Abstract
Aims
To determine whether abstinence or relapse on a quit attempt in the previous year is associated with current depressive symptoms.
Design
Prospective cohort with approximately annual waves. Mixed effect logistic regressions tested whether Time 2 (T2) quitting status was associated with reporting symptoms at T2, and whether Time 1 (T1) symptoms moderated this relationship.
Setting
Waves 5 to 8 of the Four Country International Tobacco Control Study: a quasi-experimental cohort study of smokers from Canada, USA, UK and Australia.
Participants
6978 smokers who participated in telephone surveys.
Measurements
T1 and T2 depressive symptoms in the last 4 weeks assessed with two screening items from the PRIME-MD questionnaire. Quitting status at T2: 1) No attempt since T1; 2) Attempted and relapsed; 3) Attempted and abstinent at T2.
Findings
Compared with no attempt, relapse was associated with reporting T2 symptoms (OR=1.46, 95% CI:1.33,1.59). Associations between T2 quitting status and T2 symptoms were moderated by T1 symptoms. Relapse was positively associated with T2 symptoms for those without T1 symptoms (OR=1.71, 95% CI:1.45,2.03) and those with T1 symptoms (OR=1.45, 95% CI:1.23,1.70). Abstinence was positively associated for those without T1 symptoms (OR=1.37, 95% CI:1.10,1.71) and negatively associated for those with T1 symptoms (OR=0.74, 95% CI:0.59,0.94). Age significantly moderated these associations. Relapse did not predict T2 symptoms for those aged 18 to 39 irrespective of T1 symptoms. The negative effect of abstinence on T2 symptoms for those with T1 symptoms was significant only for those aged 18 to 39 (OR = 0.61, 95% CI = 0.40, 0.94) and 40 to 55 (OR = 0.58, 95% CI = 0.40, 0.84). The positive effect of abstinence on T2 symptoms for those without T1 symptoms was significant only for those aged over 55 (OR = 1.97, 95% CI = 1.35, 2.87).
Conclusions
Most people who stop smoking appear to be at no greater risk of developing symptoms of depression than if they had continued smoking. However, people over age 55 who stop smoking may be at greater risk of developing symptoms of depression than if they had continued smoking.
Keywords: Smoking cessation, depression, relapse, abstinence
People with a lifetime history of a depressive disorder are more likely to smoke tobacco, and to smoke more heavily, than people without a history of any psychiatric disorder [1]. There are several plausible hypotheses used to explain the relationship: 1) smoking predisposes people to depressive symptoms, 2) depressive symptoms predispose people to smoking 3) there is a reciprocal relationship in which smoking contributes to the development of depression and once addicted is maintained through self-medication, or 4) that a third shared factor (e.g., neuroticism or stressful environments) predisposes people to both smoking and depression.
Biological models suggest that for addicted smokers the effect of removal of nicotine on neurobiological systems via smoking cessation can lead to increased depressive symptoms [2]. Smokers report that they smoke to alleviate negative mood and for enjoyment [3]. Similarly, some health professionals also believe that quitting smoking may precipitate or exacerbate depression in susceptible people [4]. However, empirical studies from population cohorts and clinical trials addressing this issue provide evidence to the contrary. The evidence is increasing that successful abstinence does not exacerbate depression and may reduce it.
A recent meta-analysis of longitudinal studies examining the impact of smoking cessation on mental health from population cohorts and clinical trials concluded that quitting smoking is associated with fewer symptoms of depression and anxiety [5]. There is also evidence that trying to quit and failing is predictive of increased symptoms of depression and anxiety [6, 7, 8, 9], and this association may be stronger in those with pre-existing clinical disorders [10]. It is possible that those who believe that smoking helps to manage mood may be more likely to relapse when early depressive symptoms occur during a quit attempt. However, two studies have found that smokers who believe cigarettes help manage stress actually reported lower stress levels after quitting ([10, 11].
A population based study by Bolam et al. [12] followed a cohort of smokers interested in quitting for 9 months, and found that abstinence was not associated with reporting depression or anxiety. However, they only included participants who were symptom free at baseline, thus they were not able to examine change in the mental health of people who were already symptomatic. Other longitudinal population cohorts have examined change in measures of depression or negative affect between pre- and post-quitting and found that abstinence from smoking has no effect on depressed mood [13] and may even mitigate depression [14].
Experimental studies with participants from a clinical population have followed smokers with a history of depression for 6 to 12 months following interventions for smoking cessation and found that abstinence did not increase the likelihood of experiencing depressive symptoms [15–19]. Indeed, in three studies [15,16,17], abstinence was associated with lower levels of depressive symptoms. Smoking cessation has also been linked to increased wellbeing [20,5]. In contrast, Hughes’ review [21] found that a history of clinical depression was associated with post-cessation depression, but noted methodological problems including selection bias, small samples, and a lack of adequate controls. In a randomised trial by Glassman et al. [22], increased depression was observed among abstainers compared to non-abstainers, but there was a far higher loss to follow-up among the relapsers.
Using a population-based sample, the current study aims 1) to determine whether abstinence or relapse on a quit attempt increases the likelihood of subsequently reporting either of the two core symptoms of depression (a loss of interest or pleasure and depressed mood); 2) to test whether depressive symptoms at T1 moderate the effect of quit status on depressive symptoms at T2; 3) To explore interactions between covariates (demographic variables and nicotine dependence) with quit status.
Method
Participants
Data came from 6978 participants in waves 5 to 8 (2006/2007 – 2010/2011) of the International Tobacco Control Four Country (ITC-4) project as key questions on depressive symptoms were only asked from wave 5 onwards. The ITC-4 is a quasi-experimental cohort survey of smokers in Canada, UK, USA, and Australia conducted via computer-assisted telephone interview and followed up on an annual basis. Using a stratified random-digit dialling procedure, households are contacted and screened for adult smokers (18 years and older) with the next birthday who would agree to participate in the study. Respondents were considered smokers at recruitment if they reported smoking at least 100 cigarettes in their lifetime and smoking at least once in the past 30 days. A detailed description of the ITC study conceptual framework [23] and methodology [24] can be found elsewhere. The study protocol had clearance in each of the four countries. Respondents were eligible for the current study if they provided valid data on all variables for both the baseline wave (waves 5, 6, and 7; designated as T1) and the follow-up wave (waves 6, 7, and 8; designated as T2), and were daily smokers at T1. Between waves 7 and 8, a subset of USA participants took part in additional data collection (n = 462) and their quitting activity data was aggregated with wave 8 data. Respondents could participate in a maximum of three pairs of waves. The attrition rate for the ITC-4 was 28.8% between waves 5 to 6, 26.7% between waves 6 and 7, and 28.7% between waves 7 and 8.
Design
Depressive symptoms reported at T2 were predicted from quitting activity between T1 and T2 (assessed at T2) and depressive symptoms reported at T1. There were four waves of data, i.e. three T1 to T2 comparisons.
Measures
Depressed mood and low positive affect
Depressive symptoms at T2 were the outcome of interest, which were computed as a binary measure of reporting either or both of the following two items from the Primary Care Evaluation of Mental Disorders Procedure questionnaire [25]: “During the last month, have you often been bothered by little interest or pleasure in doing things?” and “During the last month, have you often been bothered by feeling down, depressed, or hopeless?”. These are core symptoms of a depressive episode defined by the DSM-IV, and the binary measure has excellent sensitivity (96%) and moderate specificity (57%) [26]. Depressive symptoms at T1 were included as a covariate.
Quitting activity
Quitting status at T2 was the main covariate of interest. At each follow-up wave, respondents were asked whether they had made any attempts to quit smoking since the last survey (Yes or No; approximately 12 months between surveys). Those who had attempted were asked whether they were still stopped or back smoking. A variable was formed that included 1) Made no quit attempt, 2) Made a quit attempt and relapsed, which included people whose attempt lasted less than 24 hours (3% to 4%), and 3) Made a quit attempt and still abstinent. For each analysis, the reference category was ‘Made no quit attempt’.
Demographic variables
Demographic variables included age at recruitment (18–39, 40–54, and 55+ years), gender, country of residence (Canada, USA, UK, or Australia), education and income (low, moderate or high). Education and income were categorised according to appropriate criteria within each country.
Other covariates
Nicotine dependence was assessed at each wave using the Heaviness of Smoking Index [27], ranging from 0 to 6 (HSI), based on the number of cigarettes smoked per day (0 = 0–10 cigarettes per day; 1 = 11–20; 2 = 21–30; 3 = 31+), and time to first cigarette (0 = 61+min; 1 = 31–60 min; 2 = 6–30 min; 3 = 5 min or less). The HSI was recoded into three dependence categories: Low = 0; Moderate = 1–3; and High = 4–6.
Self-rated physical health was assessed with two questions: “In general, how would you describe your health?” Responses were rated on a five-point scale from (1 = ‘Poor’ to 5 = ‘Excellent’), and “To what extent, if at all, has smoking damaged your health?” (1 = ‘Not at all’ to 4 = ‘A great deal’).
Analysis plan
We explored whether quitting status (no quit attempt, relapsed, abstinent) at T2 was associated with reporting depressive symptoms at T2, while controlling for demographics, HSI, and reported symptoms at the wave prior (T1). We tested whether reported symptoms at T1 moderated the association between quit status and reported symptoms at T2 with the inclusion of an interaction term between these two variables. Interactions with the following variables were tested for moderating effects on T2 symptoms: Age, gender, country, income, education and HSI.
We used mixed-effects logistic regression (MELR) models to account for clustering of outcomes by individual (repeated measures) and by country. Mixed effects models contain both fixed and random effects. The inclusion of random effects for individual and country allows for a subject- and country-specific interpretation of the fixed effect of quit status on depression at T2. We compared 3 mixed-effects models using likelihood ratio tests with significant alpha at p < 0.05 and Akaike’s Information Criterion: 1) A random intercept for individuals; 2) We added a random intercept for country; 3) Because we cannot assume that the effect of quit status on depression is consistent across countries, we added a random effect for quit status by country to investigate potential between-country heterogeneity in the effects. The data was analysed with STATA 14.
Results
Table 1 shows the demographic characteristics of the sample at each wave. The characteristics of the sample remained fairly consistent across the three sets of waves. 44% of respondents reported one or both symptoms at waves 5 and 6, but only 37% did so at wave 7. Over 12% of the sample also reported that they had been told by a health professional that they had depression in the previous year.
Table 1.
Characteristics of the sample at each wave.
| Wave 5 to 6 n = 4676 |
Wave 6 to 7 n = 4717 |
Wave 7 to 8 n = 3710 |
|
|---|---|---|---|
| Mean no. days between T1 & T2 | 335 (sd = 40) | 394 (sd = 50) | 600 (sd = 61) |
| Age | |||
| 18 to 39 | 29.0 | 26.1 | 23.5 |
| 40 to 55 | 42.4 | 43.4 | 43.8 |
| 55 and over | 28.6 | 30.5 | 32.7 |
| Gender | |||
| Female | 57.6 | 57.3 | 56.3 |
| Country | |||
| Canada | 25.1 | 25.8 | 26.2 |
| USA | 22.9 | 23.6 | 22.8 |
| UK | 25.2 | 23.9 | 26.7 |
| Australia | 26.8 | 26.7 | 24.3 |
| Income | |||
| Low | 30.5 | 29.6 | 29.3 |
| Moderate | 33.9 | 32.9 | 32.3 |
| High | 29.3 | 30.8 | 31.1 |
| Refused | 6.4 | 6.7 | 7.3 |
| Education | |||
| Low | 52.9 | 51.9 | 52.5 |
| Moderate | 31.0 | 31.3 | 30.1 |
| High | 16.1 | 16.9 | 17.4 |
| Depressive symptoms at T1 | |||
| Neither symptom | 56.0 | 56.5 | 63.4 |
| At least one symptom | 44.0 | 43.5 | 36.6 |
| Health professional diagnosed depression in last 12 months (T1) | 14.1 | 13.6 | 12.1 |
| Quit attempt between T1 & T2 | |||
| No attempt | 63.6 | 62.6 | 56.5 |
| Relapsed | 25.9 | 26.1 | 31.1 |
| Abstinent | 10.5 | 11.3 | 12.4 |
To select the best fitting MELR model, we compared a model (model 1) that included a random intercept for individuals with a model (model 2) that also included a random intercept for country and found the latter was better (LR chi2=5.64, p=0.018). We then compared model 2 with a model (model 3) that also included a random coefficient for quitting status at T2 by country and found no significant improvement in model fit (LR chi2=2.58, p=0.108), indicating there was no significant between country heterogeneity in the effect of quit status on depression outcomes. Thus, model 2 was chosen as the final model and odds ratios reported here are for the fixed effects estimates from MELRs with random intercepts for individual and country.
Column 1 of Table 2 shows the results of the MELR model predicting either or both depressive symptom at T2 among our entire sample. The following covariates were significantly positively associated with reporting either symptom at T2: a high HSI score, reporting either symptom at T1, and relapse on the last quit attempt at T2. In contrast, those aged 55 and over, living in the UK, and having moderate to high income and education were significantly less likely to report symptoms at T2. We ran a sensitivity test with quit attempts less than 24 hours counted as ‘no attempt’, and there was no effect on the outcome. Sensitivity analyses removing anyone with a quit attempt that started in the month prior to T2 did not change the outcomes either.
Table 2.
Mixed effect logistic regression analyses for predictors of reporting symptoms vs. no symptoms at T2.
| All respondents n = 6978, Observations = 13103 |
Reported one or both symptoms at T1 n = 3747, Observations = 5468 |
No reported symptoms at T1 n = 4766, Observations = 7635 |
|
|---|---|---|---|
| Adjusted Odds Ratios | Adjusted Odds Ratios | Adjusted Odds Ratios | |
| Age | |||
| 18 to 39 | Reference | Reference | Reference |
| 40 to 55 | 0.94 (0.85, 1.03) | 0.96 (0.80,1.15) | 0.87 (0.72,1.05) |
| 55 and over | 0.78 (0.70, 0.87) | 0.74 (0.60,0.90) | 0.71 (0.57,0.87) |
| Gender | |||
| Female | Reference | Reference | Reference |
| Male | 0.93 (0.86, 1.01) | 0.94 (0.81,1.10) | 0.89 (0.76,1.04) |
| Income | |||
| Low | Reference | Reference | Reference |
| Moderate | 0.71 (0.64, 0.78) | 0.68 (0.56,0.82) | 0.61 (0.50,0.75) |
| High | 0.62 (0.56, 0.69) | 0.47 (0.38,0.58) | 0.61 (0.49,0.75) |
| No response | 0.70 (0.59, 0.82) | 0.53 (0.39,0.72) | 0.77 (0.56, 1.06) |
| Education | |||
| Low | Reference | Reference | Reference |
| Moderate | 0.87 (0.80, 0.95) | 0.85 (0.72,1.01) | 0.85 (0.72,1.02) |
| High | 0.89 (0.80, 0.999) | 0.93 (0.74,1.16) | 0.82 (0.66,1.02) |
| Heaviness of Smoking | |||
| Low | Reference | Reference | Reference |
| Moderate | 0.98 (0.85,1.14) | 1.18 (0.89,1.56) | 0.88 (0.68,1.15) |
| High | 1.23 (1.05, 1.44) | 1.71 (1.27,2.30) | 1.04 (0.78,1.38) |
| Symptoms at T1 | |||
| Neither | Reference | — | — |
| One or both | 4.64 (4.30, 5.02) | — | — |
| Status at T2 | |||
| No quit attempt | Reference | Reference | Reference |
| Relapse | 1.46 (1.33,1.59) | 1.45 (1.23,1.70) | 1.71 (1.45,2.03) |
| Abstinent | 1.04 (0.91, 1.18) | 0.74 (0.59,0.94) | 1.37 (1.10,1.71) |
The interaction between T1 symptoms and the HSI was significant (p = .002). A high HSI score predicted a higher prevalence of symptoms at T2 only among those who reported symptoms at T1. The interaction between the HSI and quitting status at T2 was not significant.
The interaction between reporting either depressive symptom at T1 and quitting status at T2 was significant (p < 0.001). Table 2 shows the results of separate (MELR) models for those who reported either symptom at T1 (column 2) and those who did not (column 3). The reference category was ‘No quit attempt’. Among those who reported at least one symptom at T1, relapse significantly predicted a higher prevalence of either symptom at T2. However, abstinence significantly predicted a lower prevalence of either symptom. Among respondents who reported neither symptom at T1, both relapse and abstinence were significantly associated with a higher prevalence of either symptom at T2. Figure 1 illustrates the association between quitting status and symptoms at T2 stratified by reported symptoms at T1.
Figure 1.
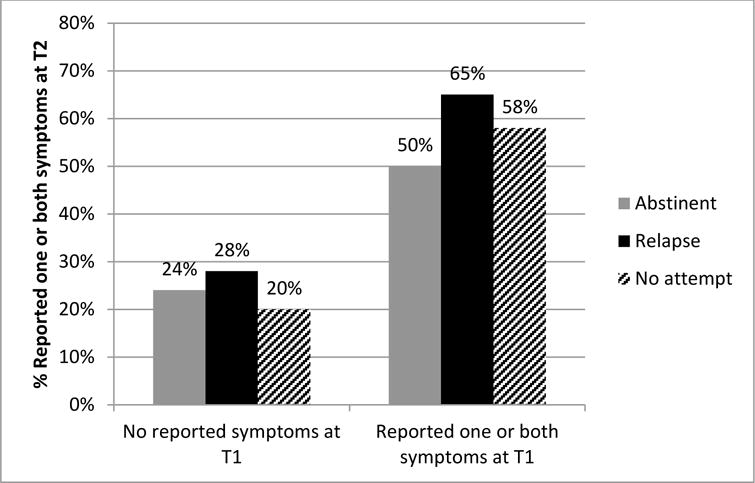
This figure shows data from all observations included in the study. The percentage that reported one or two symptoms at T2 (y-axis) is stratified by reported symptoms at T1 (x-axis) and smoking status at T2 (columns).
Total number of observations: No symptoms at T1 = 7,635, 63% no attempt; 24.5% relapse; 12.1% abstinent; One or both symptoms at T1 = 5,468, 58.1% no attempt; 31.6% relapse; 10.2% abstinent.
We then explored whether any of these relationships could be explained by differences in physical health concerns in post-hoc analyses where we added our two measures to the (MELR) analyses (results not shown in table). The effect of relapse on reported symptoms was attenuated, but still significant, both among those who reported no symptoms at T1 (OR = 1.42, 95% CI = 1.20, 1.67) and those who did report symptoms at T1 (OR = 1.21, 95% CI = 1.03, 1.42). The association between abstinence and reporting depressive symptoms at T2 was unchanged.
The interaction between quitting status at T2 and age was significant, both among those who reported symptoms at T1 (p = .009) and those who were symptom free at T1 (p = .009). Separate analyses were repeated for each age group (results not shown in table). As above, ‘No quit attempt’ was the reference condition. In the group reporting symptoms at T1 (Figure 2), abstinence was significantly associated with a lower prevalence of reported symptoms at T2 in those aged 18 to 39 (OR = 0.61, 95% CI = 0.40, 0.94) and 40 to 55 (OR = 0.58, 95% CI = 0.40, 0.84). Relapse was significantly associated with a higher prevalence of reported symptoms in those aged 40 to 55 (OR = 1.56, 95% CI = 1.23, 1.99) and aged over 55 (OR = 1.86, 95% CI = 1.36, 2.53). In those who did not report symptoms at T1 (Figure 3), abstinence was significantly associated with a higher prevalence of reported symptoms only in those aged over 55 (OR = 1.97, 95% CI = 1.35, 2.87). Relapse was also significantly associated with a higher prevalence of reported symptoms among those aged 40 to 54 (OR = 2.11, 95% CI = 1.61, 2.76) and those aged 55 and over (OR = 1.83, 95% CI = 1.36, 2.45).
Figure 2.
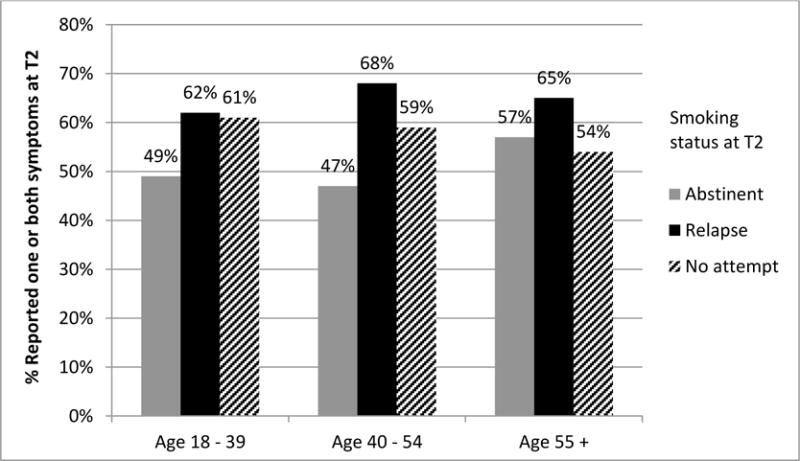
This figure includes observations from only those who reported symptoms at T1. The percentage that reported one or two symptoms at T2 (y-axis) is stratified by age group (x-axis) and smoking status at T2 (columns).
Total number of observations: Age 18 to 39 = 1,552, 57.2% no attempt; 31.3% relapse; 11.5% abstinent. Age 40 to 55 = 2,410, 59.3% no attempt; 31.5% relapse; 9.2% abstinent. Age 55+ = 1,506, 57.3% no attempt; 32.2% relapse; 10.6% abstinent.
Figure 3.
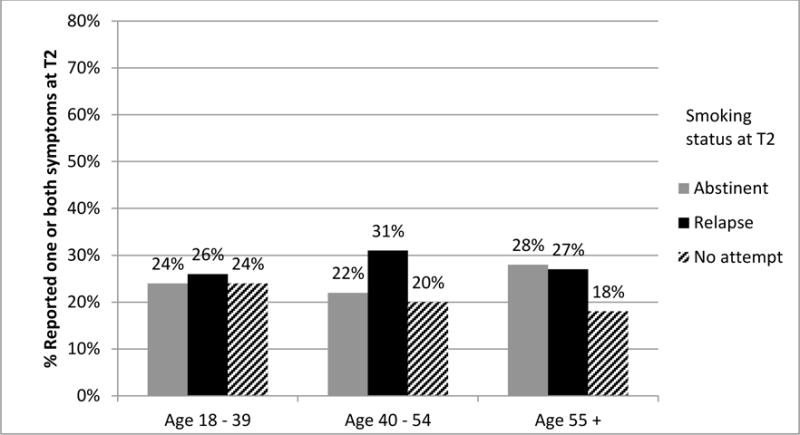
This figure includes observations from only those who reported no symptoms at T1. The percentage that reported one or two symptoms at T2 (y-axis) is stratified by age group (x-axis) and smoking status at T2 (columns).
Total number of observations: Age 18 to 39 = 1,911, 60.6% no attempt; 25.3% relapse; 14.0% abstinent. Age 40 to 55 = 3,245, 66.0% no attempt; 23.1% relapse; 10.8% abstinent. Age 55+ = 2,479, 62.2% no attempt; 25.5% relapse; 12.2% abstinent.
Given the interaction between age and quitting, we hypothesised that this could be because older smokers were more concerned by adverse physical health effects, so we tested for any potential effect.
Again, we explored possible effects of reported physical health effects and age, separately for those with and without T1 symptoms. We found some differences to the above analyses. In the group who reported symptoms at T1, the effect of relapse among those aged over 55 was no longer significant (OR = 1.32, 95% CI = 0.96, 1.81). Other effects were attenuated: In those who did not report symptoms at T1, the effect of relapse on reported symptoms among those aged 40 to 55 was now OR = 1.70, 95% CI = 1.31, 2.22, and for those aged over 55 it was OR = 1.40, 95% CI = 1.04, 1.89. The effect of abstinence was also attenuated in those aged over 55 (OR = 1.59, 95% CI = 1.09, 2.32).
Discussion
The prevalence of reporting depression was above average estimates of the prevalence in the community (e.g., the 2007 Australian National Survey of Mental Health and Wellbeing [28] reported a 12 month prevalence of 4.1% for a depressive episode and 1.3% for dysthymia). This is consistent with smokers being more likely to suffer depressive mood disorders than non-smokers [1].
Consistent with previous studies, reporting depressive symptoms at T1 was the strongest predictor of reporting depressive symptoms at T2 [e.g.,12]. Compared to not making a quit attempt, relapse among smokers aged over 40 was associated with poorer mental health outcomes regardless of symptoms at T1. For those maintaining abstinence, T1 symptoms made a difference. Among those with symptoms at T1, abstinence (opposed to no attempt) was associated with improved mental health if under age 55. But for those who did not have T1 symptoms, abstinence was associated with worse mental health, but only among those over 55. When the effects of perceived physical health were controlled for, the associations between both relapse and abstinence and worse mental health were attenuated while the association between abstinence and improved mental health was not affected.
Our findings support previous research [6, 7, 8, 9] which suggests that unsuccessful quit attempts may be a risk factor for psychological distress, but we found this occurred only among smokers aged over 40. A possible explanation for this is that failed quit attempts may be more disappointing (thus generating negative affect) to older smokers because they have a longer history of failed quit attempts, or because the consequences of failing are more salient (i.e., they have reached an age where smoking-related adverse health effects are common). The moderating effect of perceived physical health on the association between relapsing and depressive symptoms is consistent with this latter explanation.
An important positive finding of this study was that smokers younger than 55 who reported depressive symptoms prior to quitting smoking went on to report improvements in these symptoms after successfully quitting. This is consistent with previous research. Smokers who can withstand the early unpleasant effects of withdrawal may benefit in the long term, possibly because they are no longer subjected to repeated mood fluctuations between cigarettes [29] and because abstinence is associated with increased self-esteem, a more positive outlook on life, greater satisfaction with recreation activities, a better standard of living and are happier with their homes [20]. It may be helpful to advise smokers that any deterioration in mood is likely to be short-lived with long-term gains likely to be positive. It has also been shown that with the appropriate care from health professionals, smokers with a history of clinical depression can successfully quit without compromising their psychological health [18].
The association between successful quitting and depressive symptoms in smokers aged over 55 who were free from these symptoms to begin with is harder to explain. As most of the damaging physical health effects are experienced later in life, the higher level of depressive symptoms may be due to a failure to perceive expected health benefits post-quitting. That the effect was attenuated by perceived physical health is consistent with this explanation. For older smokers who are motivated and successfully quit but do not notice improvements to physical health, or become more aware of health issues related to smoking, this might stimulate depression inducing thoughts that the damage has already been done and it is too late. This hypothesis is also supported by an earlier study among older adults, in which a positive association between psychological distress and smoking cessation several years later disappeared after controlling for an increase in health problems in the intervening years [30]. An alternative hypothesis that we cannot rule out is that the self-medication hypothesis is valid for a sub-group of older smokers for whom smoking has effectively masked underlying mood problems which then emerged after quitting.
The findings that some of the observed relationships between quitting and subsequent depressive symptoms were attenuated by including measures of physical health suggest that some of the relationship is because people who are caught up in a self-harming behaviour they can’t stop are prone to become more depressed. Consistent with this is the higher rates of onset of depressive symptoms in those with a stronger smoking habit (HSI), and the finding in our companion paper that those with depression were more likely to make quit attempts [31] – a finding that may also partly explain the higher symptom rate in those who relapsed (i.e. depressive symptoms trigger quitting and only success ameliorates this). However, the finding that depression predicts increased relapse [31,32] cannot be accounted for by such a mechanism. Taken together, the findings reinforce the complexity of the relationship between smoking and depression.
Limitations
A strength of this study was that we were able to take advantage of the longitudinal nature of the ITC study and perform mixed effects logistic regressions across four waves of data collection. Thus, we were able to examine the prevalence of reported symptoms at follow-up, stratified by reported symptoms at T1 and quitting status at follow-up. However, this study has some limitations. We did not assess for a lifetime history of depression or other psychiatric disorders, which may be a predictor of quitting outcomes and future depressive symptoms. Participants were asked if they had received a diagnosis of depression in the past year; however, we were interested in participants’ subjective experience of recent depressive symptoms. As our sample was largely of those without clinically significant depression, the results may not fully generalise to clinical samples. In addition, readers should be cautious about generalising to smokers in other countries, particularly countries that differ from those studied in terms of any cultural factors, economic development, or extent of tobacco control efforts.
We also note that the T1 measures of depressive symptoms were taken approximately one year prior to T2 and symptoms may have changed prior to the reported quit attempt. It is possible that our observation of a negative relationship between abstinence and reporting symptoms among those who did report symptoms at T1 was the result of improved mood prior to quitting. However, Taylor et al [5] observed that results from population cohorts are consistent with results from clinical trials, making the reverse causality hypothesis less plausible. The measures used to assess depressive symptoms were categorical, meaning we could not assess degrees of severity. Further, the measures assessing perceived physical health were quite general and not able to detect changes across time, thus the role of perceived physical health may have been underestimated. Finally, we were unable to assess extraneous causes of change in depressive symptoms independent of smoking cessation such as normal responses to adverse life events, so we cannot say to what extent the effects found here might relate to reactive as opposed to other forms of depressed mood.
Conclusions
This study supports the hypothesis that most smokers can quit without experiencing depressive symptoms, at least over a period where any direct effect might be plausible. Our findings support the growing body of empirical research that suggests there is no reason smokers suffering depression should not be encouraged and supported to quit smoking. However, this study also suggests that the effects of smoking on depressive symptoms are not uniform across all smokers but vary by age and prior symptoms. Our finding that a quit attempt may precede affective disturbance in older smokers who were symptom free needs to be replicated, with better control for changes in perceived and actual physical health. The nature of the relationships between perceived or actual health problems, attempting to quit smoking, and depressive symptoms requires further exploration. Further research is also needed to examine the impact of failed quitting on depressive symptoms, the impact of concerns about physical health, and any effect these have on subsequent quit attempts.
Acknowledgments
Funding: We would like to thank members of the Data Management Core at the University of Waterloo for assistance in preparing the data for this analysis. The ITC Four-Country Survey is supported by multiple grants including R01 CA 100362 and P50 CA111236 (Roswell Park Transdisciplinary Tobacco Use Research Center) and also in part from grant P01 CA138389 (Roswell Park Cancer Institute, Buffalo, New York), all funded by the National Cancer Institute of the United States, Robert Wood Johnson Foundation (045734), Canadian Institutes of Health Research (57897, 79551), National Health and Medical Research Council of Australia (265903, 450110, APP1005922), Cancer Research UK (C312/A3726), Canadian Tobacco Control Research Initiative (014578); Centre for Behavioural Research and Program Evaluation, National Cancer Institute of Canada/Canadian Cancer Society.
Footnotes
Declaration of Interest: The authors declare that they have no competing interests.
References
- 1.Lasser K, Boyd W, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: a population-based prevalence study. JAMA. 2000;284:2606–2010. doi: 10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- 2.Balfour DJ, Ridley DL. The effects of nicotine on neural pathways implicated in depression: a factor in nicotine addiction? Pharmacol Biochem Behav. 2000;66:79–85. doi: 10.1016/s0091-3057(00)00205-7. [DOI] [PubMed] [Google Scholar]
- 3.Weinberger AH, George TP, McKee SA. Differences in smoking expectancies in smokers with and without a history of major depression. Addict Behav. 2011;36:434–437. doi: 10.1016/j.addbeh.2010.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coleman T, Murphy E, Cheater F. Factors influencing discussion of smoking between general practitioners and patients who smoke: a qualitative study. Brit J Gen Pract. 2000;50:207–210. [PMC free article] [PubMed] [Google Scholar]
- 5.Taylor G, McNeill A, Girling A, Farley A, Lindson-Hawley N, Aveyard P. Systematic review and meta-analysis of change in mental health after smoking cessation. BMJ. 2014;348:g1151. doi: 10.1136/bmj.g1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dube SR, Caraballo RS, Dhingra SS, Pearson WS, McClave AK, Strine TW, et al. The relationship between smoking status and serious psychological distress: findings from the 2007 Behavioral Risk Factor Surveillance System. Int J Public Health. 2009;54:i68–i74. doi: 10.1007/s00038-009-0009-y. [DOI] [PubMed] [Google Scholar]
- 7.Berlin I, Chen H, Covey LS. Depressive mood, suicide ideation and anxiety in smokers who do and smokers who do not manage to stop smoking after a target quit day. Addiction. 2010;105:2209–2216. doi: 10.1111/j.1360-0443.2010.03109.x. [DOI] [PubMed] [Google Scholar]
- 8.Capron DW, Allan NP, Norr AM, Zvolensky MJ, Schmidt NB. The effect of successful and unsuccessful smoking cessation on short-term anxiety, depression, and suicidality. Addict Behav. 2014;39:782–788. doi: 10.1016/j.addbeh.2013.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van der Deen FS, Carter KN, Wilson N, Collings S. The association between failed quit attempts and increased levels of psychological distress in smokers in a large New Zealand cohort. BMC Public Health. 2011;11:598. doi: 10.1186/1471-2458-11-598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McDermott MS, Marteau TM, Hollands GJ, Hankins M, Aveyard P. Change in anxiety following successful and unsuccessful attempts at smoking cessation: cohort study. Brit J Psychiat. 2013;202:62–67. doi: 10.1192/bjp.bp.112.114389. [DOI] [PubMed] [Google Scholar]
- 11.Hajek P, Taylor T, McRobbie H. The effect of stopping smoking on perceived stress levels. Addiction. 2010;105:1466–1471. doi: 10.1111/j.1360-0443.2010.02979.x. [DOI] [PubMed] [Google Scholar]
- 12.Bolam B, West R, Gunnell D. Does smoking cessation cause depression and anxiety? Findings from the ATTEMPT cohort. Nicotine Tob Res. 2011;13:209–214. doi: 10.1093/ntr/ntq244. [DOI] [PubMed] [Google Scholar]
- 13.Kinnunen T, Haukkala A, Korhonen T, Quiles ZN, Spiro A, III, Garvey AJ. Depression and Smoking across 25 Years of the Normative Aging Study. Int J Psychiatry Med. 2006;36:413–426. doi: 10.2190/G652-T403-73H7-2X28. [DOI] [PubMed] [Google Scholar]
- 14.Shahab L, Andrew S, West R. Changes in prevalence of depression and anxiety following smoking cessation: results from an international cohort study (ATTEMPT) Psychol Med. 2014;44:127–141. doi: 10.1017/S0033291713000391. [DOI] [PubMed] [Google Scholar]
- 15.Prochaska JJ, Hall SM, Tsoh JY, Eisendrath S, Rossi JS, Redding CA, et al. Treating tobacco dependence in clinically depressed smokers: effect of smoking cessation on mental health functioning. Am J Public Health. 2008;98:446–448. doi: 10.2105/AJPH.2006.101147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Torres LD, Barrera AZ, Delucchi K, Penilla C, Pe′rez-Stable EJ, Mun RF. Quitting smoking does not increase the risk of major depressive episodes among users of Internet smoking cessation interventions. Psychol Med. 2010;40:441–449. doi: 10.1017/S0033291709990560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kahler CW, Brown RA, Ramsey SE, Niaura R, Abrams DB, Goldstein MG, et al. Negative mood, depressive symptoms, and major depression after smoking cessation treatment in smokers with a history of major depressive disorder. J Abnorm Pschol. 2002;111:670–675. doi: 10.1037//0021-843x.111.4.670. [DOI] [PubMed] [Google Scholar]
- 18.Segan CJ, Borland R, Wilhelm KA, Bhar SS, Hannan AT, Dunt DR, et al. Helping smokers with depression to quit smoking: collaborative care with Quitline. Med J Australia. 2011;195:S7–11. doi: 10.5694/j.1326-5377.2011.tb03258.x. [DOI] [PubMed] [Google Scholar]
- 19.Tsoh YT, Humfleet GL, Munoz RF, Reus VI, Hartz DT, Hall SM. Development of major depression after treatment for smoking cessation. Am J Psychiat. 2000;157:368–374. doi: 10.1176/appi.ajp.157.3.368. [DOI] [PubMed] [Google Scholar]
- 20.Piper ME, Kenford S, Fiore MC, Baker TB. Smoking cessation and quality of life: changes in life satisfaction over 3 years following a quit attempt. Ann Behav Med. 2012;43:262–270. doi: 10.1007/s12160-011-9329-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hughes JR. Depression during tobacco abstinence. Nicotine & Tobacco Research. 2007;9:443–446. doi: 10.1080/14622200701243185. [DOI] [PubMed] [Google Scholar]
- 22.Glassman AH, Covey LS, Stetner F, Rivelli S. Smoking cessation and the course of major depression: a follow-up study. Lancet. 2001;357:1929–1932. doi: 10.1016/S0140-6736(00)05064-9. [DOI] [PubMed] [Google Scholar]
- 23.Fong GT, Cummings KM, Borland R, Hastings G, Hyland A, Giovino GA, et al. The conceptual framework of the International Tobacco Control (ITC) Policy Evaluation Project. Tob Control. 2006;15:iii3–iii11. doi: 10.1136/tc.2005.015438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thompson ME, Fong GT, Hammond D, Boudreau C, Driezen P, Hyland A, et al. Methods of the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15:iii3–iii11. doi: 10.1136/tc.2005.013870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Spitzer RL, Williams JBW, Kroenke K, Linzer M, deGruy FV, III, Hahn SR, et al. Utility of a new procedure for diagnosing mental disorders in primary care. JAMA. 1994;272:1749–1756. [PubMed] [Google Scholar]
- 26.Whooley MA, Avins AL, Miranda J, Browner WS. Case finding instruments for depression: Two questions are as good as many. J Gen Intern Med. 1997;12:439–445. doi: 10.1046/j.1525-1497.1997.00076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom K-O. The Fagerström Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. Brit J Addict. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 28.Australian Bureau of Statistics (ABS) National survey of mental health and wellbeing: summary of results, 2007. 2008 [cited 2014 Nov 17]; ABS cat. no. 4326.0. Available from: http://www.abs.gov.au.
- 29.Parrott AC. Cigarette-Derived Nicotine is not a Medicine. World J Biol Psychia. 2003;4:49–55. doi: 10.3109/15622970309167951. 2003. [DOI] [PubMed] [Google Scholar]
- 30.Sachs-Ericsson N, Schmidt NB, Zvolensky MJ, Mitchell M, Collins N, Blazer DG. Smoking cessation behavior in older adults by race and gender: The role of health problems and psychological distress. Nicotine Tob Res. 2009;11:433–443. doi: 10.1093/ntr/ntp002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cooper J, Borland R, McKee SA. Depression motivates quit attempts but predicts relapse: Differential findings for gender from the International Tobacco Control Study. Submitted to Addiction. doi: 10.1111/add.13290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hitsman B, Papandonatos GD, McChargue DE, DeMott A, Herrera MJ, Spring B, Borrelli B, Niaura R. Past major depression and smoking cessation outcome: a systematic review and meta-analysis update. Addiction. 2013;108:294–306. doi: 10.1111/add.12009. [DOI] [PMC free article] [PubMed] [Google Scholar]


