Abstract
Pain is a multidimensional experience that involves sensory, cognitive, and affective factors. The constellation of interactions between these factors renders the treatment of chronic pain challenging and financially burdensome. Further, the widespread use of opioids to treat chronic pain has led to an opioid epidemic characterized by exponential growth in opioid misuse and addiction. The staggering statistics related to opioid use highlight the importance of developing, testing, and validating fast-acting nonpharmacological approaches to treat pain. Mindfulness meditation is a technique that has been found to significantly reduce pain in experimental and clinical settings. The present review delineates findings from recent studies demonstrating that mindfulness meditation significantly attenuates pain through multiple, unique mechanisms—an important consideration for the millions of chronic pain patients seeking narcotic-free, self-facilitated pain therapy.
Keywords: mindfulness meditation, pain, fMRI, placebo, opioid
Introduction
The construction and modulation of pain is mediated by sensory, cognitive, and affective factors, rendering the treatment of chronic pain difficult and often a financial burden. Chronic pain affects over 100 million Americans and 1.5 billion people worldwide and costs the United States approximately $635 billion per year in medical expenses and lost work productivity.1 Furthermore, the pervasiveness and burden of chronic pain has dramatically increased Medicare expenditures for steroid injections (over 629%) and opioid treatments (over 423%).2 The widespread use of opioids to alleviate chronic pain has led to an opioid epidemic3 characterized by an exponential rise in opioid misuse and addiction.4, 5 The importance of addressing concerns related to these staggering statistics are reflected in new far-reaching policy changes, such as the recommendations from the Centers for Disease Control and Prevention (CDC) to develop and employ fast-acting nonpharmacological approaches to treat chronic pain.6–8 We postulate that mindfulness meditation could be such a suitable narcotic-free pain therapy for a number of reasons: firstly, mindfulness-based meditation has repeatedly been found to significantly reduce chronic pain symptomologies;9–14 second, mindfulness meditation attenuates pain through multiple unique psychological and neural processes;15–22 and further, it has recently been demonstrated that mindfulness meditation is more effective in reducing pain than placebo23 and does not engage endogenously driven opioidergic systems to reduce pain.20 However, lack of mechanistic classification and reproducibility has reduced the clinical acceptance of meditation to treat pain. While there are a wide variety of meditation traditions and techniques, the present review article will focus on delineating the analgesic mechanisms supporting mindfulness meditation in particular and take into consideration varying levels of meditative expertise and the utility of employing robust control/comparison conditions to better disentangle the specific mechanisms underlying mindfulness meditation.
What is mindfulness meditation?
Mindfulness meditation is a fairly loose term that applies to many meditation practices, which have been found to improve a wide spectrum of clinically relevant cognitive and health outcomes.24–27 In patients, training in mindfulness improves self-reports of anxiety,28–31 depression,10, 32–36 stress,37–39 and cognition.40–46 Mindfulness-related health benefits are associated with enhancements in mechanisms supporting cognitive control, emotion regulation, positive mood, and acceptance.47
Mindfulness has been described as a “non-elaborative, non-judgmental awareness” of the present-moment experience.9, 41 However, one does not need to be practicing, or even be trained in, meditation to be mindful. Varying degrees of trait mindfulness exist in the general population, outside of any formal training.48–50 Mindfulness can also be developed with mental training routines, such as meditation, and there are a variety of different practices that are subsumed under the general rubric of mindfulness meditation. Thus, it is critical that the specifics of the practice being taught or employed be recognized. Here, we will focus on two rather coarse categories of mindfulness practice, namely, focused attention (samatha in the Pali language) and open monitoring (Pali: vipassana),51 both of which are centered on developing a number of distinct cognitive skills.
During focused attention, or samatha,52 the practitioner is taught to develop cognitive control and attentional stability by training the practitioner to sustain focus on the moment-to-moment quality and characteristics of sensory, emotional, and cognitive events. In brief, samatha involves directing one’s attention to the dynamic nature of the chosen object of meditation, most often the sensations of breath or body. When attention drifts from the object of focus, for example, to a distracting sensory event, the practitioner is taught to acknowledge the event and disengage by returning their attention back to the meditative object (e.g., the breath). Often, samatha is taught as a series of distinct practices increasing in complexity (e.g., mindfulness of breath, emotions, and thoughts). While samatha practices aim primarily at gaining mental control and stabilization of attention, they naturally lead, in a somewhat ambiguous way, to the traits associated with open-monitoring meditation. As a developmental derivative of focused-attention practice, the mindfulness practitioner almost naturally transitions into an open-monitoring mental stance, also known as vipassana. It is believed that extensive training in samatha is required before the open-monitoring aligned cognitive stance develops naturally. Whereas samatha often entails focus on a single, dynamic, meditative object, open-monitoring practices are more inclusive of perceived thoughts and emotions. When applied to the full extent, these practices are associated with a non-directed acknowledgement of any sensory, emotional, or cognitive event that arises in the mind. While practicing open monitoring, the practitioner is said to experience the current event without evaluation. To this extent, mindfulness meditation has been described as a state of non-appraisal and/or a non-elaborative mental stance.51
Mindfulness and pain
For thousands of years, Buddhist monks have postulated that the practice of mindfulness meditation can significantly alter the subjective experience of pain. For instance, the ancient Buddhist text, the Sullatta Sutta (The Arrow), states that meditation practitioners have the unique ability to fully experience the sensory aspect of pain (first arrow) but to “let go” of the evaluation (second arrow) of pain. However, only recently have scientists examined the mechanisms underlying mindfulness meditation–induced pain relief and health improvements. In 1980, Nepalese “porters” were found to report significantly higher pain thresholds in response to pain-evoking electrical stimulation when compared to a well-matched control group.53 While the authors attributed these effects to religious practices (presumably meditation), it was not clear, at the time, if meditation practice directly produced analgesia. We have recently witnessed a significant increase in studies demonstrating that mindfulness meditation reduces pain reports across a spectrum of chronic pain conditions.54–66 Furthermore, the advent of neuroimaging methodologies has provided cognitive scientists the means to identify the specific neural mechanisms supporting mindfulness meditation–based analgesia.
Mindfulness meditation improves chronic pain symptomology
Mindfulness meditation–based interventions improve pain symptomology across a wide spectrum of pain-related disorders, including fibromyalgia,14, 67 migraine,68 chronic pelvic pain,61 irritable bowel syndrome,12, 13 and other conditions.69 Given that chronic low back pain is the most common clinical pain condition70 and the leading cause of disability in the United States, it is imperative to better determine if and how mindfulness meditation training affects chronic low back pain. The 8-week mindfulness-based stress reduction (MBSR) program9 is one the most studied and validated approaches for the treatment of chronic low back pain. In a seminal study, Kabat-Zinn and colleagues revealed that chronic pain patients reported improvements in pain symptomology and quality of life after completing the MBSR program9 and improvements were sustained after a 3-year follow-up.10 The work by Kabat-Zinn spawned a burgeoning of research initiatives focusing on mindfulness meditation, including a number of more recent investigations that have employed robust, carefully controlled experimental designs to examine the effectiveness of mindfulness meditation interventions on chronic pain. In an elegant study, Cherkin and colleagues compared the effects of 8 weeks of MBSR to an 8-week cognitive behavioral therapy (CBT) intervention and usual care across a number of chronic low back pain outcomes.71 The MBSR and CBT programs were found to be significantly more effective at reducing pain intensity and reports of pain being bothersome when compared to usual care after 8, 26, and 52 weeks.71 While there were no significant differences between the CBT and MBSR programs in pain-related outcomes, these findings demonstrate that mindfulness-based improvements in chronic pain could be enhanced across time. In another recent study, Morone and colleagues found that an 8-week MBSR program significantly improved numerical pain scale ratings and pain-symptom severity in older adults (i.e., older than 65 years of age) suffering from chronic low back pain when compared to a “very active” pain-related health education group.55 Taken together, these findings demonstrate that relatively brief bouts of mindfulness meditation training can significantly attenuate chronic low back pain symptomology. However, the specific analgesic neural mechanisms demonstrating how mindfulness meditation interventions produce chronic pain have yet to determined, which is a critical step in fostering the clinical validity of this ancient technique.
The construction and modulation of pain: a brief neurophysiological synopsis
Pain is a complex and subjective conscious experience constructed and modulated by a constellation of sensory, cognitive, and affective factors, including mood, psychological disposition, meaning-related cognitions (e.g., suffering), learning, desires, and pre-pain cognitive states (e.g., expectations; anxiety) to provide a continually changing experience. Feedback connections between low-level afferent and higher-order neural processes foster the cultivation of a distributed, multidimensional network associated with the subjective experience of pain. Nociceptive sensory events are first registered by peripheral primary afferents (first pain, A-delta fibers; second pain, C fibers) at the site of injury/tissue damage, which then relay this nociceptive information to the dorsal horn of the spinal cord. From the spinal cord, nociceptive information ascends contralateral to the site of pain to the brain, largely through the spinothalamic pathway. Nociceptive input is subsequently processed through feedback connections between lower-level sensory regions, including the parabrachial nucleus, periaqueductal gray matter (PAG), thalamus, and primary somatosensory (SI) and secondary somatosensory (SII) cortices.72–78 Ascending nociceptive information is then transmitted to the posterior and anterior insular cortices where it is fine-tuned to foster the subsequent evaluation of pain.79, 80 The contextual meaning of pain is then facilitated through activation of higher-order brain regions, including the anterior cingulate cortex (ACC), dorsal ACC (dACC), and prefrontal cortex (PFC).80–82 Yet, the subjective experience of pain remains to be highly influenced by the context in which it occurs. That is, previous experiences, expectations, mood, conditioning, desires, sensitization/habituation, and other cognitive factors can dramatically amplify and/or attenuate pain.78, 83–87
Nonpharmacological-based pain manipulations attenuate the subjective experience of pain through a common final pathway, including overlapping endogenously driven and neural systems. While the cognitive modulation of pain is mediated through a host of endogenous modulatory systems, including cannabinoid, serotonergic, dopaminergic, cholecystokinin, adrenergic, and other neurochemical systems (i.e., vasopressin), the endogenous opioidergic system is the most understood (and studied) pain modulatory system.88 Endogenous opioidergic mechanisms have been repeatedly demonstrated to mediate analgesia produced by placebo,89–93 conditioned pain modulation,94 acupuncture,95 hypnosis,96 and attentional control.97 Pain relief produced by these cognitive techniques are associated with significant reductions in pain-related brain activation (i.e., SI, SII, posterior insula, parietal operculum) and activation in higher-order brain regions, such as the ACC, PFC, and insula.86, 89, 98–110 Importantly, the PFC, insula, and ACC contain high concentrations of opioid receptors and are associated with producing analgesia through descending inhibitory systems.105, 111–115 The ACC and PFC project to the PAG,116 a structure that can be directly activated by opioids. The PAG projects to the rostral ventral medulla,117–119 which, in turn, projects to the spinal dorsal horn and can inhibit nociceptive processing through multiple neurotransmitter systems.120
Brain mechanisms supporting the modulation of pain by long-term meditators
A large proportion of mindfulness meditation–based experimental pain research has focused on examining the effects of meditation practice ranging from 8 weeks to multiple decades. In one of the first mindfulness meditation–focused experimental pain studies, Grant and Rainville found that long-term Zen meditation practitioners required significantly higher levels of noxious thermal stimulation to report paralleling levels of pain as age-matched controls.121 In their follow-up study with an overlapping sample, the authors found that, in the presence of noxious thermal stimulation, long-term Zen practitioners showed significant activation of sensory processing–related brain regions (thalamus, insula) and reduced activation in brain areas that process the evaluation of pain (medial PFC (mPFC), OFC). There was also a significant relationship between greater deactivation of the mPFC/OFC, meditative experience, and lower pain reports.18 Remarkably, these findings were exhibited during a non-meditative cognitive state, suggesting that long-term meditation training produces stabilized changes in the subjective evaluation of pain.
In addition, Lutz and colleagues examined the psychophysical and neural effects of meditation across 14 long-term mindfulness meditation practitioners (approximately 10,000 h of formal meditation practice in the Nyingma and Kagyu traditions of Tibetan Buddhism) during noxious heat stimulation compared to 14 non-meditating controls.19 The control group was provided with guidelines to practice mindfulness meditation and instructed to practice at home for 30 min/day for 1 week. Surprisingly, there was no difference between long-term meditators and the novice meditation group on pain intensity ratings during samatha practice. Not surprisingly, open-monitoring meditation produced significant reductions in pain unpleasantness in the expert meditation group when compared to the controls.19 This form of meditation was associated with reduced anticipatory (before the painful heat stimulus) activation in the anterior insula. Further, the reduced baseline activation in left anterior insula correlated with lifetime meditation experience. These findings and others16 indicate that reducing expectations of impending pain is at least one process/mechanism by which mindfulness meditation reduces pain.
In a study by Gard et al., the neural mechanisms supporting mindfulness meditation–based analgesia were examined in 17 long-term vipassana practitioners (mean meditation practice experience = 5979 h) in response to noxious electrical stimulation compared to 17 age-, gender-, and education-matched non-meditating controls.17 Similar to other studies,16, 19, 122 the authors did not find a significant difference between the meditation and control groups in pain intensity ratings, but did find a significant reduction in pain unpleasantness ratings compared to the control group during the mediation state in the presence of noxious stimulation.17 Greater activation of the contralateral SII/posterior insula was associated with meditation-induced pain unpleasantness ratings. The authors also found greater rACC and ventromedial PFC (vmPFC) activation during the prestimulus anticipatory phase, suggesting that cognitive control mechanisms were at play. However, meditation-induced analgesia was directly associated with greater deactivation of the PFC and increased activation of the posterior insula, which is consistent with the abovementioned work by Grant and Rainville.18 Taken together, these findings are important because they demonstrate that the neural mechanisms involved in mindfulness-based pain relief are consistent with the postulated psychological expression/experience of mindfulness (i.e., greater sensory processing and parallel reductions in pain appraisal).
These findings have advanced our knowledge of the mechanisms supporting the stabilized psychological and neural changes associated with long-term meditation practice. Yet, the utility of meditation for treating pain remains limited because of the assumption that the benefits of meditation require lengthy training regimens.15, 27 Specifically, extensive class time requirements123 and overall length of meditation training regimens have been cited as leading barriers to the clinical utility of meditation interventions.124 Furthermore, the aforementioned studies employed cross-sectional and/or case control designs, consequently limiting their generalizability because of the wide spectrum of potential between-group differences (e.g., demographics, demand characteristics, and meditative tradition) that may exist.15 Thus, random assignment and longitudinal designs are encouraged for meditation-focused studies.27 In light of these findings, we postulate that if the benefits of meditation can be elicited by brief mindfulness-based mental training regimens, then meditation may be more feasible to apply in clinical settings.
Mindfulness meditation after brief training reduces pain through unique mechanisms
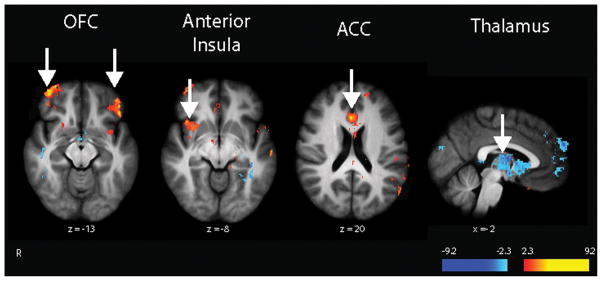
Recent studies from our laboratory have focused on disentangling the specific analgesic behavioral, neural, and pharmacologic mechanisms involved in mindfulness meditation–related pain relief. In 2011, we examined the effects of mindfulness meditation in 15 healthy pain-free subjects after participation in a brief (four sessions; 20 min/session) mindfulness meditation–based intervention on experimentally induced (ten 12-s plateaus of 49 °C) pain, using arterial spin labeling (ASL) functional magnetic resonance imaging (fMRI). ASL is a neuroimaging technique that provides a direct quantifiable measurement of global cerebral blood flow, an important consideration for breathing-focused cognitive practices, such as meditation.21 During meditation training, subjects were instructed to close their eyes, sit with a straight posture and focus on the breath sensations, acknowledge distracting thoughts and feelings, and to simply let go of arising sensory events without judgment. Participants were taught that perceived sensory and affective events are momentary and fleeting and do not require further evaluation. In the first two meditation training sessions, subjects were instructed to focus on the breath sensations occurring at the tip of the nose and full flow of the breath. Meditation, after the four-session intervention, during noxious heat produced a mean 40% reduction in pain intensity and 57% reduction in pain unpleasantness ratings. Greater activation of the subgenual ACC (sgACC), OFC, and right anterior insula (Fig. 1) was associated with mindfulness meditation–based analgesia. The sgACC is critically involved in the cognitive and affective control of pain.83, 86, 99, 125, 126 The OFC has been implicated in altering the contextual evaluation of arising sensory events,127–130 and the right anterior insula is associated with the modulation of afferent nociceptive processing,74, 75, 80, 100, 131 and processing interoceptive awareness.132–134. We also found that mindfulness meditation–based pain relief was associated with greater bilateral thalamic deactivation (Fig. 1) 21. Thus, meditation may reduce pain by fine-tuning the amplification of nociceptive sensory events through top-down control processes,15, 21, 23 potentially reflected by the significant attenuation of SI activation corresponding to the stimulation site when subjects meditated during noxious heat when compared to rest (right leg).21 We postulated that mindfulness meditation attenuates pain through engagement of top-down (OFC to thalamus) inhibition of ascending nociceptive information.15, 20, 21, 23 Thus, the cognitive state of mindfulness meditation–based analgesia does not reduce pain through one avenue but rather multiple, unique neural mechanisms. Although this study employed a longitudinal design, a control group was not included. However, our follow-up studies addressed this caveat.20, 23
Figure 1.
Mindfulness meditation–based pain relief is associated with multiple brain mechanisms. Regression analyses corresponding to those in Zeidan et al.21 revealed that reductions in mindfulness meditation–induced pain intensity were associated with greater activation (depicted in red) in the right anterior insula and rostral aspects of the anterior cingulate cortex (ACC). Greater reductions in pain unpleasantness ratings were associated with greater activation of the orbitofrontal cortex (OFC) and thalamic deactivation (depicted in blue).
Does mindfulness meditation engage mechanisms consistent with placebo analgesia?
While mindfulness meditation practice can improve health and well-being, the active mechanisms supporting mindfulness meditation have yet to be fully characterized. Importantly, a wide range of nonspecific placebo-related effects are likely involved during meditation training. Here, we define the placebo response as benefits or effects driven by nonspecific and/or inert dimensions of a drug, intervention, or manipulation. Nonspecific and potentially confounding variables, such as conditioning effects, psychosocial contexts, facilitator attention, intervention setting, body posture, and/or demand characteristics associated with the belief that one is practicing meditation,15, 27, 135 could mediate mindfulness meditation–related health improvements.136, 137 Randomized, placebo-controlled studies are the gold-standard approach to identify the effectiveness and specific mechanisms supporting the modulation of pain by mindfulness meditation. Yet, placebo-controlled meditation studies have been limited, which is problematic when considering that meditation is arguably highly susceptible to placebo-type effects.
Some recent studies have successfully disentangled the processes by which meditation affects health. For example, Creswell and colleagues examined the behavioral and inflammatory stress markers (i.e., interleukin-6 (IL-6) and neural mechanisms related to participating in an intensive 3-day mindfulness meditation intervention compared to a 3-day health enhancement relaxation program in unemployed and clinically stressed adults.138 The researchers matched all aspects of the relaxation program to the meditation intervention, including sitting in silence, meals, stretching exercises, slow walking, facilitator interviews, and even the location of the intervention. Both groups reported significant differences in perceived stress. However, increases were shown in pre- to post-meditation intervention functional neural connectivity between a central node of the default fault mode network (i.e., posterior cingulate cortex (PCC) and the dorsolateral PFC (dlPFC), a brain region implicated in cognitive and affective control. Furthermore, the dlPFC–PCC connectivity mediated reductions in circulating IL-6 from baseline to the 4-month follow-up. In contrast, the relaxation intervention group exhibited mild increases in IL-6 after the intervention. These findings provide supplementary evidence that mindfulness meditation employs unique mechanisms to improve health in clinically relevant populations.
Another research group developed an active comparison intervention, referred to as a health enhancement program (HEP), to specifically isolate and control for the effects of MBSR.139–141 The HEP was postulated to control for facilitator allegiance, time spent providing instruction/therapy, social support, and other components related to participating in an MBSR program.139 Although the HEP and MBSR program were effective at reducing self-reports of anxiety, distress, hostility,139 and attentional stability,140 there were no significant differences between groups. However, the MBSR program was more effective at reducing inflammatory responses following social stress141 and experimentally-induced pain ratings.139 These studies demonstrated the unique health-promoting properties supporting mindfulness-based health promotion. However, the question arises as to whether it is possible that the benefits of meditation may simply be related to the belief that one is practicing mindfulness meditation.
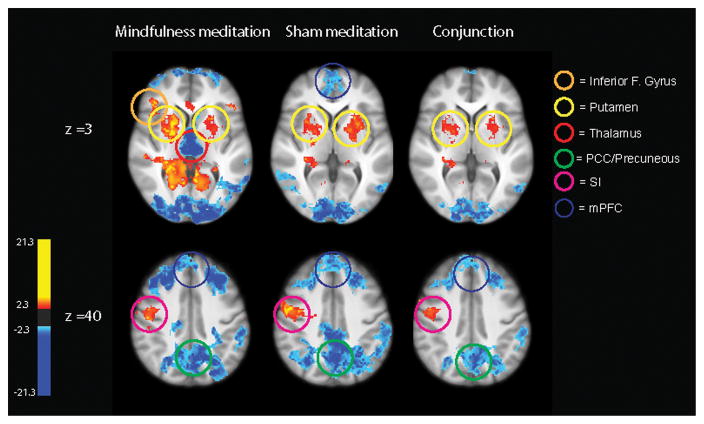
A recent study23 examined whether mindfulness meditation–based pain relief engages neural mechanisms that are distinct from placebo analgesia and sham mindfulness meditation–related analgesia. Similar pain-evoking thermal stimulation paradigms and neuroimaging methods (ASL MRI) were employed as described previously.21 Seventy-five healthy, pain-free subjects were randomly assigned to one of four 4-session (20 min/session) regimens: (1) a brief mindfulness meditation intervention similar to an intervention described previously;21, 31, 36, 46, 142 (2) placebo conditioning; (3) sham mindfulness meditation; and (4) a book-listening intervention. Participants in the placebo-conditioning group were led to believe that the effects of an experimental form of lidocaine was being tested, in which the analgesic effects of the cream (placebo cream was petroleum jelly) progressively increase as a function of repeated applications. To enhance placebo conditioning, the stimulus temperatures delivered to the treated skin were covertly reduced, from 49 °C, in a progressive fashion across sessions (placebo conditioning session 1: 48 °C; sessions 2 and 3: 47 °C; session 4: 46.5 °C). The 49 °C stimulus was administered after applying/removing the placebo cream in the post-intervention MRI session to measure the efficacy of the placebo conditioning regimen. The sham mindfulness meditation intervention was designed so that the only difference in training between the mindfulness and sham mindfulness meditation groups was the explicit mindfulness-based instructions (e.g., non-judgmental attention to the breath) given to the mindfulness meditation group. Subjects were first informed that they were randomly assigned to the mindfulness meditation intervention. Across four 20-min sessions, participants were trained to take deep breaths “as we sit here in mindfulness meditation.” The control group listened to the Natural History of Selborne143 across four sessions.
All cognitive manipulations (mindfulness meditation, placebo cream, sham mindfulness meditation) reduced pain intensity and unpleasantness ratings compared to the control group. Importantly, mindfulness meditation was significantly more effective at reducing pain than both placebo groups. Mindfulness meditation–based pain relief was associated with similar brain activation as in our previous neuroimaging study,21 including greater activation of the OFC, pregenual ACC (pgACC), and right anterior insula. Placebo-cream analgesia was associated with significant reductions in pain-related brain activation (posterior insula/parietal operculum; secondary somatosensory cortices) and produced greater activation in the thalamus and PAG compared to mindfulness meditation. Interestingly, the main effects of mindfulness meditation and sham mindfulness meditation significantly overlapped in activation of the bilateral putamen, SI corresponding to the nose/mouth, and the dACC, suggesting that the two breathing-focused practices engage similar mechanisms (Fig. 2). However, the two techniques were associated with significantly distinct neural processes when the analyses were focused on the pain-related MRI series. In contrast to mindfulness meditation, sham mindfulness meditation produced greater activation in the thalamus and deactivation of the rostral ACC. Importantly, sham mindfulness meditation–related analgesia was associated with greater reductions in respiration rate, demonstrating a mechanistic difference between sham and mindfulness meditation. That is, mindfulness meditation–related pain relief was associated with greater executive-level modulation of pain and, in contrast, sham mindfulness meditation–induced analgesia was driven by bottom-up processes consistent with placebo and relaxation.144
Figure 2.
The main effects of mindfulness meditation and sham mindfulness meditation involve similar neural processes. Mindfulness meditation and sham mindfulness meditation produced activation (red) in the bilateral putamen and primary somatosensory cortex (SI) corresponding to the nose/face regions and deactivation (blue) of the medial prefrontal cortex (mPFC) and precuneous/poster cingulate cortex (PCC). Mindfulness meditation also activated the right inferior frontal gyrus and produced deactivation of the bilateral thalamus. Conjunction analyses revealed significant overlapping activation in the bilateral putamen, SI representation of the nose/face, and deactivation of the PCC and mPFC.
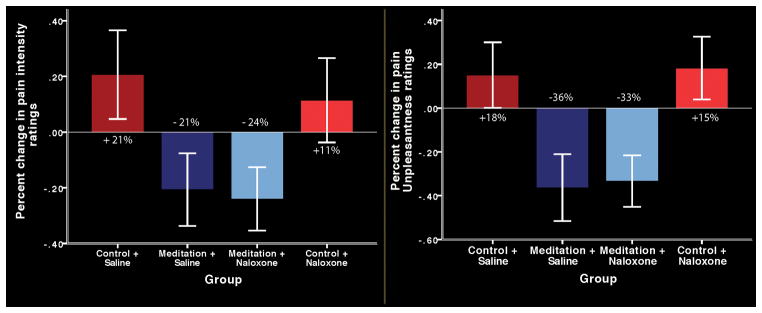
While the endogenous pain modulatory systems supporting mindfulness-based analgesia remain unknown, it is well established that the cognitive modulation of pain, including manipulations such as placebo89, 91–93, 105, 145, conditioned pain modulation,94 and attentional control,97 is partially dependent on descending pain control systems98, 146 and can be reversed by the opioid antagonist naloxone.90, 91, 97, 147 Interestingly, meditation reduces pain by engaging brain regions (sgACC, OFC, anterior insula) that contain high concentrations of opioid receptors.92, 111, 113, 148 On the other hand, mindfulness meditation also reduces activation in the PAG, a brain region involved in facilitating opioid-mediated descending pain inhibition.72, 149 Thus, a recent double-blind psychophysical study tested whether mindfulness meditation–based analgesia was mediated by endogenous opioids; 78 healthy pain-free subjects were randomized to one of four 4-session intervention groups (meditation + naloxone, book-listening control + naloxone, meditation + saline, book-listening control + saline) to determine if intravenous administration of high doses of naloxone would reverse meditation-induced analgesia. Surprisingly, it was found that, independent of naloxone or placebo-saline administration, meditation significantly reduced pain intensity and unpleasantness ratings compared to rest and the control groups (Fig. 3)20. These findings provide supplementary evidence that mindfulness meditation engages mechanisms that are distinct from placebo to reduce pain and are of critical importance to the millions of chronic-pain patients seeking a fast-acting non-opioid pain therapy. Specifically, it was proposed that the combination of mindfulness-based and pharmacologic/nonpharmacologic analgesic strategies may be particularly effective in the treatment of pain.
Figure 3.
Psychophysical pain intensity (left graph) and unpleasantness (right graph) ratings (95% confidence intervals). Meditation during saline (meditation + saline) infusion significantly (P < 0.001) reduced pain intensity and unpleasantness ratings compared with rest and the control and saline (control + saline) group. Naloxone did not reverse meditation-induced pain relief. Meditation during naloxone administration (meditation + naloxone) significantly (P < 0.001) reduced pain intensity and unpleasantness ratings compared with rest, the control + saline group, and the control and naloxone (control + naloxone) groups. There were also no significant differences in pain intensity or unpleasantness ratings between the meditation + saline and the meditation + naloxone groups (P > 0.69).
Conclusion
Mindfulness meditation engages multiple unique brain mechanisms that attenuate the subjective experience of pain. Yet, analgesic mechanisms supporting mindfulness-based meditation change as a function of increasing meditative experience/training. While meditation after brief training (less than 1 week) produces significant reductions in pain intensity and unpleasantness ratings,20, 21, 23, 122, 142 long-term meditation does not produce changes/differences in pain intensity but rather influences the unpleasantness dimension of self-reported pain.17, 121, 122 This proposed change in the subjective experience is likely attributable to a shift in approach to meditating in the context of incoming sensory information between novice and adept practitioners. For instance, a shift in meta-awareness has been proposed,45 in which adept meditators can engage an invasive sensation (e.g., pain) without appraising/evaluating the event. It remains unclear how this shift changes as a function of greater practice.51, 52, 150 Nevertheless, it is not surprising that a decoupling between sensory and appraisal-related brain regions is exhibited in adept meditators in the presence of noxious stimulation.17, 18 In contrast, novice meditators engage more effortful reappraisal processes to reduce pain, and adept meditators employ no-appraisal mechanisms.
We propose that, at the early stages of training, mindfulness meditation alters the evaluation and meaning of pain as a function of self-referential processing. Subject testimonials from our previous studies20, 21, 23, 142 provide supplementary support for this hypothesis. Study subjects routinely stated that the experience of noxious heat stimulation during meditation was “shorter,” “softer,” and accompanied with “less dwelling” and a greater ability to “fully embrace the feeling of pain,” but to simply “let go” of the appraisal of what the pain meant to them. These reports are remarkably consistent with the mindfulness principles that were instilled during their meditation training. Neuroimaging data provide supplementary support for these experiences. Novice meditators recruit higher-order brain regions (OFC, sgACC, anterior insula) to downregulate ascending nociceptive input at the level of the thalamus through shifts in executive attention.21,23 Thus, meditation after brief mental training affects sensory and affective pain-related responses. The comprehensive modulation of both the intensity- and unpleasantness-related dimensions of pain is hypothetically facilitated through changes in executive attention. Activation of the OFC may facilitate inhibitory connections of the thalamic reticular nuclei (TRN) to further reduce the elaboration of nociceptive information throughout the cortex (evidenced by reductions in thalamic, PAG, and SI activation).21, 23 Thus, brief mental training in mindfulness meditation engages cortico–thalamic–cortical interactions to reduce pain through mechanisms such as inhibitory control45 or reappraisal (or “re-perceiving”151) to essentially “close the gate” on ascending nociceptive information. In contrast, the neural mechanisms involved in long-term meditation practice are associated with significantly greater activation in somatosensory regions and deactivation of appraisal-related brain regions (vmPFC).17, 18 The decoupling between the sensory experience and the meaning and/or contextualization of what the pain means to the self, in long-term meditation practitioners, provides evidence that the analgesic effects of meditation can be developed and enhanced through greater practice, a critical consideration for those seeking long-lasting narcotic-free pain relief.
When taking into consideration the current chronic pain152 and opioid epidemic,153, 154 the use of mind–body approaches, such as mindfulness meditation, may prove to be an important resource to teach patients to self-regulate their respective experience of pain directly with a present-centered and acceptance-based focus. Converging lines of evidence demonstrate that mindfulness meditation significantly attenuates pain across clinical and experimental settings. In contrast to other health outcomes, the health-promoting effects of meditation are most pronounced for pain and pain-related comorbidities, including opioid addiction and misuse,155–158 stress,37, 138 depression,159–161 and anxiety.31, 162, 163 Some recent studies of fibromyalgia22 and chronic low back pain54 patients who received mindfulness training also see a similar decoupling of sensory and affective pain, such that pain intensity or frequency does not necessarily decrease, but coping with the pain does improve. Furthermore, across almost all mindfulness/pain–focused experiments, the unpleasantness dimension of pain was significantly more attenuated with respect to pain intensity,16–21, 23, 121, 122 which is a critically important effect when considering the use of meditation for clinical pain. For instance, the experience of chronic pain is dramatically influenced by the context in which it occurs. One example of this comes from studies assessing pain in patients and in women giving birth.164 The pain of labor was rated as significantly higher on sensory aspects compared to the affective dimension. In contrast, cancer pain was rated significantly higher on pain unpleasantness than pain intensity.165 The suggestion here is that the contextual evaluation of welcoming a new baby into the world when compared to facing one’s own death has profound implications for what might have otherwise been very similar experiences. We suggest that mindfulness, in a similar, albeit less profound manner than giving birth or dying, also alters the meaning, interpretation, and appraisal of nociceptive information, an important consideration for producing stabilized and long-lasting improvements in chronic pain symptomology, and can potentially serve as a mechanism to buffer against the chronification of pain.
Footnotes
Conflicts of interest
The authors declare no conflicts of interest.
References
- 1.Institute of Medicine (US) Committee on Advancing Pain Research C, and Education. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington D.C: National Academies Press; 2011. [PubMed] [Google Scholar]
- 2.Deyo RA, et al. Overtreating chronic back pain: time to back off? Journal of the American Board of Family Medicine : JABFM. 2009;22:62–68. doi: 10.3122/jabfm.2009.01.080102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nelson LS, Juurlink DN, Perrone J. Addressing the Opioid Epidemic. Jama. 2015;314:1453–1454. doi: 10.1001/jama.2015.12397. [DOI] [PubMed] [Google Scholar]
- 4.Han B, et al. Nonmedical Prescription Opioid Use and Use Disorders Among Adults Aged 18 Through 64 Years in the United States, 2003–2013. Jama. 2015;314:1468–1478. doi: 10.1001/jama.2015.11859. [DOI] [PubMed] [Google Scholar]
- 5.Saloner B, Karthikeyan S. Changes in Substance Abuse Treatment Use Among Individuals With Opioid Use Disorders in the United States, 2004–2013. Jama. 2015;314:1515–1517. doi: 10.1001/jama.2015.10345. [DOI] [PubMed] [Google Scholar]
- 6.Olsen Y. The CDC Guideline on Opioid Prescribing: Rising to the Challenge. Jama. 2016 doi: 10.1001/jama.2016.1910. [DOI] [PubMed] [Google Scholar]
- 7.Frieden TR, Houry D. Reducing the Risks of Relief - The CDC Opioid-Prescribing Guideline. The New England journal of medicine. 2016 doi: 10.1056/NEJMp1515917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain-United States, 2016. Jama. 2016 doi: 10.1001/jama.2016.1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. General hospital psychiatry. 1982;4:33–47. doi: 10.1016/0163-8343(82)90026-3. [DOI] [PubMed] [Google Scholar]
- 10.Kabat-Zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. Journal of behavioral medicine. 1985;8:163–190. doi: 10.1007/BF00845519. [DOI] [PubMed] [Google Scholar]
- 11.Morone NE, Greco CM, Weiner DK. Mindfulness meditation for the treatment of chronic low back pain in older adults: a randomized controlled pilot study. Pain. 2008;134:310–319. doi: 10.1016/j.pain.2007.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Garland EL, et al. Therapeutic mechanisms of a mindfulness-based treatment for IBS: effects on visceral sensitivity, catastrophizing, and affective processing of pain sensations. Journal of behavioral medicine. 2011 doi: 10.1007/s10865-011-9391-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gaylord SA, et al. Mindfulness training reduces the severity of irritable bowel syndrome in women: results of a randomized controlled trial. Am J Gastroenterol. 2011;106:1678–1688. doi: 10.1038/ajg.2011.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grossman P, et al. Mindfulness training as an intervention for fibromyalgia: evidence of postintervention and 3-year follow-up benefits in well-being. Psychotherapy and psychosomatics. 2007;76:226–233. doi: 10.1159/000101501. [DOI] [PubMed] [Google Scholar]
- 15.Zeidan F, et al. Mindfulness meditation-related pain relief: evidence for unique brain mechanisms in the regulation of pain. Neuroscience letters. 2012;520:165–173. doi: 10.1016/j.neulet.2012.03.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brown CA, Jones AK. Meditation experience predicts less negative appraisal of pain: Electrophysiological evidence for the involvement of anticipatory neural responses. Pain. 2010;150:428–438. doi: 10.1016/j.pain.2010.04.017. [DOI] [PubMed] [Google Scholar]
- 17.Gard T, Holzel BK, Sack AT, Hempel H, Vaitl D, Ott U. Pain attenuation through mindfulness is associated with decreased cognitive control and increased sensory processing in the brain. Cerebral cortex. 2011;191:36–43. doi: 10.1093/cercor/bhr352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grant JA, Courtemanche J, Rainville P. A non-elaborative mental stance and decoupling of executive and pain-related cortices predicts low pain sensitivity in Zen meditators. Pain. 2011;152:150–156. doi: 10.1016/j.pain.2010.10.006. [DOI] [PubMed] [Google Scholar]
- 19.Lutz A, et al. Altered anterior insula activation during anticipation and experience of painful stimuli in expert meditators. NeuroImage. 2013;64:538–546. doi: 10.1016/j.neuroimage.2012.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zeidan F, et al. Mindfulness-Meditation-Based Pain Relief Is Not Mediated by Endogenous Opioids. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2016;36:3391–3397. doi: 10.1523/JNEUROSCI.4328-15.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zeidan F, et al. Brain mechanisms supporting the modulation of pain by mindfulness meditation. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2011;31:5540–5548. doi: 10.1523/JNEUROSCI.5791-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vago D, Nakamura Y. Selective Attentional Bias Towards Pain-Related Threat in Fibromyalgia: Preliminary Evidence for Effects of Mindfulness Meditation Training. Cognitive Therapy and Research. 2011;35:581–594. [Google Scholar]
- 23.Zeidan F, et al. Mindfulness Meditation-Based Pain Relief Employs Different Neural Mechanisms Than Placebo and Sham Mindfulness Meditation-Induced Analgesia. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2015;35:15307–15325. doi: 10.1523/JNEUROSCI.2542-15.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grossman P, et al. Mindfulness-based stress reduction and health benefits. A meta-analysis. Journal of psychosomatic research. 2004;57:35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- 25.Goyal M, et al. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA internal medicine. 2014;174:357–368. doi: 10.1001/jamainternmed.2013.13018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Farb NA, Anderson AK, Segal ZV. The mindful brain and emotion regulation in mood disorders. Canadian journal of psychiatry Revue canadienne de psychiatrie. 2012;57:70–77. doi: 10.1177/070674371205700203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tang YY, Holzel BK, Posner MI. The neuroscience of mindfulness meditation. Nature reviews Neuroscience. 2015;16:213–225. doi: 10.1038/nrn3916. [DOI] [PubMed] [Google Scholar]
- 28.Goldin P, et al. Randomized controlled trial of mindfulness-based stress reduction versus aerobic exercise: effects on the self-referential brain network in social anxiety disorder. Frontiers in human neuroscience. 2012;6:295. doi: 10.3389/fnhum.2012.00295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goldin PR, Gross JJ. Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion. 2010;10:83–91. doi: 10.1037/a0018441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Miller JJ, Fletcher K, Kabat-Zinn J. Three-year follow-up and clinical implications of a mindfulness meditation-based stress reduction intervention in the treatment of anxiety disorders. General hospital psychiatry. 1995;17:192–200. doi: 10.1016/0163-8343(95)00025-m. [DOI] [PubMed] [Google Scholar]
- 31.Zeidan F, et al. Neural correlates of mindfulness meditation-related anxiety relief. Social cognitive and affective neuroscience. 2014;9:751–759. doi: 10.1093/scan/nst041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barnhofer T, et al. Mindfulness-based cognitive therapy as a treatment for chronic depression: A preliminary study. Behaviour research and therapy. 2009;47:366–373. doi: 10.1016/j.brat.2009.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Farb NA, et al. Minding one’s emotions: mindfulness training alters the neural expression of sadness. Emotion. 2010;10:25–33. doi: 10.1037/a0017151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Paul NA, et al. Psychological and neural mechanisms of trait mindfulness in reducing depression vulnerability. Social cognitive and affective neuroscience. 2013;8:56–64. doi: 10.1093/scan/nss070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Teasdale JD, et al. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of consulting and clinical psychology. 2000;68:615–623. doi: 10.1037//0022-006x.68.4.615. [DOI] [PubMed] [Google Scholar]
- 36.Zeidan F, et al. Effects of brief and sham mindfulness meditation on mood and cardiovascular variables. Journal of alternative and complementary medicine. 2010;16:867–873. doi: 10.1089/acm.2009.0321. [DOI] [PubMed] [Google Scholar]
- 37.Taren AA, et al. Mindfulness meditation training alters stress-related amygdala resting state functional connectivity: a randomized controlled trial. Social cognitive and affective neuroscience. 2015;10:1758–1768. doi: 10.1093/scan/nsv066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Creswell JD, et al. Brief mindfulness meditation training alters psychological and neuroendocrine responses to social evaluative stress. Psychoneuroendocrinology. 2014;44:1–12. doi: 10.1016/j.psyneuen.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 39.Creswell JD, et al. Mindfulness-Based Stress Reduction training reduces loneliness and pro-inflammatory gene expression in older adults: a small randomized controlled trial. Brain, behavior, and immunity. 2012;26:1095–1101. doi: 10.1016/j.bbi.2012.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Allen M, et al. Cognitive-affective neural plasticity following active-controlled mindfulness intervention. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2012;32:15601–15610. doi: 10.1523/JNEUROSCI.2957-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84:822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 42.Garland EL, et al. Mindfulness training modifies cognitive, affective, and physiological mechanisms implicated in alcohol dependence: results of a randomized controlled pilot trial. J Psychoactive Drugs. 2011;42:177–192. doi: 10.1080/02791072.2010.10400690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schofield TP, Creswell JD, Denson TF. Brief mindfulness induction reduces inattentional blindness. Consciousness and cognition. 2015;37:63–70. doi: 10.1016/j.concog.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 44.Taylor VA, et al. Impact of mindfulness on the neural responses to emotional pictures in experienced and beginner meditators. NeuroImage. 2011;57:1524–1533. doi: 10.1016/j.neuroimage.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 45.Vago DR, Silbersweig DA. Self-awareness, self-regulation, and self-transcendence (S-ART): a framework for understanding the neurobiological mechanisms of mindfulness. Frontiers in human neuroscience. 2012;6:296. doi: 10.3389/fnhum.2012.00296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zeidan F, et al. Mindfulness meditation improves cognition: evidence of brief mental training. Consciousness and cognition. 2010;19:597–605. doi: 10.1016/j.concog.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 47.Zeidan F. The Neurobiology of Mindfulness Meditation. In: Brown KW, Creswell JD, Ryan RM, editors. Handbook of Mindfulness Science: Theory, Research and Practice. The Guilford Press; New York, New York: 2015. [Google Scholar]
- 48.Creswell JD, et al. Neural correlates of dispositional mindfulness during affect labeling. Psychosomatic medicine. 2007;69:560–565. doi: 10.1097/PSY.0b013e3180f6171f. [DOI] [PubMed] [Google Scholar]
- 49.Taren AA, Creswell JD, Gianaros PJ. Dispositional mindfulness co-varies with smaller amygdala and caudate volumes in community adults. PloS one. 2013;8:e64574. doi: 10.1371/journal.pone.0064574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Way BM, et al. Dispositional mindfulness and depressive symptomatology: correlations with limbic and self-referential neural activity during rest. Emotion. 2010;10:12–24. doi: 10.1037/a0018312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lutz A, et al. Attention regulation and monitoring in meditation. Trends in cognitive sciences. 2008;12:163–169. doi: 10.1016/j.tics.2008.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wallace BA. The Attention Revolution: Unlocking the Power of the Focused Mind. Wisdom Publications; Somerville: 2006. [Google Scholar]
- 53.Clark WC, Clark SB. Pain responses in Nepalese porters. Science. 1980;209:410–412. doi: 10.1126/science.7384815. [DOI] [PubMed] [Google Scholar]
- 54.Morone NE, et al. “I felt like a new person.” the effects of mindfulness meditation on older adults with chronic pain: qualitative narrative analysis of diary entries. The journal of pain : official journal of the American Pain Society. 2008;9:841–848. doi: 10.1016/j.jpain.2008.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Morone NE, et al. A Mind-Body Program for Older Adults With Chronic Low Back Pain: A Randomized Clinical Trial. JAMA internal medicine. 2016;176:329–337. doi: 10.1001/jamainternmed.2015.8033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Morone NE, et al. A mind-body program for older adults with chronic low back pain: results of a pilot study. Pain medicine. 2009;10:1395–1407. doi: 10.1111/j.1526-4637.2009.00746.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Garland EL, et al. Mindfulness-oriented recovery enhancement for chronic pain and prescription opioid misuse: results from an early-stage randomized controlled trial. Journal of consulting and clinical psychology. 2014;82:448–459. doi: 10.1037/a0035798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.de Boer MJ, et al. Mindfulness, acceptance and catastrophizing in chronic pain. PloS one. 2014;9:e87445. doi: 10.1371/journal.pone.0087445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Garland EL, Howard MO. Mindfulness-oriented recovery enhancement reduces pain attentional bias in chronic pain patients. Psychotherapy and psychosomatics. 2013;82:311–318. doi: 10.1159/000348868. [DOI] [PubMed] [Google Scholar]
- 60.Ussher M, et al. Immediate effects of a brief mindfulness-based body scan on patients with chronic pain. Journal of behavioral medicine. 2014;37:127–134. doi: 10.1007/s10865-012-9466-5. [DOI] [PubMed] [Google Scholar]
- 61.Fox SD, Flynn E, Allen RH. Mindfulness meditation for women with chronic pelvic pain: a pilot study. The Journal of reproductive medicine. 2011;56:158–162. [PubMed] [Google Scholar]
- 62.Cho S, et al. Pain-related anxiety as a mediator of the effects of mindfulness on physical and psychosocial functioning in chronic pain patients in Korea. The journal of pain : official journal of the American Pain Society. 2010;11:789–797. doi: 10.1016/j.jpain.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 63.Rosenzweig S, et al. Mindfulness-based stress reduction for chronic pain conditions: variation in treatment outcomes and role of home meditation practice. Journal of psychosomatic research. 2010;68:29–36. doi: 10.1016/j.jpsychores.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 64.McCracken LM, Velleman SC. Psychological flexibility in adults with chronic pain: a study of acceptance, mindfulness, and values-based action in primary care. Pain. 2010;148:141–147. doi: 10.1016/j.pain.2009.10.034. [DOI] [PubMed] [Google Scholar]
- 65.McCracken LM, Keogh E. Acceptance, mindfulness, and values-based action may counteract fear and avoidance of emotions in chronic pain: an analysis of anxiety sensitivity. The journal of pain : official journal of the American Pain Society. 2009;10:408–415. doi: 10.1016/j.jpain.2008.09.015. [DOI] [PubMed] [Google Scholar]
- 66.McCracken LM, Gauntlett-Gilbert J, Vowles KE. The role of mindfulness in a contextual cognitive-behavioral analysis of chronic pain-related suffering and disability. Pain. 2007;131:63–69. doi: 10.1016/j.pain.2006.12.013. [DOI] [PubMed] [Google Scholar]
- 67.Davis MC, Zautra AJ. An online mindfulness intervention targeting socioemotional regulation in fibromyalgia: results of a randomized controlled trial. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine. 2013;46:273–284. doi: 10.1007/s12160-013-9513-7. [DOI] [PubMed] [Google Scholar]
- 68.Wells RE, et al. Meditation for migraines: a pilot randomized controlled trial. Headache. 2014;54:1484–1495. doi: 10.1111/head.12420. [DOI] [PubMed] [Google Scholar]
- 69.Day MA, et al. Toward a theoretical model for mindfulness-based pain management. The journal of pain : official journal of the American Pain Society. 2014;15:691–703. doi: 10.1016/j.jpain.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 70.Hoy D, et al. A systematic review of the global prevalence of low back pain. Arthritis and rheumatism. 2012;64:2028–2037. doi: 10.1002/art.34347. [DOI] [PubMed] [Google Scholar]
- 71.Cherkin DC, et al. Effect of Mindfulness-Based Stress Reduction vs Cognitive Behavioral Therapy or Usual Care on Back Pain and Functional Limitations in Adults With Chronic Low Back Pain: A Randomized Clinical Trial. Jama. 2016;315:1240–1249. doi: 10.1001/jama.2016.2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Basbaum AI, Fields HL. Endogenous pain control systems: brainstem spinal pathways and endorphin circuitry. Annu Rev Neurosci. 1984;7:309–338. doi: 10.1146/annurev.ne.07.030184.001521. [DOI] [PubMed] [Google Scholar]
- 73.Coghill RC, McHaffie JG, Yen YF. Neural correlates of interindividual differences in the subjective experience of pain. Proceedings of the National Academy of Sciences of the United States of America. 2003;100:8538–8542. doi: 10.1073/pnas.1430684100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Coghill RC, et al. Pain intensity processing within the human brain: a bilateral, distributed mechanism. Journal of neurophysiology. 1999;82:1934–1943. doi: 10.1152/jn.1999.82.4.1934. [DOI] [PubMed] [Google Scholar]
- 75.Coghill RC, et al. Distributed processing of pain and vibration by the human brain. The Journal of neuroscience : the official journal of the Society for Neuroscience. 1994;14:4095–4108. doi: 10.1523/JNEUROSCI.14-07-04095.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Derbyshire SW, et al. Pain processing during three levels of noxious stimulation produces differential patterns of central activity. Pain. 1997;73:431–445. doi: 10.1016/S0304-3959(97)00138-3. [DOI] [PubMed] [Google Scholar]
- 77.Tracey I, Mantyh PW. The cerebral signature for pain perception and its modulation. Neuron. 2007;55:377–391. doi: 10.1016/j.neuron.2007.07.012. [DOI] [PubMed] [Google Scholar]
- 78.Wiech K, Ploner M, Tracey I. Neurocognitive aspects of pain perception. Trends in cognitive sciences. 2008;12:306–313. doi: 10.1016/j.tics.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 79.Oshiro Y, et al. Brain mechanisms supporting spatial discrimination of pain. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2007;27:3388–3394. doi: 10.1523/JNEUROSCI.5128-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Oshiro Y, et al. Brain mechanisms supporting discrimination of sensory features of pain: a new model. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2009;29:14924–14931. doi: 10.1523/JNEUROSCI.5538-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lobanov OV, et al. Frontoparietal mechanisms supporting attention to location and intensity of painful stimuli. Pain. 2013;154:1758–1768. doi: 10.1016/j.pain.2013.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lobanov OV, et al. From cue to meaning: Brain mechanisms supporting the construction of expectations of pain. Pain. 2013 doi: 10.1016/j.pain.2013.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bushnell MC, Ceko M, Low LA. Cognitive and emotional control of pain and its disruption in chronic pain. Nature reviews Neuroscience. 2013;14:502–511. doi: 10.1038/nrn3516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kong J, et al. Using fMRI to dissociate sensory encoding from cognitive evaluation of heat pain intensity. Human brain mapping. 2006;27:715–721. doi: 10.1002/hbm.20213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Petrovic P, Ingvar M. Imaging cognitive modulation of pain processing. Pain. 2002;95:1–5. doi: 10.1016/s0304-3959(01)00467-5. [DOI] [PubMed] [Google Scholar]
- 86.Seminowicz DA, Mikulis DJ, Davis KD. Cognitive modulation of pain-related brain responses depends on behavioral strategy. Pain. 2004;112:48–58. doi: 10.1016/j.pain.2004.07.027. [DOI] [PubMed] [Google Scholar]
- 87.Villemure C, Bushnell MC. Cognitive modulation of pain: how do attention and emotion influence pain processing? Pain. 2002;95:195–199. doi: 10.1016/S0304-3959(02)00007-6. [DOI] [PubMed] [Google Scholar]
- 88.Millan MJ. Descending control of pain. Progress in neurobiology. 2002;66:355–474. doi: 10.1016/s0301-0082(02)00009-6. [DOI] [PubMed] [Google Scholar]
- 89.Eippert F, et al. Activation of the opioidergic descending pain control system underlies placebo analgesia. Neuron. 2009;63:533–543. doi: 10.1016/j.neuron.2009.07.014. [DOI] [PubMed] [Google Scholar]
- 90.Grevert P, Albert LH, Goldstein A. Partial antagonism of placebo analgesia by naloxone. Pain. 1983;16:129–143. doi: 10.1016/0304-3959(83)90203-8. [DOI] [PubMed] [Google Scholar]
- 91.Levine JD, Gordon NC, Fields HL. The mechanism of placebo analgesia. Lancet. 1978;2:654–657. doi: 10.1016/s0140-6736(78)92762-9. [DOI] [PubMed] [Google Scholar]
- 92.Zubieta JK, et al. Placebo effects mediated by endogenous opioid activity on mu-opioid receptors. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2005;25:7754–7762. doi: 10.1523/JNEUROSCI.0439-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Amanzio M, Benedetti F. Neuropharmacological dissection of placebo analgesia: expectation-activated opioid systems versus conditioning-activated specific subsystems. The Journal of neuroscience : the official journal of the Society for Neuroscience. 1999;19:484–494. doi: 10.1523/JNEUROSCI.19-01-00484.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.King CD, et al. Reduction of conditioned pain modulation in humans by naltrexone: an exploratory study of the effects of pain catastrophizing. J Behav Med. 2013;36:315–327. doi: 10.1007/s10865-012-9424-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Harris RE, et al. Traditional Chinese acupuncture and placebo (sham) acupuncture are differentiated by their effects on mu-opioid receptors (MORs) NeuroImage. 2009;47:1077–1085. doi: 10.1016/j.neuroimage.2009.05.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Stephenson JB. Reversal of hypnosis-induced analgesia by naloxone. Lancet. 1978;2:991–992. doi: 10.1016/s0140-6736(78)92552-7. [DOI] [PubMed] [Google Scholar]
- 97.Sprenger C, et al. Attention modulates spinal cord responses to pain. Current biology : CB. 2012;22:1019–1022. doi: 10.1016/j.cub.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 98.Tracey I, et al. Imaging attentional modulation of pain in the periaqueductal gray in humans. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2002;22:2748–2752. doi: 10.1523/JNEUROSCI.22-07-02748.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Valet M, et al. Distraction modulates connectivity of the cingulo-frontal cortex and the midbrain during pain--an fMRI analysis. Pain. 2004;109:399–408. doi: 10.1016/j.pain.2004.02.033. [DOI] [PubMed] [Google Scholar]
- 100.Koyama T, et al. The subjective experience of pain: where expectations become reality. Proceedings of the National Academy of Sciences of the United States of America. 2005;102:12950–12955. doi: 10.1073/pnas.0408576102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Zeidan F, et al. Brain Mechanisms Supporting Violated Expectations of Pain. Pain. 2015 doi: 10.1097/j.pain.0000000000000231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Salomons TV, et al. Individual differences in the effects of perceived controllability on pain perception: critical role of the prefrontal cortex. Journal of cognitive neuroscience. 2007;19:993–1003. doi: 10.1162/jocn.2007.19.6.993. [DOI] [PubMed] [Google Scholar]
- 103.Wager TD, et al. Predicting individual differences in placebo analgesia: contributions of brain activity during anticipation and pain experience. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2011;31:439–452. doi: 10.1523/JNEUROSCI.3420-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Wager TD, et al. Placebo-induced changes in FMRI in the anticipation and experience of pain. Science. 2004;303:1162–1167. doi: 10.1126/science.1093065. [DOI] [PubMed] [Google Scholar]
- 105.Wager TD, Scott DJ, Zubieta JK. Placebo effects on human mu-opioid activity during pain. Proceedings of the National Academy of Sciences of the United States of America. 2007;104:11056–11061. doi: 10.1073/pnas.0702413104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Rainville P. Brain mechanisms of pain affect and pain modulation. Current opinion in neurobiology. 2002;12:195–204. doi: 10.1016/s0959-4388(02)00313-6. [DOI] [PubMed] [Google Scholar]
- 107.Rainville P, et al. Dissociation of sensory and affective dimensions of pain using hypnotic modulation. Pain. 1999;82:159–171. doi: 10.1016/S0304-3959(99)00048-2. [DOI] [PubMed] [Google Scholar]
- 108.Rainville P, et al. Pain affect encoded in human anterior cingulate but not somatosensory cortex. Science. 1997;277:968–971. doi: 10.1126/science.277.5328.968. [DOI] [PubMed] [Google Scholar]
- 109.Roy M, et al. The modulation of pain by attention and emotion: a dissociation of perceptual and spinal nociceptive processes. European journal of pain. 2011;15:641 e641–610. doi: 10.1016/j.ejpain.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 110.Roy M, et al. Cerebral and spinal modulation of pain by emotions. Proceedings of the National Academy of Sciences of the United States of America. 2009;106:20900–20905. doi: 10.1073/pnas.0904706106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Casey KL, et al. Selective opiate modulation of nociceptive processing in the human brain. Journal of neurophysiology. 2000;84:525–533. doi: 10.1152/jn.2000.84.1.525. [DOI] [PubMed] [Google Scholar]
- 112.Willoch F, et al. Central poststroke pain and reduced opioid receptor binding within pain processing circuitries: a [11C]diprenorphine PET study. Pain. 2004;108:213–220. doi: 10.1016/j.pain.2003.08.014. [DOI] [PubMed] [Google Scholar]
- 113.Adler LJ, et al. Regional brain activity changes associated with fentanyl analgesia elucidated by positron emission tomography. Anesthesia and analgesia. 1997;84:120–126. doi: 10.1097/00000539-199701000-00023. [DOI] [PubMed] [Google Scholar]
- 114.Willoch F, et al. Central pain after pontine infarction is associated with changes in opioid receptor binding: a PET study with 11C-diprenorphine. AJNR Am J Neuroradiol. 1999;20:686–690. [PMC free article] [PubMed] [Google Scholar]
- 115.Jones AK, et al. In vivo distribution of opioid receptors in man in relation to the cortical projections of the medial and lateral pain systems measured with positron emission tomography. Neuroscience letters. 1991;126:25–28. doi: 10.1016/0304-3940(91)90362-w. [DOI] [PubMed] [Google Scholar]
- 116.Floyd NS, et al. Orbitomedial prefrontal cortical projections to distinct longitudinal columns of the periaqueductal gray in the rat. J Comp Neurol. 2000;422:556–578. doi: 10.1002/1096-9861(20000710)422:4<556::aid-cne6>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 117.Beitz AJ. The organization of afferent projections to the midbrain periaqueductal gray of the rat. Neuroscience. 1982;7:133–159. doi: 10.1016/0306-4522(82)90157-9. [DOI] [PubMed] [Google Scholar]
- 118.Mantyh PW. Connections of midbrain periaqueductal gray in the monkey. II. Descending efferent projections. J Neurophysiol. 1983;49:582–594. doi: 10.1152/jn.1983.49.3.582. [DOI] [PubMed] [Google Scholar]
- 119.Mantyh PW. Connections of midbrain periaqueductal gray in the monkey. I. Ascending efferent projections. J Neurophysiol. 1983;49:567–581. doi: 10.1152/jn.1983.49.3.567. [DOI] [PubMed] [Google Scholar]
- 120.Liebeskind JC, et al. Analgesia from electrical stimulation of the periaqueductal gray matter in the cat: behavioral observations and inhibitory effects on spinal cord interneurons. Brain Res. 1973;50:441–446. doi: 10.1016/0006-8993(73)90748-8. [DOI] [PubMed] [Google Scholar]
- 121.Grant JA, Rainville P. Pain sensitivity and analgesic effects of mindful states in Zen meditators: a cross-sectional study. Psychosomatic medicine. 2009;71:106–114. doi: 10.1097/PSY.0b013e31818f52ee. [DOI] [PubMed] [Google Scholar]
- 122.Perlman DM, et al. Differential effects on pain intensity and unpleasantness of two meditation practices. Emotion. 2010;10:65–71. doi: 10.1037/a0018440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Carmody J, Baer RA. How long does a mindfulness-based stress reduction program need to be? A review of class contact hours and effect sizes for psychological distress. Journal of clinical psychology. 2009;65:627–638. doi: 10.1002/jclp.20555. [DOI] [PubMed] [Google Scholar]
- 124.Minor HG, et al. Evaluation of a Mindfulness-Based Stress Reduction (MBSR) program for caregivers of children with chronic conditions. Soc Work Health Care. 2006;43:91–109. doi: 10.1300/J010v43n01_06. [DOI] [PubMed] [Google Scholar]
- 125.Bingel U, et al. Mechanisms of placebo analgesia: rACC recruitment of a subcortical antinociceptive network. Pain. 2006;120:8–15. doi: 10.1016/j.pain.2005.08.027. [DOI] [PubMed] [Google Scholar]
- 126.Villemure C, Bushnell MC. Mood influences supraspinal pain processing separately from attention. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2009;29:705–715. doi: 10.1523/JNEUROSCI.3822-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Eippert F, et al. Regulation of emotional responses elicited by threat-related stimuli. Human brain mapping. 2007;28:409–423. doi: 10.1002/hbm.20291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.O’Doherty J, et al. Abstract reward and punishment representations in the human orbitofrontal cortex. Nature neuroscience. 2001;4:95–102. doi: 10.1038/82959. [DOI] [PubMed] [Google Scholar]
- 129.Peters J, Buchel C. Neural representations of subjective reward value. Behav Brain Res. 2010 doi: 10.1016/j.bbr.2010.04.031. [DOI] [PubMed] [Google Scholar]
- 130.Rolls ET, Grabenhorst F. The orbitofrontal cortex and beyond: from affect to decision-making. Progress in neurobiology. 2008;86:216–244. doi: 10.1016/j.pneurobio.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 131.Starr CJ, et al. Roles of the insular cortex in the modulation of pain: insights from brain lesions. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2009;29:2684–2694. doi: 10.1523/JNEUROSCI.5173-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Critchley HD, et al. Neural systems supporting interoceptive awareness. Nature neuroscience. 2004;7:189–195. doi: 10.1038/nn1176. [DOI] [PubMed] [Google Scholar]
- 133.Medford N, Critchley HD. Conjoint activity of anterior insular and anterior cingulate cortex: awareness and response. Brain Structure and Function. 2010;214:535–549. doi: 10.1007/s00429-010-0265-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Otto T, Zijlstra FR, Goebel R. Neural correlates of mental effort evaluation--involvement of structures related to self-awareness. Social cognitive and affective neuroscience. 2014;9:307–315. doi: 10.1093/scan/nss136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Salomons TV, Kucyi A. Does Meditation Reduce Pain through a Unique Neural Mechanism? The Journal of neuroscience : the official journal of the Society for Neuroscience. 2011;31:12705–12707. doi: 10.1523/JNEUROSCI.2843-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Colloca L, et al. How the number of learning trials affects placebo and nocebo responses. Pain. 2010;151:430–439. doi: 10.1016/j.pain.2010.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Lui F, et al. Neural bases of conditioned placebo analgesia. Pain. 2010;151:816–824. doi: 10.1016/j.pain.2010.09.021. [DOI] [PubMed] [Google Scholar]
- 138.Creswell JD, et al. Alterations in Resting-State Functional Connectivity Link Mindfulness Meditation With Reduced Interleukin-6: A Randomized Controlled Trial. Biological psychiatry. 2016 doi: 10.1016/j.biopsych.2016.01.008. [DOI] [PubMed] [Google Scholar]
- 139.MacCoon DG, et al. The validation of an active control intervention for Mindfulness Based Stress Reduction (MBSR) Behaviour research and therapy. 2012;50:3–12. doi: 10.1016/j.brat.2011.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.MacCoon DG, et al. No sustained attention differences in a longitudinal randomized trial comparing mindfulness based stress reduction versus active control. PloS one. 2014;9:e97551. doi: 10.1371/journal.pone.0097551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Rosenkranz MA, et al. A comparison of mindfulness-based stress reduction and an active control in modulation of neurogenic inflammation. Brain, behavior, and immunity. 2013;27:174–184. doi: 10.1016/j.bbi.2012.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Zeidan F, et al. The effects of brief mindfulness meditation training on experimentally induced pain. The journal of pain : official journal of the American Pain Society. 2010;11:199–209. doi: 10.1016/j.jpain.2009.07.015. [DOI] [PubMed] [Google Scholar]
- 143.White G. Natural History and Antiquities of Selborne. Cassell and Company; London, England: 1908. [Google Scholar]
- 144.Benson H, Greenwood MM, Klemchuk H. The relaxation response: psychophysiologic aspects and clinical applications. International journal of psychiatry in medicine. 1975;6:87–98. doi: 10.2190/376W-E4MT-QM6Q-H0UM. [DOI] [PubMed] [Google Scholar]
- 145.Petrovic P, et al. Placebo and opioid analgesia-- imaging a shared neuronal network. Science. 2002;295:1737–1740. doi: 10.1126/science.1067176. [DOI] [PubMed] [Google Scholar]
- 146.Bantick SJ, et al. Imaging how attention modulates pain in humans using functional MRI. Brain : a journal of neurology. 2002;125:310–319. doi: 10.1093/brain/awf022. [DOI] [PubMed] [Google Scholar]
- 147.Bandura A, et al. Perceived self-efficacy and pain control: opioid and nonopioid mechanisms. J Pers Soc Psychol. 1987;53:563–571. doi: 10.1037//0022-3514.53.3.563. [DOI] [PubMed] [Google Scholar]
- 148.Borras MC, et al. fMRI measurement of CNS responses to naloxone infusion and subsequent mild noxious thermal stimuli in healthy volunteers. Journal of neurophysiology. 2004;91:2723–2733. doi: 10.1152/jn.00249.2003. [DOI] [PubMed] [Google Scholar]
- 149.Watkins LR, Mayer DJ. Organization of endogenous opiate and nonopiate pain control systems. Science. 1982;216:1185–1192. doi: 10.1126/science.6281891. [DOI] [PubMed] [Google Scholar]
- 150.Dahl CJ, Lutz A, Davidson RJ. Reconstructing and deconstructing the self: cognitive mechanisms in meditation practice. Trends in cognitive sciences. 2015;19:515–523. doi: 10.1016/j.tics.2015.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Shapiro SL, et al. Mechanisms of mindfulness. Journal of clinical psychology. 2006;62:373–386. doi: 10.1002/jclp.20237. [DOI] [PubMed] [Google Scholar]
- 152.Institute of Medicine (US) Committee on Advancing Pain Research, C., and Education. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. National Academies Press; Washington D.C: 2011. [PubMed] [Google Scholar]
- 153.Wilkerson RG, et al. The Opioid Epidemic in the United States. Emergency medicine clinics of North America. 2016;34:e1–e23. doi: 10.1016/j.emc.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 154.Stempniak M. The Opioid Epidemic. Hospitals & health networks / AHA. 2016;90:22–24. 26–29. [PubMed] [Google Scholar]
- 155.Garland EL, et al. The downward spiral of chronic pain, prescription opioid misuse, and addiction: cognitive, affective, and neuropsychopharmacologic pathways. Neuroscience and biobehavioral reviews. 2013;37:2597–2607. doi: 10.1016/j.neubiorev.2013.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Bowen S, Enkema MC. Relationship between dispositional mindfulness and substance use: findings from a clinical sample. Addictive behaviors. 2014;39:532–537. doi: 10.1016/j.addbeh.2013.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Witkiewitz K, Bowen S. Depression, craving, and substance use following a randomized trial of mindfulness-based relapse prevention. Journal of consulting and clinical psychology. 2010;78:362–374. doi: 10.1037/a0019172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Bowen S, et al. Mindfulness-based relapse prevention for substance use disorders: a pilot efficacy trial. Substance abuse. 2009;30:295–305. doi: 10.1080/08897070903250084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Eisendrath S, Chartier M, McLane M. Adapting Mindfulness-Based Cognitive Therapy for Treatment-Resistant Depression: A Clinical Case Study. Cognitive and behavioral practice. 2011;18:362–370. doi: 10.1016/j.cbpra.2010.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Eisendrath SJ, et al. Mindfulness-based cognitive therapy (MBCT) versus the health-enhancement program (HEP) for adults with treatment-resistant depression: a randomized control trial study protocol. BMC complementary and alternative medicine. 2014;14:95. doi: 10.1186/1472-6882-14-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Williams JM, et al. Mindfulness-based cognitive therapy for preventing relapse in recurrent depression: a randomized dismantling trial. Journal of consulting and clinical psychology. 2014;82:275–286. doi: 10.1037/a0035036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Goldin P, et al. MBSR vs aerobic exercise in social anxiety: fMRI of emotion regulation of negative self-beliefs. Social cognitive and affective neuroscience. 2013;8:65–72. doi: 10.1093/scan/nss054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Kabat-Zinn J, et al. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. American Journal of Psychiatry. 1992;149:936–943. doi: 10.1176/ajp.149.7.936. [DOI] [PubMed] [Google Scholar]
- 164.Price DD, Barell JJ. Inner Experience and Neuroscience. MIT Press; Cambridge, MA: 2012. [Google Scholar]
- 165.Price DD, Harkins SW, Baker C. Sensory-affective relationships among different types of clinical and experimental pain. Pain. 1987;28:297–307. doi: 10.1016/0304-3959(87)90065-0. [DOI] [PubMed] [Google Scholar]