Abstract
Please cite this paper as: Moattari et al. (2012) Influenza viral infections among the Iranian Hajj pilgrims returning to Shiraz, Fars province, Iran. Influenza and Other Respiratory Viruses 6(601), e77–e79
Background Annually over two million Muslims from across the world converge on Mecca to perform the Hajj pilgrimage. Overcrowding at the Hajj facilitates spread of communicable diseases, especially respiratory infections. The aim of this study was to determine the attack rate of seasonal and pandemic influenza among returning Iranian pilgrims after the 2009 Hajj.
Methods Clinical data and throat swabs were collected at Shiraz airport from symptomatic Iranian pilgrims of Fars province who were returning from the Hajj between 15 and 21 December 2009. The specimens were tested at the Shiraz University of Medical Sciences Influenza Research Center for influenza viruses by cell culture and real‐time reverse transcriptase polymerase chain reaction (RTrtPCR) according to standard protocol.
Findings Out of 3000 pilgrims from Fars province who attended the Hajj 2009, 275 symptomatic pilgrims were recruited into this study. Pilgrims had fever, cough, muscle ache and sore throat in various combinations. Twenty‐five (9·1%) pilgrims had influenza by virus culture and these were as follows: influenza B (n = 17), influenza A H3N2 (n = 8) and pandemic H1N1 (n = 5), whereas 33 (12%) had influenza by RTrtPCR: influenza B (n = 20), influenza A H3N2 (n = 8) and pandemic H1N1 (n = 5).
Interpretation Both seasonal and pandemic influenza infections occurred among the Iranian Hajj pilgrims; seasonal viruses were more common than the pandemic viruses even though all pilgrims were vaccinated against seasonal influenza.
Keywords: Hajj, Iran, pandemic influenza, pilgrims
Introduction
Following the first report of H1N1 pandemic influenza 2009 (pH1N1) in Mexico, human‐to‐human transmission of the virus resulted in rapid global spread reaching, within weeks, as far as Spain, UK, Africa, Asia, and Australia. 1 , 2 , 3 It was speculated that high population density and a mass gathering that took place in Iztapalapa, Mexico, during the Easter season of 2009, contributed to the rapid spread of the infection. 4 Annually more than two million Muslims, including one hundred and thousands from Iran, converge on Mecca, Saudi Arabia, to perform the Hajj pilgrimage, one of the world’s largest mass gatherings. The incredibly large and dense crowding of people facilitates the spread of communicable diseases especially respiratory infections. Several studies have reported a high attack rate of seasonal influenza among the Hajj pilgrims including those from Iran. 5 , 6 , 7 the Hajj 2009 took place amidst fear of the H1N1 pandemic in late November the same year. A few studies have been published on the epidemiology of pH1N1 at the Hajj among Egyptian and international pilgrims showing a low prevalence of the disease, but the studies were constrained by limitations as acknowledged by the authors, 8 , 9 and the epidemiology of pH1N1 among Iranian pilgrims has not yet been reported.
The aim of this study was to determine the attack rate of seasonal influenza and pH1N1 among the Iranian Hajj pilgrims returning to Shiraz, the principal city of Fars province of Iran.
Methods
Setting and participants
The target population was 3000 returning Iranian pilgrims of Fars province. Pilgrims with symptoms of fever, cough and sore throat were recruited at Shiraz airport between 15 and 21 December 2009. After briefing the study and obtaining verbal consent, research physicians collected demographic and clinical data in a standard questionnaire and obtained 275 throat swabs from the pilgrims (one swab from each subject). The specimens were placed in viral transport media and transported, under refrigeration, to the virology laboratory of Shiraz University of Medical School (SUMS) and stored at −70°C until tested. The study was approved by the Ethics Committee of SUMS dated 2 December 2009.
Virus isolation
Influenza A and B virus reference strains were obtained from the National Institute for Biological Standards and Control (NIBSC), UK. The swabs were then vortexed in 5 ml medium for a few minutes to dislodge and suspend adherent viruses. The Madin‐Darby canine kidney cell confluent monolayers were inoculated with 200 microliters of the viral suspension. The monolayers were maintained in serum free Dulbeco’s Modified Eagle’s Medium (Sigma Aldrich, Munich, Germany) supplemented with 2 mg/ml trypsin (Gibco BRL; Life Technologies, Gibco, Australia) 100 μg/ml streptomycin and 100 units/ml penicillin G. The cultures were incubated at 34°C and examined daily for cytopathic effect that was confirmed by the ability of infected cultures to agglutinate guinea pig erythrocytes no later than 7 days postinfection. 10
RNA extraction and RTrtPCR
RNA extraction was carried out using Roche High Pure Viral RNA Extraction Kit (Roche, Berlin, Germany) according to the manufacturer’s instructions. Extracted RNAs were kept at −80°C until further processing. RTrtPCR was carried out using SuperScript III Platinum One‐Step Quantitative RT‐PCR kit manufactured by Invitrogen (Carlsbad, CA, USA). Real‐time runs were performed on the Corbett 6000 Rotor‐Gene system (Corbett, Victoria, Australia). The reaction comprised 4 μl of extracted RNA combined with 16 μl of master mix including 2X reaction mix, SuperScript III RT/Platinum Taq Mix, 5·4 μl RNase–DNase free water, and 0·4 μl of each primer and probe with the concentration of 40 μl and 10 μl, respectively. Each sample of RNA was tested by separate primer/probe sets for the detection of influenza universal swine (swFLUA), swine H1 and RNase P. According to the CDC real‐time RT‐PCR protocol (2009), the cycling conditions included a 30 min RT step at 50°C, followed by enzyme inactivation at 95°C for 2 min and the PCR step comprised 45 cycles at 95°C for 15 s, 55°C for 30 s, and 72°C for 30 s. 11 Data acquisition and analysis of the real‐time PCR assay were accomplished using the Rotor‐Gene data analysis Software, Version 6.0A (Corbett).
Statistical analysis
The chi‐square test was used for comparing categorical variables, and a P value <0·05 was considered significant.
Results
Of 275 recruits, just over half (50·9%) were men. Their median age was 46 (range 20–70 years); about 45% were older than 50 years (Figure 1). All pilgrims received seasonal influenza vaccine 2 weeks before departure, but none received pH1N1 vaccine. All pilgrims complained of fever, and along with this, cough, muscle ache and sore throat in various combinations (Table 1). Overall 25 (9·1%) patients were identified to have influenza by virus culture and 33 (12%) had influenza by RTrtPCR; there was no significant difference between the diagnostic yields of the two methods (Table 2). Viruses isolated by culture included influenza B 17 (6·2%), influenza A H3N2 5 (1·8%) and pH1N1 3 (1·1%). Viruses detected by RTrtPCR were influenza B 20 (7·3%), influenza A H3N2 8 (2·9%) and pH1N1 5 (1·8%).
Figure 1.
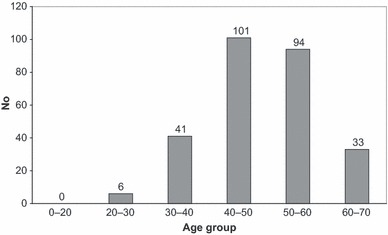
Age distribution of Hajj pilgrims in Fars province of Iran.
Table 1.
Distribution of symptoms among the Hajj pilgrims in Fars Province of Iran
| Symptoms | Number |
|---|---|
| Fever | 275 |
| Sore throat and fever | 200 |
| Myalgia and fever | 220 |
| Cough and fever | 150 |
Table 2.
Distribution of influenza viruses using culture and real‐time PCR in pharyngeal secretions of the Iranian Hajj pilgrims in 2009 (n = 275)
| Virus | Culture | Real time PCR |
|---|---|---|
| Influenza B | 17 (6·2%) | 20 (7·3%) |
| Influenza A (H3N2) | 5 (1·8%) | 8 (2·9%) |
| Pandemic influenza new (H1N1) | 3 (1·1%) | 5 (1·8%) |
Discussion
In this study, we have demonstrated that both seasonal influenza and pH1N1 are important in the Hajj pilgrims. It is a concern that despite being vaccinated, a considerable proportion of pilgrims had seasonal influenza. The attack rate of seasonal influenza of 10·2% (28/275) in our study is similar to that of most other studies conducted in previous years involving, for instance, pilgrims from Iran, UK and Saudi Arabia, 5 , 7 but higher than the prevalence of seasonal influenza reported by employees of the Saudi Government for the 2009 Hajj. 8 Memish and his colleagues have claimed that only seven recruits (five with non‐pandemic influenza A and two with influenza B) out of a total 3218 pilgrims had seasonal influenza that translates to a prevalence rate of 0·2%. The authors, however, have failed to explain the low prevalence of seasonal influenza in their study. 8 In a separate study, the authors have further claimed that none of the 184 healthcare workers they tested before and after the Hajj had influenza. 12 Interestingly, pH1N1 was not the dominant strain among Iranian pilgrims and was reported in only 1·8% pilgrims even though they were unvaccinated. This compares with 0% prevalence rate in fully vaccinated Egyptian pilgrims, 9 and 0·2% in arriving and 0·1% in departing international pilgrims of whom 39% and 29%, respectively, were vaccinated. 8 Apart from the differences in study designs, the discrepancies may have stemmed from vaccination status of the pilgrims or pre‐existing immunity. The latter may be important because about 45% pilgrims in our study were aged >50 years (Figure 1) and therefore likely to have been exposed to H1N1 before 1957. 13 It is also possible that many non‐susceptible pilgrims may have had symptomatic or non‐symptomatic influenza before traveling to the Hajj, hence accounting for the low attack rate of pH1N1 in this and other studies. It is also interesting to note that the extremely low burden of pH1N1 with a high case‐fatality ratio (of 5%) reported by Saudi authorities has sparked controversy. 14 Most of the published studies including ours may have underestimated the actual burden of influenza as the recruitment occurred after the conclusion, or before the start of the Hajj. 8 , 9 , 12 Real‐time surveillance during the peak period of the Hajj would have revealed the true picture. A recent paper reports that 22% of intensive care admissions at hospitals in the Hajj sites were because of PCR‐confirmed pH1N1. 15
The fact that despite receiving seasonal influenza vaccine a substantial proportion of pilgrims had influenza is not surprising as other reports suggest the non‐significant role of the vaccine against influenza at the Hajj. 6 , 7 , 16 It is important to explore the role of other measures, for example, surgical masks, in preventing influenza at the Hajj. 17
Conclusion
Both seasonal and pandemic influenza are important in the Hajj pilgrims. During the pandemic year, despite vaccination, seasonal influenza affected one tenth of the symptomatic Iranian pilgrims. The role of other preventive measures against influenza need to be explored and enhanced surveillance of influenza should continue.
Acknowledgements
This study was financially supported by Deputy Chancellor of Research and Deputy Chancellor of Health, SUMS. We also thank the Ethics committee of SUMS for their approval of this project.
References
- 1. Centers for Disease Control and Prevention (CDC) . Outbreak of swine‐origin influenza A (H1N1) virus infection – Mexico, March–April 2009. MMWR Morb Mortal Wkly Rep 2009; 58:467–470. [PubMed] [Google Scholar]
- 2. Trifonov V, Khiabanian H, Rabadan R. Geographic dependence, surveillance, and origins of the 2009 influenza A (H1N1) virus. N Engl J Med 2009; 361:115–119. [DOI] [PubMed] [Google Scholar]
- 3. Mukherjee P, Lim PL, Chow A et al. Epidemiology of travel‐associated pandemic (H1N1) 2009 infection in 116 patients, Singapore. Emerg Infect Dis 2010; 16:21–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zepeda‐Lopez HM, Perea‐Araujo L, Miliar‐García A et al. Inside the outbreak of the 2009 influenza A (H1N1)v virus in Mexico. PLoS ONE 2010; 5:e13256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rashid H, Shafi S, Haworth E et al. Viral respiratory infections at the Hajj: comparison between UK and Saudi pilgrims. Clin Microbiol Infect 2008; 14:569–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. El Bashir H, Haworth E, Zambon M, Shafi S, Zuckerman J, Booy R. Influenza among U.K. pilgrims to Hajj, 2003. Emerg Infect Dis 2004; 10:1882–1883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Alborzi A, Aelami MH, Ziyaeyan M et al. Viral etiology of acute respiratory infections among Iranian Hajj pilgrims, 2006. J Travel Med 2009; 16:239–242. [DOI] [PubMed] [Google Scholar]
- 8. Memish ZA, Assiri AM, Hussain R, Alomar I, Stephens G. Detection of respiratory viruses among pilgrims in Saudi Arabia during the time of declared influenza A H1N1pandemic. J Travel Med 2011; 19:19–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kandeel A, Deming M, Elkreem EA et al. Pandemic (H1N1) 2009 and Hajj pilgrims who received predeparture vaccination, Egypt. Emerg Infect Dis 2011; 17:1266–1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Merten OW, Manuguerra JC, Hannoun C, Vander Werf S. Production of influenza virus in serum‐free mammalian cell cultures. Dev Biol Stan, 1999; 98:23–37. [PubMed] [Google Scholar]
- 11. CDC protocol of realtime RTPCR for swine influenza A(H1N1) . 28 April 2009, revision 2 (6 October 2009). Geneva: World Health Organization; 2009. (available from http://www.who.int/csr/resources/publications/swineflu/realtimeptpcr/en/index.html). [Google Scholar]
- 12. Memish ZA, Assiri AM, Alshehri M, Hussain R, Alomar I. The prevalance of respiratory viruses among healthcare workers serving pilgrims in Makkah during the 2009 influenza A (H1N1) pandemic. Travel Med Infect Dis, 2012; 10:18–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Xu R, Ekiert DC, Krause JC, Hai R, Crowe JE Jr, Wilson IA. Structural basis of preexisting immunity to the 2009 H1N1 pandemic influenza virus. Science 2010; 328:357–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Haworth E, Rashid H, Booy R. Prevention of pandemic influenza after mass gatherings – learning from Hajj. J R Soc Med 2010; 103:79–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mandourah Y, Ocheltree A, Al Radi A, Fowler R. The epidemiology of Hajj‐related critical illness: lessons for deployment of temporary critical care services. Crit Care Med 2012; 40:829–834. [DOI] [PubMed] [Google Scholar]
- 16. Rashid H, Shafi S, Haworth E et al. Influenza vaccine in Hajj pilgrims: policy issues from field studies. Vaccine 2008; 26:4809–4812. [DOI] [PubMed] [Google Scholar]
- 17. Rashid H, Booy R, Heron L et al. Unmasking masks in Makkah: preventing influenza at hajj. Clin Infect Dis 2012; 54:151–153. [DOI] [PubMed] [Google Scholar]


