Abstract
Objectives. To assess the impact of a large-scale place-based intervention on obesity prevalence in Black communities.
Methods. The Racial and Ethnic Approaches to Community Health across the United States (REACH US) project was conducted in 14 predominantly Black communities in California, Illinois, Massachusetts, New York, Ohio, Pennsylvania, South Carolina, Virginia, Washington, and West Virginia. We measured trends from 2009 to 2012 in the prevalence of obesity. We used Behavioral Risk Factor Surveillance System data to compare these trends with trends among non-Hispanic Whites and non-Hispanic Blacks in the United States and in the 10 states where REACH communities were located, and with a propensity score–matched national sample of non-Hispanic Blacks.
Results. The age-standardized prevalence of obesity decreased in REACH US communities (P = .045), but not in the comparison populations (P = .435 to P = .996). The relative change was −5.3% in REACH US communities versus +2.4% in propensity score–matched controls (P value for the difference = .031). The net effect on the reduction of obesity prevalence was about 1 percentage point per year for REACH.
Conclusions. Obesity prevalence was reduced in 14 disadvantaged Black communities that participated in the REACH project.
Obesity is recognized as a national epidemic in the United States that disproportionately affects Blacks. During 2011 to 2014, 48.1% of non-Hispanic Black adults were obese, compared with 34.5% of non-Hispanic White adults.1 The obesity trend is less favorable for Blacks: over the 12-year period from 1999 through 2010, the annual increase in obesity prevalence was greater in non-Hispanic Blacks than in non-Hispanic Whites.2
Previous efforts to reduce obesity among Blacks have largely focused on individual-level weight-loss interventions, mostly conducted in clinical or university settings.3–6 Most of these studies had small sample sizes (e.g., < 200 persons), measured only short-term effects (e.g., < 6 months), or were conducted among medically at-risk persons (e.g., diabetes, hypertension).3–6 Reports on large-scale community-based interventions successfully reducing the prevalence of obesity in Black populations have been lacking. The Racial and Ethnic Approaches to Community Health across the United States (REACH US) project, launched in 2007 by the Centers for Disease Control and Prevention, develops community-based participatory approaches targeting vulnerable communities to reduce health disparities.7 A major focus of the REACH intervention was health promotion and chronic disease prevention, especially for cardiovascular disease and diabetes mellitus. Obesity reduction was one of the targeted interventions.
We report on the trend in adult obesity among 14 Black communities during the period 2009 through 2012 and compare this trend with those among non-Hispanic Whites and non-Hispanic Blacks nationwide and in the states where REACH US communities were located. We also compare this trend with that among a nationwide subsample of non-Hispanic Blacks selected through propensity score matching.
METHODS
The REACH US project funded 40 communities to develop health interventions that address health disparities among African American or Black, Hispanic or Latino, Asian, Native Hawaiian or other Pacific Islander, and American Indian/Alaska Native populations.7,8 Fourteen Black communities within the REACH US program chose cardiovascular disease or diabetes as the priority area for interventions on the basis of local needs assessment. The communities are located in the following 10 states: California, Illinois, Massachusetts, New York, Ohio, Pennsylvania, South Carolina, Virginia, Washington, and West Virginia. The 14 communities listed in the Acknowledgments section are the focus of this report.
Community Interventions in 14 Predominantly Black Communities
All communities had 3 major intervention approaches: building strong community-based coalitions; focusing on policy, systems, and environmental improvements; and culturally tailored interventions. Community coalitions were established or expanded, and included community-based organizations, local health departments, universities, and organizations or groups with primary missions unrelated to health, such as faith-based groups, YMCA, and volunteer groups. Community members actively participated in every stage of the program, including planning, implementation, and evaluation.
The REACH US program focused on policy, systems, and environmental improvements that promote healthy eating and active living, and that had positive impact on reducing the prevalence of obesity in the community. Lack of healthy food options and access were identified as challenges in REACH US communities.9,10 To address this, some coalitions worked with community leaders to limit the establishment of new fast-food restaurants and to create incentive packages to bring new grocery stores to the community or to expand healthy food options offered in corner stores and other existing retail venues.10 Neighborhood farmers’ markets, produce stands, community gardens, and school gardens were created to increase access to and reduce out-of-pocket costs for healthy foods.
In addition, the REACH US coalitions worked with partners to implement Complete Streets policies, which provide accommodations for motorists, bicyclists, pedestrians, and public transit users,11 and to support infrastructure for physical activity, such as improving the walkability and safety of neighborhood streets. To increase the available opportunities to engage in physical activity, REACH US implemented a variety of worksite wellness policies12 and revitalized the community environment to include more accessible recreational areas. Some coalitions also worked with partners to decrease out-of-pocket costs for community physical activity or recreation facilities—for example, offering discounts at gyms.
Black leaders in the community served as coalition members to act as catalysts for change in the community and ensure that interventions were culturally appropriate and tailored to the target population’s health literacy level. Community-wide educational and communication campaigns included newsletters, radio talk shows, local television cable networks, posters, and health promotion materials distributed to community health centers, neighborhood or senior centers, churches, barbershops, or beauty salons. Educational classes and workshops were offered to community members. Churches were active sites for health promotion, disease prevention, and education activities, such as health screenings, nutrition workshops, fitness classes, walking clubs, and weight-loss support groups.13 Many communities recruited and trained local lay health workers to provide culturally relevant and appropriate education, counseling, and social support.14
REACH Risk Factor Survey
As part of the REACH US project evaluation, we conducted annual cross-sectional surveys on adults aged 18 years or older from 2009 through 2012 in intervention communities. The survey used an address-based sampling approach with multimode data collection8 to account for the increasing use of cell phones. We used address sampling frames to match the intervention geographies of the REACH US programs. Surveys samples were conducted by telephone for sampled addresses that matched to telephone numbers. We also mailed self-administered questionnaires to households without a phone match and to those who did not respond by telephone. We used a uniform questionnaire in all communities and in all survey years. To obtain the data on obesity, we asked the respondents “About how much do you weigh without shoes?” and “About how tall are you without shoes?” Among sampled households contacted by telephone successfully, on average, 77% cooperated with the screening interview to determine the age and racial/ethnic eligibility of the household members. Among eligible household members, the interview completion rate was 52%. For the mailed questionnaire, the return rate was, on average, 33%. Of respondents in this report, 47% completed telephone interviews and 53% completed mailed questionnaires. Because REACH US interventions targeted Black residents regardless of Hispanic origin, the surveys included Blacks of any ethnicity. However, almost all of the Black survey respondents (which ranged from 96% to 98% over the years) were non-Hispanic Blacks.
Comparison Populations
We compared data from the Behavioral Risk Factor Surveillance System (BRFSS) from 2009 through 2012 with data from the REACH US Risk Factor Survey. Both surveys asked identical questions relevant to the current report. The BRFSS is a state-based annual telephone survey conducted in the 50 states, the District of Columbia, and US territories to gather a representative sample of noninstitutionalized residents aged 18 years and older.15 From 1984 to 2010, BRFSS included landline samples only. Beginning in 2011, cellular telephone samples were also included in the survey. We used the weighting methodology, iterative proportional fitting (“raking”), for data from 2009 through 2012 in this article. On average over the years, the median response rate was 51% and there were 458 705 respondents each year.
Data Analysis
There were 1503 respondents (4%) who did not provide height or weight information and we excluded them from this study. We performed all the analyses taking into account the complex sampling designs in the REACH US and BRFSS surveys with SUDAAN software (version 11, Research Triangle Institute, NC). We compared baseline (2009) characteristics (age, gender, education, annual family income, and employment status) among Blacks in REACH US communities with non-Hispanic White and non-Hispanic Black BRFSS respondents nationwide. We estimated the prevalence of obesity by survey year among REACH Blacks and among non-Hispanic Whites and non-Hispanic Blacks for the total US population and for the 10 states where REACH US communities were located. We defined obesity as body mass index (BMI) of 30 or more kilograms per meters squared, determined on the basis of self-reported height and weight. We age-standardized prevalence by the direct method to the US adult population in the 2000 census.16
We performed logistic regression to examine the time trend of obesity by testing the year term (2009 through 2012), with adjustment for 5 age groups, for REACH US and BRFSS separately.
Use of propensity score.
In the absence of an experimental design, the intervention sample and the comparison sample may differ in characteristics that affect the outcome of interest (i.e., obesity). To avoid the biases that this difference may generate, we used propensity score matching followed by subclassification17–20 to select and weight a subsample of comparison BRFSS non-Hispanic Black respondents who were similar to Black respondents in the REACH Risk Factor Survey each year. This approach allows an estimate of the intervention’s impact on the REACH population to be obtained as the difference in the change of prevalence of obesity between REACH US samples and the matched comparison samples from BRFSS.
For the matching step, we first created separate pools of non-Hispanic Black candidate controls for each REACH US community by apportioning BRFSS respondents randomly. The total pool sizes were on average 31 307 persons (range = 28 070–32 862 persons) per year. Then, for each REACH US respondent, we selected 1 BRFSS non-Hispanic Black respondent as a matched control. This BRFSS control had the closest estimated propensity score by using the pair nearest neighbor matching method with replacement within a propensity score caliper width of 0.25 standard deviations.19 We estimated the propensity score by using a logistic regression in which we regressed sample membership on the following covariates: gender, age, number of adults in the household, education (4 levels), employment status (4 categories), annual family income (an ordinal variable representing 8 income levels), and an indicator for date of interview. For variables with missing information (e.g., education, employment, and income), we also included missing indicators as covariates in the propensity score matching.
In the subclassification step, we reestimated the propensity score by using the REACH US and the matched BRFSS samples. We ranked all the cases and divided them into 2 subclasses by using the median propensity score among the REACH samples. If we found a significant difference in mean propensity score between the intervention and comparison samples in either subclass, we further split the sample in that subclass. We continued repeating the same procedure until no significant difference was found. Hence, the subclassification step identified homogeneous subgroups of REACH US and BRFSS respondents selected in the matching step. For each community and year, we weighted BRFSS respondents in each subclass by the estimated number of individuals in that subclass in the REACH US population.20 We estimated this number by using REACH US sampling weights. After all of these steps, we calculated the absolute standardized differences in percentages (and means) of covariates between the 2 comparison groups to confirm that the covariates were balanced.
Testing differences in time trends and calculating absolute and relative changes.
In a logistic regression model with REACH US and BRFSS matched-control samples combined, we tested the interaction term, year multiplied by sample membership (REACH US or BRFSS), to examine whether the time trends were significantly different between REACH US and BRFSS controls. We also tested the interaction term with the covariates used for propensity score matching to adjust for any residual difference in covariates within each subclass and secular change in the covariate distribution over time.
For REACH US and BRFSS matched controls, we calculated the 3-year absolute percentage point change and 3-year relative percent change in the prevalence of obesity from 2009 through 2012 in REACH US communities and in comparison populations. The prevalence estimate in the 4 survey years was the dependent variable, and we performed linear regression with a year term as the independent variable in the model. We calculated the 3-year absolute percentage point change as 3∗Β, where Β is the regression coefficient of the year term derived from the linear regression. When the prevalence estimate was log transformed as the dependent variable in the regression model, we calculated the average annual percent change as 100∗(eΒ – 1) and the 3-year percent change as 100∗(e3Β – 1).
RESULTS
Data on BMI were available for the following numbers of Black respondents in REACH US communities during the years 2009 through 2012: 8765, 9831, 9150, and 8217, respectively. Blacks in REACH US communities were in general younger than non-Hispanic Whites in the nation, but were older than non-Hispanic Blacks in 2009 BRFSS (Table 1). The REACH US communities had relatively fewer men. Education level among Blacks in REACH US communities and in the nation was lower than it was in the non-Hispanic White population. Compared with either US non-Hispanic Whites or non-Hispanic Blacks, Blacks in REACH US communities had lower annual family income, a smaller proportion of persons who were employed, and a greater proportion of persons who were unemployed or unable to work, demonstrating that the 14 REACH US Black communities were disadvantaged.
TABLE 1—
Characteristics of Adults in Black Communities in the REACH US Project, 2009, Compared With US Non-Hispanic White and Non-Hispanic Black Populations in the BRFSS, 2009
| BRFSS |
|||
| Characteristic | REACH US Communities (n = 8765), %a (95% CI) | Non-Hispanic White (n = 323 740), %a (95% CI) | Non-Hispanic Black (n = 31 547), %a (95% CI) |
| Age groups, y | |||
| 18–34 | 29.4 (28.1, 30.7) | 26.8 (26.3, 27.2) | 34.2 (32.8, 35.7) |
| 35–44 | 16.5 (15.5, 17.6) | 17.2 (16.9, 17.5) | 19.6 (18.5, 20.7) |
| 45–54 | 17.3 (16.4, 18.1) | 20.0 (19.7, 20.3) | 19.3 (18.3, 20.3) |
| 55–64 | 18.6 (17.7, 19.5) | 15.8 (15.6, 16.1) | 13.9 (13.1, 14.7) |
| ≥ 65 | 18.2 (17.5, 19.0) | 20.2 (20.0, 20.4) | 13.0 (12.3, 13.7) |
| Male | 44.5 (43.3, 45.7) | 48.9 (48.7, 49.1) | 48.1 (46.9, 49.3) |
| Education level | |||
| < high school | 15.1 (14.2, 16.0) | 10.7 (10.4, 11.0) | 18.8 (17.6, 20.0) |
| High school | 31.6 (30.4, 32.8) | 30.3 (29.9, 30.7) | 33.6 (32.4, 35.0) |
| > high school | 53.4 (52.1, 54.6) | 59.0 (58.6, 59.4) | 47.6 (46.2, 49.0) |
| Annual family income, $ | |||
| < 25 000 | 49.0 (47.6, 50.4) | 24.5 (24.1, 24.9) | 46.7 (45.3, 48.2) |
| 25 000 to < 50 000 | 28.0 (26.8, 29.2) | 27.1 (26.7, 27.4) | 28.3 (27.0, 29.7) |
| ≥ 50 000 | 23.0 (21.9, 24.3) | 48.5 (48.1, 48.9) | 24.9 (23.8, 26.1) |
| Employment status | |||
| Employed | 44.5 (43.2, 45.8) | 57.3 (56.9, 57.7) | 52.4 (51.0, 53.8) |
| Unemployed | 16.4 (15.4, 17.4) | 7.5 (7.3, 7.8) | 14.6 (13.6, 15.6) |
| Homemaker, student, retired | 27.3 (26.2, 28.4) | 29.9 (29.5, 30.2) | 22.8 (21.7, 23.9) |
| Unable to work | 11.8 (11.1, 12.6) | 5.3 (5.1, 5.5) | 10.3 (9.6, 11.0) |
Note. BRFSS = Behavioral Risk Factor Surveillance System; CI = confidence interval; REACH US = Racial and Ethnic Approaches to Community Health across the United States. Not all percentages sum to 100% because of rounding.
Weighted %.
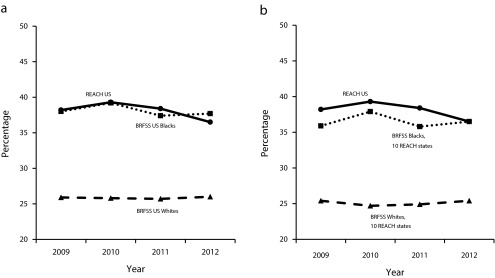
Figure 1 shows the time trend of the age-standardized, weighted prevalence of obesity from 2009 to 2012 in REACH US communities and for non-Hispanic Blacks and non-Hispanic Whites in the nation (Figure 1a) and in the 10 states where the REACH US communities were located (Figure 1b). There was a downward trend of obesity prevalence in REACH US communities, whereas we observed little change in the comparison populations. In comparison with non-Hispanic Whites in the nation, the prevalence of obesity was 12.3 percentage points higher among Blacks in REACH US communities in 2009. The disparity reduced to 10.5 percentage points in 2012 (Figure 1a). Likewise, the disparity in the prevalence of obesity reduced from 12.8 percentage points to 11.1 percentage points between Blacks in REACH US communities and non-Hispanic Whites in the 10 comparison states (Figure 1b).
FIGURE 1—
Trends of Age-Standardized Prevalence of Obesity (2009–2012) Among 14 Black Communities in the REACH US Project and Non-Hispanic Whites and Non-Hispanic Blacks (a) in the BRFSS and (b) in the 10 States Where These Communities Are Located
Note. BRFSS = Behavioral Risk Factor Surveillance System; REACH US = Racial and Ethnic Approaches to Community Health across the United States.
In the logistic regression analysis, the age-adjusted odds ratio was 0.95 (95% confidence interval = 0.98, 0.99) for time trend (year) in REACH US communities (P = .045). The odds ratios were not statistically significant for any of the other comparison populations (P values ranged from .435 to .996). We performed additional analyses including only landline respondents in BRFSS. We found no significant change in the age-adjusted prevalence of obesity from 2009 to 2012 for non-Hispanic Blacks either in the nation (P = .073) or in the 10 comparison states (P = .919; data not shown). There were significant upward trends in the prevalence of obesity in non-Hispanic Whites nationwide: 25.9%, 25.8%, 26.5%, and 27.3% for the 4 survey years, respectively (P < .001), and in the 10 comparison states: 25.4%, 24.7%, 25.6%, and 26.6%, respectively (P = .004).
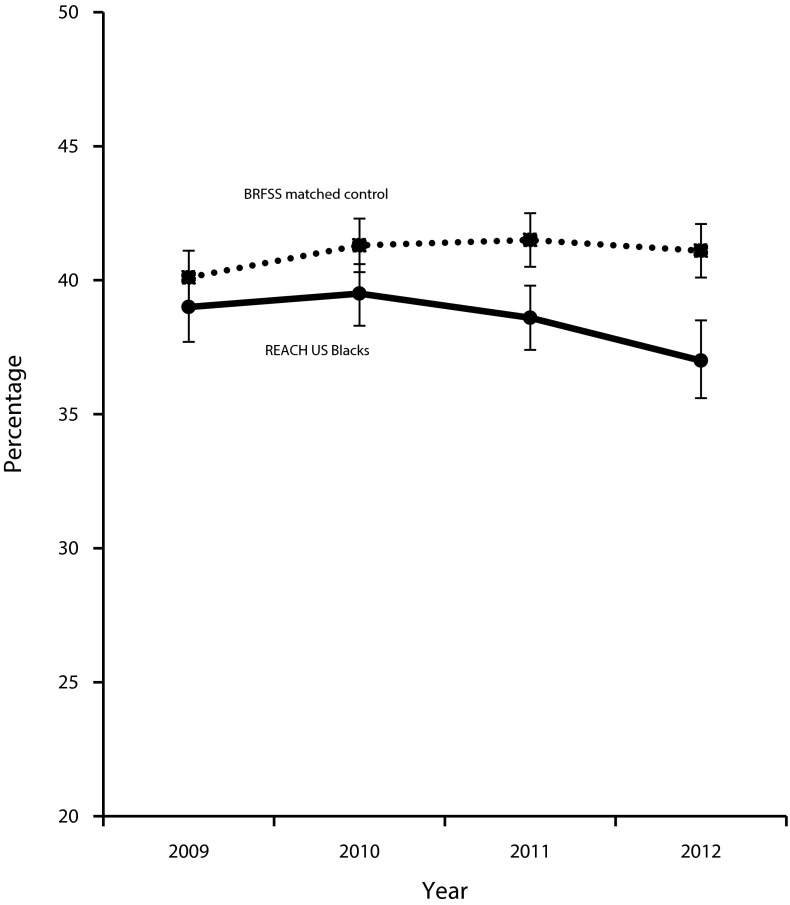
As shown in Table 1, Blacks in REACH US communities differed in many ways from those of US non-Hispanic Whites and non-Hispanic Blacks. We used propensity score analysis to select matched-control samples from BRFSS. We selected approximately one-to-one matched controls in each survey year (Table 2). Propensity score matching was not able to find controls for 523 (6%), 414 (4%), 395 (4%), and 361 (4%) REACH US respondents, respectively, in the 4 survey years. The mean absolute standardized differences in percentages (and means) of covariates between REACH US and matched controls were less than 10%, indicating that the covariates were balanced between the 2 comparison groups (data not shown). Table 2 presents the weighted prevalence of obesity and the corresponding 95% confidence intervals over time in REACH US communities and in the matched-control samples. The 3-year relative percent change in weighted prevalence was −5.3% in REACH US communities, whereas it was +2.4% in matched controls. The 3-year absolute percentage point change was −2.1 versus +1.0 in REACH and matched controls, respectively. Hence, the 3-year net effect size of the intervention was about −3 percentage points (i.e., −1 percentage point per year on average).
TABLE 2—
Prevalence of Obesity Among Black Communities in the REACH US Project and Matched Control Samples From the BRFSS: 2009–2012
| REACH US |
BRFSS Matched Controls |
|||
| Variable | No. | %a (95% CI) | No. | %a (95% CI) |
| Year | ||||
| 2009 | 8242 | 39.0 (37.7, 40.3) | 8106 | 40.1 (38.7, 41.5) |
| 2010 | 9417 | 39.5 (38.4, 40.7) | 9293 | 41.3 (40.0, 42.7) |
| 2011 | 8755 | 38.6 (37.4, 39.8) | 8642 | 41.5 (40.0, 43.1) |
| 2012 | 7856 | 37.0 (35.5, 38.4) | 7734 | 41.1 (39.3, 42.9) |
| Changes, 2009–2012 | ||||
| Absolute percentage point change | −2.1 | +1.0 | ||
| Relative percent change | −5.3 | +2.4 | ||
Note. BRFSS = Behavioral Risk Factor Surveillance System; CI = confidence interval; REACH US = Racial and Ethnic Approaches to Community Health across the United States.
Weighted %.
Figure 2 is a graphical presentation of the divergent trends of obesity prevalence between the 2 groups. Whereas the prevalence of obesity in the 2 Black groups at baseline (year 2009) was similar, it decreased over subsequent study years (2010–2012) among the REACH US respondents but not among the BRFSS matched samples. In the logistic regression analysis, the interaction term, year multiplied by sample membership (REACH US or BRFSS), was statistically significant (P = .031), indicating that the time trends of obesity prevalence are significantly different between REACH US and BRFSS controls. The result was consistent when we included all of the covariates in the regression (P = .045).
FIGURE 2—
Trends of Prevalence of Obesity (2009–2012) Among 14 Black Communities in the REACH US Project and Among a Propensity Score–Matched National Sample of Blacks From the BRFSS
Note. BRFSS = Behavioral Risk Factor Surveillance System; REACH US = Racial and Ethnic Approaches to Community Health across the United States.
We observed a significant downward trend (P = .049) of severe obesity (BMI ≥ 35 kg/m2) similarly in REACH communities, whereas a small upward trend (P = .634) occurred in BRFSS matched controls (data not shown). The 3-year relative percent change in prevalence was −7.6% and +2.2%, respectively, in the 2 comparison groups. The 3-year absolute percentage point change was −1.4 and +0.4 percentage points, respectively.
DISCUSSION
The prevalence of obesity among Black communities within the REACH US project decreased from 2009 through 2012, in contrast to obesity prevalence among non-Hispanic Whites and non-Hispanic Blacks in the United States, who showed no significant improvement during this time period. The net effect on reduction of obesity prevalence in REACH communities was about 1 percentage point per year compared with BRFSS matched controls.
Blacks are less likely than Whites to live in environments that support healthy eating and active living.21 They tend to have greater economic constraints on both food choices and opportunities for physical activity. The REACH US project addressed “upstream” causes of health disparities. Environmental and system improvements implemented in REACH made healthy eating and active living easier, more convenient, affordable, safe, and a behavior norm; these kinds of improvements are potentially more effective than individual-level approaches.22
In the REACH US project, health initiatives were based on the unique historical and cultural context of the community. Religious institutions have a long history as the center of spiritual and social support and community leadership in Black communities.23,24 They reach a large and consistent group, provide space for programming, and offer a real-world setting to conduct health promotion and lifestyle interventions. Clergy were involved in disseminating health-related messages. The switch from offering traditional to healthier and culturally preferable foods in churches and other gatherings likely facilitated the establishment of a healthier eating norm in the communities.
Including community health workers or advisors in REACH US and other projects has been an effective strategy to successfully conduct interventions and make significant contributions to reduce health disparities.14,25 These grassroots health workers had well-established ties and good reputations in the community. They provided culturally appropriate health education and served as effective links between vulnerable populations and the health care system. Through community health workers, the coalitions could reach greater numbers of community members.
In contrast to most short-term clinical trials, which have focused on overweight or obese or at-risk individuals in highly controlled settings, the REACH US project was a large-scale, community-participatory intervention at the general population level. It is an intervention in the “real-world” setting that is conducted through community engagement, social action, and collective action. A small improvement in a large population can make a bigger impact in public health than a larger improvement in a small portion of the population.26 By building capacity through the formation of a wide mix of community-based coalitions, the REACH US project ensured that community activities and programs were sustainable and the improvements achieved could be long-lasting. Establishing a collaborative infrastructure and creating cross-sector partnerships, including “nontraditional” partners, are important for the long-term success of community health efforts. Environmental change made healthy eating and active living easier and a behavior norm.22 Thus, healthy lifestyle choices are likely to be sustained.
There are several limitations of this report. First, we defined obesity on the basis of self-reported height and weight. Errors and bias in comparison with direct measures have been reported.27 However, the bias and the possible temporal changes in bias existed in our comparison populations as well. Data from the National Health and Nutrition Examination Survey showed that changes in bias over time were similar among different demographic subgroups (e.g., non-Hispanic Whites and non-Hispanic Blacks).27 Second, the REACH US project was not a clinical trial and had no formal control groups. In this report, we used propensity score matching to select an appropriate control group and to evaluate the impact of the intervention in an observational study. Although we matched on a large number of socioeconomic indicators in propensity score analyses, we did not consider some unmeasured confounders (e.g., neighborhood and environmental information). Finally, the communities used various intervention strategies in multiple settings simultaneously. It is difficult to assess the impact of a specific approach. However, it should be noted that the REACH US project was designed as a broad-based, multifaceted community intervention. Reversing the US obesity epidemic requires a comprehensive and coordinated approach.28
In this study, we observed a reduction in the prevalence of obesity in disadvantaged Black communities outside a controlled research context. This large-scale, population-wide intervention supports the idea that through community collaborations, system and environmental interventions, and cultural tailoring approaches, health disparities can be reduced and the health status of groups most affected by health inequities can be improved.
ACKNOWLEDGMENTS
The Black communities who participated in the Racial and Ethnic Approaches to Community Health Across the US Risk Factor Survey were Center for Community Health, Education, and Research, Massachusetts; Chicago Department of Health, Chicago, IL; Community Health Councils Inc, California; Institute for Urban Family Health, New York; Medical University of South Carolina, South Carolina; Mount Sinai School of Medicine, New York; Regents of the University of California, Los Angeles, CA; Seattle King County Department of Public Health, Washington; Southeast Chicago Development Commission, Illinois; To Our Children’s Future With Health Inc, Pennsylvania; University of Illinois at Chicago, Illinois; Vernon J. Harris East End Community Health Center, Virginia; West Virginia Department of Health and Human Services, West Virginia; and YMCA of Greater Cleveland, Ohio.
HUMAN PARTICIPANT PROTECTION
This study received approval from the institutional review board of the Centers for Disease Control and Prevention and the Office of Management and Budget.
REFERENCES
- 1.Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of obesity among adults and youth: United States, 2011–2014. NCHS Data Brief. 2015;(219):1–8. [PubMed] [Google Scholar]
- 2.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307(5):491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 3.Fitzgibbon ML, Tussing-Humphreys LM, Porter JS, Martin IK, Odoms-Young A, Sharp LK. Weight loss and African-American women: a systematic review of the behavioural weight loss intervention literature. Obes Rev. 2012;13(3):193–213. doi: 10.1111/j.1467-789X.2011.00945.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lemacks J, Wells BA, Ilich JZ, Ralston PA. Interventions for improving nutrition and physical activity behaviors in adult African American populations: a systematic review, January 2000 through December 2011. Prev Chronic Dis. 2013;10:E99. doi: 10.5888/pcd10.120256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kong A, Tussing-Humphreys LM, Odoms-Young AM, Stolley MR, Fitzgibbon ML. Systematic review of behavioural interventions with culturally adapted strategies to improve diet and weight outcomes in African American women. Obes Rev. 2014;15(suppl 4):62–92. doi: 10.1111/obr.12203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Newton RL, II, Griffith DM, Kearney WB, Bennett GG. A systematic review of weight loss, physical activity and dietary interventions involving African American men. Obes Rev. 2014;15(suppl 4):93–106. doi: 10.1111/obr.12209. [DOI] [PubMed] [Google Scholar]
- 7.Liburd LC. Foreword. REACH US in action: inspiring hope, rewarding courage. Fam Community Health. 2011;34(suppl 1):S2–S6. doi: 10.1097/FCH.0b013e31820af643. [DOI] [PubMed] [Google Scholar]
- 8.Liao Y, Bang D, Cosgrove S et al. Surveillance of health status in minority communities—Racial and Ethnic Approaches to Community Health Across the US (REACH US) Risk Factor Survey, United States, 2009. MMWR Surveill Summ. 2011;60(6):1–44. [PubMed] [Google Scholar]
- 9.Castillo SR, Block D, Lohff C, Krauss S. Innovation in the collection of food availability data: a case study of the Chicago Department of Public Health Sanitarian Survey. Prev Med. 2013;57(1):70–71. doi: 10.1016/j.ypmed.2013.03.006. [DOI] [PubMed] [Google Scholar]
- 10.Lewis LB, Galloway-Gilliam L, Flynn G, Nomachi J, Keener LC, Sloane DC. Transforming the urban food desert from the grassroots up: a model for community change. Fam Community Health. 2011;34(suppl 1):S92–S101. doi: 10.1097/FCH.0b013e318202a87f. [DOI] [PubMed] [Google Scholar]
- 11.Buckner-Brown J, Tucker P, Rivera M et al. Racial and ethnic approaches to community health: reducing health disparities by addressing social determinants of health. Fam Community Health. 2011;34(suppl 1):S12–S22. doi: 10.1097/FCH.0b013e318202a720. [DOI] [PubMed] [Google Scholar]
- 12.Maxwell AE, Yancey AK, AuYoung M et al. A midpoint process evaluation of the Los Angeles Basin Racial and Ethnic Approaches to Community Health Across the US (REACH US) Disparities Center, 2007–2009. Prev Chronic Dis. 2011;8(5):A115. [PMC free article] [PubMed] [Google Scholar]
- 13.Kaplan SA, Ruddock C, Golub M et al. Stirring up the mud: using a community-based participatory approach to address health disparities through a faith-based initiative. J Health Care Poor Underserved. 2009;20(4):1111–1123. doi: 10.1353/hpu.0.0221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cosgrove S, Moore-Monroy M, Jenkins C et al. Community health workers as an integral strategy in the REACH US program to eliminate health inequities. Health Promot Pract. 2014;15(6):795–802. doi: 10.1177/1524839914541442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mokdad AH, Stroup DF, Giles WH. Public health surveillance for behavioral risk factors in a changing environment. Recommendations from the Behavioral Risk Factor Surveillance Team. MMWR Recomm Rep. 2003;52(RR-9):1–12. [PubMed] [Google Scholar]
- 16.US Census Bureau. Profiles of General Demographic Characteristics (DP-1), United States: 2000. Available at: http://www.census.gov/prod/2002pubs/c2kprof00-us.pdf. Accessed May 17, 2016.
- 17.Rosenbaum P, Rubin D. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70(1):41–55. [Google Scholar]
- 18.Rosenbaum P, Rubin D. Reducing bias in observational studies using subclassification on the propensity score. J Am Stat Assoc. 1984;79(387):516–524. [Google Scholar]
- 19.Rosenbaum P, Rubin D. Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. Am Stat. 1985;1985(39):33–38. [Google Scholar]
- 20.Rubin D. Using propensity scores to help design observational studies: application to the tobacco litigation. Health Serv Outcome Res Methodology. 2001;2:169–188. [Google Scholar]
- 21.Kumanyika SK, Whitt-Glover MC, Gary TL et al. Expanding the obesity research paradigm to reach African American communities. Prev Chronic Dis. 2007;4(4):A112. [PMC free article] [PubMed] [Google Scholar]
- 22.Bauer UE, Briss PA, Goodman RA, Bowman BA. Prevention of chronic disease in the 21st century: elimination of the leading preventable causes of premature death and disability in the USA. Lancet. 2014;384(9937):45–52. doi: 10.1016/S0140-6736(14)60648-6. [DOI] [PubMed] [Google Scholar]
- 23.Campbell MK, Hudson MA, Resnicow K, Blakeney N, Paxton A, Baskin M. Church-based health promotion interventions: evidence and lessons learned. Annu Rev Public Health. 2007;28:213–234. doi: 10.1146/annurev.publhealth.28.021406.144016. [DOI] [PubMed] [Google Scholar]
- 24.Lancaster KJ, Carter-Edwards L, Grilo S, Shen C, Schoenthaler AM. Obesity interventions in African American faith-based organizations: a systematic review. Obes Rev. 2014;15(suppl 4):159–176. doi: 10.1111/obr.12207. [DOI] [PubMed] [Google Scholar]
- 25.Andrews JO, Felton G, Wewers ME, Heath J. Use of community health workers in research with ethnic minority women. J Nurs Scholarsh. 2004;36(4):358–365. doi: 10.1111/j.1547-5069.2004.04064.x. [DOI] [PubMed] [Google Scholar]
- 26.Rose G. Strategy of prevention: lessons from cardiovascular disease. Br Med J (Clin Res Ed) 1981;282(6279):1847–1851. doi: 10.1136/bmj.282.6279.1847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stommel M, Osier N. Temporal changes in bias of body mass index scores based on self-reported height and weight. Int J Obes (Lond) 2013;37(3):461–467. doi: 10.1038/ijo.2012.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Khan LK, Sobush K, Keener D et al. Recommended community strategies and measurements to prevent obesity in the United States. MMWR Recomm Rep. 2009;58(RR-7):1–26. [PubMed] [Google Scholar]