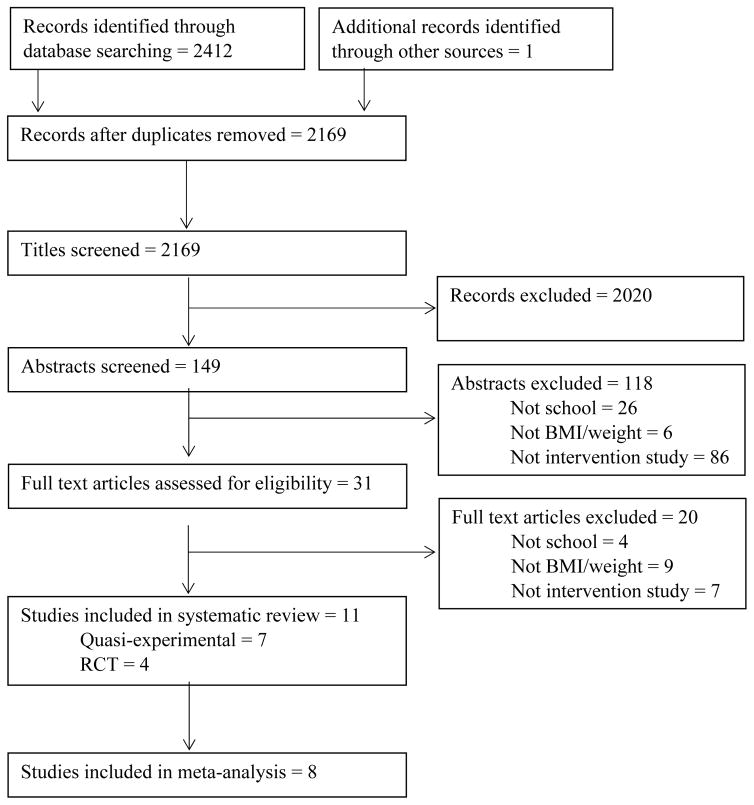
Figure 1 displays the results of the search and study selection. The search resulted in 2412 articles, with an additional study arising from a manual screen of reference lists. During screening, 243 studies were excluded due to duplication, 2020 studies were excluded based on title, and 118 were excluded based on abstract. An additional 20 articles were excluded based on exclusion criteria during full-text review. Eleven studies met all criteria and were included in the systematic review; 8 were included in the meta-analysis. Four authors19,26–28 were contacted for further information and 2 provided additional data enabling inclusion in the meta-analysis. 19,27
Figure 1.
Summary of the Literature Search
Risk of Bias
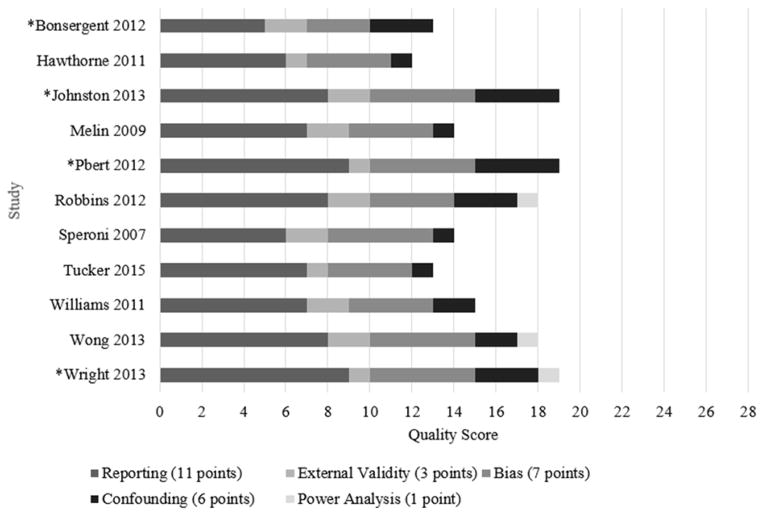
Figure 2 provides detail regarding the results of the quality appraisal. Regarding study reporting, all studies reported clear study objectives and outcomes of interest, though only one reported adverse events such as the child feeling stigmatized by participating in the intervention.29 Only 2 studies reported characteristics of patients lost to follow-up.17,30 Three studies reported attrition rates, with rates ranging from no attrition at 6 months17 to 21.2% attrition at 24 months.30 Concerning external validity, no study addressed whether the baseline sample was representative of the recruited population. Regarding internal validity, most studies did not report blinding of participants (except one which included an attention control31) or outcomes assessors. Regarding confounding, although each quasi-experimental study provided a partial list of cofounders to be considered in group comparisons, statistical adjustment for confounders was incomplete.19,26,27,29,31–33 No study reported their method of allocation concealment. Only 3 studies28,31,32 reported a priori power analyses. Quality scores ranged between 1230 and 1917,26,32 points.
Figure 2.
Risk of Bias Assessment Based on Downs and Black Checklist
*Randomized controlled trial
Characteristics of the Included Studies
An overview of study characteristics is presented in Table 1. Seven studies employed a quasi-experimental design19,26,27,29,31–33 and 4 were randomized controlled trials (RCT).17,28,30,34 All RCTs randomized participants at the school level. One RCT34 used a 2×2×2 factorial design, with one arm including nurses. The data extracted for this review were limited to the nursing arm. A second manuscript35 arising from the same study more fully described each arm; this was referenced for additional information as needed. Four studies restricted their sample to overweight or obese students17,29,32,34 and were categorized as obesity treatment interventions. Seven studies included all students in the intervention19,26–28,30,31,33 and were categorized as obesity prevention interventions.
Table 1.
Characteristics of Included Studies Grouped by Study Type (Obesity Prevention vs. Obesity Treatment)
| Author, Year | Sample Size Attrition Rate Follow-up in Months |
Sample Characteristics (Mean Age, Race, Other) | Intervention Characteristics | School Nurse (Y/N) Nursing Role |
|---|---|---|---|---|
|
Obesity Treatment Studies
| ||||
| *Bonsergent 2012 | I: 2641 C: 2713 Attrition: NR 24 |
15.6 years Race: NR Overweight/obese |
I: Students screened for height, weight, and waist circumference; overweight/obese students counseled regarding screening results; students who screened positive invited to join health education program (25% of eligible students participated) C: No intervention |
Y Assisted physician with individual counseling, body measurement |
| Melin 2009 | I: 20 C: 19 Attrition: NR 12 |
I: 8.1 years C: 8.0 years Race: NR Overweight/obese |
I: Dietitian interviewed children and families at baseline about dietary habits, PA, and well-being and gave individual health advice; monthly counseling, education, and weight monitoring with school nurses C: No intervention |
Y Individual counseling and education, body measurement |
| *Pbert 2012 | I: 42 C: 40 Attrition: 0% 6 |
I: 15.9 years C: 15.7 years Asian: NR Black: 14.3% Hispanic: 14.3% White: 73.8% Overweight/obese Free/reduced lunch: 47.6% |
I: Six counseling sessions with school nurse over two months C: Six informational pamphlets on weight management given during school nurse visits |
Y Individual counseling |
| Wong 2013a | I (A): 70 I (B): 66 C: 49 Attrition: NR 3.5 |
9–10 years Race: NR Obese |
I (A): Motivational interviewing with students focused on dieting and exercise I (B): Intervention A plus parental counseling via telephone C: No intervention |
N Motivational interviewing |
|
| ||||
|
Obesity Prevention Studies
| ||||
| Hawthorne 2011 | I: 1074 Attrition: NR 4 |
K to 6th Grade Asian: NR Black: NR Hispanic: 43% White: NR Low income school |
I: Walking track during recess; mileage check-off card for incentives and prizes C: No control group |
N Designed intervention, implemented physical activity program |
| *Johnston 2013 | I: 392 C: 237 Attrition: 21.2% 24 |
I: 7.8 years C: 7.7 years Asian: 27.0% Black: 21.4% Hispanic: 24.4% White: 27.3% |
I & C: One day training for teachers and school staff, provision of curriculum with health information, teaching aids, and health/nutrition educations materials I only: Health professional at school three days per week to assist with daily integration of curriculum, one nutrition counseling by school nurse at either parent request or by teacher referral |
Y Counseling |
| Robbins 2012 | I: 37 C: 32 Attrition: NR 6 |
I: 11.5 years C: 11.4 years Asian: NR Black: 49.7% Hispanic 21.6% White: 24.4% Free/reduced lunch: 75% |
I: Daily after school PA club; three motivational interviewing sessions with school nurse (one every two months) C: Six monthly afterschool workshop, three health education sessions with school nurse (one every two months) |
Y Motivational interviewing |
| Speroni 2007 | I: 80 C: 105 Attrition: NR 6 |
I: 9.4 years C: 9.2 years Asian: NR Black: NR Hispanic: NR White: 78.3% |
I: Weekly after school program with physical activity, fitness education, and nutrition education C: No intervention |
N Design and coordination, body measurement |
| Tucker 2015 | I (A): 48 I (B): 20 Attrition: 5.6% I (A): 7 I (B): 3 |
9–11 years Asian: 8.3% Black: 5.6% Hispanic: 5.6% White: 84.7% |
I (A) & I (B): Weekly class presentations by school nurse on Let’s Go 5-2-1-0 program behaviors (fruit/vegetable intake, screen time, physical activity, and sugary beverages); 14–21 reinforcement sessions during school lunch and/or recess with senior nursing students; group A and B received same intervention – only duration of intervention differed C: No control group |
Y Classroom education sessions |
| Williams 2011 | I: 56 C: 175 Attrition: Students who did not complete the program comprised the control group 3 |
8–10 years Asian: NR Black: 99.3% Hispanic: NR White: NR Free/reduced lunch: 80% |
I: Walking education, walking supplies, and prizes; teachers received suggestions about how to engage children and bring walking into curriculum C: Received all or part of the intervention but did not complete full 12 week program |
N Study management |
| *Wright 2013 | I: 91 C: 99 Attrition: 0% 12 |
I: 9.0 years C: 8.3 years Asian: NR Black: 2.4% Hispanic: 94% White: NR |
I: 6 week after school program with PA groups for children and support groups focusing on education and behavior modification for parents; creation of School Health Advisory Council, staff professional development seminars C: No intervention |
N Assisted with intervention design, led parent education and support groups |
NR = not reported, I = intervention, C = control, PA=physical activity * = Randomized controlled trial
Obesity treatment
Of the 4 obesity treatment studies, 2 were RCTs17,34 and 2 were quasi-experimental (pretest-posttest) design.29,32 Study samples included school-age children29,32 and teenagers.17,34 Sample sizes varied ranging from 3929 to 3191 students.34 One study was conducted in the US,17 with the remaining studies conducted in Asia32 and Europe.29,34 In one intervention, approximately half of the children were from low income households and eligible to receive free or reduced school lunches.17
Intervention follow-up varied ranging from 3.532 to 24 months.34 Intervention dosage ranged from near weekly (6 sessions over 8 weeks),17 to monthly,29 to one time only (with optional follow-up sessions, declined by approximately 75% of eligible participants).34 In one32 study, registered nurses, trained in motivational interviewing and weight management, counseled students about health behavior change during 6 sessions over 14 weeks, with decreasing frequency as the intervention progressed.
All interventions included student education and counseling17,29,32,34 with 2 of the interventions29,32 involving parents. Parent roles included participating in telephone consultations32 or attending their child’s nutritional counseling sessions.29 Three interventions were delivered during the school day.17,29,34 Effects on body measures, presented in Table 2, ranged from −0.0634 to −1.4832 for BMI, −0.0934 to −0.2229 for BMIz, and −0.0219 and −0.3233 for BMI percentile.
Table 2.
Effect Sizes of Included Studies, Grouped by Study Type (Obesity Treatment vs. Obesity Prevention)
| Author, Year | Measure | Outcome Studied | Study Result: Interventions vs Control* |
|---|---|---|---|
|
Obesity Treatment Studies
| |||
| Bonsergent 2012 | Mean change at 24 months | BMI | 0.64 (1.44) vs. 0.72 (1.49)** |
| BMIz | −0.09 (0.44) vs −0.05 (0.43)** | ||
| Melin 2009 | Mean change at 12 months | BMI | 1.9 (1.7) vs. 2.1 (1.5) |
| BMIz | −0.05 (0.5) vs. 0.04 (0.3)** | ||
| Pbert 2012 | Mean change at 2 months | BMI | 0.01 (1.64) vs. 0.14 (1.14) |
| BMIz | 0.00 (0.17) vs. 0.01 (0.11) | ||
| Mean change at 6 months | BMI | −0.01 (1.98) vs. 0.26 (1.59) | |
| BMIz | 0.00 (0.21) vs. 0.01 (0.17) | ||
| Mean difference in change at 2 months, adjusted for demographic and behavioral confounders | BMI | −0.09 (3.40) | |
| BMIz | −0.01 (0.37) | ||
| Mean difference in change at 6 months, adjusted as per 2 months | BMI | −0.22 (4.62) | |
| BMIz | −0.02 (0.47) | ||
| Wong 2013 | Mean change at 3.5 months | BMI | A: −0.67 (1.01) vs 0.81 (0.92)** |
| B: −1.17 (0.99) vs 0.81 (0.92)** | |||
|
| |||
|
Obesity Prevention Studies
| |||
| Hawthorne 2011 | Mean change at 4 months | BMI percentile | Not reported |
| Johnston 2013 | Mean change at 12 months | BMI | 0.8 (1.3) vs. 0.78 (1.4) |
| BMIz | −0.07 (0.24) vs. −0.05 (0.25) | ||
| Mean change at 24 months | BMI | 1.67 (1.67) vs. 1.92 (1.91) | |
| BMIz | −0.08 (0.27) vs. −0.02 (0.27)** | ||
| Robbins 2012 | Mean change at 6 months | BMI | 0.41 (1.02) vs. 0.74 (0.73) |
| BMIz | 0.06 (0.18) vs. 0.12 (0.18) | ||
| BMI percentile | 1.94 (4.59) vs. 3.05 (5.68) | ||
| Linear regression models, adjusted for baseline measures | BMI | −0.33 (0.22) | |
| BMIz | −0.04 (0.04) | ||
| BMI percentile | −0.57 (0.97) | ||
| Speroni 2007 | Mean change at 6 months | BMI percentile | −2.3 (p 0.01) vs. (p 0.01)** |
| Tucker 2015 | Mean change at 3 months | BMI percentile | −0.6 |
| Mean change at 7 months | −2.3 | ||
| Williams 2011 | Mean change at 3 months | BMI percentile | −2.57 vs. 1.07 |
| Wright 2013 | Mean change at 12 months, adjusted for baseline scores, race and parent marital status | BMI | Boys: −2.56 (10.68) vs. 1.35 (31.79) |
| Girls: −3.65 (14.06) vs. 1.23 (26.28) | |||
| BMIz | Boys: −0.19 (4.85) vs. 0.79 (13.16) | ||
| Girls: −0.70 (2.09) vs. 0.58 (11.90)** | |||
Results are unadjusted unless otherwise indicated. Results from unadjusted analyses used to calculate effect size.
Statistically significant at p < .05
Obesity prevention
Of the 7 obesity prevention studies, 2 were RCTs28,30 and 5 were quasi-experimental studies.19,26,27,31,33 All were conducted in the US and targeted school-age children. Sample sizes ranged from 6819 to 1074 students.26 Five studies included students from populations that are known to suffer from health disparities such as racial/ethnic minorities27,33,36 or students from low-income households.26,31,33
Intervention follow-up ranged from 319,33 to 24 months.30 Intervention intensity ranged from daily (via integrated curriculum),30 to 3 times per week,26 to weekly.19,27,28,31 One intervention was initiated via a one-time educational assembly with teachers encouraged to regularly incorporate the intervention into class curriculum.33
Intervention components varied and included parent education and counseling,28 staff education,28,30 physical activity,26–28,31,33 and student education and counseling.19,27,31 Some interventions occurred after school,26–28,31 while others occurred during the school day.19,30 Three studies actively involved parents via participation in either an educational support group 28 or attendance at student counseling30 or student nutrition education sessions.27 Control groups received either no intervention,27,28 part of but not all of the same intervention as the intervention group,33 or an attention control.30,31 Effect on body measures ranged from 0.0230 to −0.3731 for BMI, −0.0830 to −0.3431 for BMIz, and −0.0219 to −0.2231 for BMI percentile (Table 2).
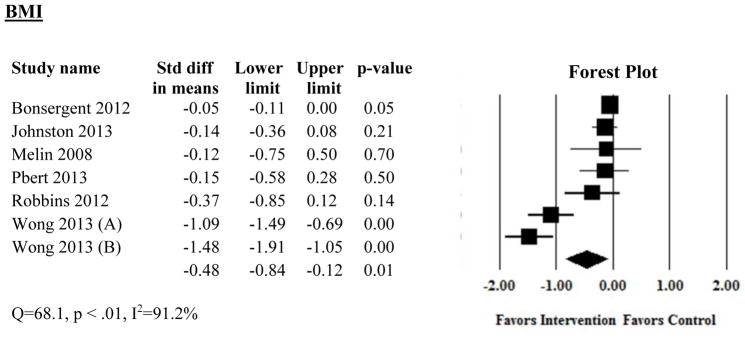
Quantitative Synthesis
Three studies were excluded from meta-analysis due to outcomes being in an unusable format (ie, “no significant change”),26 no comparison group,19 and report of only adjusted and sex-specific outcomes. In one study32 2 intervention approaches were tested compared to a control group. Forest plots present the pooled analysis for decreases in body mass index (6 studies, Figure 3), BMIz score (5 studies, Appendix B) and BMI percentile (3 studies, Appendix B) and represents data from 6050, 5863, and 416 children respectively. The pooled decrease in BMI was −0.48 (95% CI: −0.84, −0.12; I2=91.2%, Cochran Q=68.1). Heterogeneity was higher than would be expected by chance. To explore heterogeneity, we performed a sensitivity analysis by removing the study with the largest effect size32 and conducting subgroup analyses with and without the outlier. After removing this study, the pooled effect size was attenuated to −0.06 (95% CI: −0.17, −0.01; I2=0, Cochran Q=2.3). The pooled decreases in BMIz and BMI percentile were −0.10 (95% CI: −0.15, −0.05; I2=0, Cochrane Q=2.3) and −0.41 (95% CI: −0.60, −0.21; I2=0, Cochrane Q=2.0) respectively. We conducted sensitivity analyses to broaden the range of correlation assumptions from 0.80 and 0.99 between baseline and post intervention BMI, BMIz and BMI percentile. The pooled effects ranged between −0.34 (95% CI: −0.67, −0.10) and −1.12 (95% CI: −1.85, −0.38) for BMI and −0.36 (95% CI: −0.60, −0.12) to −0.62 (95%CI: −1.03, −0.21) for BMI percentile; there was no change in BMIz effect across the range of correlation assumptions. Table 3 presents the results of subgroup analysis with and without the study demonstrating the largest BMI reduction.32 When all studies were included there were significant differences in BMI reduction based on study duration and study design. However, when one study was removed, there were no differences in BMI reduction by subgroup.
Figure 3.
Forest Plots of Studies Examining Effect of Interventions on Change in Body Mass Index
Table 3.
Subgroup Analyses for Change in Body Mass Index
| Subgroup Analysis | Number of studies | Difference in Means | 95% CI |
|---|---|---|---|
| Study design* | |||
| RCT | 3 | −0.06 | −0.11, −0.01 |
| Quasi-experimental | 3 | −0.80 | −1.38, −0.21 |
| Study purpose: | |||
| Obesity treatment | 4 | −0.58 | −1.19, 0.03 |
| Obesity prevention | 2 | −0.18 | −0.38, 0.02 |
| Parent involvement: | |||
| Yes | 3 | −0.72 | −1.42, −0.01 |
| No | 3 | −0.06 | −0.11, −0.01 |
| Study duration* | |||
| <6 months | 1 | −1.28 | −1.66, −0.90 |
| >6 months | 5 | −0.06 | −0.12, −0.01 |
| ≥50% children from racial/ethnic minority group or low income household | |||
| Yes | 3 | −0.18 | −0.36, 0.01 |
| No | 3 | −0.69 | −1.47, 0.10 |
p < .05
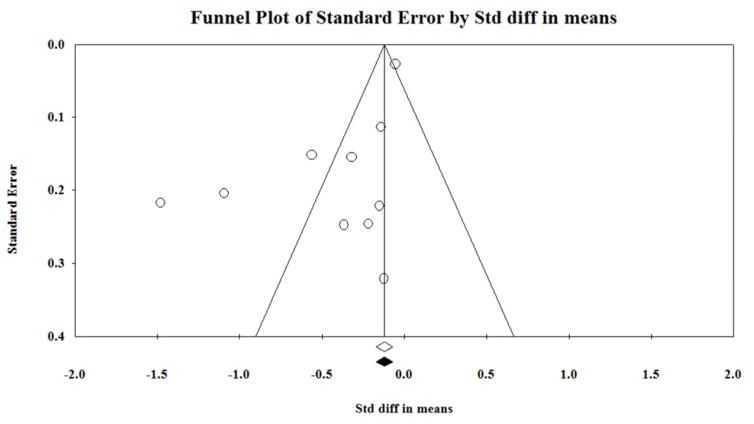
Appendix C presents the funnel plot of all studies included in the meta-analysis. The 2 dots to the left of the pyramid indicate the study with the largest effect size.32 Otherwise, there is relative symmetry of the study distribution within the pyramid demonstrating that publication bias is unlikely. The failsafe N test demonstrated that 114 additional studies would need to be added to the meta-analysis before loss of statistical significance occurred.
DISCUSSION
Our findings demonstrate that school-based interventions that involve nurses lead to small but significant decreases in BMI, BMIz and BMI percentile. Eight prior meta-analyses9–16 published between 2008 and 2015 have examined the effectiveness of school-based interventions. Four9–12 found effectiveness of school based interventions; interventions that included nutrition and physical activity components,9,10 lasted greater than one year, involved parents, and entailed a comprehensive approach were found to be most effective.10 Although 4 reviews13–16 concluded that school-based obesity interventions were not effective, subgroup analyses found that interventions of RCT design, interventions that included a nutrition component, and interventions that included only one component (versus multifaceted)15 were effective in reducing BMI.
In our analysis, pooled effect sizes were similar across all anthropometric outcomes and similar to the findings of some prior meta-analyses.9–16 Only one study demonstrated a notably large decrease in BMI across both intervention arms.32 This intervention, conducted in Hong Kong, included formal involvement of parents as a pillar of the intervention. In addition, cultural factors may have contributed to the intervention’s success, as Asian children may differ in cultural perceptions of obesity compared to Western children.37
Although obesity interventions that involve nurses are effective; barriers exist to involvement of school nurses in implementation of childhood obesity interventions. Previous studies have suggested time to be a barrier to implementation, despite school nurses’ interest in and willingness to execute obesity initiatives.38 School nurses report that lack of confidence in counseling methods and poor parental support limit the nurses’ willingness to provide obesity interventions.18,39 Across the US, understaffing of school nurses is a concern due to budget constraints for hiring and shortages of professional school nurses.20,40,41 Considering the widespread prevalence and negative health effects of childhood obesity, school administrators and policymakers must carefully consider the need for adequate school nurse staffing.
The small effect sizes for change in BMI, BMIz and BMI percentile support the argument that the substantial body weight changes needed to help children shift from obese or overweight to a healthy weight may require more intensive intervention than can be provided solely in a school setting. Many factors outside the school setting impact health, nutrition and body weight.42 The American environment has been called obesogenic43–45 with factors such as advertising of unhealthy foods,46 suburban sprawl and decreased walkability,47 and large portion sizes48 promoting obesity. Thus, even effective school-based interventions face an uphill battle because addressing obesity, a complex problem, requires multifaceted societal change.49
The findings of this review suggest that anthropometric outcomes were similar for obesity treatment and obesity prevention interventions. School-based interventions may be better suited for obesity prevention. All of the interventions in this review entailed healthy habits education or counseling which is appropriate for children of all body weights. School-based obesity prevention interventions also avoid concerns about stigmatizing children with obesity because all children, not only those who are obese, receive the intervention. In addition, it may be difficult for schools to implement intensive treatment regimens; prevention interventions may be more feasible. Intensive intervention may be easier to administer in primary care or an obesity clinic under the medical guidance of a child’s primary care provider.
Our systematic review has implications for future work. We suggest that more school nurse-led interventions be implemented and evaluated, as limited evidence exists. Future research should include studies with strong designs for inferring causality, larger samples and longer follow up times. In alignment with the National Association of School Nursing’s Research Priorities for School Nursing, school nurse-led obesity interventions should also be evaluated for their impact on chronic conditions (diabetes, asthma) and nurse sensitive indicators (attendance, health office visits). In addition, when possible, cost-benefit analyses of school nurse-led obesity interventions should be conducted.50
Limitations
Our systematic review has several limitations. Only English language and peer-reviewed studies were included. We did not consider grey literature, dissertations, and conference abstracts leading to possible omission of studies. It is plausible that our search strategy omitted studies, despite our efforts at developing a comprehensive strategy.
Conclusion
School-based obesity interventions are one potential solution to the childhood obesity crisis and school nurses are optimally poised to play a role in these interventions. Findings of this systematic review suggest that school nurses may be beneficial in implementation of sustainable interventions for reducing childhood overweight/obesity. Development of evidenced-based school-based obesity interventions that incorporate school nursing expertise can result in effective management of childhood obesity and improved child health.
IMPLICATIONS FOR SCHOOL HEALTH
Our review demonstrated that school-based interventions that involve nurses help children to significantly decrease body measures. In developing obesity interventions, schools should consider involving school nurses as key players and include them in a role beyond anthropometric measurement.38,51 For example, school nurses should actively participate in School Wellness Committees and any health-focused school working groups. If not invited, school nurses can and should advocate for their inclusion on such teams by speaking with their school administrators. School nursing leadership, such as school nurses who work in a supervisory or administrative role, can also support implementation of school-based obesity programs, by approaching other members of the school administration about the need for and success of such programs. Such conversations may include advocating for budgetary support for such programs, such as monies needed to pay school nurses for attending training sessions in preparation for program implementation. Lastly, school nurses can disseminate their work with school-based obesity programs through presentations at local or national organization meetings, such as the National Association of School Nurses. Dissemination can help other school nurses to advocate for as well as develop and implement programs at the local level.
The results of this review do not demonstrate any particular characteristics that promote or hinder effectiveness of school-based interventions that involve nurses. However, schools can consider designing their nurse-led programs to incorporate factors that have been found to increase success of other school-based interventions, such as including nutrition15 or nutrition and physical activity components,9,10 lasting longer than one year (ie, continuing a child’s involvement in the program as (s)he moves into the next grade), taking a comprehensive approach (ie, attitudinal and behavior change, health education, and environmental modification),10 and involving parents.10 School nurses can help incorporate these factors into obesity programs in multiple ways.38,51 For example, nurses can attend Parent Teacher Association meetings to discuss the goals of an obesity program with parents and encourage parental involvement. School nurses can support longer duration of child involvement in obesity programs by continuing to work with children as they progress from grade to grade. Of note, because we found that both obesity treatment and obesity prevention programs are effective, schools do not have to single out children with overweight or obesity and can consider implementing prevention programs that are appropriate for all members of the student body. Though challenging in the modern era of budget constraints and busy school nursing practice, if at all possible, school nurses should be supported in dedicating a portion of their time to development and implementation of school-based obesity prevention programs.
Because out review demonstrated effectiveness of school-based obesity interventions that involve nurses, schools can feel confident in providing school nurses with the necessary resources (ie, time, administrative support) to implement obesity programs. In doing so, schools are supporting development of sustainable, effective interventions that can promote child health and healthy body weight for their students.
Human Subjects Approval Statement
This study involves no human subjects in the research, and therefore, was exempt from institutional review board examination.
Acknowledgments
This publication was supported by the National Institute of Nursing Research through Grant Numbers T32 NR014205 (KS) and R01NR013687 (JT), the National Center for Advancing Translational Sciences through Grant Number UL1 TR000040 (KS), and the Jonas Center for Nursing and Veterans Healthcare (JT). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Jonas Center for Nursing and Veterans Healthcare.
Appendix A: Search strategy
Databases: Cumulative Index for Nursing and Allied Health Literature (CINAHL), Education Resources Information Center (ERIC), PsycINFO <June 20, 2014>
Search Strategy:
schoolchildren
school children
teen*
preschool student*
child*
youth*
adolescen*
kid*
Boy*
Girl*
paediatr*
pediatr*
student*
Elementary School Student*
Junior High School Student*
High School Student*
Middle School Student*
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18
body mass index
BMI
obes*
overweight*
body fat*
weigh*
adipos*
19 or 20 or 21 or 22 or 23 or 24 or 25
School*
Nurs*
18 and 26 and 27 and 28 (1572)
Database: MEDLINE <June 20, 2014>
Search strategy:
(schoolchildren or school children).mp
teen*.mp
exp preschool students/
child*.mp
youth*.mp
adolescen*.mp
kid*.mp
boy*.mp
girl*.mp
paediatr*.mp
pediatr*.mp
student*.mp
Elementary School Students/ or Junior High School Students/ or High School Students/ or Middle School Students/
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13
Exp body mass index/
exp obesity/
exp overweight/
body fat/
exp weight loss/
exp weight gain/
body fat/
15 or 16 or 17 or 18 or 19 or 20 or 21
exp school based intervention/
exp after school programs OR school*.mp
exp schools/
exp Junior High Schools/ or High Schools/ or exp Middle Schools/ or exp Nursery Schools/ or Elementary Schools/
23 or 24 or 25 or 26
exp nurses/ or nursing/
14 and 22 and 27 and 28 (14)
Database: Proquest <June 20, 2014>
Search Strategy:
schoolchildren
school children
teen*
preschool student*
child
youth*
adolescen*
kid*
boy*
girl*
paediatr*
pediatr*
student*
Elementary School Student*
Junior High School Student*
High School Student*
Middle School Student*
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17
body mass index
BMI
obes*
overweight*
body fat*
weigh*
adipos*
19 or 20 or 21 or 22 or 23 or 24 or 25
school*
nurs*
18 and 26 and 27 and 28 (826)
Appendix B. Forest plots of studies included in meta-analysis of intervention impact on BMI percentile and BMIz
Appendix C. Funnel plot for assessment of publication bias
The funnel plot represents the mean differences in body measures for overweight/obese youth who received obesity treatment or prevention interventions delivered in school settings with those who did not. The plot shows the standard error of the mean difference in body measure (Y axis) versus the reported mean difference (X axis). The open diamond indicates the pooled effect size and its 95% confidence interval, and the filled diamond indicates the pooled effect size and 95% confidence interval when missing studies suggested by publication bias analysis are included.
Contributor Information
Krista Schroeder, Email: ks3139@cumc.columbia.edu, Pre-doctoral Fellow, Columbia University School of Nursing, 617 West 168th Street, New York, NY 10032, Phone: (908) 763-3647.
Jasmine Travers, Email: jt2766@cumc.columbia.edu, PhD Student, Columbia University School of Nursing, 617 West 168th Street, New York, NY 10032, Phone: (631) 838-9963.
Arlene Smaldone, Email: ams130@cumc.columbia.edu, Associate Professor of Nursing, Associate Professor in Dental Behavioral Sciences (in Dental Medicine), Assistant Dean of Scholarship and Research (School of Nursing), Columbia University School of Nursing, 617 West 168th Street, New York, NY 10032, Phone: (212) 342-3048.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang Y, Lim H. The global childhood obesity epidemic and the association between socio-economic status and childhood obesity. Int Rev Psychiatry. 2012;24(3):176–188. doi: 10.3109/09540261.2012.688195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: a systematic review. Int J Obes. 2011;35(7):891–898. doi: 10.1038/ijo.2010.222. [DOI] [PubMed] [Google Scholar]
- 4.Guo SS, Chumlea WC. Tracking of body mass index in children in relation to overweight in adulthood. Am J of Clin Nutr. 1999;70(1):145S–148S. doi: 10.1093/ajcn/70.1.145s. [DOI] [PubMed] [Google Scholar]
- 5.Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS. The relation of childhood BMI to adult adiposity: the Bogalusa Heart Study. Pediatrics. 2005;115(1):22–27. doi: 10.1542/peds.2004-0220. [DOI] [PubMed] [Google Scholar]
- 6.United States Department of Health and Human Services. [Accessed February 2, 2016];Health People 2020: Nutrition and Weight Status. 2014 Available at: http://www.healthypeople.gov/2020/topics-objectives/topic/nutrition-and-weight-status.
- 7.World Health Organization. [Accessed February 2, 2016];Prioritizing areas for action in the field of population-based prevention of childhood obesity. 2012 Available at: http://www.who.int/dietphysicalactivity/childhood/WHO_new_childhoodobesity_PREVENTION_27nov_HR_PRINT_OK.pdf.
- 8.Institute of Medicine. [Accessed February 2, 2016];Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. 2012 Available at: http://iom.nationalacademies.org/Reports/2012/Accelerating-Progress-in-Obesity-Prevention.aspx. [PubMed]
- 9.Katz DL, O’Connell M, Njike VY, Yeh MC, Nawaz H. Strategies for the prevention and control of obesity in the school setting: Systematic review and meta-analysis. Int J Obes. 2008;32(12):1780–1789. doi: 10.1038/ijo.2008.158. [DOI] [PubMed] [Google Scholar]
- 10.Sobol-Goldberg S, Rabinowitz J, Gross R. School-based obesity prevention programs: a meta-analysis of randomized controlled trials. Obesity. 2013;21(12):2422–2428. doi: 10.1002/oby.20515. [DOI] [PubMed] [Google Scholar]
- 11.Wang Y, Wu Y, Wilson RF, et al. Comparative Effectiveness Reviews. Rockville, MD: Johns Hopkins University Evidence-based Practice Center; 2013. Childhood obesity prevention programs: comparative effectiveness review and meta-analysis. [PubMed] [Google Scholar]
- 12.Waters E, de Silva-Sanigorski A, Hall BJ, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev (Online) 2011:12. doi: 10.1002/14651858.CD001871.pub3. [DOI] [PubMed] [Google Scholar]
- 13.Gonzalez-Suarez C, Worley A, Grimmer-Somers K, Dones V. School-based interventions on childhood obesity: a meta-analysis. Am J Prev Med. 2009;37(5):418–427. doi: 10.1016/j.amepre.2009.07.012. [DOI] [PubMed] [Google Scholar]
- 14.Harris KC, Kuramoto LK, Schulzer M, Retallack JE. Effect of school-based physical activity interventions on body mass index in children: a meta-analysis. CMAJ. 2009;180(7):719–726. doi: 10.1503/cmaj.080966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hung LS, Tidwell DK, Hall ME, Lee ML, Briley CA, Hunt BP. A meta-analysis of school-based obesity prevention programs demonstrates limited efficacy of decreasing childhood obesity. Nutr Res. 2015;35(3):229–240. doi: 10.1016/j.nutres.2015.01.002. [DOI] [PubMed] [Google Scholar]
- 16.Kanekar A, Sharma M. Meta-analysis of school-based childhood obesity interventions in the U.K. and U.S. Int Q Community Health Educ. 2009;29(3):241–256. doi: 10.2190/IQ.29.3.d. [DOI] [PubMed] [Google Scholar]
- 17.Pbert L, Druker S, Gapinski MA, et al. A school nurse-delivered intervention for overweight and obese adolescents. J Sch Health. 2013;83(3):182–193. doi: 10.1111/josh.12014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morrison-Sandberg LF, Kubik MY, Johnson KE. Obesity prevention practices of elementary school nurses in Minnesota: findings from interviews with licensed school nurses. J Sch Nurs. 2011;27(1):13–21. doi: 10.1177/1059840510386380. [DOI] [PubMed] [Google Scholar]
- 19.Tucker S, Lanningham-Foster LM. Nurse-led school-based child obesity prevention. J Sch Nurs. 2015;31(6):450–466. doi: 10.1177/1059840515574002. [DOI] [PubMed] [Google Scholar]
- 20.Wang LY, Vernon-Smiley M, Gapinski MA, Desisto M, Maughan E, Sheetz A. Cost-benefit study of school nursing services. JAMA Pediatr. 2014;168(7):642–648. doi: 10.1001/jamapediatrics.2013.5441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Covidence. 2013
- 22.Comprehensive Meta-analysis. Comprehensive Meta-analysis. 2015
- 23.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to Meta-analysis. West Sussex, UK: John Wiley and Sons Ltd; 2009. [Google Scholar]
- 24.Lin JS, O’Connor E, Whitlock EP, et al. Behavioral Counseling to Promote Physical Activity and a Healthful Diet to Prevent Cardiovascular Disease in Adults: Update of the Evidence for the US Preventive Services Task Force. Rockville, MD: Agency for Healthcare Research and Quality; 2010. Evidence Syntheses, No. 79. [PubMed] [Google Scholar]
- 25.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hawthorne A, Shaibi G, Gance-Cleveland B, McFall S. Grand Canyon Trekkers: school-based lunchtime walking program. J Sch Nurs. 2011;27(1):43–50. doi: 10.1177/1059840510391669. [DOI] [PubMed] [Google Scholar]
- 27.Speroni KG, Earley C, Atherton M. Evaluating the effectiveness of the Kids Living Fit[TM] program: a comparative study. J Sch Nurs. 2007;23(6):329–336. doi: 10.1177/10598405070230060501. [DOI] [PubMed] [Google Scholar]
- 28.Wright K, Giger JN, Norris K, Suro Z. Impact of a nurse-directed, coordinated school health program to enhance physical activity behaviors and reduce body mass index among minority children: a parallel-group, randomized control trial. Int J Nurs Stud. 2013;50(6):727–737. doi: 10.1016/j.ijnurstu.2012.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Melin A, Lenner RA. Prevention of further weight gain in overweight school children, a pilot study. Scand J Caring Sci. 2009;23(3):498–505. doi: 10.1111/j.1471-6712.2008.00651.x. [DOI] [PubMed] [Google Scholar]
- 30.Johnston CA, Moreno JP, El-Mubasher A, Gallagher M, Tyler C, Woehler D. Impact of a school-based pediatric obesity prevention program facilitated by health professionals. J Sch Health. 2013;83(3):171–181. doi: 10.1111/josh.12013. [DOI] [PubMed] [Google Scholar]
- 31.Robbins LB, Pfeiffer KA, Maier KS, Lo Y-J, Wesolek SM. Pilot intervention to increase physical activity among sedentary urban middle school girls: a two-group pretest-posttest quasi-experimental design. J Sch Nurs. 2012;28(4):302–315. doi: 10.1177/1059840512438777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wong EMY, Cheng MMH. Effects of motivational interviewing to promote weight loss in obese children. J Clin Nurs. 2013;22(17–18):2519–2530. doi: 10.1111/jocn.12098. [DOI] [PubMed] [Google Scholar]
- 33.Williams, Warrington Get Fit Kids: A feasibility study of a pedometer-based walking program. Bariatric Nursing and Surgical Patient Care. 2011;6(3):139–143. [Google Scholar]
- 34.Bonsergent E, Thilly N, Legrand K, et al. Process evaluation of a school-based overweight and obesity screening strategy in adolescents. Glob Health Promot. 2013;20(2):76–82. doi: 10.1177/1757975913483330. [DOI] [PubMed] [Google Scholar]
- 35.Bonsergent E, Agrinier N, Thilly N, et al. Overweight and obesity prevention for adolescents: a cluster randomized controlled trial in a school setting. Am J Prev Med. 2013;44(1):30–39. doi: 10.1016/j.amepre.2012.09.055. [DOI] [PubMed] [Google Scholar]
- 36.Johnston CA, Moreno JP, Gallagher MR, et al. Achieving long-term weight maintenance in Mexican-American adolescents with a school-based intervention. J Adolesc Health. 2013;53(3):335–341. doi: 10.1016/j.jadohealth.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 37.Marsh HW, Hau K-T, Sung R, Yu C-W. Childhood obesity, gender, actual-ideal body image discrepancies, and physical self-concept in Hong Kong children: cultural differences in the value of moderation. Dev Psychol. 2007;43(3):647. doi: 10.1037/0012-1649.43.3.647. [DOI] [PubMed] [Google Scholar]
- 38.Kubik MY, Story M, Davey C. Obesity prevention in schools: current role and future practice of school nurses. Prev Med. 2007;44(6):504–507. doi: 10.1016/j.ypmed.2007.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Moyers P, Bugle L, Jackson E. Perceptions of school nurses regarding obesity in school-age children. J Sch Nurs. 2005;21(2):86–93. doi: 10.1177/10598405050210020501. [DOI] [PubMed] [Google Scholar]
- 40.Robert Wood Johnson Foundation. School Nurse Shortage May Imperil Some Children, RWJF Scholars Warn. 2013. [Google Scholar]
- 41.Gordon SC, Barry CD. Delegation guided by school nursing values: comprehensive knowledge, trust, and empowerment. J Sch Nurs. 2009;25(5):352–360. doi: 10.1177/1059840509337724. [DOI] [PubMed] [Google Scholar]
- 42.Rutter H. Where next for obesity? Lancet. 2011;378(9793):746–747. doi: 10.1016/S0140-6736(11)61272-5. [DOI] [PubMed] [Google Scholar]
- 43.Booth KM, Pinkston MM, Poston WSC. Obesity and the built environment. J Am Diet Assoc. 2005;105(5 Suppl):S110–S117. doi: 10.1016/j.jada.2005.02.045. [DOI] [PubMed] [Google Scholar]
- 44.Lobstein T, Baur L, Uauy R. Obesity in children and young people: a crisis in public health. Obes Rev, Supplement. 2004;5(1):4–104. doi: 10.1111/j.1467-789X.2004.00133.x. [DOI] [PubMed] [Google Scholar]
- 45.Lake A, Townshend T. Obesogenic environments: exploring the built and food environments. J R Soc Promot Health. 2006;126(6):262–267. doi: 10.1177/1466424006070487. [DOI] [PubMed] [Google Scholar]
- 46.Harris JL, Schwartz MB, Munsell CR, et al. Fast food FACTS 2013: Measuring progress in nutrition and marketing to children and teens. New Haven, CT: Yale Rudd Center for Food Policy and Obesity; 2013. [Google Scholar]
- 47.Vandegrift D, Yoked T. Obesity rates, income, and suburban sprawl: an analysis of US states. Health Place. 2004;10(3):221–229. doi: 10.1016/j.healthplace.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 48.Pourshahidi LK, Kerr MA, McCaffrey TA, Livingstone MBE. Influencing and modifying children’s energy intake: the role of portion size and energy density. Proc Nutr Soc. 2014;73(3):397–406. doi: 10.1017/S0029665114000615. [DOI] [PubMed] [Google Scholar]
- 49.Block JP, Roberto CA. Potential benefits of calorie labeling in restaurants. JAMA. 2014;312(9):887–888. doi: 10.1001/jama.2014.9239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.National Association of School Nurses. [Accessed September 24, 2015];Research priorities for school nurses. Available at: http://www.nasn.org/Research/ResearchPrioritiesforSchoolNursing.
- 51.National Association of School Nurses. Overweight and obesity in youth in schools - the role of the school nurse: position statement. NASN School Nurse. 2014;29(3):152–153. doi: 10.1177/1942602X14525569. [DOI] [PubMed] [Google Scholar]