Abstract
Objectives. To document how health insurance coverage changed for White, Black, and Hispanic adults after the Affordable Care Act (ACA) went into effect.
Methods. We used data from the American Community Survey from 2008 to 2014 to examine changes in the percentage of nonelderly adults who were uninsured, covered by Medicaid, or covered by private health insurance. In addition to presenting overall trends by race/ethnicity, we stratified the analysis by income group and state Medicaid expansion status.
Results. In 2013, 40.5% of Hispanics and 25.8% of Blacks were uninsured, compared with 14.8% of Whites. We found a larger gap in private insurance, which was partially offset by higher rates of public coverage among Blacks and Hispanics. After the main ACA provisions went into effect in 2014, coverage disparities declined slightly as the percentage of adults who were uninsured decreased by 7.1 percentage points for Hispanics, 5.1 percentage points for Blacks, and 3 percentage points for Whites. Coverage gains were greater in states that expanded Medicaid programs.
Conclusions. The ACA has reduced racial/ethnic disparities in coverage, although substantial disparities remain. Further increases in coverage will require Medicaid expansion by more states and improved program take-up in states that have already done so.
Large disparities in health insurance coverage related to race and ethnicity are a long-standing feature of the US health care system and a cause for concern among policymakers and health care professionals. Several studies have identified these differences in insurance coverage as an important determinant of disparities in access to care.1–5 In addition, a growing literature shows that by reducing exposure to large medical expenses, health insurance leads to better financial outcomes, such as improved credit scores and a reduced risk of bankruptcy.6–9 Thus, policies that reduce disparities in health insurance coverage are likely to have a broader effect on economic inequality.
The Affordable Care Act (ACA) has made new health insurance options available to uninsured individuals in low- and middle-income households, a group in which Blacks and Hispanics are overrepresented. A recent study by McMorrow et al.10 that used data from the National Health Interview Survey found that although the uninsured rate declined overall between 2013 and 2014, it decreased by a larger amount among Black and Hispanic adults than among White adults (8 percentage points vs 4 percentage points). The uninsured rate for Black and Hispanic adults decreased significantly in states that embraced the ACA’s Medicaid expansion and also in those that did not. For White adults, the percentage uninsured declined in both sets of states, although the estimated change was not statistically significant in nonexpansion states.
In this study, we used data from the American Community Survey (ACS) spanning the years 2008 to 2014 to provide additional evidence on how health insurance coverage changed for Black and Hispanic adults compared with White adults in the first year after the implementation of health care reform. We extended existing analyses in several ways. First, in addition to documenting changes in the rate of uninsurance, we investigated changes in the source of coverage. This more detailed analysis indicated that the significant disparities in the percentage of adults with any insurance prior to 2014 were driven by even larger disparities in private coverage, which were partially offset by the fact that minority adults were more likely than Whites to have public insurance. We found that both types of coverage increased more for Blacks and Hispanics than for Whites between 2013 and 2014. As a result, disparities in both overall coverage and private insurance coverage declined.
Second, we considered important sources of heterogeneity within the different racial and ethnic groups. In particular, it is important to account for the fact that approximately one third of all Hispanic adults living in the United States are not citizens. Immigrants who are not citizens have substantially lower rates of health insurance coverage because they are less likely to work in jobs that provide employer-sponsored insurance,11 they face restrictions on Medicaid eligibility,12 and they may be less likely to take up coverage when eligible. Because undocumented immigrants are excluded from the ACA’s major coverage expansions,12 one concern is that this group will become even more marginalized in the post-ACA health care system.13
Third, in addition to documenting changes in coverage rates, we investigated the extent to which the disparities in coverage that remained in 2014 were related to income and to state decisions regarding the ACA’s Medicaid expansion.
COVERAGE PROVISIONS OF THE ACA
The ACA includes provisions to expand both Medicaid and private coverage, with the goal of reaching many of the 50 million individuals who were uninsured in 2010 when the law was enacted. Prior to the ACA, states covered low-income children and their families through Medicaid and the Children’s Health Insurance Program. However, states typically did not provide coverage for nonelderly childless adults. In addition, some low-income parents remained uninsured because income eligibility levels for parents were typically significantly lower than those for children.14
The ACA created substantial new federal funding for states to extend coverage to all adults with family income below 138% of the federal poverty level (FPL) (or about $33 000 for a family of 4 in 2014). Although the ACA originally required states to extend their Medicaid programs to this population, a June 2012 Supreme Court ruling essentially made the expansion optional.15,16 As of January 2016, 31 states plus the District of Columbia had decided to implement the Medicaid expansion.17 In most of these states, the new eligibility rules went into effect in January 2014.
The ACA also included some provisions intended to make private health insurance more accessible. One of the earliest to take effect required health plans providing dependent coverage for children to extend that offer up to age 26 years. This requirement, which went into effect in September 2010, led to a significant increase in insurance coverage among the target population of those aged 19 to 25 years.18–22 Estimates of the number of young adults who gained coverage range from about 1 million18,22 to 3 million.21
The law also introduced a set of insurance market reforms, such as prohibiting plans from denying coverage or charging higher premiums because of an applicant’s preexisting health condition. It established an essential benefits package and new health insurance “marketplaces,” which are intended to facilitate individuals’ plan choices by standardizing benefit options and providing a Web site where enrollees can easily compare plans. Importantly, the law provides premium tax credits for families with incomes between 100% and 400% of the FPL to purchase coverage through the marketplaces, provided that they do not already have access to comprehensive coverage through an employer or a public program. Families with incomes below 250% of the FPL who are eligible for premium tax credits are also eligible for additional subsidies to cover cost sharing at the point of service. Finally, the ACA incentivizes health insurance enrollment by establishing penalties for individuals who forgo coverage, as well as for large employers that do not offer affordable coverage to their employees.
Important exceptions apply to noncitizens. Undocumented immigrants are excluded from the ACA’s major coverage expansions.12,23 For example, they are barred from purchasing coverage on the exchanges (even unsubsidized coverage).12 By contrast, lawfully present noncitizens are generally permitted to purchase coverage on the exchanges, are eligible for premium tax credits and cost-sharing subsidies based on family income, and are subject to the individual mandate.12,23 On the basis of rules that preceded the ACA, some groups of lawfully present noncitizens are ineligible for full Medicaid coverage, including most legal permanent residents who have resided in the United States for less than 5 years. Perhaps for this reason, lawfully present noncitizens with incomes below the poverty level who are ineligible for Medicaid may instead be eligible for marketplace premium tax credits and cost-sharing subsidies (a benefit unavailable to other groups below the poverty level).12,24
AMERICAN COMMUNITY SURVEY DATA
Our analysis was based on repeated cross-sectional data from the ACS spanning the years 2008 through 2014. Although the ACS has been less widely used to study health insurance coverage than another US Census Bureau data set, the Annual Social and Economic Supplement to the Current Population Survey (CPS), a significant redesign of the CPS in 2014 presents challenges for using that survey to analyze changes over time.25 Before the CPS redesign, the 2 surveys produced slightly different estimates of insurance coverage because of differences in question design. However, because these differences were constant over time, estimates of trends in insurance coverage were comparable.26 Another advantage of the ACS is that it is much larger than other surveys, making it possible to obtain precise estimates, even for narrowly defined subpopulations.27 For our analysis, we had samples of nearly 1.7 million observations per year.
METHODS
The ACS asks about current health insurance coverage and provides a list of possible sources: through an employer or union, directly from an insurance company, Medicare, Medicaid, TRICARE, Department of Veterans Affairs, Indian Health Service, or other. Respondents may choose all that apply, and those who state that they do not have coverage through any of those sources are coded as being uninsured.
In our analysis, we examined changes in the percentage of individuals who were uninsured as well as the percentage with private and public coverage. For nonelderly adults, Medicaid was the dominant source of public insurance, but this category also includes Medicare (covering disabled adults) and the Department of Veterans Affairs. About 4% of the adult respondents reported having both public and private coverage during the year. When we examined coverage by source, we categorized these individuals as having public insurance and limited the private insurance category to individuals who reported having only private coverage.
Because the coverage provisions of the ACA taking effect in 2014 were targeted mainly at nonelderly adults, we restricted our sample to individuals between ages 19 and 64 years. We also focused on non-Hispanic Whites, non-Hispanic Blacks, and Hispanics (who may be any race), in line with much of the literature on health disparities. For simplicity, we refer to these 3 groups as Whites, Blacks, and Hispanics. In some analyses, we further divided the Hispanic group into those who were US citizens and those who were not. Although, as noted earlier, some ACA eligibility rules distinguish between undocumented immigrants and those who are lawfully present in the United States, legal status is not recorded in the ACS.
It is important to note that the observed magnitude of differences between groups depends on the extent to which the analysis controls for observable characteristics. Many individual attributes that differ systematically across racial and ethnic groups—such as income and education levels—likely affect health outcomes, and there is an active debate about which attributes should be held constant when measuring disparities. Three common approaches for evaluating health disparities involve comparing (1) unadjusted differences in means, (2) differences in means after controlling for health needs and preferences (the definition adopted in the 2003 Institute of Medicine report Unequal Treatment),28 and (3) differences in means after controlling for as many variables as possible (e.g., socioeconomic status).29 Because our primary objective was to document population-level changes in insurance coverage, much of our analysis relied on the first approach, but we also stratified results by income group and state Medicaid expansion status.
RESULTS
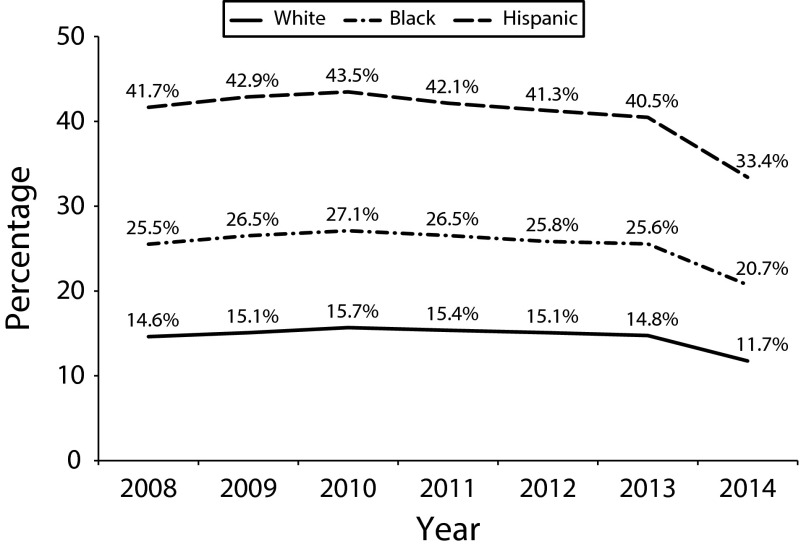
Figure 1 presents trends from 2008 through 2014 in the percentage of White, Black, and Hispanic adults who were uninsured. For each group, the percentage of adults who were uninsured increased between 2008 and 2010 before declining slightly between 2010 and 2013. Over that period, the average coverage gap between Blacks and Whites was about 11 percentage points, and the average gap between Hispanics and Whites was more than twice as large (27 percentage points).
FIGURE 1—
Percentage of US Nonelderly Adults (Aged 19–64) Uninsured, by Race and Ethnicity: American Community Survey, United States, 2008–2014
In 2014, the percentage without coverage dropped significantly for all 3 groups but more for minorities than for Whites. The percentage uninsured fell by 7.1 percentage points for Hispanics (a 17% decline relative to 2013), by 5.1 percentage points for Blacks (a 20% decline), and by 3 percentage points for Whites (a 21% decline). As a result of these differential changes, the White–Black coverage gap decreased by 2 percentage points, from 11 to 9 percentage points, and the White–Hispanic gap decreased by 4.3 percentage points, from 26.5 to 22.2 percentage points. This result is in line with the study by McMorrow et al.,10 which also found a reduction in the White–Black and White–Hispanic coverage gaps.
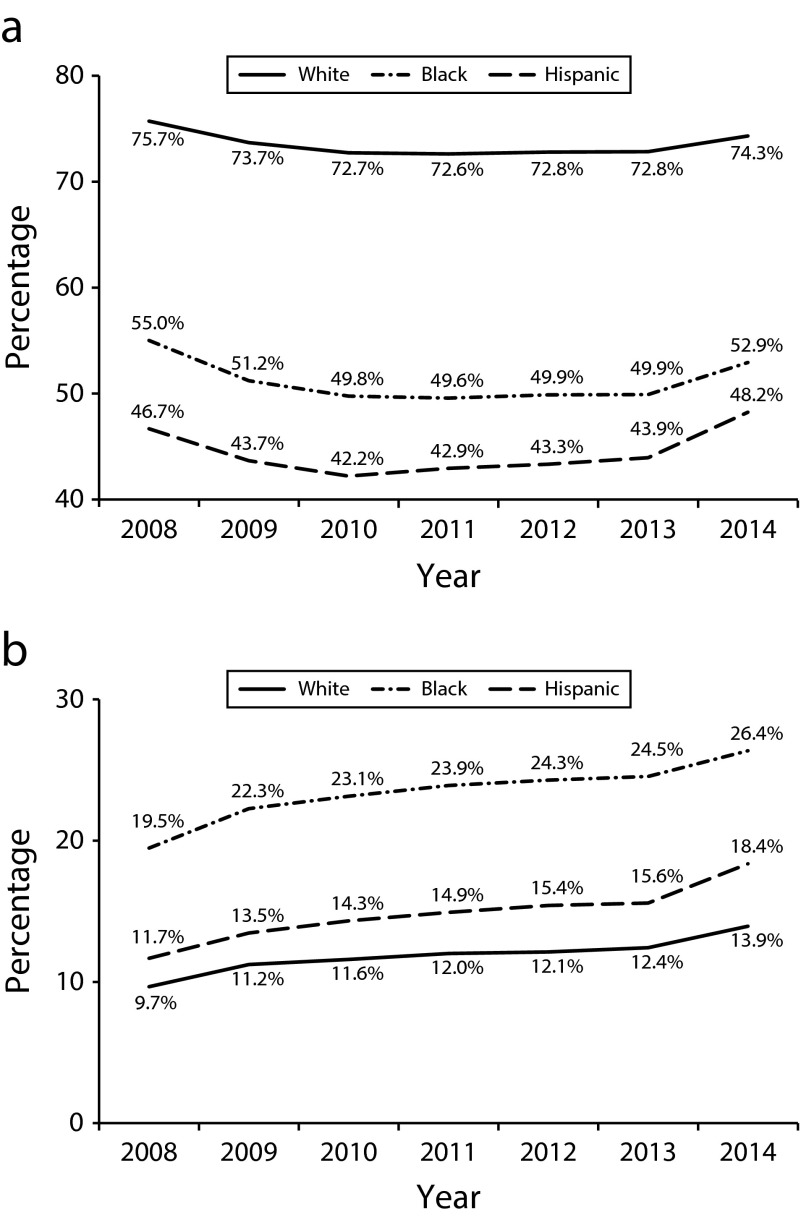
Figure 2 shows that racial and ethnic differences in the percentage of adults with any insurance represent the combined effect of very large disparities in private insurance that are partially offset by the far greater public coverage of minorities, especially Black adults. For all groups, private coverage declined between 2008 and 2013, before increasing between 2013 and 2014 (Figure 2a). Both the percentage point increase and the percent gain (relative to the 2013 level) were greater for minorities than for Whites. Private coverage increased by 4.3 percentage points for Hispanics (an 9.8% increase relative to the 2013 rate of 43.9%), by 3 percentage points for Blacks (a 6% increase), and by 1.5 percentage points for Whites (a 2.1% increase). Thus, the gaps in both any coverage and private insurance declined. However, even with these gains, the percentage of Whites and Blacks with private insurance was lower in 2014 than in 2008.
FIGURE 2—
Percentage of US Nonelderly Adults (Aged 19–64 Years) by Race and Ethnicity With (a) Private and (b) Public Health Insurance Coverage: American Community Survey, United States, 2008–2014
In contrast to the case of private insurance, the percentage of adults enrolled in public insurance programs increased steadily between 2008 and 2013. Public coverage increased even more between 2013 and 2014: by 2.8 percentage points for Hispanics, 1.9 percentage points for Blacks, and 1.5 percentage points for Whites.
Table 1 provides more detailed information on how insurance coverage changed between 2013 and 2014. Here, we distinguish between Hispanics who are and are not US citizens. The results show large differences between these 2 groups. Just prior to the ACA insurance expansions, more than 60% of Hispanic noncitizens were uninsured, compared with 28% of Hispanic citizens. The latter figure is just slightly higher than the uninsured rate for Blacks. The percentage point change between 2013 and 2014 was similar for Hispanic noncitizens and citizens (7.0 and 6.7 percentage points, respectively), although the percent increase was much larger for citizens (23.9% vs 10.9%) because their baseline rate was much lower. In adults with family income below 138% of the FPL, the uninsured rate declined more for Hispanic citizens than for Hispanic noncitizens (9.3 vs 6.1 percentage points).
TABLE 1—
Changes in the US Uninsured Rate by Race/Ethnicity, Income Category, and State Medicaid Expansion Status: American Community Survey, United States, 2013–2014
| All States |
Nonexpansion States |
Expansion States |
|||||||
| Variable | 2013, % | 2014, % | Change, Percentage Points | 2013, % | 2014, % | Change, Percentage Points | 2013, % | 2014, % | Change, Percentage Points |
| All nonelderly adults | |||||||||
| White | 14.8 | 11.7 | −3.1a | 16.5 | 14.2 | −2.3a | 13.8 | 10.5 | −3.3a |
| Black | 25.8 | 20.7 | −5.1a,b | 27.9 | 23.9 | −4.0a,b | 23.6 | 18.0 | −5.6a,b |
| Hispanic, citizen | 28.0 | 21.3 | −6.7a,b | 34.1 | 28.7 | −5.4a,b | 25.7 | 18.5 | −7.2a,b |
| Hispanic, noncitizen | 64.3 | 57.3 | −7.0a,b | 72.5 | 67.4 | −5.1a,b | 60.5 | 52.7 | −7.8a,b |
| < 139% of FPL | |||||||||
| White | 32.8 | 25.7 | −7.1a | 37.0 | 32.2 | −4.8a | 30.5 | 22.1 | −8.4a |
| Black | 35.6 | 28.9 | −6.7a,b | 40.4 | 34.9 | −5.5a | 31.5 | 23.7 | −7.8a |
| Hispanic, citizen | 40.5 | 31.2 | −9.3a,b | 53.3 | 45.8 | −7.5a,b | 35.7 | 25.6 | −10.1a,b |
| Hispanic, noncitizen | 72.7 | 66.6 | −6.1a,b | 81.5 | 78.2 | −3.3a | 68.4 | 60.9 | −7.5a,b |
| 139%–399% of FPL | |||||||||
| White | 18.0 | 14.5 | −3.5a | 18.7 | 16.1 | −2.6a | 17.7 | 13.6 | −4.1a |
| Black | 23.7 | 18.5 | −5.2a,b | 24.1 | 20.2 | −3.9a,b | 23.3 | 17.0 | −6.3a,b |
| Hispanic, citizen | 29.5 | 21.9 | −7.6a,b | 33.4 | 27.8 | −5.6a,b | 28.0 | 19.7 | −8.3a,b |
| Hispanic, noncitizen | 60.9 | 53.4 | −7.5a,b | 68.1 | 61.5 | −6.6a,b | 57.7 | 49.8 | −7.9a,b |
| ≥ 400% of FPL | |||||||||
| White | 5.2 | 4.2 | −1.0a | 5.6 | 4.7 | −0.9a | 5.0 | 3.9 | −1.1a |
| Black | 10.2 | 7.8 | −2.4a,b | 10.5 | 8.3 | −2.2a,b | 10.0 | 7.4 | −2.6a,b |
| Hispanic, citizen | 11.0 | 9.0 | −2.0a,b | 12.8 | 11.3 | −1.5a | 10.3 | 8.1 | −2.2a,b |
| Hispanic, noncitizen | 38.3 | 32.3 | −6.0a,b | 43.2 | 38.0 | −5.2a,b | 36.4 | 30.1 | −6.3a,b |
Note. FPL = federal poverty level. Expansion states are defined as all states that had implemented the Affordable Care Act Medicaid expansion by July 2014.
The change between 2013 and 2014 was significantly different from 0 at the .05 level.
The change between 2013 and 2014 was significantly different from the corresponding change for Whites at the .05 level.
Dividing the data by state Medicaid expansion status, we found that the percent uninsured was lower in expansion states in 2013 and declined more in those states than in nonexpansion states. The percentage of Blacks without health insurance decreased by 5.6 percentage points in expansion states and by 4 percentage points in nonexpansion states. For Hispanics, the uninsured rate decreased by more than 7 percentage points in expansion states and by 5.1 to 5.4 percentage points in nonexpansion states.
DISCUSSION
The data suggest that both before and after the ACA coverage expansions went into effect, differences in income explain much—but not all—of the coverage gap between Blacks and Whites. For example, in 2014, the gap was only 3.2 percentage points among adults in the lowest income category, compared with a gap of 9 points among all adults. Income also appears to explain a sizable, although smaller, portion of the coverage gap between Whites and Hispanic citizens. By contrast, even within income categories, the coverage gap between Whites and Hispanic noncitizens was extremely large. In the lowest income category, the gap was more than 40 percentage points in both nonexpansion and expansion states. Regarding the different types of coverage, Hispanic noncitizens were approximately half as likely to have public insurance as Whites in this income category (21% nationally vs 40%; data not shown). This suggests that the eligibility restrictions facing many Hispanic immigrants, along with language barriers and a reluctance to use benefits for which they qualify, have a substantial negative effect on coverage for this group.
Other differences in individual characteristics likely contributed to coverage disparities but in different ways for Blacks and Hispanics. One factor that is of particular policy significance was the share of each group living in an expansion state. In our sample, the percentage of Blacks living in expansion states was lower than the percentage of Whites—54% versus 69%—whereas both groups of Hispanics were more likely than Whites to live in an expansion state (73% for citizens and 71% for noncitizens). However, simple simulation analyses suggested that if coverage changes in nonexpansion states had been comparable to those observed in expansion states, then the national uninsured rate for Blacks would have been only slightly lower than what we actually observed. For example, if we assumed an equal percentage point change, then 22.3% of the Blacks in nonexpansion states would have been uninsured in 2014, and the national rate would have been 20.0% rather than 20.7%. Alternatively, if we assumed an equal percent decline, then the national uninsured rate for Blacks would have been 19.5%, and the coverage gap relative to Whites would have been 8.4 rather than 9 percentage points.
The fact that racial and ethnic disparities remain among low-income adults in expansion states implies that further increases in coverage will require not only the adoption of Medicaid expansion by more states but also an improvement in program take-up in states that have already done so. Evidence from a previous expansion for children suggests that linguistically and culturally targeted outreach strategies can be effective in increasing program take-up among eligible individuals.30,31
At the same time, other approaches will be necessary to improve access to care for the large portion of poor noncitizens who remain ineligible for Medicaid and exchange-based subsidies. One such approach would be the expansion of benefits to undocumented individuals using state funds. California recently became the fifth and largest state to provide health coverage to undocumented children, and legislators in the state have considered extending Medicaid coverage to undocumented adults as well.32,33 Given estimates that about half of California’s 2.7 million undocumented immigrants have incomes below 138% of the FPL,34 such a policy could significantly increase coverage among this very disadvantaged population.
We have provided a snapshot of how insurance coverage changed in the first year after the main provisions of the ACA were in place. Consistent with evidence from other data sources, our analysis of the ACS indicates that the reform has not only increased the overall rate of insurance coverage in the United States but also led to a slight reduction in coverage disparities related to race and ethnicity. Hispanics, who have the lowest rate of insurance coverage among all racial/ethnic groups, experienced greater increases in private and public coverage than did Blacks, who experienced greater gains than did Whites. For all 3 groups, coverage increased more in states that implemented the Medicaid expansion than in states that did not. However, even with the gains in coverage brought about by the ACA, more than 30 million Americans remain uninsured.35 Racial and ethnic minorities continue to make up a disproportionate share of both the overall uninsured population and the uninsured with incomes below the Medicaid eligibility threshold.
ACKNOWLEDGMENTS
This work has been supported in part by the Russell Sage Foundation (award 83-14-13). H. G. Levy also acknowledges financial support from the National Institute on Aging (grant NIA K01AG034232).
Note. Any opinions expressed are those of the authors alone and should not be construed as representing the opinions of the Russell Sage Foundation.
HUMAN PARTICIPANT PROTECTION
Because this study used only publicly available data, it was not subject to regulation by the University of Michigan institutional review board.
Footnotes
See also Galea and Vaughan, p. 1354.
REFERENCES
- 1.Hargraves JL, Hadley J. The contribution of insurance coverage and community resources to reducing racial/ethnic disparities in access to care. Health Serv Res. 2003;38(3):809–829. doi: 10.1111/1475-6773.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lillie-Blanton M, Hoffman C. The role of health insurance coverage in reducing racial/ethnic disparities in health care. Health Aff (Millwood) 2005;24(2):398–408. doi: 10.1377/hlthaff.24.2.398. [DOI] [PubMed] [Google Scholar]
- 3.Mahmoudi E, Jensen GA. Diverging racial and ethnic disparities in access to physician care: comparing 2000 and 2007. Med Care. 2012;50(4):327–334. doi: 10.1097/MLR.0b013e318245a111. [DOI] [PubMed] [Google Scholar]
- 4.Waidmann TA, Rajan S. Race and ethnic disparities in health care access and utilization: an examination of state variation. Med Care Res Rev. 2000;57(suppl 1):55–84. doi: 10.1177/1077558700057001S04. [DOI] [PubMed] [Google Scholar]
- 5.Zuvekas SH, Taliaferro GS. Pathways to access: health insurance, the health care delivery system, and racial/ethnic disparities, 1996-1999. Health Aff (Millwood) 2003;22(2):139–153. doi: 10.1377/hlthaff.22.2.139. [DOI] [PubMed] [Google Scholar]
- 6.Barcellos SH, Jacobson M. The effects of Medicare on medical expenditure risk and financial strain. Am Econ J Econ Policy. 2015;7(4):41–70. doi: 10.1257/pol.20140262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Finkelstein A, Taubman S, Wright B et al. The Oregon health insurance experiment: evidence from the first year. Q J Econ. 2012;127(3):1057–1106. doi: 10.1093/qje/qjs020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gross T, Notowidigdo MJ. Health insurance and the consumer bankruptcy decision: evidence from expansions of Medicaid. J Public Econ. 2011;95(7-8):767–778. [Google Scholar]
- 9.Mazumder B, Miller S. The effects of the Massachusetts health reform on household financial distress. Am Econ J Econ Policy. 2015;Epub ahead of print. [Google Scholar]
- 10.McMorrow S, Long SK, Kenney GM, Anderson N. Uninsurance disparities have narrowed for Black and Hispanic adults under the Affordable Care Act. Health Aff (Millwood) 2015;34(10):1774–1778. doi: 10.1377/hlthaff.2015.0757. [DOI] [PubMed] [Google Scholar]
- 11.Buchmueller TC, Lo Sasso AT, Lurie I, Dolfin S. Immigrants and employer-sponsored health insurance. Health Serv Res. 2007;42(1 pt 1):286–310. doi: 10.1111/j.1475-6773.2006.00600.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Congressional Research Service. Treatment of noncitizens under the Affordable Care Act. May 21, 2014. Available at: http://www.fas.org/sgp/crs/misc/R43561.pdf. Accessed November 16, 2015.
- 13.Zuckerman S, Waidmann TA, Lawton E. Undocumented immigrants, left out of health reform, likely to continue to grow as share of the uninsured. Health Aff (Millwood) 2011;30(10):1997–2004. doi: 10.1377/hlthaff.2011.0604. [DOI] [PubMed] [Google Scholar]
- 14.Heberlein M, Huntress M, Kenney G, Alker J, Lynch V, Mancini T. Medicaid coverage for parents under the Affordable Care Act. 2012. Available at: http://ccf.georgetown.edu/wp-content/uploads/2012/06/Medicaid-Coverage-for-Parents1.pdf. Accessed November 16, 2015.
- 15.Kaiser Family Foundation. Summary of the Affordable Care Act. April 25, 2013. Available at: http://kff.org/health-reform/fact-sheet/summary-of-the-affordable-care-act. Accessed November 16, 2015.
- 16.Kaiser Family Foundation. A guide to the Supreme Court’s decision on the ACA’s Medicaid expansion. August 1, 2012. Available at: http://kff.org/health-reform/issue-brief/a-guide-to-the-supreme-courts-decision. Accessed November 16, 2015.
- 17.Kaiser Family Foundation. Status of state action on the Medicaid expansion decision. 2016. Available at: http://kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act. Accessed January 22, 2016.
- 18.Antwi YA, Moriya AS, Simon K. Effects of federal policy to insure young adults: evidence from the 2010 Affordable Care Act’s dependent-coverage mandate. Am Econ J Econ Policy. 2013;5(4):1–28. [Google Scholar]
- 19.Cantor JC, Monheit AC, DeLia D, Lloyd K. Early impact of the Affordable Care Act on health insurance coverage of young adults. Health Serv Res. 2012;47(5):1773–1790. doi: 10.1111/j.1475-6773.2012.01458.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.O’Hara B, Brault MW. The disparate impact of the ACA-dependent expansion across population subgroups. Health Serv Res. 2013;48(5):1581–1592. doi: 10.1111/1475-6773.12067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sommers BD. Number of young adults gaining insurance due to the Affordable Care Act now tops 3 million. June 19, 2012. Available at: http://aspe.hhs.gov/basic-report/number-young-adults-gaining-insurance-due-affordable-care-act-now-tops-3-million. Accessed October 24, 2015.
- 22.Sommers BD, Buchmueller T, Decker SL, Carey C, Kronick R. The Affordable Care Act has led to significant gains in health insurance and access to care for young adults. Health Aff (Millwood) 2013;32(1):165–174. doi: 10.1377/hlthaff.2012.0552. [DOI] [PubMed] [Google Scholar]
- 23.Fried B, Pintor JK, Graven P, Blewett LA. Implementing federal health reform in the states: who is included and excluded and what are their characteristics? Health Serv Res. 2014;49(suppl 2):2062–2085. doi: 10.1111/1475-6773.12232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.HealthCare.gov. Coverage for lawfully present immigrants. 2015. Available at: http://www.healthcare.gov/immigrants/lawfully-present-immigrants. Accessed November 16, 2015.
- 25.Pascale J, Boudreaux M, King R. Understanding the new Current Population Survey health insurance questions. Health Serv Res. 2016;51(1):240–261. doi: 10.1111/1475-6773.12312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.O’Hara B, Medalia C. CPS and ACS health insurance estimates: consistent trends from 2009-2012. September 15, 2014. Available at: http://www.census.gov/hhes/www/hlthins/data/incpovhlth/2013/CPS_ACS_Trends.pdf. Accessed October 24, 2015.
- 27.Davern M, Quinn BC, Kenney GM, Blewett LA. The American Community Survey and health insurance coverage estimates: possibilities and challenges for health policy researchers. Health Serv Res. 2009;44(2 pt 1):593–605. doi: 10.1111/j.1475-6773.2008.00921.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 29.Lê Cook B, McGuire TG, Zaslavsky AM. Measuring racial/ethnic disparities in health care: methods and practical issues. Health Serv Res. 2012;47(3 pt 2):1232–1254. doi: 10.1111/j.1475-6773.2012.01387.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aizer A. Low take-up in Medicaid: does outreach matter and for whom? Am Econ Rev. 2003;93(2):238–241. [Google Scholar]
- 31.Aizer A. Public health insurance, program take-up, and child health. Rev Econ Stat. 2007;89(3):400–415. [Google Scholar]
- 32.Karlamangla S. Will nation follow California on healthcare for immigrants here illegally? Los Angeles Times. October 2, 2015. Available at: http://www.latimes.com/local/politics/la-me-immigrant-health-analysis-20151002-story.html. Accessed January 22, 2016. [Google Scholar]
- 33.Mason M. Brown OKs bill implementing state-paid healthcare for kids in U.S. illegally. Los Angeles Times. October 9, 2015. Available at: http://www.latimes.com/local/political/la-me-pc-california-immigrant-healthcare-20151009-story.html. Accessed January 22, 2016. [Google Scholar]
- 34.McConville S, Hill L, Ugo I, Hayes J. Health coverage and care for undocumented immigrants. November 2015. Available at: http://ppic.org/main/publication_quick.asp?i=1167. Accessed January 22, 2016.
- 35.Smith JC, Medalia C US Census Bureau. Health Insurance Coverage in the United States: 2014. Washington, DC: US Government Printing Office; 2015; Current Population Reports, P60-253. Available at: http://www.census.gov/content/dam/Census/library/publications/2015/demo/p60-253.pdf. Accessed November 16, 2015. [Google Scholar]