Abstract
Colorectal cancer is one of the most common cancers in the world. It is well known that the chronic inflammation can promote the progression of colorectal cancer (CRC). Recently, a number of studies revealed a potential association between colorectal inflammation, cancer progression, and infection caused by enterotoxigenic Bacteroides fragilis (ETBF). Bacterial enterotoxin activates spermine oxidase (SMO), which produces spermidine and H2O2 as byproducts of polyamine catabolism, which, in turn, enhances inflammation and tissue injury. Using qPCR analysis, we estimated the expression of SMOX gene and ETBF colonization in CRC patients. We found no statistically significant associations between them. Then we selected genes involved in polyamine metabolism, metabolic reprogramming, and inflammation regulation and estimated their expression in CRC. We observed overexpression of SMOX, ODC1, SRM, SMS, MTAP, c-Myc, C/EBPβ (CREBP), and other genes. We found that two mediators of metabolic reprogramming, inflammation, and cell proliferation c-Myc and C/EBPβ may serve as regulators of polyamine metabolism genes (SMOX, AZIN1, MTAP, SRM, ODC1, AMD1, and AGMAT) as they are overexpressed in tumors, have binding site according to ENCODE ChIP-Seq data, and demonstrate strong coexpression with their targets. Thus, increased polyamine metabolism in CRC could be driven by c-Myc and C/EBPβ rather than ETBF infection.
1. Introduction
Colorectal cancer (CRC) is one of the most common cancers in the world. It has been estimated that in 2012 about 1.4 million people were diagnosed and more than 690 thousand died [1]. The lifetime risk of developing colorectal cancer is about 5% worldwide. Women have a higher risk for colon cancer that men [2]. The prognosis of colorectal cancer is closely related to the stage of disease at diagnosis [3]. CRC can have no symptoms in early stages, and mean 5-year survival rate for peoples detected at an early stage is about 90% compared to 10% for people diagnosed for cancer with distant metastases [4]. Certain factors increase a risk of developing the disease. These are age [5], polyps of the colon [6], history of cancer, heredity [7–9], smoking [10], diet and microbiota [11, 12], lack of physical activity [13], chronic inflammation (colitis and IBD) [14, 15], viruses [16, 17], and exogenous hormones [18]. The chronic inflammation caused by infection is one more risk factor for colorectal cancer [19, 20]. Some pathogenic strains of Escherichia coli (cyclomodulin-positive) are able to induce chronic inflammation and can be involved in carcinogenesis. Cyclomodulin-positive E. coli strains were more prevalent in both the mucosa and tumors of patients with colorectal cancer (26% patients) versus diverticulosis control (6% patients) [19]. In addition, the number of colonic polyps was elevated in multiple intestinal neoplasia (Min) mice inoculated with a colon cancer-associated E. coli strain (11G5) [19].
Recent studies have demonstrated that the enterotoxigenic Bacteroides fragilis (ETBF) bacterium is an important cause of chronic inflammation in human and animal colon. It has been presented that the bft gene, which encodes Bacteroides fragilis toxin (BFT), is associated with colorectal neoplasia and may be a risk factor for developing CRC [21]. It was observed that BFT produced by bacteria upregulates both spermine oxidase (SMOX) gene expression at mRNA and protein levels in cultures of human normal colonic epithelial cells [20]. SMOX encodes SMO protein, which plays an important role in the regulation of polyamine metabolism. SMO catalyzes the oxidation of spermine to spermidine and produces hydrogen peroxide (H2O2) and aldehydes [22]. This results in apoptosis, DNA damage, and consequently the development of cancer. For example, cytotoxin produced by Helicobacter pylori strains causes an increase in spermine oxidase levels in human gastric epithelial cells. These pathogenic H. pylori strains contain cytotoxin-associated gene A (CagA) and represent a risk factor for gastric cancer. The strong association of H. pylori (Cag+) infection, SMO levels, apoptosis, and oxidative DNA damage has been observed [23, 24].
In recent years, we have seen a steady increase in the number of studies examining the role of intracellular polyamine metabolism in tumor development. Several important enzymes, spermidine/spermine N1-acetyltransferase (SSAT), N1-acetylpolyamine oxidase (APAO), and SMO, appear to play critical roles in many cancers. All such enzymes are highly inducible by multiple stress signals, including ones caused with bacterial pathogens, and have the potential to alter polyamine homeostasis. APAO and SMO enzymes produce reactive oxygen species (ROS), H2O2, and aldehydes, which are potentially harmful to cells. ROS are key signaling molecules, which play an important role in several pathways (e.g., NF-κB, ERK1/2, p38, PI3K, and others) and can contribute to the induction of inflammation and cancer [25].
Thus, the abundant pathogenic microbiota alters the host tissue microenvironment leading to chronic inflammation, immune dysregulation, and elevated levels of ROS. All these may result in activation of oncogenes, downregulation of tumor suppressor genes, DNA damage, and cell and tissue injury, thereby contributing to tumor growth. In the colon, the alteration of polyamine catabolism caused by infection with consequent H2O2 generation and DNA damage may be a common cause of inflammation and promotion of carcinogenesis. Moreover, an increase in polyamine catabolism rates and the production of H2O2 has been involved in the response to chemotherapeutic agents or specific antitumor polyamine analogues in several tumors, including colorectal cancer [26–30]. However, the clinical, molecular, and prognostic associations of infection and the expression of polyamine metabolism gene in colorectal cancer remain unclear.
2. Material and Methods
2.1. Tissue Specimens
A total of 50 paired specimens of stages I–IV colorectal cancer (CRC) and adjacent morphologically normal tissues were taken from patients with primary carcinoma of the colon and rectum, which had not been exposed to radiation or chemotherapy, during surgical resection. Each sample was frozen and placed in liquid nitrogen immediately after surgery. The specimens were characterized according to the American Joint Committee on Cancer (AJCC) staging system [31]. The diagnosis was verified by histopathology and only samples containing 70–80% or more tumor cells were used in the study. The tissue samples were collected in accordance with the guidelines issued by the Ethics Committee, National Medical Research Radiological Center, the Ministry of Health of the Russian Federation. All patients gave written informed consent, which is available upon request. The study was carried out in accordance with the principles outlined in the Declaration of Helsinki (1964).
2.2. RNA and DNA Isolation and cDNA Synthesis
Total RNA was isolated using Micro-Dismembrator S (Sartorius, Germany) and RNeasy Mini Kit (Qiagen, Germany) in accordance with the manufacturer's instructions. For the detection of bacteria, DNA was extracted using the QIAamp DNA Mini Kit (Qiagen, Germany) and further treated with proteinase K in accordance with the manufacturer's protocol. Purified RNA and DNA were quantified using Qubit 2.0 fluorometer (Invitrogen, USA) and their quality was determined by Agilent Bioanalyzer 2100 (Agilent Technologies, USA). All RNA samples were treated with DNase I (Thermo Fisher Scientific, USA), and cDNA was synthesized using M-MLV Reverse Transcriptase (Thermo Fisher Scientific, USA) and random hexamers according to standard manufacturer's protocol.
2.3. qPCR
To detect and quantitate Bacteroides fragilis we used the primers targeting Bft1 gene. These primers were taken from the work of Viljoen et al. [32]: forward 5′-GACGGTGTATGTGATTTGTCTGAGAGA-3′, reverse 5′-ATCCCTAAGATTTTATTATCCCAAGTA-3′. EvaGreen Dye (Biotium Inc., USA) was used as fluorescent DNA-binding dye for the detection and quantification of PCR products. Purified bacterial control DNA was obtained from Orekhovich Institute of Biomedical Chemistry, Russian Academy of Sciences (Moscow).
To evaluate gene expression, we used TaqMan Gene Expression Assays (Thermo Fisher Scientific, USA). This consists of a pair of specific unlabeled PCR primers and a TaqMan probe with a FAM dye label on the 5′ end and minor groove binder (MGB) nonfluorescent quencher (NFQ) on the 3′ end. All probes contained the dye FAM at 5′-end and RTQ1 at 3′-end. qRT-PCR was performed as described earlier using RPN1 and GUSB reference genes [33–35].
All reactions were performed using AB 7500 Real-Time PCR System (Thermo Fisher Scientific, USA) with RQ (Relative Quantitation) software (Thermo Fisher Scientific, USA). PCR program was as follows: 10 min at 95°C and then 50 two-step cycles 15 s at 95°C and 60 s at 60°C. The total reaction volume was 20 μL in triplicate. PCR products were analyzed in 2% agarose gels, and nucleotide sequences of the amplicons were verified by Sanger sequencing with ABI Prism 3100 Genetic Analyzer (Thermo Fisher Scientific, USA).
2.4. Analysis of qRT-PCR Data
For the detection and quantification of bacterial DNA, absolute quantification method was used. A standard curve was constructed using serial 10-fold dilutions of control bacterial DNA. The genome size of Bacteroides fragilis (5.3 Mb) and the mass of DNA per genome were used to calculate the concentration of bacterial DNA [36]. Spearman's rank correlation analysis was used to check the dependence between target gene expression levels and the concentration of bacterial DNA within the same samples.
mRNA qRT-PCR data were analyzed using the relative quantification method (ΔΔCt) taking into account the efficiency of the PCR amplification using ATG (Analysis of Transcription of Genes) tool as described in [34, 37]. The relative inner variability between mRNA levels of reference genes (RPN1 and GUSB) was not higher than twofold in tumor and normal tissues; therefore, twofold and higher mRNA level changes for the target genes were considered as significant. We used nonparametric Mann-Whitney U test to validate the significance of gene expression alterations (p ≤ 0.01 was taken as the criterion of statistical significance). All statistical analyses were performed in the R environment. Pearson correlation coefficient was used to evaluate the coexpression of human genes (p ≤ 0.001 was taken as the criterion of statistical significance). We supplemented the coexpression analysis with ENCODE ChIP-Seq data using previously developed CrossHub tool [38].
3. Results
3.1. Expression of SMOX Gene and Bacteroides fragilis Quantification
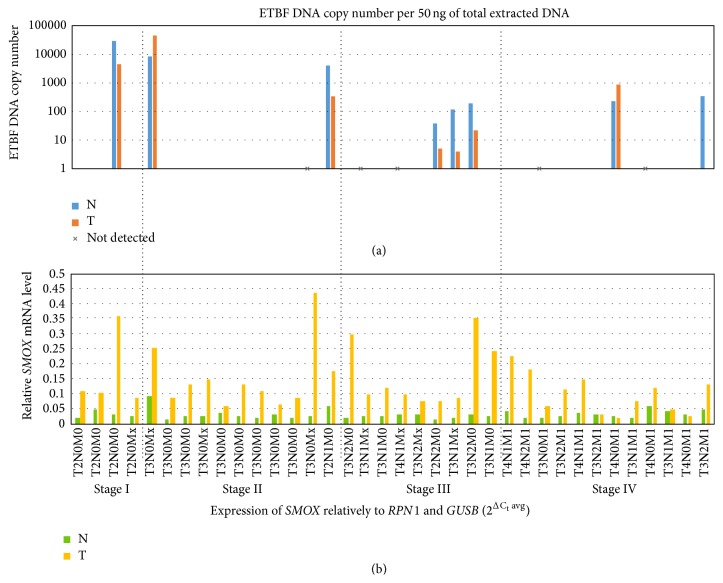
We analyzed 36 paired samples of primary colorectal carcinomas and adjacent normal tissues to quantify ETBF. Serial dilution of genomic DNA from ETBF was used as standard. At least one copy of ETBF DNA per 50 ng of total extracted DNA was detected in 8 paired tumor and adjacent normal samples, including three samples, which showed a significantly increased amount of the ETBF DNA (>1000 copies/1 ng of extracted DNA). Most of the tested samples (23/36) demonstrated less than a copy of bacterial DNA per 50 ng of total extracted DNA. Five samples were found to be ETBF-negative (Figure 1).
Figure 1.
(a) Enterotoxigenic B. fragilis (ETBF) DNA copy number per 50 ng of total extracted DNA in paired samples of colorectal cancer (logarithmic scale). (b) SMOX expression level relatively to two reference genes: RPN1 and GUSB. The samples with high rates of ETBF colonization tend to have higher expression of SMOX, especially in normal tissue (compared to the other norms). However, no statistically significant correlation between SMOX expression and ETBF colonization was observed.
3.2. Expression Quantification of Genes Involved in Polyamine Metabolism and Regulation of Inflammatory Response
The set of 36 colorectal tumors and adjacent normal tissues was extended with an additional set of 14 paired samples in order to increase the statistical significance of the results. Thus, we used a set of 50 colorectal cancers to evaluate the expression of target genes, which encode enzymes of polyamine metabolism and genes participating in immune response and inflammation signaling.
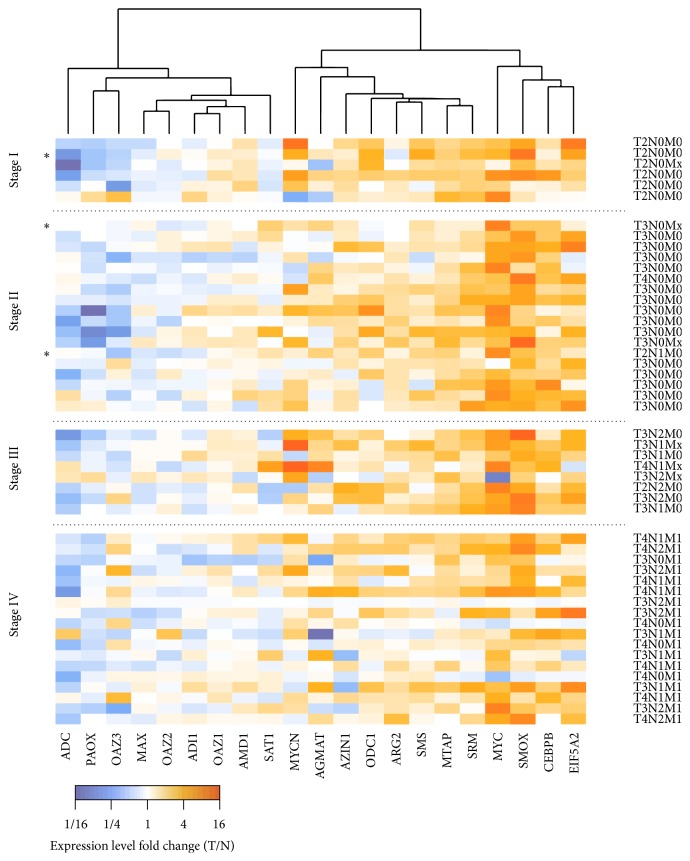
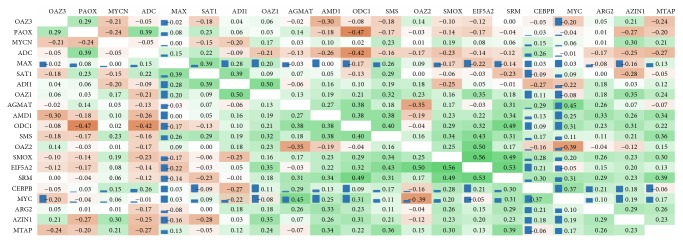
Using RT-qPCR, we evaluated the relative expression level of 17 genes involved in polyamine metabolism and 4 genes mediating metabolic reprogramming, and the regulation of inflammatory response and cell proliferation: c-Myc (MYC), n-Myc (MYCN), Max, and C/EBPβ gene encoding CCAAT/enhancer binding protein (CEBPB). The results are given in Figure 2 (tumor/normal relative expression level) and Figure 3 (coexpression analysis coupled to ENCODE ChIP-Seq data).
Figure 2.
Results of the qPCR expression analysis of genes involved in polyamine metabolism and inflammation regulation in paired colorectal cancer samples. Cell color indicates expression level change in tumor compared to normal: increase (orange) and decrease (blue). Genes are rearranged according to the similarity of expression profiles. Samples with a high concentration of enterotoxigenic B. fragilis DNA (>1000 copies per 1 ng of total DNA) are marked with an asterisk.
Figure 3.
Results of coexpression analysis for genes participating in polyamine metabolism. Pearson correlation coefficients between the expression levels changes of genes participating in polyamine metabolism and inflammation across 50 colorectal cancer samples are presented. Cell color reflects these values (green: positive, brown: negative). Normalized ChIP-Seq score (according to ENCODE data) is indicated with blue bars.
Two genes, c-Myc and SMOX, demonstrated the highest upregulation in CRC. Both genes were overexpressed (at least 2 times) in 40 out of 50 samples (80%). C/EBPβ, eIF5A2, and SRM revealed upregulation in 50% samples. Several pairs of genes that demonstrated statistically significant coexpression were also found to have ChIP-Seq associations: c-Myc-AGMAT, c-Myc-ODC1, c-Myc-SRM, c-Myc-AMD1, C/EBPβ-SRM, C/EBPβ-AGMAT, C/EBPβ-SMOX, and C/EBPβ-eIF5A2. Moreover, C/EBPβand c-Myc demonstrated strong coexpression (r s = 0.37) and extremely high ChIP-Seq signal intensity according to ENCODE ChIP-Seq data (C/EBPβ binding to c-Myc). This suggests C/EBPβ to be a possible upstream regulator of c-Myc. In contrast to c-Myc, n-Myc showed statistically significant coexpression only with AZIN1.
4. Discussion
Bacteroides fragilis contains up to 1%-2% of the normal colonic microbial flora in humans [39, 40]. Pathogenic strains of B. fragilis that produce enterotoxin are associated with the development of inflammatory diarrheal disease in both children and adults [41, 42], IBD [43], and colitis [44], thereby contributing to chronic inflammation and onset of colon tumors. It was supposed that B. fragilis toxin (BFT), produced only by enterotoxigenic strains (ETBF), binds to a specific intestinal epithelial cell receptor and induces several signal transduction pathways [45, 46]. BFT cleaves E-cadherin [47, 48] and activates Wnt/β-catenin pathway signaling [49]. BFT was also shown to be involved in activation of tyrosine kinases, MAPKs, and NF-κB signaling pathways and to be able to increase cellular proliferation mediated by the elevated expression of c-Myc oncogene [50–53]. Moreover, as mentioned above, BFT may be implicated in polyamine catabolism through upregulation of SMO protein levels and enzyme activity [20]. Recent studies suggested SMO enzyme as a potential source of an inflammation-associated ROS produced during polyamine catabolism [54]. Thus, the association between ETBF colonization rates of CRC patients and the expression of SMOX gene appears to be an important link between chronic inflammation caused by infection, tumor onset, and progression.
In this study, we quantitated ETBF strain colonization rates and evaluated the expression of SMOX gene at mRNA level in CRC patients using qPCR. We found that the majority of CRC patients were colonized with toxin-producing strains of B. fragilis, but only small amounts of bacterial DNA were identified. A significantly increased content of bacterial DNA was detected in three patients with I and II stages of CRC (in both tumor and normal tissues). In contrast, pathogenic cyclomodulin-positive E. coli strains, a possible cofactor of colorectal carcinogenesis, were predominantly found on mucosa of patients with stages III/IV [19]. Additional studies and extended sampling are needed to reveal possible associations between ETBF colonization and disease stage.
The expression of SMOX gene revealed no statistically significant correlation with the amount of bacterial DNA, but the samples with a high concentration of bacterial DNA (>1000 copies per 50 ng) demonstrated high SMOX expression levels in both normal tissue and tumor (relatively to GUSB and RPN1 reference genes, Figure 1). These results do not contradict the hypothesis that ETBF strains can be proinflammatory and oncogenic bacteria, but additional studies are needed to understand the possible role of ETBF in colorectal carcinogenesis [21]. These results are consistent with a mechanism of SMOX induction independent of ETBF infection.
Next, we tested differential expression of 17 genes participating in polyamine metabolism and 4 genes involved in the mediation of metabolic preprogramming, cell proliferation (с-Myc, n-Myc, and Max) and inflammation (C/EBPβ). c-Myc and n-Myc form dimers with Max, translocate to the nucleus, and then activate the transcription of many genes participating in cell cycle regulation, glycolysis, energy metabolism, hypoxic adaptation, DNA replication, and other processes [55–58]. C/EBPβ is a transcription factor, which can form either homodimers or heterodimers with other CCAAT/enhancer binding proteins (alpha, delta, and gamma). C/EBPβ is known to be a mediator of inflammation and immunity [59, 60]. The most important C/EBPβ targets are interleukins IL-6, IL-4, IL-5, and TNF-α [61–64]. We found upregulation of c-Myc, n-Myc, and C/EBPβ in the analyzed samples. However, we did not find overexpression of Max. This is in agreement with a previous finding: overexpression of c-Myc and n-Myc but not Max is observed in many tumors [55, 58, 65, 66]. Our data showed increased expression of SMOX gene at all stages of colorectal cancer, this tendency being more pronounced at the early stages (Figure 2). Spearman correlation coefficient between disease stage and tumor/normal fold change of SMOX mRNA level is r s = −0.19: SMOX expression tends to be lower with disease stage. However, this tendency is not statistically significant (p > 0.05). Different tumors demonstrate dramatically distinct SMOX expression profiles. SMO was found to be elevated in both prostate adenocarcinoma and prostatic intraepithelial neoplasia [67] whereas breast cancer showed SMOX underexpression at both mRNA and protein levels [68]. Other genes that showed statistically significant correlation with disease stage were MTAP (r s = −0.30, p = 0.03), and SRM (r s = −0.27, p = 0.05), which tended to decrease the expression level with tumor stage, and OAZ3 (r s = 0.42, p = 0.003), which increased its expression with disease progression.
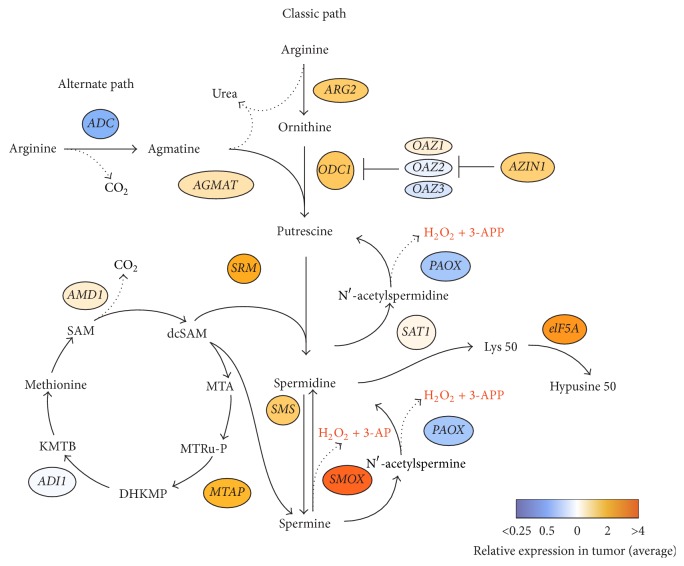
Polyamines are organic cations, which are essential for cell proliferation and growth, and their levels are frequently altered in many human tumors [69, 70]. Polyamines have also been shown to play an important role in inflammation-induced carcinogenesis [71]. Intracellular polyamine metabolism occurs via two pathways: classical and alternate (Figure 4). Polyamines (putrescine, spermidine, and spermine) are synthesized by mammalian cells, while agmatine is produced only by plants and bacteria, including intestinal microbial flora [72–74]. L-arginine carboxylase (ADC), found only in nonmammals, catalyzes a reaction of decarboxylation of L-arginine to agmatine [72, 75]. The latter is further hydrolyzed to putrescine and urea by agmatinase, which is encoded by AGMAT gene. Recent reports also supposed that different pathogens, such as viruses and bacteria, could upregulate agmatinase at mRNA and protein levels, thereby inducing polyamine synthesis [76, 77].
Figure 4.
Classic path of polyamine metabolism consists of the following: (1) arginine is converted to ornithine through the action of ARG (arginase) in the urea cycle; (2) putrescine is formed from the reaction of ornithine decarboxylation catalyzed by ODC1 (ornithine decarboxylase-1). OAZ can bind to ODC1 to form OAZ-ODC1 complex and subsequently reduce polyamine synthesis. AZIN1 (antizyme inhibitor-1) brakes the ODC1-OAZ complex and liberates ODC1; (3) AMD1 (S-adenosylmethionine decarboxylase) decarboxylates S-adenosylmethionine (SAM) to decarboxylated SAM (dcSAM); (4) dcSAM provides aminopropyl groups to putrescine to produce spermidine by spermidine synthase (SRM) and spermine by spermine synthase (SMS). MTA (methylthioadenosine) is generated as a byproduct. Spermine can be recycled back to spermidine directly by spermine oxidase (SMOX). Spermine and spermidine can be recycled to spermidine and putrescine by spermidine/spermine-N1-acetyltransferase (SAT1) followed by oxidation by polyamine oxidase (PAOX) [101]. MTA can be processed to the methionine: MTA phosphorylase (MTAP) catalyzes the cleavage of MTA yielding 5-methylthioribose-1-phosphate (MTRu-P), which is further metabolized to DHKMP (1,2-dihydro-3-keto-5-methylthiopentene). ADI (acireductone dioxygenase) catalyzes DHKMP to 2-oxo-4-methylthiobutyrate (KMTB) and transamination of KMTB results in formation of methionine [102–104].
In the present study, we revealed that the expression of ADC gene decreased on the average by half in CRC samples compared to adjacent normal tissues. These findings indicate that, in case of colorectal cancer, the enhanced polyamine synthesis is not associated with alternate path and the intestinal microbiota does not significantly contribute to these processes.
The three major enzymes that are involved in polyamine metabolism (SSAT, APAO, and SMO) are encoded by SAT1, PAOX, and SMOX genes, respectively. One of the products of both SMO and APAO-mediated reactions are H2O2 and highly toxic aldehydes, which may also cause oxidative damage. SSAT cellular toxicity is thought to be caused by produced acetylated polyamines, which are utilized by APAO. APAO is constitutively expressed, while SSAT is an inducible enzyme [78]. SSAT expression is induced by different stimuli, such as toxins, hormones, cytokines, nonsteroidal anti-inflammatory agents, natural products, and pathogens. It is regulated via several pathways including TNF-α and NF-κB [79–82]. SSAT expression can be also mediated by Nrf2 in response to the addition of H2O2 in human hepatoma HUH7 cells [83]. We found that SAT1 gene was differentially expressed in many CRC samples (either up- or downregulated), while a decreased expression of PAOX gene was observed. This indicates that the SSAT/APAO pathway is not hyperactive and does not seem to be a cause of oxidative damage in colorectal cancer. Inflammatory response agents and stress pathways are not the result of the induction of SSAT expression at mRNA level. Thus, it is possible that the increased SMOX gene expression and enzyme activity make the greatest contribution to the oxidative stress damage caused by polyamine catabolism in colorectal cancer [20].
It is known that specific protein products of oncogenes and tumor suppressor genes can regulate polyamine metabolism [84–86]. The results of coexpression analysis coupled to ENCODE ChIP-Seq data strongly suggest c-Myc and C/EBPβ as regulators of the expression of key enzymes of polyamine metabolism that are upregulated in colorectal cancer: SMOX, AZIN1, MTAP, SRM, AMD1, ODC1, and AGMAT. It should be mentioned that genes encoding polyamine metabolic enzymes are regulated transcriptionally/post-transcriptionally by changes in the levels of intracellular polyamines. Additional studies (c-Myc and C/EBPβ knockdown assays) are needed to prove our finding. Not surprisingly, three of these genes, ODC1, AMD1, and SRM, are already known c-Myc targets [87–89]. Besides these genes, c-Myc is also known to regulate eIF5A2. However, this gene did not demonstrate coexpression with c-Myc but did show ChIP-Seq association (c-Myc binding site). It is known that c-Myc induces the expression of ornithine decarboxylase (ODC), which catalyzes the first rate-limiting step in polyamine synthesis [89]. It has been also shown that bacterial infections can stimulate polyamine synthesis through ODC [90], whereas suppression of ODC leads to the depletion of cellular polyamine levels in human colorectal cancer cells [82, 91]. ODC inhibition with difluoromethylornithine (DFMO) is a possible anticancer therapy. It was reported that the treatment of normal intestinal epithelial cells of rats (IEC-6) with the DFMO led to the depletion of polyamines and subsequently inhibited cell growth and induced cell cycle arrest. A combination of drugs including DFMO could reduce recurrent adenomatous polyps in patients with history of resected sporadic colorectal adenomas [92].
n-Myc (MYCN) is oncogenic transcription factor, which can directly upregulate ODC expression in neuroblastomas [93]. Moreover, it has been shown that the reduction of n-Myc protein levels through inhibition of glycolysis may decrease ODC expression and potentiate polyamine levels in human neuroblastoma cell lines [84]. We showed that expression of ODC1 gene was increased in a number of CRC samples, as well as mRNA level of c-Myc and n-Myc genes. However, n-Myc showed no expression correlations with ODC1 and no ENCODE ChIP-Seq data are available for n-Myc.
It is worthy of note that the expression of OAZ1, OAZ2, and OAZ3 genes, which encode major regulators of ornithine decarboxylation to putrescine through inhibition of ODC catalytic activity, and the expression of AZIN1 gene, which is involved in inhibition of antizyme (OAZ) family, did not change in the majority of CRC samples compared with normal samples. This indicates that the production of putrescine, catalyzed by ODC during polyamine catabolism, is not suppressed in colorectal cancer.
We have observed a significant increase in eIF5A2 mRNA levels in colorectal tumors. Cytosolic protein encoded by eIF5A2 gene undergoes posttranslational modification of Lys 50 to hypusine [94]. Spermidine as a substrate is involved in the first step of this process. The eIF5A2 protein is essential for eukaryotic cell proliferation, but the molecular function of eIF5A remains incompletely clear. It was shown that c-Myc can possibly transactivate the eIF5A2 gene [95, 96]. eIF5A2, in turn, was demonstrated to regulate MTA1 (metastasis-associated 1) via c-Myc in gastric cancer and colorectal carcinoma [97, 98]. Our data suggests that eIF5A2 can play an important oncogenic role in CRC and enhance the involvement of polyamines in this pathological process.
We elevated the expression of C/EBPβ gene, an important transcription factor, which controls the expression of genes involved in inflammatory response [60, 99, 100]. We observed a positive correlation between C/EBPβ gene expression and many key genes such as ADC, SMOX, AGMAT, and SRM involved in polyamine metabolism.
5. Conclusions
In summary, our results show that dysregulation of polyamine metabolism in all stages of CRC can be associated with chronic inflammation mediators rather than with the infection caused by ETBF. This is the first report that presents changed levels of expression of the key components of polyamine metabolism. We characterized some important aspects of the expression of SMOX and PAOX genes, which are responsible for cellular ROS generation. Two transcription factors, oncogenic с-Myc (responsible for metabolic reprogramming and cell proliferation) and C/EBPβ (mediator of inflammation and immune response), were found to be the most likely regulators of several key enzymes of polyamine metabolic pathway.
Acknowledgments
This work was supported by the Russian Science Foundation Grant no. 14-15-01083. The authors thank Orekhovich Institute of Biomedical Chemistry for the purified control DNA of Bacteroides fragilis, National Medical Research Center of Radiology for the colorectal cancer samples, and Shemyakin-Ovchinnikov Institute of Bioorganic Chemistry for the statistical analysis.
Competing Interests
The authors declare that they have no competing interests.
Authors' Contributions
Anastasiya V. Snezhkina and George S. Krasnov contributed equally to this work.
References
- 1.Torre L. A., Bray F., Siegel R. L., Ferlay J., Lortet-Tieulent J., Jemal A. Global cancer statistics, 2012. CA: A Cancer Journal for Clinicians. 2015;65(2):87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 2.Haggar F. A., Boushey R. P. Colorectal cancer epidemiology: incidence, mortality, survival, and risk factors. Clinics in Colon and Rectal Surgery. 2009;22(4):191–197. doi: 10.1055/s-0029-1242458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maclennan I., Hill J. How can doctors diagnose colorectal cancer earlier? British Medical Journal. 1993;306(6894):p. 1707. doi: 10.1136/bmj.306.6894.1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kohler B. A., Sherman R. L., Howlader N., et al. Annual report to the nation on the status of cancer, 1975–2011, featuring incidence of breast cancer subtypes by race/ethnicity, poverty, and state. Journal of the National Cancer Institute. 2015;107(6) doi: 10.1093/jnci/djv048.djv048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maffei S., Colantoni A., Kaleci S., Benatti P., Tesini E., de Leon M. P. Clinical features of colorectal cancer patients in advanced age: a population-based approach. Internal and Emergency Medicine. 2016;11(2):191–197. doi: 10.1007/s11739-015-1286-5. [DOI] [PubMed] [Google Scholar]
- 6.Aarons C. B., Shanmugan S., Bleier J. I. S. Management of malignant colon polyps: current status and controversies. World Journal of Gastroenterology. 2014;20(43):16178–16183. doi: 10.3748/wjg.v20.i43.16178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stigliano V., Sanchez-Mete L., Martayan A., Anti M. Early-onset colorectal cancer: a sporadic or inherited disease? World Journal of Gastroenterology. 2014;20(35):12420–12430. doi: 10.3748/wjg.v20.i35.12420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Strate L. L., Syngal S. Hereditary colorectal cancer syndromes. Cancer Causes and Control. 2005;16(3):201–213. doi: 10.1007/s10552-004-3488-4. [DOI] [PubMed] [Google Scholar]
- 9.Brewer D. A., Bokey E. L., Fung C., Chapuis P. H. Heredity, molecular genetics and colorectal cancer: a review. Australian and New Zealand Journal of Surgery. 1993;63(2):87–94. doi: 10.1111/j.1445-2197.1993.tb00051.x. [DOI] [PubMed] [Google Scholar]
- 10.Chen K., Xia G., Zhang C., Sun Y. Correlation between smoking history and molecular pathways in sporadic colorectal cancer: a meta-analysis. International Journal of Clinical and Experimental Medicine. 2015;8(3):3241–3257. [PMC free article] [PubMed] [Google Scholar]
- 11.Park Y., Hunter D. J., Spiegelman D., et al. Dietary fiber intake and risk of colorectal cancer: a pooled analysis of prospective cohort studies. Journal of the American Medical Association. 2005;294(22):2849–2857. doi: 10.1001/jama.294.22.2849. [DOI] [PubMed] [Google Scholar]
- 12.Akin H., Tözün N. Diet, microbiota, and colorectal cancer. Journal of Clinical Gastroenterology. 2014;48, supplement 1:S67–S69. doi: 10.1097/MCG.0000000000000252. [DOI] [PubMed] [Google Scholar]
- 13.Tayyem R. F., Shehadeh I. N., AbuMweis S. S., et al. Physical inactivity, water intake and constipation as risk factors for colorectal cancer among adults in Jordan. Asian Pacific Journal of Cancer Prevention. 2013;14(9):5207–5212. doi: 10.7314/APJCP.2013.14.9.5207. [DOI] [PubMed] [Google Scholar]
- 14.Yashiro M. Ulcerative colitis-associated colorectal cancer. World Journal of Gastroenterology. 2014;20(44):16389–16397. doi: 10.3748/wjg.v20.i44.16389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dyson J. K., Rutter M. D. Colorectal cancer in inflammatory bowel disease: what is the real magnitude of the risk? World Journal of Gastroenterology. 2012;18(29):3839–3848. doi: 10.3748/wjg.v18.i29.3839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nayudu S. K., Balar B. Colorectal cancer screening in human immunodeficiency virus population: are they at average risk? World Journal of Gastrointestinal Oncology. 2012;4(12):259–264. doi: 10.4251/wjgo.v4.i12.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tafvizi F., Fard Z. T., Assareh R. Epstein-Barr virus DNA in colorectal carcinoma in Iranian patients. Polish Journal of Pathology. 2015;66(2):154–160. doi: 10.5114/pjp.2015.53012. [DOI] [PubMed] [Google Scholar]
- 18.Beral V., Banks E., Reeves G., Appleby P. Use of HRT and the subsequent risk of cancer. Journal of Epidemiology and Biostatistics. 1999;4(3):191–210. [PubMed] [Google Scholar]
- 19.Bonnet M., Buc E., Sauvanet P., et al. Colonization of the human gut by E. coli and colorectal cancer risk. Clinical Cancer Research. 2014;20(4):859–867. doi: 10.1158/1078-0432.CCR-13-1343. [DOI] [PubMed] [Google Scholar]
- 20.Goodwin A. C., Destefano Shields C. E., Wu S., et al. Polyamine catabolism contributes to enterotoxigenic Bacteroides fragilis-induced colon tumorigenesis. Proceedings of the National Academy of Sciences of the United States of America. 2011;108(37):15354–15359. doi: 10.1073/pnas.1010203108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boleij A., Hechenbleikner E. M., Goodwin A. C., et al. The bacteroides fragilis toxin gene is prevalent in the colon mucosa of colorectal cancer patients. Clinical Infectious Diseases. 2015;60(2):208–215. doi: 10.1093/cid/ciu787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vujcic S., Diegelman P., Bacchi C. J., Kramer D. L., Porter C. W. Identification and characterization of a novel flavin-containing spermine oxidase of mammalian cell origin. Biochemical Journal. 2002;367(3):665–675. doi: 10.1042/BJ20020720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chaturvedi R., de Sablet T., Peek R. M., Wilson K. T. Spermine oxidase, a polyamine catabolic enzyme that links Helicobacter pylori CagA and gastric cancer risk. Gut microbes. 2012;3(1):48–56. doi: 10.4161/gmic.19345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chaturvedi R., de Sablet T., Asim M., et al. Increased Helicobacter pylori-associated gastric cancer risk in the Andean region of Colombia is mediated by spermine oxidase. Oncogene. 2015;34(26):3429–3440. doi: 10.1038/onc.2014.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mittal M., Siddiqui M. R., Tran K., Reddy S. P., Malik A. B. Reactive oxygen species in inflammation and tissue injury. Antioxidants and Redox Signaling. 2014;20(7):1126–1167. doi: 10.1089/ars.2012.5149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Van Zuylen L., Bridgewater J., Sparreboom A., et al. Phase I and pharmacokinetic study of the polyamine synthesis inhibitor SAM486A in combination with 5-fluorouracil/leucovorin in metastatic colorectal cancer. Clinical Cancer Research. 2004;10(6):1949–1955. doi: 10.1158/1078-0432.ccr-02-0995. [DOI] [PubMed] [Google Scholar]
- 27.Allen W. L., McLean E. G., Boyer J., et al. The role of spermidine/spermine N1-acetyltransferase in determining response to chemotherapeutic agents in colorectal cancer cells. Molecular Cancer Therapeutics. 2007;6(1):128–137. doi: 10.1158/1535-7163.MCT-06-0303. [DOI] [PubMed] [Google Scholar]
- 28.Pledgie A., Huang Y., Hacker A., et al. Spermine oxidase SMO(PAOh1), not N1-acetylpolyamine oxidase PAO, is the primary source of cytotoxic H2O2 in polyamine analogue-treated human breast cancer cell lines. The Journal of Biological Chemistry. 2005;280(48):39843–39851. doi: 10.1074/jbc.m508177200. [DOI] [PubMed] [Google Scholar]
- 29.Pledgie-Tracy A., Billam M., Hacker A., et al. The role of the Polyamine catabolic enzymes SSAT and SMO In the synergistic effects of standard chemotherapeutic agents with a Polyamine analogue In human breast cancer cell lines. Cancer Chemotherapy and Pharmacology. 2010;65(6):1067–1081. doi: 10.1007/s00280-009-1112-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mank-Seymour A. R., Murray T. R., Berkey K. A., Xiao L., Kern S., Casero R. A., Jr. Two active copies of the X-linked gene spermidine/spermine N1-acetyltransferase (SSAT) in a female lung cancer cell line are associated with an increase in sensitivity to an antitumor polyamine analogue. Clinical Cancer Research. 1998;4(8):2003–2008. [PubMed] [Google Scholar]
- 31.Hari D. M., Leung A. M., Lee J.-H., et al. AJCC cancer staging manual 7th edition criteria for colon cancer: do the complex modifications improve prognostic assessment? Journal of the American College of Surgeons. 2013;217(2):181–190. doi: 10.1016/j.jamcollsurg.2013.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Viljoen K. S., Dakshinamurthy A., Goldberg P., Blackburn J. M. Quantitative profiling of colorectal cancer-associated bacteria reveals associations between Fusobacterium spp., enterotoxigenic Bacteroides fragilis (ETBF) and clinicopathological features of colorectal cancer. PLoS ONE. 2015;10(3) doi: 10.1371/journal.pone.0119462.e0119462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fedorova M. S., Kudryavtseva A. V., Lakunina V. A., et al. Downregulation of OGDHL expression is associated with promoter hypermethylation in colorectal cancer. Molecular Biology. 2015;49(4):608–617. doi: 10.1134/s0026893315040044. [DOI] [PubMed] [Google Scholar]
- 34.Senchenko V. N., Anedchenko E. A., Kondratieva T. T., et al. Simultaneous down-regulation of tumor suppressor genes RBSP3/CTDSPL, NPRL2/G21 and RASSF1A in primary non-small cell lung cancer. BMC Cancer. 2010;10, article 75 doi: 10.1186/1471-2407-10-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Krasnov G. S., Oparina N. I., Dmitriev A. A., et al. Novel reference gene RPN1 for normalization of quantitative data in lung and kidney cancer. Molekuliarnaia Biologiia. 2011;45(2):238–248. [PubMed] [Google Scholar]
- 36.Doležel J., Bartoš J., Voglmayr H., Greilhuber J., Thomas R. A. Nuclear DNA content and genome size of trout and human. Cytometry Part: A. 2003;51(2):127–129. doi: 10.1002/cyto.a.10013. [DOI] [PubMed] [Google Scholar]
- 37.Senchenko V. N., Krasnov G. S., Dmitriev A. A., et al. Differential expression of CHL1 Gene during development of major human cancers. PLoS ONE. 2011;6(3) doi: 10.1371/journal.pone.0015612.e15612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Krasnov G. S., Dmitriev A. A., Melnikova N. V., et al. CrossHub: a tool for multi-way analysis of The Cancer Genome Atlas (TCGA) in the context of gene expression regulation mechanisms. Nucleic Acids Research. 2016;44(7, article e62) doi: 10.1093/nar/gkv1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Moore W. E. C., Cato E. P., Holdeman L. V. Some current concepts in intestinal bacteriology. American Journal of Clinical Nutrition. 1978;31(10):S33–S42. doi: 10.1093/ajcn/31.10.S33. [DOI] [PubMed] [Google Scholar]
- 40.Sears C. L., Geis A. L., Housseau F. Bacteroides fragilis subverts mucosal biology: from symbiont to colon carcinogenesis. The Journal of Clinical Investigation. 2014;124(10):4166–4172. doi: 10.1172/jci72334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sears C. L., Islam S., Saha A., et al. Association of enterotoxigenic Bacteroides fragilis infection with inflammatory diarrhea. Clinical Infectious Diseases. 2008;47(6):797–803. doi: 10.1086/591130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wick E. C., Sears C. L. Bacteroides spp. and diarrhea. Current Opinion in Infectious Diseases. 2010;23(5):470–474. doi: 10.1097/qco.0b013e32833da1eb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Swidsinski A., Weber J., Loening-Baucke V., Hale L. P., Lochs H. Spatial organization and composition of the mucosal flora in patients with inflammatory bowel disease. Journal of Clinical Microbiology. 2005;43(7):3380–3389. doi: 10.1128/JCM.43.7.3380-3389.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Housseau F., Sears C. L. Enterotoxigenic Bacteroides fragilis (ETBF)-mediated colitis in Min (Apc+/−) mice: a human commensal-based murine model of colon carcinogenesis. Cell Cycle. 2010;9(1):3–5. doi: 10.4161/cc.9.1.10352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wu S., Shin J., Zhang G., Cohen M., Franco A., Sears C. L. The Bacteroides fragilis toxin binds to a specific intestinal epithelial cell receptor. Infection and Immunity. 2006;74(9):5382–5390. doi: 10.1128/iai.00060-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sears C. L. Enterotoxigenic Bacteroides fragilis: a rogue among symbiotes. Clinical Microbiology Reviews. 2009;22(2):349–369. doi: 10.1128/cmr.00053-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wu S., Lim K.-C., Huang J., Saidi R. F., Sears C. L. Bacteroides fragilis enterotoxin cleaves the zonula adherens protein, E-cadherin. Proceedings of the National Academy of Sciences of the United States of America. 1998;95(25):14979–14984. doi: 10.1073/pnas.95.25.14979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wu S., Rhee K.-J., Zhang M., Franco A., Sears C. L. Bacteroides fragilis toxin stimulates intestinal epithelial cell shedding and γ-secretase-dependent E-cadherin cleavage. Journal of Cell Science. 2007;120, part 11:1944–1952. doi: 10.1242/jcs.03455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.David J. M., Rajasekaran A. K. Dishonorable discharge: the oncogenic roles of cleaved e-cadherin fragments. Cancer Research. 2012;72(12):2917–2923. doi: 10.1158/0008-5472.can-11-3498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kim J. M., Cho S. J., Oh Y.-K., Jung H.-Y., Kim Y.-J., Kim N. Nuclear factor-kappa B activation pathway in intestinal epithelial cells is a major regulator of chemokine gene expression and neutrophil migration induced by Bacteroides fragilis enterotoxin. Clinical and Experimental Immunology. 2002;130(1):59–66. doi: 10.1046/j.1365-2249.2002.01921.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kim J. M., Jung H. Y., Lee J. Y., Youn J., Lee C.-H., Kim K.-H. Mitogen-activated protein kinase and activator protein-1 dependent signals are essential for Bacteroides fragilis enterotoxin-induced enteritis. European Journal of Immunology. 2005;35(9):2648–2657. doi: 10.1002/eji.200526321. [DOI] [PubMed] [Google Scholar]
- 52.Wu S., Powell J., Mathioudakis N., Kane S., Fernandez E., Sears C. L. Bacteroides fragilis enterotoxin induces intestinal epithelial cell secretion of interleukin-8 through mitogen-activated protein kinases and a tyrosine kinase-regulated nuclear factor-κB pathway. Infection and Immunity. 2004;72(10):5832–5839. doi: 10.1128/iai.72.10.5832-5839.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wu S., Morin P. J., Maouyo D., Sears C. L. Bacteroides fragilis enterotoxin induces c-Myc expression and cellular proliferation. Gastroenterology. 2003;124(2):392–400. doi: 10.1053/gast.2003.50047. [DOI] [PubMed] [Google Scholar]
- 54.Hong S.-K. S., Chaturvedi R., Piazuelo M. B., et al. Increased expression and cellular localization of spermine oxidase in ulcerative colitis and relationship to disease activity. Inflammatory Bowel Diseases. 2010;16(9):1557–1566. doi: 10.1002/ibd.21224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dang C. V. MYC on the path to cancer. Cell. 2012;149(1):22–35. doi: 10.1016/j.cell.2012.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Krasnov G. S., Dmitriev A. A., Snezhkina A. V., Kudryavtseva A. V. Deregulation of glycolysis in cancer: glyceraldehyde-3-phosphate dehydrogenase as a therapeutic target. Expert Opinion on Therapeutic Targets. 2013;17(6):681–693. doi: 10.1517/14728222.2013.775253. [DOI] [PubMed] [Google Scholar]
- 57.Krasnov G. S., Dmitriev A. A., Lakunina V. A., Kirpiy A. A., Kudryavtseva A. V. Targeting VDAC-bound hexokinase II: a promising approach for concomitant anti-cancer therapy. Expert Opinion on Therapeutic Targets. 2013;17(10):1221–1233. doi: 10.1517/14728222.2013.833607. [DOI] [PubMed] [Google Scholar]
- 58.Dang C. V., Le A., Gao P. MYC-induced cancer cell energy metabolism and therapeutic opportunities. Clinical Cancer Research. 2009;15(21):6479–6483. doi: 10.1158/1078-0432.ccr-09-0889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Huber R., Pietsch D., Panterodt T., Brand K. Regulation of C/EBPβ and resulting functions in cells of the monocytic lineage. Cellular Signalling. 2012;24(6):1287–1296. doi: 10.1016/j.cellsig.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 60.Rahman S. M., Janssen R. C., Choudhury M., et al. CCAAT/enhancer-binding protein β (C/EBPβ) expression regulates dietary-induced inflammation in macrophages and adipose tissue in mice. The Journal of Biological Chemistry. 2012;287(41):34349–34360. doi: 10.1074/jbc.m112.410613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Natsuka S., Akira S., Nishio Y., et al. Macrophage differentiation-specific expression of NF-IL6, a transcription factor for interleukin-6. Blood. 1992;79(2):460–466. [PubMed] [Google Scholar]
- 62.Davydov I. V., Krammer P. H., Li-Weber M. Nuclear factor-IL6 activates the human IL-4 promoter in T cells. The Journal of Immunology. 1995;155(11):5273–5279. [PubMed] [Google Scholar]
- 63.van Dijk T. B., Baltus B., Raaijmakers J. A. M., Lammers J.-W. J., Koenderman L., De Groot R. P. A composite C/EBP binding site is essential for the activity of the promoter of the IL-3/IL-5/granulocyte-macrophage colony-stimulating factor receptor βc gene. Journal of Immunology. 1999;163(5):2674–2680. [PubMed] [Google Scholar]
- 64.Greenwel P., Tanaka S., Penkov D., et al. Tumor necrosis factor alpha inhibits type I collagen synthesis through repressive CCAAT/enhancer-binding proteins. Molecular and Cellular Biology. 2000;20(3):912–918. doi: 10.1128/MCB.20.3.912-918.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kawagoe H., Kandilci A., Kranenburg T. A., Grosveld G. C. Overexpression of N-Myc rapidly causes acute myeloid leukemia in mice. Cancer Research. 2007;67(22):10677–10685. doi: 10.1158/0008-5472.can-07-1118. [DOI] [PubMed] [Google Scholar]
- 66.van Noesel M. M., Pieters R., Voûte P. A., Versteeg R. The N-myc paradox: N-myc overexpression in neuroblastomas is associated with sensitivity as well as resistance to apoptosis. Cancer Letters. 2003;197(1-2):165–172. doi: 10.1016/s0304-3835(03)00101-0. [DOI] [PubMed] [Google Scholar]
- 67.Goodwin A. C., Jadallah S., Toubaji A., et al. Increased spermine oxidase expression in human prostate cancer and prostatic intraepithelial neoplasia tissues. Prostate. 2008;68(7):766–772. doi: 10.1002/pros.20735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cervelli M., Bellavia G., Fratini E., et al. Spermine oxidase (SMO) activity in breast tumor tissues and biochemical analysis of the anticancer spermine analogues BENSpm and CPENSpm. BMC Cancer. 2010;10, article 555 doi: 10.1186/1471-2407-10-555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nowotarski S. L., Woster P. M., Casero R. A., Jr. Polyamines and cancer: implications for chemotherapy and chemoprevention. Expert Reviews in Molecular Medicine. 2013;15, article e3 doi: 10.1017/erm.2013.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wang W., Liu L. Q., Higuchi C. M. Mucosal polyamine measurements and colorectal cancer risk. Journal of Cellular Biochemistry. 1996;63(2):252–257. doi: 10.1002/(SICI)1097-4644(19961101)63:2<252::AID-JCB12>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 71.Babbar N., Murray-Stewart T., Casero R. A., Jr. Inflammation and polyamine catabolism: the good, the bad and the ugly. Biochemical Society Transactions. 2007;35(2):300–304. doi: 10.1042/bst0350300. [DOI] [PubMed] [Google Scholar]
- 72.Coleman C. S., Hu G., Pegg A. E. Putrescine biosynthesis in mammalian tissues. Biochemical Journal. 2004;379(3):849–855. doi: 10.1042/BJ20040035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tabor C. W., Tabor H. Polyamines. Annual Review of Biochemistry. 1983;53:749–790. doi: 10.1146/annurev.bi.53.070184.003533. [DOI] [PubMed] [Google Scholar]
- 74.Babbar N., Gerner E. W. Targeting polyamines and inflammation for cancer prevention. Recent Results in Cancer Research. 2011;188:49–64. doi: 10.1007/978-3-642-10858-7_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Galea E., Regunathan S., Eliopoulos V., Feinstein D. L., Reis D. J. Inhibition of mammalian nitric oxide synthases by agmatine, an endogenous polyamine formed by decarboxylation of arginine. Biochemical Journal. 1996;316, part 1:247–249. doi: 10.1042/bj3160247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mistry S. K., Burwell T. J., Chambers R. M., et al. Cloning of human agmatinase. An alternate path for polyamine synthesis induced in liver by hepatitis B virus. American Journal of Physiology—Gastrointestinal and Liver Physiology. 2002;282(2):G375–G381. doi: 10.1152/ajpgi.00386.2001. [DOI] [PubMed] [Google Scholar]
- 77.Alteri C. J., Smith S. N., Mobley H. L. T. Fitness of Escherichia coliduring urinary tract infection requires gluconeogenesis and the TCA cycle. PLoS Pathogens. 2009;5(5) doi: 10.1371/journal.ppat.1000448.e1000448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Casero R. A., Jr., Wang Y., Stewart T. M., et al. The role of polyamine catabolism in anti-tumour drug response. Biochemical Society Transactions. 2003;31(2):361–365. doi: 10.1042/BST0310361. [DOI] [PubMed] [Google Scholar]
- 79.Pegg A. E. Spermidine/spermine-N 1-acetyltransferase: a key metabolic regulator. American Journal of Physiology—Endocrinology and Metabolism. 2008;294(6):E995–E1010. doi: 10.1152/ajpendo.90217.2008. [DOI] [PubMed] [Google Scholar]
- 80.Morada M., Pendyala L., Wu G., Merali S., Yarlett N. Cryptosporidium parvum induces an endoplasmic stress response in the intestinal adenocarcinoma HCT-8 cell line. The Journal of Biological Chemistry. 2013;288(42):30356–30364. doi: 10.1074/jbc.m113.459735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Babbar N., Hacker A., Huang Y., Casero R. A., Jr. Tumor necrosis factor α induces spermidine/spermine N 1-acetyltransferase through nuclear factor κB in non-small cell lung cancer cells. Journal of Biological Chemistry. 2006;281(34):24182–24192. doi: 10.1074/jbc.m601871200. [DOI] [PubMed] [Google Scholar]
- 82.Babbar N., Gerner E. W., Casero R. A., Jr. Induction of spermidine/spermine N 1-acetyltransferase (SSAT) by aspirin in Caco-2 colon cancer cells. Biochemical Journal. 2006;394(1):317–324. doi: 10.1042/bj20051298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Smirnova O. A., Isaguliants M. G., Hyvonen M. T., et al. Chemically induced oxidative stress increases polyamine levels by activating the transcription of ornithine decarboxylase and spermidine/spermine- N1-acetyltransferase in human hepatoma HUH7 cells. Biochimie. 2012;94(9):1876–1883. doi: 10.1016/j.biochi.2012.04.023. [DOI] [PubMed] [Google Scholar]
- 84.Ruiz-Pérez M. V., Medina M. Á., Urdiales J. L., Keinänen T. A., Sánchez-Jiménez F. Polyamine metabolism is sensitive to glycolysis inhibition in human neuroblastoma cells. The Journal of Biological Chemistry. 2015;290(10):6106–6119. doi: 10.1074/jbc.m114.619197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Paz E. A., Garcia-Huidobro J., Ignatenko N. A. Polyamines in cancer. Advances in Clinical Chemistry. 2011;54:45–70. doi: 10.1016/b978-0-12-387025-4.00002-9. [DOI] [PubMed] [Google Scholar]
- 86.Iyengar R. V., Pawlik C. A., Krull E. J., et al. Use of a modified ornithine decarboxylase promoter to achieve efficient c-MYC- or N-MYC-regulated protein expression. Cancer Research. 2001;61(7):3045–3052. [PubMed] [Google Scholar]
- 87.Forshell T. P., Rimpi S., Nilsson J. A. Chemoprevention of B-cell lymphomas by inhibition of the Myc target spermidine synthase. Cancer Prevention Research. 2010;3(2):140–147. doi: 10.1158/1940-6207.CAPR-09-0166. [DOI] [PubMed] [Google Scholar]
- 88.Marinkovic D., Marinkovic T., Kokai E., Barth T., Möller P., Wirth T. Identification of novel Myc target genes with a potential role in lymphomagenesis. Nucleic Acids Research. 2004;32(18):5368–5378. doi: 10.1093/nar/gkh877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wagner A. J., Meyers C., Laimins L. A., Hay N. c-Myc induces the expression and activity of ornithine decarboxylase. Cell Growth and Differentiation. 1993;4(11):879–884. [PubMed] [Google Scholar]
- 90.Chaturvedi R., Cheng Y., Asim M., et al. Induction of polyamine oxidase 1 by Helicobacter pylori causes macrophage apoptosis by hydrogen peroxide release and mitochondrial membrane depolarization. The Journal of Biological Chemistry. 2004;279(38):40161–40173. doi: 10.1074/jbc.m401370200. [DOI] [PubMed] [Google Scholar]
- 91.Hughes A., Smith N. I., Wallace H. M. Polyamines reverse non-steroidal anti-inflammatory drug-induced toxicity in human colorectal cancer cells. Biochemical Journal. 2003;374(2):481–488. doi: 10.1042/BJ20030280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Meyskens F. L., Jr., McLaren C. E., Pelot D., et al. Difluoromethylornithine plus sulindac for the prevention of sporadic colorectal adenomas: a randomized placebo-controlled, double-blind trial. Cancer Prevention Research. 2008;1(1):32–38. doi: 10.1158/1940-6207.capr-08-0042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ben-Yosef T., Yanuka O., Halle D., Benvenisty N. Involvement of Myc targets in c-myc and N-myc induced human tumors. Oncogene. 1998;17(2):165–171. doi: 10.1038/sj.onc.1201939. [DOI] [PubMed] [Google Scholar]
- 94.Park M. H. The post-translational synthesis of a polyamine-derived amino acid, hypusine, in the eukaryotic translation initiation factor 5A (eIF5A) Journal of Biochemistry. 2006;139(2):161–169. doi: 10.1093/jb/mvj034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Fernandez P. C., Frank S. R., Wang L., et al. Genomic targets of the human c-Myc protein. Genes and Development. 2003;17(9):1115–1129. doi: 10.1101/gad.1067003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Gerner E. W. Cancer chemoprevention locks onto a new polyamine metabolic target. Cancer Prevention Research. 2010;3(2):125–127. doi: 10.1158/1940-6207.CAPR-09-0252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Meng Q.-B., Kang W.-M., Yu J.-C., et al. Overexpression of eukaryotic translation initiation factor 5A2 (EIF5A2) correlates with cell aggressiveness and poor survival in gastric cancer. PLoS ONE. 2015;10(3) doi: 10.1371/journal.pone.0119229.e0119229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zhu W., Cai M.-Y., Tong Z.-T., et al. Overexpression of EIF5A2 promotes colorectal carcinoma cell aggressiveness by upregulating MTA1 through C-myc to induce epithelial-mesenchymaltransition. Gut. 2012;61(4):562–575. doi: 10.1136/gutjnl-2011-300207. [DOI] [PubMed] [Google Scholar]
- 99.Roos A. B., Barton J. L., Miller-Larsson A., et al. Lung epithelial-C/EBPβ contributes to LPS-induced inflammation and its suppression by formoterol. Biochemical and Biophysical Research Communications. 2012;423(1):134–139. doi: 10.1016/j.bbrc.2012.05.096. [DOI] [PubMed] [Google Scholar]
- 100.Chinery R., Brockman J. A., Dransfield D. T., Coffey R. J. Antioxidant-induced nuclear translocation of CCAAT/enhancer-binding protein β. A critical role for protein kinase A-mediated phosphorylation of Ser299. The Journal of Biological Chemistry. 1997;272(48):30356–30361. doi: 10.1074/jbc.272.48.30356. [DOI] [PubMed] [Google Scholar]
- 101.Brooks W. H. Increased polyamines alter chromatin and stabilize autoantigens in autoimmune diseases. Frontiers in Immunology. 2013;4, article 91 doi: 10.3389/fimmu.2013.00091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sauter M., Moffatt B., Saechao M. C., Hell R., Wirtz M. Methionine salvage and S-adenosylmethionine: essential links between sulfur, ethylene and polyamine biosynthesis. Biochemical Journal. 2013;451(2):145–154. doi: 10.1042/bj20121744. [DOI] [PubMed] [Google Scholar]
- 103.Lu S. C., Mato J. M. S-adenosylmethionine in liver health, injury, and cancer. Physiological Reviews. 2012;92(4):1515–1542. doi: 10.1152/physrev.00047.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Sufrin J. R., Finckbeiner S., Oliver C. M. Marine-derived metabolites of S-adenosylmethionine as templates for new anti-infectives. Marine Drugs. 2009;7(3):401–434. doi: 10.3390/md7030401. [DOI] [PMC free article] [PubMed] [Google Scholar]