Abstract
Background
Spirituality may influence how patients cope with their illness.
Objectives
We assessed whether spirituality may influence adherence to management of outpatients with heart failure.
Methods
Cross sectional study enrolling consecutive ambulatory heart failure patients in whom adherence to multidisciplinary treatment was evaluated. Patients were assessed for quality of life, depression, religiosity and spirituality utilizing validated questionnaires. Correlations between adherence and psychosocial variables of interest were obtained. Logistic regression models explored independent predictors of adherence.
Results
One hundred and thirty patients (age 60 ± 13 years; 67% male) were interviewed. Adequate adherence score was observed in 38.5% of the patients. Neither depression nor religiosity was correlated to adherence, when assessed separately. Interestingly, spirituality, when assessed by both total score sum (r = 0.26; p = 0.003) and by all specific domains, was positively correlated to adherence. Finally, the combination of spirituality, religiosity and personal beliefs was an independent predictor of adherence when adjusted for demographics, clinical characteristics and psychosocial instruments.
Conclusion
Spirituality, religiosity and personal beliefs were the only variables consistently associated with compliance to medication in a cohort of outpatients with heart failure. Our data suggest that adequately addressing these aspects on patient’s care may lead to an improvement in adherence patterns in the complex heart failure management.
Keywords: Heart Failure, Medication Adherence / psychology, Surveys and Questionnaires, Outpatients, Spirituality, Religion
Introduction
Heart failure (HF) continues to challenge multidisciplinary health care teams.1 Its prevalence remains elevated and its management usually requires poly-pharmacy along with satisfactory self-awareness of the disease.2,3 The course of HF, in its chronicity and frequently inexorable outcomes, shares similarities with many cancer diseases and resembles their impact on poor quality of life standards.4 Patients face important limitations to adequately adhere to the complexity of HF management.5
Adherence appears as an important aspect in the course of HF. It influences patients' pattern of decompensation and subsequent hospital re-admissions.6 In addition, adequate adherence standards may help to improve quality of life.7 Many factors are thought to influence patient adherence to HF management. Clinical aspects such as comorbidities commonly associated with HF have been addressed in this regard.5 Socio-economic background, psychological aspects and patients' level of formal education have also been investigated as influential in adherence patterns in the HF population.8,9 Nonetheless, data addressing such issues on large cohorts being followed in specialized HF clinics remains scarce.
Spirituality has recently been studied in the setting of chronic diseases with poor quality of life and predictable ominous outcomes. Spiritual wellbeing refers to one's spirituality as "the state of affairs".10 This concept has been applied to unravel specifics on spiritual status in the palliative care setting, but very little data exists on spirituality associated to such a chronic and prevalent condition as HF. Spirituality has been shown to potentially influence how patients with HF cope with their syndrome, consequently having an impact on functional status, health status and quality of life.11,12 Recent data indicates that spirituality could favorably influence mortality in patients with HF.13 However, how spirituality relates to adherence patterns in stable outpatients with HF remains relatively unexplored. Few reports with controversial results, partially limited by convenience sampling and instruments utilized, failed to demonstrate a positive association between spirituality and degree of compliance in HF patients.14 Nevertheless, for many other chronic disorders there is sustained evidence that spirituality could improve compliance.15
In this study, we examined associations between spirituality and adherence to management in outpatients with HF, independently of psychosocial and educational background.
Patients and Methods
Study design
This is a cross-sectional study which enrolled HF outpatients followed at a tertiary care University Hospital in Porto Alegre, Brazil, from August, 2012 to June, 2013. The study protocol was approved by the Institutional Research and Ethics Committee and all enrolled participants signed a written informed consent prior to study entry.
Participants
Consecutive ambulatory patients (mainly composed by patients with newly diagnosed left ventricular dysfunction, post HF hospital admission and/or refractory symptoms) being followed for a minimum of six months in the HF Clinic at the Hospital de Clínicas de Porto Alegre were invited to participate. Patients in any New York Heart Association functional class, regardless of HF etiology, were eligible. Exclusion criteria were inability to understand the study protocol and to answer the questions without assistance due to cognitive impairment or auditory deficit.
Study end-points and procedures
Patients were assessed for adherence to therapy, quality of life, depression, religiosity and spirituality utilizing validated questionnaires. All utilized instruments were previously validated to Brazilian Portuguese language.16-21 Interviews were performed following the clinic appointment by research staff previously trained in questionnaire application. Time required for answering all the instruments ranged from 50 to 70 minutes. Patients answered questions orally and staff filled questionnaires as requested. Demographics and clinical characteristics were obtained from electronic chart review and clinical data were acquired during the clinic visit by a researcher who was unaware of questionnaire results. Definitions of psychosocial variables of interest are detailed below.
Adherence to therapy. The adherence to pharmacologic and non-pharmacologic therapy was assessed according to the Repetitive Education and Monitoring For Adherence for Heart Failure (REMADHE) study protocol, which has been adapted and is currently used in clinical practice in our HF Clinic.17,22 The questionnaire is composed by ten-questions involving four domains: use of medications (one question); food and fluids (seven questions); alcohol consumption (one question); and medical appointments (one question). The score ranges between 0 and 26 points, with higher scores indicating better patient's adherence. A REMADHE score equal to or higher than 18 points indicates adequate level of adherence.22
Quality of life: Two instruments were used to assess quality of life: generic and disease-specific questionnaires. Generic quality of life assessment was performed with the utilization of the World Health Organization Quality of Life (WHOQoL-Bref) while disease-specific was assessed by the Minnesota Living With Heart Failure Questionnaire (MLHFQ).23,24 The WHOQoL-Bref is an abbreviated version of the WHOQOL-100 which is composed of 26 questions: a question about quality of life in general, a question about satisfaction with one's self health status, and 24 questions divided into four domains - physical, psychological, social relations and environment. The MLHFQ evaluates quality of life related to HF symptomatology within the previous month and correlates proportionally to functional class.25 Higher WHOQoL-Bref scores indicate better quality of life in general, whereas lower MLHFQ represent better HF-related quality of life.
Depression: Depression was evaluated by the Patient Health Questionnaire (PHQ-9), which is a screening tool for detection of depression, based on symptom occurrence within the previous two weeks. It comprehends nine questions based on the major criteria for the diagnosis of major depression according to the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV).26,27 Depression is classified, according to the score, as moderate depressive symptoms (total score between 10 and 14), moderate major depression (score between 15 and 19) and severe major depression (score equal or higher than 20).26
Religiosity, Spirituality and Personal Beliefs: Two instruments were used to evaluate these dimensions.
) The Duke University Religion Index (DUREL) scale is a tool for assessment of spirituality that is focused on religious aspects.28 Its transcultural adaptation was developed and validated by Moreira-Almeida.18 The DUREL scale has five items that describe three dimensions of religiosity, known to best correlate with health-related outcomes: organizational (ORA); non-organizational (NORA); and intrinsic religiosity (IR). The score ranges from 1 to 30 points and higher scores indicate elevated levels of religiosity.
) The World Health Organization Quality of Life Spirituality, Religiosity and Personal Beliefs (WHOQoL-SRPB) instrument is an additional module of the WHOQOL to evaluate spirituality, religion and personal beliefs (SRPB) as a component of the quality of life construct. It is composed by 32 items distributed in eight factors (Spiritual Connection, Meaning of Life, Awe & Wonder, Wholeness & Integration, Spiritual Strength, Inner Peace, Hope & Optimism and Faith) in a general index composed of 4 items (SRPB Global), originally of the SRPB domain of the WHOQOL-100.19,29
Statistical analyses
Normally distributed (according to Shapiro-Wilks testing) continuous variables were expressed as mean ± standard deviation, while non-normally distributed ones were expressed as median and interquartile ranges. Categorical variables were reported as absolute numbers and percentages. Normally distributed continuous variables were analyzed by unpaired t-test. Non-normally distributed continuous variables were analyzed using Mann Whitney U test. Chi-square test (or exact Fisher test when appropriate) was used to compare categorical variables. Spearman coefficients were used for evaluation of correlations between adherence and psychosocial variables of interest. Kruskal Wallis was used to compare scores of spirituality across REMADHE quartiles. Logistic regression models were used to explore the association of spirituality to an adequate level of adherence (REMADHE ≥ 18 points). Adjusting covariates for multivariable models were tested for colinearity and selected among demographic, clinical and psychosocial variables of either clinical or statistical significance. The report by Black and co-workers, that correlated spirituality and adherence utilizing different instruments, was used to estimate a sample size of 130 subjects in the current study (α = 5%, β = 80%; effect size 25%).14 All analyses were performed using the SPSS 20.0 statistical package (SPSS Inc., Chicago, IL, USA). A p value lower than 0.05 was considered of statistical significance.
Results
One hundred and thirty patients were interviewed between August, 2012 and June, 2013. Demographic and clinical characteristics of the studied population are detailed in Table 1. A description of the average scores obtained through the study instruments is provided in Table 2. Overall, there was a low level of adherence, according to REMADHE scores. Adequate adherence was observed in 38.5% of the population.
Table 1.
Demographics and clinical characteristics of the study population
| N | 130 | |
|---|---|---|
| Demographics | ||
| Age, years | 60 ± 13 | |
| Gender, male | 88 (67.5%) | |
| Ethnicity | ||
| Caucasian | 113 (87%) | |
| African-descendent | 9 (7%) | |
| Other | 8 (6%) | |
| Education | ||
| Functionally illiterate | 5 (4%) | |
| Elementary, non-graduated | 79 (61%) | |
| Elementary, graduated | 26 (20%) | |
| High school, non-graduated | 6 (5%) | |
| High school, graduated | 14 (11%) | |
| Marital status | ||
| Single | 31 (24%) | |
| Married | 78 (60%) | |
| Divorced | 15 (11.5%) | |
| Widowed | 6 (4.5%) | |
| Heart failure history | ||
| Etiology | ||
| Ischemic | 42 (32.5%) | |
| Idiopathic | 28 (21.5%) | |
| Hypertensive | 29 (22.5%) | |
| Valvular | 14 (10%) | |
| Alcoholic | 10 (7.5%) | |
| Other | 7 (5%) | |
| Ejection fraction, % | 36 ± 13 | |
| Functional class, NYHA | ||
| I-II | 97 (74.5%) | |
| III-IV | 33 (25.5%) | |
| Cardiac devices (ICD or CRT-D) | 23 (18%) | |
| Hospital admissions in the previous year | ||
| None | 82 (63%) | |
| One | 26 (20%) | |
| More than one | 22 (17%) | |
| Comorbidities | ||
| Hypertension | 75 (57.5%) | |
| Dyslipidemia | 64 (49%) | |
| Previous myocardial infarction | 39 (30%) | |
| Previous cardiac surgery | 24 (18.5%) | |
| Diabetes | 50 (38.5%) | |
| COPD | 10 (7.5%) | |
| Chronic kidney impairment | 52 (40%) | |
| Previous stroke | 20 (15.5%) | |
| Collagen tissue disease | 11 (9%) | |
| Smoking, past or present | 66 (50.5%) | |
| Alcoholism, past or present | 29 (22.5%) | |
| Neoplasia | 18 (14%) | |
NYHA: New York Heart Association; ICD: implantable cardiac defibrillator; CRT-D: cardiac resynchronization therapy-defibrillator; COPD: chronic obstructive pulmonary disease. Data expressed as mean ± SD and number (percentage). Ejection fraction assessed by bi-dimensional echocardiography (Simpson method).
Table 2.
Description of psychosocial instruments applied in the study population
| N | 130 | |
|---|---|---|
| Adherence (REMADHE) | 16.2 ± 4.1 | |
| Quality of life | ||
| Generic (WHOQoL-Bref) | ||
| Total | 13.0 ± 3.7 | |
| Domains | ||
| Physical | 12.2 ± 3.1 | |
| Psychological | 14.1 ± 2.7 | |
| Social | 13.7 ± 2.1 | |
| Environmental | 14.8 ± 1.9 | |
| Disease-specific (MLHFQ) | 50.5 ± 16.9 | |
| Depression (PHQ-9) | 4.8 ± 5.3 | |
| Religiosity (DUREL) | ||
| Total | 23.5 ± 4.6 | |
| Intrinsic | 15.5 ± 2.8 | |
| Organizational | 3.3 ± 1.6 | |
| Non-organizational | 4.7 ± 1.3 | |
| Spirituality (WHOQoL-SRPB) | ||
| Total | 3.8 ± 0.61 | |
| Domains | ||
| Connect | 3.7 ± 0.7 | |
| Meaning | 3.9 ± 0.6 | |
| Awe | 3.8 ± 0.8 | |
| Whole | 3.7 ± 0.6 | |
| Strength | 3.8 ± 0.8 | |
| Peace | 3.8 ± 0.7 | |
| Hope | 3.8 ± 0.8 | |
| Faith | 3.8 ± 0.7 | |
REMADHE: Repetitive Education and Monitoring for Adherence for Heart Failure; WHOQoL-Bref: World Health Organization Quality of Life; MLHFQ: Minnesota Living with Heart Failure Questionnaire; PHQ-9: Patient Health Questionnaire 9; DUREL: Duke University Religion Index; WHOQoL-SRPB: World Health Organization Quality of Life Spirituality, Religiosity and Personal Beliefs; Data expressed as mean ± SD.
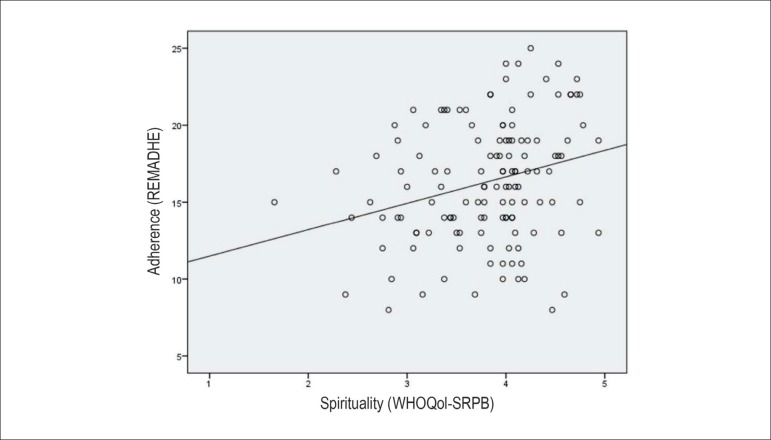
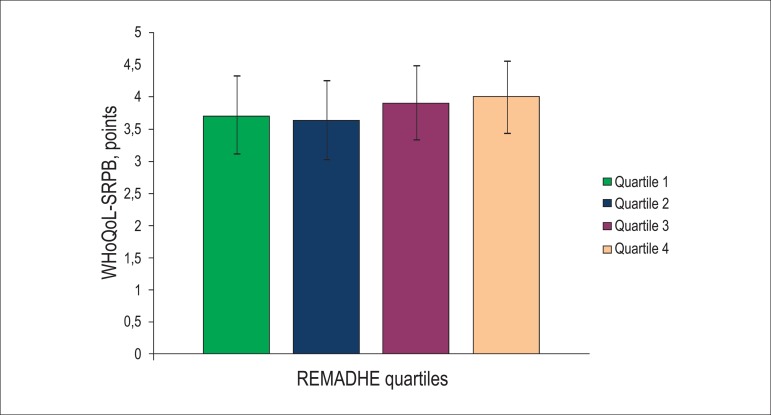
The correlations between the adherence score with clinical characteristics and psychosocial scores are demonstrated in Table 3. A description of associations of demographic and clinical variables with the adherence score is also described in the Supplemental Table. Among demographics, REMADHE score differed only according to marital status. Clinical characteristics associated to higher adherence scores were ischemic HF etiology, presence of an implantable cardiac defibrillator and chronic kidney impairment. Adherence was positively correlated to the generic quality-of-life measure, but not to the disease-specific HF score. Neither depression nor religiosity was correlated to adherence. Interestingly, spirituality, when assessed by both total WHOQoL-SRPB score sum and by many specific domains, was positively correlated to adherence. Although significantly correlated to adherence score, the magnitude of spirituality association was relatively weak (Figure 1). Notably, there was a trend towards higher spirituality scores across quartiles of the adherence score (Figure 2).
Table 3.
Correlations of clinical and psychosocial variables with adherence score (REMADHE)
| r | p | ||
|---|---|---|---|
| Clinical characteristics | |||
| Age, years | 0.10 | 0.24 | |
| Ejection fraction, % | -0.09 | 0.30 | |
| NYHA functional class | 0.03 | 0.70 | |
| Quality of Life | |||
| Generic (WHOQoL-Bref) | |||
| Total | 0.21 | 0.02 | |
| Domains | |||
| Physical | 0.13 | 0.16 | |
| Psychological | 0.28 | 0.001 | |
| Social | 0.08 | 0.36 | |
| Environmental | 0.21 | 0.01 | |
| Disease-specific (MLHFQ) | -0.09 | 0.29 | |
| Depression (PHQ-9) | -0.12 | 0.16 | |
| Religiosity (DUREL) | |||
| Total | 0.13 | 0.14 | |
| Intrinsic | 0.20 | 0.02 | |
| Organizational | 0.02 | 0.79 | |
| Non-organizational | -0.006 | 0.95 | |
| Spirituality (WHOQoL-SRPB) | |||
| Total | 0.26 | 0.003 | |
| Domains | |||
| Connect | 0.31 | < 0.0001 | |
| Meaning | 0.23 | 0.008 | |
| Awe | 0.27 | 0.002 | |
| Whole | 0.19 | 0.02 | |
| Strength | 0.21 | 0.02 | |
| Peace | 0.23 | 0.01 | |
| Hope | 0.19 | 0.03 | |
| Faith | 0.27 | 0.002 | |
REMADHE: Repetitive Education and Monitoring for Adherence for Heart Failure; NYHA: New York Heart Association; WHOQoL-Bref: World Health Organization Quality of Life; MLHFQ: Minnesota Living with Heart Failure Questionnaire; PHQ-9: Patient Health Questionnaire 9; DUREL: Duke University Religion Index; WHOQoL-SRPB: World Health Organization Quality of Life Spirituality, Religiosity and Personal Beliefs; r: indicates Spearman coefficients; p: for Spearman coefficients.
Figure 1.
Correlation plot between adherence (REMADHE) and spirituality (WHOQoL-SRPB) scores (Spearman coefficient = 0.26; p = 0.003)
Figure 2.
Score of spirituality (WHOQoL-SRPB) according to quartiles of adherence as per REMADHE score. p-value of 0.052 by Kruskal-Wallis test Error bars represent standard-deviation.
Spirituality was also found to be significantly correlated to other psychosocial variables evaluated. WHOQoL-SRPB was moderately correlated to both generic (WHOQoL-Bref [r = 0.47; p = 0.0001]) and disease-specific (MLHFQ [r = -0.34; p = 0.0001]) measures of quality-of-life. There was an inverse correlation between WHOQoL-SRPB and depression classification by PHQ-9 (r = -0.49; p < 0.0001). Of note, there was a positive correlation between WHOQoL-SRPB and religiosity assessed by DUREL (r= 0.55; p= 0.0001), which was also observed within domains of both instruments (Table 4).
Table 4.
Correlations between spirituality and religiosity scores
| DUREL | DUREL-ORA | DUREL-NORA | DUREL-IR | ||||||
|---|---|---|---|---|---|---|---|---|---|
| r | p | r | p | r | p | r | p | ||
| WHOQoL-SRPB | 0.55 | 0.0001 | 0.36 | 0.0001 | 0.29 | 0.001 | 0.57 | 0.0001 | |
| Connect | 0.54 | 0.0001 | 0.29 | 0.0001 | 0.34 | 0.0001 | 0.59 | 0.0001 | |
| Meaning | 0.38 | 0.0001 | 0.19 | 0.03 | 0.18 | 0.04 | 0.44 | 0.0001 | |
| Awe | 0.36 | 0.0001 | 0.27 | 0.02 | 0.10 | 0.25 | 0.38 | 0.0001 | |
| Whole | 0.47 | 0.0001 | 0.30 | 0.0001 | 0.27 | 0.002 | 0.48 | 0.0001 | |
| Strength | 0.49 | 0.0001 | 0.33 | 0.0001 | 0.28 | 0.001 | 0.51 | 0.0001 | |
| Peace | 0.39 | 0.0001 | 0.27 | 0.002 | 0.20 | 0.02 | 0.41 | 0.0001 | |
| Hope | 0.37 | 0.0001 | 0.29 | 0.001 | 0.22 | 0.01 | 0.31 | 0.0001 | |
| Faith | 0.54 | 0.0001 | 0.33 | 0.0001 | 0.34 | 0.0001 | 0.56 | 0.0001 | |
DUREL: Duke University Religion Index; ORA: organizational religious activity; NORA: non-organizational religious activity; IR: intrinsic religiosity; WHOQoL-SRPB: World Health Organization Quality of Life Spirituality, Religiosity and Personal Beliefs; r: indicates Spearman coefficient; p: for Spearman coefficients.
Among multivariable models to identify clinical and psychosocial variables associated to the presence of adequate adherence, WHOQoL-SRPB was an independent predictor when adjusted for demographics, clinical characteristics and psychosocial instruments (Table 5). Aside from WHOQoL-SRBP, DUREL was the only additional psychosocial instrument to demonstrate borderline significance for association to adequate adherence.
Table 5.
Logistic regression models for association of spirituality (WHOQoL-SRPB) to adequate adherence to therapy (REMADHE ≥ 18 points)
| Model 1 | β coefficient | OR (CI 95%) | p |
| WHOQoL-SRPB, 1-point increase | 1.01 | 2.76 (1.31 – 5.81) | 0.007 |
| Age, 1-year increase | -0.01 | 0.98 (0.95 – 1.01) | 0.32 |
| Ejection fraction, 1% increase | -0.01 | 0.98 (0.95 – 1.02) | 0.40 |
| Marital status, married | 0.56 | 1.75 (0.76 – 4.08) | 0.19 |
| Instruction, ≥ elementary school graduation | 0.31 | 1.36 (0.59 – 3.11) | 0.47 |
| Model 2 | β coefficient | OR (CI 95%) | p |
| WHOQoL-SRPB, 1-point increase | 1.17 | 3.23 (1.49 – 7.01) | 0.003 |
| Heart failure of ischemic etiology | -0.31 | 0.73 (0.32 – 1.67) | 0.45 |
| Implantable cardiac defibrillator | -0.91 | 0.40 (0.15 – 1.05) | 0.06 |
| Chronic kidney disease | -0.72 | 0.48 (0.21 – 1.08) | 0.08 |
| Marital status, married | -0.36 | 0.69 (0.31 – 1.57) | 0.38 |
| Model 3 | β coefficient | OR (CI 95%) | p |
| WHOQoL-SRPB | -0.12 | 4.89 (1.64 – 14.58) | 0.004 |
| WHOQoL-Bref | 1.59 | 1.03 (0.98 – 1.06) | 0.19 |
| MLHFQ | 0.03 | 1.02 (0.98 – 1.06) | 0.26 |
| PHQ-9 | 0.02 | 1.03 (0.92 – 1.16) | 0.60 |
| DUREL | 0.03 | 0.89 (0.79 – 1.00) | 0.05 |
WHOQoL-SRPB: World Health Organization Quality of Life Spirituality, Religiosity and Personal Beliefs; REMADHE: Repetitive Education and Monitoring for Adherence for Heart Failure; OR: odds ratio; CI: confidence interval; WHOQoL-Bref: World Health Organization Quality of Life; MLHFQ: Minnesota Living with Heart Failure Questionnaire; PHQ-9: Patient Health Questionnaire 9; DUREL: Duke University Religion Index.
Model 1 – adjusted for demographic and clinical variables selected by clinical significance;
Model 2 – adjusted for demographic and clinical variables selected by significance in univariate analyses;
Model 3 – adjusted for other psychosocial instruments of quality-of-life, depression and religiosity; Odds ratio represents the magnitude of association per 1-point increase in each score
Discussion
The main finding of the present study is that SRPB were consistently associated with adherence to treatment in a cohort of HF patients followed in a tertiary care clinic. Importantly, in our study, this association was independent of relevant demographic and clinical data known to influence adherence to HF management.
This is the first study to show a clear association of spirituality and adherence to treatment in HF. However, our study cannot determine if there is a direct effect of spirituality in adherence or if spirituality is only a marker of broader and more complex effect. For example, someone who is spiritualized is probably more prone to follow recommendations coming from someone he has a close relationship with (e.g., a physician). We identified three previous studies addressing the possible interactions between HF and spirituality.14,30,31 Black et al.14 sent a package of instruments (Spiritual Assessment Scale and the Heart Compliance Questionnaire) by mail to a convenience sample of 213 patients with a return rate of 45%. The authors did not find a significant correlation between spirituality and compliance. The study by Thomas30 using a convenience sample of 97 patients showed a positive result with moral-ethical-spiritual self which accounted for 10.8% of the variance in adherence. Dickson et al.31 studying socio-cultural influences on HF self-care in an ethnic minority, black population, using a mixed-methods strategy, found that spirituality was linked to self-care. More recently, issues related to wellbeing were shown to impact positively in patients with stage B asymptomatic HF - spirituality apparently played a role in mediating these effects.32
Although religiosity and spirituality have been associated with better healthcare practices, such observations failed to translate into better cardiovascular disease outcome in an adequately-powered study.33-35 The hypothesis that SRPB could affect compliance in chronic diseases and, particularly, in HF has also been raised by different authors.14,30,36 There are some possible models proposed to explain such relationship. Black et al.14 suggested that spiritual beliefs influence health beliefs which could lead to the practice of health-related activities such as the use of medications, control of weight, and diet compliance. Thomas30 applied the Roy's Self Concept model to identify several potential predictors of medical compliance.30,7 In this model, any stimulus is perceived either as a threat or a challenge to one's self-concept of body image, body sensation, self-consistency and moral-ethical-spiritual self. Briefly, stimuli perceived as a threat are reacted to in a negative way and consequently avoided, while stimuli perceived as a challenge are reacted to in a positive way and consequently followed. Thomas30 found that patients who perceived the HF regimen as a threat either to body image, self-consistency, body sensation or self-ideal were less likely to adhere to it. On the contrary, those to whom the regimen was perceived as a challenge to moral-ethical-spiritual self were most likely to adhere to medical therapy. Lastly, a recent survey conducted on HF patients showed that they would have welcomed spiritual care in their management.38
Our study has some limitations. First, as we used a cross-sectional design we can only conclude about association between spirituality and adherence, but not a causal relationship. Second, our sample was obtained in Brazil, a country where spirituality and religion are very notoriously important values. Additional studies are necessary to assess if these findings are replicable in different cultural and religious backgrounds. Finally, the effect of spirituality in adherence to different aspects of the HF management - pharmacological and non-pharmacological therapy - was not individually assessed. The REMADHE tool used in our study does not discriminate between the various components of the HF management in depth. If available, such information could be useful to better allocate the role of multidisciplinary care, vis a vis the spirituality of patients, and be taken into consideration accordingly, to improve patients' adherence.
Conclusions
Our study highlights that spirituality could be an important variable associated with adherence to treatment in the setting of outpatients with HF, suggesting that physicians and health professionals should be aware of its importance to improve clinical practice outcomes and implement measures to address the spiritual needs of patients. Further studies are warranted to better determine whether pharmacologic and non-pharmacologic measures in the management of HF are equally influenced by spirituality-related behavior.
Supplemental Table.
Adherence score according to demographics and clinical characteristics.
| REMADHE, points | p (t test) | ||
|---|---|---|---|
| Demographics | |||
| Age | |||
| < 60 | 15.9 ± 4.1 | 0.31 | |
| ≥ 60 | 16.6 ± 3.7 | ||
| Gender | |||
| Male | 16.6 ± 3.8 | 0.16 | |
| Female | 15.6 ± 4.2 | ||
| Ethnicity | |||
| Caucasian | 16.5 ± 3.9 | 0.23 | |
| Other | 15.2 ± 3.8 | ||
| Education | |||
| Elementary graduated or higher degree | 16.0 ± 3.8 | 0.56 | |
| Other | 16.5 ± 4.0 | ||
| Marital status | |||
| Married | 17.0 ± 4.1 | 0.01 | |
| Other | 15.2 ± 3.5 | ||
| Heart failure history | |||
| Etiology | |||
| Ischemic | 17.4 ± 3.6 | 0.02 | |
| Non-ischemic | 15.8 ± 4.0 | ||
| Ejection fraction | |||
| ≤ 35% | 16.4 ± 3.9 | 0.83 | |
| > 35% | 16.2 ± 3.9 | ||
| Functional class, NYHA | |||
| I-II | 16.1 ± 4.0 | 0.38 | |
| III-IV | 16.8 ± 3.7 | ||
| Cardiac Defibrillator | |||
| Yes | 17.7± 3.2 | 0.05 | |
| No | 16.0 ± 4.1 | ||
| Admissions in the previous year | |||
| None | 16.1 ± 4.0 | 0.52 | |
| Any | 16.6 ± 3.8 | ||
| Comorbidities | |||
| Hypertension | |||
| Yes | 16.6 ± 3.7 | 0.34 | |
| No | 15.9 ± 4.2 | ||
| Previous myocardial infarction | |||
| Yes | 17.2 ± 3.6 | 0.11 | |
| No | 15.9 ± 4.0 | ||
| Previous cardiac surgery | |||
| Yes | 16.5 ± 4.4 | 0.8 | |
| No | 16.3 ± 3.9 | ||
| Diabetes | |||
| Yes | 16.0 ± 3.7 | 0.50 | |
| No | 16.5 ± 4.0 | ||
| Chronic kidney impairment | |||
| Yes | 17.2 ± 3.8 | 0.04 | |
| No | 15.8 ± 3.9 | ||
| Previous stroke | |||
| Yes | 16.6 ± 2.7 | 0.69 | |
| No | 16.3 ± 4.1 | ||
| Smoking, past or present | |||
| Yes | 14.3 ± 4.1 | 0.28 | |
| No | 15.8 ± 4.2 | ||
| Alcoholism, past or present | |||
| Yes | 16.1 ± 4.0 | 0.34 | |
| No | 16.9 ± 3.7 | ||
| Neoplasia | |||
| Yes | 15.6 ± 4.4 | 0.38 | |
| No | 16.4 ± 3.9 | ||
Footnotes
Sources of Funding
This study was funded by Fundo de Incentivo à Pesquisa do Hospital das Clínicas de Porto Alegre.
Study Association
This article is part of the thesis of master submitted by Juglans Souto Alvarez, from Universidade Federal do Rio Grande do Sul.
References
- 1.Jaarsma T, van der Wal MH, Lesman-Leegte I, Luttik ML, Hogenhuis J, Veeger NJ, et al. Effect of moderate or intensive disease management program on outcome in patients with heart failure Coordinating Study Evaluating Outcomes of Advising and Counseling in Heart Failure (COACH) Arch Intern Med. 2008;168(3):316–324. doi: 10.1001/archinternmed.2007.83. [DOI] [PubMed] [Google Scholar]
- 2.Artinian NT, Magnan M, Sloan M, Lange MP. Self-care behaviors among patients with heart failure. Heart Lung. 2002;31(3):161–172. doi: 10.1067/mhl.2002.123672. [DOI] [PubMed] [Google Scholar]
- 3.Riegel B, Moser DK, Anker SD, Appel LJ, Dunbar SB, Grady KL, et al. State of the science promoting self-care in persons with heart failure: a scientific statement from the American Heart Association. Circulation. 2009;120(12):1141–1163. doi: 10.1161/CIRCULATIONAHA.109.192628. [DOI] [PubMed] [Google Scholar]
- 4.Murray SA, Kendall M, Grant E, Boyd K, Barclay S, Sheikh A. Patterns of social, psychological, and spiritual decline toward the end of life in lung cancer and heart failure. J Pain Symptom Manage. 2007;34(4):393–402. doi: 10.1016/j.jpainsymman.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 5.Ni H, Nauman D, Burgess D, Wise K, Crispell K, Hershberger RE. Factors influencing knowledge of and adherence to self-care among patients with heart failure. Arch Intern Med. 1999;159(14):1613–1619. doi: 10.1001/archinte.159.14.1613. [DOI] [PubMed] [Google Scholar]
- 6.Moser DK, Doering LV, Chung ML. Vulnerabilities of patients recovering from an exacerbation of chronic heart failure. Am Heart J. 2005;150(5):984. doi: 10.1016/j.ahj.2005.07.028. [DOI] [PubMed] [Google Scholar]
- 7.Wu JR, Moser DK, De Jong MJ, Rayens MK, Chung ML, Riegel B, et al. Defining an evidence-based cutpoint for medication adherence in heart failure. Am Heart J. 2009;157(2):285–291. doi: 10.1016/j.ahj.2008.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krantz MJ, Ambardekar AV, Kaltenbach L, Hernandez AF, Heidenreich PA, Fonarow GC. Patterns and predictors of evidence-based medication continuation among hospitalized heart failure patients (from Get With the Guidelines-Heart Failure) Am J Cardiol. 2011;107(12):1818–1823. doi: 10.1016/j.amjcard.2011.02.322. [DOI] [PubMed] [Google Scholar]
- 9.Fonarow GC, Yancy CW, Heywood JT. Adherence to heart failure quality-of-care indicators in US hospitals analysis of the ADHERE Registry. Arch Intern Med. 2005;165(13):1469–1477. doi: 10.1001/archinte.165.13.1469. [DOI] [PubMed] [Google Scholar]
- 10.Bekelman DB, Dy SM, Becker DM, Wittstein IS, Hendricks DE, Yamashita TE, et al. Spiritual well-being and depression in patients with heart failure. J Gen Intern Med. 2007;22(4):470–477. doi: 10.1007/s11606-006-0044-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jones AM, O'Connell JE, Gray CS. Living and dying with congestive heart failure addressing the needs of older congestive heart failure patients. Age Ageing. 2003;32(6):566–568. doi: 10.1093/ageing/afg120. [DOI] [PubMed] [Google Scholar]
- 12.Westlake C, Dracup K. Role of spirituality in adjustment of patients with advanced heart failure. Prog Cardiovasc Nurs. 2001;16(3):119–125. doi: 10.1111/j.0889-7204.2001.00592.x. [DOI] [PubMed] [Google Scholar]
- 13.Park CL, Aldwin CM, Choun S, George L, Suresh DP, Bliss D. Spiritual peace predicts 5-year mortality in congestive heart failure patients. Health Psychol. 2016;35(3):203–210. doi: 10.1037/hea0000271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Black G, Davis BA, Heathcotte K, Mitchell N, Sanderson C. The relationship between spirituality and compliance in patients with heart failure. Prog Cardiovasc Nurs. 2006;21(3):128–133. doi: 10.1111/j.0889-7204.2006.04804.x. [DOI] [PubMed] [Google Scholar]
- 15.Stewart WC, Adams MP, Stewart JA, Nelson LA. Review of clinical medicine and religious practice. J Relig Health. 2013;52(1):91–106. doi: 10.1007/s10943-012-9578-9. [DOI] [PubMed] [Google Scholar]
- 16.Carvalho VO, Guimaraes GV, Carrara D, Bacal F, Bocchi EA. Validation of the Portuguese version of the Minnesota Living with Heart Failure Questionnaire. Arq Bras Cardiol. 2009;93(1):39–44. doi: 10.1590/s0066-782x2009000700008. [DOI] [PubMed] [Google Scholar]
- 17.Bocchi EA, Cruz F, Guimaraes G, Pinho Moreira LF, Issa VS, Ayub Ferreira SM, et al. Long-term prospective, randomized, controlled study using repetitive education at six-month intervals and monitoring for adherence in heart failure outpatients the REMADHE trial. Circ Heart Fail. 2008;1(2):115–124. doi: 10.1161/CIRCHEARTFAILURE.107.744870. [DOI] [PubMed] [Google Scholar]
- 18.Taunay TC, Gondim Fde A, Macêdo DS, Moreira-Almeida A, Gurgel LA, Andrade LM, et al. Validity of the Brazilian version of the Duke Religious Index (DUREL) Rev Psiquiatr Clin. 2012;39(4):130–135. [Google Scholar]
- 19.Panzini RG, Maganha C, Rocha NS, Bandeira DR, Fleck MP. Brazilian validation of the Quality of Life Instrument/spirituality, religion and personal beliefs. Rev Saude Publica. 2011;45(1):153–165. doi: 10.1590/s0034-89102011000100018. [DOI] [PubMed] [Google Scholar]
- 20.Santos IS, Tavares BF, Munhoz TN, Almeida LS, Silva NT, Tams BD, et al. Sensitivity and specificity of the Patient Health Questionnaire-9 among adults from the general population. Cad Saúde Pública. 2013;29(8):1533–1543. doi: 10.1590/0102-311x00144612. [DOI] [PubMed] [Google Scholar]
- 21.Fleck MP, Louzada S, Xavier M, Chachamovich E, Vieira G, Santos L, et al. Application of the Portuguese version of the abbreviated instrument of quality life WHOQOL-bref. Rev Saude Publica. 2000;34(2):178–183. doi: 10.1590/s0034-89102000000200012. [DOI] [PubMed] [Google Scholar]
- 22.Mussi CM, Ruschel K, de Souza EN, Lopes AN, Trojahn MM, Paraboni CC, et al. Home visit improves knowledge, self-care and adhesion in heart failure: Randomized Clinical Trial HELEN-I. Rev Lat Am Enfermagem. 2013;21 Spec No:20–28. doi: 10.1590/s0104-11692013000700004. [DOI] [PubMed] [Google Scholar]
- 23.Psychol Med. 3. Vol. 28. The WHOQOL Group; 1998. Development of the World Health Organization WHOQOL-BREF quality of life assessment; pp. 551–558. [DOI] [PubMed] [Google Scholar]
- 24.Rector TS, Cohn JN. Am Heart J. 4. Vol. 124. Pimobendan Multicenter Research Group; 1992. Assessment of patient outcome with the Minnesota Living with Heart Failure questionnaire reliability and validity during a randomized, double-blind, placebo-controlled trial of pimobendan; pp. 1017–1025. [DOI] [PubMed] [Google Scholar]
- 25.Kubo SH, Schulman S, Starling RC, Jessup M, Wentworth D, Burkhoff D. Development and validation of a patient questionnaire to determine New York Heart Association classification. J Card Fail. 2004;10(3):228–235. doi: 10.1016/j.cardfail.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 26.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.de Lima Osorio F, Vilela Mendes A, Crippa JA, Loureiro SR. Study of the discriminative validity of the PHQ-9 and PHQ-2 in a sample of Brazilian women in the context of primary health care. Perspect Psychiatr Care. 2009;45(3):216–227. doi: 10.1111/j.1744-6163.2009.00224.x. [DOI] [PubMed] [Google Scholar]
- 28.Koenig HG, Bussing A. The Duke University Religion Index (DUREL) a five-item measure for use in epidemiological studies. Religions. 2010;1(1):78–85. [Google Scholar]
- 29.WHOQOL SRPB Group A cross-cultural study of spirituality, religion, and personal beliefs as components of quality of life. Soc Sci Med. 2006;62(6):1486–1497. doi: 10.1016/j.socscimed.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 30.Thomas CM. The influence of self-concept on adherence to recommended health regimens in adults with heart failure. J Cardiovasc Nurs. 2007;22(5):405–416. doi: 10.1097/01.JCN.0000287037.85067.3d. [DOI] [PubMed] [Google Scholar]
- 31.Dickson VV, McCarthy MM, Howe A, Schipper J, Katz SM. Sociocultural influences on heart failure self-care among an ethnic minority black population. J Cardiovasc Nurs. 2013;28(2):111–118. doi: 10.1097/JCN.0b013e31823db328. [DOI] [PubMed] [Google Scholar]
- 32.Mills PJ, Redwine L, Wilson K, Pung MA, Chinh K, Greenberg BH, et all The Role of Gratitude in Spiritual Well-being in Asymptomatic Heart Failure Patients. Spiritual Clin Pract (Wash D C ) 2015;2(1):5–17. doi: 10.1037/scp0000050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oman D, Kurata JH, Strawbridge WJ, Cohen RD. Religious attendance and cause of death over 31 years. Int J Psychiatry Med. 2002;32(1):69–89. doi: 10.2190/RJY7-CRR1-HCW5-XVEG. [DOI] [PubMed] [Google Scholar]
- 34.Kark JD, Shemi G, Friedlander Y, Martin O, Manor O, Blondheim SH. Does religious observance promote health mortality in secular vs religious kibbutzim in Israel. Am J Public Health. 1996;86(3):341–346. doi: 10.2105/ajph.86.3.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Feinstein M, Liu K, Ning H, Fitchett G, Lloyd-Jones DM. Burden of cardiovascular risk factors, subclinical atherosclerosis, and incident cardiovascular events across dimensions of religiosity The multi-ethnic study of atherosclerosis. Circulation. 2010;121(5):659–666. doi: 10.1161/CIRCULATIONAHA.109.879973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Naghi JJ, Philip KJ, Phan A, Cleenewerck L, Schwarz ER. The effects of spirituality and religion on outcomes in patients with chronic heart failure. J Relig Health. 2012;51(4):1124–1136. doi: 10.1007/s10943-010-9419-7. [DOI] [PubMed] [Google Scholar]
- 37.Roy C, Whetsell MV, Frederickson K. The Roy adaptation model and research. Nurs Sci Q. 2009;22(3):209–211. doi: 10.1177/0894318409338692. [DOI] [PubMed] [Google Scholar]
- 38.Ross L, Austin J. Spiritual needs and spiritual support preferences of people with end-stage heart failure and their carers implications for nurse managers. J Nurs Manag. 2015;23(1):87–95. doi: 10.1111/jonm.12087. [DOI] [PubMed] [Google Scholar]