Abstract
Please cite this paper as: Shanks et al. (2011) Low but highly variable mortality among nurses and physicians during the influenza pandemic of 1918–1919. Influenza and Other Respiratory Viruses DOI: 10.1111/j.1750‐2659.2010.00195.x.
Background During the 1918–1919 influenza pandemic, nurses and physicians were intensively exposed to the pandemic A/H1N1 strain. There are few published summaries of the mortality experiences of nurses and physicians during the pandemic.
Methods Mortality records from U.S. and British Armies during the First World War and obituary notices in national medical association journals were reviewed to ascertain death notices of nurses and physicians likely to have died of influenza.
Results Illness‐related mortality among U.S. military nurses (1·05%) was one and one‐half times higher than among U.S. medical officers (0·68%), nearly two times higher than among British medical officers (0·55%), and nine times higher than among British nurses (0·12%). Among U.S. nursing officers, mortality was approximately twice as high among those assigned in the United States than in Europe. Among civilian physicians, mortality during the influenza pandemic was markedly increased in Canada, New Zealand, South Africa and the United States but not Australia.
Conclusions During the 1918 pandemic, mortality among nurses and physicians was relatively low compared to their patients and significantly varied across locations and settings. Medical‐care providers (particularly U.S. nursing officers) who were new to their assignments when pandemic‐related epidemics occurred may have had higher risk of influenza‐related mortality because of occupational exposures to bacterial respiratory pathogens that they had not previously encountered.
Keywords: 1918, health‐care providers, influenza, military, mortality
Introduction
The 1918–1919 influenza pandemic struck at the end of the First World War. The pandemic spread rapidly around the world and killed tens of millions of people; its effects were not equally distributed across populations or locations. 1 Recently, we reviewed medical and administrative data collected by the Australian Imperial Force to examine the epidemiology of the influenza pandemic among its members. 2 When cause‐specific mortality experiences were examined across occupational groups, we found that medical and nursing personnel had lower pneumonia/influenza‐specific mortality than any other major occupational group. Reviews of other military 3 and civilian 4 records suggested that among nurses and physicians attending patients during the 1918–1919 influenza pandemic, acute respiratory illnesses were very common, but fatal outcomes were relatively rare.
For this report, we reviewed mortality lists (by name) of English‐speaking armies to assess the generalizability of the finding of relatively low death rates among nurses and doctors during the 1918–1919 influenza pandemic. The data suggest that military nursing and medical officers may have suffered less pneumonia/influenza mortality than the officers and men for whom they cared; also, there were mortality differences between nursing and medical officers of the same Armies. In addition, we collected obituary notices of civilian physicians from national medical association journals. 5 When civilian physician mortality was compared across five English‐speaking countries, there were relatively few deaths among those from Australia. This report examines these differences in mortality to further explicate the epidemiology and pathogenesis of the 1918–1919 influenza pandemic and contribute to the discussion on health‐care professionals’ obligation to provide care during an infectious disease emergency. 6
Methods
Deaths of medical and nursing officers of the Australian, 7 , 8 Canadian, 9 New Zealand, 10 United Kingdom, 11 , 12 and United States 13 , 14 , 15 armies were ascertained from official reports of the respective organizations. Denominators for estimates of cumulative mortality incidence were also taken from official records. Because of differences in record keeping, monthly denominators were not available for the entire period or for each subgroup of interest. Also, the locations of some deaths, i.e., home country or deployed in Europe, were not specifically documented and had to be estimated.
For the Australian Army, pneumonia/influenza mortality was determined by review of individual military records. For the other four Armies, deaths not secondary to wounds were considered ‘disease‐related’ (based on the estimate that during the fall 1918, most [>95%] disease deaths were associated with the influenza pandemic). Because nursing and medical officers of all four British Armies functioned under the same policies and procedures, Australian, Canadian, New Zealand, and UK data were combined and are reported as ‘British’. 12 For each subgroup of interest, cumulative illness‐related mortality (CMI %) was estimated for the pandemic period September 1918–February 1919 which included the main mortality wave in October 1918. Pneumonia/influenza‐related mortality in the U.S. Army overall provided a benchmark for assessing the experiences of U.S. and British Army nursing and medical officers.
Civilian physician mortality was determined by collecting all obituaries indicative of respiratory death during 1918–1919 in Australia (Medical Journal of Australia), 16 Canada (Canadian Medical Association Journal), 17 New Zealand (New Zealand Medical Journal), 18 South Africa (South African Medical Record) 19 and the United States (Journal of the American Medical Association). 5 British Medical Journal entries were not felt to be complete enough to be useful for epidemiological purposes. Dates of death were taken directly from the obituaries; if no death dates were given, the publication date was used for analysis.
Results
Military nurses and physicians
During the First World War, more than 47 000 U.S. Army soldiers died of disease, most disease‐related deaths were caused by pneumonias, and most pneumonia deaths occurred during the influenza pandemic period in late 1918. 20 Among U.S. Army soldiers during the pandemic period, pneumonia/influenza‐related mortality rates were more than four times higher among those assigned in the United States than in Europe (Table 1).
Table 1.
Deaths due to medical (non‐combat) causes in U.S and British (Australian, Canadian, New Zealand, UK) Armies between Sep 1918 – Feb 1919 for nursing or medical officers with cumulative mortality incidence per 100 (CMI %) and CMI% ratios shown using denominators from Nov 1918. Dynamic distribution of officers between home country and deployed overseas is estimated to be 50% for purposes of calculations. Estimated rates during influenza pandemic from U.S Army overall are generated from pneumonia/influenza deaths at 40 largest U.S installations and in American Expeditionary Force deployed to Europe
| In home country | Deployed in Europe | Total (September 1918–February 1919) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Deaths | CMI (%) | CMI ratio, nurses:medical | Deaths | CMI (%) | CMI ratio, nurses:medical | Deaths | CMI (%) | CMI ratio, nurses:medical | |
| U.S. Army | |||||||||
| Nurses | 144 | 1·37 | 1·53 (1·21, 1·93) | 76 | 0·72 | 1·58 (1·14, 2·18) | 220 | 1·05 | 1·55 (1·28, 1·87) |
| Medical officers | 139 | 0·90 | Ref | 71 | 0·46 | Ref | 210 | 0·68 | Ref |
| Subtotal, U.S. | 283 | 1·09 | 147 | 0·57 | 430 | 0·83 | |||
| British forces | |||||||||
| Nurses | 7 | 0·05 | 0·22 (0·09, 0·54) | 23 | 0·18 | 0·20 (0·13, 0·33) | 30 | 0·12 | 0·21 (0·14, 0·32) |
| Medical officers | 18 | 0·24 | Ref | 65 | 0·87 | Ref | 83 | 0·55 | Ref |
| Subtotal, British | 25 | 0·12 | 88 | 0·43 | 113 | 0·28 | |||
| Overall | |||||||||
| Nurses | 151 | 0·64 | 0·94 (0·75, 1·18) | 99 | 0·42 | 0·71 (0·55, 0·92) | 250 | 0·53 | 0·84 (0·71, 0·99) |
| Medical officers | 157 | 0·68 | Ref | 136 | 0·59 | Ref | 293 | 0·64 | Ref |
| Total | 308 | 0·66 | 235 | 0·51 | 543 | 0·58 | |||
| U.S. Army, overall | 14 607 | 1·37 | 5486 | 0·32 | 20 093 | 0·72 | |||
| U.S. physicians, overall | 637* | 0·41 | |||||||
CMI, cumulative illness‐related mortality.
*Total pneumonia/influenza deaths September–December 1918. 20
At the time of the Armistice in November 1918, approximately 21 000 U.S. military nurses, 26 000 British (Australian, Canadian, New Zealand, UK) military nurses, 31 000 U.S. medical officers, and 15 000 British medical officers were serving in their respective home lands or deployed overseas. Nursing and medical officers’ deaths during the First World War were generally caused by disease and usually well documented by their respective medical units. Specific diagnoses of lethal respiratory infections were only available for affected members of the Australian Army. However, the striking peak of mortality incidence in October 1918 and the much lower mortality incidence during the preceding and subsequent months suggest that the vast majority of non‐combat deaths in October 1918 were directly or secondarily related to infections with the pandemic strain of influenza virus (Figure 1).
Figure 1.
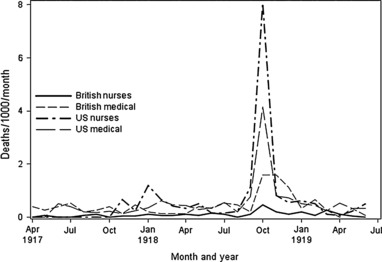
Monthly medical deaths per 1000 in USA and British (Australian, Canadian, New Zealand, and United Kingdom) Armies for nursing and medical officers based on figures supplied by either U.S. Army Surgeon General’s Office 14 or British War Office. 11 , 12
During the fall‐winter 1918–1919, 250 nursing officers and 293 medical officers of the U.S. and British armies died from non‐battle‐related illnesses (Table 1). During the period, cumulative mortality incidence was higher overall among medical officers (0·64%) than nursing officers (0·53%). However, there were marked differences in the mortality experiences of nursing officers and medical officers of the U.S. and British armies – in general and in relation to the locations of their assignments (Table 1).
Approximately one of 95 (1·05%) U.S. Army nursing officers died during the influenza pandemic period (September 1918–February 1919) (Table 1). The crude medical mortality among U.S. Army nursing officers overall was nine times higher than among their British Army counterparts. During the pandemic period, mortality among U.S. Army nursing officers assigned in the United States was nearly two times higher than among those assigned in Europe (but approximately equal to the mortality among U.S. Army soldiers in the United States overall).
Approximately one of 148 (0·68%) U.S. Army medical officers died during the pandemic period. Mortality was more than twice as high among U.S. Army medical officers assigned in the United States than among physicians in the United States in general. Of note, mortality was approximately 40% lower among U.S. Army medical officers than nursing officers – overall and among those in the United States and overseas, specifically.
In contrast to the extreme differences in mortality among U.S. and British nursing officers, mortality was only 20% higher among U.S. than British Army medical officers; among medical officers deployed in Europe, mortality was nearly 50% lower among those in the U.S. than British Army. As among U.S. Army nurses, mortality among U.S. medical officers was approximately two‐times higher among those in the United States than in Europe. In contrast, among British nursing and medical officers, mortality rates were approximately three to four times higher among those deployed in Europe than serving in their home countries. Of note, mortality in the U.S. Army overall (1·37%) was comparable to that among U.S. Army nurses in the United States and exceeded that in all other groups of nurses and medical officers (Table 1).
Civilian physician mortality
During the pandemic period, higher numbers of deaths among physicians were evident from the long lists of obituaries published in national medical association journals (Figure 2). Mortality rates could not be estimated for this report because the numbers of physicians at risk (i.e., denominators for rate calculations) at given times and locations could not be reliably estimated. There was a contemporaneous report that nearly 2% of South African physicians died during the pandemic; the report noted that physicians born in South Africa died at much higher rates than those born in the UK (data were not provided). 19 , 21 The influenza pandemic reached Australia in early 1919; however, there was no clear epidemic of influenza‐related mortality among Australian physicians. Australian physicians were generally similar to South African physicians in training and practice; however, influenza‐related mortality among Australian physicians was approximately one‐tenth that among their South African counterparts. Six hundred and thirty‐seven physicians in the United States reportedly died from pneumonia/influenza during the influenza pandemic in 1918. The estimate may be incomplete; it may only account for members of the American Medical Association. 5 A summary of possible explanations of pandemic influenza mortality appears in Table 2.
Figure 2.
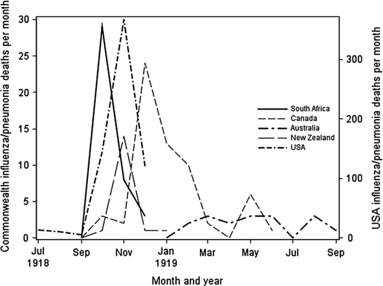
Monthly medical deaths in civilian physicians as reported in national medical association journals 1918–1919. Rates were not generated because of uncertainty of denominators at the time when many physicians were returning from military service. Note that USA physician deaths are on a separate scale. 5
Table 2.
Potential explanations for mortality differences among health‐care workers during the influenza pandemic 1918–1919
| Possible explanation | Comment |
|---|---|
| Differences in immunologic susceptibility and/or exposure to the pandemic influenza strain (Unlikely) | The influenza A/H1N1 pandemic strain was novel, and essentially all persons were immunologically susceptible Most populations worldwide (excepting a few island and other geographically isolated populations) experienced widespread epidemics of pandemic influenza in 1918–1919 During influenza‐related epidemics in 1918–1919, health‐care workers were continuously exposed in crowded clinics and open wards to acutely ill, infectious patients |
| Differences in the inherent virulence of pandemic influenza A/H1N1 viruses (Unlikely) | There is little if any genetic diversity among 1918–1919 influenza A/H1N1 pandemic strains that have been recovered and genetically analyzed During pandemic‐related epidemics in isolated populations and settings (presumably caused by single pandemic influenza strains), there were broad spectrums of clinical manifestations and outcomes of influenza Across subgroups of populations with little demographic diversity (e.g., age, ethnicity, gender, occupation, and access to health care), large differences (10–30 fold) in mortality during pandemic‐related epidemics |
| Differences in naturally acquired immunity against infection with the pandemic influenza A/H1N1 virus (Unlikely) | Virtually all individuals alive in 1918 were immunologically susceptible to infection with the pandemic A/H1N1 strain Young adults (i.e., Australian soldiers) who were hospitalized with respiratory illnesses during widespread spring‐summer 1918 epidemics (‘first wave’) were protected from death – but not from clinically significant illness – during the highly lethal fall‐winter 1918–1919 epidemics (‘second wave’) |
| After infection (days to weeks) with the pandemic influenza strain, different likelihoods of exposure to potentially virulent bacterial strains (Likely) | Most deaths during the 1918–1919 pandemic were caused by secondary bacterial pneumonias Those likely exposed to numerous and varied bacterial strains during pandemic‐related epidemics had relatively high mortality risk, e.g., current residents of urban (versus rural) areas; new Army recruits; soldiers recently assembled on troop transport ships; influenza patients on crowded hospital wards |
| After infection (days to weeks) with the pandemic influenza strain, different likelihoods of exposure to bacterial strains to which hosts were immunologically susceptible (Likely) | Pre‐existing immunity to a broad spectrum of respiratory bacteria decreased the likelihood of exposures of influenza‐infected hosts to bacterial strains to which they were immunologically naive Those exposed to numerous and varied bacterial strains prior to the fall 1918 were relatively protected from death during the pandemic, e.g., doctors and nurses (versus other Australian soldiers); military recruits from urban (versus rural) areas; ‘seasoned’ soldiers (versus new recruits); Navy crewmen (versus soldiers in transit) on troop transport ships |
Discussion
During influenza epidemics in late 1918, nurses and physicians were repeatedly exposed to the pandemic influenza virus and diverse other respiratory pathogens. Many nurses and physicians became ill, but relatively few died. It is difficult to accurately estimate mortality rates among health‐care workers at the end of the First World War. For example, in the United States in 1918, there were massive numbers of health‐care workers moving from civilian to military practice settings and large numbers of military health‐care workers were deploying from the United States to Europe.
Among members of the British Expeditionary Force in France and Belgium, approximately 5 per 1000 soldiers and 1 per 1000 nurses and doctors died of disease between September and December 1918. In the U.S. Army during the pandemic period, mortality rates were similar among nurses and soldiers in general; however, mortality rates in both of these groups exceeded that among medical officers (Table 1). The mortality rate among U.S. physicians in general (4·1 per 1000) was slightly higher than that estimated in the U.S. general population (3·9 per 1000); however, because mortality during the pandemic was particularly high among young adults, the mortality rate among physicians was actually lower than among comparably aged males in the general population. 1 Together, the observations suggest that the pandemic strain of the virus was not inherently and independently lethal; host immune factors were significant determinants of the clinical courses and ultimate outcomes of illnesses caused by the pandemic influenza strain.
During pandemic‐related influenza epidemics in the military during the fall‐winter 1918–1919, there were mortality differences between nurses and medical officers in general, between nurses and medical officers of the same Armies, and between nurses and medical officers of the same Armies in relation to their assignment locations. Of note, however, the natures and magnitudes of the mortality differences between nursing and medical officers were not consistent. For example, in the U.S. Army, mortality was higher among nurses than medical officers, while in the British Army, mortality was much higher among medical officers than nurses. Also, among all military medical officers deployed in Europe, mortality was four times higher among U.S. than British nurses; however, mortality was almost two times higher among British than U.S. medical officers. The findings add support to the conclusion that the pandemic strain of the influenza virus – to which nearly all nurses and medical officers were likely exposed and immunologically susceptible – was not inevitably or independently lethal.
In 1918, the U.S. Army was rapidly mobilizing, training, and deploying forces to Europe. In the last 6 months of the war, in response to a massive recruitment campaign, 48% of all nursing officers and 29% of all medical officers who served during the war joined the U.S. Army. 15 In the early 20th century, nursing education was largely experiential; students cared for patients in hospitals under the supervision of senior nurses. In 1918, many newly recruited U.S. Army nurses were training on the wards of military hospitals (particularly, in the United States). As a result, when pandemic‐related epidemics hit with full force in the fall 1918, many U.S. Army nurses were new not only to the military and their current assignments – but also to the practice of nursing. In 1918, many medical officers also responded to recruitment drives; however, physicians were not eligible for military service until they had completed several years of study. Thus, in the fall 1918, large proportions of the nurses and medical officers of the U.S. Army were new to the military and their practice settings; in general, however, the physicians had more medical experience, including more contact with ill patients, than their nursing counterparts.
The situation in the U.S. Army sharply contrasted with that in the British Armies. In 1918, after 4 years of continuous fighting in Europe, British nursing and medical officers were part of a well established and relatively stable organization. The preponderance of experienced or ‘seasoned’ nurses and physicians in the British Armies may have contributed to the relatively low disease mortality among them during the pandemic. Of note in this regard, of seven Australian military nurses who died from pneumonia/influenza in 1918–1919, three were new ‘recruits’ who cared for sick soldiers in quarantine camps in Australia. Also, during the pandemic, mortality was relatively low among UK nurses in general – perhaps related to how they were deployed and utilized. Young women volunteers were often sent to Voluntary Aid Detachments which were not counted as part of the Army (thus, not included in this report); more experienced nurses were assigned to the highly regimented Queen Alexandra’s Imperial Military Nursing Service that staffed the military hospitals. We hypothesize that, among physicians deployed in France, mortality rates may have been higher among those in the British than those in the U.S. Army because in the British Army, the least experienced doctors served ‘in the trenches’ prior to gaining staff positions in UK‐based hospitals.
In the pre‐antibiotic, pre‐vaccine era, it is difficult to attribute differences in survival to differences in medical care – especially because nursing and medical officers were part of the same military medical systems. During pandemic‐related influenza epidemics, military nurses and medical officers were continuously and intensively exposed to highly contagious and acutely ill soldiers. Many (perhaps most) nurses and physicians were exposed to the pandemic influenza virus and developed clinical illnesses. Yet, mortality rates sharply varied among nurses and medical officers of the same Armies, across different Armies, in different geographic locations, and in different practice settings. A possible explanation for the findings is that influenza‐related mortality risk among medical‐care providers varied in relation to the nature and diversity of their previous patient care experiences and the recency of their current assignments. Those with the least prior experience and newest in their living and occupational settings were at relatively high risk of exposures to strains of respiratory pathogens to which they were immunologically naïve – particularly, at times in the clinical courses of their influenza illnesses when they were most vulnerable to secondary bacterial pneumonias.
As in the military, civilian physicians were at risk of death because of pneumonia/influenza while caring for patients during the pandemic. In some locations, there were clear peaks in influenza‐related mortality, e.g., ‘Black October’ in South Africa, ‘Black November’ in New Zealand. 21 , 22 Australia was a notable exception in that there were relatively few physician deaths and no discernable epidemic peak. It is estimated that more than 12 000 persons died in Australia during the influenza pandemic; the effects of the pandemic were delayed until 1919, likely due to a strict maritime quarantine. 23 Pandemic‐related mortality in Australia was approximately one‐half that in New Zealand which encountered the pandemic several months earlier. 22 Although there was a five‐fold difference in the populations of Australia and New Zealand, there were similar numbers of pandemic‐related physician deaths in the adjacent countries. Dr John H L Cumpston, the Chief Quarantine Officer of Australia in 1918–1919 believed that influenza was circulating in Australia in 1918. 23 In a later review, he stated that ‘Without doubt, the epidemic of 1919 had begun in the winter months of 1918. … During October, November, and December of 1918, there was, in each of the six States of Australia, an unusual prevalence of influenza quite above the annual average, but there was no extensive or virulent epidemic’. 23 Perhaps, the exposures of Australian physicians to patients with influenza‐like illnesses in late 1918 protected them from mortality (if not clinical illness) during the pandemic‐related epidemics in 1919. If so, the experience would be similar to that of the Australian Army in Europe and the Middle East in 1918; among them, soldiers who were treated for acute respiratory illnesses in the spring‐summer 1918 had similar illness, but much lower mortality, rates during the lethal fall 1918 influenza epidemic wave. 2 The variability in pandemic‐related death rates among physicians in Australia and other countries may reflect differences in the sequence and timing of the epidemic spread of different influenza virus strains (e.g., as in the diamond and gold mines of South Africa). 24
During the 1918–1919 influenza pandemic, most nurses and physicians continued to work safely – without patient isolation equipment or procedures; personal protective equipment or measures; antiviral or antibacterial medications; or vaccines against influenza or respiratory bacteria. In spite of their technological poverty, nurses and physicians stuck to their posts in the face of the most lethal medical disaster in history. 3 , 25 , 26 , 27 Preparations for the next influenza pandemic should be informed by the dedication, persistence, and experiences of health‐care providers who confronted and survived the 1918–1919 pandemic.
Funding
The Global Emerging Infections Surveillance and Response System (GEIS) at the Armed Forces Health Surveillance Center of the U.S. Department of Defence providing funding for this project.
Contributors
GDS conceived the epidemiological study, gathered the initial data, assisted in the analysis and wrote the first draft of the manuscript. AM, MW, JB assisted with the data collection, analysis, interpretation and writing of the manuscript.
Disclaimer
The opinions expressed are those of the authors and do not necessarily reflect those of the Australian Defence Force or the U.S. Department of Defense.
Conflicts of interest statement
No author claims any conflict of interest.
Acknowledgements
The authors have been privileged to access information concerning those nurses and physicians who served in the First World War and the civilian health‐care workers who continued to care for their patients in 1918–1919. We recognize the extraordinary sacrifices made by these women and men in the face of a lethal pandemic they did not understand. We thank Prof Tracy Hussell for immunology discussions as well as Ms Debbie Gerlock the archivist at the U.S. Army Surgeon General’s Office of Medical History and Ms Odette Hopwood the librarian at Australian Defence Force Library Services, Gallipoli Barracks for help in locating data.
References
- 1. Murray CJ, Lopez AD, Chin B, Feehan D, Hill KH. Estimation of potential global pandemic influenza mortality on the basis of vital registry data from the 1918–20 pandemic: a quantitative analysis. Lancet 2006; 368:2211–2218. [DOI] [PubMed] [Google Scholar]
- 2. Shanks G, MacKenzie A, McLaughlin R et al. Mortality risk factors during the 1918–1919 influenza pandemic in the Australian army. J Infect Dis 2010; 201:1880–1889. [DOI] [PubMed] [Google Scholar]
- 3. MRC . Studies of Influenza in Hospitals of the British Armies in France 1918. Special Report series no 36. London: HMSO, 1919:6–17. [Google Scholar]
- 4. Report on the Pandemic of Influenza 1918–1919. Reports on Public Health and Medical Subjects. London: Ministry of Health, 1920. [Google Scholar]
- 5. Deaths of physicians in 1918. JAMA 1919; 72:42–43. [Google Scholar]
- 6. Coleman C, Reis A. Potential penalties for health care professionals who refuse to work during a pandemic. JAMA 2008; 299:1471–1473. [DOI] [PubMed] [Google Scholar]
- 7. Butler AG. The Australian Army Medical Services in the War of 1914–1918, Vol. 3. Melbourne: Australian War Memorial, 1943. [Google Scholar]
- 8. Statistics of Casualties Australian Imperial Force. London, 1919. [Google Scholar]
- 9. MacPhail A. Official history of the Canadian Forces in the Great War 1914–1919: The Medical Services. Ottawa: FA Acland, 1925. [Google Scholar]
- 10. Roll of Honour of the New Zealand Army 1914–1919. Wellington: Govt of New Zealand, 1928. [Google Scholar]
- 11. Soldiers Died in the Great War 1914–1919. Version 2.0. Uckfield: The Naval and Military Press Ltd., 2004. [Google Scholar]
- 12. Military Effort of the British Empire during the Great War 1914–1920. London: HMSO, 1922. [Google Scholar]
- 13. The Medical Department in the United States Army in the World War, Vol. 1, Suppl. Carlisle Barracks, PA: Medical Field Service School, 1925. (Army Medical Bulletin No 27). [Google Scholar]
- 14. Ireland M, ed. The Medical Department of the United States Army in the World War: Statistics, Vol. XV. Washington: GPO, 1925. [Google Scholar]
- 15. Ireland M, ed. The Medical Department of the United States Army in the World War: Administration, Vol. I. Washington: GPO, 1925. [Google Scholar]
- 16. Obituary. Med J Aust 1919:497. [Google Scholar]
- 17. Obituary. Can Med Assoc J 1918; 9:1122–1126. [Google Scholar]
- 18. Wright‐St Clair R. Influenza in New Zealand and the doctors who died from it. New Zealand Med J 1983; 96:765–768. [PubMed] [Google Scholar]
- 19. The incidence of the influenza epidemic on the profession South African Medical Record, Vol. 16. 1918; 373–374. [Google Scholar]
- 20. Vaughn V, Palmer G. Communicable disease in the United States Army during the summer and autumn of 1918. J Lab Clin Med 1919; 4:647–686. [Google Scholar]
- 21. Phillips H. ‘Black October’: The Impact of the Spanish Influenza Epidemic of 1918 on South Africa. Pretoria: The Government Printer, 1990. [Google Scholar]
- 22. Rice GW. Black November: The 1918 Influenza Pandemic in New Zealand, 2nd edn Christchurch: Canterbury University Press, 2005. [Google Scholar]
- 23. Cumpston J. Health and Disease in Australia: A History. edited by Lewis M. Canberra: Australian Government Publishing Service, 1986. [Google Scholar]
- 24. Shanks G, Brundage JF, Frean J. Why did many more diamond miners than gold miners die in South Africa during the 1918 influenza pandemic? Int Health 2010; 2:47–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Brundage JF, Shanks G. Deaths from bacterial pneumonia during the 1918–1919 influenza pandemic. Emerg Infect Dis 2008; 14:1193–1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Stone W, Swift G. Influenza and influenzal pneumonia at Fort Riley, Kansas. JAMA 1919; 72:487–493. [Google Scholar]
- 27. Lamb F, Brannin E. The epidemic respiratory infection at Camp Cody, NM. JAMA 1919; 72:1056–1062. [Google Scholar]


