Abstract
Medical intelligence, security and global health are distinct fields that often overlap, especially as the drive towards a global health security agenda gathers pace. Here, we outline some of the ways in which this has happened in the recent past during the recent Ebola epidemic in West Africa and in the killing of Osama Bin laden by US intelligence services. We evaluate medical intelligence and the role it can play in global health security; we also attempt to define a framework that illustrates how medical intelligence can be incorporated into foreign policy action in order delineate the boundaries and scope of this growing field.
Keywords: Medical intelligence, security, global health
Intelligence, security and global health are distinct conceptual domains with a long history of overlapping priorities and, often, clashing interests. In the last few years, the interfaces of these sectors have been very much prominent in the public arena as disease and insecurity have become increasingly intertwined in a globalised system. From the securitisation of diseases such as Ebola or Severe Acute Respiratory Syndrome (SARS), to exploiting public health programmes in Pakistan for military gains, these fields have experienced an uneasy association as disparate agendas find themselves aligned in activity and outcome. A clear framework must be outlined to ensure the fields of health, security and intelligence can coexist and overlap harmoniously. We aim to outline such a framework here.
Methods
An extensive literature review was carried out of the health and security literatures in peer-reviewed journals and media sources, as well as open source intelligence documents from various national and international agencies. This literature review formed the empirical basis for the formulation of the Medical Intelligence Framework proposed in the paper, which was arrived at through case-study analysis and discussion between the authors.
William McNeil described disease as ‘the hidden hand throughout history’.1 As global populations become ever more linked, health risks to one person rapidly become health risks to entire populations, directly influencing geopolitics and national security.2 Securitisation theory can illuminate the political moves that elevate health concerns to global security threats, particularly as defined by the Copenhagen School as the identification of an existential threat to a referent object such as the state, population or global networks of power, i.e. markets.16 In this framing, securitisation is a condition of designation by elites rather than a fundamental state of threat. State actors have become increasingly receptive to the concept of disease securitisation, encouraging the development of national bodies established for the purpose of medical intelligence within military and civilian organisations. Indeed, during the process of determining the sustainable development goals, a proposition was made for a goal on Global Health Security. The proposed sustainable development goal 18 was formulated as follows: ‘Take appropriate action to reduce the vulnerability of people around the world to new, acute, or rapidly spreading risks to health, particularly those threatening to cross international borders’.5 Although it was not adopted, this proposition highlights the growing agenda to integrate security into modern conceptions of global health.
Policymakers have recognised the destabilising threat that infectious disease and health system failures have on peace and global stability (Kaufman, 2001). The motives for securitising disease have largely been based on the ability of disease outbreaks to compromise the relative power of a state, particularly during periods of conflict.2 This motive adds a further layer of complexity to the normative definitions of security as a form of emancipation that is broadly in line with definitions of global health posited by Sen and Koplan with their focus on freedom and health equity.6,7 By this definition, almost any condition of ill-health could justify securitisation due to its ability to impair human capabilities; however, in practice the rationale for securitising has not been focused on disease-affected communities, rather its perceived threat to the global community.2 A useful term to define which health threats should be securitised can be borrowed from the WHO. A Public Health Emergency of International Concern refers to an extraordinary, unusual or unexpected event that has a serious and potentially international public health impact.9 This definition allows common and expected diseases to be disregarded and instead focuses on deadly diseases with the potential to cause mass harm internationally.
Medical intelligence represents a critical intelligence capability (Kaufman, 2001) to monitor and evaluate risks to health within frameworks that either prioritise military considerations or form a significant component of national security interests. Medical intelligence is defined as follows:
That category of intelligence resulting from the collection, evaluation, analysis, and interpretation of foreign medical, bio-scientific, and environmental information which is of interest to strategic planning and to military medical planning and operations for the conservation of the fighting force and formation of assessments of foreign medical capabilities in both military and civilian sectors.4
It must be emphasised that this definition refers to intelligence assessments of the medical capabilities of a nation (i.e. health structures and infrastructures) rather than the ongoing dynamic assessment of current or potential disease outbreaks. However, both are important in contributing to securitisation.
Medical intelligence as defined by NATO is an intelligence rather than a medical function and may be operationalised for the benefit of national strategic interests. As a domain, it is relatively small within national intelligence structures, but important for its role in global surveillance systems; it is a sector that engages in activity directly relevant to global health, yet maintains firm priorities aligned with strategic security interests rather than any doctrine of health equity or humanitarian action. Nevertheless, this domain is notable for its scope to enhance the conditions and interests with which global health actors outside national security are interested. The role of the medical intelligence sector in the securitisation of disease has been particularly prominent given the particularities of infectious disease in provoking disease outbreaks affecting military operations, as well as communities and countries within which lie various strategic or foreign policy interests. The relatively novel idea that infectious disease cannot only perpetuate conflict, but also precipitate it, is changing the way that policymakers address health within their agendas.
In 2000, the US National Intelligence Council produced an unique report entitled ‘The Global Disease Threat and its Implications for the United States’, which was rapidly followed by a White House statement declaring HIV and emerging and re-emerging infectious diseases a national security threat (Kaufman, 2001).10 Diseases such as Ebola, HIV, multi-drug resistant tuberculosis and multi-drug resistant streptococci were named as direct threats to the USA rather than diseases that simply affected marginalised or far-away populations.
Military and civilian intelligence organisations, including medical institutions such as the Centers for Disease Control maintain disease surveillance systems that provide systematic assessments of abnormal health events such as the case rates of specific diseases, e.g. Ebola (Edit Confirmed, 2006). The work of medical intelligence structures aligned with national interests provides a core component of the health systems strengthening agenda that is fundamental to global health activity.
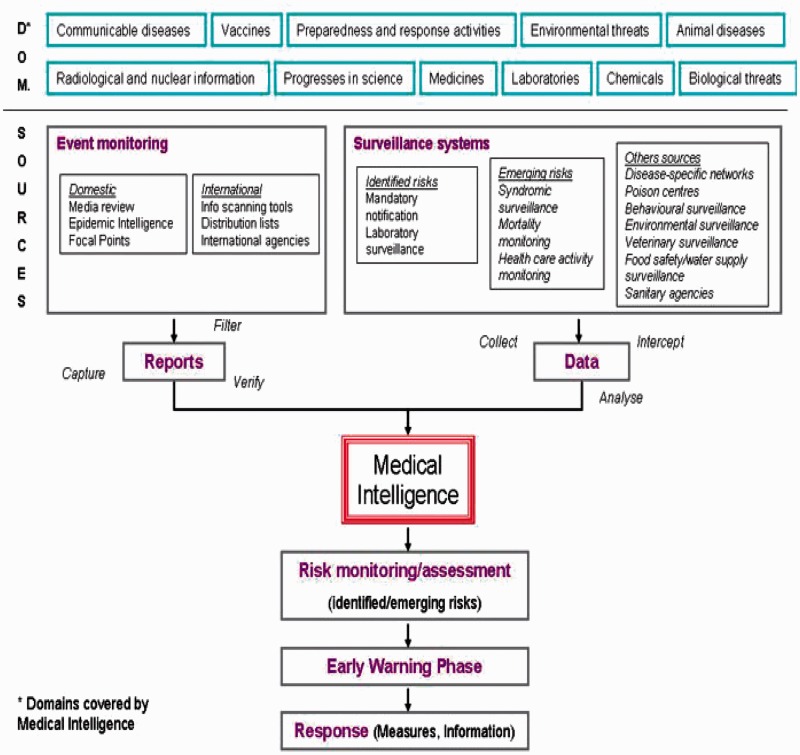
The clear interface of global health with intelligence structures is shown in Figure 1; communicable disease, vaccines, environmental threats, animal disease, medicines and laboratories have variously been implicated in a range of agendas from health system strengthening, universal health coverage, global health and national security agendas. In this framework, disease and epidemic intelligence is considered part of medical intelligence. This differs from the NATO definition of medical intelligence, which focuses primarily on health infrastructure assessment. The USA sites its National Center for Medical Intelligence within its Defence Intelligence Agency, placing the activities of disease surveillance firmly within the remit of military organisations. This trend towards militarisation raises ethical questions that challenge the interweaving of medical, security and foreign policy issues. The use of military intelligence in the process of securitisation minimises the ill-health of what are frequently the world’s poorest populations to a condition meriting attention purely on the basis of threat to armed elites, rather than a moral or ethical concern. Further, the designation of a disease security threat has the potential to legitimate the enactment of a state of exception, which may precipitate the blurring of ethical standards in the wake of an increasingly normalised paradigm of risk and threat.15
Figure 1.
European Commission – Medical Intelligence Framework.
The medical intelligence community has been heavily involved in evaluating the rapidly deteriorating security and health situation following the recent unprecedented Ebola outbreak in West Africa. The role of medical intelligence structures was to assess how likely the virus was to spread, what such a pattern of spread would look like, what its associated strategic threats would be, and what an appropriate response should involve.12 In September 2014, the NATO Health Surveillance Capability Branch took this activity one step further and called on NATO to integrate non-state-non-human actor threats into its Collective Defence doctrine, specifically in response to the unfolding Ebola emergency. This would be an important measure as it would lend legitimacy to the use of a NATO ‘collective response’ that is typically initiated following identified ‘threats to peace’ to support NATO force interventions.
The securitisation of disease through a national intelligence framework raises important questions similar to those that have arisen with civil/military health debates regarding the protection of the humanitarian/public health space. In the murky space of entanglements between military intelligence and medical NGOs, protections must be afforded to safeguard the humanitarian and public health spaces as a supposedly neutral good, especially when action is a consequence of a contested health securitisation agenda. Figure 2 proposes a medical intelligence pathway to limit the blurring of these boundaries.
Figure 2.
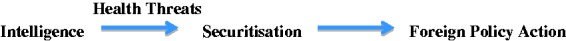
Medical intelligence pathway.
This sequence relies on health threats catalysing action within the securitisation agenda, with policy action occurring in response to such threats. The failure to adhere to this framework, for example in the killing of Osama Bin Laden in 2011, well demonstrates the adverse consequences associated with the infringement of the public health space and the blurring of foreign policy concerns with medical initiatives. The operation to locate and kill Osama Bin Laden took place by creating a fake childhood Hepatitis B immunisation programme in Abbottabad, Pakistan in order to confirm the presence of Bin Laden’s family members in the region.14 DNA samples were taken from the children of the city and compared to DNA from Bin Laden’s dead sister that was held by US intelligence services.13 Although the Hepatitis B campaign was entirely devised for intelligence purposes, the CIA has maintained that since the immunisations were real the programme can be considered to be a legitimate public health programme. Clearly, the boundaries between disease securitisation and intelligence activity were blurred and the global health community has raised grave concerns about the damage caused by the programme, which has led to the destruction of the already tenuous trust in public health measures throughout Pakistan and the wider region. The intelligence operation has resulted in a large-scale reduction in childhood vaccination uptake, with predictable damaging consequences for child health.13
The adoption of health as a tool for action by intelligence services in this context differs significantly from the schematic proposed earlier in Figure 2. In this instance, the constituent elements, although identical, result in an entirely different political frame (Figure 3).
Figure 3.
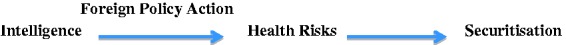
Intelligence pathway in the killing of Osama Bin Laden.
In a global health security agenda, the involvement of intelligence structures best occurs to anticipate and evaluate health risks, rather than, as seen in this instance, create them. Harmonising civil–military cooperation in complex humanitarian contexts has long been a cause for debate between the relevant actors. Involving national intelligence structures in a more prominent way within a broadly defined ‘security’ agenda creates a series of contested motives, roles and actions to be integrated into a Global Health Agenda. The implications for global health governance structures are likely to necessitate a greater embrace of securitisation by the WHO, especially as it seeks to demonstrate its relevance to donor nations in the aftermath of its much cited failures during the Ebola response. What this means in practice is, for better or worse, a greater alignment of global health strategy with national and trans-national intelligence sectors and their data sources such as the internet and social media. Non-governmental organisations such as Médecins Sans Frontières will protest the difficulty maintaining the perception of neutrality in this paradigm of global health, although in practice the operating challenges imposed may not differ substantively from existing civil/military concerns.
As the concept of a Global Health Security Agenda gains traction, the fields of intelligence and public health, in addition to the humanitarian community and the military, will necessarily have to accept a blurring of their respective discourses and a sharing of goals. There remain enormous challenges to be resolved in terms of defining and respecting each other’s spaces where it is most critical, while supporting cooperation in order to optimise shared goals.
Declarations
Competing Interests
None declared
Funding
None declared
Ethical approval
No ethical approval was required for this review as any data were from publicly available sources, and no patient specific data were required.
Guarantor
RS.
Contributorship
GB obtained the data from published sources and wrote the initial paper as part of a student selected module for her medical degree. GB then re-drafted and revised the manuscript with RS and CM; RS proposed the idea and supervised the project during the medical school student selected module. RS then re-drafted and amended the manuscript with GB and CM; CM re-drafted and amended the manuscript with GB and RS.
Acknowledgements
None.
Provenance
Not commissioned; peer-reviewed by Stuart Gordon.
References
- 1.McNeill WH. Plagues and Peoples, New York, NY: Anchor Press Doubleday, 1976. [Google Scholar]
- 2.Curley MG, Herrington J. The securitisation of avian influenza: international discourses and domestic politics in Asia. Rev Int Stud 2011; 37: 141–166. [Google Scholar]
- 3.Kaufman DC. Medical Intelligence: A Theatre Engagement Tool. Strategy Research Project, USA: Defense Intelligence Agency, 2001. [Google Scholar]
- 4.US Military Glossary. See http://usmilitary.about.com/library/glossary/blglossary.htm (last checked 1 February 2016).
- 5.Kickbusch I, Orbinski J, Winkler T, Schnabel A. We need a sustainable development goal 18 on global health security. Lancet Infect Dis 2015; 14: 257–257. [DOI] [PubMed] [Google Scholar]
- 6.Sen A. Development as Freedom, New Delhi, India: Oxford University Press, 1999. [Google Scholar]
- 7.Koplan JP. Towards a common definition of global health. Lancet 2010; 373: 1993–1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Enemark C. Disease and Security: Natural Plagues and Biological Weapons in East Asia, London: Routledge, 2007, pp. 8–8. [Google Scholar]
- 9.World Health Organization. International Health Regulations, 2nd edn Geneva: WHO, 2008. [Google Scholar]
- 10.National Intelligence Council. National Intelligence Estimate: The Global lnfectious Disease Threat and Its Implications for the United States. See http://www.cia.gov/cia/publications/nie/reponie99-17d.html (2000, last checked 1 February 2016). [PubMed]
- 11.European Commission. Health Preparedness Paper. See http://ec.europa.eu/health/preparedness_response/generic_preparedness/planning/medical_intelligence_en.htm (2006, last checked 1 February 2016).
- 12.NATO MILMEDCOE Deployment Health Surveillance Capability Branch. 2014 Ebola Outbreak West Africa Risk Assessment. Budapest: NATO Centre of Excellence for Military Medicine, 2014. http://www.coemed.org/images/stories/2014_12_23_dhsc_ebola_updates.pdf (last accessed 10 June 2016).
- 13.Deonandan R. The killing of bin Laden and the undermining of public health. Internet J Publ Health 2012; 2: 1–1. [Google Scholar]
- 14.Shah S. CIA organized fake vaccination drive to get Osama bin Laden’s family DNA. The Guardian, 11 July 2011. See http://www.guardian.co.uk/world/2011/jul/11/cia-fake-vaccinations-osama-bin-ladens-dna (last checked 1 February 2016).
- 15.Agamben G. State of Exception. Attell K (Trans.). Chicago, IL: University of Chicago Press, 2005.
- 16.McDonald R. Securitization and the construction of security. Eur J Int Relat 2008; 14: 4–4. [Google Scholar]