Highlights
-
•
Nonbacterial thrombotic endocarditis (NBTE) is a rare complication of cancer.
-
•
NBTE may precede the diagnosis of an occult gynecologic malignancy.
-
•
Malignancy-induced NBTE must be considered in patients with unprovoked venous thromboembolism.
-
•
The most effective treatment is anticoagulation and treatment of the underlying cancer.
Keywords: Endocarditis, Valvular vegetations, Ovarian cancer, Endometrial cancer, Anticoagulation, Chemotherapy
1. Introduction
Nonbacterial thrombotic endocarditis (NBTE) is often discovered at the time of autopsy or in late-stage malignancies, limiting the information available about the clinical course of patients with this syndrome. The most common malignancies associated with NBTE are lung, pancreatic, gastric cancer and adenocarcinomas of an unknown primary site (el-Shami et al., 2007). In gynecologic malignancies, NBTE is most commonly reported in ovarian cancer (Delgado and Smith, 1975). Our case is unique not only because the patient survived an event of NBTE with synchronous primary ovarian and endometrial cancer but also because the actual clinical manifestation that prompted a cardiac workup was not related to the NBTE.
2. Case
A 63-year-old menopausal woman presented with new onset of severe dyspnea on exertion and chest tightness. The electrocardiogram (EKG) revealed T-wave inversion and the cardiac troponins were elevated. She was treated for acute coronary syndrome while a 2-dimensional echocardiogram and cardiac catheterization did not show structural abnormalities or ischemia. Due to persistent dyspnea, a Computed Tomography Angiography (CTA) of the chest was performed which revealed small peripheral pulmonary emboli bilaterally and treatment with rivaroxaban (Xarelto) was initiated.
After completing three weeks of treatment with rivaroxaban, the patient experienced her first episode of postmenopausal bleeding. A pelvic ultrasound revealed a 10.4 × 6.0 × 6.4 cm uterus, with endometrial thickening measuring 3.2 cm and a complex endometrial mass measuring 1.0 × 2.1 × 1.7 cm. In addition, contiguous with the fundus of the uterus was a complex mass measuring 11.0 × 11.0 × 12.3 cm. The ovaries were not visualized bilaterally. Computed Tomography (CT) of the abdomen and pelvis confirmed the sonographic findings. An endometrial biopsy was attempted, however, final pathology revealed insufficient tissue.
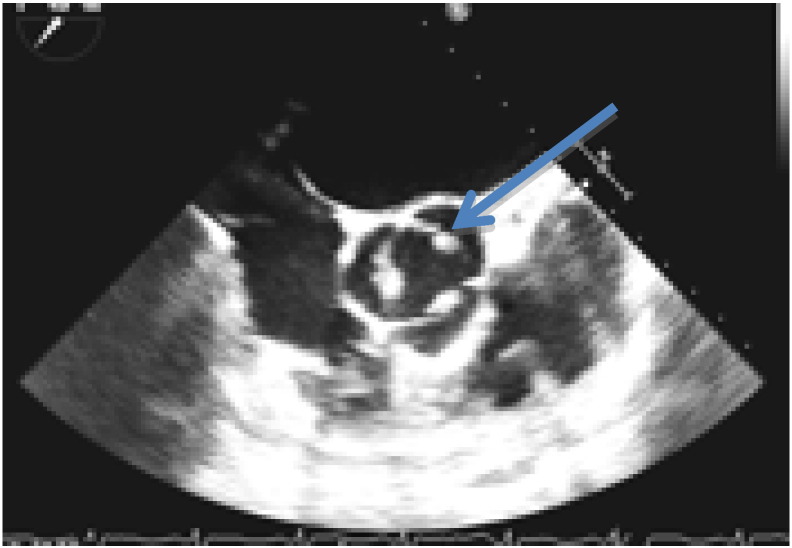
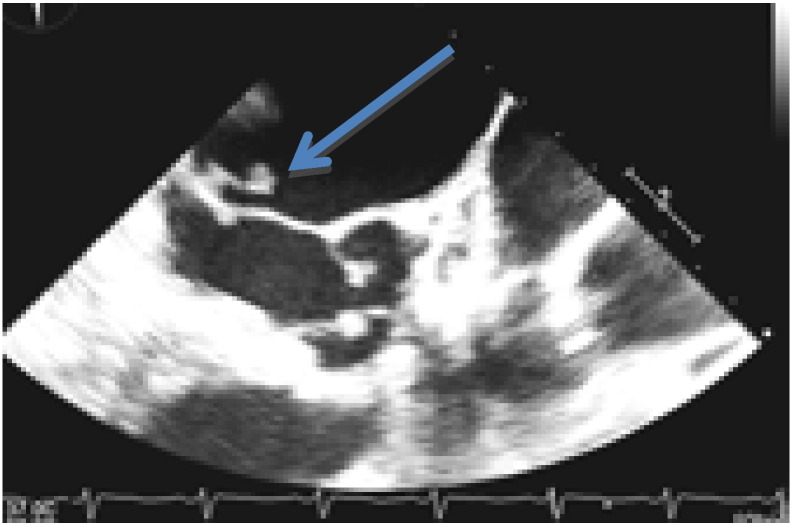
Due to the high suspicion of malignancy the patient was transferred to a tertiary medical center for a gynecologic oncology consultation. Given the recent history of a pulmonary embolism, a Doppler of the lower extremities was obtained and deep vein thrombosis was ruled out. A chest X-ray showed cardiomegaly while the EKG demonstrated normal sinus rhythm with left axis deviation, left ventricular hypertrophy and nonspecific ST segment abnormalities. A transthoracic echocardiogram showed a trileaflet aortic valve with an echodensity suggestive of prominent vegetations visible on at least two leaflets of the aortic valve (Fig. 1). Moreover, there was mild anterior and posterior mitral leaflet thickening and suspicion of thickening of the tricuspid valve, although not well defined (Fig. 2). A transesophageal echocardiogram confirmed the presence of aortic and mitral valve vegetations.
Fig. 1.
Transthoracic echocardiography (TTE) showing focal thickening on the right coronary cusp and non-coronary cusp of the aortic valve (arrow).
Fig. 2.
Transthoracic echocardiography (TTE) showing anterior and posterior mitral leaflet thickening (arrow).
The physical examination revealed a grade I/VI systolic heart murmur but no peripheral signs of infectious endocarditis. Serial blood cultures were collected which were negative. As the infectious workup was negative, patient was started on a heparin algorithm for NBTE. Lupus anticoagulant antibodies, cardiolipin antibodies, Beta 2 glycoprotein antibodies, protein S, protein C, antithrombin III and Factor V Leiden levels were all normal. In the presence of a pelvic mass, elevated carbohydrate antigen (CA) 125 and carcinoembryogenic antigen and a normal colonoscopy, it was concluded that the patient's cardiac vegetations were most likely related to an undiagnosed gynecologic malignancy and the decision was made to proceed to an exploratory laparotomy.
Due to increased risk of systemic emboli, a retrievable inferior vena cava (IVC) filter was placed preoperatively. The patient underwent exploratory laparotomy that revealed a large left ovarian mass with frozen section consistent with an invasive malignancy. Surgical staging and optimal cytoreduction were achieved. On postoperative day three the patient was transitioned from the heparin algorithm to a weight-based regimen with enoxaparin. Final pathology revealed a left ovarian high grade papillary serous adenocarcinoma extending into the pelvic sidewall with positive pelvic washings, the right ovary had clusters of atypical cells consistent with a serous adenocarcinoma as well and the uterus revealed a focus of well differentiated endometrioid adenocarcinoma of the endometrium. Consensus decision of the tumor board regarding the diagnosis of the patient was stage IIC ovarian serous adenocarcinoma with synchronous stage IA endometrial adenocarcinoma (based on the International Federation of Obstetricians and Gynecologists staging system).
The patient completed six cycles of dense dose paclitaxel and carboplatin with a good response. Prior to the fourth cycle of chemotherapy, a repeat transthoracic echocardiogram demonstrated complete resolution of aortic and mitral valve vegetations (Fig. 3). Six months after completion of full dose anticoagulation treatment with enoxaparin, a repeat CTA of chest showed resolution of prior pulmonary emboli lesions. The IVC filter was removed and the patient was transitioned to prophylactic enoxaparin for an additional six months. At two- year follow-up, her CA125 has normalized, there is no radiographic evidence of disease recurrence and she has not had any further thromboembolic events.
Fig. 3.
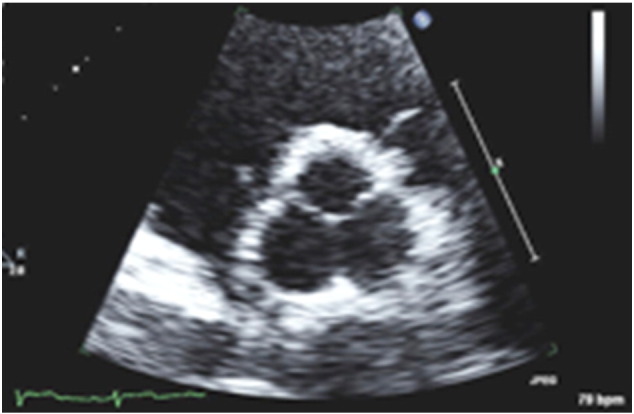
Transesophageal echocardiogram (TTE) post debulking and chemotherapy showing resolution of previous aortic valve vegetations.
3. Discussion
In the 1860s Dr. Armand Trousseau described a malignancy-induced hypercoagulable state predisposing patients with cancer to thromboembolic phenomena, eponymously named Trousseau's syndrome. Nonbacterial thrombotic endocarditis, formerly known as marantic endocarditis stemming from the Greek word μαραντικός (marantikos) which means “wasting away,” is a subset of Trousseau's syndrome and manifests most frequently in autoimmune hypercoagulable states and secondarily in malignancy (el-Shami et al., 2007).
Malignancy-induced NBTE is characterized by sterile small vegetations composed of fibrin and platelet aggregates that lack bacteria and inflammation. The platelet/fibrin aggregates often adhere to undamaged valves with a propensity for the left heart valves, mitral more than aortic. The exact pathogenesis is not entirely elucidated, but it is thought that macrophages and monocytes release immunologic factors that damage the endothelium leading to thrombus formation. The lack of cellular organization makes the vegetations quite friable and easily embolizable (Delgado and Smith, 1975, Aryana et al., 2006).
The definitive diagnosis of NBTE is made by obtaining a pathologic specimen surgically or upon autopsy. However, procurement of a cardiac specimen is often unrealistic. Therefore, the diagnosis is usually made based on clinical and echocardiographic evidence, in the absence of infectious findings. New significant murmurs and valvular destruction in NBTE are uncommon, which can distinguish it from infectious endocarditis. Symptoms of systemic or pulmonary embolization appear to be the most common complication that lead to a search and diagnosis of NBTE. When there is a high index of suspicion, transthoracic followed by transesophageal echocardiography should be performed to assess for vegetations (el-Shami et al., 2007, Aryana et al., 2006).
NBTE associated with gynecologic malignancy has been described infrequently and in most of the cases the diagnosis was made postmortem (Delgado and Smith, 1975). Three previously published cases have shown an association between NBTE and ovarian clear cell carcinoma (Aryana et al., 2006, Devulapalli et al., 2012). Two patients were diagnosed with NBTE after a systemic embolization to multiple organs and one following a cerebrovascular accident. In the latter case, the patient was treated with enoxaparin while workup revealed progression of disease. An unusual presentation combining NBTE, paraneoplastic cerebellar degeneration and systemic emboli was reported that lead to the diagnosis of ovarian adenocarcinoma (Singh et al., 2007). The patient was treated with heparin and passed away three weeks later. A case of infectious endocarditis superimposed on NBTE with synchronous endometrioid ovarian and endometrial adenocarcinoma was described in 2006 (Numnum et al., 2006). In that case, despite resolution of NBTE on warfarin, the patient's prognosis was very poor due to metastatic disease. Another recently published case report with synchronous ovarian and endometrial cancer describes a patient with massive pulmonary embolism who subsequently experienced neurological manifestations prompting workup that revealed acute ischemic cerebral lesions and NBTE (Erturk et al., 2015). Finally, isolated cases of ovarian cancer complicated by NBTE with disseminated intravascular coagulation have also been described in literature (Tanaka et al., 2009).
Our patient's clinical presentation is unique as her initial pulmonary embolism was not a complication of NBTE, indeed her echocardiogram at that time was normal. Notably, our patient's NBTE was diagnosed almost a month after the episode of the pulmonary embolism despite being on anticoagulation treatment. It was not until vaginal bleeding raised the suspicion of an underlying malignancy that lead to a more comprehensive workup with a subsequent echocardiogram revealing the NBTE.
Despite the poor prognosis of NBTE, our patient improved dramatically due to the aggressive and prompt treatment with immediate initiation of systemic anticoagulation, optimal surgical debulking and systemic chemotherapy. While the optimal anticoagulation has not yet been determined, current recommendations of systemic anticoagulation with low molecular weight heparin or unfractionated heparin have proven most effective (Whitlock et al., 2012). Although no trial has compared heparin versus warfarin, reports indicate a higher recurrence of thromboembolic events on warfarin in cancer patients (Lee et al., 2003).
Finally, screening guidelines for patients with unprovoked venous thromboembolisms are not entirely clear. A recent study showed that screening with full body CT scan imaging for occult cancer in unprovoked thromboembolisms did not provide clinically significant benefit. However, the study included men and women over the age of 18 years (Carrier et al., 2015). It would be interesting to see the clinical benefit of imaging with less invasive modalities, such as ultrasound, in a population similar to our patient i.e. female and above the age of 40.
4. Conclusion
In the female population, a thromboembolic event may precede the diagnosis of an occult gynecologic malignancy or indicate progression of disease. The diagnosis and treatment of NBTE remains a clinical challenge. Gynecologic oncologists should have a high index of suspicion for malignancy-induced NBTE as they will be the ones primarily taking care of these patients. Furthermore, although NBTE portends a very poor prognosis, we believe that it is important for gynecologic oncologists to be aware of cases in which patients improved after an NBTE diagnosis and treatment. To date, the most effective treatment for malignancy-induced NBTE remains low molecular weight heparin, although more prospective data on new anticoagulant agents such as indirect and direct thrombin inhibitors is imperative. Our case demonstrates that prompt diagnosis and treatment of NBTE with anticoagulation and treatment of the underlying malignancy is essential to prevent debilitating, if not deadly, sequelae.
Conflict of interest statement
We have no conflicts of interest or disclosures.
Consent
Witten informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
References
- Aryana A., Esterbrooks D.J., Morris P.C. Nonbacterial thrombotic endocarditis with recurrent embolic events as manifestation of ovarian neoplasm. J. Gen. Intern. Med. 2006;21(12):C12–C15. doi: 10.1111/j.1525-1497.2006.00614.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrier M., Lazo-Langner A., Shivakumar S., Tagalakis V., Zarychanski R., Solymoss S., Routhier N., Douketis J., Danovitch K., Lee A.Y., Le Gal G., Wells P.S., Corsi D.J., Ramsay T., Coyle D., Chagnon I., Kassam Z., Tao H., Rodger M.A., SOME Investigators Screening for occult cancer in unprovoked venous thromboembolism. N. Engl. J. Med. 2015;373(8):697–704. doi: 10.1056/NEJMoa1506623. [DOI] [PubMed] [Google Scholar]
- Delgado G., Smith J. Gynecological malignancy associated with nonbacterial endocarditis (NBTE) Gynecol. Oncol. 1975;3:205–209. doi: 10.1016/s0090-8258(75)80004-7. [DOI] [PubMed] [Google Scholar]
- Devulapalli S., Pinto N., Gandothra C., Jayam-Trouth A., Kurukumbi M. A rare case of occipital stroke as a consequence of nonbacterial thrombotic endocarditis in ovarian clear cell carcinoma: a case report. Case Rep. Neurol. 2012;4(1):84–91. doi: 10.1159/000338811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- el-Shami K., Griffiths E., Streiff M. Nonbacterial thrombotic endocarditis in cancer patients: pathogenesis, diagnosis, and treatment. Oncologist. 2007;12(5):518–523. doi: 10.1634/theoncologist.12-5-518. [DOI] [PubMed] [Google Scholar]
- Erturk N.K., Erturk A., Basaran D., Ozgul N. Synchronous ovarian and endometrial endometrioid adenocarcinoma presenting with nonbacterial thrombotic endocarditis and pulmonary thromboembolism: adenocarcinoma with thrombotic events. Case Rep. Obstet. Gynecol. 2015;2015:825404. doi: 10.1155/2015/825404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee A.Y., Levine M.N., Baker R.I., Bowden C., Kakkar A.K., Prins M., Rickles F.R., Julian J.A., Haley S., Kovacs M.J., Gent M., Randomized Comparison of Low-Molecular-Weight Heparin versus Oral Anticoagulant Therapy for the Prevention of Recurrent Venous Thromboembolism in Patients with Cancer (CLOT) Investigators Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N. Engl. J. Med. 2003;349(2):146–153. doi: 10.1056/NEJMoa025313. [DOI] [PubMed] [Google Scholar]
- Numnum T.M., Leath C.A., 3rd, Straughn M.J., Jr. Synchronous primary endometrial and ovarian carcinoma in a patient with marantic endocarditis. Obstet. Gynecol. 2006;108(3 Pt 2):748–750. doi: 10.1097/01.AOG.0000190220.13074.87. [DOI] [PubMed] [Google Scholar]
- Singh V., Bhat I., Havlin K. Marantic endocarditis (NBTE) with systemic emboli and paraneoplastic cerebellar degeneration: uncommon presentation of ovarian cancer. J. Neuro-Oncol. 2007;83(1):81–83. doi: 10.1007/s11060-006-9306-y. [DOI] [PubMed] [Google Scholar]
- Tanaka H., Ito M., Yoshida K., Asakura T., Taniguchi H. Nonbacterial thrombotic endocarditis complicated with stage Ia ovarian cancer. Int. J. Clin. Oncol. 2009;14(4):369–371. doi: 10.1007/s10147-008-0852-5. [DOI] [PubMed] [Google Scholar]
- Whitlock R.P., Sun J.C., Fremes S.E., Rubens F.D., Teoh K.H., American College of Chest Physicians Antithrombotic and thrombolytic therapy for valvular disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e576S–e600S. doi: 10.1378/chest.11-2305. [DOI] [PMC free article] [PubMed] [Google Scholar]