Abstract
Interactions between intestinal neuroendocrine peptides/amines and the immune system appear to have an important role in the pathophysiology of inflammatory bowel disease (IBD). The present study investigated the effects of activator protein (AP)-1 and nuclear factor (NF)-κB inhibitors on inflammation-induced alterations in enteroendocrine cells. A total of 48 male Wistar rats were divided into the following four groups (n=12 rats/group): Control, trinitrobenzene sulfonic acid (TNBS)-induced colitis only (TNBS group), TNBS-induced colitis with 3-[(dodecylthiocarbonyl)-methyl]-glutarimide (DTCM-G) treatment (DTCM-G group), and TNBS-induced colitis with dehydroxymethylepoxyquinomicin (DHMEQ) treatment (DHMEQ group). A total of 3 days following administration of TNBS, the rats were treated as follows: The control and TNBS groups received 0.5 ml vehicle (0.5% carboxymethyl cellulose; CMC), respectively; the DTCM-G group received DTCM-G (20 mg/kg body weight) in 0.5% CMC; and the DHMEQ group received DHMEQ (15 mg/kg body weight) in 0.5% CMC. All injections were performed intraperitoneally twice daily for 5 days. The rats were sacrificed, and tissue samples obtained from the colon were examined histopathologically and immunohistochemically. Inflammation was evaluated using a scoring system. In addition, the sections were immunostained for chromogranin A (CgA), serotonin, peptide YY (PYY), oxyntomodulin, pancreatic polypeptide (PP) and somatostatin, and immunostaining was quantified using image-analysis software. The density of cells expressing CgA, PYY and PP was significantly lower in the TNBS group compared with in the control group, whereas the density of cells expressing serotonin, oxyntomodulin and somatostatin was significantly higher in the TNBS group compared with in the control group. None of the endocrine cell types differed significantly between the control group and either the DTCM-G or DHMEQ groups. All of the colonic endocrine cell types were affected in rats with TNBS-induced colitis. The expression density of these endocrine cell types was restored to control levels following treatment with AP-1 or NF-κB inhibitors. These results indicated that the immune system and enteroendocrine cells interact in IBD.
Keywords: chromogranin A, colitis, enteroendocrine cells, oxyntomodulin, pancreatic polypeptide, peptide YY, serotonin, somatostatin, trinitrobenzene sulfonic acid
Introduction
It has previously been suggested that interactions between intestinal neuroendocrine peptides/amines and the immune system have a significant role in the pathophysiology of inflammatory bowel disease (IBD) (1–12). Understanding this role may shed light on the etiology of IBD and lead to potential therapeutic strategies for the treatment of IBD, involving the use of agonists or antagonists to these peptides/amines.
Abnormalities in the enteroendocrine cells of patients with IBD and in animal models of human IBD have previously been reported (6,10,11,13–29). Some of the alterations observed in enteroendocrine cells are similar in ulcerative colitis (UC), Crohn's disease (CD) and microscopic colitis (MC), including an increased density of cells expressing serotonin, whereas others differ between these three diseases. A recent study involving an animal model of human CD, namely trinitrobenzene sulfonic acid (TNBS)-induced colitis, demonstrated that abnormalities in enteroendocrine cells were strongly correlated with changes in immune cells (30). These observations support the presence of interactions between intestinal hormones and the immune system, as represented by immune cells in IBD (1–12).
3-[(Dodecylthiocarbonyl)-methyl]-glutarimide (DTCM-G) is an inhibitor of activator protein (AP)-1, which has been reported to exhibit potent anti-inflammatory activity in animal experiments (31,32). Dehydroxymethylepoxyquinomicin (DHMEQ) is a novel inhibitor of nuclear factor (NF)-κB with a low molecular weight (33,34). Similar to DTCM-G, DHMEQ has been reported to exert potent anti-inflammatory effects in experimental animal models of human IBD (32,35). The aim of the present study was to identify the effects of these two novel anti-inflammatory agents on inflammation-induced alterations to enteroendocrine cells.
Materials and methods
Rats
A total of 48 male Wistar rats (Hannover GALAS™; Taconic Europe A/S, Lille Skensved, Denmark) with a mean body weight of 202 g (range, 166–249 g) were housed in Macrolon III cages with ad libitum access to food and water. The rats were fed a standard diet (B&K Universal, Nittedal, Norway) and were maintained at a temperature of 20–22°C, a relative humidity of 50–60%, and under a 12/12-h light/dark cycle. The rats were allowed to acclimate in the animal house for at least 7 days prior to experimentation, and were divided into the following four groups (n=12 rats/group): Control, TNBS-induced colitis only (TNBS group), TNBS-induced colitis with DTCM-G treatment (DTCM-G group), and TNBS-induced colitis with DHMEQ treatment (DHMEQ group).
The present study was performed in accordance with the Directive for the Protection of Vertebrate Animals used for Experimental and other Scientific Purposes (86/609/EEC), in compliance with the Helsinki Declaration. The local ethical committee for experimental animals at the University of Bergen (Bergen, Norway) approved the protocols used in the present study.
Induction of colitis using TNBS
TNBS-colitis was induced in the TNBS, DTCM-G and DHMEQ groups as previously described (36). The dose of TNBS chosen in the present study induces severe inflammation in rats (36). Briefly, after a 24 h fast, a single dose of TNBS (Sigma-Aldrich Produktions GmbH, Steinheim, Germany) was administered to the colon of each rat (25 mg/animal in 50% ethanol solution; 0.5 ml/rat), followed by 2 ml of air, at 8 cm from the anal margin via an 8.5-cm-long, 2.5-mm-diameter round-tipped Teflon feeding tube (AngTheo, Lidingö, Sweden). The rats were anesthetized by isoflurane inhalation (Merck Pharmaceuticals, Kenilworth, NJ, USA) during the procedure. The animals were kept prone with their hind legs raised for 2–3 min following administration of TNBS. The rats were supervised until recovery and were subsequently monitored several times daily. The control group received the same treatment as the TNBS group, except that 0.9% saline was introduced into the colon instead of TNBS.
DTCM-G and DHMEQ treatments
A total of 3 days following administration of TNBS, the rats were treated as follows: The control and TNBS groups received 0.5 ml vehicle (0.5% carboxymethyl cellulose; CMC), respectively; the DTCM-G group received DTCM-G (20 mg/kg body weight) in 0.5% CMC; and the DHMEQ group received DHMEQ (15 mg/kg body weight) in 0.5% CMC. All injections were performed intraperitoneally twice daily for 5 days. The doses of DTCM-G and DHMEQ used here were the same as those earlier reported to ameliorate TNBS-induced colitis in rats (32). The synthesis of DTCM-G and DHMEQ is described in previous studies (31,37–41). The rats were checked twice daily, and any animals exhibiting signs of pain were given a subcutaneous injection of 1 ml 0.3-g/ml Temgesic solution (Merck Pharmaceuticals).
At the end of the experiments, the rats were sacrificed by CO2 inhalation and a post-mortem laparotomy was carried out. Tissue samples obtained from the colon were examined histopathologically and immunohistochemically.
Histopathological and immunohistochemical examinations
The colonic tissues were fixed in 4% buffered paraformaldehyde overnight, embedded in paraffin, and cut into 5-µm sections. The sections were routinely stained with hematoxylin and eosin in the pathology laboratory. Inflammation was evaluated using the scoring system as described by Hunter et al (42), in which the total score was calculated as the summation of four parameter scores: Inflammatory infiltration (0–3), the number of gut walls engaged (0–3), damage to the mucosal architecture (0–3) and edema (0 or 1). The total score of this scale ranged between 0 and 10.
The sections were also immunostained and visualized using the ultraView Universal DAB Detection kit (version 1.02.0018; Ventana Medical Systems, Inc., Basel, Switzerland) and the BenchMark Ultra IHC/ISH staining module (Ventana Medical Systems, Inc.). The sections were incubated with one of the following primary antibodies for 32 min at 37°C: Monoclonal mouse antibody raised against the N-terminal of purified chromogranin A (CgA; no. M869; Dako, Glostrup, Denmark), monoclonal mouse anti-serotonin (no. M0758; Dako), polyclonal rabbit anti-porcine peptide YY (PYY; no. PYY 11A; Alpha Diagnostic International, San Antonio, TX, USA), polyclonal rabbit anti-synthetic-human pancreatic polypeptide (PP; no. #114; Diagnostic Biosystems Inc., Pleasanton, CA, USA), polyclonal rabbit anti-porcine oxyntomodulin 'glicentin/glucagon' (no. BP508; Acris Antibodies GmbH, Herford, Germany), and polyclonal rabbit anti-synthetic-human somatostatin (no. A566; Dako); these antibodies were used at dilutions of 1:1,000, 1:1,500, 1:1,000, 1:800, 1:400 and 1:200, respectively.
Quantification of endocrine cells
The endocrine cells were quantified using image-analysis software (version 1.7, cellSens; Olympus Corporation, Tokyo, Japan). The number of endocrine cells in the epithelium was counted manually in each field by pointing and clicking the computer mouse. The area of the epithelial cells was determined by manually drawing an enclosed region using the computer mouse. Cell counting was conducted in ten randomly chosen microscopic fields, as observed using a 40x objective, for which each field represented a tissue area of 0.035 mm2. The data are presented as the numbers of endocrine cells per square millimeter of epithelium, and measurements were made by the same person (M.E-S.), who was not aware of the identities of the slides.
Statistical analysis
Differences between the control, TNBS, DTCM-G and DHMEQ groups were analyzed using the Kruskal-Wallis nonparametric test followed by Dunn's post-hoc test. Data are presented as the mean ± standard error of the mean. Statistical analysis was conducted using Prism 6 (GraphPad Software, Inc., La Jolla, CA, USA) and P<0.05 was considered to indicate a statistically significant difference.
Results
Body weight and mortality
The initial body weight did not differ between the control, TNBS, DTCM-G and DHMEQ groups (P=0.08); however, there were differences in reductions in body weight at the end of the experiment (P<0.0001): 0.0±0.0, 21.5±1.1, 1.7±0.6 and 1.6±0.8%, respectively. Multiple comparisons indicated that the body weight reductions differed significantly between the TNBS group, and the DTCM-G and DHMEQ groups (P<0.001). Three animals succumbed in the TNBS group: Two due to spontaneous mortality and one was sacrificed due to animal welfare reasons. There were no cases of mortality in the other three groups.
Histopathological and immunohistochemical examinations
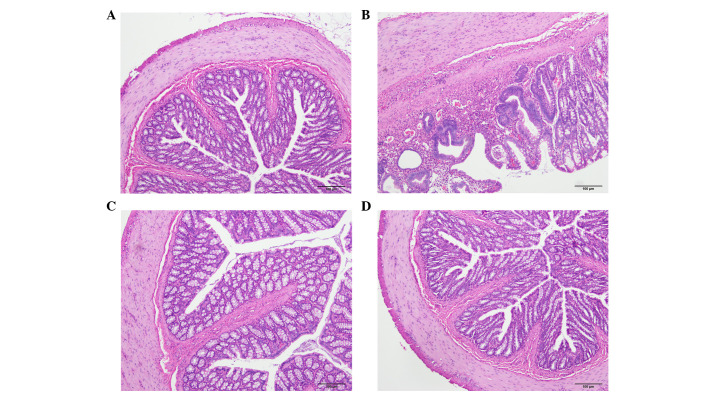
The histopathological inflammation scores were 6.6±0.9, 2.0±1.0 and 2.2±0.6 in the TNBS, DTCM-G and DHMEQ groups, respectively (Fig. 1). Multiple comparisons revealed a statistically significant difference between the three groups (P=0.002). The scores differed between the TNBS group, and the DTCM-G and DHMEQ groups (P=0.03 and P=0.01, respectively).
Figure 1.
Histopathological appearance of the colon in rats in the (A) control, (B) trinitrobenzene sulfonic acid, (C) 3-[(dodecylthiocarbonyl)-methyl]-glutarimide and (D) dehydroxymethylepoxyquinomicin groups.
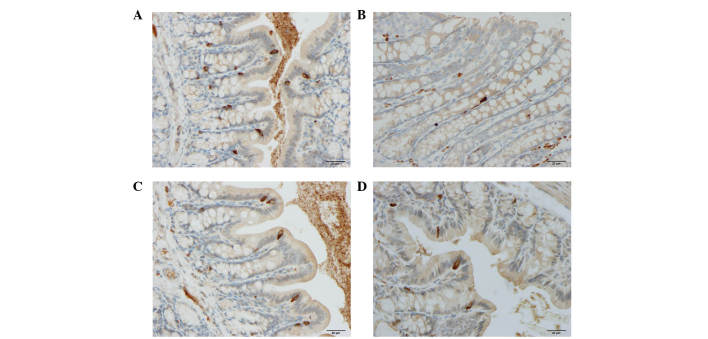
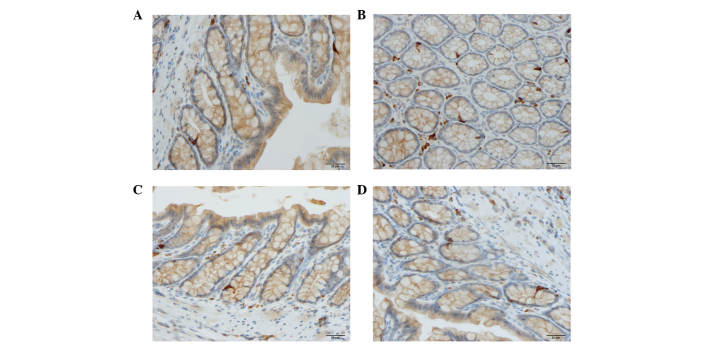
Cells expressing CgA, serotonin, PYY, oxyntomodulin, PP and somatostatin were detected in all colonic tissues from all of the groups. The endocrine cells were predominantly located at the crypts of Lieberkühn. These cells were flask-shaped and occasionally contained a long basal cytoplasmic process, often known as a 'neuropod' (43–46) (Figs. 2 and 3).
Figure 2.
Chromogranin A-expressing cells in the colon of rats in the (A) control, (B) trinitrobenzene sulfonic acid, (C) 3-[(dodecylthiocarbonyl)-methyl]-glutarimide and (D) dehydroxymethylepoxyquinomicin groups.
Figure 3.
Serotonin-expressing cells in the colon of rats in the (A) control, (B) trinitrobenzene sulfonic acid, (C) 3-[(dodecylthiocarbonyl)-methyl]-glutarimide and (D) dehydroxymethylepoxyquinomicin groups.
Quantification of endocrine cells
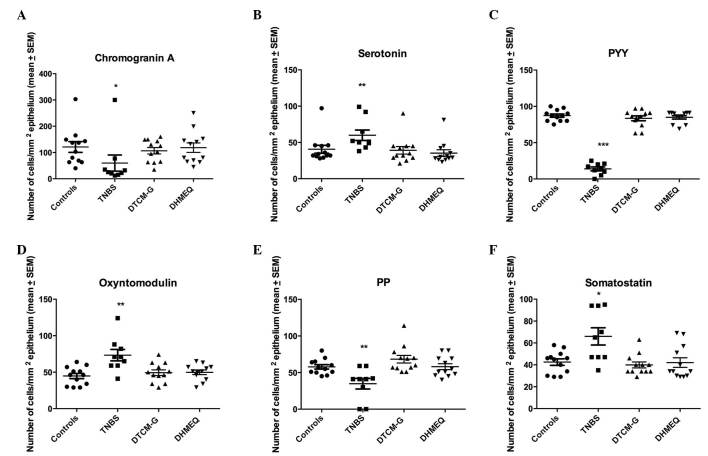
Results of the quantification of the various types of endocrine cells in all four experimental groups are presented in Fig. 4.
Figure 4.
Densities of different colonic endocrine cell types in the control, trinitrobenzene sulfonic acid (TNBS), 3-[(dodecylthiocarbonyl)-methyl]-glutarimide (DTCM-G) and dehydroxymethylepoxyquinomicin (DHMEQ) groups. Immunostaining was conducted to detect (A) chromogranin A, (B) serotonin, (C) peptide YY (PYY), (D) oxyntomodulin, (E) pancreatic polypeptide (PP) and (F) somatostatin. *P<0.05, **P<0.01, ***P<0.001 vs. the controls, as determined by Dunn's post-hoc test. SEM, standard error of the mean.
CgA-expressing cells
The density of cells expressing CgA was 121±20.4, 59.8±30.7, 106.6±12.2 and 118.4±18.0 cells/mm2 epithelium in the control, TNBS, DTCM-G and DHMEQ groups, respectively. The Kruskal-Wallis test revealed a significant difference among the four experimental groups (P=0.01). The density of cells expressing CgA was significantly lower in the TNBS group compared with in the control group (P=0.01); however, there was no significant difference between the control, DTCM-G and DHMEQ groups.
Serotonin-expressing cells
The density of cells expressing serotonin was 40.7±5.5, 59.9±7.7, 39.2±5.2 and 35.3±4.7 cells/mm2 epithelium in the control, TNBS, DTCM-G and DHMEQ groups, respectively. The Kruskal-Wallis test revealed a significant difference among the four experimental groups (P=0.002). The density of cells expressing serotonin was higher in the TNBS group compared with in the control group (P=0.003); however, there was no significant difference between the control, DTCM-G, and DHMEQ groups.
PYY-expressing cells
The density of cells expressing PYY was 87.3±2.2, 13.9±2.7, 83.6±3.3 and 84.9±2.3 in the control, TNBS, DTCM-G and DHMEQ groups, respectively. The Kruskal-Wallis test revealed a significant difference among the four experimental groups (P<0.0001). The density of cells expressing PYY was significantly lower in the TNBS group compared with in the control group (P<0.001); however, there was no significant difference between the control, DTCM-G and DHMEQ groups.
Oxyntomodulin-expressing cells
The density of cells expressing oxyntomodulin in the control, TNBS, DTCM-G and DHMEQ groups was 44.8±3.6, 73.3±7.9, 49.3±3.9 and 49.8±3.2 cells/mm2 epithelium, respectively. The Kruskal-Wallis test revealed a statistically significant difference among the four experimental groups (P=0.006). The density of cells expressing oxyntomodulin was significantly higher in the TNBS group compared with in the control group (P=0.001).
PP-expressing cells
The density of cells expressing PP in the control, TNBS, DTCM-G and DHMEQ groups was 57.8±3.0, 34.8±7.2, 68.3±5.2 and 58.1±4.0 cells/mm2 epithelium, respectively. The Kruskal-Wallis test revealed a significant difference among the four experimental groups (P=0.002). The density of cells expressing PP was significantly lower in the TNBS group compared with in the control group (P=0.003); however, there was no significant difference between the DTCM-G, DHMEQ and control groups.
Somatostatin-expressing cells
The density of cells expressing somatostatin was 42.9±2.9, 66.0±7.9, 39.9±2.7 and 42.1±4.4 cells/mm2 epithelium in the control, TNBS, DTCM-G and DHMEQ groups, respectively. The Kruskal-Wallis test revealed a significant difference among the four experimental groups (P=0.002). The density of cells expressing somatostatin was significantly higher in the TNBS group compared with in the control group (P=0.01); however, there was no significant difference between the control, DTCM-G and DHMEQ groups.
Discussion
TNBS-induced colitis resulted in alterations in the densities of all colonic endocrine cells. The density of cells expressing CgA, PYY and PP decreased, whereas the density of those expressing serotonin, oxyntomodulin and somatostatin increased. These changes occurred rapidly, 3 days after the induction of inflammation. Explaining the underlying mechanisms requires consideration of the recently published findings, which have reported that mature intestinal endocrine cells are capable of expressing up to seven hormones (47,48). It may be hypothesized that the inflammatory substances produced during inflammation, including cytokines, affect the endocrine cell expression of certain hormones, thus upregulating the expression of some hormones whilst downregulating others. The change in the density of particular endocrine cell types may therefore depend on switching hormone expression rather than changing the actual number of these cells. In support of this assumption are L-cells, which are known to express both PYY and oxyntomodulin (49,50). In the present study it seems that L-cells exhibited downregulated expression of PYY, whereas the expression of oxyntomodulin was upregulated.
Comparisons of the findings of the present study with those of previous studies reveal both discrepant and consistent results. The decreased density of CgA-expressing cells observed in the present study disagrees with previously reported increases in CgA-expressing cells in UC and CD (13,23); however, the increased density of serotonin-expressing colonic cells in TNBS-induced colitis in the present study is in agreement with previously published findings in patients with UC, CD and MC, and in animal models of colitis (13,15,51–53). In addition, the present observation of a decrease in the density of cells expressing PYY disagrees with previous observations in UC and interleukin (IL)-2 gene knockout mice (13,52). Furthermore, whereas the increased density of cells expressing oxyntomodulin detected in the present study is in concordance with previous findings in IL-2 knockout mice, it disagrees with the findings of a previous study, which demonstrated that the density of oxyntomodulin-expressing cells was unchanged in UC (13,52). The decreased density of cells expressing PP observed in the present study is in concordance with what has previously been reported in UC and CD (13). Conversely, the density of cells expressing somatostatin has been reported to be decreased in the colon of patients with UC and CD, and in animal models of induced colitis (28,29,54); however, the present study detected an increase in the density of cells expressing somatostatin in TNBS-induced colitis. When considering all of these differences, it should be kept in mind that the type of inflammation differs between UC, CD and MC, and that animal models of colitis are not identical to human UC and CD.
Treatment with either DTCM-G or DHMEQ for 5 days ameliorated TNBS-induced inflammation, as indicated by the reduced histopathological inflammation scores for the treated rats. This finding is in concordance with the results of previous studies in TNBS- and dextran sodium sulfate-induced colitis in rats and mice (3,32,35). In the present study, the attenuation of inflammation was associated with restoration of the normal densities of all colonic endocrine cell types to normal levels. DTCM-G affects inflammation by inhibiting AP-1, whereas the anti-inflammatory effects of DHMEQ are due to the inhibition of NF-κB. The effects of these agents on the density of colonic endocrine cells are most likely to be attributed to their effects on inflammation. Furthermore, it may be hypothesized that attenuation of inflammation by treatment with anti-inflammatory agents that reduce the secretion of inflammatory substances may result in restoration of normal expression levels of hormones in colonic cells.
CgA peptides and serotonin are considered to have proinflammatory actions (54–66), whereas somatostatin exerts anti-inflammatory effects (4,67–82). The exact roles of PYY, oxyntomodulin and PP in inflammation remain to be elucidated. Serotonin stimulates gastric and intestinal motility, modulates visceral sensitivity, and stimulates intestinal secretion (83,84), whereas PYY delays gastric emptying and mediates the ileal brake. In addition, PYY inhibits gastric and pancreatic secretion, and stimulates the absorption of water and electrolytes (6,83,85). The increase in serotonin and decrease in PYY detected in TNBS-induced colitis in the present study may lead to accelerated gastrointestinal motility and an increase in intestinal secretion, giving rise to diarrhea, which is the cardinal symptom of colitis.
In conclusion, TNBS-induced colitis affected the density of all colonic endocrine cell types investigated in the present study. The observed changes in these densities may have been caused by switching the expression from one hormone to another, rather than changing the actual number of cells. Treatment with anti-inflammatory agents, AP-1 and NF-κB inhibitors, restored the density of these endocrine cells to normal. These results support the hypothesis that interactions between the immune system and enteroendocrine cells have a significant role in the pathophysiology of IBD and in the development of the clinical symptoms of colitis.
Acknowledgments
The present study was supported by grants from Helse-Vest (grant no. 911978) and Helse-Fonna (grant no. 40515).
References
- 1.Khan WI, Ghia JE. Gut hormones: Emerging role in immune activation and inflammation. Clin Exp Immunol. 2010;161:19–27. doi: 10.1111/j.1365-2249.2010.04150.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Margolis KG, Gershon MD. Neuropeptides and inflammatory bowel disease. Curr Opin Gastroenterol. 2009;25:503–511. doi: 10.1097/MOG.0b013e328331b69e. [DOI] [PubMed] [Google Scholar]
- 3.Bampton PA, Dinning PG. High resolution colonic manometry-what have we learnt?-A review of the literature 2012. Curr Gastroenterol Rep. 2013;15:328. doi: 10.1007/s11894-013-0328-2. [DOI] [PubMed] [Google Scholar]
- 4.Ameri P, Ferone D. Diffuse endocrine system, neuroendocrine tumors and immunity: What's new? Neuroendocrinology. 2012;95:267–276. doi: 10.1159/000334612. [DOI] [PubMed] [Google Scholar]
- 5.Farzi A, Reichmann F, Holzer P. The homeostatic role of neuropeptide Y in immune function and its impact on mood and behaviour. Acta Physiol (Oxf) 2015;213:603–627. doi: 10.1111/apha.12445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vona-Davis LC, McFadden DW. NPY family of hormones: Clinical relevance and potential use in gastrointestinal disease. Curr Top Med Chem. 2007;7:1710–1720. doi: 10.2174/156802607782340966. [DOI] [PubMed] [Google Scholar]
- 7.Wheway J, Herzog H, Mackay F. NPY and receptors in immune and inflammatory diseases. Curr Top Med Chem. 2007;7:1743–1752. doi: 10.2174/156802607782341046. [DOI] [PubMed] [Google Scholar]
- 8.Wheway J, Herzog H, Mackay F. The Y1 receptor for NPY: A key modulator of the adaptive immune system. Peptides. 2007;28:453–458. doi: 10.1016/j.peptides.2006.09.030. [DOI] [PubMed] [Google Scholar]
- 9.Wheway J, Mackay CR, Newton RA, Sainsbury A, Boey D, Herzog H, Mackay F. A fundamental bimodal role for neuropeptide Y1 receptor in the immune system. J Exp Med. 2005;202:1527–1538. doi: 10.1084/jem.20051971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.El-Salhy M, Suhr O, Danielsson A. Peptide YY in gastrointestinal disorders. Peptides. 2002;23:397–402. doi: 10.1016/S0196-9781(01)00617-9. [DOI] [PubMed] [Google Scholar]
- 11.El-Salhy M, Mazzawi T, Gundersen D, Hatlebakk JG, Hausken T. The role of peptide YY in gastrointestinal diseases and disorders (Review) Int J Mol Med. 2013;31:275–282. doi: 10.3892/ijmm.2012.1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.El-Salhy M, Hausken T. The role of the neuropeptide Y (NPY) family in he pathophysiology of inflammatory bowel disease (IBD) Neuropeptides. 2015;55:137–144. doi: 10.1016/j.npep.2015.09.005. [DOI] [PubMed] [Google Scholar]
- 13.El-Salhy M, Danielsson A, Stenling R, Grimelius L. Colonic endocrine cells in inflammatory bowel disease. J Intern Med. 1997;242:413–419. doi: 10.1046/j.1365-2796.1997.00237.x. [DOI] [PubMed] [Google Scholar]
- 14.El-Salhy M, Gundersen D, Hatlebakk JG, Hausken T. Chromogranin a cell density as a diagnostic marker for lymphocytic colitis. Dig Dis Sci. 2012;57:3154–3159. doi: 10.1007/s10620-012-2249-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.El-Salhy M, Gundersen D, Hatlebakk JG, Hausken T. High densities of serotonin and peptide YY cells in the colon of patients with lymphocytic colitis. World J Gastroenterol. 2012;18:6070–6075. doi: 10.3748/wjg.v18.i42.6070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.El-Salhy M, Lomholt-Beck B, Gundersen TD. High chromogranin A cell density in the colon of patients with lymphocytic colitis. Mol Med Rep. 2011;4:603–605. doi: 10.3892/mmr.2011.492. [DOI] [PubMed] [Google Scholar]
- 17.Moran GW, Pennock J, McLaughlin JT. Enteroendocrine cells in terminal ileal Crohn's disease. J Crohns Colitis. 2012;6:871–880. doi: 10.1016/j.crohns.2012.01.013. [DOI] [PubMed] [Google Scholar]
- 18.Moran GW, Leslie FC, McLaughlin JT. Crohn's disease affecting the small bowel is associated with reduced appetite and elevated levels of circulating gut peptides. Clin Nutr. 2013;32:404–411. doi: 10.1016/j.clnu.2012.08.024. [DOI] [PubMed] [Google Scholar]
- 19.Besterman HS, Mallinson CN, Modigliani R, Christofides ND, Pera A, Ponti V, Sarson DL, Bloom SR. Gut hormones in inflammatory bowel disease. Scand J Gastroenterol. 1983;18:845–852. doi: 10.3109/00365528309182104. [DOI] [PubMed] [Google Scholar]
- 20.Hirotani Y, Mikajiri K, Ikeda K, Myotoku M, Kurokawa N. Changes of the peptide YY levels in the intestinal tissue of rats with experimental colitis following oral administration of mesalazine and prednisolone. Yakugaku Zasshi. 2008;128:1347–1353. doi: 10.1248/yakushi.128.1347. [DOI] [PubMed] [Google Scholar]
- 21.Tari A, Teshima H, Sumii K, Haruma K, Ohgoshi H, Yoshihara M, Kajiyama G, Miyachi Y. Peptide YY abnormalities in patients with ulcerative colitis. Jpn J Med. 1988;27:49–55. doi: 10.2169/internalmedicine1962.27.49. [DOI] [PubMed] [Google Scholar]
- 22.Sciola V, Massironi S, Conte D, Caprioli F, Ferrero S, Ciafardini C, Peracchi M, Bardella MT, Piodi L. Plasma chromogranin a in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2009;15:867–871. doi: 10.1002/ibd.20851. [DOI] [PubMed] [Google Scholar]
- 23.Bishop AE, Pietroletti R, Taat CW, Brummelkamp WH, Polak JM. Increased populations of endocrine cells in Crohn's ileitis. Virchows Arch A Pathol Anat Histopathol. 1987;410:391–396. doi: 10.1007/BF00712758. [DOI] [PubMed] [Google Scholar]
- 24.Manocha M, Khan WI. Serotonin and GI Disorders: An update on clinical and experimental studies. Clin Transl Gastroenterol. 2012;3:e13. doi: 10.1038/ctg.2012.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stoyanova II, Gulubova MV. Mast cells and inflammatory mediators in chronic ulcerative colitis. Acta Histochem. 2002;104:185–192. doi: 10.1078/0065-1281-00641. [DOI] [PubMed] [Google Scholar]
- 26.Yamamoto H, Morise K, Kusugami K, Furusawa A, Konagaya T, Nishio Y, Kaneko H, Uchida K, Nagai H, Mitsuma T, Nagura H. Abnormal neuropeptide concentration in rectal mucosa of patients with inflammatory bowel disease. J Gastroenterol. 1996;31:525–532. doi: 10.1007/BF02355052. [DOI] [PubMed] [Google Scholar]
- 27.Payer J, Huorka M, Duris I, Mikulecky M, Kratochvílová H, Ondrejka P, Lukác L. Plasma somatostatin levels in ulcerative colitis. Hepatogastroenterology. 1994;41:552–553. [PubMed] [Google Scholar]
- 28.Watanabe T, Kubota Y, Sawada T, Muto T. Distribution and quantification of somatostatin in inflammatory disease. Dis Colon Rectum. 1992;35:488–494. doi: 10.1007/BF02049408. [DOI] [PubMed] [Google Scholar]
- 29.Koch TR, Carney JA, Morris VA, Go VL. Somatostatin in the idiopathic inflammatory bowel diseases. Dis Colon Rectum. 1988;31:198–203. doi: 10.1007/BF02552546. [DOI] [PubMed] [Google Scholar]
- 30.El-Sahy M, Hatlebakk JG. Changes in endocrine and immune cells following colitis induction by TNBS in rats. Mol Med Rep. doi: 10.3892/mmr.2016.5902. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Takeiri M, Tachibana M, Kaneda A, Ito A, Ishikawa Y, Nishiyama S, Goto R, Yamashita K, Shibasaki S, Hirokata G, et al. Inhibition of macrophage activation and suppression of graft rejection by DTCM-glutarimide, a novel piperidine derived from the antibiotic 9-methylstreptimidone. Inflamm Res. 2011;60:879–888. doi: 10.1007/s00011-011-0348-z. [DOI] [PubMed] [Google Scholar]
- 32.El-Salhy M, Umezawa K, Gilja OH, Hatlebakk JG, Gundersen D, Hausken T. Amelioration of Severe TNBS Induced colitis by novel AP-1 and NF-κB inhibitors in rats. Scientfic World Journal. 2014;2014:813804. doi: 10.1155/2014/813804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Umezawa K, Ariga A, Matsumoto N. Naturally occurring and synthetic inhibitors of NF-kappaB functions. Anticancer Drug Des. 2000;15:239–244. [PubMed] [Google Scholar]
- 34.Umezawa K. Possible role of peritoneal NF-kappaB in peripheral inflammation and cancer: Lessons from the inhibitor DHMEQ. Biomed Pharmacother. 2011;65:252–259. doi: 10.1016/j.biopha.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 35.Funakoshi T, Yamashita K, Ichikawa N, Fukai M, Suzuki T, Goto R, Oura T, Kobayashi N, Katsurada T, Ichihara S, et al. A novel NF-kappaB inhibitor, dehydroxymethylepoxyquinomicin, ameliorates inflammatory colonic injury in mice. J Crohns Colitis. 2012;6:215–225. doi: 10.1016/j.crohns.2011.08.011. [DOI] [PubMed] [Google Scholar]
- 36.El-Salhy M, Wendelbo IH, Gundersen D, Hatlebakk JG, Hausken T. Evaluation of the usefulness of colonoscopy with mucosal biopsies in the follow-up of TNBS-induced colitis in rats. Mol Med Rep. 2013;8:446–450. doi: 10.3892/mmr.2013.1528. [DOI] [PubMed] [Google Scholar]
- 37.Ota E, Takeiri M, Tachibana M, Ishikawa Y, Umezawa K, Nishiyama S. Synthesis and biological evaluation of molecular probes based on the 9-methylstreptimidone derivative DTCM-glutarimide. Bioorg Med Chem Lett. 2012;22:164–167. doi: 10.1016/j.bmcl.2011.11.045. [DOI] [PubMed] [Google Scholar]
- 38.Ishikawa Y, Tachibana M, Matsui C, Obata R, Umezawa K, Nishiyama S. Synthesis and biological evaluation on novel analogs of 9-methylstreptimidone, an inhibitor of NF-kappaB. Bioorg Med Chem Lett. 2009;19:1726–1728. doi: 10.1016/j.bmcl.2009.01.107. [DOI] [PubMed] [Google Scholar]
- 39.Ueki S, Yamashita K, Aoyagi T, Haga S, Suzuki T, Itoh T, Taniguchi M, Shimamura T, Furukawa H, Ozaki M, et al. Control of allograft rejection by applying a novel nuclear factor-kappaB inhibitor, dehydroxymethylepoxyquinomicin. Transplantation. 2006;82:1720–1727. doi: 10.1097/01.tp.0000250548.13063.44. [DOI] [PubMed] [Google Scholar]
- 40.Matsumoto N, Ariga A, To-e S, Nakamura H, Agata N, Hirano S, Inoue J, Umezawa K. Synthesis of NF-kappaB activation inhibitors derived from epoxyquinomicin C. Bioorg Med Chem Lett. 2000;10:865–869. doi: 10.1016/S0960-894X(00)00114-1. [DOI] [PubMed] [Google Scholar]
- 41.Umezawa N, Matsumoto N, Iwama S, Kato N, Higuchi T. Facile synthesis of peptide-porphyrin conjugates: Towards artificial catalase. Bioorg Med Chem. 2010;18:6340–6350. doi: 10.1016/j.bmc.2010.07.018. [DOI] [PubMed] [Google Scholar]
- 42.Hunter MM, Wang A, Hirota CL, McKay DM. Neutralizing anti-IL-10 antibody blocks the protective effect of tapeworm infection in a murine model of chemically induced colitis. J Immunol. 2005;174:7368–7375. doi: 10.4049/jimmunol.174.11.7368. [DOI] [PubMed] [Google Scholar]
- 43.Pang XH, Li TK, Xie Q, He FQ, Cui de J, Chen YQ, Huang XL, Gan HT. Amelioration of dextran sulfate sodium-induced colitis by neuropeptide Y antisense oligodeoxynucleotide. Int J Colorectal Dis. 2010;25:1047–1053. doi: 10.1007/s00384-010-0964-z. [DOI] [PubMed] [Google Scholar]
- 44.Bohorquez DV, Chandra R, Samsa LA, Vigna SR, Liddle RA. Characterization of basal pseudopod-like processes in ileal and colonic PYY cells. J Mol Histol. 2011;42:3–13. doi: 10.1007/s10735-010-9302-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bohórquez DV, Samsa LA, Roholt A, Medicetty S, Chandra R, Liddle RA. An enteroendocrine cell-enteric glia connection revealed by 3D electron microscopy. PloS one. 2014;9:e89881. doi: 10.1371/journal.pone.0089881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bohórquez DV, Shahid RA, Erdmann A, Kreger AM, Wang Y, Calakos N, Wang F, Liddle RA. Neuroepithelial circuit formed by innervation of sensory enteroendocrine cells. J Clin Invest. 2015;125:782–786. doi: 10.1172/JCI78361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ghia JE, Li N, Wang H, Collins M, Deng Y, El-Sharkawy RT, Côté F, Mallet J, Khan WI. Serotonin has a key role in pathogenesis of experimental colitis. Gastroenterology. 2009;137:1649–1660. doi: 10.1053/j.gastro.2009.08.041. [DOI] [PubMed] [Google Scholar]
- 48.Dryden S, Wang Q, Frankish HM, Pickavance L, Williams G. The serotonin (5-HT) antagonist methysergide increases neuropeptide Y (NPY) synthesis and secretion in the hypothalamus of the rat. Brain Res. 1995;699:12–18. doi: 10.1016/0006-8993(95)00841-D. [DOI] [PubMed] [Google Scholar]
- 49.Spångeus A, Forsgren S, el-Salhy M. Does diabetic state affect co-localization of peptide YY and enteroglucagon in colonic endocrine cells? Histol Histopathol. 2000;15:37–41. doi: 10.14670/HH-15.37. [DOI] [PubMed] [Google Scholar]
- 50.Pyarokhil AH, Ishihara M, Sasaki M, Kitamura N. The developmental plasticity of colocalization pattern of peptide YY and glucagon-like peptide-1 in the endocrine cells of bovine rectum. Biomed Res. 2012;33:35–38. doi: 10.2220/biomedres.33.35. [DOI] [PubMed] [Google Scholar]
- 51.Bertrand PP, Bertrand RL. Serotonin release and uptake in the gastrointestinal tract. Auton Neurosci. 2010;153:47–57. doi: 10.1016/j.autneu.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 52.Qian BF, El-Salhy M, Melgar S, Hammarström ML, Danielsson A. Neuroendocrine changes in colon of mice with a disrupted IL-2 gene. Clin Exp Immunol. 2000;120:424–433. doi: 10.1046/j.1365-2249.2000.01255.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Oshima S, Fujimura M, Fukimiya M. Changes in number of serotonin-containing cells and serotonin levels in the intestinal mucosa of rats with colitis induced by dextran sodium sulfate. Histochem Cell Biol. 1999;112:257–263. doi: 10.1007/s004180050445. [DOI] [PubMed] [Google Scholar]
- 54.Spiller R. Serotonin and GI clinical disorders. Neuropharmacology. 2008;55:1072–1080. doi: 10.1016/j.neuropharm.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 55.Egger M, Beer AG, Theurl M, Schgoer W, Hotter B, Tatarczyk T, Vasiljevic D, Frauscher S, Marksteiner J, Patsch JR, et al. Monocyte migration: A novel effect and signaling pathways of catestatin. Eur J Pharmacol. 2008;598:104–111. doi: 10.1016/j.ejphar.2008.09.016. [DOI] [PubMed] [Google Scholar]
- 56.Feistritzer C, Mosheimer BA, Colleselli D, Wiedermann CJ, Kähler CM. Effects of the neuropeptide secretoneurin on natural killer cell migration and cytokine release. Regul Pept. 2005;126:195–201. doi: 10.1016/j.regpep.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 57.Ferrero E, Magni E, Curnis F, Villa A, Ferrero ME, Corti A. Regulation of endothelial cell shape and barrier function by chromogranin A. Ann N Y Acad Sci. 2002;971:355–358. doi: 10.1111/j.1749-6632.2002.tb04495.x. [DOI] [PubMed] [Google Scholar]
- 58.Wang H, Steeds J, Motomura Y, Deng Y, Verma-Gandhu M, El-Sharkawy RT, McLaughlin JT, Grencis RK, Khan WI. CD4+ T cell-mediated immunological control of enterochromaffin cell hyperplasia and 5-hydroxytryptamine production in enteric infection. Gut. 2007;56:949–957. doi: 10.1136/gut.2006.103226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cloez-Tayarani I, Changeux JP. Nicotine and serotonin in immune regulation and inflammatory processes: A perspective. J Leukoc Biol. 2007;81:599–606. doi: 10.1189/jlb.0906544. [DOI] [PubMed] [Google Scholar]
- 60.Stefulj J, Cicin-Sain L, Schauenstein K, Jernej B. Serotonin and immune response: Effect of the amine on in vitro proliferation of rat lymphocytes. Neuroimmunomodulation. 2001;9:103–108. doi: 10.1159/000049013. [DOI] [PubMed] [Google Scholar]
- 61.Betten A, Dahlgren C, Hermodsson S, Hellstrand K. Serotonin protects NK cells against oxidatively induced functional inhibition and apoptosis. J Leukoc Biol. 2001;70:65–72. [PubMed] [Google Scholar]
- 62.Laberge S, Cruikshank WW, Beer DJ, Center DM. Secretion of IL-16 (lymphocyte chemoattractant factor) from serotonin-stimulated CD8+ T cells in vitro. J Immunol. 1996;156:310–315. [PubMed] [Google Scholar]
- 63.Soga F, Katoh N, Inoue T, Kishimoto S. Serotonin activates human monocytes and prevents apoptosis. J Invest Dermatol. 2007;127:1947–1955. doi: 10.1038/sj.jid.5700824. [DOI] [PubMed] [Google Scholar]
- 64.Di Sabatino A, Volta U, Salvatore C, Biancheri P, Caio G, De Giorgio R, Di Stefano M, Corazza GR. Small amounts of gluten in subjects with suspected nonceliac gluten sensitivity: A randomized, double-blind, placebo-controlled, cross-over trial. Clin Gastroenterol Hepatol. 2015;13:1604–1612. doi: 10.1016/j.cgh.2015.01.029. [DOI] [PubMed] [Google Scholar]
- 65.Macia L, Yulyaningsih E, Pangon L, Nguyen AD, Lin S, Shi YC, Zhang L, Bijker M, Grey S, Mackay F, et al. Neuropeptide Y1 receptor in immune cells regulates inflammation and insulin resistance associated with diet-induced obesity. Diabetes. 2012;61:3228–3238. doi: 10.2337/db12-0156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.De la Fuente M, Bernaez I, Del Rio M, Hernanz A. Stimulation of murine peritoneal macrophage functions by neuropeptide Y and peptide YY. Involvement of protein kinase C. Immunology. 1993;80:259–265. [PMC free article] [PubMed] [Google Scholar]
- 67.Ferone D, Resmini E, Boschetti M, Arvigo M, Albanese V, Ceresola E, Pivonello R, Albertelli M, Bianchi F, Giusti M, Minuto F. Potential indications for somatostatin analogues: Immune system and limphoproliferative disorders. J Endocrinol Invest. 2005;28(11 Supply International):111–117. [PubMed] [Google Scholar]
- 68.ten Bokum AM, Hofland LJ, van Hagen PM. Somatostatin and somatostatin receptors in the immune system: A review. Eur Cytokine Netw. 2000;11:161–176. [PubMed] [Google Scholar]
- 69.Ferone D, Pivonello R, Kwekkeboom DJ, Gatto F, Ameri P, Colao A, de Krijger RR, Minuto F, Lamberts SW, van Hagen PM, Hofland LJ. Immunohistochemical localization and quantitative expression of somatostatin receptors in normal human spleen and thymus: Implications for the in vivo visualization during somatostatin receptor scintigraphy. J Endocrinol Invest. 2012;35:528–534. doi: 10.3275/7871. [DOI] [PubMed] [Google Scholar]
- 70.Ferone D, Pivonello R, Van Hagen PM, Dalm VA, Lichtenauer-Kaligis EG, Waaijers M, Van Koetsveld PM, Mooy DM, Colao A, Minuto F, et al. Quantitative and functional expression of somatostatin receptor subtypes in human thymocytes. Am J Physiol Endocrinol Metab. 2002;283:E1056–E1066. doi: 10.1152/ajpendo.00205.2001. [DOI] [PubMed] [Google Scholar]
- 71.Dalm VA, van Hagen PM, van Koetsveld PM, Achilefu S, Houtsmuller AB, Pols DH, van der Lely AJ, Lamberts SW, Hofland LJ. Expression of somatostatin, cortistatin and soma-tostatin receptors in human monocytes, macrophages and dendritic cells. Am J Physiol Endocrinol Metab. 2003;285:E344–E353. doi: 10.1152/ajpendo.00048.2003. [DOI] [PubMed] [Google Scholar]
- 72.Lichtenauer-Kaligis EG, Dalm VA, Oomen SP, Mooij DM, van Hagen PM, Lamberts SW, Hofland LJ. Differential expression of somatostatin receptor subtypes in human peripheral blood mononuclear cell subsets. Eur J Endocrinol. 2004;150:565–577. doi: 10.1530/eje.0.1500565. [DOI] [PubMed] [Google Scholar]
- 73.Armani C, Catalani E, Balbarini A, Bagnoli P, Cervia D. Expression, pharmacology and functional role of somatostatin receptor subtypes 1 and 2 in human macrophages. J Leukoc Biol. 2007;81:845–855. doi: 10.1189/jlb.0606417. [DOI] [PubMed] [Google Scholar]
- 74.Taniyama Y, Suzuki T, Mikami Y, Moriya T, Satomi S, Sasano H. Systemic distribution of somatostatin receptor subtypes in human: An immunohistochemical study. Endocrine J. 2005;52:605–611. doi: 10.1507/endocrj.52.605. [DOI] [PubMed] [Google Scholar]
- 75.Hagströmer L, Emtestam L, Stridsberg M, Talme T. Expression pattern of somatostatin receptor subtypes 1–5 in human skin: An immunohistochemical study of healthy subjects and patients with psoriasis or atopic dermatitis. Exp Dermatol. 2006;15:950–957. doi: 10.1111/j.1600-0625.2006.00487.x. [DOI] [PubMed] [Google Scholar]
- 76.Talme T, Ivanoff J, Hägglund M, Van Neerven RJ, Ivanoff A, Sundqvist KG. Somatostatin receptor (SSTR) expression and function in normal and leukaemic T-cells. Evidence for selective effects on adhesion to extracellular matrix components via SSTR2 and/or 3. Clin Exp Immunol. 2001;125:71–79. doi: 10.1046/j.1365-2249.2001.01577.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rosskopf D, Schürks M, Manthey I, Joisten M, Busch S, Siffert W. Signal transduction of somatostatin in human B lymphoblasts. American journal of physiology. Cell physiology. 2003;284:C179–C190. doi: 10.1152/ajpcell.00160.2001. [DOI] [PubMed] [Google Scholar]
- 78.Casnici C, Lattuada D, Perego C, Franco P, Marelli O. Inhibitory effect of somatostatin on human T lymphocytes proliferation. Int J Immunopharmacol. 1997;19:721–727. doi: 10.1016/S0192-0561(97)00033-7. [DOI] [PubMed] [Google Scholar]
- 79.Radosević-Stasić B, Trobonjaca Z, Lucin P, Cuk M, Polić B, Rukavina D. Immunosuppressive and antiproliferative effects of somatostatin analog SMS 201–995. Int J Neurosci. 1995;81:283–297. doi: 10.3109/00207459509004892. [DOI] [PubMed] [Google Scholar]
- 80.Sirianni MC, Annibale B, Fais S, Delle Fave G. Inhibitory effect of somatostatin-14 and some analogues on human natural killer cell activity. Peptides. 1994;15:1033–1036. doi: 10.1016/0196-9781(94)90067-1. [DOI] [PubMed] [Google Scholar]
- 81.Helyes Z, Elekes K, Németh J, Pozsgai G, Sándor K, Kereskai L, Börzsei R, Pintér E, Szabó A, Szolcsányi J. Role of transient receptor potential vanilloid 1 receptors in endotoxin-induced airway inflammation in the mouse. Am J Physiol Lung Cell Mol Physiol. 2007;292:L1173–L1181. doi: 10.1152/ajplung.00406.2006. [DOI] [PubMed] [Google Scholar]
- 82.Helyes Z, Pintér E, Sándor K, Elekes K, Bánvölgyi A, Keszthelyi D, Szoke E, Tóth DM, Sándor Z, Kereskai L, et al. Impaired defense mechanism against inflammation, hyperalgesia and airway hyperreactivity in somatostatin 4 receptor gene-deleted mice. Proc Natl Acad Sci USA. 2009;106:13088–13093. doi: 10.1073/pnas.0900681106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.El-Salhy M, Seim I, Chopin L, Gundersen D, Hatlebakk JG, Hausken T. Irritable bowel syndrome: The role of gut neuroendocrine peptides. Front Biosci (Elite Ed) 2012;4:2783–2800. doi: 10.2741/e583. [DOI] [PubMed] [Google Scholar]
- 84.El-Salhy M, Gundersen D, Hatlebakk JG, Hausken T. Irritable bowel syndrome: Diagnosis, pathogenesis and treatment options. Nova Science Publishers; Inc, New York: 2012. [Google Scholar]
- 85.El-Salhy M, Gundersen D, Gilja OH, Hatlebakk JG, Hausken T. Is irritable bowel syndrome an organic disorder? World J Gastroenterol. 2014;20:384–400. doi: 10.3748/wjg.v20.i2.384. [DOI] [PMC free article] [PubMed] [Google Scholar]