Abstract
Granulomatous response in association with breast cancer and within the cancer draining lymph nodes is an extremely rare phenomenon. Granulomatous inflammation is an immune response commonly seen against infectious agents and certain non-neoplastic conditions. The etiopathogenesis of granulomas associated with malignancies is not clear but it may be because of an immunologic reaction to tumour antigens. We hereby report a 50-yr-old postmenopausal female presented to Surgical Outpatient Department, Aligarh Muslim University, India, with complaints of lump and pain in her left breast for 6 months. We have also discussed about its etiopathogenesis, final diagnosis, treatment & patient outcome.
Key Words: Granulomatous response, Breast cancer, India
Introduction
A granuloma is an immune mechanism seen commonly against I) Infections like Mycobacteria, certain fungi and parasites; II) Certain non-neoplastic conditions like Sarcoidosis, foreign bodies, wegener’s granulomatosis, Crohn’s disease and III) Certain malignancies like Hodgkin’s disease and non-Hodgkin T cell lymphomas, seminoma of the testis, renal cell carcinoma, nasopharyngeal carcinoma and ovarian dysgerminoma (1, 2). “Sarcoid like granulomas occur in 4.4% of carcinomas, 13.8% of patients with Hodgkin disease, 7.3% of cases with non-Hodgkin lymphoma, 50% of seminomas and 0.4% of sarcomas” (3). It has also been reported very rarely in breast, gastric, colonic and laryngeal malignancy (4, 5). Gorton and Linell were the first to report sarcoid like granulomas in lymphnodes draining carcinomas (6). Oberman reported three cases of breast carcinoma in which there were epithelioid granulomas adjacent to the invasive breast cancer, but axillary lymphnodes were not involved in any of the cases (7).
Granulomatous response in breast cancer is thought to be due to immunologic response to tumour antigens as these granulomas have tumor cells in the centre (8, 9). Various reasons have been given for the granulomatous response in cancer draining lymph nodes like foreign body reaction to the tumor or metastasis or it may also be due to systemic illnesses like sarcoidosis or tuberculosis (9). In developing countries like India where the incidence of tuberculosis is high, it is difficult to distinguish between a coexistent tubercular infection and a non-specific granulomatous response.
Owing to the rarity of presentation of granulomas at the site of carcinoma as well as in the draining lymphnodes this case is being reported here.
Case report:
A 50 yr old postmenopausal female presented to Surgical Outpatient Department, Aligarh Muslim University, India, with complaints of lump and pain in her left breast for 6 months. She had 3 children with history of adequate breast feeding in all. There was no history of any similar complaints in the family, trauma to the breast or hormonal therapy. An informed consent was taken from the patient.
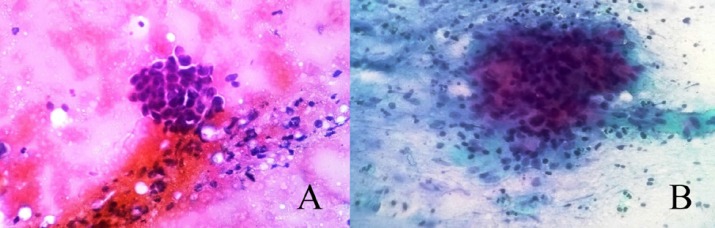
On examination, right breast was normal, left breast had a 4X4 cm, hard lump, fixed to the breast tissue in the upper outer quadrant. Multiple, mobile, enlarged lymph nodes in the central group were present in the ipsilateral axilla. The patient was investigated and her ESR was raised to 46 mm in the first hour. Mammography showed a small opacity with few micro calcifications in the upper outer quadrant of left breast suggestive of breast carcinoma. Fine needle aspiration cytology (FNAC) showed clusters of malignant duct epithelial cells having raised nuclear-cytoplasmic ratio, pleomorphic nuclei with clumped chromatin and prominent nucleoli. Apart from this many epithelioid cell granulomas were also seen (Fig. 1 ). FNAC from axillary lymph nodes was suggestive of reactive lymphadenitis.
Fig. 1.
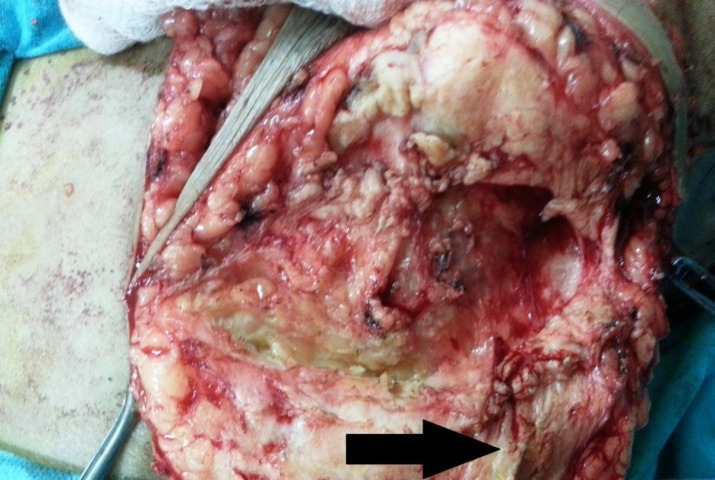
Peroperative image showing hard fibrous tissue around the tumor mass [arrow]
Because of prevalence of tuberculosis in low socioeconomic groups in India, a diagnosis of breast carcinoma with tubercular mastitis was made on cytology. Mantoux test was done by injecting 0.1 ml (10 I.U.) of purified protein derivative (PPD) intradermally which was also positive. However, chest X-Ray was normal. Owing to high suspicion, antitubercular treatment (ATT) was started and patient was planned for modified radical mastectomy (MRM). Per-operatively there was hard fibrous tissue present in the left breast separately around the tumor mass (Fig. 2).
Fig. 2.
A: FNAC smear from the breast showing cluster of malignant ductal epithelial cells having raised nucleocytoplasmic ratio, clumped chromatin and prominent nucleoli (hematoxylin & eosin 400X). B:FNAC smear from the breast showing cluster of epithelioid cells, lymphocytes and macrophages (papanicolaou 400X)
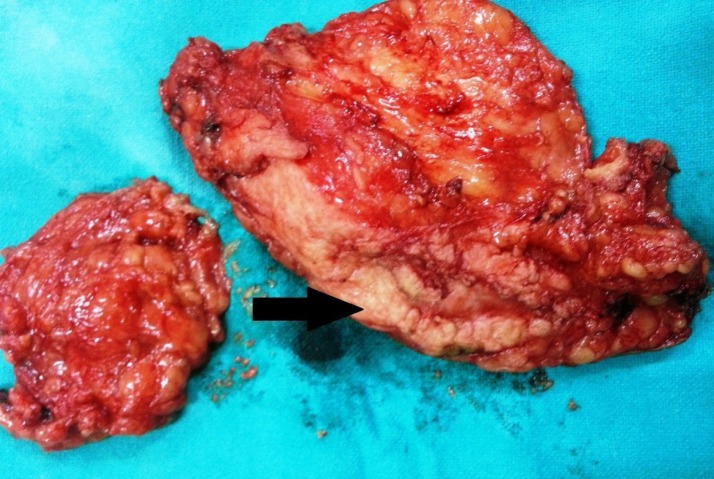
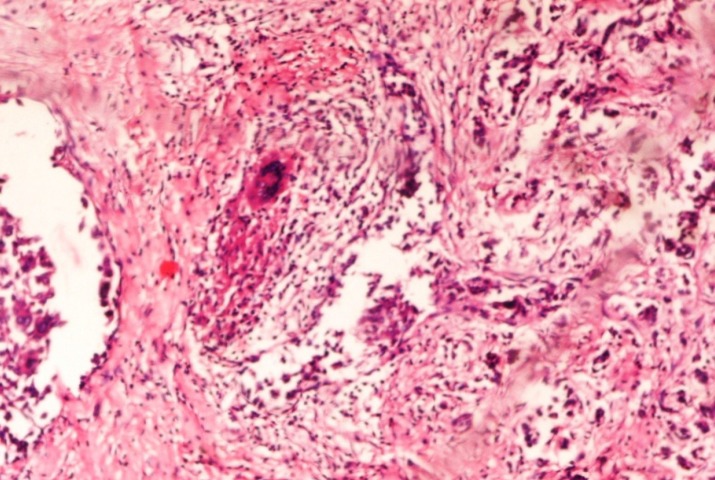
The resected specimen with axillary lymphnodes (Fig. 3) was sent for histopathological examination which showed sheets, tubules and individually scattered malignant cells along with many non-caseating granulomas composed of epithelioid cells, lipophages, lymphocytes, langhans giant cells and foreign body type of giant cells (Fig. 4). All the margins were free from the tumor. Sections from axillary lymph nodes showed similar granulomas but no metastatic deposits were seen (Fig.5). No caseous necrosis was seen and acid fast staining was negative (Fig. 6). PCR for Mycobacterium tuberculosis was also negative. Hence, the diagnosis of coexistent breast carcinoma and tuberculosis, made on the basis of Mantoux test, raised ESR and FNAC was refuted and ATT was stopped.
Fig. 3.
Resected specimen of the breast with surrounding hard fibrous tissue [arrow] and axillary lympnodes
Fig.4.
Section from the left breast showing cords and nests of malignant cells along with non-caseating granulomas (hematoxylin & eosin 100X
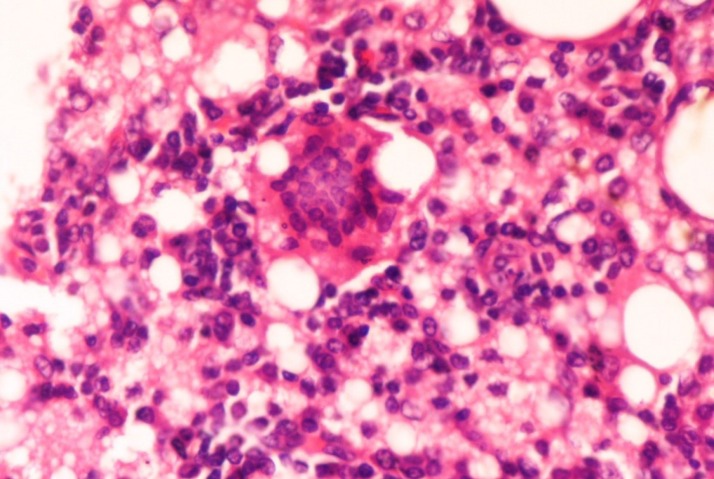
Fig. 5.
Section from lymph node showing foreign body giant cell, lymphocytes, epithelioid cells and lipophages (hematoxylin & eosin 400X
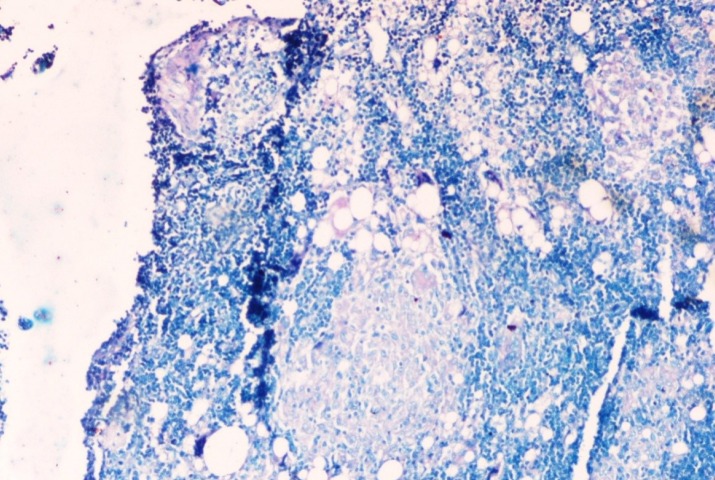
Fig. 6.
Ziehl Neelsen stained section of the axillary lymph node negative for acid fast bacilli (ZN 400X
Discussion
Oberman was the first person who reported three cases of granulomas in specific context with breast cancer (7). Alujevic et al. and Santini et al. each separately reported a case of invasive breast carcinoma with a granulomatous response and deposition of stromal amyloid (10, 11). Daroca described three cases of medullary carcinoma of the breast with stromal granulomas (12). Bässler and Birke reported five cases of breast carcinoma with stromal granulomas; four of them were infiltrating ductal carcinomas and one was an infiltrating lobular carcinoma (13).
Hall et al. suggested that the local granulomatous response is a reaction to the presence of necrotic and poorly viable tumor and the granulomas in nearby lymph nodes may be a response to tumor derived debris (14). However, certain coexistent systemic diseases like tuberculosis, sarcoidosis and fungal infections may also result in granulomas in association with tumours. In developing countries where the incidence of tuberculosis is high, it is the first differential diagnosis, thought of in the presence of granulomas along with any cancer. In such cases it is sometimes difficult to differentiate it from tumour related granulomatous response, which may lead to over diagnosis and inappropriate treatment (15).
In the present case, the 50 yr old postmenopausal patient presented with complaints of pain and lump in left breast for which she underwent FNAC. A diagnosis of coexistent infiltrating ductal carcinoma breast and tuberculosis was made on cytology. However, on histopathology of the MRM specimen, non-caseating granulomas surrounded by lipophages were seen in association with breast carcinoma. Axillary lymph nodes showed similar granulomas without any evidence of metastasis. AFB staining and PCR for mycobacterium tuberculosis DNA were negative. Hence, the possibility of coexistent TB with breast carcinoma was ruled out and a final diagnosis of infiltrating ductal carcinoma left breast with granulomatous response against tumor antigens was made. ATT was stopped after confirmation of the diagnosis. Recovery of the patient was good after surgery and she was discharged on fifth postoperative day. On 3 months follow-up, there was no evidence of any local recurrence or distant metastasis. She also received six cycles of adjuvant chemotherapy along with radiotherapy.
Conclusion
Pathologists and surgeons should be aware that granulomatous response against tumor antigens in a patient with breast cancer should be carefully differentiated from coexistent tubercular mastitis as incorrect diagnosis may lead to undue patient suffering and improper treatment.
Acknowledgements
There was no financial disclosure.
Conflict of interest
None of the authors have any conflict of interest to disclose.
References
- 1.Coyne JD. Colonic carcinoma with granulomatous (sarcoid) reaction. J Clin Pathol. 2002;55:708–9. doi: 10.1136/jcp.55.9.708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hes O, Hora M, Vanecek T, Sima R, Sulc M, Havlicek F et al. Conventional renal cell carcinoma with granulomatous reaction: A report of three cases. Virchows Arc. 2003;443:1432–2307. doi: 10.1007/s00428-003-0860-9. [DOI] [PubMed] [Google Scholar]
- 3.Sehgal S, Goyal P, Ghosh S, Mittal D, Singh S. Malignancy and Granulomatosis: Causality or Coincidence? Narrative Systematic Review. Iran J Pathol. 2014;9 (4):237–244. [Google Scholar]
- 4.Bigotti G, Coli A, Magistrelli P, De Ninno M, Antonacci V, Crucitti A, et al. Gastric adenocarcinoma associated with granulomatous gastritis report and review of the literature. Tumori. 2002;88(2):163–6. doi: 10.1177/030089160208800216. [DOI] [PubMed] [Google Scholar]
- 5.Ophir D, Nissim F, Marshak G. Granulomatous reaction in lymph nodes draining laryngeal carcinoma. Head Neck Surg. 1986;8(3):214–7. doi: 10.1002/hed.2890080315. [DOI] [PubMed] [Google Scholar]
- 6.Gorton G, Linell F. Malignant tumours and sarcoid reactions in regional lymph nodes. Acta Radiol. 1957;47(5):381–392. doi: 10.3109/00016925709170911. [DOI] [PubMed] [Google Scholar]
- 7.Oberman HA. Invasive carcinoma of the breast with granulomatous response. Am J Clin Pathol. 1987;88(6):718–721. doi: 10.1093/ajcp/88.6.718. [DOI] [PubMed] [Google Scholar]
- 8.Alalshee T, Hamed T, Shafi SM. Granulomatous reaction associated with breast carcinoma: A report of two cases. Saudi J Med Med Sci. 2014;2:120–2. [Google Scholar]
- 9.Bhatia A, Kumar Y, Kathpalia AS. Granulomatous inflammation in lymph nodes draining cancer: A coincidence or a significant association. Int J Med Med Sci. 2009;1(2):013–016. [Google Scholar]
- 10.Alujevic A, Juric G, Separovic V, Kruslin B. Invasive breast carcinoma with granulomatous stromal response. Zentralbl Gynakol. 1997;119:343–5. [PubMed] [Google Scholar]
- 11.Santini D, Pasquinelli G, Alberghini M, Martinelli GN, Taffurelli M. Invasive breast carcinoma with granulomatous response and deposition of unusual amyloid. J Clin Pathol. 1992;45:885–8. doi: 10.1136/jcp.45.10.885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Daroca PJ. Medullary carcinoma of the breast with granulomatous stroma. Hum Pathol. 1987;18:761–3. doi: 10.1016/s0046-8177(87)80255-1. [DOI] [PubMed] [Google Scholar]
- 13.Bässler R, Birke F. Histopathology of tumour associated sarcoid-like stromal reaction in breast cancer. An analysis of 5 cases with immunohistochemical investigations. Virchows Arch A Pathol Anat Histopathol. 1988;412:231–9. doi: 10.1007/BF00737147. [DOI] [PubMed] [Google Scholar]
- 14.Hall PA, Kingston J, Stansfield AG. Extensive necrosis in malignant lymphoma with granulomatous reaction mimicking tuberculosis. Histopathology. 1988;13:339–46. doi: 10.1111/j.1365-2559.1988.tb02044.x. [DOI] [PubMed] [Google Scholar]
- 15.Khurram M, Tariq M, Shahid P. Breast cancer with associated granulomatous axillary lymphadenitis: A diagnostic and clinical dilemma in regions with high prevalence of tuberculosis. Pathol Res Pract. 2007;203(10):699–704. doi: 10.1016/j.prp.2007.07.004. [DOI] [PubMed] [Google Scholar]