Abstract
Objectives. To describe mortality among adults with intellectual disability in England in comparison with the general population.
Methods. We conducted a cohort study from 2009 to 2013 using data from 343 general practices. Adults with intellectual disability (n = 16 666; 656 deaths) were compared with age-, gender-, and practice-matched controls (n = 113 562; 1358 deaths).
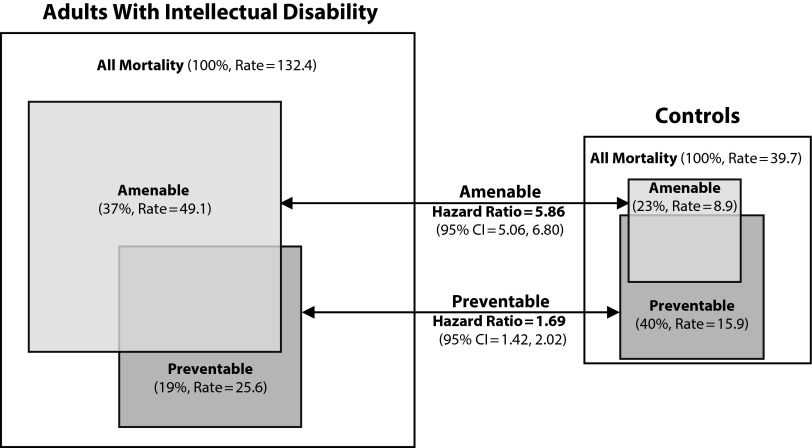
Results. Adults with intellectual disability had higher mortality rates than controls (hazard ratio [HR] = 3.6; 95% confidence interval [CI] = 3.3, 3.9). This risk remained high after adjustment for comorbidity, smoking, and deprivation (HR = 3.1; 95% CI = 2.7, 3.4); it was even higher among adults with intellectual disability and Down syndrome or epilepsy. A total of 37.0% of all deaths among adults with intellectual disability were classified as being amenable to health care intervention, compared with 22.5% in the general population (HR = 5.9; 95% CI = 5.1, 6.8).
Conclusions. Mortality among adults with intellectual disability is markedly elevated in comparison with the general population, with more than a third of deaths potentially amenable to health care interventions. This mortality disparity suggests the need to improve access to, and quality of, health care among people with intellectual disability.
People with intellectual disability experience poorer physical health and receive poorer quality health care than people without intellectual disability for a range of reasons, including discrimination.1 These inequalities are a concern for health care systems in the United Kingdom, the United States, and other developed countries, where the prevalence of intellectual disability has been estimated at approximately 1%.2 Studies have reported that people with intellectual disability experience high mortality rates, shorter life expectancies, and excess premature mortality, with variable estimates of increased risk of death ranging between 3 and 18 times higher than those of the general population.3–6 A national confidential inquiry into premature deaths among people with intellectual disability in the United Kingdom highlighted the potential to prevent premature mortality,7 concluding that people with intellectual disability die on average 16 years earlier than the general population and that potentially modifiable poor care and service provision contributes to this mortality gap.
The lack of reliable information on the health experience of people with intellectual disability has been identified as an important barrier to developing effective health care strategies for this group.8 According to the US Public Health Service, it has been unable to report on the health status of individuals with intellectual disability, one of its most vulnerable populations, on a truly representational basis.9 In other populations, an understanding of mortality patterns, especially cause-specific and potentially avoidable mortality, has been a driver in developing priorities for health care interventions and monitoring the effectiveness of health services.
Unfortunately, as a result of incomplete recording of intellectual disability on death certificates and difficulties in relating death certificate data to a particular population at risk, studies based on death certification data alone are inadequate for understanding the mortality experience of people with intellectual disability.10 Other studies are often based on local registers and may not be representative,3 or they may be based on smaller samples with long follow-ups and may therefore no longer be contemporary.5 Linkages between data sources that record mortality and those that identify people with intellectual disability have the potential to yield accurate evidence on health and mortality disparities.8
We used a large English primary care database, linked to death certification data, to describe mortality rates between 2009 and 2013 in a group of adults with intellectual disability and to compare these rates with those found in the general population. We assessed all-cause mortality, cause-specific mortality, and mortality considered potentially avoidable through medical intervention.
METHODS
We derived our data from the Clinical Practice Research Datalink, a large, validated primary care database that has been shown to be representative of the UK population,11 98% of whom are registered with a general (family) practitioner. In our analyses, we included 343 English practices that were recording data on January 1, 2009, and were anonymously linked to Office of National Statistics (ONS) death registration data.
Identification of Patients With Intellectual Disability
In England, people with intellectual disability live almost exclusively in the community, either in private households or in communal or shared settings. Since 2006, doctors have been financially incentivized to electronically maintain a register of all adults with intellectual disability in their practice.12 We used nationally agreed-upon codes for intellectual disability, along with a few additional codes for chromosomal and metabolic disorders usually associated with intellectual disability, to identify patients.13 Our sample comprised 16 666 patients, 18 to 84 years of age, who were registered for more than 30 days between 2009 and 2013.
We identified some important subgroups that could be easily identified from primary care records: Down syndrome patients, patients with epilepsy in addition to intellectual disability, intellectual disability patients with autistic spectrum disorder, intellectual disability patients with high levels of support needs, and intellectual disability patients living in a communal or shared setting. We classified patients as having high levels of support needs if they had a record of severe or profound intellectual disability or, in cases in which no record of severity was available (59%), they had at least 2 of the following: cerebral palsy or significant mobility problems (e.g., wheelchair use), severe visual impairment, severe hearing impairment, epilepsy (excluding absence seizures), continence problems, and percutaneous endoscopic gastrostomy feeding. We assessed communal living arrangements by searching for specific codes or the presence of 3 or more people with intellectual disability with the same address flag, indicating that they were living at the same address.
Study Design
Our study involved a retrospective matched cohort design. Adults with intellectual disability were followed from the latest date available of the following: January 1, 2009; January 1 of the year of their 18th birthday; or their date of registration. They were followed until the earliest date of recording of death, deregistration from practice, or when the practice stopped providing data to the Clinical Practice Research Datalink (up to March 31, 2013). We compared them with up to 7 age-, gender-, and practice-matched individuals with no record of intellectual disability (control group; n = 113 562) who were registered at the beginning of the study period. The average length of follow-up for all patients in our cohort was approximately 3 years (1097 days).
Cause of Death
We derived information on underlying cause of death from ONS death registration data for patients who died during the study (656 adults with intellectual disability, 1358 control group members). In the case of 38 of these deaths, we were unable to obtain data on cause of death. We summarized main causes of death using chapter headings from the International Classification of Diseases, 10th Revision,14 but also explored some subgroups of interest. When examining how often intellectual disability was recorded on death certificates, we searched all recorded main and contributory causes of death for intellectual disability–associated codes, including an extended range of conditions weakly associated with intellectual disability such as cerebral palsy.10
Potentially Avoidable Deaths and Mortality Amenable to Care
In the United Kingdom, the ONS has defined indicators of potentially avoidable mortality to assess whether prior intervention for the underlying cause of death would reduce mortality for certain conditions.15 The ONS defines deaths as potentially avoidable (according to underlying cause of death) when there is scope for intervention to reduce mortality.15 Potentially avoidable deaths are further classified as amenable to good-quality health care (treatable), preventable through public health action, or both. With the exception of accidental deaths, these definitions primarily include deaths occurring among individuals younger than 75 years. For example, deaths from breast cancer are identified as amenable to health care, through screening and treatment, and deaths from lung cancer are identified as preventable, through tobacco control. Because some causes of death are defined as both amenable and preventable (e.g., ischemic heart disease), the number of deaths that are potentially avoidable is lower than the combined number of deaths that are amenable and preventable.
Adjustment for Comorbidities and Other Factors
We present unadjusted and adjusted comparisons. However our unadjusted analyses already adjusted for differences in our matched factors: age, gender, and practice (including regional and urban–rural variations). In addition, we adjusted comparisons between adults with intellectual disability and control group members using 9 comorbid conditions that are independent predictors of mortality in the general population16: atrial fibrillation, cancer, chronic obstructive pulmonary disease, dementia, diabetes, epilepsy, heart failure, severe mental illness (psychosis, schizophrenia, bipolar affective disorder), and stroke. English general practices are encouraged to use nationally agreed-upon codes12 to record these conditions, and we identified these codes in patients’ records before their study entry date. We favored this approach over the Charlson index, which does not account for epilepsy or severe mental illness, both of which are much more common among adults with intellectual disability.13
Other covariates of interest were smoking and socioeconomic status. In computing the latter, we used the Index of Multiple Deprivation,17 a composite small-area ecological measure of deprivation based on postcodes. A summary of comorbidity, smoking, and deprivation data among adults with intellectual disability and controls is provided in Table A, available as a supplement to the online version of this article at http://www.ajph.org.
Statistical Analysis
We present crude death rates and hazard ratios (HRs) for comparisons between adults with intellectual disability and matched controls. Hazard ratios were calculated via Cox regression (SAS version 9.4; SAS Institute Inc, Cary, NC), with further adjustment for covariates (on a multiplicative scale) and stratification on matched sets (i.e., matched according to gender, age, and practice). For subgroup comparisons, we compared the hazard ratios and confidence intervals derived from each intellectual disability versus control comparison (e.g., adults with intellectual disability and Down syndrome vs controls) and calculated P values for between-group differences. In supplementary analyses focusing only on intellectual disability patients, we fit models that directly compared each subgroup category (e.g., those with vs without Down syndrome), adjusted for age and gender differences and stratified according to practice.
RESULTS
A total of 656 (3.9%) adults with intellectual disability died over the study period, compared with 1358 (1.2%) of the matched controls (Table 1). In the intellectual disability group, death rates were elevated among those with Down syndrome (6.6%), a high number of support needs (5.9%), and epilepsy (5.8%) and among those living in communal or shared arrangements (7.8%).
TABLE 1—
Characteristics of and Numbers of Deaths in the Intellectual Disability and Matched Control Groups: Selected UK General Practices, 2009–2013
| Intellectual Disability Group |
Control Group |
||||
| Characteristic of Intellectual Disability Adult | Mean Age, y (SD) | No. | Deaths, No. (%) | No. | Deaths, No. (%) |
| Total | 39.9 (16.2) | 16 666 | 656 (3.94) | 113 562 | 1 358 (1.20) |
| Gender | |||||
| Male | 41.3 (16.4) | 6 989 | 291 (4.16) | 47 587 | 538 (1.13) |
| Female | 38.8 (15.9) | 9 677 | 365 (3.77) | 65 975 | 820 (1.24) |
| Age, y | |||||
| 18–34 | 24.2 (5.1) | 6 981 | 48 (0.69) | 46 939 | 69 (0.15) |
| 35–54 | 44.2 (5.4) | 6 283 | 167 (2.66) | 43 123 | 276 (0.64) |
| ≥ 55 | 64.0 (7.1) | 3 402 | 441 (12.96) | 23 500 | 1 013 (4.31) |
| Down syndrome | |||||
| Yes | 39.1 (14.4) | 1 793 | 118 (6.58) | 12 226 | 92 (0.75) |
| No | 40.0 (16.4) | 14 873 | 538 (3.62) | 101 336 | 1 266 (1.25) |
| High level of support needsa | |||||
| Yes | 41.4 (16.4) | 3 263 | 194 (5.94) | 22 298 | 302 (1.35) |
| No | 39.5 (16.1) | 13 403 | 462 (3.45) | 91 264 | 1 056 (1.16) |
| Communal/shared accommodations | |||||
| Yes | 47.2 (15.7) | 3 392 | 265 (7.81) | 23 117 | 416 (1.80) |
| No | 38.0 (15.8) | 13 274 | 391 (2.90) | 90 445 | 942 (1.04) |
| Autism spectrum disorder | |||||
| Yes | 30.5 (13.3) | 1 532 | 15 (0.98) | 10 374 | 44 (0.42) |
| No | 40.8 (16.1) | 15 134 | 641 (4.24) | 103 188 | 1 314 (1.27) |
| Epilepsy | |||||
| Yes | 41.0 (15.3) | 2 884 | 167 (5.79) | 19 705 | 205 (1.04) |
| No | 39.6 (16.3) | 13 782 | 489 (3.55) | 93 857 | 1 153 (1.23) |
| Any subgroup categorizationb | |||||
| Yes | 40.6 (16.4) | 8 541 | 446 (5.22) | 58 194 | 703 (1.21) |
| No | 39.1 (16.0) | 8 125 | 210 (2.58) | 55 368 | 655 (1.18) |
Classified by a general practitioner as having severe or profound intellectual disability or has ≥ 2 of the following: epilepsy, cerebral palsy or significant mobility problem (wheelchair use or greater), severe visual impairment, severe hearing impairment, continence problem, or use of percutaneous endoscopic gastrostomy feeding.
Down syndrome, high level of support needs, communal/shared accommodations, autism, or epilepsy.
All-Cause Mortality
The crude mortality rate was 132.4 per 10 000 people per year among adults with intellectual disability, compared with 39.7 among controls (Table 2). The resulting hazard ratio (3.62; 95% confidence interval [CI] = 3.33, 3.93) was only partially explained by differences between the groups in comorbidities, smoking, and deprivation (adjusted HR = 3.05; 95% CI = 2.73, 3.41). The higher mortality risk among adults with intellectual disability was seen at all ages, and although it was higher among men than it was among women, the difference was not statistically significant after adjustment (P = .07).
TABLE 2—
All-Cause Mortality Crude Rates and Hazard Ratios for the Intellectual Disability and Matched Control Groups: Selected UK General Practices, 2009–2013
| Mortality Rate |
Unadjusted Model |
Adjusted Modela |
||||
| Characteristic of Intellectual Disability Adult | Intellectual Disability Group (n = 16 666) | Control Group (n = 113 562) | HR (95% CI) | Pb | HR (95% CI) | Pb |
| Total | 132.4 | 39.7 | 3.62 (3.33, 3.93) | 3.05 (2.73, 3.41) | ||
| Gender | .01 | .07 | ||||
| Male | 139.5 | 37.5 | 4.10 (3.61, 4.66) | 3.50 (2.94, 4.16) | ||
| Female | 127.3 | 41.5 | 3.30 (2.96, 3.68) | 2.81 (2.43, 3.24) | ||
| Age, y | ||||||
| 18–34 | 25.3 | 5.6 | 4.29 (3.13, 5.88) | 2.43 (1.56, 3.77) | ||
| 35–54 | 83.1 | 19.6 | 4.17 (3.52, 4.92) | .88 | 3.22 (2.53, 4.08) | .25 |
| ≥55 | 420.0 | 129.6 | 3.39 (3.07, 3.75) | .21 | 3.03 (2.65, 3.46) | .32 |
| Down syndrome | < .001 | < .001 | ||||
| Yes | 220.0 | 24.9 | 9.21 (7.22, 11.76) | 10.39 (7.13, 15.13) | ||
| No | 121.8 | 41.6 | 3.19 (2.92, 3.49) | 2.66 (2.36, 3.00) | ||
| High level of support needsc | < .001 | .001 | ||||
| Yes | 190.2 | 43.9 | 4.77 (4.08, 5.59) | 4.95 (4.03, 6.07) | ||
| No | 117.4 | 38.7 | 3.28 (2.98, 3.62) | 3.15 (2.79, 3.55) | ||
| Communal/shared accommodations | < .001 | < .001 | ||||
| Yes | 254.7 | 56.5 | 4.99 (4.36, 5.73) | 4.30 (3.52, 5.26) | ||
| No | 99.9 | 35.1 | 3.05 (2.74, 3.39) | 2.64 (2.30, 3.02) | ||
| Autism spectrum disorder | .05 | .40 | ||||
| Yes | 36.3 | 16.0 | 2.39 (1.45, 3.96) | 2.22 (1.01, 4.86) | ||
| No | 141.2 | 41.8 | 3.66 (3.37, 3.98) | 3.07 (2.74, 3.43) | ||
| Epilepsy | < .001 | < .001 | ||||
| Yes | 188.0 | 33.7 | 6.04 (5.04, 7.24) | 7.76 (6.10, 9.86) | ||
| No | 120.3 | 41.0 | 3.18 (2.90, 3.50) | 2.91 (2.60, 3.27) | ||
| Any subgroup categorizationd | < .001 | < .001 | ||||
| Yes | 173.8 | 39.8 | 4.85 (4.36, 5.38) | 4.27 (3.64, 5.01) | ||
| No | 87.9 | 39.6 | 2.35 (2.04, 2.70) | 2.12 (1.79, 2.51) | ||
Note. CI = confidence interval; HR = hazard ratio. Rates are per 10 000 people per year.
Adjusted for 9 comorbidities (atrial fibrillation, cancer, chronic obstructive pulmonary disease, dementia, diabetes, epilepsy, heart failure, severe mental illness, and stroke), deprivation, and smoking status with the exception of the subgroup analyses focusing on epilepsy and high number of support needs, in which epilepsy was not included in the adjustment.
For differences between subgroups (for age, 18–34 years was the baseline group).
Classified by a general practitioner as having severe or profound intellectual disability or has ≥ 2 of the following: epilepsy, cerebral palsy or significant mobility problem (wheelchair use or greater), severe visual impairment, severe hearing impairment, continence problem, or use of percutaneous endoscopic gastrostomy feeding.
Down syndrome, high level of support needs, communal/shared accommodations, autism, or epilepsy.
Among adults with intellectual disability, those with Down syndrome had a very high relative risk of death in comparison with controls (HR = 9.21; 95% CI = 7.22, 11.76), and this risk was significantly different from that seen among those in the intellectual disability group without Down syndrome (P < .001) and was not explained by further adjustment. Similarly, intellectual disability patients with high levels of support needs had a death rate nearly 5 times higher than that of controls, and the rate among those in communal or shared living arrangements was more than 4 times higher; both rates were significantly different from the comparable rates among other adults in the intellectual disability group before as well as after adjustment (P < .01). Epilepsy within the intellectual disability population was a strong determinant of mortality risk, both relative to the control group (HR = 6.04; 95% CI = 5.04, 7.24) and relative to other adults in the intellectual disability group without epilepsy (P < .001). Additional (unmatched) analyses that directly compared adults with intellectual disability in each subgroup (Table B, available as a supplement to the online version of this article at http://www.ajph.org) confirmed the findings shown in Table 2.
Cause-Specific Mortality
The higher mortality risk among adults with intellectual disability produced different patterns of cause-specific mortality, with the most common main causes of mortality being circulatory diseases (21.6%), respiratory diseases (18.8%), neoplasms (14.9%), and nervous system diseases (11.6%). The pattern among controls was different, with neoplasms (37.4%), circulatory diseases (26.5%), respiratory diseases (9.9%), and external causes (7.4%) being most common.
The cause-specific death rate was higher among adults with intellectual disability than it was among controls for all main causes (Table 3). However, suicides and traffic accidents (a subgroup of external causes) were more common among controls. Hazard ratios for main causes of death showed that the greatest relative increases were for diseases of the genitourinary system, including urinary tract infections (HR = 10.89; 95% CI = 6.09, 19.47), and nervous system disorders, including epilepsy (HR = 13.79; 95% CI = 9.70, 19.62). Other common causes of death (e.g., circulatory, digestive, respiratory diseases) all had hazard ratios between 3 and 7. Notable disparities within the respiratory death category included pneumonia and aspiration pneumonia, for which death rates among adults with intellectual disability were more than 10 times higher than were rates among controls.
TABLE 3—
Cause-Specific Death Rates for the Intellectual Disability and Matched Control Groups: Selected UK General Practices, 2009–2013
| Intellectual Disability Group (n = 16 666) |
Control Group (n = 113 562) |
||||
| Cause of Death | No. | Rate | No. | Rate | HR (95% CI) |
| Diseases of the circulatory systema | 142 | 28.7 | 360 | 10.5 | 3.05 (2.56, 3.64) |
| Neoplasms | 98 | 19.8 | 508 | 14.9 | 1.44 (1.18, 1.76) |
| Diseases of the respiratory systemb | 123 | 24.8 | 135 | 3.9 | 6.68 (5.38, 8.29) |
| Diseases of the digestive system | 46 | 9.3 | 87 | 2.5 | 4.02 (2.92, 5.54) |
| Diseases of the genitourinary system | 23 | 4.6 | 15 | 0.4 | 10.89 (6.09, 9.47) |
| Mental and behavioral disorders | 35 | 7.1 | 31 | 0.9 | 7.99 (5.19, 12.31) |
| Diseases of the nervous systemc | 76 | 15.3 | 39 | 1.1 | 13.79 (9.70, 19.62) |
| External causesd | 27 | 5.5 | 101 | 3.0 | 1.85 (1.26, 2.71) |
| Endocrine, nutritional, and metabolic diseases | 13 | 2.6 | 16 | 0.5 | 5.38 (2.79, 10.07) |
| Infectious and parasitic disorders | 3 | 0.6 | 14 | 0.4 | 2.30 (0.70, 7.48) |
| Diseases of the musculoskeletal system | 6 | 1.2 | 8 | 0.2 | 5.50 (2.22, 13.61) |
| Congenital/chromosomal abnormalities | 45 | 9.1 | 2 | 0.1 | . . .e |
| Other (skin/blood diseases, residual codes) | 10 | 2.0 | 13 | 0.4 | 5.03 (2.40, 10.54) |
| Not available | 9 | 1.8 | 29 | 0.8 | 2.27 (1.19, 4.43) |
| Total | 656 | 132.4 | 1358 | 39.7 | 3.62 (3.33, 3.93) |
Note. CI = confidence interval; HR = hazard ratio. Rates are per 10 000 people per year. Unadjusted hazard ratios are shown for common broad causes of mortality among adults with intellectual disability with the exception of congenital/chromosomal abnormalities, for which a hazard ratio would not be informative.
Source. We summarized main causes of death using chapter headings from the International Classification of Diseases, 10th Revision.14
Notable subgroups: cerebrovascular disease (intellectual disability group, n = 34, rate = 6.9; control group, n = 57, rate = 1.7) and ischemic heart diseases (intellectual disability group, n = 62, rate = 12.5; control group, n = 188, rate = 5.5).
Notable subgroups: pneumonia (intellectual disability group, n = 67, rate = 13.5; control group, n = 39, rate = 1.1) and aspiration pneumonitis (intellectual disability group, n = 21, rate = 4.2; control group, n = 6, rate = 0.2).
Notable subgroup: epilepsy (intellectual disability group, n = 29, rate = 5.9; control group, n = 3, rate = 0.1).
Notable subgroups: accidental poisoning (intellectual disability group, n = 3, rate = 0.6; control group, n = 13, rate = 0.4), intentional or undetermined (intellectual disability group, n = 4, rate = 0.8; control group, n = 49, rate = 1.4), traffic accident (intellectual disability group, n = 1, rate = 0.2; control group, n = 20, rate = 0.6), and other accident (intellectual disability group, n = 17, rate = 3.4; control group, n = 15, rate = 0.4).
Hazard ratio could not reliably be estimated.
The most common underlying cause of death among adults with Down syndrome was respiratory diseases (n = 24; 20.3%). However, Down syndrome (or another chromosomal abnormality) was listed as the underlying cause in 30 deaths, and in 26 of these cases respiratory disease was listed as a secondary cause. If respiratory diseases had instead been classified as the underlying cause in these 26 deaths, the percentage of Down syndrome deaths caused by respiratory diseases would have increased to 42.4%.
Potentially Avoidable Mortality Amenable to Health Care
The percentage of all deaths classified as potentially avoidable (amenable to care or preventable) was similar among adults with intellectual disability (46.3%) and controls (47.5%). However, the percentages of deaths amenable to care and preventable were very different between the 2 groups (Figure 1), with a higher percentage of deaths amenable to care observed among intellectual disability adults (37.0%, compared with 22.5% among controls). This difference was reflected in the hazard ratio for deaths amenable to care (HR = 5.86; 95% CI = 5.06, 6.80) in contrast to preventable deaths (HR = 1.69; 95% CI = 1.42, 2.02). In addition, standard ONS definitions do not include a number of causes of deaths among people with intellectual disability that might be considered amenable to care, such as deaths from urinary tract infections (n = 12; 1.8%) and aspiration pneumonitis (n = 21; 3.2%).
FIGURE 1—
Percentages of Deaths in the Intellectual Disability and Matched Control Groups Categorized as Amenable and Preventable: Selected UK General Practices, 2009–2013
Note. CI = confidence interval. Sizes of squares correspond to both rates and percentages of overall mortality; rates are per 10 000 people per year. Overall avoidable mortality is the total shaded area covered by the amenable and preventable squares, with the overlap area being counted only once: intellectual disability rate = 61.4 (46.3% of all mortality), control rate = 18.9 (47.5%), and hazard ratio = 3.44 (95% CI = 3.05, 3.89).
Recording of Intellectual Disability on Death Certificates
In 456 (69.5%) deaths among adults with intellectual disability, there was no mention of intellectual disability or a related condition as either a main or contributory cause of death. In the remaining 200 cases that had a recorded cause associated with intellectual disability, the most common causes listed were Down syndrome (n = 88), cerebral palsy (n = 39), and developmental disorder of scholastic skills (n = 50).
DISCUSSION
We have confirmed and quantified a 3 to 4 times higher risk of death among adults with intellectual disability than we confirmed among the general population, and this risk is seen across all common causes of death and is not explained by the higher frequency of comorbid conditions in the intellectual disability group. Furthermore, our results show that adults with epilepsy or Down syndrome experience markedly higher mortality than other people with intellectual disability. Although potentially avoidable deaths accounted for a similar proportion of deaths among adults with intellectual disability and the general population, there was a notable discrepancy in deaths amenable to health care, with the rate of such deaths being almost 6 times higher among adults with intellectual disability than they were in the general population.
Context
A number of data sources have been used in studies of mortality among people with intellectual disability, including local registers, death certification data alone, and national registers.18 Our finding of an increased overall risk of death among people with intellectual disability is consistent with the results of most studies. The largest existing UK study, an investigation based on a follow-up of a regional disease register in Leicestershire, reported a similar increased risk of death.3,19 Our finding that fewer than a third of death certificates recorded intellectual disability as a secondary cause of death emphasizes the limitations of studies based on death certificates alone.
Overall, our description of cause-specific mortality is similar to those in other cohorts; however, an increased risk of cancer death has not been consistently described, with some studies suggesting a similar19 or lower risk of cancer death.5 Our findings may represent an important change resulting from an aging population of people with intellectual disability. Other studies have reported increased mortality rates among people with intellectual disability and epilepsy,10 with a particular concern over the contribution of sudden unexpected death associated with epilepsy.20,21
Mortality among people with Down syndrome has been more widely studied.22–25 The findings from these investigations are consistent with the high risk of death we found among people with Down syndrome. For example, researchers in a large Danish population study concluded that people with standard trisomy 21 had a mortality hazard ratio of 8.9,24 and a smaller American study showed that community-residing adults with Down syndrome were almost 4 times as likely to die as adults with other types of intellectual disability.25
The UK confidential inquiry mentioned earlier reported a high proportion of deaths amenable to health care intervention, but the study researchers were able to compare this proportion only with the national average; they were unable to quantify absolute and relative risks.7 Our study extends this work and provides quantitative estimates of these risks among people with intellectual disability. However, it should be noted that existing definitions of amenable mortality do not include some important treatable causes of deaths among people with intellectual disability, including urinary tract infections and aspiration, and thus are likely to underestimate the true burden of amenable mortality.
Strengths and Limitations
The main strength of our study is the inclusion of a large unselected population of adults with known intellectual disability and the fact that we were able to compare their experience with age- and gender-matched individuals from the same general practice. Our use of both primary care and death registration data is a crucial step in addressing an acknowledged lack of population-based comparative studies of mortality among people with intellectual disability.8 This linkage allows for better ascertainment of adults with intellectual disability as well as control and stratification by factors not available in death registration data such as those focusing on comorbidity and smoking. Within-practice matching overcomes concerns regarding geographical differences in health care access or quality and inconsistencies in clinical recording between practices.
The main limitation of our study is the potential for incomplete and inaccurate recording in primary care and death certification data. In England, doctors have been encouraged to electronically maintain a register of all adults with intellectual disability,12 so although it is reasonable to assume that most patients with severe intellectual disability will be identified, some milder cases may be missed. This may result in an overestimation of the mortality risk in the intellectual disability population as a whole, but we still found a doubling of risk when we restricted our analyses to patients with no significant impairments recorded. Recording of intellectual disability severity itself was less complete; however, we created a composite measure incorporating other relevant information in the patient record (including, if available, severe or profound classifications), although the consistency of recording of some of these factors may vary across practices.
Many patients with Down syndrome had this condition recorded as the underlying cause of death, with respiratory disease as a secondary cause. Although it could be argued that respiratory disease was the more appropriate underlying cause of death, in this scenario either cause would still be classified as amenable to care and, hence, avoidable. However, it may be that some causes of death are less avoidable among adults with intellectual disability because of the underlying cause of the intellectual disability itself. For example, the immune defects observed among people with Down syndrome may lead to infections being more common and less amenable to treatment.26
Implications and Conclusions
Mortality data are essential in identifying priorities for local, national, and global health strategies. Understanding mortality among people with intellectual disability is important in ensuring that interventions are appropriately targeted to this group’s specific health needs. Our work contributes to this aim by quantifying mortality disparities between adults with intellectual disability and the general population.
The consistently higher mortality risk among adults with intellectual disability was seen at all ages and was not explained by their higher levels of comorbidity.13 Although some conditions may be underdiagnosed or underreported,27 our results suggest that underlying differences in functional status are more pertinent, highlighting the overall greater health care needs of people with intellectual disability. Consistent guidance on recording of intellectual disability as a contributory but not underlying cause on death certificates would be helpful for ongoing surveillance of the health of people with intellectual disability in all countries.28
Although many of the leading causes of death among adults with intellectual disability are similar to those found in the general population, there are important differences. One is the higher burden of respiratory deaths, which is important given that national strategies in developed countries assign a lower priority to respiratory health. The large contributions of pneumonia and aspiration are particularly important as a potential focus for improving health care among people with intellectual disability. The large contributions of urinary and neurological causes of death highlight further potential opportunities to improve care for people with intellectual disability through better management of urinary tract infections and optimization of seizure control.
Our most important finding is that more than a third of deaths among adults with intellectual disability were amenable to health care, with these deaths driving the overall higher risk of potentially avoidable deaths. The difference in the relative contribution of preventable and amenable deaths to avoidable mortality among people with intellectual disability and the general population may be partly explained by differences in lifestyle exposures, in particular tobacco and alcohol use. Adherence to current medical guidelines may also differ owing to difficulties encountered in communicating with patients with intellectual disability.27 However, the high absolute risk of deaths amenable to health care intervention reflects established concerns regarding difficulty accessing health care, delays in diagnosis, and poorer management experienced by people with intellectual disability.1,7
Our findings emphasize that strategies for improving health among people with intellectual disability need to prioritize access to and quality of health care as well as preventive interventions. Existing population-wide strategies for working-age adults in high-income countries focus on cardiovascular risk and lifestyle factors, which, although important for people with intellectual disability, do not address their different health care needs. Confronting the health and mortality disparities experienced by people with intellectual disability is a key challenge for health care systems and a potentially important indicator of their equity and effectiveness.
ACKNOWLEDGMENTS
This project was funded by the Health Services and Delivery Research Programme of the National Institute for Health Research (project number 12/64/154).
Sunil M. Shah died prior to the publication of this article. His coauthors would like to pay tribute to him as the principal investigator for this study, which he led from inception.
We thank the members of ResearchNet, a service user network for people with intellectual disability, and the Merton Carers Partnership Group, a group of family caregivers for adults with intellectual disability, for their support of and advice on this project.
Note. The views and opinions expressed are those of the authors and do not necessarily reflect those of the Health Services and Delivery Research Programme, the National Institute for Health Research, the English National Health Service, or the English Department of Health.
HUMAN PARTICIPANT PROTECTION
This study was approved by the United Kingdom Independent Scientific Advisory Committee, which evaluates protocols using Clinical Practice Research Datalink data.
REFERENCES
- 1.Michael J. Healthcare for all: report of the independent inquiry into access to healthcare for people with learning disabilities. Available at: http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_099255. Accessed April 28, 2016.
- 2.Maulik PK, Mascarenhas MN, Mathers CD, Dua T, Saxena S. Prevalence of intellectual disability: a meta-analysis of population-based studies. Res Dev Disabil. 2011;32(2):419–436. doi: 10.1016/j.ridd.2010.12.018. [DOI] [PubMed] [Google Scholar]
- 3.Tyrer F, Smith LK, McGrother CW. Mortality in adults with moderate to profound intellectual disability: a population-based study. J Intellect Disabil Res. 2007;51(7):520–527. doi: 10.1111/j.1365-2788.2006.00918.x. [DOI] [PubMed] [Google Scholar]
- 4.Hollins S, Attard MT, von Fraunhofer N, McGuigan S, Sedgwick P. Mortality in people with learning disability: risks, causes, and death certification findings in London. Dev Med Child Neurol. 1998;40(1):50–56. [PubMed] [Google Scholar]
- 5.Patja K, Molsa P, Iivanainen M. Cause-specific mortality of people with intellectual disability in a population-based, 35-year follow-up study. J Intellect Disabil Res. 2001;45(1):30–40. doi: 10.1046/j.1365-2788.2001.00290.x. [DOI] [PubMed] [Google Scholar]
- 6.Lavin KE, McGuire BE, Hogan MJ. Age at death of people with an intellectual disability in Ireland. J Intellect Disabil. 2006;10(2):155–164. doi: 10.1177/1744629506064011. [DOI] [PubMed] [Google Scholar]
- 7.Heslop P, Blair PS, Fleming P, Hoghton M, Marriott A, Russ L. The Confidential Inquiry into premature deaths of people with intellectual disabilities in the UK: a population-based study. Lancet. 2014;383(9920):889–895. doi: 10.1016/S0140-6736(13)62026-7. [DOI] [PubMed] [Google Scholar]
- 8.Heslop P, Lauer E, Hoghton M. Mortality in people with intellectual disabilities. J Appl Res Intellect Disabil. 2015;28(5):367–372. doi: 10.1111/jar.12196. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. US surveillance of health of people with intellectual disability. Available at: http://www.cdc.gov/ncbddd/disabilityandhealth/pdf/209537-A_IDmeeting%20short%20version12-14-09.pdf. Accessed April 28, 2016.
- 10.Glover GA, Ayub M. How people with learning disabilities die. Available at: http://www.improvinghealthandlives.org.uk/uploads/doc/vid_9033_IHAL2010-06%20Mortality.pdf. Accessed April 28, 2016.
- 11.Herrett E, Gallagher AM, Bhaskaran K et al. Data resource profile: Clinical Practice Research Datalink (CPRD) Int J Epidemiol. 2015;44(3):827–836. doi: 10.1093/ije/dyv098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.NHS Employers. General medical services contract. Available at: http://www.nhsemployers.org/your-workforce/primary-care-contacts/general-medical-services/quality-and-outcomes-framework. Accessed April 28 2016.
- 13.Carey IM, Shah SM, Hosking FJ et al. Health characteristics and consultation patterns of people with intellectual disability: a cross-sectional database study in English general practice. Br J Gen Pract. 2016;66(645):e264–e270. doi: 10.3399/bjgp16X684301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.International Classification of Diseases, 10th Revision. Geneva, Switzerland: World Health Organization; 1992. [Google Scholar]
- 15.Office for National Statistics. Definition of avoidable mortality. Available at: http://www.ons.gov.uk/ons/about-ons/get-involved/consultations/archived-consultations/2011/definitions-of-avoidable-mortality/definition-of-avoidable-mortality.pdf. Accessed April 28, 2016.
- 16.Carey IM, Shah SM, Harris T, DeWilde S, Cook DG. A new simple primary care morbidity score predicted mortality and better explains between practice variations than the Charlson index. J Clin Epidemiol. 2013;66(4):436–444. doi: 10.1016/j.jclinepi.2012.10.012. [DOI] [PubMed] [Google Scholar]
- 17.Department for Communities and Local Government. English indices of deprivation 2010. Available at: https://www.gov.uk/government/statistics/english-indices-of-deprivation-2010. Accessed April 28, 2016.
- 18.Heslop P, Glover G. Mortality of people with intellectual disabilities in England: a comparison of data from existing sources. J Appl Res Intellect Disabil. 2015;28(5):414–422. doi: 10.1111/jar.12192. [DOI] [PubMed] [Google Scholar]
- 19.Tyrer F, McGrother C. Cause-specific mortality and death certificate reporting in adults with moderate to profound intellectual disability. J Intellect Disabil Res. 2009;53(11):898–904. doi: 10.1111/j.1365-2788.2009.01201.x. [DOI] [PubMed] [Google Scholar]
- 20.Kiani R, Tyrer F, Jesu A et al. Mortality from sudden unexpected death in epilepsy (SUDEP) in a cohort of adults with intellectual disability. J Intellect Disabil Res. 2014;58(6):508–520. doi: 10.1111/jir.12047. [DOI] [PubMed] [Google Scholar]
- 21.Young C, Shankar R, Palmer J et al. Does intellectual disability increase sudden unexpected death in epilepsy (SUDEP) risk? Seizure. 2015;25:112–116. doi: 10.1016/j.seizure.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 22.Hill DA, Gridley G, Cnattingius S et al. Mortality and cancer incidence among individuals with Down syndrome. Arch Intern Med. 2003;163(6):705–711. doi: 10.1001/archinte.163.6.705. [DOI] [PubMed] [Google Scholar]
- 23.Yang Q, Rasmussen SA, Friedman JM. Mortality associated with Down’s syndrome in the USA from 1983 to 1997: a population-based study. Lancet. 2002;359(9311):1019–1025. doi: 10.1016/s0140-6736(02)08092-3. [DOI] [PubMed] [Google Scholar]
- 24.Zhu JL, Hasle H, Correa A et al. Survival among people with Down syndrome: a nationwide population-based study in Denmark. Genet Med. 2013;15(1):64–69. doi: 10.1038/gim.2012.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Esbensen AJ, Seltzer MM, Greenberg JS. Factors predicting mortality in midlife adults with and without Down syndrome living with family. J Intellect Disabil Res. 2007;51(12):1039–1050. doi: 10.1111/j.1365-2788.2007.01006.x. [DOI] [PubMed] [Google Scholar]
- 26.Ram G, Chinen J. Infections and immunodeficiency in Down syndrome. Clin Exp Immunol. 2011;164(1):9–16. doi: 10.1111/j.1365-2249.2011.04335.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baxter H, Lowe K, Houston H, Jones G, Felce D, Kerr M. Previously unidentified morbidity in patients with intellectual disability. Br J Gen Pract. 2006;56(523):93–98. [PMC free article] [PubMed] [Google Scholar]
- 28.Landes SD, Peek CW. Death by mental retardation? The influence of ambiguity on death certificate coding error for adults with intellectual disability. J Intellect Disabil Res. 2013;57(12):1183–1190. doi: 10.1111/j.1365-2788.2012.01614.x. [DOI] [PubMed] [Google Scholar]