Abstract
Background
The benefit of therapeutic hypothermia (TH) in Acute Liver Failure (ALF) has not been previously demonstrated in a controlled fashion. This study aimed to determine the impact of TH on 21-day survival and complications in ALF patients at high risk for cerebral edema.
Methods
Retrospective cohort study of ALF patients in the US ALFSG with Grade III or IV hepatic encephalopathy. TH (32°C – 35°C) was used in 97 (8%) patients; 1135 (92%) not cooled were controls.
Results
Intracranial pressure (ICP) was monitored in 38 (40%) TH ALF patients (vs. 22% controls, p=0.0001). Rates of bleeding (12% in both), bloodstream (17% vs. 18) and tracheal infections (21% vs. 23%, p> 0.5 for all) were similar. Unadjusted 21-day overall (62% vs. 60%) and transplant-free survival (45 vs. 39%, p>0.4 for both) were similar. Multivariable models were created for acetaminophen (APAP) (n= 582) and non-APAP (n=613) patients. For APAP patients, MELD (Odds ratio 0.91 per increment; 95% CI 0.89–0.94, p <0.001) and vasopressors (OR 0.16; 0.11–0.24, p < 0.0001) were associated with decreased 21-day spontaneous survival. Survival was improved with TH in APAP patients aged < 25y (Age 25: OR 2.735; 95% CI 1.001 – 7.467) but worsened in 64y or older APAP patients (Age = 64: OR 0.167; 95%CI 0.028 – 0.999). For non-APAP patients, MELD (OR 0.93 per increment; 0.91–0.95, p < 0.0001) and vasopressors (OR 0.60; 0.40–0.90, p=0.01) were associated with worse outcomes while TH had no impact (p= 0.93).
Conclusions
Therapeutic hypothermia in ALF was not associated with increased bleeding or infections. While young APAP-ALF patients may benefit, TH did not consistently impact 21-day survival. A prospective trial is required to clarify the utility of TH in ALF patients.
Keywords: Acute liver failure, cerebral edema, fulminant hepatic failure, intracranial hypertension, therapeutic hypothermia
Introduction
Acute liver failure (ALF) is defined by hepatic encephalopathy (HE) and synthetic dysfunction within 26 weeks of the first symptoms of liver disease(1). The most common cause of ALF in North America is acetaminophen (APAP) (2, 3). Particularly in APAP-induced ALF, cerebral edema and intracranial hypertension (ICH) continue to be major causes of morbidity and mortality(4, 5). Medical interventions to reduce ICH might prevent brain injury; the presence of clinically significant ICH prior to emergency LT portends a higher likelihood of ischemic brain injury (6, 7). Reducing ICH may be undertaken using osmotic agents (mannitol or hypertonic saline)(8), control of blood pressure, ammonia-lowering therapies (e.g., hemofiltration(9)) and therapeutic hypothermia (TH) (10). While these interventions are frequently employed, it is not clear which are more effective. Indeed, multiple interventions may be initiated simultaneously in these patients.
Therapeutic cooling might protect against cerebral edema by various mechanisms: normalization of cerebral blood flow, decreased cerebral metabolic rate, decreased cytokine production and decreased conversion of glutamate to glutamine, the active osmole precipitating cerebral edema in astrocytes(11–13). This has been shown in animal and humans: decreased intracranial pressure (ICP), cerebral blood flow and increased cerebral perfusion pressure (CPP) have been demonstrated using moderate (32 – 35 C) hypothermia(10, 14). Despite the potential utility of TH, there are concerns that lowering core temperature might lead to increased bleeding events(15), microbial infections(16), cardiac dysrhythmias(17) and potentially reduced hepatic regeneration(18). Currently there are no controlled data examining the effect of TH in ALF and no evidence based guidelines for its use in these patients.
The aim of this study was to determine retrospectively the role and value of TH in prevention or management of cerebral edema in ALF in the large prospective ALFSG registry; whether TH impacted transplant-free survival compared to those not receiving TH (controls). Furthermore, we examined in this ALF cohort whether treatment with TH was associated with more complications (infection, bleeding, dysrhythmias) as suggested by the current literature.
MATERIALS AND METHODS
The reporting of this study followed the STROBE guideline (19).
Design and Setting
The ALF registry has prospectively collected clinical and laboratory data on over 2,300 patients with ALF over the past 15 years. In the present study, we focused on patients who had highest risk for cerebral edema or ICH, namely those with grade III or IV HE, by performing a retrospective cohort study of 1232 ALF patients with Grade III or IV HE enrolled into the US ALFSG registry between January 1998 and August 2013. While the use of TH was governed by local center protocol, we identified that ~ 8% (97/1232) of our study patients were treated with this intervention. All enrolling centers were tertiary academic centers and all but one were liver transplant centers. The Institutional Review Board at each participating center approved the ALFSG protocols. Because of HE in all patients, next of kin provided consent for study participation. Each center implemented monitoring and therapeutic interventions according to institutional standards of care. TH implied the use of an active cooling device (e.g., Arctic Sun™) with temperature target between 32–35C. The individual practicing clinician determined decisions regarding initiation and maintenance of TH and the type of active cooling device. Passive cooling (e.g. due to the use of renal replacement therapy (RRT)) did not meet criteria for TH within the ALFSG registry. While there were no study-wide protocols for application of TH across the US ALFSG sites, based on previously published US and UK literature some indications for TH may include hyperammonemia (ammonia > 150 µmol/L), listing for LT, meeting King’s College criteria, or presence of multisystem organ failure(20, 21).
Participants
Inclusion criteria were: 1) evidence of ALF according to the enrollment criteria for the ALFSG (see operational definitions) AND 2) age ≥18 years; and 3) Grade III or IV HE during the first seven days of study admission (West Haven Criteria)(22, 23). Exclusion criteria were: 1) Cirrhosis/acute on chronic liver failure; 2) patients < 18 years; and 3) HE coma grade 1 or 2.
Operational Definitions
For the purposes of this study, ALF was defined as INR ≥ 1.5 and HE within the first 26 weeks of liver disease in a patient with an acute hepatic insult (24). HE grade was defined by the West Haven Criteria (simplified) as follows; grade 1 ~ any alteration in mentation, grade 2 being somnolent or obtunded but easily rousable or presence of asterixis, grade 3 being rousable with difficulty and, grade 4: unresponsive to deep pain (22, 23).
Variables
The exposure of interest was use of active TH in patients with ALF (both APAP and non-APAP). The primary outcomes of interest were overall and spontaneous survival at 21 days (absence of transplant). Secondary outcomes included complications possibly attributed to or prevented by TH ~ infection (bacteremia, tracheal aspirates), bleeding (gastrointestinal or other), coagulopathy (requirement for hematological factors), cardiac dysrhythmias. Confounding factors, which may impact the primary outcome (mortality), included age, gender, etiology of ALF (APAP vs. non-APAP), requirement for organ support (vasopressors, mechanical ventilation [MV]), renal replacement therapy (RRT), and LT.
Data Sources and Collection
Data were collected prospectively as part of the US ALFSG and retrospectively analyzed. Prior to February 2010, each individual site sent case report forms to the University of Texas Southwestern for entry into a central database. Following this date, individual sites entered data electronically into a central database housed at the ALFSG Data Coordinating Center at the Medical University of South Carolina (Charleston, SC, USA). Registry data assessed in this study included demographics (age, race, sex), etiology of ALF, biochemistry, days of TH, daily minimum and maximum temperature, requirement for organ support during first 7 days, requirement for ICP related therapies and outcomes including receipt of LT and death at 21 days.
Statistical Analysis
Statistical analysis was performed using IBM SPSS version 19 (2010) and SAS version 9.2 (SAS Institute, North Carolina, USA). In the event of missing values, data were not replaced or estimated. Data were analyzed using descriptive statistics to characterize demographics and other clinical variables. Categorical variables were compared using the Chi-square test or Fisher’s exact test (< 5 cell counts). For continuous variables, normally distributed variables were reported as means with standard deviations (SD) and compared by Student’s t-test. Non-normally distributed continuous data were reported as medians with inter-quartile ranges (IQR) and compared by Wilcoxon rank sum test. Survival was defined as the dichotomous outcome, alive at 21-days (transplant and transplant free) after enrollment into the Registry. Transplant and transplant free refer to whether patients received LT during the first 21-days of follow-up. A two-sided significance level of <0.05 was used for all comparisons.
Multivariable analysis
In order to control for variables that may confound the effect of TH on 21-day spontaneous (transplant-free) survival multivariable logistic regression analyses were performed. Two separate logistic regression models to predict spontaneous survival at 21-days were performed. Transplant was considered as a composite endpoint with death at 21 days. The pre-specified prognostic variables included age at admission into the registry, gender, MELD score (admission), requirement during the 7-days post study admission of MV, vasopressors, RRT and TH. Model performance was assessed using the c-statistic and the Hosmer-Lemeshow test for goodness of fit. Multivariate associations are reported as odds ratios (OR) with 95% confidence limits.
RESULTS
General characteristics of 1232 ALF patients with Grade III/IV hepatic coma
Therapeutic hypothermia was used in 97 (8%) of patients with Grade III-IV HE. All patients were cooled between 32–35 C and for a median of 2 (1–3) days. Of 28 enrolling sites, 19 (68%) performed TH in at least one ALF patient; 24 patients were cooled for > 3 (4–7) days. The median target temperature was significantly cooler in TH patients (while being cooled) than controls (34.1 vs. 36.6 C, p < 0.0001).
Demographic, biochemical and therapeutic characteristics of treated patients (n=97) and controls (n=1135) are shown in Table 1. There were no significant differences in gender (71% female) and race (77% Caucasian) between groups. The most common etiology of ALF was APAP (TH 64%, Controls 47%, p= 0.04). Overall, TH patients were significantly younger (36 vs. 40 years; p < 0.03). On study admission (Table 1), hematological indicators were similar (platelet count TH 105 vs. controls 125; p=0.10). There were no differences between TH and control patients in admission serum creatinine (1.5 vs. 2.0 mg/dL; p=0.08), phosphate (mg/dL) (2.8 vs. 3.2, p= 0.06) and MELD scores (median 32 vs. 34, p=0.23). On admission, there were no differences in the presence of pupillary dilatation between TH patients and controls (22% vs. 18%, p=0.3).
Table 1.
Demographic, Clinical and Biochemical Parameters in 1232 ALF patients with Grade III/IV Hepatic encephalopathy treated with therapeutic hypothermia (N=97) and controls (n=1135).
| No Hypothermia (control) group (N=1135) |
Hypothermia group (N=97) |
|||||
|---|---|---|---|---|---|---|
| N | Number (%) or median (IQR) |
N | Number (%) or median (IQR) |
P value | ||
| Age | 1135 | 40.0 (29.0 – 51.0) | 97 | 36.0 (29.0 – 46.0) | 0.03 | |
| Sex (female) | 1135 | 801 (70.6%) | 97 | 75 (77.3%) | 0.16 | |
| Race | 1135 | 97 | 0.88 | |||
| White | 865 (76.2%) | 76 (78.4%) | ||||
| African-American | 174 (15.3%) | 14 (14.4%) | ||||
| Other | 96 (8.5%) | 7 (7.2%) | ||||
| Ethnicity | 1133 | 95 | 0.13 | |||
| Hispanic/Latino | 92 (8.1%) | 12 (12.6%) | ||||
| Not Hispanic/Latino | 1041 (91.9%) | 83 (87.4%) | ||||
| Etiology | 1134 | 96 | 0.04 | |||
| Acetaminophen | 537 (47.4%) | 61 (63.5%) | ||||
| Viral hepatitis | 111 (9.8%) | 9 (9.4%) | ||||
| Drug Induced | 112 (9.9%) | 6 (6.3%) | ||||
| Indeterminate | 148 (13.1%) | 7 (7.3%) | ||||
| Other | 226 (19.9%) | 13 (13.5%) | ||||
| Admission biochemistry | ||||||
| Hemoglobin (g/dl) | 1125 | 10.6 (9.3 – 12.2) | 97 | 10.0 (8.9 – 12.0) | 0.10 | |
| White Blood count (x109/L) | 1130 | 10.8 (7.1 – 15.8) | 97 | 10.0 (6.6 – 15.1) | 0.30 | |
| Platelet count (x109/L) | 1128 | 124.5 (77.5 – 187.0) | 97 | 105.0 (70.0 – 172.0) | 0.10 | |
| INR | 1116 | 2.8 (2.0 – 4.4) | 97 | 3.0 (2.1 – 4.8) | 0.60 | |
| AST (IU/L) | 1122 | 1648.0 (524.0 – 5775.0) | 95 | 2315.0 (576.0 – 6109.0) | 0.32 | |
| ALT (IU/L) | 1118 | 1954.0 (697.0 – 4441.0) | 94 | 2651.0 (963.0 – 4500.0) | 0.19 | |
| Bilirubin (mg/dl) | 1123 | 7.1 (3.9 – 19.1) | 94 | 6.8 (4.3 – 11.8) | 0.39 | |
| pH | 993 | 7.4 (7.3 – 7.5) | 91 | 7.4 (7.4 – 7.5) | 0.37 | |
| Ammonia (venous; µmol/L) | 353 | 108.0 (73.0 – 168.0) | 54 | 116.0 (79.0 – 170.0) | 0.25 | |
| Creatinine (mg/dL) | 1134 | 2.0 (1.0 – 3.4) | 96 | 1.5 (1.0 – 3.1) | 0.08 | |
| Lactate (mmol/L) | 668 | 5.0 (3.0 – 10.2) | 65 | 5.4 (3.1 – 9.1) | 0.84 | |
| Phosphate (mg/dL) | 989 | 3.2 (2.1 – 4.8) | 92 | 2.8 (2.0 – 4.1) | 0.06 | |
| PO2/FiO2 ratio | 865 | 3.3 (2.1 – 4.4) | 87 | 3.4 (2.4 – 4.5) | 0.56 | |
| MELD (admission) | 1105 | 33.6 (27.4 – 40.2) | 93 | 32.1 (26.7 – 38.2) | 0.23 | |
| Target Temperature* | 1135 | 36.6 (36.1 – 37.0) | 97 | 34.1 (32.9 – 35.3) | <0.0001 | |
| Organ support (7-days)** | ||||||
| Mechanical ventilation | 1135 | 975 (85.9%) | 97 | 97 (100.0%) | <0.0001 | |
| Vasopressors | 1135 | 491 (43.3%) | 97 | 59 (60.8%) | 0.0008 | |
| Renal Replacement therapy | 1135 | 451 (39.7%) | 97 | 61 (62.9%) | <0.0001 | |
| ICP therapies (7-days) | ||||||
| Mannitol | 1135 | 304 (26.8%) | 97 | 60 (61.9%) | <0.0001 | |
| Hypertonic saline | 1134 | 64 (5.6%) | 97 | 33 (34.0%) | <0.0001 | |
| Barbiturates | 1135 | 105 (9.3%) | 97 | 16 (16.5%) | 0.02 | |
| Sedatives | 1135 | 873 (76.9%) | 97 | 88 (90.7%) | 0.002 | |
| ICP Monitor Placement | 1002 | 218 (21.8%) | 97 | 38 (39.2%) | 0.0001 | |
| Blood products (7-days) | ||||||
| Red Blood Cells | 1135 | 530 (46.7%) | 97 | 50 (51.6%) | 0.36 | |
| Fresh Frozen Plasma | 1135 | 768 (67.7%) | 97 | 80 (82.5%) | 0.003 | |
| Recombinant VIIA | 1134 | 19 (1.7%) | 97 | 7 (7.2%) | 0.0003 | |
| Platelets | 1135 | 330 (29.1%) | 97 | 38 (39.2%) | 0.04 | |
- Abbreviations: INR, international normalized ratio; ALT, alanine aminotransferase; AST, aspartate aminotransferase; pO2, partial pressure of oxygen, FiO2, fraction of inspired oxygen.
- **Median target temperature where available in the No Hypothermia Group over all inpatient days (up to 7) and in the hypothermia group over all inpatient days actively treated with hypothermia.
- **7-days: Values refer to therapies at any time during the 7-days of study
During the first 7 study days, TH patients were more likely to be on RRT (63% vs. 40%), MV (100% vs. 86%) and vasopressors (61% vs. 43%, p < 0.001 for all). More TH patients received intracranial hypertension (ICH) directed therapies; including mannitol (62% vs. 27%), hypertonic saline (34% vs. 6%), barbiturates (17% vs. 9%) and sedatives (91% vs. 77%; p < 0.03 for all). More TH patients had ICP monitors in situ (39% vs. 22%, p=0.0001) and received blood products (fresh frozen plasma: 83% vs. 68%, p=0.003; platelets: 39% vs. 29%, p=0.04) than controls. Where data were available in those monitored with an ICP monitor, more TH patients had an ICP value over 25 mm Hg (ICH ~ (23/38 ~ 61% vs. 35/218 ~ 16%, p < 0.0001).
Outcomes in 1232 ALF patients with Grade III-IV HE
Complications and outcomes are shown in Table 2. During the first 7 days of study, TH patients were more likely to have cardiac arrhythmias (38% vs. 27%, p=0.03) but not when considering arrhythmias (n=29) following initiation of TH (28% vs. 27%, p=0.9). More TH patients had abnormalities of chest radiograph (87% vs. 77%, p=0.02) than controls. Though more TH patients had an abnormal head CT compared with controls the difference was not statistically significant (53% vs. 41%, p=0.08). In addition, there were no significant differences in other complications (seizures, GI bleeding, bacteremia, tracheal aspirate infection, p >0.1 for all comparisons). In 12 TH patients who developed GI bleeding, most of the bleeding events (n=10, 83%) occurred following initiation of TH. In comparing 24 patients receiving TH for > 3 days to those who received TH for less than 3 days (n=73) there were no significant differences in arrhythmias (38% vs. 37, p=0.94), bloodstream (29 vs. 12%, p=0.07) and tracheal infections (33 vs. 16%, p=0.09). In comparing 29 patients who had recorded temperatures below 33 °C for at least on day vs. 68 patients who were not there were no significant differences in arrhythmias (52% vs. 32%, p=0.07) and bloodstream infections (28 vs. 12%, p=0.07) but significantly more tracheal infections (35 vs. 15%, p=0.03).
Table 2.
Outcomes of 1232 Acute Liver Failure Patients with Grade III/IV Hepatic Encephalopathy treated with (n=97) or without (n=1135) Therapeutic Hypothermia.
| No Hypothermia Control Group (N=1135) |
Hypothermia group (N=97) |
|||||
|---|---|---|---|---|---|---|
| N | Number (%) | N | Number (%) | P value | ||
| ICU Complications (7-days) | ||||||
| Seizures | 1135 | 93 (8.2%) | 97 | 13 (13.4%) | 0.08 | |
| Arrhythmias | 1135 | 310 (27.3%) | 97 | 37 (38.1%) | 0.03* | |
| Gastrointestinal bleeding | 1135 | 138 (12.2%) | 97 | 12 (12.4%) | 0.95 | |
| Acute Respiratory Distress Syndrome | 1134 | 24 (2.1%) | 97 | 4 (4.1%) | 0.20 | |
| Abnormal CT of head | 319 | 132 (41.4%) | 80 | 42 (52.5%) | 0.08 | |
| Abnormal Chest X-ray | 1091 | 837 (76.7%) | 94 | 82 (87.2%) | 0.02 | |
| Bacteremia/Blood stream infection | 1135 | 207 (18.2%) | 97 | 16 (16.5%) | 0.67 | |
| Tracheal aspirate infection | 1135 | 264 (23.3%) | 97 | 20 (20.6%) | 0.55 | |
| Listed for LT | 1132 | 452 (39.9%) | 96 | 42 (43.8%) | 0.46 | |
| Received LT | 1129 | 277 (24.5%) | 97 | 17 (17.5%) | 0.12 | |
| Time to Hospital Discharge | ||||||
| From enrollment to home/other facility (days) | 439 | 12.0 (8.0 – 18.0) | 35 | 16.0 (11.0 – 20.0) | 0.03 | |
| 21-day spontaneous survival | 1135 | 446(39.3%) | 97 | 44 (45.4%) | 0.24 | |
| Overall Survival | 1135 | 679 (59.8%) | 97 | 60 (61.9%) | 0.70 | |
| Acetaminophen | ||||||
| Transplanted | 533 | 65 (12.2%) | 61 | 6 (9.8%) | 0.59 | |
| 21 day spontaneous survival | 537 | 298 (55.5%) | 61 | 35 (57.4%) | 0.78 | |
| 21 day overall survival | 537 | 354 (65.9%) | 61 | 41(67.2%) | 0.84 | |
| Non-acetaminophen | ||||||
| Transplanted | 596 | 212 (35.6%) | 36 | 11 (30.6%) | 0.54 | |
| 21 day spontaneous survival | 598 | 148 (24.8%) | 36 | 9 (25%) | 0.90 | |
| 21 day overall survival | 598 | 325 (54.3%) | 36 | 19 (52.8%) | 0.85 | |
- *When comparing arrhythmias following initiation of TH, there was no significant difference between the two groups (control 27% vs. TH 28%, p=0.9).
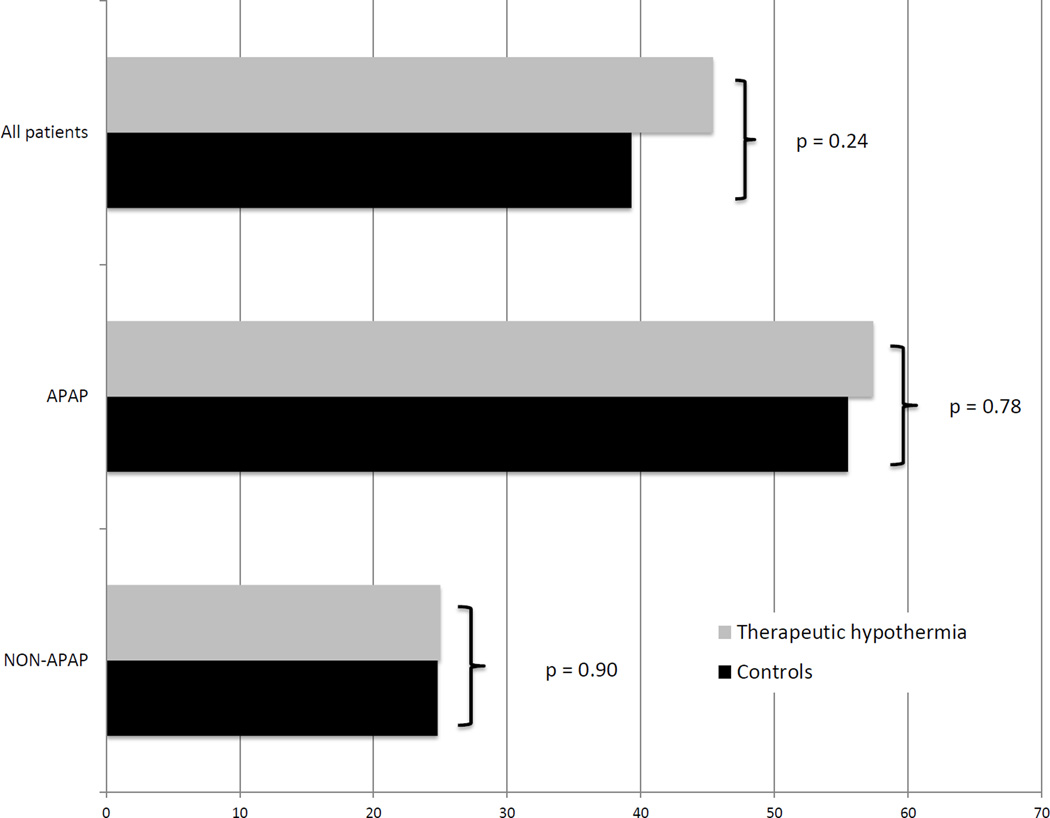
TH was used slightly more often in patients who were listed for LT (44% vs. 40%) and slightly less receiving TH received a LT (18% vs. 25%), but these differences were not statistically significant (p > 0.10 for both, see Table 2). Overall 21-day spontaneous survival was similar between TH patients and controls when all patients were included (45% vs. 39%, p= 0.24), and did not change when only APAP (57 vs. 56%, p=0. 78) or non-APAP (25% vs. 25%, p=0.90;see Figure 1) patients were considered. In the TH group, 11 (15%) died of neurological complications (cerebral edema or intracranial hemorrhage) compared with 105 (14%), p-value=0.75) in the control group.
Figure 1.
- All patients: Controls= 1135, Therapeutic Hypothermia (TH) =97 (p= 0.24)
- Acetaminophen (APAP) patients: Controls = 537, TH=61 (p= 0.78)
- Non-acetaminophen (non-APAP) patients: Controls= 598, TH=36 (p= 0.90)
Multivariable analysis of APAP-induced ALF patients
Within the study population, rates of LT (12% vs.34 %, p < 0.0001) and 21-day mortality (34% vs. 46%, p <0.0001) differed between APAP and non-APAP patients. The cohort was therefore stratified to APAP and non-APAP etiology of ALF to assess adjusted transplant-free survival by controlling for confounding factors. The APAP-ALF model included 582 patients (16 subjects were excluded due to missing data for at least one prognostic variable). Multivariable logistic regression results are shown in Table 3. The c-statistic (i.e., how well the model distinguishes between transplant-free survivors and transplanted/non-survivors at 21 days) was 0.812 (good predictive accuracy). Increasing admission MELD (Odds Ratio: OR 0.91 (95% CI 0.89–0.94 per increment); p <0.0001) and requirement for vasopressors within 7 days (OR 0.16 (0.11–0.24), p < 0.0001) were significantly associated with decreased 21-day transplant free (spontaneous) survival after controlling for confounding factors. RRT and MV were not included in the final model due to colinearity with other variables. Gender was not significant in the final model. A qualitative interaction effect was found between age and TH (p=0.023). When accounting for other factors, younger APAP patients were more likely to spontaneously survive to 21 days when treated with TH and older APAP patients were less likely to spontaneously survive when treated with TH (see Supplimentary Table 1). The odds ratio is > 1 (protective, does not cross unity) for those aged 18–25 (n=101) (Age 25: OR: 2.735 (1.001 – 7.467)). The odds ratio is < 1 (deleterious, does not cross unity) for those over 63 (n=13) (Age 64: OR: 0.167 (0.028 – 0.999)).
Table 3.
Multivariable Analysis: Predictors of 21-day spontaneous survival in 582 patients with acetaminophen-induced Acute Liver Failure.
| Univariate (N=598) | Multivariate (N=582, c=0.812) | |||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | p-value | Odds Ratio | 95% CI | p-value | |
| Age | 0.998 | 0.986 – 1.011 | 0.79 | *** | ||
| Male | 0.766 | 0.514 – 1.143 | 0.19 | 1.350 | 0.815 – 2.239 | 0.24 |
| Mechanical ventilation | 0.199 | 0.096 – 0.413 | <0.0001* | |||
| Renal replacement therapy | 0.491 | 0.354 – 0.682 | <0.0001* | |||
| Vasopressors | 0.154 | 0.108 – 0.221 | <0.0001 | 0.164 | 0.111 – 0.244 | <0.0001 |
| MELD | 0.912 | 0.893 – 0.931 | <0.0001 | 0.913 | 0.893 – 0.935 | <0.0001 |
| Hypothermia | 1.075 | 0.629 – 1.836 | 0.79 | *** | ||
| Age*hypothermia | 0.024 | |||||
- *Ventilator and Renal replacement therapy were co-linear with vasopressors and MELD and not included in final model
- Final model included age, gender, vasopressors, MELD and hypothermia
- 16 patients had missing data
- Variables included in final model if significant on univariable logistic regression included MELD on admission and vasopressors during 7 days in study
- The multivariable model had a c-statistic of 0.812, Hosmer-Lemeshow p=0.9125
- When adjusting for other confounding factors, younger APAP patients were more likely to spontaneously survive to 21 days when treated with TH and older APAP patients were less likely to spontaneously survive when treated with TH. The odds ratio is > 1 (protective, does not cross unity) for those aged 18–25 (Age 25: OR: 2.735 (1.001 – 7.467)). The odds ratio is < 1 (deleterious, does not cross unity) for those over 64 (Age 64: OR: 0.167 (0.028 – 0.999)) (see Supplementary file eTable 1)
Multivariable analysis of 613 Non-Acetaminophen-induced ALF patients
Multivariable logistic regression results of 613 non-APAP ALF patients are shown in Table 4 (21 patients had missing data). The model c-statistic was 0.70. Male gender (OR 1.618 [1.083, 22.146]) was independently associated with improved 21-day transplant free survival. Requirement for vasopressors (OR 0.60 [0.40, 0.904]), and increased MELD (OR 0.929 [0.906, 0.952]) were associated with significantly decreased 21-day transplant-free survival. Age (p=0.11 per year) and hypothermia (p=0.93) were not significantly associated with 21-day transplant-free survival in Non-APAP ALF patients after controlling for confounding factors.
Table 4.
Multivariable Analysis: Predictors of 21-day spontaneous survival in 613 patients with non-acetaminophen-induced Acute Liver Failure.
| Univariate (N=632) | Multivariate (N=613, c=0.700) | |||||
|---|---|---|---|---|---|---|
| Variable | Odds Ratio | 95% CI | p-value | Odds Ratio |
95% CI | p-value |
| Age | 0.984 | 0.972 – 0.996 | 0.0086 | 0.99 | 0.977 – 1.002 | 0.11 |
| Male | 1.291 | 0.893 – 1.867 | 0.17 | 1.618 | 1.083 – 2.416 | 0.019 |
| Mechanical ventilation | 0.837 | 0.518 – 1.350 | 0.47 | |||
| Renal replacement therapy | 0.861 | 0.592 – 1.253 | 0.44 | |||
| Vasopressors | 0.519 | 0.355 – 0.757 | 0.0007 | 0.602 | 0.4 – 0.904 | 0.014 |
| MELD | 0.929 | 0.907 – 0.952 | <0.001 | 0.929 | 0.906 – 0.952 | <0.0001 |
| Hypothermia | 1.051 | 0.481 – 2.293 | 0.90 | 0.962 | 0.394 – 2.347 | 0.93 |
- Final model included age, gender, vasopressors, MELD and hypothermia
- 19 patients had missing data
- The multivariable model had a c-statistic of 0.70, Hosmer-Lemeshow p=0.1577
DISCUSSION
Summary of Key Results
In this retrospective study we aimed to evaluate a large multi-center experience with TH (n=97) in the treatment of patients with ALF with advanced (III/IV) HE (total cohort n=1232). TH was used infrequently, in only ~8% of registrants. It was overall not associated with increased bleeding or infectious complications. TH potentially increased infection rates in those with recorded temperatures below 33 °C. TH did not appear to improve overall and transplant-free survival. ICP monitoring was not universally used in TH patients (~ 40%). After controlling for confounding by severity of illness (MELD, organ support), TH was not significantly associated with 21-day spontaneous survival in non-APAP patients. In APAP patients, TH may potentially be associated with benefit in patients less than 26 years of age.
Comparison with Previous Literature
This ALF cohort (TH and control patients) shared similar demographics with all patients entering into the overall ALFSG registry and with other series from North America and Europe; most were female, young, and APAP was the most common etiology. Patients who received TH were significantly younger than controls (36 versus 40 years, p=0.03) and were more likely to be diagnosed with APAP-induced ALF (64% vs. 47%, p=0.04). The higher percent of TH use in APAP cases may be explained by the ‘hyperacute’ nature of ALF in patients with this etiology of injury where progression of liver injury/multi-organ dysfunction often occurs very rapidly and where ICH is thought to be more frequent(1). Similar to our findings, Bernal and colleagues have previously reported that patients with the highest risk of clinically significant ICH had high serum ammonia levels, required RRT, were hemodynamically unstable (required vasopressors) and were younger (20). In our cohort, patients who underwent TH also had increased requirements for RRT and vasopressors during the first 7 days. Overall, TH did not affect outcomes, but its selective use in those thought to be at highest risk: under 26 years of age with acetaminophen overdose, bears further study.
The severity of illness between the TH and control group was similar when examined by MELD score or by hematological parameters. However, TH patients were on RRT and required vasopressor support, and were on MV more frequently than controls, suggesting more severe multi-organ systems failure not captured by MELD in these individuals. That this was likely true is reflected in the more frequent use of ICH directed therapies as well as the reporting of a higher frequency of an abnormal CT of the brain in patients in the TH group. Thus, it was not surprising that more TH patients had ICP monitors used than controls (39% vs. 22%, p=0.0001) given the higher likelihood these patients had evidence for, or might be expected to have, cerebral edema. Unfortunately, we can only speculate on this point, as we were unable to objectively determine in those without ICP monitoring whether increased ICP was indeed present. TH patients more frequently received blood products (fresh frozen plasma: 83% vs. 68%; platelets: 39% vs. 29%) than controls (p < 0.05 for both). While it is plausible that the use of the blood products was due to more frequent ICP monitor placement in TH patients and the perception of the need to correct the coagulation abnormalities, there were no differences amongst TH patients with (n=38) and without (n=59) ICP monitor in situ regarding use of fresh frozen plasma (18 vs. 17%, p=0.85) or platelets (58% vs. 63%) during 7 days of inpatient study.
Despite animal(11–13) and uncontrolled human data(10, 14) suggesting a potential benefit of TH in mitigating ICH in ALF, our study failed to show a consistent measurable benefit for TH on overall survival. While an interaction term was observed between age and TH for 21-day spontaneous survival in APAP-ALF patients suggesting a possible benefit in patients aged ≤ 25 (OR/95% CI > 1), this study did not show a consistent benefit of TH in other groups of either APAP or non-APAP ALF patients, after adjusting for confounding by severity of illness. These results are consistent with recent findings in the anoxic brain injury population, where initial studies of TH following cardiac arrest showed benefit(25, 26), but a more recent larger study by Nielsen and colleagues concluded that cooling to a core body temperature of 33° C yielded no significant improvement in outcome compared to 36°C(27). Hence, while it is well accepted that hyperthermia portends a worse outcome in ALF patients at risk for ICH, it is possible that more-than-moderate TH may not necessarily yield additive benefit over normothermia.
As the safety of using TH for ALF patients has previously been called into question, we specifically examined the frequency of complications in this cohort as granular data was captured in our case report forms. While there have been theoretical concerns of inhibition of hepatic regeneration(18), infection, bleeding and arrhythmias have been cited as more significant concerns. Regarding hepatic regeneration, almost half (45.4%) of the patients undergoing TH in this cohort were able to survive without the need of liver transplant. A recent meta-analysis by Geurts and colleagues revealed that while overall rates of infection were similar, general critical care patients receiving TH had higher rates of pneumonia and sepsis/bacteremia(16). In our study, rates of bloodstream infection and tracheal infection were not different between ALF patients receiving TH and controls. Furthermore despite concerns of potentially exacerbating coagulopathy(15) we did not observe differences in gastrointestinal bleeding rates between treatment groups. In addition, while there were significantly more cardiac arrhythmias identified in our ALF patients treated with TH (p=0.03), there was no significant difference when considering arrhythmias occurring following TH initiation (p=0.9). Finally, though no survival benefit could be demonstrated, TH was well tolerated with few adverse events.
Study limitations
Our study has limitations that warrant consideration. First, it is a retrospective analysis of prospectively collected data, thereby potentially predisposed to selection bias. Individual centers vary in volume and made independent decisions about listing for LT, insertion of an ICPM, and use of TH. The practicing clinician made decisions about initiation and discontinuation of TH. While common indications for TH described in the methods are based on recent recommendations from data from King’s College Hospital(20) and the US ALFSG(21), identifying patients at highest risk of cerebral edema, both of these studies were published after this cohort began. Patients were not assigned randomly to receive TH and it is possible that TH was undertaken in sicker patients (i.e. higher risk of cerebral edema) as patients in the TH group also received more ICP-directed therapies, had more abnormal findings on CT of the brain and had higher use of vasopressor agents. We attempted to control for confounding by performing multivariable analysis accounting for severity of liver dysfunction (MELD) and multi-organ failure (requirement for vasopressors, RRT and MV). SOFA and APACHE II could not be accurately calculated due to lack of detailed information on vasopressor doses (SOFA) and GCS (APACHE II; only hepatic coma grade available).
Because each center determined its own protocol, there was no uniformity in the timing or parameters for use of TH amongst centers or even at a center over time given that the study period was over 15 years. However, despite these limitations, we were able to observe whether TH was used with or without ICP monitoring, and examine whether the use of this intervention was associated with changes in survival at 21 days or with increased complications during the 7-day period of data collection on study entry.
To unequivocally answer these issues of bias, a prospective randomized study with standardized management protocols would be required. While no prospective studies have been published to date, a prospective randomized multicenter European Study is ongoing. Hence in the absence of published prospective controlled data in patients with ALF, the data presented largely suggests no benefit of TH, but also no harm.
CONCLUSIONS
In ALF patients with high-grade hepatic coma, TH appears safe and was not associated with increased bleeding or infectious complications. No differences in overall and transplant free survival in ALF patients with high grade HE were evident between the groups, even after adjusting for confounding factors related to severity of illness, however a subset of young patients with APAP etiology for ALF might benefit from TH. ICP monitoring was not universally used in patients receiving TH in this cohort (~ 40%). While our results cannot conclusively confirm or refute the utility of TH in ALF patients, prospective studies are awaited to conclusively account for confounding by etiology and illness severity.
Supplementary Material
Acknowledgments
This study was funded by National Institutes of Health grant (DK U-01 58369) for the United States Acute Liver Failure Study Group provided by the National Institute of Diabetes and Digestive and Kidney Diseases. Members and institutions participating in the Acute Liver Failure Study Group 1998–2011 are as follows: W.M. Lee, M.D. (Principal Investigator); Anne M. Larson, M.D., Iris Liou, M.D., University of Washington, Seattle, WA; Timothy Davern, M.D., University of California, San Francisco, CA (current address: California Pacific Medical Center, San Francisco, CA), Oren Fix, M.D., University of California, San Francisco; Michael L.Schilsky, M.D., Cary Caldwell, M.D. and Sukru Emre M.D.,Yale University, New Haven, CT; Timothy McCashland, M.D., University of Nebraska, Omaha, NE; J. Eileen Hay, M.B.B.S., Mayo Clinic, Rochester, MN; Natalie Murray, M.D., Baylor University Medical Center, Dallas, TX; A. Obaid S. Shaikh, M.D., University of Pittsburgh, Pittsburgh, PA; Andres Blei, M.D., Northwestern University, Chicago, IL (deceased), Daniel Ganger, M.D., Northwestern University, Chicago, IL; Atif Zaman, M.D., University of Oregon, Portland, OR; Steven H.B. Han, M.D., University of California, Los Angeles, CA; Robert Fontana, M.D., University of Michigan, Ann Arbor, MI; Brendan McGuire, M.D., University of Alabama, Birmingham, AL; Raymond T. Chung, M.D., Massachusetts General Hospital, Boston, MA; Alastair Smith, M.B., Ch.B., Duke University Medical Center, Durham, NC; Robert Brown, M.D., Cornell/Columbia University, New York, NY; Jeffrey Crippin, M.D., Washington University, St Louis, MO; Edwin Harrison, Mayo Clinic, Scottsdale, AZ; Adrian Reuben, M.B.B.S., Medical University of South Carolina, Charleston, SC; Santiago Munoz, M.D., Albert Einstein Medical Center, Philadelphia, PA; Rajender Reddy, M.D., University of Pennsylvania, Philadelphia, PA; R. Todd Stravitz, M.D., Virginia Commonwealth University, Richmond, VA; Lorenzo Rossaro, M.D., University of California Davis, Sacramento, CA; Raj Satyanarayana, M.D., Mayo Clinic, Jacksonville, FL; and Tarek Hassanein, M.D., University of California, San Diego, CA. The University of Texas Southwestern Administrative Group included Grace Samuel, Ezmina Lalani, Carla Pezzia, and Corron Sanders, Ph.D., Nahid Attar, Linda S. Hynan, Ph.D., and the Medical University of South Carolina Data Coordination Unit included Valerie Durkalski, Ph.D., Wenle Zhao, Ph.D., Catherine Dillon, Holly Battenhouse and Tomoko Goddard.
Special acknowledgement to Dr. Valerie Durkalski for statistical and manuscript advice.
Abbreviations
- ALF
Acute Liver Failure
- APAP
Acetaminophen
- CRRT
Continuous renal replacement therapy
- HBV
Hepatitis B
- HE
Hepatic Encephalopathy
- ICH
Intracranial hypertension
- ICP
Intracranial Pressure
- ICPM
Intracranial Pressure monitor/monitoring
- ICU
Intensive Care Unit
- LT
Liver transplant
- MELD
Model for End-stage Liver Disease
- MV
Mechanical ventilation
- RRT
Renal replacement therapy
- TH
Therapeutic hypothermia
- US ALFSG
United States Acute Liver Failure Study Group
Footnotes
Conflict of interest: CJK, RTS, HB, WML and MLS have no conflicts of interest. All authors do not have any competing financial interests.
Format: This paper followed the STROBE guideline for reporting retrospective studies (BMJ 2007).
Presentations: This study was presented in poster form at the European Association for the Study of Liver (EASL) International Liver Congress (ILC 2014) in London, UK on April 10th, 2014.
Contributions:
C.J.K. – Performed data analysis and interpretation, drafted and revised the final manuscript.
R.T.S. – Participated in the design of the study, and significantly revised the final manuscript.
H.B.- Participated in study design, performed statistical analysis and significantly edited the manuscript.
W.M.L.- Principal investigator of the overall US ALFSG who developed the initial registry and significantly revised the manuscript.
M.L.S. ~ Conceived the idea for the study, contributed to data analysis and interpretation and drafting and revisions of the final manuscript
All authors have reviewed and approved the final manuscript.
W.M.L., the principal investigator of the overall US ALFSG will provide access to source data upon request.
Contributor Information
Constantine J. Karvellas, Email: dean.karvellas@ualberta.ca.
R. Todd Stravitz, Email: rstravit@hsc.vcu.edu.
Holly Battenhouse, Email: battenho@musc.edu.
William M. Lee, Email: william.lee@utsouthwestern.edu.
Michael L. Schilsky, Email: michael.schilsky@yale.edu.
REFERENCES
- 1.O’Grady JG, Williams R. Classification of acute liver failure. Lancet. 1993;342(8873):743. [PubMed] [Google Scholar]
- 2.Fagan E, Wannan G. Reducing paracetamol overdoses. BMJ. 1996;313(7070):1417–1418. doi: 10.1136/bmj.313.7070.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Larson AM, Polson J, Fontana RJ, Davern TJ, Lalani E, Hynan LS, et al. Acetaminophen-induced acute liver failure: results of a United States multicenter, prospective study. Hepatology. 2005;42(6):1364–1372. doi: 10.1002/hep.20948. [DOI] [PubMed] [Google Scholar]
- 4.Ware AJ, D’Agostino AN, Combes B. Cerebral edema: a major complication of massive hepatic necrosis. Gastroenterology. 1971;61(6):877–884. [PubMed] [Google Scholar]
- 5.Bernal W, Wendon J. Acute liver failure; clinical features and management. Eur J Gastroenterol Hepatol. 1999;11(9):977–984. doi: 10.1097/00042737-199909000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Lidofsky SD, Bass NM, Prager MC, Washington DE, Read AE, Wright TL, et al. Intracranial pressure monitoring and liver transplantation for fulminant hepatic failure. Hepatology. 1992;16(1):1–7. doi: 10.1002/hep.1840160102. [DOI] [PubMed] [Google Scholar]
- 7.Davies MH, Mutimer D, Lowes J, Elias E, Neuberger J. Recovery despite impaired cerebral perfusion in fulminant hepatic failure. Lancet. 1994;343(8909):1329–1330. doi: 10.1016/s0140-6736(94)92471-6. [DOI] [PubMed] [Google Scholar]
- 8.Murphy N, Auzinger G, Bernel W, Wendon J. The effect of hypertonic sodium chloride on intracranial pressure in patients with acute liver failure. Hepatology. 2004;39(2):464–470. doi: 10.1002/hep.20056. [DOI] [PubMed] [Google Scholar]
- 9.Slack AJ, Auzinger G, Willars C, Dew T, Musto R, Corsilli D, et al. Ammonia clearance with haemofiltration in adults with liver disease. Liver international : official journal of the International Association for the Study of the Liver. 2014;34(1):42–48. doi: 10.1111/liv.12221. [DOI] [PubMed] [Google Scholar]
- 10.Jalan R, Olde Damink SW, Deutz NE, Hayes PC, Lee A. Moderate hypothermia in patients with acute liver failure and uncontrolled intracranial hypertension. Gastroenterology. 2004;127(5):1338–1346. doi: 10.1053/j.gastro.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 11.Cordoba J, Crespin J, Gottstein J, Blei AT. Mild hypothermia modifies ammonia-induced brain edema in rats after portacaval anastomosis. Gastroenterology. 1999;116(3):686–693. doi: 10.1016/s0016-5085(99)70191-5. [DOI] [PubMed] [Google Scholar]
- 12.Rose C, Michalak A, Pannunzio M, Chatauret N, Rambaldi A, Butterworth RF. Mild hypothermia delays the onset of coma and prevents brain edema and extracellular brain glutamate accumulation in rats with acute liver failure. Hepatology. 2000;31(4):872–877. doi: 10.1053/he.2000.5923. [DOI] [PubMed] [Google Scholar]
- 13.Chatauret N, Zwingmann C, Rose C, Leibfritz D, Butterworth RF. Effects of hypothermia on brain glucose metabolism in acute liver failure: a H/C-nuclear magnetic resonance study. Gastroenterology. 2003;125(3):815–824. doi: 10.1016/s0016-5085(03)01054-0. [DOI] [PubMed] [Google Scholar]
- 14.Jalan R, SW OD, Deutz NE, Lee A, Hayes PC. Moderate hypothermia for uncontrolled intracranial hypertension in acute liver failure. Lancet. 1999;354(9185):1164–1168. doi: 10.1016/s0140-6736(98)12440-6. [DOI] [PubMed] [Google Scholar]
- 15.Forman KR, Wong E, Gallagher M, McCarter R, Luban NL, Massaro AN. Effect of temperature on thromboelastography and implications for clinical use in neonates undergoing therapeutic hypothermia. Pediatric research. 2014 doi: 10.1038/pr.2014.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Geurts M, Macleod MR, Kollmar R, Kremer PH, van der Worp HB. Therapeutic hypothermia and the risk of infection: a systematic review and meta-analysis. Critical care medicine. 2014;42(2):231–242. doi: 10.1097/CCM.0b013e3182a276e8. [DOI] [PubMed] [Google Scholar]
- 17.Kim F, Nichol G, Maynard C, Hallstrom A, Kudenchuk PJ, Rea T, et al. Effect of prehospital induction of mild hypothermia on survival and neurological status among adults with cardiac arrest: a randomized clinical trial. JAMA : the journal of the American Medical Association. 2014;311(1):45–52. doi: 10.1001/jama.2013.282173. [DOI] [PubMed] [Google Scholar]
- 18.Munoz SJ. Hypothermia may impair hepatic regeneration in acute liver failure. Gastroenterology. 2005;128(4):1143–1144. doi: 10.1053/j.gastro.2005.02.048. author reply 4–5. [DOI] [PubMed] [Google Scholar]
- 19.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335(7624):806–808. doi: 10.1136/bmj.39335.541782.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bernal W, Hall C, Karvellas CJ, Auzinger G, Sizer E, Wendon J. Arterial ammonia and clinical risk factors for encephalopathy and intracranial hypertension in acute liver failure. Hepatology. 2007;46(6):1844–1852. doi: 10.1002/hep.21838. [DOI] [PubMed] [Google Scholar]
- 21.Stravitz RT, Kramer AH, Davern T, Shaikh AO, Caldwell SH, Mehta RL, et al. Intensive care of patients with acute liver failure: recommendations of the U.S. Acute Liver Failure Study Group. Critical care medicine. 2007;35(11):2498–2508. doi: 10.1097/01.CCM.0000287592.94554.5F. [DOI] [PubMed] [Google Scholar]
- 22.Conn HO, Lieberthal MM, editors. The hepatic coma syndromes and lactulose. Baltimore: Williams & Wilkins; 1979. [Google Scholar]
- 23.Atterbury CE, Maddrey WC, Conn HO. Neomycin-sorbitol and lactulose in the treatment of acute portal-systemic encephalopathy. A controlled, double-blind clinical trial. Am J Dig Dis. 1978;23(5):398–406. doi: 10.1007/BF01072921. [DOI] [PubMed] [Google Scholar]
- 24.O’Grady JG, Schalm SW, Williams R. Acute liver failure: redefining the syndromes. Lancet. 1993;342(8866):273–275. doi: 10.1016/0140-6736(93)91818-7. [DOI] [PubMed] [Google Scholar]
- 25.Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. The New England journal of medicine. 2002;346(8):557–563. doi: 10.1056/NEJMoa003289. [DOI] [PubMed] [Google Scholar]
- 26.Hypothermia after Cardiac Arrest Study G. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. The New England journal of medicine. 2002;346(8):549–556. doi: 10.1056/NEJMoa012689. [DOI] [PubMed] [Google Scholar]
- 27.Nielsen N, Wetterslev J, Cronberg T, Erlinge D, Gasche Y, Hassager C, et al. Targeted temperature management at 33 degrees C versus 36 degrees C after cardiac arrest. The New England journal of medicine. 2013;369(23):2197–2206. doi: 10.1056/NEJMoa1310519. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.