Abstract
Introduction
Electronic health records (EHRs), computerized order entry (CPOE), and patient portals have experienced increased adoption by healthcare systems. The objective of this study was to review evidence regarding the impact of such health information technologies (HIT) on surgical practice.
Materials and Methods
A search of Medline, EMBASE, CINAHL, and the Cochrane Library was performed to identify data-driven, non-survey studies about the effects of HIT on surgical care. Domain experts were queried for relevant articles. Two authors independently reviewed abstracts for inclusion criteria and analyzed full-text of eligible articles.
Results
2890 citations were identified. 32 observational studies and 2 RCTs met eligibility criteria. EHR or CPOE improved appropriate antibiotic administration for surgical procedures in 13 comparative observational studies. 5 comparative observational studies indicated electronically generated operative notes had increased accuracy, completeness, and availability in the medical record. The Internet as an information resource about surgical procedures was generally inadequate. Surgical patients and providers demonstrated rapid adoption of patient portals, with increasing proportions of online versus in-person outpatient surgical encounters.
Conclusion
The overall quality of evidence about the effects of HIT in surgical practice was low. Current data suggest an improvement in appropriate perioperative antibiotic administration and accuracy of operative reports from CPOE and EHR applications. Online consumer health educational resources and patient portals are popular among patients and families, but their impact has not been studied well in surgical populations. With increasing adoption of HIT, further research is needed to optimize the efficacy of such tools in surgical care.
Keywords: health information technology, electronic medical record, computerized order entry, patient portal, internet, electronic operative note
1. Introduction
Health information technology (HIT) has experienced rapid evolution and adoption over the last several decades, and the use of HIT in the process of healthcare delivery poses new challenges for both patients and providers.[1-5] A global trend has shown a rise in consumer demand for HIT by patients.[6] Within the United States, specific legislation has dramatically affected the adoption and use of HIT by healthcare organizations. The Affordable Care Act of 2010 provided financial incentives to health care providers and organizations for demonstrating Meaningful Use of certified electronic health records (EHRs) and promoted widespread adoption of HIT by healthcare organizations. In 2015, financial penalties for failure to achieve Meaningful Use of EHRs began.[7, 8] The emergence of EHRs, computerized provider order entry (CPOE), and patient portals has transformed the way health information is stored, used, and communicated among healthcare providers, patients, and caregivers.
HIT has been widely adopted across clinical specialties and practice settings. In 2013, 78.4% of office-based physicians reported having an EHR, an increase of 21% between 2012 and 2013.[9] There is evidence that this rise continues. As of October 2015, over 85% of Regional Extension Centers enrolled Critical Access/Rural Hospitals and 8 out of 10 primary care providers are demonstrating Meaningful Use of certified EHR technology.[10] 94% of non-federal acute care hospitals have possession of a certified EHR and 59.4% have adopted a basic EHR system, up from 15.6% in 2010.[11]
This increase in the implementation and adoption of HIT has prompted substantial growth in research about such systems.[12] The overwhelming majority of research on the effects of HIT has been conducted in primary care and medical specialty settings, with a paucity of data on how the use of HIT affects surgeons and the care of surgical patients.[13-15] The objective of this study is to review comprehensively the available evidence on the impact of HIT on surgical practice. We aimed specifically to determine the effects of EHRs, CPOE, patient portals, and Internet-based information resources on the care of surgical patients.
2. Materials and Methods
2.1 Data Sources and Search Strategy
We performed a systematic search of Medline, EMBASE, CINAHL, and the Cochrane Library to identify published literature on the effects of EHRs, CPOE, patient portals, or online health information resources on surgeons and their patients from 1990 to July 2015. The search was focused specifically on studies performed exclusively in surgical patients or subsets. Medical Subject Heading (MeSH) terms and keywords used for the search included those pertaining to computerized health record systems, electronic health records, information technology, medical order entry systems, personal health record, computerized order entry, patient or web portals, access to information, patient participation, surgery, surgical procedures, or operative care.
The search query employed was: ("Medical Records Systems, Computerized"[MeSH Terms] OR "Electronic Health Records" [MeSH Terms] OR “personal health record”[Title/Abstract] OR “information technology”[Title/Abstract] OR “Medical Order Entry Systems"[MeSH Terms] OR “computerized order entry”[Title/Abstract] OR "patient portal" OR "web portal" OR "Access to Information"[MeSH Terms] OR "Patient Participation"[MeSH Terms] OR "Patient Access to Records"[MeSH Terms]) AND ("surgeons"[MeSH Terms] OR "surgical procedures, operative"[MeSH Terms] OR “surg*”[Title/Abstract]) AND ("1990"[PDAT] : "2015"[PDAT]). In addition, we also queried surgeons with expertise in informatics or HIT and mined the bibliographies of all retrieved articles for citations of potentially relevant articles. Prior systematic reviews were utilized to identify original studies.
2.2 Study Selection
We selected for analysis all experimental, observational, randomized, or non-randomized studies published in scientific journals, peer-reviewed conference proceedings or sources identified by domain experts. Editorials, government reports, letters to the editor, conference abstracts, or non–data-driven studies were excluded. Articles not published in English and without full text availability were excluded. We included only studies that examined the effects of HIT related specifically to surgical practice or contained a separate surgical subgroup analysis.
Two authors independently reviewed the abstracts of all retrieved articles to identify publications meeting inclusion criteria and then performed full text review of relevant articles. Disagreements were resolved with assessment by a third reviewer and discussion to achieve consensus.
2.3 Data Analysis and Grading Criteria
Study classification was performed in a similar manner as prior systematic reviews in health information technology.[12, 15-17] We classified articles into descriptive qualitative studies, descriptive quantitative studies, and hypothesis-testing studies. Articles were classified as “hypothesis-testing” if the investigators used statistical analysis to compare data between groups. Hypothesis-testing studies were further classified by study design (e.g., randomized, controlled trial (RCT) and retrospective or prospective observational studies).
The authors summarized the data available for each category of HIT, which allowed formulation of a general consensus and determination of what areas were lacking evidence. Due to the heterogeneity of the studies identified, a meta-analysis was not performed.
3. Results
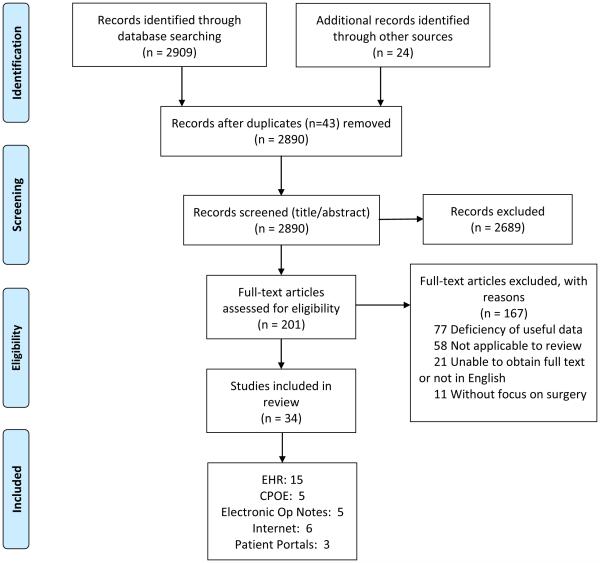
The systematic database search retrieved 2909 potentially relevant publications. An additional 24 articles were identified from expert recommendations and bibliographies of retrieved articles. After removal of duplicate articles and abstract review, 201 potentially eligible articles underwent full-text review, of which 34 studies were retained for data analysis (Figure 1). The majority of articles were excluded based on the lack of data-driven evidence.
Figure 1. Outline of Review of Health Information Technology for Surgical Patient Care.
Systematic database search retrieved 2909 potentially relevant publications and an additional 24 articles were identified from expert recommendations and bibliographies of selected articles. After removal of duplicate articles and abstract review, 201 articles underwent full-text review. 34 studies were retained for data analysis, 15 examined the impact of electronic health records (EHRs); 5, computerized provider order entry (CPOE); 5 electronic operative notes; 6 online health information resources; and 3 patient portals.
Table 1 presents a summary of the evidence for the effects of HIT in surgical care. Of the 34 studies analyzed, 15 examined the impact of EHRs; 5, CPOE; 5, electronic operative notes; 6, online health information resources; and 3, patient portals. The vast majority of the evidence was low (9 studies) or very low (20 studies) in quality. Five research studies had moderate levels of evidence, and only one article reported high quality evidence. Four of the five articles with moderate levels of evidence evaluated EHRs, and one examined an online informational resource. All included studies on CPOE, electronic operative notes, and patient web portals in surgical care had low or very low levels of evidence.
Table 1.
Health Information Technology Research in Surgical Care
| Author | Study Name | Year | Type of Study | Cohort Size (Study/Control) |
Institution | Finding/Addition to literature/Limitations | Result |
|---|---|---|---|---|---|---|---|
| ELECTRONIC HEALTH RECORDS | |||||||
| Larsen et al. | Improved Perioperative Antibiotic Use and Reduced Surgical Wound Infections Through Use of Computer Decision Analysis |
1989 | Prospective Observational Study |
1621/1830 | LDS Hospital | Developed a computerized decision analysis tool to determine which patients qualified for receipt of pre-operative antibiotics. Found a decrease in surgical site infections in the patients stratified to the computerized decision analysis cohort; however, this was not statistically significant after adjusting for the larger quantity of clean cases in the cohort. Found an improvement in timing of prophylactic antibiotic administration, likely due to the impact of placing physician reminder stickers in patient charts. |
Positive |
| Evans et al. | Reducing the Duration of Prophylactic Antibiotic Use Through Computer Monitoring of Surgical Patients |
1990 | Prospective Observational Study |
3665/3991 | LDS Hospital | The EHR was used for a clinical decision support system for identifying surgical patients who could have their antibiotics discontinued, followed by a clinical pharmacist who would place a stop-order. No decrease in the number of patients receiving antibiotics too long, but there was a decrease in the number of antibiotic doses for the patients identified as having no indication for antibiotics, from 19 to 13 days. |
Positive |
| Durieux et al. | A Clinical Decision Support System for Prevention of Venous Thromboembolism |
2000 | Prospective Observational Study |
1112/859 | Lariboisiere Hospital |
Implemented a clinical decision support system which determined based on patient characteristics the risk of a venous thromboembolism and recommendation for prophylaxis in an orthopedic surgery population. There was an improvement in compliance with guidelines from 82.8% in the control (no CDSS) to 94.9% in the intervention group. |
Positive |
| Stengel et al. | Comparison of Handheld Computer-Assisted and Conventional Paper Chart Documentation of Medical Records |
2004 | Randomized Controlled Trial |
36/36 | Berlin Trauma Center |
Compared traditional paper charting to coding software on a handheld computer for use at the bedside. The handheld device allowed automatically generated ICD codes related to complaints and clinical findings, resulting in significantly more coded diagnoses. There was a significant decrease in the time required for handheld documentation during the study period. |
Positive |
| St. Jacques et al. |
Improving Timely Surgical Antibiotic Prophylaxis Redosing Administration Using Computerized Record Prompts |
2005 | Retrospective Observational Study |
148/139 | Vanderbilt University Medical Center |
Using a part of the computerized record system, the anesthesia computer charting software, computerized alerts notified providers of an approaching redose time 30 minutes prior to the specified time interval. On time antibiotic redosing increased after the implementation of the reminder system, from 20% to 57%. |
Positive |
| O’Reilly et al. | An Anesthesia Information System Designed to Provide Physician-Specific Feedback Improves Timely Administration of Prophylactic Antibiotics. |
2006 | Prospective Observational Study |
Unknown | University of Michigan Health System |
Implemented a reminder system for antibiotic administration in an anesthesia information management system. The rate of antibiotic compliance increased from 69% to 92% during a 1-year study period. |
Positive |
| Wax et al. | The Effect of an Interactive Visual Reminder in an Anesthesia Information Management System on Timeliness of Prophylactic Antibiotic Administration. |
2007 | Retrospective Observational Study |
4987/9478 | Mount Sinai | Retrospectively analyzed the effect of the addition of an event icon for antibiotic administration in the operating room. Compliance for administration of antibiotics increased from 82.4% to 89.1% before and after the even icon implementation. |
Positive |
| Staes et al. | Computerized Alerts Improve Outpatient Laboratory Monitoring of Transplant Patients |
2008 | Prospective Observational Study |
348/2123 | LDS Hospital | Compared a traditional reporting system using clinic staff to track new laboratory results to a system with integrated computerized alerts in transplant patients. 34% of traditionally reported labs did not reach the office and although the results were available in the EHR, no alert notified physicians that the new result was present. 0.8% of computerized lab notifications were not reported. Nurses were able to review the results much quicker with the computerized notification (9.2 hours compared to 33.4 hours). |
Positive |
| Haut et al. | Improved Prophylaxis and Decreased Rates of Preventable Harm with the Use of a Mandatory Computerized Clinical Decision Support Tool for Prophylaxis for Venous Thromboembolism in Trauma |
2010 | Retrospective Observational Study |
399/1200 | Johns Hopkins Hospital |
Implemented a clinical decision support system (CDSS) which determined based on patient characteristics the risk of a venous thromboembolism (VTE) and recommendation for prophylaxis in adult trauma patients. The compliance rate for evidence-based VTE prophylaxis improved from 66.2% at baseline (no CDSS) to 84.4% and there was a decrease in preventable VTE rates after CDSS implementation. |
Positive |
| Nair et al. | Feedback Mechanisms Including Real-Time Electronic Alerts to Achieve Near 100% Timely Prophylactic Antibiotic Administration in Surgical Cases |
2010 | Prospective Observational Study |
3159/8550 | University of Washington |
Retrospective review of the paper anesthesia charting reports and prospective study on the implementation of an AIMS to determine antibiotic documentation rates. Real-time feedback and reminders to the anesthesia team to administer and document antibiotics made the largest improvement (9.3%). |
Positive |
| Schwann et al. | Point-of-care Electronic Prompts: an Effective Means of Increasing Compliance, Demonstrating Quality, and Improving Outcome. |
2011 | Prospective Observational Study |
9127/10617 | Lehigh Valley Health Network |
Prospectively analyzed the effect of point of care electronic prompts via an AIMS on the administration of prophylactic antibiotics and surgical-site infections. Compliance with antibiotic administration increased from 31% to 92% and the overall rate of SSI decreased from 1.1% to 0.7% for the 6-month period before and after prompts implementation. |
Positive |
| Yang et al. | The Effect of Electronic Medical record Application on the Length of Stay in a Chinese General Hospital: a Department- and Disease-focused Interrupted Time-series Study |
2013 | Retrospective Observational Study |
31153/56022 | Xijing Hospital | Compared the length of hospital stay(LOS) for patients before and after the implementation of an EHR. Orthopedic and cardiac surgery units with patients having the specific diagnoses of intervertebral disc disorders and ventricular septal defects had decreased LOS by an average of 2.3-2.8 days. Authors note that this may be due other factors which simultaneously underwent change related to LOS. |
Positive |
| Choi et al. | Organizational Performance and Regulatory Compliance as Measured by Clinical Pertinence Indicators Before and After Implementation of Anesthesia Information Management Systems (AIMS) |
2014 | Retrospective Observational Study |
3997/984 | Maimonides Medical Center |
Compared patients who had data documented in AIMS versus the traditional paper charts. One outcome was the completeness of the documentation which significantly increased with EHR charting (p< 0.001). They also analyzed each of the separate parameters and found that although there was an improvement in documentation of medication dosages, physiological status, mental status, and pain improved, there was not a significant improvement in compliance with antibiotic administration. Of note, their system did not have an interactive prompt as a reminder for antibiotic administration. |
Positive |
| Pinto Thirukumaran et al. |
The Impact of Electronic Health Record Implementation and Use on Performance of the Surgical Care Improvement Project Measures |
2015 | Retrospective Observational Study |
1816 | Strong Memorial Hospital/Highland Hospital |
Compared SCIP measures pre-EHR to post-EHR. They found a decline in odds of urinary catheter removal and blood glucose control after surgery in the months immediately following EHR deployment. After 3 months of deployment, there was a statistically insignificant improvement in scores for these measures. |
Negative |
| Flatow et al | Quality Outcomes in the Surgical Intensive Care Unit after Electronic Health Record Implementation |
2015 | Retrospective Observational Study |
1274/1229 | Mount Sinai | Analyzed quality indicators in a surgical ICU 2 years before and after the implementation of an EHR. There was no difference in LOS, C.diff colitis, readmission rate, and case mix indexes. Found an 85% decrease in central line associated blood stream infections per 1000 catheter days and a 28% decrease in mortality within the SICU. However, the study had a significant number of cofounders including the use of daily goals sheets for central line necessity, hiring of more physician extenders, and palliative care involvement for early patient transfers. |
Positive |
| COMPUTERIZED PROVIDER ORDER ENTRY (CPOE) | |||||||
| Webb et al. | Reducing Surgical Site Infections through a Multidisciplinary Computerized Process for Preoperative Prophylactic Antibiotic Administration |
2006 | Prospective Observational Study |
unknown | Atlanta Veterans Administration Hospital |
Implemented a computerized order entry option for preoperative antibiotics with practice improvement, improving appropriate and timely administration. Found a significant decrease in clean wound infection rates from 2.7% to 1.4% during the 1-year study period. |
Positive |
| Liu et al. | Using Information Technology to Reduce the Inappropriate use of Surgical Prophylactic Antibiotic |
2008 | Prospective Observational Study |
858 | Taichun Veterans General Hospital |
Implemented a physician education program and computerized reminder system to order post-operative antibiotics according to guidelines. There was no change in postoperative wound infection rates, but there was a decrease in the use of prophylactic antibiotics for clean cases and decreased duration of prophylactic antibiotics for clean contaminated cases. |
Positive |
| Haynes et al. | Effectiveness of an Information Technology Intervention to Improve Prophylactic Antibacterial use in the Postoperative Period |
2010 | Prospective Observational Study |
2608/2808 | University of Pennsylvania |
Studied the implementation of an order set preventing prophylactic antibiotics to be ordered for longer than a specified time period (20 hours or 44 hours after surgery in non-cardiac and cardiac surgery patients respectively). Timely discontinuation of antibiotics increased from 38.8% to 55.7%. This discontinuation was virtually only present in locations of the hospital where the electronic CPOE would trigger, suggesting it was not an educational improvement. |
Positive |
| Appari et al. | Medication Administration Quality and Health Information Technology: a National Study of US Hospitals |
2011 | Retrospective Observational Study |
Unknown | Dartmouth, The Health Information and Management Systems Society Analytics Database |
Analyzed data from nationwide hospitals to determine if the use of EHR and/or CPOE had an effect on the administration of recommended medications. Found a small increase in the odds of receiving the appropriate preoperative antibiotics and VTE prophylaxis in hospitals with EHR and CPOE. Also found hospitals demonstrated better medication compliance with increased experience with EHR or CPOE. |
Positive |
| Van Sise et al. | Improving the Selection of Recommended Prophylactic Antibiotics Using an Electronic Medical Record |
2012 | Retrospective Observational Study |
934/938 | Stony Brook Hospital |
Retrospectively looked at the use of prophylactic antibiotics before and after the addition of computerized order sets for antibiotics. There was an increase in the use of recommended antibiotics from 43.4% to 58.1% after order set CPOE. |
Positive |
| ELECTRONIC OPERATIVE NOTES | |||||||
| Laflamme et al. |
Efficiency, Comprehensiveness and cost effectiveness when comparing dictation and electronic templates for operative reports |
2005 | Prospective observational study |
138/198 | Wishard Memorial Hospital |
Compared template electronic notes to traditional dictated notes. Time to verified completed document was 0.46 hours v 374 hours for the template group compared to dictation group. Estimated an average monthly saving of 650 dollars from not having to pay for dictation services. “Key elements” were present in 97% of template electronic reports and 85% of dictated reports. Mean time to produce the report was slightly longer in the template group (6.77 minutes compared to 5.96 minutes. |
Positive |
| Cowan et al. | Electronic Templates versus Dictation for the Completion of Mohs Micrographic Surgery Operative Notes |
2007 | Retrospective Observational Study |
58/52 | Johns Hopkins Medical Center |
Compared dictated operative notes using a template to electronic template operative notes. The dictated notes required more than a minute longer to complete than those complete by templates. Editing of notes for dictations was 201 seconds compared to 41.6 seconds for electronically generated notes. Template electronic notes took 0.115 days to sign versus 20.7 days to sign dictated notes. For dictated notes, 81 % had at least one error. 5.77 % of electronic template notes had one or more errors. |
Positive |
| Park et al. | Electronic Synoptic Operative Reporting: Assessing the Reliability and Completeness of Synoptic Reports for Pancreatic Resection |
2010 | Prospective/Retrospective Observational Study |
112/102 | MSKCC | Electronic synoptic operative reports were developed for pancreatic resections and compared to prior dictated operative notes by the same surgeon for the same procedure. The operative reports were evaluated with a checklist. Electronic notes had significantly higher completeness checklist scores compared to dictated notes (88.8% versus 59.6%) and were available in median 0.5 days compared with 5.8 days for dictated operative notes. Notes were completed in an average of 4 minutes, which was not compared to dictation. |
Positive |
| Hoffer et al. | Structured electronic operative reporting: Comparison with dictation in kidney cancer surgery |
2011 | Retrospective Observational Study |
158/97 | Princess Margaret Hospital and the Ontario Cancer Center |
Creation of an electronic, online service for electronic operative note creation for urologists. Increased completion rate from 68% to 92% with structured notes compared to dictated notes. There was no difference between attending staff and trainees, and physicians chose which method they wanted to use. 30% of dictated notes were completed in over 5 days and the median time for electronic notes was 2 days. |
Positive |
| Ghani et al. | Smart electronic operation notes in surgery: An innovative way to improve patient care |
2014 | Retrospective Observational Study |
50/50 | Royal London Hospital |
Audit of 50 operative notes before and after the implementation of electronic operative notes showed an improvement in operative note completeness. Prior to electronic note, 60% contained closure details, 69% included antibiotics at induction, and 66% had legible hand writing. After electronic operative notes, 100% included closure details, antibiotics, and were legible. |
Positive |
| INTERNET | |||||||
| Melloul et al. | Donor Information for Living Donor Liver Transplantation: where can Comprehensive Information Be Found? |
2012 | Qualitative Research | NA | Internet | Used the EQIP (Ensuring quality information for patients) instrument to analyze living donor liver transplantation information found through the first 100 websites identified through 3 search engines, resulting in 32 unique websites. A median number of 16 out of 36 criteria were met. |
NA |
| Bruce-Brand et al. | Assessment of the Quality and Content of Information on Anterior Cruciate Ligament Reconstruction on the Internet |
2013 | Qualitative Research | NA | Internet | Used the JAMA benchmark, DISCERN criteria, and HONcode certification to analyze the content returned when ACL reconstruction was queried by analyzing the first 60 returned sites on 4 search engines. Websites with HONcode certification had significantly higher mean DISCERN scores. Academic institutions had higher DISCERN scores. |
NA |
| Fast et al. | Evaluating the quality of Internet health resources in pediatric urology |
2013 | Qualitative Research | NA | Internet | Used DISCERN and HONcode to analyze 60 websites identified with Google for the terms circumcision, posterior urethral valves, and vesicoureteral reflux. 25-30% of the websites were HONcode certified. Out of the maximum score of 80, the average DISCERN Plus score was 60, 40, and 45 respectively. |
NA |
| Sullivan et al. | Can Internet Information on Vertebroplasty be a Reliable Means of Patient Self- Education? |
2014 | Qualitative Research | NA | Internet | Used a rating system to determine if the first 35 articles on 3 search engines contain one indication, one risk and one benefit on vertebroplasty. 43% of sites were adequate with sites lacking most in risks and contraindications to procedures, especially in academic centers. |
NA |
| Corcelles et al. | Assessment of the quality of Internet information on sleeve gastrectomy |
2015 | Qualitative Research | NA | Internet | Used the JAMA benchmark, DISCERN criteria, and HONcode certification to analyze the content in 50 sites for sleeve gastrectomy. Using the mean of three separate scorers, the average score 46.3 out of 80. Academic institutions had higher DISCERN scores. |
NA |
| Fortier et al. | Web-Based Tailored Intervention for Preparation of Parents and Children for Outpatient Surgery |
2015 | Randomized Controlled Trial |
38/44 | Children’s Hospital of Orange County and Yale Children’s |
Implemented a web-based tailored pre-operative educational intervention for both parents and children. Found significantly decreased anxiety of children upon entrance to the OR and introduction of the mask as well as decreased parent anxiety in preoperative holding according to the Modified Yale Preoperative Scale and the State-Trait Anxiety Inventory, respectively. |
Positive |
| PATIENT WEB PORTALS | |||||||
| Burke et al. | Transforming Patient and Family Access to Medical Information |
2010 | Prospective Observational Study |
252 | Miami Children’s Hospital | Developed a web-based patient accessible electronic health record that contained textual and image data. 252 of 270 (93%) of parents offered access became users of the system. Image data was accessed more frequently than textual data. The resource was used more frequently while patients were in the hospital (67% v 33% of total logins). No patients or families requested to see their paper charts during the study period. |
Positive |
| Baucom et al. | Case Report: Patient Portal Versus Telephone Recruitment for a Surgical Research Study |
2014 | Prospective Observational Study |
391/74 | Vanderbilt University Medical Center |
Study compares the recruitment of patients who have undergone a ventral hernia repair for a research study either through telephone call or patient web portal messaging. Patients recruited through the portal were slightly younger and more recently had undergone their operation compared to patients recruited via telephone. The portal was successful at recruiting 16% of the total study participants. |
Positive |
| Shenson et al. | Rapid Growth in Surgeons’ Use of Secure Messaging in a Patient Portal |
2015 | Retrospective Observational Study |
20484 | Vanderbilt University Medical Center |
Analyzed three years of patient-initiated portal message threads and found that secure messages accounted for 11.5% of all surgical outpatient interactions during the study period. The use of portal messaging gradually increased over the three year period (5.4 % in 2008 to 15.3% in 2010). |
Neutral |
The following paragraphs present the evidence for the effects of HIT on surgical patients and practice, organized by type of technology.
3.1 Electronic Health Records
Fifteen articles were identified containing data-driven studies on the impact of EHRs on the care of surgical patients.[18-32] These articles varied in their study design and outcomes.
Four studies examined the impact of EHRs on the care of post-surgical patients. Pinto Thirukumaran and colleagues conducted a historical comparison study, which found that Surgical Care Improvement Project (SCIP) measures of quality such as early Foley catheter removal and adequate blood glucose control declined significantly in the first 3 months after EHR implementation but leveled off after 3 months.[31] Another study, analyzing a 4.5 year period before and after the implementation of an EHR at Xijing Hospital in China, found that the length of hospital stay significantly decreased in surgical patients admitted to cardiovascular and orthopedic surgical specialties for the specific diagnoses of intervertebral disc disorders and ventricular septal defects by an average of 2.3-2.8 days.[29] Flatow and colleagues found an 85% decrease in central line associated blood stream infections per 1000 catheter days and a 28% decline in mortality within a surgical intensive care unit after the institution of an EHR; however, there were many associated confounders.[32]
Stengel and colleagues conducted a RCT that randomized 80 patients to charting with either traditional paper-based methods or using hand-held devices on an orthopedic surgery inpatient unit.[21] This study showed a significant improvement in the daily documentation with the handheld device as measured by the generation of International Classification of Disease (ICD) diagnosis codes, with an increase in the median number of diagnoses per patients from 4 to 9. In addition, the investigators reported a significant decrease in the time required for handheld documentation (from 10-15 minutes to 2-3 minutes) as the study period progressed, but they did not compare the time for completion of the hand-written notes to the electronic notes.
Six articles were focused on the effects of computerized alerts to notify providers of critical information, such as laboratory results or the need for prophylactic antibiotic dosing, another major SCIP initiative.[22-27] Staes and colleagues performed a prospective observational study focused on outpatient laboratory monitoring of liver transplant patients at the LDS Hospital in Salt Lake City, Utah. The investigators compared laboratory reporting by traditional methods such as fax and postal mail with a computerized alerting system in an EHR. They found a significant improvement in the review of laboratory results in transplant patients using a computerized alerting system.[25] With the traditional reporting process, 34% of laboratory results did not reach the office and although the results were available in the EHR, no alert notified physicians that the new result was present. Using electronic reporting, 0.8% of computerized lab notifications were not reported to an appropriate clinician. Nurses were able to review the results much quicker with the computerized notification (9.2 hours compared to 33.4 hours).
The remaining studies on computerized alerts were centered on anesthesia information management systems (AIMS), integrated electronic record systems for anesthesia providers. Although surgeons themselves may not interact with the AIMS directly, these systems have direct impact on surgical patients. AIMS can provide structured data entry fields and point-of-care electronic alerts, preventing providers from continuing documentation until certain fields are complete. In a recent retrospective observational study, Choi and colleagues reviewed anesthesia documentation during a 3-year period before and 1-year period after the institution of AIMS, and evaluated documentation quality based on three metrics, clinical pertinence indicators from SCIP, elements of performance (EP) from The Joint Commission (TJC), and guidelines from the Centers for Medicare and Medicaid Services (CMS). They found a significant improvement in adequate documentation including medication dosages, physiological status, mental status, and pain scales, attributable to data entry fields that required completion prior to advancing.[30] They did not find improvement in compliance of antibiotic administration, noting that the AIMS could have been optimized by inclusion of a computerized alert as a reminder to administer the antibiotics within 60 minutes of incision. Schwann and colleagues prospectively analyzed a 6-month period before and after implementation of medical record point-of-care electronic alerts for prophylactic antibiotic administration and found a significant increase in antibiotic compliance, from 31% to 92%, and decrease in overall surgical site infections, from 1.1% to 0.7%.[27] Other researchers also found electronic alerts in the AIMS to increase appropriate and timely antibiotic administration, but the existence of other confounding factors could not be excluded, such as continuing education or changing practice patterns. The improvement was greater in studies starting out with poor compliance. For example, appropriate perioperative antibiotic administration rates increased from 20% to 57% in 2005 at Vanderbilt University Medical Center and from 69% to 92% in 2006 at University of Michigan Health Center.[22, 23] More recent studies with baseline antibiotic compliance rates over 80% showed a less than 10% improvement.[24, 26]
Four large-scale observational studies evaluated clinical decision support systems (CDSSs) specific for surgical patients.[18-20, 28] CDSSs include software designed to make recommendations and directly aid clinicians in appropriate decision-making.[33] In 1989, Larsen and colleagues assessed infection rates before and after implementing a computerized decision analysis tool for determining if surgical patients should receive pre-operative antibiotics.[18] Although they reported a decrease in surgical site infections (SSIs) after deploying the computerized decision support (1.8% to 0.9%), this effect was not statistically significant after adjusting for the larger quantity of clean cases in the cohort with decision support. They did have an 18% improvement in timing of prophylactic antibiotic administration, likely due to the impact of placing physician reminder stickers in the patient charts of those undergoing procedures deemed to benefit from antibiotic use. In two studies, a CDSS used patient characteristics to risk stratify the need for venous thromboembolism (VTE) prophylaxis. In 2000, Durieux and colleagues showed an improvement in compliance with VTE prophylaxis guidelines from 82.8% in the control (i.e., no CDSS) to 94.9% in the intervention group among orthopedic surgery patients in an alternating time-series designed study, with three 10-week intervention periods, four 10-week control periods, and a 4-week washout between each period.[20] In 2010, Haut and colleagues conducted a historical comparison study on a similar CDSS for adult trauma patients and found compliance improved from 66.2% in a 1-year baseline period (no CDSS) to 84.4% in a 3-year period after CDSS implementation.[28] They also found a significant decrease in preventable VTE events, from 4 events in the 1-year control period to 4 events in the 3-year intervention period.
3.2 Computerized Provider Order Entry
The review identified five articles highlighting the use of CPOE in surgical practice.[34-38] Four observational studies showed an improvement in appropriate prophylactic antibiotic administration with the use of CPOE or electronic pre-operative order sets.[34-36, 38] Webb and colleagues reported a decrease in the incidence of clean wound SSIs from 2.7% to 1.4% during a 1-year study period with the implementation of CPOE along with educational practice improvement initiatives.[34]
Prophylactic antibiotics may not be indicated for all cases, and inappropriate perioperative antibiotic administration is not without risk. One study at a Veteran’s Hospital in Taiwan showed that a physician education program in conjunction with computerized reminders decreased the ordering of prophylactic antibiotics in clean cases in otolaryngology.[35] Although prophylactic antibiotics are often indicated, multiple repeated doses of antibiotics in the postoperative setting without infection are not, and may increase hospital antibacterial resistance.[39, 40] Haynes and colleagues implemented a CPOE system that restricted the ability of providers to order antibiotics specified as prophylactic beyond a recommended time point.[36] The computerized decision support in conjunction with CPOE determined the appropriate duration of antibiotic therapy, improving timely discontinuation of antibiotics from 38.8% to 55.7% over an 8-month period.
Appari and colleagues used nationwide databases to determine if the use of EHR and/or CPOE has an effect on the administration of recommended medications.[37] They performed a comparison of the Health Information and Management Systems Society (HIMSS) Analytics Database, which surveys 5281 non-federal acute-care hospitals in the United States for hospital characteristics and operational status of HIT applications, and CMS Hospital Compare Database, which provides medication-related process quality measures for more than 3470 non-federal acute-care hospitals. In hospitals with EHR and CPOE, they found 13% and 29% increases in the odds of receiving preoperative antibiotics and appropriate VTE prophylaxis, respectively. Interestingly, the effect was more prominent in institutions where EHR or CPOE had been in place for a longer period of time and each additional 2 years of technology use was associated with 6-15% higher odds of compliance. This study was conducted prior to the Affordable Care Act and limited by a lack of data about dates of HIT implementation for many hospitals.
3.3 Electronic Operative Notes
This review found 5 studies evaluating the use of electronic operative notes in surgical care.[41-45] Each article reported either a retrospective or prospective observational study consisting of sample sizes with less than 200 notes in each arm. All studies showed greatly improved inclusion of crucial information, such as closure details, anesthesia, and antibiotics in electronically generated notes.
Ghani and colleagues compared 50 electronic and 50 handwritten operative notes for emergency orthopedic trauma surgery, finding that all electronically generated notes were legible in comparison to 66% of hand-written operative notes.[45] Four of the studies reported a significant decrease in the time to finalization of electronic notes, with electronic notes being completed in 0.115. − 0.5 days compared to 5.8 −20.7 days for dictated notes.[41-44] Most studies compared non-templated hand-written or dictated notes to templated electronic notes and included operative reports from different surgeons. Creation of the note took slightly longer (mean 6.77 versus 5.96 minutes; p = 0.036) for electronic notes compared with dictated notes in a 2005 study of reports for common obstetrical and gynecologic procedures performed at the Wishard Memorial Hospital, a county hospital in Indianapolis, Indiana.[41]
Cowan and colleagues showed that for a specific operation, Mohs micrographic surgery, editing of the notes was much shorter for electronic notes than for dictation (41.6 seconds versus 201.1 seconds).[42] They compared dictated notes based on an outline of the procedure to electronic notes based on a template using a system designed at Johns Hopkins Medical Center.[42] Even though both notes were generated based on a template, significantly more of the dictated notes contained an error (81.03%) compared to electronic notes (5.77%).
Park and colleagues conducted a historical case controlled comparison of electronic notes to previously dictated notes by the same surgeon performing the same procedure of pancreatic resections.[43] Electronic notes had significantly higher completeness checklist scores compared to dictated notes (88.8% versus 59.6%) and were available in median 0.5 days compared with 5.8 days for dictated operative notes. Electronic notes were completed in an average of 4 minutes.
3.4 Surgical Consumer Health Information on the Internet
A total of 6 articles studied Internet resources for surgical patients and disease processes. Five of the articles analyzed the quality of information available on the Internet for a particular disease or procedure, including resources about living donor liver transplantation, anterior cruciate ligament reconstruction, circumcision, posterior urethral valves, vesicoureteral reflux, vertebroplasty, and sleeve gastrectomy.[46-50] These studies used popular search engines to determine the quality of websites returned in response to health related terms. Three of these studies used the DISCERN criteria and presence or absence of the HONcode seal to determine the quality of information.[47, 48, 50] One article used author-generated criteria to grade the websites and another used the Ensuring Quality Information for Patients (EQIP) tool.[46, 49]
DISCERN is a reliable instrument designed to judge the quality of written consumer health information regarding treatment choices.[51] The DISCERN score ranges from 0-80 based upon publication reliability, the quality of information on different treatment choices, and the overall rating.[50] The Health On the Net (HON) Foundation is a nonprofit, nongovernmental organization, accredited for establishing ethical standards for health-related information on the Internet.[52, 53] Obtaining HONcode certification requires individual websites to apply for evaluation. The HONcode seal accredits websites based on the transparency and quality of the information provided.[50] The EQIP instrument is a checklist applicable to all information types for evaluation of quality, readability, and design aspects of written information. It has been expanded for use in evaluation of health-related information.
Regardless of the scoring criteria utilized, all studies reported that the quality of health information on the Internet about these specific surgical procedures was poor.[46-49] Mean DISCERN criteria scores ranged from 40 – 60 (out of 80) and only 4-30% of the websites bore the HONcode seal. Websites with HONcode certification had significantly higher mean DISCERN scores (58.0 v 39.8).[47] Two studies found that academic institutions had improved quality of websites based upon DISCERN scores (approximate 10-point improvement) compared to average quality of all websites combined (including physicians, academic, commercial, social network, non-physicians, and unspecified websites).[47, 50] These studies were limited in that they typically analyzed one surgical procedure or problem.
Fortier and colleagues conducted a small-scale RCT in 2015 which evaluated a tailored web-based intervention for surgical patients.[54] Children undergoing elective outpatient surgery and their parents were randomized to the use of an Internet-based intervention preoperatively or standard of care (no intervention). Anxiety levels for both children and parents on the day of surgery were decreased with the intervention according to the Modified Yale Preoperative Scale and the State-Trait Anxiety Inventory, respectively. The study consisted of a small sample size of approximately 40 patients in each arm, and participation was limited to children without developmental delays and parents with available Internet access.
3.5 Patient Web Portals
The review identified three articles that studied the effects of patient web portals on surgical care.[55-57] All of these studies were observational and involved web-based applications allowing patients and their family members to view portions of the EHR or interact with healthcare systems through messaging. In one study, parents of patients undergoing congenital cardiac surgery at Miami Children’s Hospital from 2006 to 2009 were offered access to a system that allowed users to view admission notes, discharge summaries, discharge instructions, operative images, and daily bedside images of the patient. During the study period, 252 of 270 of parents (93%) offered access became users of the system. Users accessed the system more often while the patients were in hospital than after discharge (67% v 33% of total logins). Imaging data were viewed significantly more frequently than textual data.[55] At Vanderbilt University Medical Center, a comprehensive patient portal was shown to be a useful resource in the recruitment of participants for a study of outcomes after ventral hernia repair, with 44% of study participants having a registered portal account and 16% of the participants recruited through portal messaging.[56] Shenson and colleagues examined the growth in adoption of patient-provider secure messaging through the same portal relative to outpatient clinic visits at Vanderbilt University Medical Center in the 3-year period after portal implementation. This study demonstrated that in surgical specialties, portal messaging accounted for 11.5% of all outpatient interactions (i.e., message exchanges and clinic visits) in surgical practice. Furthermore, portal message exchanges between surgical patients and providers continued to increase over time, with messaging accounting for 5.4 % of outpatient interactions in 2008 and 15.3% in 2010.[57] The exact nature of patient and provider interactions conducted through messaging was not explored.
4. Discussion
This comprehensive review reveals a paucity of research about the effects of HIT in surgical practice and an overall poor quality of available evidence. Our review identified 34 studies evaluating HIT effects on the care of surgical patients, and the grade of evidence was predominately low. The Affordable Care Act has stimulated rapid implementation and adoption of EHRs and CPOE. Increasing access to and use of the Internet by patients has prompted the emergence of consumer HIT. Although these technologies are becoming ubiquitous in healthcare as organizations respond to regulatory requirements and consumer demands, they are not new. Computer-based health records were implemented as early as the late 1950s using punch card technologies, and patients have been seeking health information on the Internet for decades. Many of the pioneering researchers in the fields of health informatics were primary care or medical specialty providers. Therefore, research about the development and evaluation of HIT for surgical providers and patients has been limited.[58, 59]
Available evidence about the use of a variety of HIT tools by surgical providers does however demonstrate three consistent trends in the effects of these technologies: enhanced quality of surgical documentation, increased adherence to guidelines for medication administration sometimes with associated better clinical outcomes, and improvements in patient care with tools for alerting providers. Improved documentation quality was an early goal for EHR systems and has been demonstrated in non-surgical settings.[60, 61] With regard to surgical documentation, one small randomized trial of EHRs for hospitalized orthopedic surgery patients and several non-randomized comparative studies of templated electronic operative reports for a variety of surgical procedures and specialties have shown significant improvements in inclusion of diagnoses and critical elements for documentation of operative procedures, respectively. Few of these studies examined the time required for completion of documentation, although electronic operative reports were available in the medical record significantly earlier than dictated procedure notes. The content of narrative dictated operative reports is often inconsistent and incomplete.[62] Electronic operative reports have several additional advantages as data from discrete fields can be employed for research and determination of outcomes.[63] Thus, the improvements in documentation quality and benefits of data reuse are likely to outweigh the increased time for report generation in the long term, although further research is needed to prove this hypothesis.
Appropriate perioperative antibiotic administration and VTE prophylaxis have been the focus of surgical quality initiatives over the last several decades, and this review provides some evidence that HIT can improve this aspect of surgical practice. Several non-randomized comparative studies revealed that adjuncts to the EHR and CPOE, such as clinical decision support and computerized alerts could improve quality measure documentation and receipt of the appropriate medication for the appropriate length of time. Few studies, however, translate these process measures into improvements in clinical outcomes. A small, but statistically significant, decrease in the incidence of SSI and incidence of VTE was found in two studies.[28, 34]
Our review provides good evidence that computerized alerting systems within EHRs can improve surgical patient care. Reminders improved laboratory monitoring of transplant patients and prophylactic antibiotic dosing in the operating room, and CPOE effectively prohibited physicians from ordering inappropriate post-operative “prophylactic” antibiotics beyond the recommended time frame.[36] We believe computerized reminder systems could support a wide range of quality-improvement activities for surgical care. The widespread implementation of EHR and CPOE systems are an appropriate framework for the integration of further CDSS in various surgical specialties and practice settings. However, for these systems to be accepted and improve patient care, they will need to be well incorporated into clinical workflows, which have not been well studied in surgery.
Consumer health informatics is an emerging area of research. Evidence about the use of consumer-oriented HIT in surgical practice is too limited to offer strong recommendations, but this review did identify several important areas for future research. In 2004, patient access to electronic health records became a federal mandate, leading to the emergence of technologies such as patient portals.[55] Patient portals are web-based applications that provide a means for patients and families to interact with health care systems and access health information.[56] Our review identified two studies that demonstrated rapid adoption of patient portals by surgical providers and patients. However, the effects of these interactive and engagement technologies are unknown and should be the subject of future research.
Several studies showed that Internet-based health information resources for specific surgical problems and procedures are often incomplete and sometimes misleading, based on criteria developed by clinical or web experts. With the increasing use of Internet resources by both providers and patients, there are growing concerns about the quality and validity of the available information.[47, 64] Prior reviews have identified hundreds of invalidated instruments for measuring the quality of health information on the Internet.[65, 66] Consumer health information needs are poorly understood and understudied, and the value of a particular resource to a patient or caregiver may not be best measured by such criteria. This review identified one RCT that showed a decrease in the anxiety of the parents of children undergoing outpatient surgery after using a web-based educational intervention.[54] Future studies of consumer HIT should employ both high quality designs and consumer-focused outcomes to measure effectively the impact of such resources and tools in a specific context.
Our study has several limitations. First, our review only included literature available in the English language, and it is likely that relevant studies published in other languages were missed. Our research team is seeking collaborators to assist with inclusion of such studies in future work. Second, we did not define an explicit question to be answered by this review, as the quantity and nature of the available literature in the domain of surgery was not known. This review serves as one of the first comprehensive summaries of HIT applied to the domain of surgery in the information age and defines important gaps in knowledge and areas for future research. Finally, the paucity of data and heterogeneity of studies precluded a formal meta-analysis. As this field evolves and additional evidence becomes available, future reviews should address very specific effects and combine findings when appropriate.
Conclusions
In all areas of health care, including surgery, there has been rapid implementation and adoption of HIT by providers and patients. Existing large cross-sectional studies about the effects of HIT are confounded by variations in patient populations and practice patterns across clinical specialties. There is a paucity of data and overall low quality of evidence regarding HIT in surgical practice. We identified three consistent trends in the effects of these technologies in surgery including an improvement in the quality of surgical documentation, increased adherence to guidelines for medication administration, and improvements in patient care with provider alerts. Further research is needed to optimize the incorporation of electronic documentation, CPOE, and CDSS into surgical workflow and to evaluate the effects of HIT on surgical outcomes. In addition, more and better quality studies with consumer-focused outcomes are needed to evaluate the effects of web-based patient educational and engagement technologies to determine the impact of such resources on surgical patients.
Acknowledgements
Jamie Robinson was supported by the 5T15LM007450 training grant from the National Library of Medicine.
Footnotes
Author Contributions
GP Jackson conceived the work, reviewed articles, supervised the project, and assisted in manuscript preparation. H Huth assisted in review and selection of included studies. JR Robinson coordinated the review methods, reviewed articles, and prepared the manuscript. All authors reviewed and approved the final manuscript.
Disclosures
None of the authors have reported conflicts of interest related to the research.
Presentation February 3, 2016 at the 11th Annual Academic Surgical Congress
References
- 1.Institute of Medicine . Crossing the Quality Chasm: A New Health System for the 21st Century. National Academy Pr; Washington, DC: 2001. [Google Scholar]
- 2.Institute of Medicine . Key Capabilities of an Electronic Health Record System. National Academy Pr; Washington, DC: 2003. [Google Scholar]
- 3.Key Capabilities of an Electronic Health Record System. Institute of Medicine, Committee on Data Standards for Patient Safety Board on Health Care Services; Washington, DC: 2003. [Google Scholar]
- 4.Institute of Medicine . Health IT and Patient Safety Building Safer Systems for Better Care. National Academy Pr; Washington, DC: 2011. [PubMed] [Google Scholar]
- 5.DesRoches CMPM, Jha AK, editors. Robert Wood Johnson Foundation. Mathematica Policy Research aHSoPH Health Information Technology in the United States 2015. [Google Scholar]
- 6.Eliades GRM, Hueltenschmidt N, Singh K. Healthcare 2020. InsightsBain and Company. 2012 [Google Scholar]
- 7.Blumenthal D, Tavenner M. The "meaningful use" regulation for electronic health records. N Engl J Med. 2010;363:501–504. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- 8.2015 Edition Health Information Technology (Health IT) Certification Criteria, 2015 Edition Base Electronic Health Record (EHR) Definition, and ONC Health IT Certification Program Modifications. Final rule. Fed Regist. 2015;80:62601–62759. [PubMed] [Google Scholar]
- 9.Hsiao CJ, Hing E. Use and characteristics of electronic health record systems among office-based physician practices: United States, 2001-2013. NCHS Data Brief. 2014:1–8. [PubMed] [Google Scholar]
- 10.HealthIT.gov HealthIT.gov Dashboard. 2015 [Google Scholar]
- 11.Charles DGM, Furukawa MF. Adoption of Electronic Health Record Systems among U.S. Non-federal Acute Care Hospitals: 2008-2013. ONC Data Brief. 2014 May; No.16. [Google Scholar]
- 12.Jones SS, Rudin RS, Perry T, Shekelle PG. Health information technology: an updated systematic review with a focus on meaningful use. Ann Intern Med. 2014;160:48–54. doi: 10.7326/M13-1531. [DOI] [PubMed] [Google Scholar]
- 13.Bates DW, Leape LL, Cullen DJ, Laird N, Petersen LA, et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. Jama. 1998;280:1311–1316. doi: 10.1001/jama.280.15.1311. [DOI] [PubMed] [Google Scholar]
- 14.Bates DW, Teich JM, Lee J, Seger D, Kuperman GJ, et al. The impact of computerized physician order entry on medication error prevention. J Am Med Inform Assoc. 1999;6:313–321. doi: 10.1136/jamia.1999.00660313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144:742–752. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- 16.Goldzweig CL, Towfigh A, Maglione M, Shekelle PG. Costs and benefits of health information technology: new trends from the literature. Health Aff (Millwood) 2009;28:w282–293. doi: 10.1377/hlthaff.28.2.w282. [DOI] [PubMed] [Google Scholar]
- 17.Buntin MB, Burke MF, Hoaglin MC, Blumenthal D. The benefits of health information technology: a review of the recent literature shows predominantly positive results. Health Aff (Millwood) 2011;30:464–471. doi: 10.1377/hlthaff.2011.0178. [DOI] [PubMed] [Google Scholar]
- 18.Larsen RA, Evans RS, Burke JP, Pestotnik SL, Gardner RM, et al. Improved perioperative antibiotic use and reduced surgical wound infections through use of computer decision analysis. Infect Control Hosp Epidemiol. 1989;10:316–320. doi: 10.1086/646035. [DOI] [PubMed] [Google Scholar]
- 19.Evans RS, Pestotnik SL, Burke JP, Gardner RM, Larsen RA, et al. Reducing the duration of prophylactic antibiotic use through computer monitoring of surgical patients. DICP. 1990;24:351–354. doi: 10.1177/106002809002400401. [DOI] [PubMed] [Google Scholar]
- 20.Durieux P, Nizard R, Ravaud P, Mounier N, Lepage E. A clinical decision support system for prevention of venous thromboembolism: effect on physician behavior. Jama. 2000;283:2816–2821. doi: 10.1001/jama.283.21.2816. [DOI] [PubMed] [Google Scholar]
- 21.Stengel D, Bauwens K, Walter M, Kopfer T, Ekkernkamp A. Comparison of handheld computer-assisted and conventional paper chart documentation of medical records. A randomized, controlled trial. J Bone Joint Surg Am. 2004;86-a:553–560. doi: 10.2106/00004623-200403000-00014. [DOI] [PubMed] [Google Scholar]
- 22.Jacques P, St, Sanders N, Patel N, Talbot TR, Deshpande JK, et al. Improving timely surgical antibiotic prophylaxis redosing administration using computerized record prompts. Surgical infections. 2005;6:215–221. doi: 10.1089/sur.2005.6.215. [DOI] [PubMed] [Google Scholar]
- 23.O'Reilly M, Talsma A, VanRiper S, Kheterpal S, Burney R. An anesthesia information system designed to provide physician-specific feedback improves timely administration of prophylactic antibiotics. Anesth Analg. 2006;103:908–912. doi: 10.1213/01.ane.0000237272.77090.a2. [DOI] [PubMed] [Google Scholar]
- 24.Wax DB, Beilin Y, Levin M, Chadha N, Krol M, et al. The effect of an interactive visual reminder in an anesthesia information management system on timeliness of prophylactic antibiotic administration. Anesth Analg. 2007;104:1462–1466. doi: 10.1213/01.ane.0000263043.56372.5f. table of contents. [DOI] [PubMed] [Google Scholar]
- 25.Staes CJ, Evans RS, Rocha BH, Sorensen JB, Huff SM, et al. Computerized alerts improve outpatient laboratory monitoring of transplant patients. J Am Med Inform Assoc. 2008;15:324–332. doi: 10.1197/jamia.M2608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nair BG, Newman SF, Peterson GN, Wu WY, Schwid HA. Feedback mechanisms including real-time electronic alerts to achieve near 100% timely prophylactic antibiotic administration in surgical cases. Anesth Analg. 2010;111:1293–1300. doi: 10.1213/ANE.0b013e3181f46d89. [DOI] [PubMed] [Google Scholar]
- 27.Schwann NM, Bretz KA, Eid S, Burger T, Fry D, et al. Point-of-care electronic prompts: an effective means of increasing compliance, demonstrating quality, and improving outcome. Anesth Analg. 2011;113:869–876. doi: 10.1213/ANE.0b013e318227b511. [DOI] [PubMed] [Google Scholar]
- 28.Haut ER, Lau BD, Kraenzlin FS, Hobson DB, Kraus PS, et al. Archives of surgery. Vol. 147. Chicago, Ill: 2012. Improved prophylaxis and decreased rates of preventable harm with the use of a mandatory computerized clinical decision support tool for prophylaxis for venous thromboembolism in trauma; pp. 901–907. 1960. [DOI] [PubMed] [Google Scholar]
- 29.Yang P, Cao Y, Liu D, Bai Y, Pan F, et al. The effect of electronic medical record application on the length of stay in a Chinese general hospital: a department- and disease-focused interrupted time-series study. J Med Syst. 2014;38:53. doi: 10.1007/s10916-014-0053-x. [DOI] [PubMed] [Google Scholar]
- 30.Choi CK, Saberito D, Tyagaraj C, Tyagaraj K. Organizational performance and regulatory compliance as measured by clinical pertinence indicators before and after implementation of Anesthesia Information Management System (AIMS) J Med Syst. 2014;38:5. doi: 10.1007/s10916-013-0005-x. [DOI] [PubMed] [Google Scholar]
- 31.Pinto Thirukumaran C, Dolan JG, Reagan Webster P, Panzer RJ, Friedman B. The impact of electronic health record implementation and use on performance of the Surgical Care Improvement Project measures. Health Serv Res. 2015;50:273–289. doi: 10.1111/1475-6773.12191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Flatow VH, Ibragimova N, Divino CM, Eshak DSA, Twohig BC, et al. Quality Outcomes in the Surgical Intensive Care Unit after Electronic Health Record Implementation. Applied Clinical Informatics. 2015;6:611–618. doi: 10.4338/ACI-2015-04-RA-0044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hunt DL, Haynes RB, Hanna SE, Smith K. Effects of computer-based clinical decision support systems on physician performance and patient outcomes: a systematic review. Jama. 1998;280:1339–1346. doi: 10.1001/jama.280.15.1339. [DOI] [PubMed] [Google Scholar]
- 34.Webb AL, Flagg RL, Fink AS. Reducing surgical site infections through a multidisciplinary computerized process for preoperative prophylactic antibiotic administration. American journal of surgery. 2006;192:663–668. doi: 10.1016/j.amjsurg.2006.08.014. [DOI] [PubMed] [Google Scholar]
- 35.Liu SA, Chiu YT, Lin WD, Chen SJ. Using information technology to reduce the inappropriate use of surgical prophylactic antibiotic. Eur Arch Otorhinolaryngol. 2008;265:1109–1112. doi: 10.1007/s00405-008-0588-x. [DOI] [PubMed] [Google Scholar]
- 36.Haynes K, Linkin DR, Fishman NO, Bilker WB, Strom BL, et al. Effectiveness of an information technology intervention to improve prophylactic antibacterial use in the postoperative period. J Am Med Inform Assoc. 2011;18:164–168. doi: 10.1136/jamia.2009.002998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Appari A, Carian EK, Johnson ME, Anthony DL. Medication administration quality and health information technology: a national study of US hospitals. J Am Med Inform Assoc. 2012;19:360–367. doi: 10.1136/amiajnl-2011-000289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Van Sise MA, Chappelle J, Figueroa R. Improving the selection of recommended prophylactic antibiotics using an electronic medical record. Obstet Gynecol. 2012;120:1382–1385. doi: 10.1097/aog.0b013e318273754d. [DOI] [PubMed] [Google Scholar]
- 39.Classen DC, Evans RS, Pestotnik SL, Horn SD, Menlove RL, et al. The timing of prophylactic administration of antibiotics and the risk of surgical-wound infection. N Engl J Med. 1992;326:281–286. doi: 10.1056/NEJM199201303260501. [DOI] [PubMed] [Google Scholar]
- 40.Su HY, Ding DC, Chen DC, Lu MF, Liu JY, et al. Prospective randomized comparison of single-dose versus 1-day cefazolin for prophylaxis in gynecologic surgery. Acta Obstet Gynecol Scand. 2005;84:384–389. doi: 10.1111/j.0001-6349.2005.00583.x. [DOI] [PubMed] [Google Scholar]
- 41.Laflamme MR, Dexter PR, Graham MF, Hui SL, McDonald CJ. Efficiency, comprehensiveness and cost-effectiveness when comparing dictation and electronic templates for operative reports. AMIA Annu Symp Proc. 2005:425–429. [PMC free article] [PubMed] [Google Scholar]
- 42.Cowan DA, Sands MB, Rabizadeh SM, Amos CS, Ford C, et al. Electronic templates versus dictation for the completion of Mohs micrographic surgery operative notes. Dermatol Surg. 2007;33:588–595. doi: 10.1111/j.1524-4725.2007.33120.x. [DOI] [PubMed] [Google Scholar]
- 43.Park J, Pillarisetty VG, Brennan MF, Jarnagin WR, D'Angelica MI, et al. Electronic synoptic operative reporting: assessing the reliability and completeness of synoptic reports for pancreatic resection. Journal of the American College of Surgeons. 2010;211:308–315. doi: 10.1016/j.jamcollsurg.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 44.Hoffer DN, Finelli A, Chow R, Liu J, Truong T, et al. Structured electronic operative reporting: comparison with dictation in kidney cancer surgery. International journal of medical informatics. 2012;81:182–191. doi: 10.1016/j.ijmedinf.2011.11.008. [DOI] [PubMed] [Google Scholar]
- 45.Ghani Y, Thakrar R, Kosuge D, Bates P. 'Smart' electronic operation notes in surgery: an innovative way to improve patient care. Int J Surg. 2014;12:30–32. doi: 10.1016/j.ijsu.2013.10.017. [DOI] [PubMed] [Google Scholar]
- 46.Melloul E, Raptis DA, Oberkofler CE, Dutkowski P, Lesurtel M, et al. Donor information for living donor liver transplantation: where can comprehensive information be found? Liver Transpl. 2012;18:892–900. doi: 10.1002/lt.23442. [DOI] [PubMed] [Google Scholar]
- 47.Bruce-Brand RA, Baker JF, Byrne DP, Hogan NA, McCarthy T. Assessment of the quality and content of information on anterior cruciate ligament reconstruction on the internet. Arthroscopy. 2013;29:1095–1100. doi: 10.1016/j.arthro.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 48.Fast AM, Deibert CM, Hruby GW, Glassberg KI. Evaluating the quality of Internet health resources in pediatric urology. Journal of pediatric urology. 2013;9:151–156. doi: 10.1016/j.jpurol.2012.01.004. [DOI] [PubMed] [Google Scholar]
- 49.Sullivan TB, Anderson JT, Ahn UM, Ahn NU. Can Internet information on vertebroplasty be a reliable means of patient self-education? Clin Orthop Relat Res. 2014;472:1597–1604. doi: 10.1007/s11999-013-3425-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Corcelles R, Daigle CR, Talamas HR, Brethauer SA, Schauer PR. Assessment of the quality of Internet information on sleeve gastrectomy. Surg Obes Relat Dis. 2015;11:539–544. doi: 10.1016/j.soard.2014.08.014. [DOI] [PubMed] [Google Scholar]
- 51.Charnock D, Shepperd S, Needham G, Gann R. DISCERN: an instrument for judging the quality of written consumer health information on treatment choices. J Epidemiol Community Health. 1999;53:105–111. doi: 10.1136/jech.53.2.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Boyer C, Baujard V, Geissbuhler A. Evolution of health web certification through the HONcode experience. Stud Health Technol Inform. 2011;169:53–57. [PubMed] [Google Scholar]
- 53.Foundation HotN The commitment to reliable health and medical information on the internet. Health on the Net. 2015 [Google Scholar]
- 54.Fortier MA, Bunzli E, Walthall J, Olshansky E, Saadat H, et al. Web-based tailored intervention for preparation of parents and children for outpatient surgery (WebTIPS): formative evaluation and randomized controlled trial. Anesth Analg. 2015;120:915–922. doi: 10.1213/ANE.0000000000000632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Burke RP, Rossi AF, Wilner BR, Hannan RL, Zabinsky JA, et al. Transforming patient and family access to medical information: utilisation patterns of a patient-accessible electronic health record. Cardiol Young. 2010;20:477–484. doi: 10.1017/S1047951110000363. [DOI] [PubMed] [Google Scholar]
- 56.Baucom RB, Ousley J, Poulose BK, Rosenbloom ST, Jackson GP. Case report: patient portal versus telephone recruitment for a surgical research study. Appl Clin Inform. 2014;5:1005–1014. doi: 10.4338/ACI-2014-07-CR-0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Shenson JA, Cronin RM, Davis SE, Chen Q, Jackson GP. Rapid growth in surgeons' use of secure messaging in a patient portal. Surgical endoscopy. 2015 doi: 10.1007/s00464-015-4347-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Collen M, Ball M. The History of Medical Informatics in the United States. Springer-Verlag; London: 2015. [Google Scholar]
- 59.Shortliffe EH, Cimino JJ. Computer Applications in Health Care and Biomedicine. Springer-Verlag; London: 2014. Biomedical Informatics. [Google Scholar]
- 60.Kuhn T, Basch P, Barr M, Yackel T. Clinical documentation in the 21st century: executive summary of a policy position paper from the American College of Physicians. Ann Intern Med. 2015;162:301–303. doi: 10.7326/M14-2128. [DOI] [PubMed] [Google Scholar]
- 61.Cimino JJ. Improving the electronic health record--are clinicians getting what they wished for? Jama. 2013;309:991–992. doi: 10.1001/jama.2013.890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Harvey A, Zhang H, Nixon J, Brown CJ. Comparison of data extraction from standardized versus traditional narrative operative reports for database-related research and quality control. Surgery. 2007;141:708–714. doi: 10.1016/j.surg.2007.01.022. [DOI] [PubMed] [Google Scholar]
- 63.Edhemovic I, Temple WJ, de Gara CJ, Stuart GC. The computer synoptic operative report--a leap forward in the science of surgery. Annals of surgical oncology. 2004;11:941–947. doi: 10.1245/ASO.2004.12.045. [DOI] [PubMed] [Google Scholar]
- 64.Silberg WM, Lundberg GD, Musacchio RA. Assessing, controlling, and assuring the quality of medical information on the Internet: Caveant lector et viewor--Let the reader and viewer beware. Jama. 1997;277:1244–1245. [PubMed] [Google Scholar]
- 65.Purcell GP, Wilson P, Delamothe T. The quality of health information on the internet. As for any other medium it varies widely; regulation is not the answer. 2002;324:557–558. doi: 10.1136/bmj.324.7337.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gagliardi A, Jadad AR. Examination of instruments used to rate quality of health information on the internet: chronicle of a voyage with an unclear destination. BMJ (Clinical research ed.) 2002;324:569–573. doi: 10.1136/bmj.324.7337.569. [DOI] [PMC free article] [PubMed] [Google Scholar]