Abstract
Introduction
The objective of this study was to determine the association between sociodemographic factors and the elimination of allergen sources from homes of asthmatic children.
Method
In a cross-sectional analysis of data from 845 asthmatic children, multiple linear regression investigated the association between socioeconomic factors and failure to reduce allergen sources (i.e., stuffed toys, pets, carpeting, curtains, and cushions); failure to use linen covers; and not laundering linens weekly in hot water. Logistic regression assessed the relationship between socioeconomic status and exposure to environmental tobacco smoke.
Results
Mother’s employment status was significantly associated with the quality of the home environment (P = .0002). Homemakers demonstrated fewer poor practices (3.1) compared with full-time or part-time employed mothers (3.6). Children whose mothers reported no post-secondary education were more likely to have environmental tobacco smoke exposure compared with those who had a post-secondary CE education or higher (OR 2.4, 95% CI 1.7, 3.5).
Discussion
Children whose mothers worked at home and were better educated were at reduced risk for exposure to sources of indoor allergens.
Keywords: Asthma, disease management, children, socioeconomic status, allergen, environment
Asthma is the most common chronic pediatric condition, with a prevalence of nearly 9% in the United States (Akinbami, 2006). Asthma causes significant morbidity and reduces quality of life in children and their families (Public Health Agency of Canada, 2000). A poor indoor environment aggravates asthma in children and poses a barrier to achieving asthma control. Thus, the Canadian Pediatric Asthma Consensus guidelines and the U.S. National Asthma Education and Prevention Program guidelines recommend strategies to manage asthma, including identifying allergens and engaging in behavior to reduce exposures in sensitized children (Becker et al., 2005; National Heart, Lung & Blood Institute [NHLBI], 2007). Similarly, guidelines from Australia, Britain, and the Global Initiative for Asthma recommend environmental control practices (British Thoracic Society [BTS], 2005; Global Initiative for Asthma [GINA], 2005; National Asthma Council Australia [NACA], 2006).
Asthma prevalence is higher among children from low-income families (Crain et al., 1994; Evans, 1992; Halfon & Newacheck, 1993; Weitzman, Gortmaker, & Sobol, 1990; Wissow, Gittelsohn, Szklo, Starfield, & Mussman, 1988) and is often more severe (Erzen et al., 1997; Mielck, Reitmeir, & Wjst, 1996). Among U.S. inner-city children, the most common risk factors for asthma morbidity were household environmental exposures (Krieger, Song, Takaro, & Stout, 2000; Warman, Silver, & Wood, 2006). The home has been recognized as an important source of environmental exposures and as a target for interventions to improve asthma management (Swartz, Banasiak, & Meadows-Oliver, 2005). One study found that that were no differences in the environmental control practices among inner-city families compared with other families, despite a worse asthma status (Hansel et al., 2006). Data from the Childhood Asthma Management Program (CAMP) study found that home exposures to allergens reported by children or parents that exacerbate the child’s asthma were surprisingly common (Weiss, Horner, Shapiro, & Sternberg, 2001). These findings suggest a need to raise awareness regarding the importance of reducing risks in the home environment.
Evidence suggests that children who are sensitive to dust mites benefit from home visits to counsel on allergen avoidance and asthma management (Carter, Perzanowski, Raymond, & Platts-Mills, 2001; Nishioka, Saito, Akiyama, & Yasueda, 2006). Similarly, an intervention based on behavioral and physical strategies demonstrated success in reducing exposure to airborne particulate matter in the bedrooms of low-income asthmatic children (Eggleston et al., 2005).
The literature suggests that lower socioeconomic status may be associated with greater exposure to environmental allergens. To reduce exposure, parents must engage in risk reduction behavior. While studies have surveyed parents on exposures to specific allergens such as dust and molds, few have directly examined whether parents engage in the practices needed to reduce children’s exposures to allergens. In addition, few studies have examined the effect of socioeconomic status on home environment risk reduction. The primary objective of this study was to determine the association between socioeconomic factors and home environment risk reduction behavior in households with asthmatic children. A secondary objective was to determine the association between socioeconomic factors and exposure to environmental tobacco smoke (ETS).
METHODS
Study Design
Cross-sectional data from a clinical study conducted between November 2000 and March 2003 were analyzed. The data were collected from a sample of 879 children or their parents with recruitment stratified by site to represent the spectrum of asthma severity. Recruitment sites included a pediatric respiratory practice, an allergy practice, a 19-physician family practice, two outpatient hospital-based asthma clinics, and two hospital emergency departments. The inclusion criteria were boys and girls aged between 1 and 18 years residing in Ontario, Canada, with a clinical diagnosis of asthma or reactive airway disease documented in their medical record and a prescription for an anti-asthmatic medication in the previous year. This approach would enable inclusion of likely cases of persistent as well as intermittent asthma (Kozyrskyj, Mustard, & Becker, 2004). Complete records on 845 children were available and used in the analysis. Excluded records were missing data on socioeconomic status and health services use. Parents provided written informed consent and children assented. The study was approved by the Research Ethics Board of the Toronto Hospital for Sick Children.
Data
The database included information collected in face-to-face interviews using structured questionnaires with parents and with children older than 12 years regarding family demographics, socioeconomic status, home environment, exposure to ETS, drug plan access, asthma history, health services use, frequency of symptoms including cough, wheeze, and shortness of breath, and asthma medication and spacer use. The following questions regarding the home environment were included:
“Are any furry animals or birds kept inside your home environment?” (Yes/No)
“Does your bedroom have (check all that apply): wall-to-wall carpeting; curtains; upholstered or soft furnishings such as a soft chair; stuffed animals or stuffed toys; mattress and pillows covered in airtight covers; bed sheets and pillow cases that are washed in hot water weekly; a room located in the basement.”
“Please tell me whether the following items worsen your asthma (check all that apply): cat or other animal; pollen or ragweed; dust; air pollution; cigarette smoke; colds/sinus infections; cold air; strong smells, paints, or perfumes; weather changes; exercise; seasons (spring or late summer).”
“Are you presently exposed to second-hand smoke on a regular basis (check all that apply): at home; in a car; at work; at school; at day care; at other peoples’ homes; in public places (e.g., malls, restaurants); somewhere else.”
Analyses were undertaken in SAS 9.1 (SAS Institute Inc., Cary, NC). This study assessed the number of home environment risk reduction practices undertaken based on a count of nine binary variables. A lower score indicated fewer risks present in the home environment. These variables included seven measures representing common sources of allergens in a child’s bedroom (presence of stuffed animals/toys; wall-to-wall carpeting; curtains; upholstered or soft furnishings; absence of airtight covers on pillows or mattress; bed sheets and pillowcases not washed weekly in hot water; bedroom in the basement) and the presence of pets (furry animal or bird). Exposure to ETS also was ascertained. Table 1 indicates how each variable was defined.
TABLE 1.
Home environment risk variables
| Indicator | Variable description |
|---|---|
| Toys | Presence of stuffed animals or toys (Y/N) |
| No airtight covers | Mattress and pillow NOT covered in airtight covers (Y/N) |
| Basement | Child’s bedroom located in the basement (Y/N) |
| Carpet | Wall-to-wall carpeting in child’s bedroom (Y/N) |
| Curtains | Curtains in child’s bedroom (Y/N) |
| Cushions | Upholstered or soft furnishings in child’s bedroom (Y/N) |
| Covers not washed | Bed sheets and pillowcases NOT washed in hot water weekly (Y/N) |
| Pets | Furry animal or bird in the home (Y/N) |
| Environmental tobacco smoke | Child exposed to second-hand smoke in home, car, day care, other people’s home, public places, school, work, or elsewhere (Y/N) |
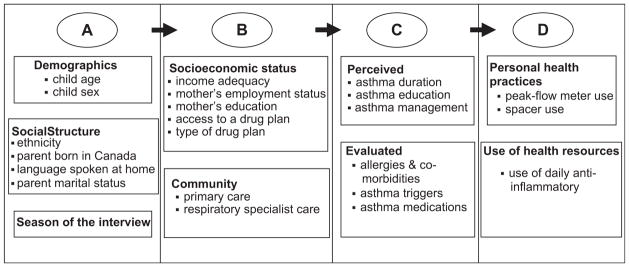
Explanatory variables were selected based on a literature review of the determinants of asthma control in children. As presented in Figure 1, Andersen’s conceptual framework (Andersen, 1995) was adapted to this patient population to group potential explanatory variables into the following categories: Demographics (age, child sex), Social Structure (ethnicity, parent born in Canada, primary language spoken at home, parent marital status, season of the interview), Community (primary care visits in past 6 months, respiratory specialist visits in past 6 months), Need (asthma duration, asthma education, receipt of an asthma action plan, co-morbidities, number of asthma triggers, asthma medication regimen), and Health Care Use (peak-flow meter use, spacer use, use of daily anti-inflammatory medication). The five separate variables that reflected Socioeconomic Status included income adequacy (household income adjusted for family size [(Statistics Canada, 1995]), mother’s employment status, mother’s education, access to a drug plan, and type of plan.
FIGURE 1.
Determinants of asthma control in children. A, predisposing characteristics; B, enabling resources; C, need; D, health care use. Data from Andersen, R. M., 1995.
Statistical Analysis
A forward stepwise linear regression was used to analyze the number of poor home environment practices present with a range from zero to nine. Initially, univariate regression models were developed with each explanatory variable. Any explanatory variable that had a univariate coefficient with a probability of greater than 0.2 was eliminated.
Intermediate linear regression models
The conceptual model presented in Figure 1 provided the framework and rationale for grouping related variables together and testing them for significance. Because of the many potential explanatory variables, the construction of a multiple linear regression model proceeded in stages. A number of separate regression models were created corresponding to categories from the adapted Andersen framework, including Demographics, Need, Community, and Health Care Use. The explanatory variables within each category were regressed on the number of indicators of poor environment control. Explanatory variables were entered into the category model sequentially according to the highest adjusted R square value associated with their univariate statistics.
Main regression model
The variables in the Socioeconomic Status category were initially entered into the main model because they were the primary focus of the analysis. Sex and age group were retained because of their established clinical relevance. Next, the Social Structure variables were entered, which provided the secondary focus of the model. Variables from the intermediate regression models previously described then were entered into the main model from the highest to lowest adjusted R square values associated with each intermediate regression model.
In the main model, all of the variables were added one at a time and were retained if the probability associated with the regression coefficient was less than 0.05. The tolerance in the main model was evaluated after the addition of each explanatory variable to assess colinearity. If the tolerance was less than or equal to 0.1, the variable was removed (Yu & Tempe, 2000). After each variable was added to the model, interactions with all of the preceding terms in the model were tested independently. Any interaction term that was significant at the 5% level was added to the model. At each step, any term that did not retain significance was removed. For significant variables with more than two categories, multiple comparisons were performed using the Student-Newman-Keuls test to determine which groups were significantly different at the 5% level. All regression coefficients were estimated adjusted for other covariates and were reported with 95% confidence intervals (CIs).
Logistic regression
A forward stepwise logistic regression was conducted based on whether a child was exposed to ETS. The same process used for building the linear regression model was applied to select and order the explanatory variables entered into the logistic model. If significant correlations existed between the explanatory variables at the 5% level, the least significant variables were removed to reduce colinearity. The Likelihood Ratio Test was used to remove non-significant independent variables from the model, and the Pearson χ2 goodness of fit test was used to test the overall fit of the model. Odds ratios were determined with 95% CIs.
RESULTS
Sample Characteristics
Of 879 children or their parents in the recruited sample, complete records on 845 children were available. With respect to asthma triggers (cat, dust, pollen, air pollution, cigarette smoke, colds/sinus infections, cold air, strong smells, weather changes, exercise, and seasonal effects), 6% of respondents reported only one, 7% reported two, 11% reported three, 13% reported four, and 62% reported five or more. In the previous 6 months, the mean number of primary care visits was 2.5 (standard deviation [SD] 3.4, Median = 1.0), and the mean number of respiratory specialist visits was 1.4 (SD 2.1, Median = 1.0). Sample demographics are presented in Table 2.
TABLE 2.
Sample characteristics (n = 845)
| Characteristic | |
|---|---|
| Child age, mean (SD) | 6.9 (4.2) |
| ≤4 y | 32% |
| >4 to <10 y | 43% |
| ≥10 y | 24% |
| Child sex | |
| Male | 61% |
| Female | 39% |
| Mother’s education | |
| Post-secondary education | 71% |
| Less than post-secondary education | 29% |
| Mother’s ethnicity | |
| Canadian/North American | 48% |
| European/East European | 21% |
| Other | 31% |
| Primary care visits in previous 6 mo, mean (SD); median | 2.5 (3.4); 1.0 |
| Asthma triggers, mean (SD) | 5.5 (2.6) |
| Currently taking at least one daily dose of anti-inflammatory agent | 53% |
| Exposed to environmental tobacco smoke | 22% |
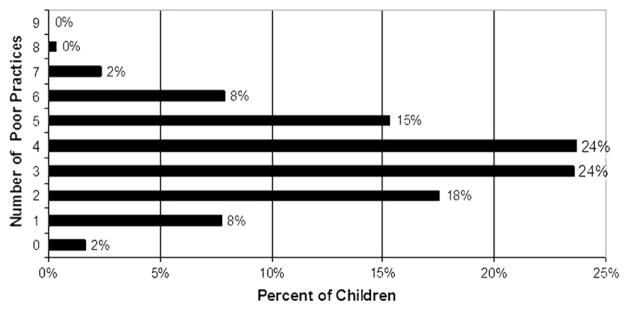
Figure 2 illustrates the distribution of children’s exposure to poor risk reduction behaviors. Only 2% reported the absence of all nine home environment risks, while most children were exposed to three or four home environment risks, with an average of 3.5 per child (SD 1.6). The most prevalent indicators of a poor environment in the child’s bedroom included lack of mattress or pillow covers, presence of stuffed animals or toys, wall-to-wall carpeting, and curtains, which were present for 76%, 69%, 55% and 45% of children, respectively. Exposure to ETS was reported for 22% of children, while 35% of homes had a furry pet. For most cases, linens were washed weekly in hot water, although 15% of children had cushions in their bedrooms and 5% had bedrooms in the basement.
FIGURE 2.
Count of poor risk reduction behaviors.
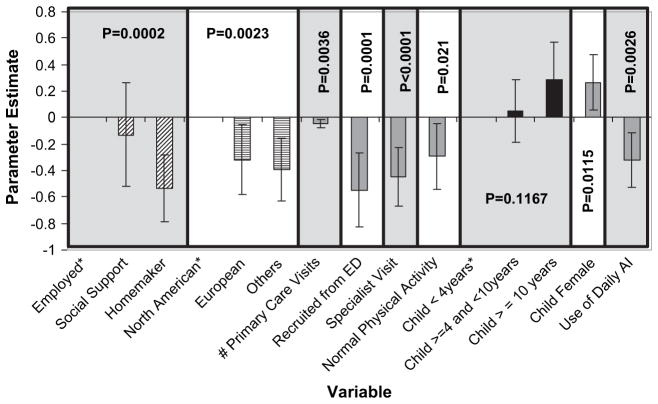
Indoor Environment and Sociodemographic Status
It was hypothesized that lower sociodemographic status may be associated with fewer practices aimed at reducing allergens sources in the home. Figure 3 displays the explanatory variable regression coefficients and confidence intervals to demonstrate the size and direction of effect of each variable. The mother’s employment was significant (P = .0002) among the markers of family socioeconomic status. Compared with full-time or part-time employed mothers and compared with those receiving welfare benefits or who were students, homemakers demonstrated significantly fewer poor practices (P = .05). The mean number of poor practices present in each of these three subgroups was 3.6, 3.5, and 3.1, respectively.
FIGURE 3.
Significant explanatory variables in linear regression of number of poor home environment practicesValues are variable regression coefficients adjusted for all other covariatesVertical bars represent 95% confidence intervalsEmployed, mother was employed or self-employed (full-time or part-time); Social Support, mother was receiving social assistance, disability support, or was a student; Homemaker, mother was a homemaker; North American, Canadian or North American; European, European or East European; Others, other ethnicity; # Primary Care Visits, number of primary care visits in the past 6 months; recruited from the ED, recruited from an emergency department versus an outpatient recruitment site; Specialist Visits, had a respiratory specialist visit in the past 6 months; Normal Physical Activity, physical activity level compared with other children was normal or more active; Use of Daily AI, used anti-inflammatory asthma medication at least once per day. *Indicates a reference category.
Ethnicity also was significant (P = .0023). Toronto is a highly multi-ethnic city, and more than 15 separate ethnic backgrounds were reported. For the purpose of analysis, children were classified as North American, European (including East European), or other ethnicity. These groups were associated with a mean exposure to 3.7, 3.4, and 3.3 poor practices, respectively. North American children were exposed to more poor practices compared with other groups. The analysis demonstrated fewer poor practices (a better home environment) with more previous primary care visits (P = .0036) and with a previous respiratory specialist visit (P < .0001). A better home environment also was associated with recruitment of study subjects from an emergency department compared with an outpatient site (P = .0001), with physical activity normal or better than peers (P = .021) and with daily use of an anti-inflammatory asthma medication (P = .0026). The child’s age was not a significant predictor of poor home environment (P = .1167). The sex of the child was important, with more poor practices reported for girls (P = .0115). Receipt of asthma education or an asthma action plan was not significantly associated with fewer poor practices.
Environmental Tobacco Smoke Exposure and Sociodemographic Status
The logistic regression analysis examined whether lower socioeconomic status was associated with ETS exposure. As seen in Table 3, the final model was significant (P < .0001) and included mother’s education (P < .0001) and child age (P < .0001) and was adjusted for child sex. Children from families where the mother reported no post-secondary (post–high school) education were more likely to have exposure to ETS compared with those with a post-secondary education or higher (odds ratio 2.4; 95% CI 1.7, 3.5). The child’s age was positively associated with exposure to tobacco smoke.
TABLE 3.
Significant explanatory variables in logistic regression of exposure to environmental tobacco smoke
| Explanatory variable | Regression coefficient | Probability | Odds ratio | Odds ratio, 95% confidence interval |
|---|---|---|---|---|
| Mother’s post-secondary education (no vs. yes) | 0.4423 | <.0001 | 2.422 | (1.692, 3.466) |
| Child age (y) | 0.1467 | <.0001 | 1.158 | (1.113, 1.205) |
| Sex (female vs. male) | −0.0237 | 0.7928 | 0.954 | (0.669, 1.359) |
DISCUSSION
Controlling allergen exposures in the home is an important element of asthma management promulgated by Canadian and American practice guidelines (Becker et al., 2005; NHLBI, 2007). This study indicates that a number of environmental control behaviors that could reduce exposure of children with asthma to sources of allergens are not being practiced. The reasons can be complex and may relate to parental, child, and health practitioner factors. Health care practitioners may not be conveying the importance of environmental control behavior to parents or parents may not be adhering to the advice they receive. Our study indicated that the extent of behavior to reduce the risk of allergen exposure in the home is related to employment status of the mother. Compared with working mothers or those receiving government benefits, the children of homemakers were exposed to significantly fewer poor practices. Homemakers may be able to better monitor their child’s asthma and practice enhanced indoor environmental control.
The child’s ethnicity was also a significant factor. Compared with European or other ethnicities, North American children were exposed to more sources of allergens in the home. This finding may reflect disparate social, cultural, and behavioral practices. While ethnicity may be an important social structure factor, it is complex and difficult to compare across geographic regions.
This study found that a previous respiratory specialist visit was associated with better risk reduction behavior. This finding was supported by a previous study, which suggested that a specialist visit improved the likelihood that a caregiver has received advice and has implemented an environmental control program (Hansel et al., 2006). Similarly, increased primary care visits and daily controller medication use may suggest a more informed or proactive caregiver.
The results showed that compared with children recruited from outpatient offices, children from the emergency department had exposure to fewer sources of allergens in the home. These children may have represented a more severe subgroup of asthmatics whose parents improved their environmental control practices subsequent to their emergency department experience. Because of the cross-sectional nature of the analysis, a causal relationship between behavior and significant covariates cannot be confirmed. When asthmatic children recruited from the emergency department were examined previously, a significant relationship between indoor environmental exposure to allergens and health-care utilization, morbidity, or severity was not found (Hansel et al., 2006; Teach, Crain, Quint, Hylan, & Joseph, 2006).
Studies from the United States indicated that asthmatic children from low-income families often are sensitized to multiple allergens to which they are frequently exposed (Crain et al., 2002; Perry et al., 2006), including cockroaches, dust mites, and molds (Gruchalla et al., 2005). Although information on skin testing was not available for the present study, the total number of triggers that were reported as worsening asthma was not significantly associated with the number of poor practices. This finding is consistent with the previous finding that environmental control practices were independent of the child’s allergen sensitizations (Hansel et al., 2006).
International asthma guidelines agree that a smoke-free environment is recommended for children (Becker et al., 2005; BTS, 2005; GINA, 2005; NACA, 2006; NHLBI, 2007). In the present study, 22% of subjects reported ETS exposure. This finding is similar to those of other studies that reported exposure rates of 28% and 25% in children with asthma (Leech, Wilby, & McMullen, 1999; Warman et al., 2006). Approximately 70% of the study mothers had some level of post-secondary education, which is above the national average. The logistic regression demonstrated that children whose mothers had no post-secondary education had a 140% higher probability of being exposed to ETS. An inverse relationship between socioeconomic status and the rate of smoking has been documented in the United States and Canada (Finkelstein et al., 2002; Rudick, Anthonisen, & Manfreda, 1993). This finding emphasizes the importance of targeting lower socioeconomic families for comprehensive educational interventions that address the child’s indoor environment as well as the caregiver’s health behavior.
This study had several limitations. Because the analysis was cross-sectional, causation could not be inferred from the observed significant associations. Longitudinal studies are required to determine the health consequences of exposure to indoor allergens as a function of socioeconomic status. While the database included information on whether children received asthma education or an asthma action plan, it is not known if specific advice regarding avoidance of home allergens was received. The children in this study were selected using a clustered sampling strategy, which may have over-represented children from higher socioeconomic families and those with more severe asthma. All of the data were self- or parent proxy-reported, and accuracy was therefore dependent upon participant recall. Reports of health services by parent proxy respondents in this study showed good to excellent agreement with administrative data (Ungar, Davidson-Grimwood, & Cousins, 2007). The study sample represented a broad urban and suburban population of children with asthma. It will be important to quantify the characteristics of the indoor environment for children in rural and other geographic areas, because of differences in housing types and allergen sensitivities (Gruchalla et al., 2005). Subsequent to pilot testing, to enhance the accuracy of responses, potentially sensitive interview questions regarding direct exposure to cockroaches and other known asthma allergens in the home were removed. Rather, questions about behaviors to remove potential sources of allergens were posed. While cockroaches represent an important allergen for asthmatic children, the benefits of programs to reduce cockroach allergen have not been clearly substantiated (Teach et al., 2006). In contrast, an intervention aimed at reducing a variety of indoor allergens (including cockroaches) and ETS using an educational component in combination with a remediation program successfully reduced symptoms among inner-city asthmatic children (Morgan et al., 2004). A child’s bedroom has been associated with elevated concentrations of dust mite allergens and is more predictive of the exposure to common aeroallergens compared to single risk factors (Perry et al., 2006). Therefore, a focus on behaviors aimed at reducing multiple risk factors in the child’s bedroom is favored.
In conclusion, this study showed that sociodemographic factors related to the presence of the mother and her education were associated with important differences in risk reduction behaviors in the home environment. These findings have relevance to the practices of a variety of health providers, including physicians, nurses, asthma educators, respiratory therapists, and pharmacists, all of whom play complementary roles in asthma education and management. The findings can be incorporated into existing nursing practice and asthma educator asthma education programs to strengthen the emphasis on home environmental control. They can be the subject of direct information targeted campaigns designed to improve patient and caregiver awareness of and compliance with environmental control practices (Carter et al, 2001; Finkelstein et al., 2002; Hansel et al., 2006; Soussan et al., 2003; Warman et al., 2006). Because children spend such a large proportion of their time indoors and in their bedrooms, understanding the need to avoid allergens is a critical component to achieving asthma control in this vulnerable population. Health practitioners are well positioned to raise awareness regarding the importance of these practices.
Acknowledgments
Funded by operating grants from AllerGen Network Centre for Excellence and the Canadian Institutes for Health Research to Wendy J. Ungar, MSc, PhD. The funding sources had no involvement in study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
The contributions of Dr. Peter Bikangaga, Dr. Milton Gold and Dr. Teresa To are gratefully acknowledged.
Contributor Information
Wendy J. Ungar, Senior Scientist, Child Health Evaluative Sciences, The Hospital for Sick Children, Toronto, Canada; Associate Professor, Department of Health Policy, Management and Evaluation, University of Toronto, Canada; and Adjunct Scientist, Institute for Clinical Evaluative Sciences, Sunnybrook Health Sciences Centre, Toronto, Canada.
Shannon F. Cope, Research Coordinator, Child Health Evaluative Sciences, The Hospital for Sick Children, Toronto, Canada; and MSc Graduate, Department of Health Policy, Management and Evaluation, University of Toronto, Canada.
Anita Kozyrskyj, Research Scientist, Faculty of Pharmacy; Departments of Community Health Sciences, and Pediatrics and Child Health, Faculty of Medicine, Manitoba Centre for Health Policy, University of Manitoba, Winnipeg, Canada.
J. Michael Paterson, Scientist, Institute for Clinical Evaluative Sciences, Sunnybrook Health Sciences Centre, Toronto, Canada; and Scientist, Centre for Evaluation of Medicines, Hamilton; and Department of Family Medicine, McMaster University, Hamilton, Canada.
References
- Akinbami L. Centers for Disease Control and Prevention National Center for Health Statistics. The state of childhood asthma, United States, 1980–2005. Advance Data. 2006;381:1–24. [PubMed] [Google Scholar]
- Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior. 1995;36:1–10. [PubMed] [Google Scholar]
- Becker A, Berube D, Chad Z, Dolovich M, Ducharme F, D’Urzo T, et al. Canadian Pediatric Asthma Consensus guidelines, 2003 (updated to December 2004) Canadian Medical Association Journal. 2005;173(6 Suppl):S12–S14. doi: 10.1503/cmaj.045064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- British Thoracic Society. British Guideline on the Management of Asthma. Scottish Intercollegiate Guidelines Network; 2005. Retrieved July 1, 2007, from http://www.sign.ac.uk/pdf/sign63.pdf. [Google Scholar]
- Carter MC, Perzanowski MS, Raymond A, Platts-Mills TA. Home intervention in the treatment of asthma among inner-city children. Journal of Allergy and Clinical Immunology. 2001;108:7327–7337. doi: 10.1067/mai.2001.119155. [DOI] [PubMed] [Google Scholar]
- Crain EF, Walter M, O’Connor GT, Mitchell H, Gruchalla RS, Kattan M, et al. Home and allergic characteristics of children with asthma in seven U.S. urban communities and design of an environmental intervention: The Inner-City Asthma Study. Environmental Health Perspectives. 2002;110:939–945. doi: 10.1289/ehp.02110939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crain EF, Weiss KB, Bijur PE, Hersh M, Westbrook L, Stein REK, et al. An estimate of the prevalence of asthma and wheezing among nner-city children. Pediatrics. 1994;94:356– 362. [PubMed] [Google Scholar]
- Eggleston PA, Butz A, Rand C, Curtin-Brosnan J, Kanchanaraksa S, Swartz L, et al. Home environmental intervention in inner-city asthma: A randomized controlled clinical trial. Annals of Allergy, Asthma & Immunology. 2005;95:518–524. doi: 10.1016/S1081-1206(10)61012-5. [DOI] [PubMed] [Google Scholar]
- Erzen K, Carriere K, Dik N, Mustard C, Roos L, Manfreda J, et al. Income level and asthma prevalence and care patterns. American Journal of Respiratory and Critical Care Medicine. 1997;155:1060–1065. doi: 10.1164/ajrccm.155.3.9116987. [DOI] [PubMed] [Google Scholar]
- Evans R., III Asthma among minority children: A growing problem. Chest. 1992;101(6 Suppl):368S–371S. [PubMed] [Google Scholar]
- Finkelstein JA, Fuhlbrigge A, Lozano P, Grant EN, Shulruff R, Arduino KE, et al. Parent-reported environmental exposures and environmental control measures for children with asthma. Archives of Pediatrics & Adolescent Medicine. 2002;156:258–264. doi: 10.1001/archpedi.156.3.258. [DOI] [PubMed] [Google Scholar]
- Global Initiative for Asthma. Pocket guide for asthma management and prevention in children. 2005 Retrieved July 1, 2007, from http://www.ginasthma.org/Guidelineitem.asp?I1=2&I2=1&intId=1171.
- Gruchalla RS, Pongracic J, Plaut M, Evans R, III, Visness CM, Walter M, et al. Inner City Asthma Study: Relationships among sensitivity, allergen exposure, and asthma morbidity. Journal of Allergy and Clinical Immunology. 2005;115:478–485. doi: 10.1016/j.jaci.2004.12.006. [DOI] [PubMed] [Google Scholar]
- Halfon N, Newacheck PW. Childhood asthma and poverty: Differential impacts and utilization of health services. Pediatrics. 1993;91:56–61. [PubMed] [Google Scholar]
- Hansel NN, Eggleston PA, Krishnan JA, Curtin-Brosnan J, Rand CS, Patino CM, et al. Asthma-related health status determinants of environmental control practices for inner-city preschool children. Annals of Allergy, Asthma & Immunology. 2006;97:409–417. doi: 10.1016/S1081-1206(10)60809-5. [DOI] [PubMed] [Google Scholar]
- Kozyrskyj AL, Mustard CA, Becker AB. Identifying children with persistent asthma from health care administrative records. Canadian Respiratory Journal. 2004;11:141–145. doi: 10.1155/2004/976852. [DOI] [PubMed] [Google Scholar]
- Krieger JW, Song L, Takaro TK, Stout J. Asthma and the home environment of low-income urban children: Preliminary findings from the Seattle-King County health homes project. Journal of Urban Health. 2000;77:50–67. doi: 10.1007/BF02350962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leech JA, Wilby K, McMullen E. Environmental tobacco smoke exposure patterns: A subanalysis of the Canadian Human Time-Activity Pattern Survey. Canadian Journal of Public Health. 1999;90:244–249. doi: 10.1007/BF03404125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mielck A, Reitmeir P, Wjst M. Severity of childhood asthma by socioeconomic status. International Journal of Epidemiology. 1996;25:388–393. doi: 10.1093/ije/25.2.388. [DOI] [PubMed] [Google Scholar]
- Morgan WJ, Crain EF, Gruchalla RS, O’Connor GT, Kattan M, Evans R, III, et al. Results of a home-based environmental intervention in urban children with asthma. New England Journal of Medicine. 2004;351:1068–1080. doi: 10.1056/NEJMoa032097. [DOI] [PubMed] [Google Scholar]
- National Asthma Council Australia. Asthma Management Handbook. Melbourne, Australia: Author; 2006. [Google Scholar]
- National Heart Lung & Blood Institute. Expert Panel Report 3 (EPR-3): Guidelines for the diagnosis and management of asthma—2007. 2007 Retrieved December 3, 2007, from http://www.nhlbi.nih.gov/guidelines/asthma/index.htm.
- Nishioka K, Saito A, Akiyama K, Yasueda H. Effect of home environment control on children with atopic or non-atopic asthma. Allergology International. 2006;55:141–148. doi: 10.2332/allergolint.55.141. [DOI] [PubMed] [Google Scholar]
- Perry TT, Wood RA, Matsui EC, Curtin-Brosnan J, Rand C, Eggleston PA, et al. Room-specific characteristics of suburban homes as predictors of indoor allergen concentrations. Annals of Allergy, Asthma & Immunology. 2006;97:628–635. doi: 10.1016/S1081-1206(10)61092-7. [DOI] [PubMed] [Google Scholar]
- Public Health Agency of Canada. The prevention and management of asthma in Canada: A report from the National Asthma control Task Force. 2000 Retrieved July 1, 2007, from http://www.phac-aspc.gc.ca/publicat/pma-pca00/index.html.
- Rudick C, Anthonisen N, Manfreda J. Recruiting healthy participants for a large clinical trial. Controlled Clinical Trials. 1993;14:685–795. doi: 10.1016/0197-2456(93)90025-9. [DOI] [PubMed] [Google Scholar]
- Soussan D, Liard R, Zureik M, Touron D, Rogeaux Y, Neukirch F, et al. Treatment compliance, passive smoking, and asthma control: A three year cohort study. Archives of Diseases in Childhood. 2003;88:229–233. doi: 10.1136/adc.88.3.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistics Canada. National Population Health Survey 1994–95. Ottawa, Ontario, Canada: Author; 1995. National Population Health Survey—Household Component—Longitudinal public usemicrodata files. [Google Scholar]
- Swartz MK, Banasiak NC, Meadows-Oliver M. Barriers to effective pediatric asthma care. Journal of Pediatric Health Care. 2005;19:71–79. doi: 10.1016/j.pedhc.2004.10.006. [DOI] [PubMed] [Google Scholar]
- Teach S, Crain E, Quint D, Hylan M, Joseph J. Indoor environmental exposures among children with asthma seen in an urban emergency department. Pediatrics. 2006;117(Suppl 4):S152–S158. doi: 10.1542/peds.2005-2000M. [DOI] [PubMed] [Google Scholar]
- Ungar WJ, Davidson-Grimwood S, Cousins M. Parents were accurate proxy reporters of urgent pediatric asthma health services—a retrospective agreement analysis. Journal of Clinical Epidemiology. 2007;60:1176–1183. doi: 10.1016/j.jclinepi.2007.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warman K, Silver EJ, Wood PR. Asthma risk factor assessment: What are the needs of inner-city families? Annals of Allergy, Asthma & Immunology. 2006;97(1 Suppl 1):S11–S15. doi: 10.1016/s1081-1206(10)60779-x. [DOI] [PubMed] [Google Scholar]
- Weiss ST, Horner A, Shapiro G, Sternberg AL. The prevalence of environmental exposure to perceived asthma triggers in children with mild-to-moderate asthma: Data from the Childhood Asthma Management Program (CAMP) Journal of Allergy & Clinical Immunology. 2001;107:634–640. doi: 10.1067/mai.2001.113869. [DOI] [PubMed] [Google Scholar]
- Weitzman M, Gortmaker S, Sobol A. Racial, social, and environmental risks for childhood asthma. American Journal of Diseases in Childhood. 1990;144:1189–1194. doi: 10.1001/archpedi.1990.02150350021016. [DOI] [PubMed] [Google Scholar]
- Wissow LS, Gittelsohn AM, Szklo M, Starfield B, Mussman M. Poverty, race, and hospitalization for childhood asthma. American Journal of Public Health. 1988;78:777–782. doi: 10.2105/ajph.78.7.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu CH. An overview of remedial tools for collinearity in SAS. Paper presentated at the 2000 Western Users of SAS Software Conference; Scottsdale, AZ. 2000. [Google Scholar]