Abstract
IMPORTANCE
Generalized anxiety disorder (GAD) is common in older adults; however, access to treatment may be limited, particularly in rural areas.
OBJECTIVE
To examine the effects of telephone-delivered cognitive behavioral therapy (CBT) compared with telephone-delivered nondirective supportive therapy (NST) in rural older adults with GAD.
DESIGN, SETTING, AND PARTICIPANTS
Randomized clinical trial in the participants’ homes of 141 adults aged 60 years and older with a principal or coprincipal diagnosis of GAD who were recruited between January 27, 2011, and October 22, 2013.
INTERVENTIONS
Telephone-delivered CBT consisted of as many as 11 sessions (9 were required) focused on recognition of anxiety symptoms, relaxation, cognitive restructuring, the use of coping statements, problem solving, worry control, behavioral activation, exposure therapy, and relapse prevention, with optional chapters on sleep and pain. Telephone-delivered NST consisted of 10 sessions focused on providing a supportive atmosphere in which participants could share and discuss their feelings and did not provide any direct suggestions for coping.
MAIN OUTCOMES AND MEASURES
Primary outcomes included interviewer-rated anxiety severity (Hamilton Anxiety Rating Scale) and self-reported worry severity (Penn State Worry Questionnaire–Abbreviated) measured at baseline, 2 months’ follow-up, and 4 months’ follow-up. Mood-specific secondary outcomes included self-reported GAD symptoms (GAD Scale 7 Item) measured at baseline and 4 months’ follow-up and depressive symptoms (Beck Depression Inventory) measured at baseline, 2 months’ follow-up, and 4 months’ follow-up. Among the 141 participants, 70 were randomized to receive CBT and 71 to receive NST.
RESULTS
At 4 months’ follow-up, there was a significantly greater decline in worry severity among participants in the telephone-delivered CBT group (difference in improvement, −4.07; 95%CI, −6.26 to −1.87; P = .004) but no significant differences in general anxiety symptoms (difference in improvement, −1.52; 95%CI, −4.07 to 1.03; P = .24). At 4 months’ follow-up, there was a significantly greater decline in GAD symptoms (difference in improvement, −2.36; 95%CI, −4.00 to −0.72; P = .005) and depressive symptoms (difference in improvement, −3.23; 95%CI, −5.97 to −0.50; P = .02) among participants in the telephone-delivered CBT group.
CONCLUSIONS AND RELEVANCE
In this trial, telephone-delivered CBT was superior to telephone-delivered NST in reducing worry, GAD symptoms, and depressive symptoms in older adults with GAD.
TRIAL REGISTRATION
clinicaltrials.gov Identifier: NCT01259596.
Generalized anxiety disorder (GAD) is characterized by excessive and uncontrollable worry accompanied by restlessness, fatigue, poor concentration, irritability, muscle tension, and/or sleep disturbance.1 Generalized anxiety disorder is one of the most common anxiety disorders in older adults.2 It is associated with poor quality of life,3 increased health care utilization,3 impaired memory,4 and potentially increased morbidity and mortality.5–7
Medications and psychotherapy are the primary treatments for GAD. Cognitive behavioral therapy (CBT) has been found to be superior to minimal contact or usual care for late-life GAD.8–11 Although pharmacological treatments have demonstrated some success in treating GAD,12,13 they are associated with some potentially serious adverse effects for older adults14,15 and alternatives to pharmacotherapy are needed. Further, many older adults prefer psychotherapy to pharmacotherapy for the treatment of anxiety.16
There are a number of barriers that older adults face, particularly those who live in rural areas. Mobility and transportation limitations can make travel to a professional’s office difficult.17 Older adults are also less likely to receive psychotherapy if they live in a county without a mental health professional,18 which is more of a problem for rural residents. Further, professionals specializing in late-life mental health disorders are even less common in rural areas. Thus, alternate methods of providing treatment may increase mental health care utilization by this underserved population.
In the current study, we adapted CBT for administration by telephone in an effort to overcome barriers to care while still providing an evidence-based treatment. We compared telephone-delivered CBT (CBT-T) with telephone-delivered non-directive supportive therapy (NST-T), a structurally equivalent comparison group19 with similar levels of outcome expectations and credibility.20,21 Thus, this design allowed for a comparison between the gold standard for anxiety disorders and a commonly available type of psychotherapy in clinical practice. We compared the effects of CBT-T and NST-T on anxiety, worry, GAD symptoms, and depressive symptoms at 4 months’ postrandomization. We hypothesized that participants who received CBT-T would demonstrate greater declines in symptoms than participants who received NST-T.
Methods
Participants were adults aged 60 years and older with a principal/coprincipal diagnosis of GAD based on the Structured Clinical Interview for DSM-IV22 and lived in 1 of 41 rural counties in North Carolina with an urban population of less than 20 000 people. Exclusion criteria included current psychotherapy, active alcohol/substance abuse, dementia, or global cognitive impairment based on the Telephone Interview for Cognitive Status–Modified23; psychotic symptoms, active suicidal ideation with plan and intent, change in psychotropic medications in the last month, bipolar disorder, and hearing loss that would prevent a person from participating in telephone sessions. This study was approved by the Wake Forest School of Medicine Institutional Review Board. Participants provided verbal informed consent to be screened and written informed consent to undergo the diagnostic interview. The full study protocol can be found in the trial protocol in Supplement 1.
Procedure
The procedures of this study have already been described in detail.24 A commercial mailing company was used to mail study flyers to older adults living in rural counties. Interested participants called and completed a brief screener. Then, they completed a diagnostic interview by telephone and were mailed self-reporting measures. Eligible participants were randomized to 1 of 2 treatments and 1 of 3 therapists. Randomization was stratified on baseline depression diagnosis (lifetime major depression/dysthymia vs no depression) and psychotropic medication use (yes/no) and was administered via a secure web-based data management system using a permuted block algorithm and random block lengths. Randomization procedures were performed by staff who were not involved in the assessments.
Assessment
All study assessments were completed either by telephone or mail. The baseline assessment consisted of self-reported demographic information (age, sex, race/ethnicity, marital status, education, income, employment status, and living status), health-related information (comorbidities, medications, and smoking status), and primary and secondary outcomes. Race/ethnicity data were collected for future moderator analyses. With the exception of the health-related information provided during the diagnostic interview, this information was completed via self-reported measures. A brief follow-up assessment was conducted 2 months after randomization. At 4 months after randomization, all measures except demographic characteristics were reassessed. The primary hypotheses of this study were based on 4 months’ postrandomization data. Type I error was allocated at 0.025 for each outcome so that if either end point was significant, the trial would be considered to have positive results. Only anxiety and mood-related outcomes are presented. Interviewers were masked to participants’ treatment groups.
Primary Outcomes
Anxiety symptoms were assessed with the Structured Interview Guide for the Hamilton Anxiety Rating Scale (HAMA),25,26 a 14-item interviewer-rated measure of general anxiety. Ratings were made on a 5-point scale, ranging from 0 (none) to 4 (very severe). The HAMA has been validated in samples of older adults with GAD and demonstrates good interrater reliability (r = 0.81–0.85).11,27,28 A total of 10% of HAMA interviews were randomly selected and rated by an assessor masked to condition and otherwise not involved with the study (intraclass correlation coefficient = 0.95).
Worry was assessed with the Penn State Worry Questionnaire–Abbreviated (PSWQ-A),29,30 an 8-item self-reported measure of the frequency and intensity of worry. Participants rated each item on a 5-point scale and responses were summed, with higher scores indicating greater worry. The PSWQ-A has better test-retest reliability and comparable validity as the full-length version.29,31 The internal consistency of the PSWQ-A in our previous study was 0.86.32
Secondary Outcomes
The GAD Scale 7 Item33 is a self-reported measure of DSM-IV symptoms of GAD. Participants rated 7 questions on a 4-point Likert scale and responses were summed to create a total score. It has good internal consistency (α = 0.89–0.92) and test-retest reliability (intraclass correlation coefficient = 0.83).33,34
The Beck Depression Inventory (BDI)35 is a 21-item measure of depressive symptoms. Responses were summed, with higher scores indicating greater depressive symptoms. The BDI has good psychometric properties in samples of older adults with GAD.36
Process Measures
The Expectancy Rating Scale37 is a 4-item questionnaire that assesses beliefs in how logical the treatment seems, confidence in undergoing treatment and recommending it to others, and expectations for success. It was administered after the first session.
The Client Satisfaction Questionnaire38 is an 8-item questionnaire that assesses patient satisfaction with treatment. It was administered at the 4-month assessment.
Interventions
Treatment was delivered by 2 graduate-level social workers and 1 postdoctoral clinical psychologist. Therapists delivered both treatments and were masked to assessment data. They received weekly supervision for CBT-T (G.A.B.) and NST-T (S.C.D.). Participants randomized to CBT-T received 9 to 11 weekly 50-minute telephone therapy sessions that corresponded with the CBT workbook. Each workbook chapter39 included CBT techniques that have demonstrated efficacy in treating adults40,41 and older adults with GAD.8,11,42 Chapters addressed recognition of anxiety symptoms, relaxation, cognitive restructuring, the use of coping statements, problem solving, worry control, behavioral activation, exposure therapy, and relapse prevention (with optional chapters on sleep and pain). Participants randomized to NST-T received 10 weekly 50-minute therapy sessions. Telephone-directed nondirective supportive therapy was based on the Borkovec et al protocol20,43 and provided a high-quality therapeutic relationship with a warm, genuine, and accepting atmosphere through the use of supportive and reflective communications; it did not provide advice, suggestions, or coping methods. Participants in both groups received 4 booster sessions at 2, 4, 8, and 12 weeks following completion of the weekly sessions.
Therapist Fidelity
All therapy sessions were audiotaped and 10% (1 session from each participant) were randomly selected to be rated by 2 post-doctoral-level clinicians not affiliated with the study. The sessions were evaluated for therapist adherence to the protocol and competence in delivering the interventions on a 9-point scale used in other late-life GAD psychotherapy studies.8,10 Mean therapist ratings for adherence and competence were higher than 6.0 (good) for both treatments for all therapists, which was the a priori requisite.
Power Considerations
Assuming that each primary outcome would be tested at the 4-month assessment using a .03 2-sided significance level (ie, a Bonferroni correction), power calculations for analysis of covariance on the PSWQ-A outcome indicated the need for a total of 80 participants per treatment to attain 90% power, 70 participants per treatment to provide 85% power, and 60 participants per treatment to attain 78% power.24 We planned to randomize 88 participants per treatment to account for an expected dropout rate of approximately 10%. In October 2013, conditional power calculations based on having 80 evaluable participants per treatment were presented to the data safety monitoring board to illustrate the effect on power of stopping recruitment early. At that time, the total number of participants with 4-month assessment measurements was projected to be 120 and it was determined that further randomization, even to a total of 160 evaluable participants per treatment, would most likely not have an effect on conclusions for the 2 primary outcomes. Thus, randomization was stopped and follow-up continued (see eAppendix 1 in Supplement 2 for details).
Statistical Analyses
All analyses were performed using SAS, version 9.4 (SAS Institute Inc). Baseline characteristics were summarized overall and by treatment using means and percentages. The percentage of therapy sessions attended was calculated for each person, assuming a maximum of 10 sessions per person (ie, some CBT-T participants had an optional 11th session but were only credited with 10 sessions for the computation). The mean percentage of sessions attended was then compared between treatments.
The prespecified analysis plan included all randomized participants as allocated to their original treatment group and used maximum likelihood estimation within a population-averaged repeated-measures analysis of covariance, with an unstructured covariance matrix to account for the fact that the multiple follow-up measurements from participants were not independent (PROC MIXED of SAS was used). This approach is consistent with the principle of intent to treat when at least 1 follow-up measure is obtained prior to dropout.44 The pre-specified time for comparison of the primary outcomes between treatments was the 4-month visit and the hypothesis test and was performed as a linear contrast within the analysis of covariance model using a 2-sided .02 significance level (see eAppendix 1 in Supplement 2 for explanation of significance level based on interim analysis). The analysis of covariance model for the primary outcomes contained terms for the baseline value of the outcome, therapist (a factor to which participants were randomized), lifetime depressive disorder (used to stratify randomization), use of psychotropic medications at baseline (used to stratify randomization), treatment effect, time effect, and time-by-treatment interaction term. Prespecified secondary outcomes included the BDI and GAD-7 and were analyzed using the same approach as specified for the primary outcomes. Nominal significance levels were reported for these 2 secondary outcomes and they were tested at the .05 level. Under independence between these outcomes, the probability of type I error was 0.0975 but less than 0.075 if the outcomes were positively correlated at0.4 or larger.45 There were no prespecified subgroup analyses. Because some participants did not have any follow-up measurements, a full intent-to-treat sensitivity analysis used multiple imputation to explore the effect of missing outcomes on the overall conclusions for each outcome (HAMA, PSWQ-A, GAD-7, and BDI). A description of this analysis and the findings are included in eAppendix 2 in Supplement 2. Lastly, treatment response rates and the proportions without 4-month measurements were compared using the Fisher exact or χ2 tests and a Wilcoxon test was used to compare levels of treatment expectancies and satisfaction between treatments.
Results
Recruitment, Attrition, and Sample Characteristics
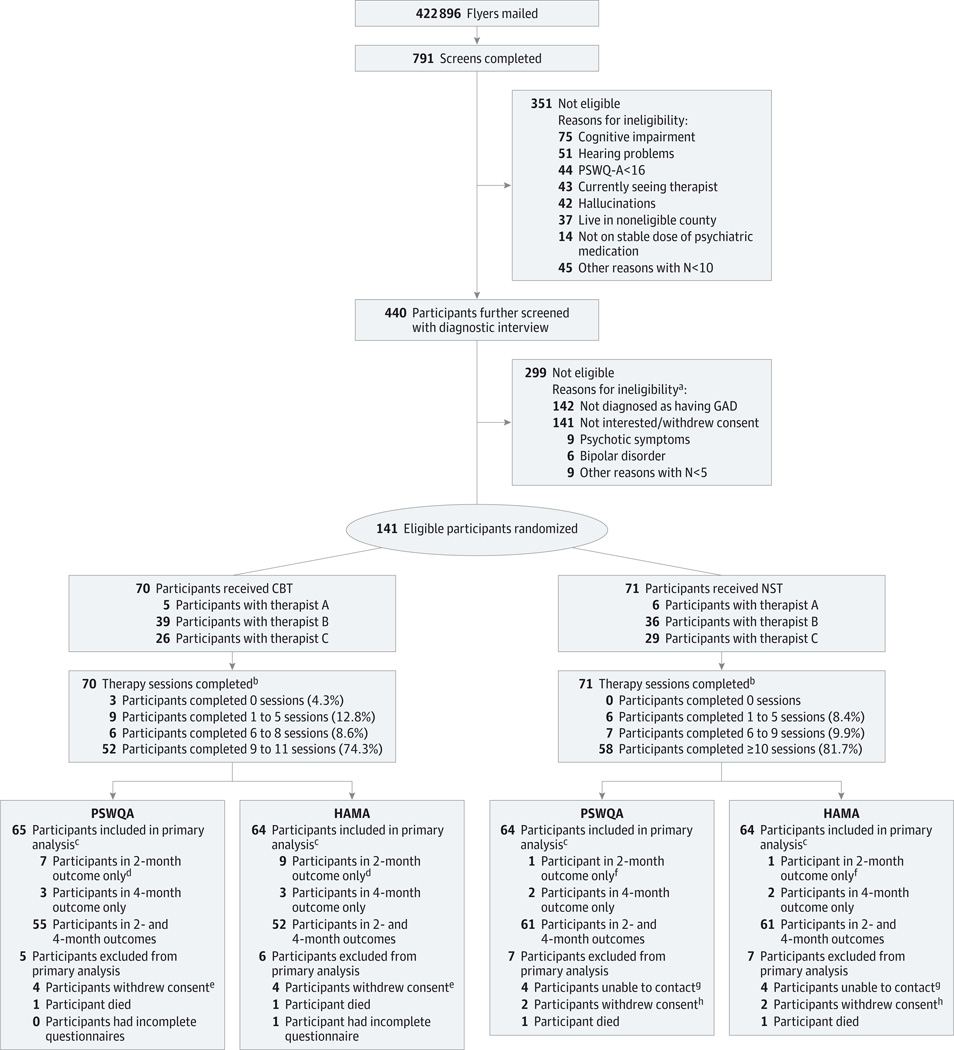
Recruitment occurred between January 27, 2011, and October 22, 2013. The initial recruitment goal was 176 participants; however, recruitment was slower than anticipated. Recruitment was stopped when 141 participants were randomized (CBT-T, n = 70; NST-T, n = 71). Figure 1 displays participant flow from randomization through study follow-up and provides details on dropout rates. Almost 75% of participants in CBT-T (52/70) completed the required 9 sessions and more than 81% (58/71) of participants in NST-T completed the required 10 sessions. Two participants died and 1 participant became seriously ill prior to the first session. Data completion rates for the outcome measures ranged from 85.8% to 89.9% at the 2-month assessment and 79.7% to 90.0% at the 4-month assessment (percentages based on the total number randomized). Fifteen of 70 participants in CBT-T (21.4%) and 8 of 71 participants in NST-T (11.3%) were missing at least 1 of the primary outcomes at the 4-month assessment (P = .12 by Fisher exact test). Ten of 70 participants in CBT-T (14.2%) and 3 of 71 participants in NST-T (4.2%) withdrew consent at some point prior to the 4-month visit (P = .05 by Fisher exact test).
Figure 1.
CONSORT Flow Diagram
a Some participants had multiple reasons for ineligibility.
b Telephone-delivered cognitive behavioral therapy (CBT-T) could be completed with between 9 and 11 sessions. Telephone-delivered nondirective supportive therapy (NST-T) required 10 sessions to be complete.
c Prespecified primary analysis used all participants with any follow-up data at 2 or 4 months’ follow-up. Those excluded from the prespecified primary analysis did not have any follow-up information. Sensitivity analyses using multiple imputation also were performed to include all participants.
d There were 10 total participants missing either the Penn State Worry Questionnaire–Abbreviated (PSWQ-A) or Hamilton Anxiety Rating Scale (HAMA): 2 with the following health problems, 2 indicated they did not have the time, 4 completed the PSWQ-A but not HAMA, and 2 with unknown or other reasons (6 of these participants withdrew consent after providing month 2 data).
e Two participants cited self or family health problems, 1 participant cited that he or she did not like randomized therapy, and 1 participant had an unknown reason.
f One participant cited health problems and withdrew consent after providing 2-months’ follow-up data.
g Two participants cited personal or family health problems and 2 had unknown reasons (2 participants withdrew consent after providing 2-month follow-up data).
h Two participants cited health problems.
The Table presents the demographic and health-related characteristics and baseline outcome values.
Table.
Baseline Characteristics of Randomized Participants
| Characteristic | No. (%) | ||
|---|---|---|---|
| Total (n = 141) |
CBT-T (n = 70) |
NST-T (n = 71) |
|
| Sex | |||
| Male | 26 (18.4) | 12 (17.1) | 14 (19.7) |
| Female | 115 (81.6) | 58 (82.9) | 57 (80.3) |
| Race/ethnicity | |||
| African American | 8 (5.7) | 4 (5.7) | 4 (5.6) |
| White | 128 (90.8) | 64 (91.4) | 64 (90.1) |
| Other | 5 (3.5) | 2 (2.9) | 3 (4.2) |
| Age, y | |||
| 60–64 | 66 (46.8) | 29 (41.4) | 37 (52.1) |
| 65–69 | 38 (27.0) | 20 (28.6) | 18 (25.4) |
| 70–74 | 19 (13.5) | 8 (11.4) | 11 (15.5) |
| ≥75 | 18 (12.8) | 13 (18.6) | 5 (7.0) |
| Education | |||
| Less than high school | 7 (5.0) | 4 (5.7) | 3 (4.2) |
| High school grad or GED | 18 (12.8) | 9 (12.9) | 9 (12.7) |
| Some college | 53 (37.6) | 19 (27.1) | 34 (47.9) |
| College degree | 63 (44.7) | 38 (54.3) | 25 (35.2) |
| Income, $ | |||
| ≤24 999 | 33 (23.4) | 12 (17.1) | 21 (29.6) |
| 25 000–49 999 | 41 (29.1) | 21 (30.0) | 20 (28.2) |
| 50 000–74 999 | 19 (13.5) | 10 (14.3) | 9 (12.7) |
| ≥75 000 | 16 (11.4) | 7 (10.0) | 9 (12.7) |
| Missing | 32 (22.7) | 20 (28.6) | 12 (16.9) |
| Marital status | |||
| Never been married | 1 (0.7) | 1 (1.4) | 0 (0.0) |
| Married or living with someone | 75 (53.2) | 37 (52.9) | 38 (53.5) |
| Divorced | 27 (19.2) | 13 (18.6) | 14 (19.7) |
| Separated | 9 (6.4) | 4 (5.7) | 5 (7.0) |
| Widowed | 29 (20.6) | 15 (21.4) | 14 (19.7) |
| Currently employed | 38 (27.0) | 17 (24.3) | 21 (29.6) |
| Living status | |||
| With others | 87 (61.7) | 41 (58.6) | 46 (64.8) |
| Alone | 54 (38.3) | 29 (41.4) | 25 (35.2) |
| Smoking status | |||
| Never | 68 (48.2) | 37 (52.9) | 31 (43.7) |
| Current | 14 (9.9) | 6 (8.6) | 8 (11.3) |
| Former | 59 (41.8) | 27 (38.6) | 32 (45.1) |
| Current psychotropic medication usage | |||
| Anxiolytics | 38 (27.0) | 22 (31.4) | 16 (22.5) |
| Hypnotics | 12 (8.5) | 5 (7.1) | 7 (9.9) |
| Antidepressants | 54 (38.3) | 29 (41.4) | 25 (35.2) |
| Antipsychotics/neuroleptics | 3 (2.1) | 1 (1.4) | 2 (2.8) |
| Stimulants | 1 (0.7) | 0 (0.0) | 1 (1.4) |
| History of self-reported health problems | |||
| Hypertension | 92 (65.7) | 43 (62.3) | 49 (69.0) |
| Myocardial infarction | 9 (6.4) | 4 (5.8) | 5 (7.0) |
| Congestive heart failure | 8 (5.7) | 4 (5.7) | 4 (5.6) |
| Stroke | 11 (7.9) | 5 (7.2) | 6 (8.5) |
| Diabetes mellitus | 29 (20.6) | 9 (12.9) | 20 (28.2) |
| Score, mean (SD) | |||
| TICS-m | 36.9 (4.6) | 36.7 (4.5) | 37.2 (4.6) |
| PSWQA | 31.0 (5.57) | 30.6 (5.53) | 31.4 (5.62) |
| HAMA | 21.0 (7.70) | 20.1 (7.14) | 21.9 (8.18) |
| BDI | 23.0 (9.08) | 21.6 (8.84) | 24.4 (9.18) |
| GAD-7 | 11.7 (4.29) | 11.1 (4.25) | 12.3 (4.28) |
| Presence of comorbid depression diagnosis | |||
| Total | 102 (72.3) | 51 (72.9) | 51 (71.8) |
| Current | 54 (38.3) | 23 (32.9) | 31 (43.7) |
| Past | 48 (34.0) | 28 (40.0) | 20 (28.2) |
| Presence of comorbid anxiety diagnosis | 72 (51.1) | 31 (44.3) | 41 (57.8) |
Abbreviations: BDI, Beck Depression Inventory; CBT-T, telephone-delivered cognitive behavioral therapy; GAD, generalized anxiety disorder; GAD-7, Generalized Anxiety Disorder Scale 7 Item; GED, general educational development test; HAMA, Hamilton Anxiety Rating Scale; NST-T, telephone-delivered nondirective supportive therapy; PSWQ-A, Penn State Worry Questionnaire–Abbreviated; TICS-m, Telephone Interview for Cognitive Status–Modified.
Primary Outcomes
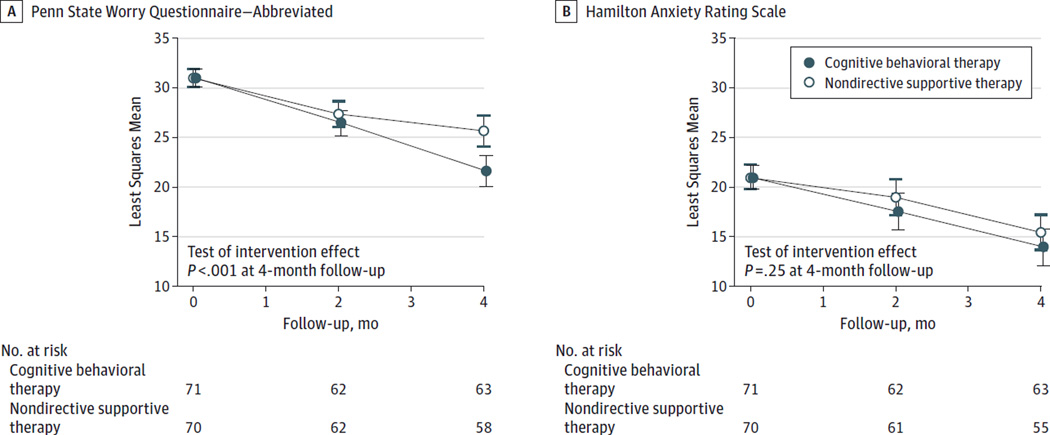
Figure 2 displays the results for the primary outcomes. There was a significant decline in anxiety symptoms (HAMA) among participants in both treatments (CBT-T: −7.04; 95% CI, −8.88 to −5.21; NST-T: −5.53; 95% CI, −7.28 to −3.77) but there was no significant effect of treatment on general anxiety symptoms (difference in improvement, −1.52; 95%CI, −4.07 to 1.03; P = .24). Similarly, there was a significant decline in worry (PSWQ-A) among participants in both treatments (CBT-T: −9.44; 95%CI, −11.02 to −7.86; NST-T: −5.37; 95%CI, −6.89 to −3.85). However, there was a significantly greater decline in worry among participants in CBT-T (difference in improvement, −4.07; 95%CI, −6.26 to −1.87; P = .004).
Figure 2.
Treatment Effects on Primary Outcomes
Secondary Outcomes
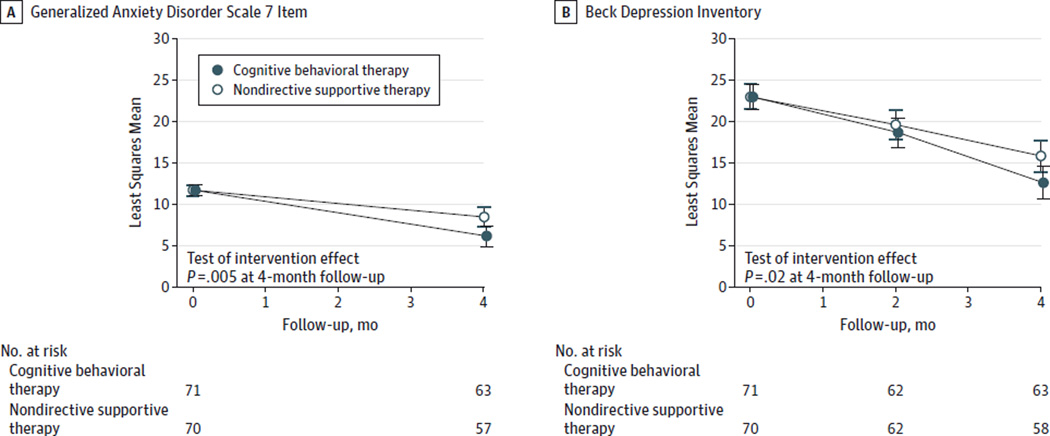
Figure 3 displays the results for the secondary outcomes. There was a significant decline in self-reported GAD symptoms (GAD-7) among participants in both treatments (CBT-T: −5.63; 95%CI, −6.82 to −4.44; NST-T: −3.27; 95%CI, −4.40 to −2.14), with a significantly greater decline among participants in CBT-T (difference in improvement, −2.36; 95% CI, −4.00 to −0.72; P = .005). Similarly, depressive symptoms (BDI) declined among all participants (CBT-T: −10.77; 95%CI, −12.73 to −8.81; NST-T: −7.54; 95% CI, −9.44 to −5.64). Similar to GAD symptoms, there was a significantly greater decline in depressive symptoms among participants in CBT-T (difference in improvement, −3.23; 95% CI, −5.97 to −0.50; P = .02).
Figure 3.
Treatment Effects on Secondary Outcomes
Treatment Response Rates
A meaningful response to treatment has been defined as a 5.5-point decrease in PSWQ-A scores from baseline to posttreatment.10,46,47 A significantly greater proportion of participants in CBT-T experienced a reduction in PSWQ-A scores by at least 5.5 points (72.4%) compared with participants in NST-T (42.9%; P = .001).
Treatment Expectancies and Satisfaction With Treatment
There were no significant differences between the means (SD) of treatments with respect to their expectations of the treatment (CBT-T, 29.6 [7.51]; NST-T, 29.4 [7.45]; P = .09). However, mean (SD) satisfaction was significantly higher among participants in CBT-T (27.9 [4.48]) compared with participants in NST-T (25.2 [5.86]; P = .01).
Assessment of Safety
A total of 8 participants (4 in each condition) experienced a greater than 1 SD increase in PSWQ-A scores (3 at the 2-month assessment and 1 at the 4-month assessment) or in BDI scores (2 at the 2-month assessment, 1 at the 4-month assessment, and 1 at both the 2-month and 4-month assessments). These participants were assessed for immediate need for psychiatric treatment. Referrals for additional therapy or medication management were provided if needed.
Discussion
We found that both treatments reduced symptoms of worry, depression, and GAD. However, CBT-T was superior to NST-T, resulting in a significantly greater reduction in these symptoms. To our knowledge, this is the first study of a telephone-delivered intervention for the treatment of late-life GAD as well as the largest head-to-head comparison of individual CBT with an active psychotherapy comparator.
Telephone-delivered psychotherapy is 1 way to overcome some barriers to mental health treatment that rural older adults face. Although we did not compare telephone-delivered psychotherapy with face-to-face treatment, research suggests that telephone-delivered treatment may be equally efficacious and yield lower attrition rates.48 The effect of telephone-delivered CBT on worry in the current study (prepost change/baseline SD, 1.37) is comparable with those found in other studies of late-life GAD in which CBT was delivered in a face-to-face format.8,11,42,49,50 Further, our findings suggest that telephone-delivered psychotherapy is well liked. First, scores on the satisfaction measure were high. Second, adherence was high in this study; more than 75% of the sample completed at least 9 sessions. Third, attrition was lower in the current study (11.3%) than comparable studies of psychotherapy for late-life GAD (attrition rates for similar studies range from 13.5% to 33%).10,42
Few studies have focused specifically on psychotherapy for treating late-life GAD and only 1 study42 has compared CBT with another type of active psychotherapy. This randomized design allowed for a rigorous test of CBT, controlling for common therapeutic elements across psychotherapies. Stanley and colleagues42 compared CBT with supportive therapy delivered in a group format (N = 48) and found no significant differences between the 2 treatments. Potential explanations for the difference include sample size (only 31 participants completed their treatment) and the CBT intervention (theirs consisted of the following 3 components: relaxation, cognitive therapy, and exposure while the current treatment included 8 to 10 different topics). Although we found that both treatments improved symptoms, CBT-T was significantly better than NST-T at reducing worry, GAD, and depressive symptoms.
There were a number of strengths of this study, including a rigorous test of CBT by comparing it with an active treatment in a randomized clinical trial, adaptation of treatment to meet the needs of a rural population, high treatment adherence and integrity, and low attrition rates. To address any potential effect of depression on treatment, randomization was stratified by the presence of major depression or dysthymia. Notably, CBT-T demonstrated superiority in treating comorbid depression symptoms. Similarly, the use of psychotropic medications, another possible confounding variable, was also used as a stratification variable. Nonetheless, there were some limitations. Although scores on the HAMA declined, there were no significant differences between the 2 conditions. One possibility may be owing to poor reliability of this interviewer-rated measure. However, 10% of HAMA interviews were randomly selected and rated by a masked reviewer. The intraclass correlation coefficient was 0.95, suggesting that interviewer variance was not responsible for the lack of difference. An alternative explanation is that while it is superior at reducing the worry symptoms specific to GAD, CBT-T is less effective for somatic symptoms of anxiety. Further, biased responding by participants on self-reported measures cannot be ruled out; however, there was no reason to believe it would be differential among randomized groups. Another limitation was the largely white well-educated sample that potentially limited generalizability of the findings, particularly to those with lower educational or literacy levels. Finally, a decrease in symptoms from baseline to follow-up may have reflected regression to the mean.
Conclusions
Among rural older adults diagnosed as having GAD, both CBT-T and NST-T are associated with reductions in anxiety, worry, GAD, and depressive symptoms. However, CBT-T was superior to NST-T in reducing worry, GAD, and depressive symptoms. There was no differential effect of treatment on anxiety symptoms.
Supplementary Material
Acknowledgments
Funding/Support: This work was funded by grant R01 MH083664 from the National Institute of Mental Health (Dr Brenes).
Role of the Funder/Sponsor: The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Additional Contributions: We thank Elizabeth Arnold, PhD, Wake Forest School of Medicine, and Melinda A. Stanley, PhD, Baylor College of Medicine, for providing treatment adherence and integrity ratings for the therapy sessions. We also thank those who served on the data safety monitoring board, including Patricia Arean, PhD, University of California at San Francisco School of Medicine, John Preisser, PhD, University of North Carolina Gillings School of Global Public Health, and Julie Wetherell, PhD, University of California at San Diego School of Medicine, chair. All contributors received compensation for their work.
Footnotes
Author Contributions: Dr Brenes had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Brenes, Miller.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Brenes, Danhauer, Lyles, Miller.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Brenes, Hogan, Miller.
Obtained funding: Brenes, Miller.
Administrative, technical, or material support: Brenes, Danhauer, Lyles, Miller.
Study supervision: Brenes, Danhauer, Miller.
Conflict of Interest Disclosures: None reported.
Disclaimer: The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute of Mental Health.
REFERENCES
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 2.Lenze EJ, Wetherell JL. A lifespan view of anxiety disorders. Dialogues Clin Neurosci. 2011;13(4):381–399. doi: 10.31887/DCNS.2011.13.4/elenze. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Porensky EK, Dew MA, Karp JF, et al. The burden of late-life generalized anxiety disorder: effects on disability, health-related quality of life, and healthcare utilization. Am J Geriatr Psychiatry. 2009;17(6):473–482. doi: 10.1097/jgp.0b013e31819b87b2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mantella RC, Butters MA, Dew MA, et al. Cognitive impairment in late-life generalized anxiety disorder. Am J Geriatr Psychiatry. 2007;15(8):673–679. doi: 10.1097/JGP.0b013e31803111f2. [DOI] [PubMed] [Google Scholar]
- 5.Carrière I, Ryan J, Norton J, et al. Anxiety and mortality risk in community-dwelling elderly people. Br J Psychiatry. 2013;203(3):303–309. doi: 10.1192/bjp.bp.112.124685. [DOI] [PubMed] [Google Scholar]
- 6.Martens EJ, de Jonge P, Na B, Cohen BE, Lett H, Whooley MA. Scared to death? generalized anxiety disorder and cardiovascular events in patients with stable coronary heart disease: the Heart and Soul Study. Arch Gen Psychiatry. 2010;67(7):750–758. doi: 10.1001/archgenpsychiatry.2010.74. [DOI] [PubMed] [Google Scholar]
- 7.Phillips AC, Batty GD, Gale CR, et al. Generalized anxiety disorder, major depressive disorder, and their comorbidity as predictors of all-cause and cardiovascular mortality: the Vietnam Experience Study. Psychosom Med. 2009;71(4):395–403. doi: 10.1097/PSY.0b013e31819e6706. [DOI] [PubMed] [Google Scholar]
- 8.Stanley MA, Beck JG, Novy DM, et al. Cognitive-behavioral treatment of late-life generalized anxiety disorder. J Consult Clin Psychol. 2003;71(2):309–319. doi: 10.1037/0022-006x.71.2.309. [DOI] [PubMed] [Google Scholar]
- 9.Stanley MA, Wilson NL, Amspoker AB, et al. Lay providers can deliver effective cognitive behavior therapy for older adults with generalized anxiety disorder: a randomized trial. Depress Anxiety. 2014;31(5):391–401. doi: 10.1002/da.22239. [DOI] [PubMed] [Google Scholar]
- 10.Stanley MA, Wilson NL, Novy DM, et al. Cognitive behavior therapy for generalized anxiety disorder among older adults in primary care: a randomized clinical trial. JAMA. 2009;301(14):1460–1467. doi: 10.1001/jama.2009.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wetherell JL, Gatz M, Craske MG. Treatment of generalized anxiety disorder in older adults. J Consult Clin Psychol. 2003;71(1):31–40. doi: 10.1037//0022-006x.71.1.31. [DOI] [PubMed] [Google Scholar]
- 12.Lenze EJ, Mulsant BH, Shear MK, et al. Efficacy and tolerability of citalopram in the treatment of late-life anxiety disorders: results from an 8-week randomized, placebo-controlled trial. Am J Psychiatry. 2005;162(1):146–150. doi: 10.1176/appi.ajp.162.1.146. [DOI] [PubMed] [Google Scholar]
- 13.Lenze EJ, Rollman BL, Shear MK, et al. Escitalopram for older adults with generalized anxiety disorder: a randomized controlled trial. JAMA. 2009;301(3):295–303. doi: 10.1001/jama.2008.977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Strien AM, Koek HL, van Marum RJ, Emmelot-Vonk MH. Psychotropic medications, including short acting benzodiazepines, strongly increase the frequency of falls in elderly. Maturitas. 2013;74(4):357–362. doi: 10.1016/j.maturitas.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 15.de Vries OJ, Peeters G, Elders P, et al. The elimination half-life of benzodiazepines and fall risk: two prospective observational studies. Age Ageing. 2013;42(6):764–770. doi: 10.1093/ageing/aft089. [DOI] [PubMed] [Google Scholar]
- 16.Mohlman J. A community based survey of older adults’ preferences for treatment of anxiety. Psychol Aging. 2012;27(4):1182–1190. doi: 10.1037/a0023126. [DOI] [PubMed] [Google Scholar]
- 17.Pepin R, Segal DL, Coolidge FL. Intrinsic and extrinsic barriers to mental health care among community-dwelling younger and older adults. Aging Ment Health. 2009;13(5):769–777. doi: 10.1080/13607860902918231. [DOI] [PubMed] [Google Scholar]
- 18.Wei W, Sambamoorthi U, Olfson M, Walkup JT, Crystal S. Use of psychotherapy for depression in older adults. Am J Psychiatry. 2005;162(4):711–717. doi: 10.1176/appi.ajp.162.4.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baskin TW, Tierney SC, Minami T, Wampold BE. Establishing specificity in psychotherapy: a meta-analysis of structural equivalence of placebo controls. J Consult Clin Psychol. 2003;71(6):973–979. doi: 10.1037/0022-006X.71.6.973. [DOI] [PubMed] [Google Scholar]
- 20.Borkovec TD, Costello E. Efficacy of applied relaxation and cognitive-behavioral therapy in the treatment of generalized anxiety disorder. J Consult Clin Psychol. 1993;61(4):611–619. doi: 10.1037//0022-006x.61.4.611. [DOI] [PubMed] [Google Scholar]
- 21.Craske MG, Maidenberg E, Bystritsky A. Brief cognitive-behavioral versus nondirective therapy for panic disorder. J Behav Ther Exp Psychiatry. 1995;26(2):113–120. doi: 10.1016/0005-7916(95)00003-i. [DOI] [PubMed] [Google Scholar]
- 22.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview DSM-IV-TR Axis I Disorders-Patient Edition (SCID-I/P) New York: Biometrics Department, New York State Psychiatric Institute; 2002. [Google Scholar]
- 23.Welsh KA, Breitner JCS, Magruder-Habib KM. Detection of dementia in elderly using telephone screening of cognitive status. Neuropsychiatry Neuropsychol Behav Neurol. 1993;6(2):103–110. [Google Scholar]
- 24.Brenes GA, Danhauer SC, Lyles MF, Miller ME. Telephone-delivered psychotherapy for rural-dwelling older adults with generalized anxiety disorder: study protocol of a randomized controlled trial. BMC Psychiatry. 2014;14:34. doi: 10.1186/1471-244X-14-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32(1):50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 26.Shear MK, Vander Bilt J, Rucci P, et al. Reliability and validity of a structured interview guide for the Hamilton Anxiety Rating Scale (SIGH-A) Depress Anxiety. 2001;13(4):166–178. [PubMed] [Google Scholar]
- 27.Barrowclough C, King P, Colville J, Russell E, Burns A, Tarrier N. A randomized trial of the effectiveness of cognitive-behavioral therapy and supportive counseling for anxiety symptoms in older adults. J Consult Clin Psychol. 2001;69(5):756–762. doi: 10.1037//0022-006x.69.5.756. [DOI] [PubMed] [Google Scholar]
- 28.Stanley MA, Beck JG, Zebb BJ. Psychometric properties of four anxiety measures in older adults. Behav Res Ther. 1996;34(10):827–838. doi: 10.1016/0005-7967(96)00064-2. [DOI] [PubMed] [Google Scholar]
- 29.Hopko DR, Stanley MA, Reas DL, et al. Assessing worry in older adults: confirmatory factor analysis of the Penn State Worry Questionnaire and psychometric properties of an abbreviated model. Psychol Assess. 2003;15(2):173–183. doi: 10.1037/1040-3590.15.2.173. [DOI] [PubMed] [Google Scholar]
- 30.Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behav Res Ther. 1990;28(6):487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- 31.Crittendon J, Hopko DR. Assessing worry in older and younger adults: psychometric properties of an abbreviated Penn State Worry Questionnaire (PSWQ-A) J Anxiety Disord. 2006;20(8):1036–1054. doi: 10.1016/j.janxdis.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 32.Brenes GA, Miller ME, Williamson JD, McCall WV, Knudson M, Stanley MA. A randomized controlled trial of telephone-delivered cognitive-behavioral therapy for late-life anxiety disorders. Am J Geriatr Psychiatry. 2012;20(8):707–716. doi: 10.1097/JGP.0b013e31822ccd3e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 34.Löwe B, Decker O, Müller S, et al. validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care. 2008;46(3):266–274. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- 35.Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive Therapy of Depression. New York, NY: Guilford Press; 1979. [Google Scholar]
- 36.Beck JG, Stanley MA, Zebb BJ. Characteristics of generalized anxiety disorder in older adults: a descriptive study. Behav Res Ther. 1996;34(3):225–234. doi: 10.1016/0005-7967(95)00064-x. [DOI] [PubMed] [Google Scholar]
- 37.Borkovec TD, Nau SD. Credibility of analogue therapy rationales. J Behav Ther Exp Psychiatry. 1972;3(4):257–260. [Google Scholar]
- 38.Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. Assessment of client/patient satisfaction: development of a general scale. Eval Program Plann. 1979;2(3):197–207. doi: 10.1016/0149-7189(79)90094-6. [DOI] [PubMed] [Google Scholar]
- 39.Wetherell JL, Sorrell JT, Thorp SR, Patterson TL. Psychological interventions for late-life anxiety: a review and early lessons from the CALM study. J Geriatr Psychiatry Neurol. 2005;18(2):72–82. doi: 10.1177/0891988705276058. [DOI] [PubMed] [Google Scholar]
- 40.Borkovec TD, Whisman MA. Psychological treatment for Generalized Anxiety Disorder. In: Mavissakalian M, Prien R, editors. Long-Term Treatment of Anxiety Disorders. Washington, DC: American Psychiatric Press; 1996. [Google Scholar]
- 41.Gould RA, Otto MW, Pollack MH, Yap L. Cognitive behavioral and pharmacological treatment of generalized anxiety disorder: a preliminary meta-analysis. Behav Ther. 1997;28(2):285–305. [Google Scholar]
- 42.Stanley MA, Beck JG, Glassco JD. Treatment of generalized anxiety in older adults: a preliminary comparison of cognitive-behavioral and supportive approaches. Behav Ther. 1996;27(4):565–581. [Google Scholar]
- 43.Borkovec TD, Newman MG, Pincus AL, Lytle R. A component analysis of cognitive-behavioral therapy for generalized anxiety disorder and the role of interpersonal problems. J Consult Clin Psychol. 2002;70(2):288–298. [PubMed] [Google Scholar]
- 44.Molenberghs G, Kenward MG. Missing Data in Clinical Studies. West Sussex, England: John Wiley & Sons, Ltd; 2007. [Google Scholar]
- 45.Moyé LA. Multiple Analyses in Clinical Trials: Fundamentals for Investigators. New York, NY: Springer-Verlag; 2010. [Google Scholar]
- 46.Roseman AS, Cully JA, Kunik ME, et al. Treatment response for late-life generalized anxiety disorder: moving beyond symptom-based measures. J Nerv Ment Dis. 2011;199(10):811–814. doi: 10.1097/NMD.0b013e31822feda6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Barrera TL, Cully JA, Amspoker A, et al. Cognitive-behavioral therapy for late-life anxiety: a randomized controlled trial with veteran and community participants. J Anxiety Disord. 2015;33:72–80. doi: 10.1016/j.janxdis.2015.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mohr DC, Ho J, Duffecy J, et al. Effect of telephone-administered vs face-to-face cognitive behavioral therapy on adherence to therapy and depression outcomes among primary care patients: a randomized trial. JAMA. 2012;307(21):2278–2285. doi: 10.1001/jama.2012.5588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stanley MA, Hopko DR, Diefenbach GJ, Bourland SL, Rodriguez H, Wagener P. Cognitive-behavior therapy for late-life generalized anxiety disorder in primary care: preliminary findings. Am J Geriatr Psychiatry. 2003;11(1):92–96. [PubMed] [Google Scholar]
- 50.Wetherell JL, Ayers CR, Sorrell JT, et al. Modular psychotherapy for anxiety in older primary care patients. Am J Geriatr Psychiatry. 2009;17(6):483–492. doi: 10.1097/JGP.0b013e3181a31fb5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.