Abstract
Objectives. To evaluate knowledge and prescribing changes following a 2-month public health detailing campaign (one-to-one educational visits) about judicious opioid analgesic prescribing conducted among health care providers in Staten Island, New York City, in 2013.
Methods. Three detailing campaign recommendations were (1) a 3-day supply of opioids is usually sufficient for acute pain, (2) avoid prescribing opioids for chronic noncancer pain, and (3) avoid high-dose opioid prescriptions. Evaluation consisted of a knowledge survey, and assessing prescribing rates and median day supply per prescription. Prescribing data from the 3-month period before the campaign were compared with 2 sequential 3-month periods after the campaign.
Results. Among 866 health care providers visited, knowledge increased for all 3 recommendations (P < .01). After the campaign, the overall prescribing rate decreased similarly in Staten Island and other New York City counties (boroughs), but the high-dose prescribing rate decreased more in Staten Island than in other boroughs (P < .01). Median day supply remained stable in Staten Island and increased in other boroughs.
Conclusions. The public health detailing campaign improved knowledge and likely prescribing practices and could be considered by other jurisdictions to promote judicious opioid prescribing.
Opioid analgesic misuse and overdose constitute a national public health crisis.1 In New York City, opioid analgesic overdose deaths increased 267% (from 0.9 to 3.3 per 100 000 New Yorkers) between 2000 and 2011. Among New York City’s 5 counties (boroughs), Staten Island’s opioid analgesic overdose death rate was more than 3 times higher than that of other boroughs in 2011.2
Nationally, rising rates of opioid analgesic–associated overdose deaths have occurred concurrently with increases in opioid prescribing.3 In addition, higher dosages and longer duration of opioid treatment are associated with increased overdose risk.4–6 Compared with other New York City boroughs, Staten Island patterns of filled opioid prescriptions carry increased overdose risk, including higher per capita rates of opioid prescriptions and of high-dose opioid prescriptions (> 100 total daily morphine milligram equivalents [MME]), and longer median prescription duration.7 In light of the association between opioid prescribing practices and opioid overdose risk, effective strategies that change opioid prescribing patterns are urgently needed, particularly to encourage practices consistent with judicious opioid prescribing, such as those included in the Centers for Disease Control and Prevention’s recently released guidelines, and those previously released by the New York City Department of Health and Mental Hygiene (DOHMH).3–6,8,9
In response to the disproportionate opioid analgesic overdose death rate and higher-risk prescribing practices identified in Staten Island, DOHMH conducted a public health detailing campaign on judicious opioid prescribing among Staten Island health care providers during June 10 through August 6, 2013. Public health detailing, modeled after the pharmaceutical sales strategy, is an approach used to facilitate change in clinical practice through brief one-to-one educational visits. Public health detailing campaigns are focused on specific clinical topics, emphasize a limited number of key messages, and offer practice tools, provider information, and patient education resources at the one-to-one visits.10 Previous public health detailing campaigns conducted by DOHMH successfully changed self-reported clinical practice behavior.11 A meta-analysis of educational outreach visits by trained persons to health care professionals, as is performed in public health detailing, found associated changes in prescribing practices.12 In Utah, a detailing campaign specifically designed to change opioid prescribing practices demonstrated that group detailing of health care providers was associated with improved self-reported opioid prescribing practices.13 In 1 North Carolina county, evaluation of a one-to-one opioid analgesic detailing campaign that focused on chronic pain suggested that the intervention changed prescribing behaviors, but did not report opioid prescription data or self-reported prescribing practices.14 In light of this body of literature, we hypothesized that knowledge changes promoted by our detailing campaign would improve opioid prescribing practices in Staten Island.
Our detailing campaign on judicious opioid prescribing in Staten Island was based on DOHMH’s judicious opioid prescribing guidelines that had been released citywide in 2011.9 As kick-off events to the detailing campaign, we convened 2 physician conferences focused on judicious opioid prescribing that were led by the Health Commissioner and held at the main Staten Island hospitals.
Promotion of judicious opioid prescribing was one part of DOHMH’s multipronged public health response that was implemented during 2011 to 2013 to address the opioid analgesic overdose crisis. In addition to the Staten Island detailing campaign and the guidelines upon which it was based, salient components of the multipronged response included dissemination of borough-specific overdose mortality data highlighting the disproportionate overdose mortality rate in Staten Island, airing public service announcements featuring Staten Islanders, and adapting guidelines for emergency departments citywide. Full details are published elsewhere.15 These efforts occurred in addition to ongoing, previously established DOHMH initiatives to increase access to medication-assisted treatment of opioid use disorder (e.g., methadone, buprenorphine), and to support harm-reduction strategies (e.g., distribution of naloxone), both of which address all types of opioid drugs, including heroin. Concurrently, there was substantial local Staten Island media coverage about the risks of opioid analgesics, and a state law (Internet System for Tracking Over-Prescribing [I-STOP]) took effect in August 2013 requiring prescribers to review patient data in New York State’s Prescription Monitoring Program (PMP), a registry of filled controlled substance prescriptions, before prescribing controlled substances.16 Among all of these elements, the only sources of messaging addressing specific prescribing recommendations during 2011 to 2013 were DOHMH’s citywide judicious opioid prescribing guidelines (2011) and the emergency department–adapted version (January 2013), and the Staten Island public health detailing campaign and its accompanying kick-off physician conferences (June–August 2013).
Our objective was to evaluate changes in knowledge and prescribing practices associated with DOHMH’s public health detailing campaign to promote judicious opioid prescribing conducted in Staten Island.
METHODS
Our intervention design for the public health detailing campaign used a broad and inclusive public health approach—targeting a large proportion of health care providers in a community, regardless of individual prescribing practices. We included physicians, nurse practitioners (NPs), and physician assistants (PAs), because all of these professions are permitted to prescribe opioids in New York State. We obtained health care provider information from the National Provider Identifier Registry; at the time of the detailing campaign, an estimated 1648 physicians, NPs, and PAs with identified specialties were known to practice in Staten Island; of these, 1182 were targeted on the basis of being specialties likely to involve outpatient, non–end-of-life care (e.g., internal medicine, orthopedic surgery).
Intervention
To conduct the public health detailing campaign, health department representatives arrived unannounced to practices, first introducing front-desk staff to the campaign, and then either waiting to visit with health care providers or returning at a mutually agreed upon time. Strategies used to highlight the campaign’s relevance to health care providers and other office staff included showing visual displays of the disproportionate opioid analgesic overdose death rate in Staten Island and framing the problem as a community issue. During the one-to-one visits with health care providers, health department representatives delivered detailing campaign recommendations and provided “action kits” that contained additional resources. Detailing campaign recommendations, based on the previously published DOHMH judicious opioid prescribing guidelines, were (1) a 3-day supply of opioids is usually sufficient for acute pain, (2) avoid prescribing opioids for chronic noncancer pain, (3) avoid high-dose opioid prescriptions (i.e., ≥ 100 total daily MMEs).9 Regarding the latter recommendation, instruction on MMEs is generally not a routine part of clinical training, and, therefore, was anticipated to be novel technical information for health care providers. Resources in the action kit included a letter from the city Health Commissioner, a copy of the DOHMH judicious opioid prescribing guidelines, New York City borough-specific data on opioid analgesic overdose deaths and prescribing patterns, information about an online MME calculator developed by DOHMH, and patient informational material.
Figure 1 shows a poster for patient examination rooms developed for the detailing campaign with messaging tailored to Staten Islanders. Representatives attempted to garner buy-in from as many office staff as possible, recognizing that non–health care provider staff members play an instrumental role in championing new practice initiatives. Our operational protocol allowed representatives to detail additional health care providers who met targeting criteria but who had not been identified with the National Provider Identifier Registry when encountered in the field. An initial and follow-up visit was attempted for each health care provider. Ninety-one percent of initial visits were completed during the first 4 weeks of the detailing campaign. All follow-up visits were completed during the last 4 weeks of the detailing campaign. The average time between initial and follow-up visits was 4 weeks. The average duration of initial and follow-up visits were each 13 minutes.
FIGURE 1—
Patient Examination Room Poster Promoted During Opioid Analgesic Public Health Detailing Campaign: Staten Island, NY, 2013
The 2 main outcomes were changes in knowledge among detailed health care providers and changes in opioid prescribing patterns among all Staten Island prescribers.
Evaluating Knowledge Change
Data source.
To evaluate changes in health care provider knowledge, representatives verbally administered a brief, standardized survey to health care providers at initial (baseline) and follow-up visits including 1 question on each of the 3 recommendations (Table 1). At all visits, the survey was administered before discussion of the recommendations and reviewing kit material.
TABLE 1—
Health Care Provider Baseline and Follow-up Survey Responses—Opioid Analgesic Public Health Detailing Campaign: Staten Island, NY, 2013
| Recommendation | Survey Question | Correct Baseline Response, No. (%) | Correct Follow-up Response, No. (%) | Pa |
| A 3-d supply of opioid analgesics is usually sufficient for acute pain. (N = 842) | Is a 3-d supply of opioids usually sufficient to control acute pain in your patients?b | 537 (64) | 762 (90) | < .001 |
| Avoid prescribing opioid analgesics for chronic noncancer pain. (N = 814) | Is there evidence for using opioids to treat chronic pain that is not related to cancer?c | 444 (55) | 519 (64) | < .001 |
| Avoid high-dose opioid analgesic prescriptions. (N = 780) | When prescribing opioids, it can be useful to calculate the total morphine equivalents that a patient is taking per day. How many morphine equivalents do you consider to be a threshold for increased overdose risk?d | 171 (22) | 454 (58) | < .01 |
P value generated from the McNemar test.
For first survey question, correct baseline and follow-up response: yes; incorrect responses: no, sometimes, do not know.
For second survey question, correct baseline and follow-up response: no; incorrect responses: yes, somewhat, do not know.
For third survey question, correct baseline and follow-up response: 100 morphine milligram equivalents (MME); incorrect responses: 1–19 MME, 20–49 MME, 50–99 MME, 101–119 MME, 120–149 MME, 150–199 MME, ≥ 200 MME, it depends, there is no threshold, do not know.
Measures and statistical analysis.
We dichotomized responses as consistent (correct) or inconsistent (incorrect) with recommendations. Among health care providers with both baseline and follow-up visit surveys, we compared the proportion of responses that were consistent with recommendations at baseline versus at follow-up by using the McNemar test. To assess for differences among participants lost to follow up, we compared baseline responses of health care providers who completed both baseline and follow-up visit surveys to those with only baseline surveys.
Evaluating Opioid Analgesic Prescribing Patterns
Data source.
To evaluate changes in opioid prescribing patterns among Staten Island prescribers, we used de-identified data from New York State’s PMP about schedule II opioid prescriptions written by New York City prescribers and filled by New York City residents, with borough as the most specific geographic unit available. We defined New York City prescribers’ location by license location; for prescribers with more than 1 license location, we used the most frequent location.
Measures and statistical analysis.
We calculated 3 prescribing indicators: prescribing rate (number of prescriptions per 10 000 New York City residents), high-dose prescribing rate (number of high-dose prescriptions, defined as greater than 100 total daily MMEs per 10 000 New York City residents), and median day supply per prescription. We calculated these indicators for three 3-month periods: precampaign period (March–May 2013), postcampaign period 1 (September–November 2013), and postcampaign period 2 (December 2013–February 2014) to assess immediate and longer-term changes.
We compared these indicators for Staten Island versus the other 4 New York City boroughs combined (Bronx, Brooklyn, Manhattan, and Queens) by New York City license location. We combined the other 4 New York City boroughs because previous PMP analysis clearly indicated that Staten Island patterns of filled opioid prescriptions carried increased overdose risk compared with the other boroughs. We age-adjusted rates by using New York City population estimates for 2013 and Census 2000 US standard population. We tested rate changes between the precampaign period and postcampaign periods 1 and 2 for Staten Island and separately for the other New York City boroughs by using z-test comparisons. To compare rate changes over time between Staten Island and the other New York City boroughs, we used a difference-in-differences method, testing rate trends with Poisson regression model, with offset of person-time. The model included main effect terms (borough, time) and an interaction term between the main effects (borough*time). We performed analyses in SAS version 9.2 (SAS Institute Inc, Cary, NC).
RESULTS
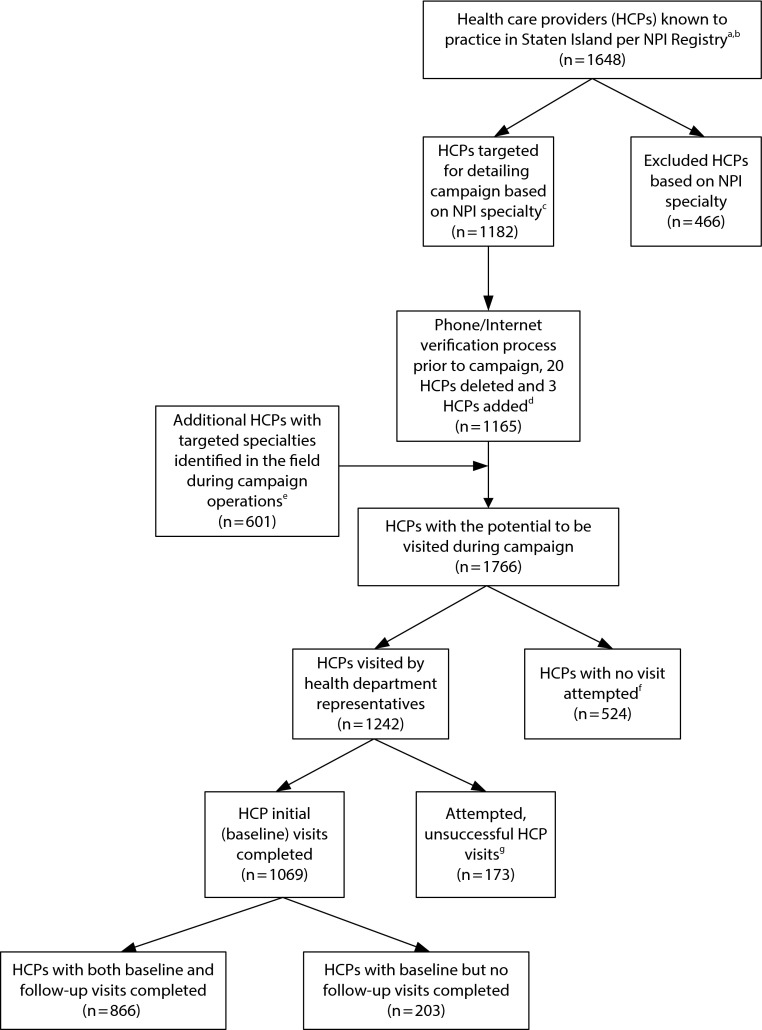
A total of 1069 health care providers were surveyed at initial visits (90% of the total number targeted [1182] during detailing campaign planning). Among those surveyed at initial visits, 866 (81%) were surveyed at follow-up visits. Baseline responses to the 3 questions did not significantly differ between health care providers with both baseline and follow-up visit surveys and those with only baseline surveys. At baseline, 64% of respondents responded that a 3-day supply is usually sufficient for acute pain, compared with 90% at follow-up (P < .001); 55% responded at baseline that evidence is insufficient for using opioids to treat chronic noncancer pain, compared with 64% at follow-up (P < .001); and, at baseline, 22% correctly reported DOHMH’s high-dose threshold (100 total daily MME), compared with 58% at follow-up (P < .01; Table 1). Figure 2 shows the flow of health care providers, starting with those known to practice in Staten Island according to the National Provider Identifier Registry and ending with the final sample of those who completed both baseline and follow-up visit surveys.
FIGURE 2—
Flowchart of Health Care Providers, Opioid Analgesic Public Health Detailing Campaign: Staten Island, NY, 2013
Note. NPI = National Provider Identifier.
aHCP types were physicians, nurse practitioners, and physician assistants.
bRepresents HCPs with identified specialties.
cTargeted specialties were those likely to involve outpatient, non–end-of-life care.
dContact information for targeted HCPs from NPI-based list were preverified by calling and searching the Internet. Pertinent information was updated; HCPs were only removed from the list at this point if definitive information was obtained indicating that an HCP was no longer practicing in Staten Island.
eMethods by which health department representatives encountered these additional HCPs included identifying them while visiting practices of HCPs who were on NPI-based list, and canvassing assigned geographical territories for signage indicating practices of HCPs who were not on NPI-based list. Detailing campaign operational protocol allowed for health department representatives to detail additional HCPs who met targeting criteria but who had not been identified by using the NPI-based list, when encountered in the field.
fReasons that visits were not attempted included upon arrival, health department representatives were told that HCPs had moved away and were no longer working at location; representatives did not attempt visit because running out of campaign time and already met quota by identifying and detailing additional HCPs who were not on NPI-based list; and office practices closed because of storm damage and no other indication of alternative practice location.
gReasons that visits were attempted but unsuccessful included absent survey or visit information; HCPs known to work at particular practices and health department representatives arrived at practices multiple times, but HCPs not present; HCPs known to work at particular practices but working irregular or reduced hours due to storm recovery, therefore difficult to execute visit; HCPs temporarily working in multiple locations due to storm recovery, therefore difficult to execute visit.
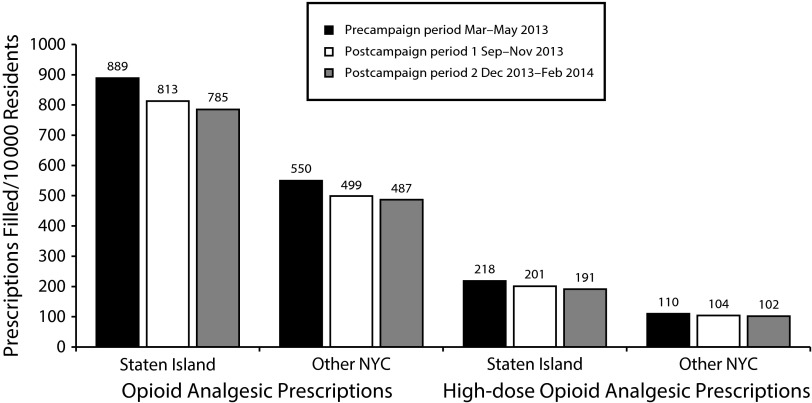
The prescribing indicators for each detailing campaign period are displayed in Table 2 and Figure 3. The prescribing rate in Staten Island decreased from 889 prescriptions per 10 000 New York City residents in the precampaign period to 785 prescriptions per 10 000 New York City residents in postcampaign period 2, an 11.5% decrease (P < .05). In the other 4 New York City boroughs, the prescribing rate decreased from 550 prescriptions per 10 000 New York City residents in the precampaign period to 487 prescriptions per 10 000 New York City residents in postcampaign period 2, an 11.5% decrease (P < .05). In difference-in-differences analyses comparing the precampaign period to postcampaign period 1, and, separately, the precampaign period to postcampaign period 2, the interaction terms did not differ from zero (B = −0.0115; 95% confidence interval [CI] = −0.0254, 0.0024; and B = −0.0035; 95% CI = −0.0175, 0.0106, respectively), demonstrating no significant differences in trends in prescribing rates between Staten Island and the other New York City boroughs (Table 2).
TABLE 2—
Rates, Median Day Supply and Difference-in-Differences Regression Results for Opioid Analgesic Prescriptions and High-Dose Prescriptions Filled by New York City Residents by Prescriber Location: New York City (NYC), March 2013–February 2014
| Variables | Precampaign Period Mar–May 2013 | Postcampaign Period 1 Sept–Nov 2013 | Postcampaign Period 2 Dec 2013–Feb 2014 |
| Rate of prescriptions filled per 10 000 residentsa (no. prescriptions; % changeb) | |||
| Opioid analgesic prescriptions | |||
| Staten Island | 889 (45 509) | 813 (41 903; −8.5*) | 785 (40 635; −11.5*) |
| Other NYC | 550 (454 123) | 499 (413 380; −9.3*) | 487 (404 047; −11.5*) |
| High-dose opioid analgesic prescriptions (> 100 MME)c | |||
| Staten Island | 218 (11 025) | 201 (10 221; −7.8*) | 191 (9 757; −12.4*) |
| Other NYC | 110 (90 857) | 104 (85 995; −5.5*) | 102 (84 201; −7.3*) |
| Day supply, median (IQR) | |||
| Opioid analgesic prescriptions, median (IQR) | |||
| Staten Island | 30 (10, 30) | 30 (10, 30) | 30 (10, 30) |
| Other New York City | 20 (5, 30) | 23 (5, 30) | 23 (5, 30) |
| Difference-in-differences regression,d B (95% CI) | |||
| Opioid analgesic prescriptions, B (95% CI) | |||
| BBorough | −0.4722 (−0.4818, −0.4625) | −0.4722 (−0.4818, −0.4625) | |
| BPostcampaign | −0.0826 (−0.0958, −0.0693) | −0.1135 (−0.1269, −0.1001) | |
| BBorough*postcampaign | −0.0115 (−0.0254, 0.0024) | −0.0035 (−0.0175, 0.0106) | |
| High-dose opioid analgesic prescriptions,c B (95% CI) | |||
| BBorough | −0.6662 (−0.6859, −0.6464) | −0.6652 (−0.6850, −0.6454) | |
| BPostcampaign | −0.0757 (−0.1026, −0.0488) | −0.1224 (−0.1496, −0.0951) | |
| BBorough*postcampaign | 0.0207 (−0.0078, 0.0492) | 0.0462 (0.0174, 0.0751) | |
Note. CI = confidence interval; IQR = interquartile range; MME = morphine milligram equivalent. Analysis includes Schedule II (excluding codeine-2) opioid analgesic prescriptions. Prescriptions written by veterinarians, written under institutional licenses, missing prescriber ID, or missing patient ID are excluded. Data are limited to New York City prescribers who wrote at least 1 opioid analgesic prescription from March 2013 to February 2014. Analysis is limited to prescribers with license location in the 5 New York City boroughs (counties). Staten Island is reported separately and compared with the other 4 boroughs combined (Bronx, Brooklyn, Manhattan, and Queens). The total number of Staten Island prescribers and other New York City prescribers represented in this table are 2529 and 38 871, respectively.
Source. New York State Bureau of Narcotics Enforcement, Prescription Monitoring Program, New York State, 2013–2014.
Rates are number of opioid analgesic prescriptions filled per 10 000 NYC residents. Age-adjusted rates are calculated using intercensal estimates updated December 2014, and are weighted to US Census Standard 2000.
Percent change between the precampaign period and postcampaign periods 1 and 2 were tested for Staten Island, and separately for the other NYC boroughs by using z-test comparisons.
A high-dose opioid analgesic prescription is greater than 100 MME. One MME is equivalent to 1 mg of morphine.
To compare rate changes over time between Staten Island and the other New York City boroughs, a difference-in-differences approach was taken; rate trends were tested using Poisson regression model with offset of person-time. Age was included in the model to control for confounding.
P < .05.
FIGURE 3—
Rate of Opioid Analgesic Prescriptions and High-Dose Prescriptions Filled by New York City Residents by Prescriber Location: New York City (NYC), March 2013–February 2014
Note. Analysis includes Schedule II (excluding codeine-2) opioid analgesic prescriptions. Prescriptions written by veterinarians, written under institutional licenses, missing prescriber ID, or missing patient ID are excluded. Data are limited to New York City prescribers who wrote at least 1 opioid analgesic prescription from March 2013 to February 2014. Analysis is limited to prescribers with license location in the 5 New York City boroughs (counties). Rates are number of opioid analgesic prescriptions filled per 10 000 New York City residents. Age-adjusted rates are calculated by using intercensal estimates updated December 2014, and are weighted to US Census Standard 2000. A high-dose opioid analgesic prescription is greater than 100 morphine milligram equivalents (MME). One MME is equivalent to 1 mg of morphine.
Source. New York State Bureau of Narcotics Enforcement, Prescription Monitoring Program, New York State, 2013–2014.
The high-dose prescribing rate in Staten Island decreased from 218 prescriptions per 10 000 New York City residents in the precampaign period to 191 prescriptions per 10 000 New York City residents in postcampaign period 2, a 12.4% decrease (P < .05). In the other 4 New York City boroughs, the high-dose prescribing rate decreased from 110 prescriptions per 10 000 New York City residents in the precampaign period to 102 prescriptions per 10 000 New York City residents in postcampaign period 2, a 7.3% decrease (P < .05; Table 2 and Figure 3). In difference-in-differences analysis comparing the precampaign period to postcampaign period 1, the interaction term did not differ from zero (B = 0.0207; 95% CI = −0.0078, 0.0492), demonstrating no significant difference in rate trends between Staten Island and the other New York City boroughs. However, in the difference-in-differences analysis comparing the precampaign period to postcampaign period 2, the interaction term differed from zero (B = 0.0462; 95% CI = 0.0174, 0.0751), indicating that rate trends in high-dose prescribing between Staten Island and the other New York City boroughs were significantly different at postcampaign period 2 (Table 2).
The median day supply in Staten Island was 30 (maximum allowable) in all study periods. In the other 4 New York City boroughs, the median day supply was 20 in the precampaign period and increased to 23 in both postcampaign periods (Table 2).
DISCUSSION
Evaluation of DOHMH’s public health detailing campaign to promote judicious opioid prescribing in Staten Island demonstrated an association with improvements in health care provider knowledge about opioid prescribing recommendations, and suggested a decrease in the rate of high-dose prescribing. To our knowledge, this is the first published study of a one-to-one detailing campaign about judicious opioid prescribing that both found an association with improvements in opioid analgesic–related knowledge and suggested a change in prescribing practices. This extends the findings of previously published studies on opioid analgesic detailing initiatives, which found changes in self-reported prescribing behavior, but did not include prescribing data.13,14 Like these previous studies, our detailing campaign was conducted in the context of a multipronged public health response.
The smallest increase in knowledge was observed for the recommendation related to insufficient evidence for use of opioids to treat chronic noncancer pain. This finding likely reflects the extensive promotion and use of opioids for chronic noncancer pain in the United States in the past.17,18 Only recently have several studies highlighted the lack of evidence for pain relief or improved function from long-term opioid use for chronic noncancer pain.17,19–22 Repeated dissemination of these findings and of evidence-based clinical guidelines such as the DOHMH prescribing guidelines for opioids is warranted to promote practices consistent with scientific evidence.
The greater decrease in the rate of high-dose prescribing in Staten Island compared with the other New York City boroughs was plausibly influenced by the public health detailing campaign. To our knowledge, the detailing campaign in Staten Island was the only source of specific information regarding high-dose prescribing and MMEs that was disseminated in New York City during the study period. Furthermore, concurrent messaging on opioids in the media and related to I-STOP did not address high-dose prescribing during this time period. The magnitude of decrease in the rate of high-dose prescribing did not reach statistical significance until postcampaign period 2. This lag might be attributable to the time it took for prescriber behavior to become engrained, or the time needed to taper down high-dose prescriptions.
The lack of decrease in median day supply per prescription in Staten Island and the increase in the other New York City boroughs were unexpected and concerning. This finding might reflect increased use of opioids to treat chronic pain (which would be inconsistent with the detailing campaign messages); alternatively, this finding could also be observed if the number of prescriptions for acute pain decreased disproportionately to the decrease in the number of prescriptions for chronic pain. Future research should explore systems-level strategies as mechanisms to decrease median day supply, including default settings for opioid prescriptions in electronic health records and prior authorization policies consistent with judicious opioid-prescribing principles.
The fact that overall prescribing rates decreased across all New York City boroughs is favorable for the public health of New Yorkers. This trend might reflect implementation of the I-STOP law requiring review of patient PMP data before prescribing a controlled substance, or, perhaps, might signal an increased general awareness about opioid analgesic–associated risks, given the increasing attention to this topic up to the national level.16,23
Public health interventions regarding opioid analgesics should be considered in the context of heroin because opioid analgesics and heroin are chemically similar, their epidemiological trends are potentially intertwined, and certain interventions can address both (e.g., medication-assisted treatment and naloxone). In a separate analysis, we found a 29% decrease from 2011 to 2013 in the opioid analgesic overdose mortality rate in Staten Island compared with the other 4 New York City boroughs, after DOHMH’s multipronged opioid analgesic public health response. During the same period, heroin overdose mortality rates increased similarly in both Staten Island and the other 4 New York City boroughs, while the opioid analgesic overdose mortality rate in the other 4 New York City boroughs did not change.15
A practical challenge of planning the detailing campaign was that no up-to-date, comprehensive list of health care providers in Staten Island was available for DOHMH to use. We used the free, publically available National Provider Identifier Registry; this information was imperfect, as health department representatives identified and detailed health care providers that met our criteria for targeting, but had not been detected through the National Provider Identifier Registry. The challenge of reliably identifying and locating health care providers was exacerbated by the timing of the detailing campaign, which was conducted less than 1 year after Hurricane Sandy, when Staten Islanders were still recovering from storm damage. Upon arrival, health department representatives encountered office practices under repair or closed because of storm damage; in addition, some health care providers had reduced work hours or were temporarily working from 2 locations because of rebuilding efforts. Lacking access to a gold-standard list of practicing health care providers is not unique to this intervention, and reflects a broader problem faced by public health that limits program planning targeting health care providers (S. C. Shih, written communication, April 2016). Despite this challenge, we detailed close to the number of health care providers targeted.
This study had several limitations. First, the evaluation of knowledge change about prescribing recommendations did not have a nondetailed comparison group because identifying an appropriate comparison group was not feasible (the majority of health care providers who met our inclusion criteria in Staten Island were detailed, leaving few nondetailed health care providers). However, the paired analysis accounted for individual change in responses from pre- to posttest.
Second, prescribing patterns for Staten Island prescribers who were detailed could not be compared with nondetailed Staten Island prescribers because PMP data used for analysis were de-identified. Our approach strengthens the study findings, because inclusion of all Staten Island prescribers biases the results toward the null as not all prescribers received the intervention.
Third, the widespread attention on the risks of opioid analgesics in Staten Island and on I-STOP implementation statewide precludes definitive attribution of knowledge and overall prescribing changes to the public health detailing campaign. However, we hypothesize that the observed knowledge changes and greater decreases in high-dose prescribing in Staten Island were influenced by the public health detailing campaign because, to our knowledge, the Staten Island detailing campaign along with the kick-off physician conferences at 2 Staten Island hospitals were the only sources of specific messaging about DOHMH prescribing recommendations during the study period. This messaging included technical information regarding high-dose prescribing and MMEs, which is not common knowledge to health care providers (as evidenced by the low percentage [22%] of baseline survey respondents correctly answering the question about high-dose prescribing). These factors increase the plausibility that the greater decreases in high-dose prescribing in Staten Island were influenced by the detailing campaign.
Finally, an assessment of opioid analgesic and heroin overdose mortality using the same analytic periods as for the prescribing data analysis used in this study was not possible because of small borough-level numbers and unstable rate estimates.
In conclusion, this study demonstrated that a public health detailing campaign can improve health care provider knowledge about opioid prescribing practices and might change specific prescribing behavior. With national rates of opioid analgesic overdose deaths continuing at epidemic levels, and the recent release of the Centers for Disease Control and Prevention’s national guidelines for judicious opioid prescribing, an urgency exists to help health care providers change prescribing practices.8,24 Public health detailing could be considered by other jurisdictions as a strategy to promote judicious opioid prescribing, particularly in high-risk areas. Together with a comprehensive public health approach to address opioid analgesic misuse and overdose, prescriber detailing might play a critical role in reducing morbidity and mortality related to opioids.
ACKNOWLEDGMENTS
This study was supported in part by funding from the Centers for Disease Control and Prevention under CDC-RFA-HM08-805.
We would like to acknowledge Vibhuti Arya, Daniella Bradley O’Brien, Magda Desdunes, Marissa Kaplan-Dobbs, Michelle Dresser, Sungwoo Lim, Colleen Mccullough, Kimberly Sebek, Sarah Chen-Ju Shih, Leslie Short, of the New York City Department of Health and Mental Hygiene at the time of the study; and the OnCall detailing team.
Note. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
HUMAN PARTICIPANT PROTECTION
The New York City Department of Health and Mental Hygiene institutional review board determined this study to be program evaluation.
REFERENCES
- 1.Centers for Disease Control and Prevention. CDC grand rounds: prescription drug overdoses—a U.S. epidemic. MMWR Morb Mortal Wkly Rep. 2012;61(1):10–13. [PubMed] [Google Scholar]
- 2.Paone D, Tuazon E, Nolan M, Bradley O’Brien D. Unintentional drug poisoning (overdose) deaths in New York City, 2000–2012. Queens, NY: New York City Department of Health and Mental Hygiene; 2013. Epi Data Brief No. 33.
- 3.Centers for Disease Control and Prevention. Vital signs: overdoses of prescription opioid pain relievers—United States, 1999–2008. MMWR Morb Mortal Wkly Rep. 2011;60(43):1487–1492. [PubMed] [Google Scholar]
- 4.Dunn KM, Saunders KW, Rutter CM et al. Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med. 2010;152(2):85–92. doi: 10.1059/0003-4819-152-2-201001190-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bohnert AS, Valenstein M, Bair MJ et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315–1321. doi: 10.1001/jama.2011.370. [DOI] [PubMed] [Google Scholar]
- 6.Paulozzi LJ, Zhang K, Jones CM, Mack KA. Risk of adverse health outcomes with increasing duration and regularity of opioid therapy. J Am Board Fam Med. 2014;27(3):329–338. doi: 10.3122/jabfm.2014.03.130290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tuazon E, Levin D, Bradley O’Brien D, Paone D. Patterns of opioid analgesic prescriptions for New York City Residents. Queens, NY: New York City Department of Health and Mental Hygiene; 2013. Epi Data Brief No. 32.
- 8.Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. MMWR Recomm Rep. 2016;65(1):1–49. doi: 10.15585/mmwr.rr6501e1. [DOI] [PubMed] [Google Scholar]
- 9.Paone D, Dowell D, Heller D. Preventing misuse of prescription opioid drugs. City Health Information. 2011;30(4):23–30. Available at: http://www1.nyc.gov/assets/doh/downloads/pdf/chi/chi30-4.pdf. Accessed June 17, 2016. [Google Scholar]
- 10.Larson K, Levy J, Rome MG, Matte TD, Silver LD, Frieden TR. Public health detailing: a strategy to improve the delivery of clinical preventive services in New York City. Public Health Rep. 2006;121(3):228–234. doi: 10.1177/003335490612100302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dresser MG, Short L, Wedemeyer L et al. Public health detailing of primary care providers: New York City’s experience, 2003–2010. Am J Public Health. 2012;102(suppl 3):S342–S352. doi: 10.2105/AJPH.2011.300622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thomson O’Brien MA, Oxman AD, Davis DA, Haynes RB, Freemantle N, Harvey EL. Educational outreach visits: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2000;(2):CD000409. doi: 10.1002/14651858.CD000409. [DOI] [PubMed] [Google Scholar]
- 13.Cochella S, Bateman K. Provider detailing: an intervention to decrease prescription opioid deaths in Utah. Pain Med. 2011;12(suppl 2):S73–S76. doi: 10.1111/j.1526-4637.2011.01125.x. [DOI] [PubMed] [Google Scholar]
- 14.Albert S, Branson FW, Sanford CK, Dasgupta N, Graham J, Lovette B. Project Lazarus: community-based overdose prevention in rural North Carolina. Pain Med. 2011;12(suppl 2):S77–S85. doi: 10.1111/j.1526-4637.2011.01128.x. [DOI] [PubMed] [Google Scholar]
- 15.Paone D, Tuazon E, Kattan J et al. Decrease in rate of opioid analgesic overdose deaths—Staten Island, New York City, 2011–2013. MMWR Morb Mortal Wkly Rep. 2015;64(18):491–494. [PMC free article] [PubMed] [Google Scholar]
- 16.New York State Office of Alcoholism and Substances Abuse Services. Internet System for Tracking Over-Prescribing (I-STOP) Act. Available at: http://www.oasas.ny.gov/StopRxMisuse/ISTOP.cfm. Accessed June 22, 2016.
- 17.Trescot AM, Glaser SE, Hansen H, Benyamin R, Patel S, Manchikanti L. Effectiveness of opioids in the treatment of chronic non-cancer pain. Pain Physician. 2008;11(2) suppl:S181–S200. [PubMed] [Google Scholar]
- 18.Van Zee A. The promotion and marketing of Oxycontin: commercial triumph, public health tragedy. Am J Public Health. 2009;99(2):221–227. doi: 10.2105/AJPH.2007.131714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martell BA, O’Connor PG, Kerns RD et al. Systematic review: opioid treatment for chronic back pain: prevalence, efficacy, and association with addiction. Ann Intern Med. 2007;146(2):116–127. doi: 10.7326/0003-4819-146-2-200701160-00006. [DOI] [PubMed] [Google Scholar]
- 20.Manchikanti L, Ailinani H, Koyyalagunta D. A systematic review of randomized trials of long-term opioid management for chronic non-cancer pain. Pain Physician. 2011;14(2):91–121. [PubMed] [Google Scholar]
- 21.Furlan AD, Sandoval JA, Mailis-Gagnon A et al. Opioids for chronic noncancer pain: a meta-analysis of effectiveness and side effects. CMAJ. 2006;174(11):1589–1594. doi: 10.1503/cmaj.051528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Noble M, Treadwell JR, Tregear SJ. Long-term opioid management for chronic noncancer pain. Cochrane Database Syst Rev. 2010;(1):CD006605. doi: 10.1002/14651858.CD006605.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Department of Health and Human Services. HHS takes strong steps to address opioid-drug related overdose, death and dependence. Available at: http://www.hhs.gov/about/news/2015/03/26/hhs-takes-strong-steps-to-address-opioid-drug-related-overdose-death-and-dependence.html. Accessed April 7, 2016.
- 24.Centers for Disease Control and Prevention. National Center for Health Statistics, National Vital Statistics System, Mortality File. Number and age-adjusted rates of drug-poisoning deaths involving opioid analgesics and heroin: United States, 2000–2014. Available at: http://www.cdc.gov/nchs/data/health_policy/AADR_drug_poisoning_involving_OA_Heroin_US_2000-2014.pdf. Accessed April 11, 2016.