Highlights
-
•
Class E injuries are the most common major bile duct injuries and can cause serious clinical condition including bile leak.
-
•
Iatrogenic operative injuries may be a cause of spontaneous postoperative choledochoduodenal fistula even in transaction type complete injuries.
-
•
Spontaneous closure of a postoperative bile fistula doesn’t guarantee that it is not a transaction type injury.
Keywords: Laparoscopy, Cholecystectomy, Bile duct, Injury, Fistula, Duodenum
Abstract
Introduction
Bile leak after cholecystectomy which is the frequency less than 2% is an important problem for patients. Some bile duct injuries occuring after laparoscopic cholecystectomy are the complex bile duct injuries and can cause bile leak and fistula.
Presentation of case
A 74-year-old woman has high output bile drainage from abdominal drain after laparoscopic cholecystectomy so an ERCP was performed. It was clear that there was a complete transaction of bile ducts, however this finding was inconsistent with the patient’s clinical situation. The bile drainage of the patient was ceased and she was discharged to home without any problem. Four months later the patient was admitted again for recurrent cholangitis episodes. Patient was operated to perform a biliary-enteric diversion for the suspicion of biliary stricture. There was a thin fistula tract over the duodenum that was previously seperated from the proximal choledochus. The distal part of the bile duct was ended blindly. A hepaticojejunostomy anastomosis over a transhepatic stenting was performed.
Discussion
The circumferential injuries are the most common and devastating injuries leading to bile leak, peritonitis and varying degrees of sepsis. The probability of a bile fistula to close spontaneously is almost impossible in cases of iatrogenic circumferential full thickness injuries.
Conclusion
In the present case we have reported a case of Bismuth type 2 (Strasberg type E2) injury in which the biliary drainage was closed spontaneously with the formation of spontaneous biliary-duodenal fistula. It is an extremely interesting case that has not been reported in the literature previously.
1. Introduction
Laparoscopic approach has become standart treatment for gallstone disease because the recovery time is faster and the mortality rate is lower than open cholecystectomy [1]. Since it is less invasive, has shorter hospital stay and return to daily activity is faster, the patient satisfaction is high [2]. However there are several studies in literature reporting higher rates of bile duct injury and subsequent biliary sepsis after laparoscopic cholecystectomy (LC) [3], [4]. Up to 61% of the patient, bile duct injury is accompanied by major vascular injury mostly the right hepatic arterial system [5]. The outcome of the patient usually depends on the injury type, reoperation time, presence of extensive abdominal biliary sepsis and the physiological reserve of the patient. The circumferential injuries are the most common and devastating injuries leading to bile leak, peritonitis and varying degrees of sepsis. The surgeon who recognize a circumferential injury intraoperatively or early postoperative period, should convert the laparoscopy into open surgery and make a biliary-enteric anastomosis. Unfortunately only 20% of the surgeons who perform the LC are able to perform successful tension free biiary-enteric anastomosis [6], [7]. However in delayed cases with diffuse peritonitis, the surgeon should simply place adequate drains in the hilum and subhepatic space and wait for definitive reconstruction until the inflammation and bile sepsis are resolved and biliary drainage is managed in a controllable manner. It is almost impossible to cease the biliary drainage spontaneously in cases of iatrogenic circumferential full thickness injuries. In the present case we have reported a case of Bismuth type 2 (Strasberg type E2) injury in which the biliary drainage was closed spontaneously with the formation of spontaneous biliary-duodenal fistula. It is an extremely interesting case that has not been reported in the literature previously.
2. Case
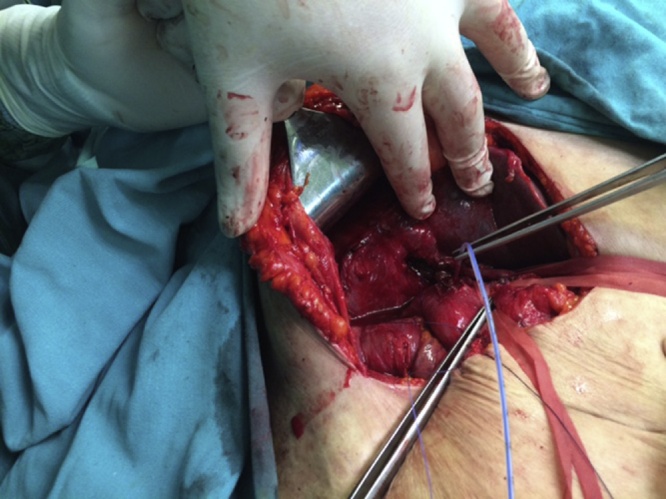
A 74-year-old woman with a history of laparoscopic cholecystectomy three days before was referred to our centre for high output bile drainage from abdominal drain. There were severe abdominal pain, distention, nausea and vomiting. The results of abdominal examination revealed abdominal tenderness and peritoneal irritation signs were positive. The patient had an abdominal drain in which the bile is leaking. She was found to have normal CBC (complete blood count) value. However the total and direct bilirubin values were 1.4/0.6 mg/dl (N. 0.3–0.12/0–0.3). Other biochemical tests were all in normal ranges. Ultrasound (USG) and computed tomography (CT) of the abdomen showed severe fluid collection in various parts of the abdominal cavity. A percutaneous drain was placed through the rectouterine space under USG guidance. Initially the daily output was between 600 and 1000 cc bile from both drains, so an ERCP was performed. Cholangiogram demonstrated complete duct obstruction at the mid-part of the choledochus, additionally proximal bile ducts and intrahepatic radicals couldn’t be visualized (Fig. 1). It was clear that there was a complete transaction of bile ducts (Bismuth type 1 or 2), however this finding was inconsistent with the patient’s clinical situation. Because following three weeks of supportive treatment, the bile drainage of the patient was ceased and she was discharged to home without any problem. Four months later the patient was admitted again for recurrent cholangitis episodes. On two dimensional coronal thick-slab MR cholangiopancreatogram, there were dilated intrahepatic bile ducts and abrupt termination at the level of confluence of the right and left biliary ducts in keeping with accidental ligation. The proximal 2 cm segment of the extrahepatic bile ducts is not visualized, while the distal portion of the common bile duct is normal (Fig. 2) (Strasberg type E2 injury). Based on these findings the patient was operated to perform a biliary-enteric diversion for the suspicion of biliary stricture. At operation it was found that duodenum was strictly adherent to the liver hilum and the hepatoduodenal structures. The duodenum was dissected away from the hilar structures. The proximal site of choledochus and duodenum were demonstrated and identified. The lumen of the proximal bile duct was determined near to the bifurcation. There was a thin fistula tract over the duodenum that was previously seperated from the proximal choledochus (Fig. 3). The distal part of the bile duct was dissected and cannulated proximally and found that it was ended blindly. These findings showed us that there was a spontaneous fistula formation between the duodenum and hilar side of the choledochus. The duodenum was repaired in two layers with absorbable sutures. A hepaticojejunostomy anastomosis over a transhepatic stenting was performed. The postoperative course of the patient was uneventful and she was discharged at 7th postoperative day and the transhepatic stent was removed at 3rd month.
Fig. 1.
Cholangiography demonstrating complete clippage of bile duct and non-visualization of proximal choledochus and intrahepatic ducts.
Fig. 2.
MR cholangiopancreatogram demonstrating grossly dilated intrahepatic bile ducts and abrupt termination at the level of confluence of the right and left biliary ducts.
Fig. 3.
Duodenal site of the choledochoduodenal fistula probing with 7 Fr catheter.
3. Discussion
The frequency of bile leak after cholecystectomy is less than 2% [8], [9]. The combined Strasberg-Bismuth system is the most commonly used classification for bile duct injury occured after laparoscopic cholecystectomy [5]. Class E injuries are circumferential injuries to the major hepatic ducts and are subdivided into 5 subgroups. These are the most common major bile duct injuries and can cause serious clinical condition including bile leak, fistula, sepsis, peritonitis and eventually biliary cirrhosis [5]. The patient in the present case had Class E2 biliary injury. Imaging is frequently critical to the early diagnosis of bile collection and treatment of such complication [10]. In our patient we obtained an abdominal CT, USG and found that there are extensive bile collection all around the abdominal cavity. So a percutaneous drain was placed through the rectouterine space under USG guidance.
The management of the patient with bile leak depends on the injury type, detection time and general condition of the patient. The spontaneous closure of the bile leak in such patients is actually just a hope, because they usually require urgent or elective repair. In our patient, although it was clear that there was a complete transaction of bile ducts, this finding was inconsistent with the patient’s clinical situation. Because following 3rd weeks of supportive treatment, the bile drainage of the patient was surprisingly decreased and she was discharged to home without any problem.
Since anatomic location of the injury dictates the treatment, early use of ERCP is essential to delineate the significant transaction type injury as well as to promote the closure of the others. The potential benefits of ERCP are to decrease the basal pressure of Oddi sphincter as well as crossing the leak site with the stent. A total of 2092 ERCP were performed in our unit so far and 4% of them were due to bile leak [11]. However five of them were transaction type circumferential biliary injury. Cholangiogram of the patient in the present case demonstrated complete duct obstruction at the mid-part of the choledochus, additionally proximal bile ducts and intrahepatic radicals couldn’t be visualized. Such kind of major injuries as in the present case are usually treated with biliary-enteric reconstruction after bile sepsis has subsided and the general condition of the patient is improved. This case indicates that iatrogenic operative injuries may be a cause of spontaneous postoperative choledochoduodenal fistula even in transaction type complete injuries. In the present case this fistulization fortunately caused the bile leak to cease which is a potentially fatal complication. We believe that bile produced inflammation in the abdominal cavity produced severe adhesion between proximal cut edge of bile duct and duodenum first and then connection between them [12]. But the fistulization healed with stricture formation at late period four months later characterizing with recurrent cholangitis episodes. Different radiological interventions can be performed to diagnose the benign strictures depending on the clinician’s preference. But the diagnostic accuracy of the MRCP is relatively high as compared to CT and USG in postoperative benign strictures [13]. In our case MRCP precisely demonstrated the stricture formation at the bifurcation level and the non visualisation of 2 cm length subsequent bile duct through duodenum.
In summary the consequence of the inflammatory process was a choledochoduodenal fistula and a postinflammatory stricture formation then. If the patient remained asymptomatic, she wouldn’t be treated. But the patient’s complaints were due to recurrent cholangitis, so the definitive repair became necessary. So the spontaneous closure of a postoperative bile fistula doesn’t guarantee that it is not a transaction type injury. ERCP and MRCP findings should be kept in mind always in combining with patient’s clinical situation.
Conflicts of interest
We have no conflict of interest to declare.
Funding
We have no funding for our research.
Ethical approval
Our paper contains a case report so we have no ethical approval.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Sezgin Yılmaz: writing the paper.
Murat Akıcı: data collection.
Nazan Okur: data analysis.
Ogün Erşen: corresponding author and design.
Serkan Türel: study concept.
Enes Şahin: design.
Guarantor
Prof. Sezgin Yılmaz, MD.
References
- 1.Hannan E.L., Imperato P.J., Nenner R.P., Starr H. Laparoscopic and open cholecystectomy in New York State: mortality, complications, and choice of procedure. Surgery. 1999;125(2):223–231. [PubMed] [Google Scholar]
- 2.Holohan T.V. Laparoscopic cholecystectomy. Lancet. 1991;338(8770):801–803. doi: 10.1016/0140-6736(91)90678-i. [DOI] [PubMed] [Google Scholar]
- 3.Cox M.R., Wilson T.G., Jeans P.L., Padbury R.T., Toouli J. Minimizing the risk of bile duct injury at laparoscopic cholecystectomy. World J. Surg. 1994;18(3):422–426. doi: 10.1007/BF00316827. [DOI] [PubMed] [Google Scholar]
- 4.Ferguson C.M., Rattner D.W., Warshaw A.L. Bile duct injury in laparoscopic cholecystectomy. Surg. Laparosc. Endosc. 1992;2(March (1)):1–7. [PubMed] [Google Scholar]
- 5.McKenzie S., Schwartz R. The management of bile duct injuries occurring during laparoscopic cholecystectomy. Curr. Surg. 2006;63(1):20–23. doi: 10.1016/j.cursur.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 6.Schmidt S.C., Langrehr J.M., Hintze R.E., Neuhaus P. Long-term results and risk factors influencing outcome of major bile duct injuries following cholecystectomy. Br. J. Surg. 2005;92(1):76–82. doi: 10.1002/bjs.4775. [DOI] [PubMed] [Google Scholar]
- 7.Stewart L., Way L.W. Bile duct injuries during laparoscopic cholecystectomy: factors that influence the results of treatment. Arch. Surg. 1995;130(10):1123–1128. doi: 10.1001/archsurg.1995.01430100101019. [DOI] [PubMed] [Google Scholar]
- 8.Kaffes A.J., Hourigan L., De Luca N., Byth K., Williams S.J., Bourke M.J. Impact of endoscopic intervention in 100 patients with suspected postcholecystectomy bile leak. Gastrointest. Endosc. 2005;61(2):269–275. doi: 10.1016/s0016-5107(04)02468-x. [DOI] [PubMed] [Google Scholar]
- 9.McMahon A.J., Fullarton G., Baxter J.N., O’Dwyer P.J. Bile duct injury and bile leakage in laparoscopic cholecystectomy. Br. J. Surg. 1995;82(3):307–313. doi: 10.1002/bjs.1800820308. [DOI] [PubMed] [Google Scholar]
- 10.Greenfield N.P., Azziz A.S., Jung A.J., Yeh B.M., Aslam R., Coakley F.V. Imaging late complications of cholecystectomy. Clin. Imaging. 2012;36(6):763–767. doi: 10.1016/j.clinimag.2012.01.024. [DOI] [PubMed] [Google Scholar]
- 11.Yilmaz S., Ersen O., Ozkececi T., Turel K.S., Kokulu S., Kacar E. Results of the open surgery after endoscopic basket impaction during ERCP procedure. World J. Gastrointest. Surg. 2015;7(2):15–20. doi: 10.4240/wjgs.v7.i2.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maier J., Rudez J., Huber A. Two possibly iatrogenic biliary-duodenal fistulas in a single patient after medical and surgical interventions. Can. J. Surg. 2008;51(2):E28–E29. [PMC free article] [PubMed] [Google Scholar]
- 13.Singh A., Mann H.S., Thukral C.L., Singh N.R. Diagnostic accuracy of MRCP as compared to ultrasound/CT in patients with obstructive jaundice. J. Clin. Diagn. Res. 2014;8(3):103–107. doi: 10.7860/JCDR/2014/8149.4120. [DOI] [PMC free article] [PubMed] [Google Scholar]