Summary
Objectives
Transitions in patient care pose an increased risk to patient safety. One way to reduce this risk is to ensure accurate medication reconciliation during the transition. Here we present an evaluation of an electronic medication reconciliation module we developed to reduce the transition risk in patients referred for home healthcare.
Methods
Nineteen physicians with experience in managing home health referrals were recruited to participate in this within-subjects experiment. Participants completed medication reconciliation for three clinical cases in each of two conditions. The first condition (paper-based) simulated current practice – reconciling medication discrepancies between a paper plan of care (CMS 485) and a simulated Electronic Health Record (EHR). For the second condition (electronic) participants used our medication reconciliation module, which we integrated into the simulated EHR. To evaluate the effectiveness of our medication reconciliation module, we employed repeated measures ANOVA to test the hypotheses that the module will: 1) Improve accuracy by reducing the number of unaddressed medication discrepancies, 2) Improve efficiency by reducing the reconciliation time, 3) have good perceived usability.
Results
The improved accuracy hypothesis is supported. Participants left more discrepancies unaddressed in the paper-based condition than the electronic condition, F (1,1) = 22.3, p < 0.0001 (Paper Mean = 1.55, SD = 1.20; Electronic Mean = 0.45, SD = 0.65). However, contrary to our efficiency hypothesis, participants took the same amount of time to complete cases in the two conditions, F (1, 1) =0.007, p = 0.93 (Paper Mean = 258.7 seconds, SD = 124.4; Electronic Mean = 260.4 seconds, SD = 158.9). The usability hypothesis is supported by a composite mean ability and confidence score of 6.41 on a 7-point scale, 17 of 19 participants preferring the electronic system and an SUS rating of 86.5.
Conclusion
We present the evaluation of an electronic medication reconciliation module that increases detection and resolution of medication discrepancies compared to a paper-based process. Further work to integrate medication reconciliation within an electronic medical record is warranted.
Keywords: Medication reconciliation, medical transition care, electronic medical records, patient safety, home health agency referrals
1. Background
Patients are particularly at risk for adverse events and readmission during transitions in care [1, 2]. A common source of risk for adverse events and readmission associated with transitions in care is failure to correctly reconcile the patient’s medications as they move from one care setting to the next [3, 4]. The Joint Commission on Accreditation of Healthcare Organizations (JCAHO) defines medication reconciliation as “the process of comparing a patient’s medication orders to all of the medications that the patient has been taking” [5].
A provider engaged in the process of medication reconciliation must detect differences in medication lists, determine the reasons for discrepancies (e.g. did another provider change the prescription? Is the patient non-adherent?), and decide which prescription is most appropriate for the patient. The provider must then change medication orders and records as needed so that the patient receives the correct medications [6]. In this project our team developed an electronic module intended to provide cognitive support for physicians as they engage in medication reconciliation. In this paper we describe the evaluation of the module regarding its effects on the accuracy and efficiency of medication reconciliation as well the perceived usability of the module.
1.1 Other Researchers’ Work
Several research groups have reported on the design or evaluation of technology-based tools to detect and resolve discrepancies in medication lists [7–9]. Some of these studies have focused on the inpatient setting, in which the workflow of medication reconciliation differs significantly from the home health setting [7]. Other studies have provided design requirements for a tool but have not evaluated its effects on providers [9]. In one case where a medication reconciliation tool was evaluated, reduction in medication discrepancies, and reductions in time to complete reconciliation were reported [8]. One limitation of that tool is it was developed as a stand-alone system, isolated from the Electronic Health Record (EHR) (the primary information tool that providers use in their daily work) [8]. In this project we sought to design and evaluate an electronic module that is intended to be integrated with the EHR and support medication reconciliation and related communication between referring and home health providers for efficient and accurate patient care.
1.2 Our Previous Qualitative Work
Prior to this study we held several group and individual interviews with Veterans Health Administration (VA) clinicians, and Home Health (HH) clinical and IT personnel. During these interviews we discussed the current process of referral and how the HH agency responds. A referral is typically generated by a VA clinician under the direction of a physician, signed electronically by the physician and then sent to the HH agency. If the referral includes skilled nursing care, a nurse is sent to the patient’s home to conduct an assessment, develop a plan of care and initiate the plan of care. During the initial assessment in the patient’s home the nurse reviews the medications the patient (and/or caregivers) report that the patient is taking – compiling a “home health” medication list that includes the medication, form, dose and frequency. The HH plan of care is sent as a paper form back to the VA providers for approval. The HH plan of care contains services to be provided, clinical goals, observations and the medication list compiled by the home health nurse. During our preliminary interviews with VA clinical providers we noted how providers detect and reconcile discrepancies between the VA medication list and medications on the HH plan of care. We observed that referring providers make medication reconciliation notes (e.g., changes in medications’ dose or frequency) directly on the paper HH plan of care. Referring providers noted that the reconciliation process is often tedious with potential for failure to detect or correct discrepancies. Some physicians reported having residents, nurse care managers or pharmacists review the medication lists, identify discrepancies and gather relevant information before they would review and sign the HH plan of care. At times, the reconciliation process may also include phone calls between team members and the HH nurse to clarify or correct high-risk discrepancies.
2. Method
2.1 Electronic Module Design
Based on our previous qualitative work we developed an initial design for an electronic medication reconciliation module. We focused on the two medication lists that are part of the referral and response process. The first medication list is the patient’s current VA medication list that is included in the initial referral. The second is the medication list on the HH plan of care. Using principles of user-centered design we developed paper prototypes of the module’s user interface [10, 11]. We shared the paper prototypes with a small sample of VA physicians to iteratively refine and expand the design. As we developed the electronic module we continued to iteratively refine its appearance and functionality by ad-hoc testing with some of the same physicians who had interacted with the paper prototypes as well as a few physicians who were naïve to the module.
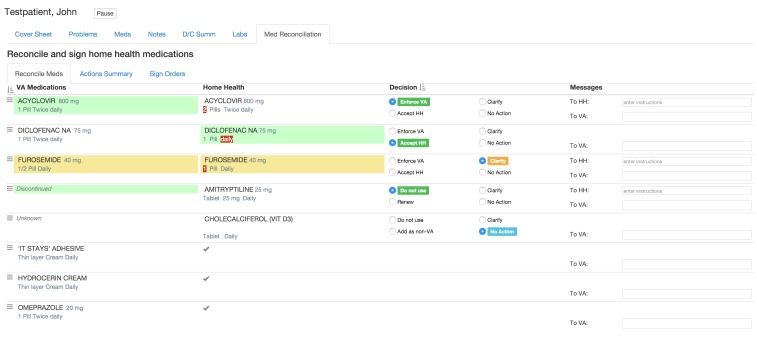
Our design starts from our observation assumption that the medication list sent on the referral is the point of reference for providers reconciling the medication lists, and discrepancies are defined in terms of differences relative to this list. As depicted in ► Figure 1, the module presents the referring provider’s medication list, labeled “VA medications,” as the reference list and the home health list, labeled “Home Health,” as a list of discrepancies relative to the reference list. The display uses visual cues to alert the user to each potentially relevant medication discrepancy. Medications are sorted based on the types of discrepancy between the lists: dose and frequency discrepancies are shown at the top, followed by VA medications that are missing from the HH list, then medications on the Home Health list that are not on the VA list. Medications with no discrepancy between the lists are shown at the bottom. This design is intended to maximize the relevant information gained for the effort expended.
Fig. 1.
Screenshot of Electronic Module
We noted that when physicians considered discrepancies, they had questions about the history of the medication use, (e.g., when was the medication prescribed and why) and the therapeutic value or effect as measured by lab values. Answering these questions requires access to the patient medical history that will be available when the module is integrated into the actual electronic health record.
The module is also designed to facilitate efficient action. Selecting an action can be accomplished by clicking on the medication in the VA Medications list to “Enforce VA” or by clicking on the medication in the Home Health list to “Accept HH.” These actions can also be accomplished by selecting the corresponding radio button in the “Decision” column. The background color of a medication entry changes to green to indicate what has been selected; this provides direct feedback to the user on their actions. Users can also select “Clarify” to denote the need for more information. When Clarify is selected the background color of both the VA and HH entries changes to yellow. A user can enter a question or request in the “Messages” column to request clarification on any aspect of the medication (e.g., who prescribed, does the dose accurately reflect what the patient is taking, etc.). Messages can be directed to either home health providers (“To HH:”) or to a colleague at their facility (“To VA:”). It should be noted that message creation and routing was not the focus of our initial design and evaluation.
2.2 Study Design
To test our electronic module, we designed a study based on three primary hypotheses.
The electronic module will improve reconciliation accuracy by reducing the number of unaddressed medication discrepancies between medication lists.
The electronic module will improve efficiency by reducing the time required to reconcile the medication lists.
-
The electronic module will have good usability as measured by
Users’ perception of the ability to detect and correct discrepancies with confidence in the overall process.
Users’ preference for use of the electronic module over the paper-based process.
User’s ratings on a widely used System Usability Scale (SUS).
Participants
Participants were 19 MDs who had experience in home healthcare referrals and were familiar with the home health plan of care (CMS-485) certification process (see ► Table 1). All participants were associated with the George E. Wahlen VA Medical Center in Salt Lake City, Utah, and had experience with the VA Computerized Patient Records System (CPRS). Participants were recruited via email and in-person contact (staff meetings and clinical in-services). None of the participants had prior exposure to the design or prototypes of the medication reconciliation module.
Table 1.
Participant demographics
| Characteristic | Mean (standard deviation) |
|---|---|
| Sex | 11 Females, 8 Males |
| Attending/Resident | 17 attending physicians, 2 residents |
| Age | 39.8 (6.1) |
| Years since medical school | 12.3 (7.3) |
| Home health referral/month | 8.2 (11.5) |
| Home health CMS 485’s reviewed/month | 9.9 (9.1) |
Design
The study was a within-subjects design comparing the paper-based process to use of the electronic module. Participants viewed and reconciled three simulated patient cases using a paper-based process – similar to the current reconciliation method used at the George E Wahlen VAMC – followed by three simulated patient cases using our electronic module.
We developed 6 simulated clinical cases. For each simulated case, we incorporated either four or six medication discrepancies between the home health (HH) list and the VA list. These manipulated medication discrepancies included, medications added by home health, VA medications missing from the home health list, and discrepancies in dose or schedule between the VA and HH lists. The discrepancies were created by one of the authors (BG) with the intention that each one, if detected, would be deemed by physicians to be sufficiently clinically important to reconcile. For example, one case included the following discrepancies: a blood pressure medication on the home health list that was not prescribed by a VA provider, a uric acid lowering medication (a treatment for gout) prescribed by VA but missing from the home health list, a difference in dose for a cholesterol lowering medication, and a pain medication on the home health list that had been discontinued according to VA records. Since this patient had no history of hypertension, had gout and cardiovascular disease on his problem list, and a reason was noted in his chart for discontinuing the pain medication, each of these discrepancies should have been addressed in the medication reconciliation process. Similar types of discrepancies were created for all cases used in this study. To ensure that the medication discrepancies created for these cases were clinically important and realistic, they were reviewed and revised by two other authors – an experienced geriatrician (RR) and a geriatric nurse practitioner (AB).
Each of the six cases in our study represented a patient who had been referred for home health services and consisted of a returned Home Health Certification and Plan of Care (aka CMS 485) ready for review and approval. To provide a contextual medical history we also developed for each case a minimal simulated Electronic Health Record (EHR) to mimic the Computerized Patient Record System (CPRS) that VA providers use regularly in their clinical practice. This simulated record, depicted in ► Figure 1, consisted of several display panels that are viewable one at a time (tabs); including a patient cover sheet, problem list, medication list, notes (with 3–5 notes per case), a discharge summary and labs tab. To ensure realism and familiarity, the information presented in the simulated EHR consisted of de-identified screenshots of actual clinical records. All cases were de-identified by removing personal identifying information and dates, and were assigned obviously fictitious names for unique identification.
We grouped the 6 cases into 3 pairs by matching the number of medication discrepancies (either four or six discrepancies in each case). To reduce bias due to participants being initially less familiar with the system, we designated one pair as a warm-up. Participants completed the same warm-up cases for each condition (paper-based or electronic). The presentation of the other four cases (2 pairs) was randomized. The presentation system (described below) performed the randomization by using electronically generated numbers in steps. The first step was to randomly assign the order of the pairs. The next step was repeated for each pair, the system randomly assigned one simulated case to the paper-based condition and the other case to the electronic condition.
To conduct the study and record participants’ interactions with our medication reconciliation module and simulated EHR, we developed a client-server software system that managed the data presentation and, as mentioned, facilitated the random case assignment. The system recorded various user actions: start reconciliation case, sign off on the case, switching between different EHR display panels (e.g. Problems, Notes, Labs, and sub-panels in the Med Reconciliation panel as shown in ► Figure 1), sorting or filtering the medication list, and selecting a reconciliation action. Recorded reconciliation actions included information on whether the action was triggered by using the radio buttons or by clicking on the medication itself. We also recorded whether the action meant selection or cancelation (a second click on a medication). For each such event we recorded the time, type of event and any additional related information. In anticipation of potential interruptions during the study due to unforeseen work related emergency calls, we provided a Pause/Continue button. Fortunately, this button was never used. For the paper-based condition we considered the total amount of elapsed time to complete each case by requiring the user to press a Start/Done button (a Pause/Continue button was again provided, but never used by participants). To simulate interaction with CPRS during the paper-based condition we provided users with an additional button to open the simulated EHR display. The paper-based condition EHR display was the same as the electronic-based condition shown in ► Figure1 except the EHR did not include the “Med Reconciliation” tab.
2.3 Procedure
This study was reviewed by the IRB at the University of Utah and the Salt Lake City VA Research and Development Committee and determined to be exempt from requirements of documenting informed consent. Researchers met individually with the participants in a location of the participant’s choice (office, conference room or clinic exam room). Using a laptop, the researcher logged into the system that managed the study and entered a unique participant identifier. A consent cover letter that briefly explained the purpose of the study and participants’ rights was presented first. Participants were oriented to the study by the researcher who used a study guide to help ensure study consistency. Participants were informed that the study was intended to compare the current paper-based process with an electronic process of reconciling the patient’s VA medication list with the medication list found on the Home Health Certification and Plan of Care/CMS 485 (referred to as the HH medication list). To simulate real-world clinical practice, participants were instructed to conduct the review as efficiently as possible, “as if you have just a few minutes between clinic appointments to review these cases.”
Participants first completed the “warm-up” paper case and were then given an opportunity to ask questions. The participants then reconciled two addition paper medication lists. After completing the paper-based process for the three patients, the participants moved to the “warm-up” electronic case followed by two additional electronic cases.
Usability Measures
After the participant completed medication reconciliation for all six cases, we collected demographic information on a paper form (► Table 1). To assess participants’ perceptions of the usability of the electronic medication reconciliation module they were presented with two short paper surveys. The first survey asked participants to rate, on a 1–7 Likert scale (strongly disagree – strongly agree), whether the module improved their ability to detect discrepancies between the VA and HH medication lists, improved their ability to correct discrepancies between the VA and HH medication lists, and improved their confidence in the results of their reconciliation. In addition, participants were asked to choose which of the two processes they would prefer to use in the future (paper process vs. the electronic module). These questions were developed based on our initial qualitative work with physicians in which we observed concerns regarding each of these dimensions: detection of discrepancies (e.g. worries over things being missed), correction of discrepancies (e.g. are notes on the CMS 485 being addressed?) and overall confidence in the process.
Finally, participants completed the System Usability Scale (SUS); the SUS is a widely used “quick and dirty” tool with 10 standard questions (rated on a 1 = strongly disagree to 5 = strongly agree scale) to reflect user’s perceptions of the usability of a system [12].
Measurements
For both the paper-based and electronic conditions we measured the number of discrepancies the user addressed – a count of missing items, dose and frequency discrepancies for each case. The participants’ actions in the electronic medication reconciliation module were exported by the system to an electronic data file for analysis. In the paper-based medication reconciliation condition, participants were instructed to note the discrepancies and make changes to the medication list directly on the paper CMS-485 form. These changes were later coded and entered into an Excel spreadsheet by one author (HK). Participants’ reconciliation time for each case for both conditions was tracked electronically by the system. Participants’ responses to the two usability surveys were entered into an Excel spreadsheet by one author (HK).
2.4 Analysis
We used R statistical computing software [13] for all analyses. Analyses for differences in accuracy and efficiency between the paper-based and electronic conditions were performed using a one-way within-subject ANOVA. Conditions were nested within participants as the error term. The significance threshold was set at p < .05. We considered the first case in each condition (i.e., paper-based and electronic) as a warm-up case and did not include that data in our analyses. The following results are based on the remaining two cases in each condition, for a total analysis of four cases for each of the 19 participants. The analyses for the usability measures are also described and reported below.
3. Results
3.1 Accuracy
In this study we proposed three hypotheses regarding accuracy, efficiency and usability. The first hypothesis postulated that the electronic module would improve reconciliation accuracy as measured by the number of discrepancies between medication lists that were addressed. To test this hypothesis, we compared the number of unaddressed discrepancies between the VA and HH medication lists in the paper-based versus electronic conditions. In comparison to electronic reconciliation, participants left more discrepancies unaddressed in the paper-based reconciliation, F (1,1) = 22.3, p < 0.0001 (Paper Mean = 1.55, SD = 1.20; Electronic Mean = 0.45, SD = 0.65) (► Table 2). This finding supports our hypothesis that the electronic module improves reconciliation accuracy.
Table 2.
Analyses results of first two hypotheses and post-hoc hypothesis
| Related Hypothesis | Operationalization | Paper cases Mean (SD) | Electronic cases Mean (SD) | F-value | p-value |
|---|---|---|---|---|---|
| Improved accuracy | Unaddressed discrepancies | 1.55 (1.20) | 0.45 (0.65) | 21.9 | <0.0001 |
| Improved efficiency | Time (sec) to complete case | 258.76 (124.4) | 260.4 (158.9) | 0.01 | 0.92 |
| Increased search | Tabs viewed within record | 7.1 (2.94) | 15.3 (12.8) | 12.4 | <0.0001 |
3.2 Efficiency
Our second hypothesis postulated that the electronic module would improve efficiency by reducing the time required to reconcile the medication lists compared to the paper-based process. To test this hypothesis, we compared the elapsed time taken to reconcile medication lists using the paper-based process vs. the electronic module. Contrary to our hypothesis, the analysis showed that participants took the same amount of time to complete cases in each condition, F (1, 1) =0.007, p = 0.93 (Paper Mean = 258.7 seconds, SD = 124.4; Electronic Mean = 260.4 seconds, SD = 158.9).
Based on comments participants spontaneously made during the study, we hypothesized that an unintended consequence of the electronic module was that participants were spending more time foraging in the simulated EHR for information related to the appropriateness of medications. This post-hoc hypothesis is supported by examining the number of times participants switched between display panels (i.e., tab switches) in the simulated EHR during the paper-based vs. electronic conditions (by one-way ANOVA) F (1,19) = 12.4, p < 0.0001, (Paper Mean = 7.1 tab switches, SD = 2.94; Electronic Mean = 15.3 tab switches, SD = 12.8) (► Table 2).
3.3 Usability
Our third hypothesis postulated that users would perceive that the electronic module has good usability. Usability measures included questions on perceived improvements in ability to detect and correct discrepancies and confidence in the reconciliation process, identifying a process preference (paper-based or electronic) and a standard System Usability Scale (SUS). To test ability and confidence we calculated the mean and standard deviation across three questions in the post experiment survey – measured on a 7-point Likert scale from 1 = strongly disagree to 7 = strongly agree. The questions were: 1. Using the electronic medication reconciliation module improved my ability to detect discrepancies between the VA medication list and the home health medication list (Mean = 6.6, SD = 0.85). 2. Using the electronic medication reconciliation module improved my ability to correct discrepancies between the VA medication list and the home health medication list (Mean = 6.5, SD = 0.70). 3. Using the electronic medication reconciliation module improved my confidence in the results of my medication reconciliation between the VA medication list and the home health medication lists (Mean = 6.2, SD =1.30). The composite mean ability and confidence score is 6.41 on a 7-point scale (SD = 0.73).
To address the process preference we asked participants to circle the preferred system on the post experiment survey. An overwhelming 17 of 19 participants stated they preferred the electronic module. No participants expressed a preference for the paper-based process; however, 2 participants gave the following qualified responses: “On the right track but not quite there” and “Some combination of the two.” The second comment was followed up with “I think the app is fine” and a complaint about the data in the simulated EHR being incomplete.
We scored the SUS responses per the procedures recommended by Brooke [12]. The mean SUS score was 86.5 (SD = 12.1). While it is important to emphasize that these scores are not percentages, this score does suggest that the system has excellent overall usability when benchmarked against other systems that have been rated using the SUS [14].
3.4 General use
Because we are also interested in how the user interacts with the system, the software system that managed the data presentation also captured data not directly related to our hypotheses. We found that overwhelmingly participants selected the radio button rather than the medication in the VA or HH lists to “Enforce VA” or “Accept Home Health” during the electronic condition (radio button Mean =11.17, SD = 2.77; selection of medication Mean = 1.50, SD = 2.23). Eleven of the participants never selected a medication in the columns. The “Clarify” button was selected at least once by all but two participants, (Mean = 4.22; SD = 3.61; Min = 0, Max = 12).
4. Discussion
In this study we designed and developed an electronic module for medication reconciliation between referring providers and home health. We predicted the electronic module would improve reconciliation accuracy as measured by addressing discrepancies between medication lists. Consistent with our prediction, the electronic module improved the accuracy of medication reconciliation by increasing the number of addressed discrepancies compared to the current paper-based process. However, contrary to our hypothesis and in contrast to a prior study [8] comparing medication lists for electronic medication reconciliation, we found that use of our module did not reduce the overall time to reconcile medication lists as compared to the paper-based process. The times were essentially identical under the two conditions. Based on participant comments and our post-hoc analysis of user’s exploration of the simulated record, we believe participants used the “found time” created by making the mechanics of medication reconciliation more efficient to explore the simulated electronic medical record to determine the appropriateness of the medications. We noted that participants did not explore the patient record as extensively in the paper-based process, even though the same simulated records were available. Specifically, providers moved between display panels (tabs) within the simulated EHR in the electronic condition more than twice as much as in the paper condition. This need for a simple and direct access to the patient record during medication reconciliation is consistent with previous studies that noted providers’ desire for interoperability between medication reconciliation tools and patient records [15].
Our hypothesis that users would perceive good usability in the electronic reconciliation module was supported. Participants reported improved ability to detect and correct discrepancies with increased confidence in the results. The standard SUS rating was recorded as “excellent.” The electronic process was the preferred process and was overwhelmingly well received. A common response was “When can I start using this?”
We note, however, that physicians also requested several changes. A few physicians requested that the module display the matching medications in the HH list fully (instead of with a checkmark) because they wanted to visually confirm the match. Another request called for the ability to change medication prescriptions beyond the intended medication reconciling task (“Enforce VA”, “Accept HH” or “Clarify”). Specifically, physicians wanted the ability to edit the dose and frequency or to remove the medication completely, including medications that matched on both the VA and HH lists. This request emphasizes the need for medication reconciliation functionality to be integrated within the EHR and the value our participants attribute to such an electronic medication reconciliation module.
The results of our study are in concordance with others that sought to identify and increase the salience of discrepancies between medication lists [8, 16]. Not previously explored however, we sought to and were successful in increasing the relevancy of the medication reconciliation task by placing it in context of a transition of care to a home health provider.
4.1 Limitations
There are limitations to our study. Even though our cases were based on real patients, the providers in our study were unfamiliar with the patient’s records. This lack of familiarity may have caused the providers to study the patient records more carefully than usual practice, effectively reducing the error rate. However, we note that lack of familiarity may occur in actual practice, since in some cases the provider reconciling the lists may not be familiar with the patient (e.g., a patient starts with a new primary care provider after being discharged from a hospital). Generalization to real world task performance may also be limited by participants’ awareness of being monitored, potentially leading to a Hawthorne effect. Another potential limitation is the participants’ lack of familiarity with the medication reconciliation module. Task performance may have been impaired because the novelty of the module potentially affected cognitive load as participants created a mental model of module functionality. Finally, testing at a single VA Medical Center may limit the generalizability of this study.
4.2 Future Work.
This study revealed at least two areas requiring more work; information search and communication between stakeholders. Our finding that participants spent more time searching beyond the information presented in a medication reconciliation module underscores the need for additional research that focuses on facilitating efficient information search and summarization capabilities to enrich providers’ information space. The need for enriching the information space and efficient information search has been noted in general Computerized Physician Order Entry (CPOE) research [17]. Specifically, there is a need to explore ways to provide efficient access to prescribing information (e.g., who prescribed and why, how long the patient has been taking the medication, any side effects that have been exhibited), easy access to relevant lab information and access to general information on the medications (e.g., indications for use, formularies and side effects).
Having readily available access to this information is important as determining the reasons behind specific medication utilization and discrepancies can be critical for identifying errors and ensuring accurate medication reconciliation [18]. This raises the urgent need for addition methods and tools to facilitate efficient and secure communication and information exchange between organizations, providers and patients.
Because providers and home health clinicians are generally not part of the same health system and have physical distance between them, there is significant difficulty with effective communication [19]. Recognition of the need for more information is indicated by the extensive use of the “Clarify” button. It is therefore important to develop modes of communication that ensure medication reconciliation and other care issues can be effectively and efficiently addressed.
Work in these two areas should contribute to the general need for improved decision support user-interfaces, best practices for user interactions, and dissemination of guidelines for developing effective EHR tools.
5. Conclusions
In this study we found that electronic medication reconciliation can support more accurate detection and resolution of medication discrepancies than a paper-based process. The electronic module for detection and resolution of discrepancies was overwhelmingly well received and participants requested that it be incorporated into their EHR as soon as possible. In addition, physicians took advantage of the integration with the patient record to verify the appropriateness of medications.
We believe these results suggest that electronic medication reconciliation should be implemented as a tightly integrated component of EHRs in order to support accurate and efficient patient care. Further development and integration of electronic medication reconciliation with the capability to communicate across settings, is warranted to improve transitions in care and patient safety.
Acknowledgment
The research reported here was supported by Pilot Study Grant N19-FY14Q1-S2-P01023 by the United States (U.S.) Department of Veterans Affairs, Veterans Health Administration, Office of Rural Health. Dr. Randall Rupper is the Associate Director, Clinical, Geriatric Research Education and Clinical Center at the George E. Wahlen Department of Veterans Affairs Medical Center, Salt Lake City, Utah
Footnotes
Clinical Relevance Statement
This work is clinically relevant in that it shows the feasibility of electronic medication reconciliation. This work also highlights some strengths and potential weaknesses of electronic medication discrepancy detection and identifies future work.
Conflict of Interest
The authors declare that they have no conflicts of interest in the research.
Human Subjects Protections
This study did not involve medical testing on human subjects. This study was reviewed by our Institutional Review Board and found to be exempt. Participants read a cover letter outlining the intent of our research and were informed they could withdraw from participating at any time with no loss of benefit.
Disclaimer
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
References
- 1.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. The New England journal of medicine 2009; 360(14): 1418-1428. Epub 2009/04/03. doi: 10.1056/NEJMsa0803563. PubMed PMID: 19339721. [DOI] [PubMed] [Google Scholar]
- 2.Mor V, Intrator O, Feng Z, Grabowski DC. The revolving door of rehospitalization from skilled nursing facilities. Health affairs (Project Hope) 2010; 29(1):57–64. Epub 2010/01/06. doi: 10.1377/hlthaff.2009.0629. PubMed PMID: 20048361; PubMed Central PMCID: PMCPMC2826971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stitt DM, Elliott DP, Thompson SN. Medication discrepancies identified at time of hospital discharge in a geriatric population. The American journal of geriatric pharmacotherapy 2011; 9(4): 234-240. Epub 2011/07/19. doi: 10.1016/j.amjopharm.2011.06.002. PubMed PMID: 21763215. [DOI] [PubMed] [Google Scholar]
- 4.Unroe KT, Pfeiffenberger T, Riegelhaupt S, Jastrzembski J, Lokhnygina Y, Colon-Emeric C. Inpatient medication reconciliation at admission and discharge: A retrospective cohort study of age and other risk factors for medication discrepancies. The American journal of geriatric pharmacotherapy 2010; 8(2): 115-126. Epub 2010/05/05. doi: 10.1016/j.amjopharm.2010.04.002. PubMed PMID: 20439061; PubMed Central PMCID: PMCPMC3740385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The Joint Commission. Using medication reconciliation to prevent errors Sentinel Event Alert Issue 35. Epub January 25, 2006. [PubMed] [Google Scholar]
- 6.Varkey P, Cunningham J, O’Meara J, Bonacci R, Desai N, Sheeler R. Multidisciplinary approach to inpatient medication reconciliation in an academic setting. American Journal of Health-System Pharmacy 2007; 64(8): 850-854. doi: 10.2146/ajhp060314. [DOI] [PubMed] [Google Scholar]
- 7.Mueller SK, Sponsler K, Kripalani S, Schnipper JL. Hospital-based medication reconciliation practices: A systematic review. Archives of Internal Medicine 2012; 172(14): 1057-1069. doi: 10.1001/archinternmed.2012.2246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Plaisant C, Wu J, Hettinger AZ, Powsner S, Shneiderman B. Novel user interface design for medication reconciliation: an evaluation of Twinlist 2015 2015–02–07 00:00:00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cadwallader J, Spry K, Morea J, Russ AL, Duke J, Weiner M. Design of a medication reconciliation application: facilitating clinician-focused decision making with data from multiple sources. Applied clinical informatics 2013; 4(1): 110-125. Epub 2013/05/08. doi: 10.4338/aci-2012–12-ra-0057. PubMed PMID: 23650492; PubMed Central PMCID: PMCPMC3644819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holtzblatt K, Wendell JB, Wood S. Rapid contextual design:A how-to guide to key techniques for user-centered design. San Francisco, CA: Morgan Kaufmann; 2005. 313 p. [Google Scholar]
- 11.Nielsen J. Usability Engineering: AP Professional; 1994. [Google Scholar]
- 12.Brooke J. SUS-A quick and dirty usability scale. Usability evaluation in industry 1996; 189(194):4–7. [Google Scholar]
- 13.Team RC. R: A language and environment for statistical computing. 3.1.2 ed. Vienna, Austria.: R Foundation for Statistical Computing; 2014. [Google Scholar]
- 14.Bangor A, Kortum P, Miller J. Determining what individual SUS scores mean: adding an adjective rating scale. J Usability Studies 2009; 4(3): 114-123. [Google Scholar]
- 15.Monkman H, Borycki EM, Kushniruk AW, Kuo M-H. Exploring the Contextual and Human Factors of Electronic Medication Reconciliation Research: A Scoping Review. In: Context Sensitive Health Informatics: Human and Sociotechnical Approaches. Studies in Health Technologies and Informatics; [166–72]. [PubMed] [Google Scholar]
- 16.Tresner-Kirsch D, Keybl M, Henderson J, Clark C, Aberdeen J, Turchin A, Palchuk M. Automated Detection of Discrepancies in Pharmaceutical Order-Entry Data. MITRE Corporation; 2015. [Google Scholar]
- 17.Del Fiol G, Workman T, Gorman PN. Clinical questions raised by clinicians at the point of care: A systematic review. JAMA Internal Medicine 2014; 174(5): 710-718. doi: 10.1001/jamainternmed.2014.368. [DOI] [PubMed] [Google Scholar]
- 18.Gleason KM, McDaniel MR, Feinglass J, Baker DW, Lindquist L, Liss D, Noskin GA. Results of the Medications at Transitions and Clinical Handoffs (MATCH) study: an analysis of medication reconciliation errors and risk factors at hospital admission. Journal of general internal medicine 2010; 25(5): 441-447. Epub 2010/02/25. doi: 10.1007/s11606–010–1256–6. PubMed PMID: 20180158; PubMed Central PMCID: PMCPmc2855002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Press MJ, Gerber LM, Peng TR, Pesko MF, Feldman PH, Ouchida K, Sridharan S, Bao Y, Barron Y, Casalino LP. Postdischarge Communication Between Home Health Nurses and Physicians: Measurement, Quality, and Outcomes. Journal of the American Geriatrics Society 2015; 63(7): 1299-1305. doi: 10.1111/jgs.13491. [DOI] [PubMed] [Google Scholar]