Abstract
Objectives
Life satisfaction is an important component of overall well-being. Decline in life satisfaction is related to many adverse health outcomes including mortality.
Methods
We investigate the association of various psychosocial and health-related factors to life satisfaction in 237 non-demented community-dwelling older adults.
Results
Lower levels of depressive symptoms, less perceived stress, higher levels of social support, and better self-perceived general health were significantly associated with higher life satisfaction. Social support buffered the adverse impact of depressive symptoms on life satisfaction where more depressive symptoms were associated with much lower life satisfaction at low levels of social support than at high levels of social support.
Discussion
We discuss study implications, future research directions, and possible interventions that involve boosting social support in at-risk older adults.
Keywords: aging, social support, depression, quality of life
Introduction
Life satisfaction is an important component of overall well-being and is extensively studied for its association with beneficial physical, social, and psychological factors (Berg, Hassing, McClearn, & Johansson, 2006; Berg, Hoffman, Hassing, McClearn, & Johansson, 2009; Gerstorf, Ram, Röcke, Lindenberger, & Smith, 2008; Hamarat et al., 2001; Hsu, 2012; McDowell, 2010). Low life satisfaction is related to many adverse health outcomes (Mroczek & Spiro, 2005) including death due to injuries, increased suicide, and all-cause death, (Koivumaa-Honkanen et al., 2000; Lyyra, Törmäkangas, Read, Rantanen, & Berg, 2006). For older adults, life satisfaction is not only predictive of survival (John, MacKenzie & Menec, 2014) but sharp declines in life satisfaction more strongly predict proximity to death than age (Gerstorf et al., 2008).
Older adults 65 and older, comprise almost 13% of the U.S. population (about 40 million citizens), with a projected increase to over 72 million by 2030 (Administration of Aging, 2013). Globally the number of individuals age 60 and older is expected to surge from 605 million in 2000 to over 2 billion in 2050 (World Health Organization, 2012). Unfortunately, the older adulthood life cycle is often characterized by reductions in physical functioning, cognition, or other important psychosocial factors (Kim & Sok, 2012; Lyyra et al., 2006). Given life satisfaction’s strong link to health outcomes and successful aging, it is important not only to understand the factors associated with life satisfaction ratings in the growing elderly population but also to address the lack of research on potential moderators of the association between such variables and life satisfaction.
Conceptually, life satisfaction is based on a person’s subjective appraisal of life quality and value in comparison to a standard or ideal template that is also self-defined and self-imposed (Diener, Emmons, Larsen, & Griffin, 1985; Diener, 2000; McDowell, 2010). According to Diener (1984), life satisfaction is one component of subjective well-being—i.e., the “cognitive judgment” component, which refers to whether people consider their lives, on the whole, to be satisfying. The other component of subjective well-being is more hedonic in nature and consists of the ratio of positive to negative affect, over time, in a person’s life (Diener, 1984; Diener & Emmons, 1985). Life satisfaction is also conceptualized as an indicator of quality of life (Diener et al., 1985; Lou, 2010; McDowell, 2010; St. John & Montgomery, 2010), and the terms life satisfaction and well-being are sometimes used interchangeably (Kim & Sok, 2012; Koivumaa-Honkanen et al., 2000). In the current study we use the term life satisfaction to indicate the subjective evaluation of a person’s life.
Previous research with older adults indicates that self-rated health, social support, perceived stress, mood disturbance, cognitive ability, and physical functioning are associated with life satisfaction (Berg et al., 2006; Berg et al., 2009; Gerstorf, et al., 2008; Hsu, 2012; St. John & Montgomery, 2010). For example, susceptibility to stress may increase with diminished age-related physical and cognitive functioning (Krause, 2005). Chronic stressors, such as caring for an ailing spouse, may further exacerbate these physical and cognitive declines for a person dealing with functional limitations or other life changes. A cross-sectional study that examined differences in life satisfaction among young adults, middle-aged adults, and older adults found that perceived stress was not significantly related to of life satisfaction in older adults (Hamarat, Thompson, Zabrucky, Steele, Matheny & Aysan, 2001). However, this study was cross-sectional and the sample was largely homogenous, with a majority of older adults having 16 years of education (Hamarat et al., 2001). In addition, the authors did not report participants’ racial/ethnic characteristics or cognitive status, and results therefore may not be representative of a more diverse sample of older adults (Hamarat et al., 2001).
In terms of adverse psychological factors, depressive symptoms are negatively associated with life satisfaction ratings across the life span and were related to decreased life satisfaction in a large representative sample of adults and older adults (Strine, Chapman, Balluz, Moriarty, & Mokdad, 2008) and in the oldest-old (Berg et al., 2006; Berg et al., 2009). Similarly, anxiety may negatively impact life satisfaction (Strine et al., 2008). For example, individuals diagnosed with clinically significant anxiety reported deficits in 15 of 16 quality of life domains, and even subclinical anxiety symptoms can have deleterious effects on life satisfaction (Henning et al., 2007). Less is known about the association of anxiety to life satisfaction among older adults who do not meet the criteria for anxiety disorders.
There are known associations between life satisfaction and self-reported health (Berg et al., 2006; Kim & Sok, 2012; Koivumaa-Honkanen et al., 2000; Mroczek & Spiro, 2005), although sex differences may influence this relationship. For example, self-rated overall health was associated with life-satisfaction in older women, while neither objective nor subjective health measures were related to life satisfaction in men (Berg et al., 2006). For the related variable of physical activity, one study found that vigorous walking for 30 minutes or more was associated with life satisfaction (Koivumaa-Honkanen et al., 2000). Conversely, physical inactivity was related to a decrease in life satisfaction in a population-based sample (Strine et al., 2008). With regard to the relationship between leisure activities and life satisfaction among older adults, one study found that walking and reading literature were correlated with life satisfaction in the old-old but not after controlling for other variables (Hilleras, Jorm, Herlitz & Winblad, 2001). Overall, leisure activities in which older adults choose to engage and from which they derive pleasure or enjoyment may be relevant to life satisfaction, and this association merits further investigation.
Within the older adult literature, the quality of one’s relationships and the specific nature of the social support provided are consistently correlated with life satisfaction (Berg et al., 2006; Zhu, Hu, & Efird, 2012). Overall, individuals with higher levels of perceived social support have higher levels of life satisfaction. The robust findings for social support are a basis for the socioemotional selectivity theory (Carstensen, 1992; Fung & Carstensen, 2004), which posits that as people move towards older adulthood and become increasingly aware of the finite time they have left, they pursue relationships that are meaningful and close, while pruning more peripheral relationships. It is clear that sufficient social support for older adults is especially important. Despite the direct and beneficial relationship of social support to life satisfaction, little is known about the role of social support to either enhance or diminish life satisfaction’s association with other beneficial and adverse factors.
According to the stress-buffering hypothesis model (Cohen & Willis, 1985), the impact of social support is far-reaching and can attenuate the effects of various adverse events, such as the association of stress and depressive symptoms (Raffaelli et al., 2012; Takizawa et al., 2006; Hashimoto, Kurita, Haratani, Fukii & Ishibashi, 1999). Moreover, in the literature on life satisfaction and the related constructs of well-being and quality of life, social support emerges as one of the few factors that consistently demonstrate a direct association with these outcomes. Comparatively little is known about the indirect or buffering effects of social support on adverse events in relation to life satisfaction among older adults. The existing findings are mixed. One study found that emotional social support diminished the effect of financial strain on life satisfaction in the oldest-old, but not in young-old participants (Krause, 2005). Another study demonstrated that social support was directly associated with anxiety disorders and quality of life ratings in older adults but found no evidence of a buffering effect of social support on quality of life or stress ratings (Panayiotou & Karekla, 2013).
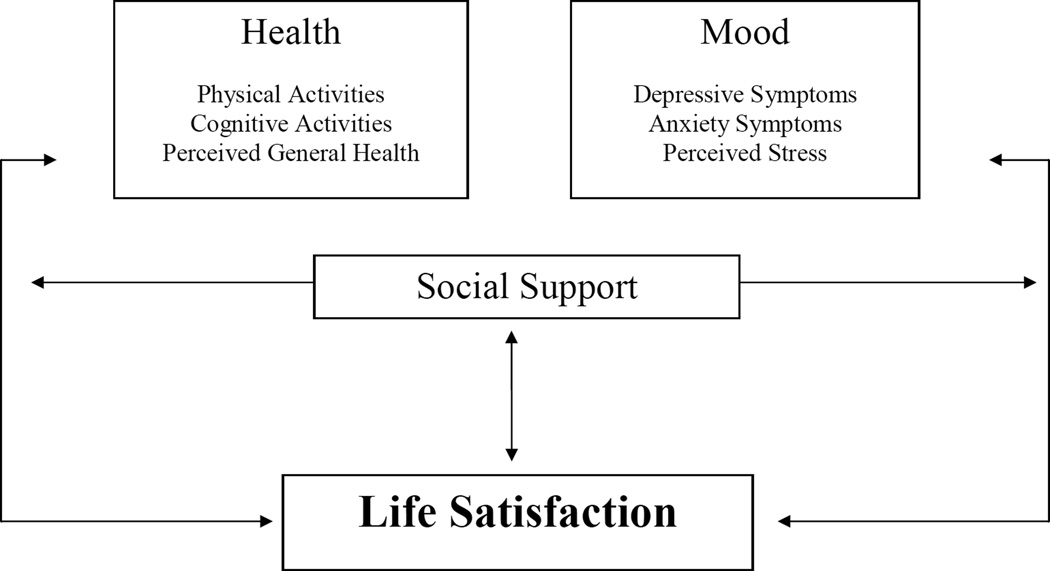
There is a need for further exploration of life satisfaction to important health factors alongside investigation of the role of social support in moderating the impact of beneficial and adverse factors on life satisfaction. Figure 1 depicts a predicted model of both the direct association of selected factors on life satisfaction as well as the proposed moderating impact of social support on the relationship between these factors and life satisfaction. The current study has three primary goals. First, we aim to replicate previous findings on the association of depressive symptoms, anxiety symptoms, perceived stress, social support, self-reported health, and physical activity to life satisfaction ratings in a diverse sample of non-demented older adults. We predict that higher scores on self-reported health and social support measures and that lower scores for adverse mood symptoms (e.g., depression, anxiety, and perceived stress) will be associated with higher life satisfaction in older adults. Second, we seek to fill gaps in the literature by investigating the association of life satisfaction to the little studied but relevant health factors of physical and cognitive leisure activities. We predict that higher scores on physical and cognitive exercise engagement will be related to higher life satisfaction. We did not generate specific hypotheses concerning the relationship between life satisfaction and the demographic variables of sex, age, and race/ethnicity given the equivocal nature of findings or the limited amount of research on these variables. Third, we aim to fill an important gap in the literature by investigating the possible buffering impact of social support on variables found to be significantly associated with life satisfaction.
Figure 1.
Predicted model of relation among the study variables and life satisfaction.
Methods
Sample
Participants were a subset of individuals from the Einstein Aging Study, a longitudinal, community-based study of cognitive aging based in the Bronx, New York (for details see Katz et al., 2012; Lipton et al., 2003). Eligible participants were at least 70 years old, Bronx residents, noninstitutionalized, and English speaking. Exclusion criteria included sensory disturbances that preclude neuropsychological testing, active psychiatric symptomatology, nonambulatory status, and having a diagnosis of dementia (determined at a consensus case conference, see Katz et al., 2012 for details). While no participant had a clinical diagnosis of dementia, approximately 22% of participants carried a diagnosis of mild cognitive impairment, suggesting a preclinical dementia condition (Petersen et al., 2001; Winblad et al., 2004). The remaining participants were cognitively intact across neuropsychological domains, though a subset (approximately 31% of participants) presented with significant self-reported and/or informant-reported complaints about their memory and other aspects of cognition (Rabin et al., 2014).
All participants provided written informed consent according to procedures approved by the local institutional review board. Participants were evaluated initially on two occasions approximately two weeks apart. During the first visit at the annual Einstein Aging Study assessment, participants completed standard neuropsychological measures of memory, executive functioning, language, and other cognitive domains, self-report measures of general health, perceived stress, and a neurological examination (for further details see Katz et al., 2012). During the second visit, participants completed the life satisfaction outcome measure and other self-report questionnaires utilized in this study (described below). Information about health status and demographic variables was also obtained. Of the 260 participants eligible for inclusion, 237 satisfactorily completed the life satisfaction questionnaire. No significant demographic differences were found between the 237 participants who completed the life satisfaction measure as compared to the 22 excluded participants who did not.
Measures
Outcome Variable
Life satisfaction was assessed using the Satisfaction with Life Scale (SWL; Diener, Emmons, Larsen, & Griffin, 1985), a 5-item self-report measure of global life satisfaction. Responses were scored using a Likert scale ranging from “strongly disagree=1” to “strongly agree=7,” with higher ratings indicating greater agreement. Sample items include, “In most ways my life is close to ideal” and “I am satisfied with my life.” All statements were positively phrased. Total scores were derived from summing across the items and scores range from 5 (low satisfaction) to 35 (high satisfaction). The SWL has demonstrated good internal consistency and reliability with alpha coefficients ranging from 0.79 to 0.89 and test-retest coefficients ranging from 0.5 to 0.84 (Diener et al., 1985; Pavot, 2008; McDowell, 2010). Cronbach’s alpha for the current sample was 0.87.
Demographic and Mood Variables
Age and education were measured in years, sex was dichotomized as male/female, and race/ethnicity was dichotomized as white/non-white.
Depressive symptoms were assessed using the Geriatric Depression Scale – Short form (GDS; Sheikh & Yesavage, 1986), a 15-item self-report scale used to identify emotional and psychological aspects of depression in the elderly. The scale omits items related to somatic and physiological complaints since some bodily disturbances are the result of medication side effects and not directly caused by depression. Items are dichotomized on a “Yes=1” or “No=0” scale (range 1 to 15), with higher scores indicating increased presentation of depressive symptoms; a cutoff score of 5 or higher is typically associated with clinically meaningful depression. Previous analysis of the GDS reported an internal consistency-reliability of 0.80 (Marc, Raue, & Bruce, 2008).
The Adult Manifest Anxiety Scale–Elderly version (AMAS-E; Reynolds, Richmond, & Lowe, 2003) is a 44-item self-report scale that assesses anxiety symptoms in older adults in the areas of fear of aging, physiological anxiety, and worry/oversensitivity; there is also a lie scale that does not contribute to the total score. The summation of these dichotomously scored clinical items represents the Total Anxiety scale (scores range from 0 to 37). Higher scores indicate a greater frequency of manifested anxiety symptoms. An alpha coefficient of 0.91 was previously reported for the total anxiety score (Lowe & Reynolds, 2006).
The Perceived Stress Scale (Cohen, Kamarck, & Mermelstein, 1983) is a self-report measure that evaluates respondents’ general perception of stress and stressful situations over the past month. Items on the perceived stress scale examine the extent to which a respondent believes his or her life has been “unpredictable, uncontrollable, or overloaded” (Cohen, 1983). The scale consists of 7 positive and 7 negative items and uses a 5-point scale (“never=0” to “very often=4”). Total scores are obtained by reversing the scores on the positive items and then summing all 14 items (scores range from 0–56). A recent meta-analysis (Lee, 2012) found that perceived stress scale had an acceptable Cronbach’s alpha across 11 studies and data from 769 participants in the EAS study indicate a Cronbach’s alpha of 0.82 (Ziang et al., 2013).
Social Support
Social support were assessed using the self-report Medical Outcomes Study (MOS) Social Support Survey (Sherbourne & Stewart, 1991), which inquires about affective, informational, emotional, tangible, and positive aspects of social support. Availability of various types of social support is measured by 19 items scored on a Likert scale ranging from “none of the time=1” to “all of the time=5.” Sample items include, “Someone to take you to a doctor if you needed it,” and “Someone who understands your problems.” Total social support scores are based on a sum across all items and range from 19 to 95. In a previous study, the total social support score was found to be reliable with a Cronbach’s alpha of 0.97 (Sherbourne & Stewart, 1991).
Exercise and General Health
Physical and Cognitive Exercise
The type and extent of cognitive and physical activity participants engaged in during a typical week over the past year was measured using a 27-item self-report inventory (Rabin, 2012, unpublished). The approximate duration spent on each activity per session was measured with choices of 30 minutes, 1 hour, or greater than one-hour. Questionnaire items 1–16 consisted of cardiovascular and strength exercises while items 17–27 included varying types of cognitively engaging tasks. Physical and cognitive exercise scores were calculated by summing the number of times that participants reported engaging in each physical or cognitive activity for at least 30 minutes. Notably, we omitted aggregate activity scores below 30 minutes based on the minimum recommendations for exercise engagement for older adults by the American College of Sports Medicine and the American Heart Association (Nelson et al., 2007). Additionally, it can be argued that because the exercise scores were based on activity duration in the past week, less than 30 minutes of cumulative exercise is relatively inactive.
General Health
The Short Form (SF)-36 is a brief, self-report health survey designed to assess health within the last month across 8 different dimensions. The scale has been previously used within a community-dwelling population of older adults and was found to have high internal consistency for all dimensions, except for social function (Walters, Monroe, & Brazier, 2001). For the current study, we utilized the general health dimension, which asks participants to rate their current health, future health expectations, and health status in contrast to that of others. Items are scored on a 1–5 point Likert scale and are then transformed to range from 0–100, with higher scores indicating better perceived general health.
Data Analysis
Life satisfaction was the outcome variable. We analyzed it as a continuous variable and also as a categorical variable with three levels of life satisfaction: low (scores equal to or less than 1 standard deviation below the mean), medium (scores within 1 standard deviation of the mean), and high (scores equal to or greater than 1 standard deviation above the mean). Descriptive statistics of mean and standard deviation were used for the continuous variables and frequency and percentage for the categorical variables.
We used analysis of variance (ANOVA) to compare the continuous variables (followed by Tukey post-hoc tests for any variables statistically differing) and the Pearson chi-square test to compare the categorical variables. As the GDS had a skewed distribution, we logarithmically transformed scores to allow for parametric analysis. We used inferential statistics of multivariate linear regression to determine associations with the outcome variable of life satisfaction using three models. Model 1 included the demographic variables of age, sex, race/ethnicity, and education along with the mood variables (depressive symptoms, anxiety symptoms, and perceived stress). Model 2 included the variables in Model 1 and social support. Model 3 included the variables in Model 2 and the health-related variables of cognitive and physical exercise and self-rated overall health.
Variables significantly associated with life satisfaction in the final multivariate regression model were included in additional regression analyses to determine the potential buffering impact of social support with these variables. Each of the models included the interaction of social support with one of these variables. All variables were mean centered to reduce any potential multicollinearity. We used the simple slope method (Aiken & West, 1991) to plot data at 1 SD above –and 1 SD below the mean. SPSS Version 20 was used for the analyses. All p-values were two-tailed.
Results
Table 1 shows the overall sample characteristics. Mean age was almost 81 years and mean education included some college. Women comprised slightly more than two-thirds of the sample and slightly more than one-third were of non-white race/ethnicity. Mean levels of depressive and anxious symptoms were not clinically elevated based on age-appropriate norms. Notably, only 20 participants had scores of 5 or higher on the GDS, indicating clinically meaningful symptoms and the majority of those individuals (70%) were in the low life satisfaction category. The mean perceived stress scale score was 17.8. The average social support score was 71.4. Health-related values included a mean physical exercise score of 10.7, a mean cognitive exercise score of 17.1, and a SF-36 general health score indicating higher perceived general health than shown in age-appropriate norms (Ware, Kosinki, & Dewey, 2000). The mean score for the outcome variable life satisfaction indicated average levels of life satisfaction (Diener, 2009), though it is unclear whether scores reflect age-appropriate norms.
Table 1.
Characteristics of Variables of 237 Participants at 3 levels of Life Satisfaction
| Variables | Whole Sample Mean (SD) or Percentage (#) |
Low SWL Mean (SD) or Percentage (#) (n=42) |
Medium SWL Mean (SD) or Percentage (#) (n=163) |
High SWL Mean (SD) or Percentage (#) (n=32) |
P-Value |
|---|---|---|---|---|---|
| Age (years) | 80.8 (5.43) | 80.5 (5.11) | 80.9 (5.56) | 80.8 (5.36) | .918 |
| Education (years) | 14.4 (3.49) | 14.3 (3.20) | 14.4 (3.47) | 14.6 (3.99) | .944 |
| Sex (% female) | 68.8% (163) | 78.6% (33) | 65.0% (163) | 75.0% (24) | .172 |
| Race/ethnicity (non-white) | 39.7% (94) | 28.6% (12) | 43.6% (71) | 34.4% (11) | .168 |
| GDS | 1.6 (1.97) | 3.4 (3.10) | 1.3 (1.41) | 0.6 (0.76) | <.001 |
| AMAS-E | 11.6 (8.30) | 15.0 (7.97) | 11.4 (8.01) | 8.5 (8.81) | .003 |
| Perceived Stress | 17.8 (7.50) | 22.8 (7.81) | 17.3 (6.98) | 14.3 (7.04) | <.001 |
| Social Support | 71.4 (6.70) | 59.8 (17.50) | 71.8 (15.86) | 83.4 (10.23) | <.001 |
| Physical exercise | 10.7 (8.20) | 10.0 (11.33) | 10.5 (6.89) | 12.6 (9.47) | .339 |
| Cognitive exercise | 17.1 (9.21) | 18.9 (10.50) | 16.3 (8.79) | 18.1 (9.77) | .218 |
| SF-36 General Health | 68.7 (18.98) | 56.5 (19.58) | 69.9 (17.89) | 78.8 (15.62) | <.001 |
| SWL Total Score | 24.9 (6.61) | -- | -- | -- | -- |
Note: GDS=Geriatric Depression Scale, short form, AMAS-E=Adult Manifest Anxiety Scale-Elderly Version, SF-36=Short Form-36, SWL=Satisfaction with Life Scale; Low= SWL scores equal to or less than 1SD below the mean, Medium = SWL scores within 1SD of the mean, and high = SWL scores equal to or greater than 1 SD above the mean.
Table 1 also compares the variables across three levels of life satisfaction. Depressive symptoms and anxiety symptoms significantly differed with post-hoc analyses showing that participants with low life satisfaction had significantly higher scores than those with high life satisfaction (p<.001 and p=.003, respectively). Perceived stress significantly differed with post-hoc analysis showing that participants with low life satisfaction had significantly higher scores than those with high life satisfaction (p<.001). Social support and self-reported general health significantly differed with post-hoc analyses showing that participants with high life satisfaction had significantly higher scores than those with low life satisfaction (p<.001).
Table 2 shows linear regression analyses for life satisfaction. In all models, fewer depressive symptoms and lower perceived stress were significantly associated with higher life satisfaction. In all models, higher social support and higher self-report SF-36 general health were significantly associated with higher life satisfaction scores. None of the demographic or exercise variables were significantly associated with life satisfaction.
Table 2.
Factors Associated with Life Satisfaction: Linear Regression Analyses
| Variables | Model 1 (n=227) |
Model 2 (n=226) |
Model 3 (n=224) |
|||
|---|---|---|---|---|---|---|
| B | SE | B | SE | B | SE | |
| Age (years) | .11 | .07 | .11 | .07 | .12 | .07 |
| Education (years) | −.08 | .11 | −.06 | .10 | .02 | .11 |
| Sex (female) | −1.18 | .80 | −1.00 | .80 | −.81 | .80 |
| Race/ethnicity (non-white) | .67 | .77 | .78 | .74 | .85 | .75 |
| Education (years) | −.08 | .11 | −.06 | .10 | .02 | .11 |
| GDS | −8.53*** | 1.46 | −7.01*** | 1.45 | −5.24*** | 1.62 |
| AMAS-E | −.06 | .05 | −.50 | .50 | −.05 | .05 |
| Perceived Stress | −.21*** | .06 | −.18** | .06 | −.16** | .06 |
| Social Support | -- | -- | .09*** | .02 | .10*** | .02 |
| Physical Exercise | -- | -- | -- | -- | .01 | .05 |
| Cognitive Exercise | -- | -- | -- | -- | −.04 | .04 |
| SF-36 General Health | -- | -- | -- | -- | .05* | .02 |
Note: B=beta, SE=standard error, GDS=Geriatric Depression Scale short form, AMAS-E=Adult Manifest Anxiety Scale-Elderly Version, SF-36=Short Form-36, SWL=Satisfaction with Life Scale; dashes indicate a variable not included in the model;
p<.05,
p<.01,
p<.001
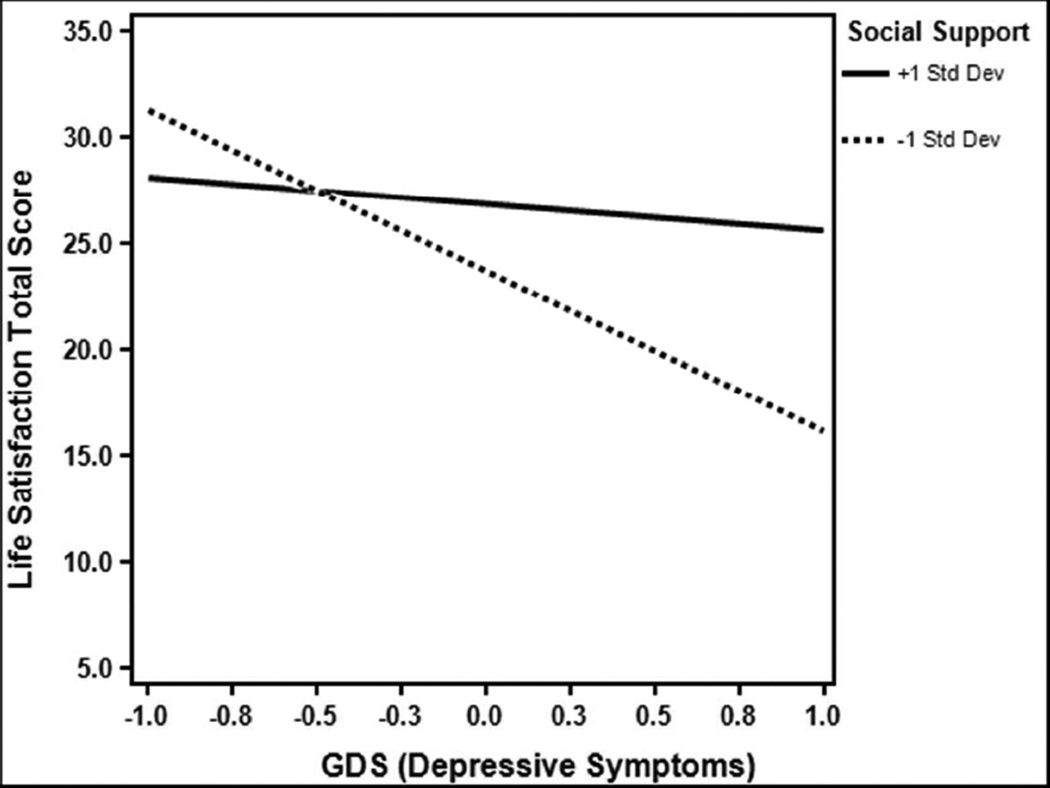
Table 3 shows linear regression analyses including only the statistically significant variables from the linear regression analyses shown in Table 2. These three additional analyses considered the interaction of social support with the other statistically significant variables of depressive symptoms, perceived stress, and SF-36 general health. As previously shown in Table 2, all three models showed that fewer depressive symptoms, lower perceived stress, higher social support, and higher self-report SF-36 general health were significantly associated with higher life satisfaction scores. Model 1 shows a statistically significant interaction of social support and depressive symptoms with life satisfaction. Figure 2 shows that social support buffered the adverse impact of depressive symptoms on life satisfaction where higher depressive symptoms were associated with much lower life satisfaction at low levels of social support than at high levels of social support. Model 2 did not show any statistically significant interaction of social support and perceived stress. Model 3 did not show any statistically significant interaction of social support and SF-36 general health.
Table 3.
Regression Examining Buffering Role of Social Support on Life Satisfaction
| Variables | Model 1 (n=227) |
Model 2 (n=228) |
Model 3 (n=224) |
|||
|---|---|---|---|---|---|---|
| B | SE | B | SE | B | SE | |
| GDS | −4.42*** | .37 | −4.14* | 1.66 | −4.90** | 1.61 |
| Perceived Stress | −.15** | .05 | −.19*** | .06 | −.16** | .05 |
| Social Support | .09** | .02 | .10*** | .02 | .10*** | .02 |
| SF-36 General Health | .06** | .02 | .06** | .02 | .06** | .02 |
| Social Support x GDS | .19* | .07 | -- | -- | -- | -- |
| Social Support x Perceived Stress | -- | -- | .01 | .003 | -- | -- |
| Social Support x SF-36 General Health | -- | -- | -- | -- | −.002 | .001 |
Note: B=beta, SE=standard error, GDS=Geriatric Depression Scale short form, SF-36=Short Form-36, SWL=Satisfaction with Life Scale; dashes indicate a variable not included in the model;
p<.05,
p<.01,
p<.001
Figure 2.
Interaction of social support and depressive symptoms with life satisfaction
Note: Logarithmic depressive symptoms scored used. Horizontal axis stretched for ease of interpretation.
Discussion
We examined the association of various demographic, mood, social support, activity (physical and cognitive exercise), and general health variables to life satisfaction in a community-based sample of non-depressed, non-demented older adults. Fewer depressive symptoms, lower perceived stress, higher social support, and higher self-rated general health were consistently associated with higher life satisfaction. Social support was important for buffering the impact of greater depressive symptoms on life satisfaction.
We found in a univariate analysis comparing the three life satisfaction categories (i.e., low, medium, high) that adverse mood factors (depressive and anxious symptoms and perceived stress) were significantly greater in those with low life satisfaction as compared to those with high life satisfaction. Additionally, older adults with high life satisfaction had better overall perceived general health and higher social support than the low life satisfaction groups. These results are not surprising given the known beneficial association of life satisfaction to many variables (Berg et al., 2006; 2009; Hsu, 2012; Norberg, Diefenback, & Tolin, 2008).
Social support was significantly and positively associated with life satisfaction in all regression models, including those that examined interactions with measures of depressive symptoms, perceived stress, and general health. This is consistent with the existing literature (Berg et al., 2006; Berg et al., 2009; Hsu, 2012; Kim & Sok, 2012; Lou, 2010), which identifies social support as the factor that consistently has the most meaningful impact on life satisfaction. Old age is often accompanied by changes or declines in aspects of health and overall functioning, and it is possible that the perception of a strong social support network enables older adults to maintain a positive view of their lives in the face of such changes. Moreover, such a social support system may aid the elderly in positively re-adjusting how they evaluate their lives in the face of decline or loss.
Fewer depressive symptoms were significantly associated with lower life satisfaction in the analytic models that included this variable. This is consistent with the known important role of depressive symptoms on life satisfaction (Berg et al., 2006; Berg et al., 2009; Strine et al., 2008). The dynamic interplay between depressive symptoms and life satisfaction is not a surprising one. Negative self-appraisal and thoughts of worthlessness are common depressive characteristics. This depressive purview tends to be all encompassing and affects the way people perceive and interpret their experiences in a global way. By contrast, anxiety symptoms did not contribute significantly to life satisfaction in the multivariate analyses. One study reports that anxiety comorbid with depression was associated with lower quality of life scores than anxiety alone (Norberg, Diefenback, & Tolin, 2008). Another study reports that anxiety has an impact on life satisfaction but its association is overshadowed in the presence of comorbid depressive symptoms (Henning et al., 2007). Our results are consistent with the emphasis on the role of depressive symptoms overshadowing anxiety symptoms. It is also possible that the lack of significance for anxiety in our study was due to the relatively low levels of both depressive and anxiety symptoms in our sample.
Perceived stress was inversely associated with life satisfaction in the analytic models that included this variable. Overall, participants who reported lower levels of stress had higher levels of life satisfaction. This is not surprising as stress can be psychologically or physiologically taxing and a subjective appraisal of high or uncontrollable levels of stress would be expected to be mirrored in a lowered appraisal of one’s life. Moreover, chronic or overwhelming stress is often accompanied by feelings of depression (Potter, Hartman, & Ward, 2009).
Higher self-reported health ratings were positively associated with life satisfaction in the analytical models that included this variable. Specifically, participants who reported better overall health also had higher life satisfaction ratings, consistent with previous findings examining perceived health and life satisfaction in the elderly (Berg et al., 2006; Berg et al., 2009). Health maintenance, optimal functional capacity, and successful aging are consistently emphasized and underscored as ideal outcomes in the older adult life cycle. It is therefore understandable that greater life satisfaction is reported by individuals who believe that they have met those standards.
The demographic variables of age, sex, ethnicity and education had no statistically significant associations with life satisfaction in any of the analytical models. Findings for sex and life satisfaction are largely equivocal, with some previous research indicating that men report higher life satisfaction than women (Hsu, 2012; Padoani et al., 1998), while other studies report no such difference for sex in overall life satisfaction (Berg et al., 2006; Berg et. al, 2009; Hamarat et al., 2001). Our findings and our participants are more closely aligned with those of Berg and colleagues (2006; 2009) who also reported no difference. Other research also supports the current results on the lack of association between demographic factors and life satisfaction (Hamarat et al., 2001).
Although physical exercise is important for a variety of health-related outcomes and aspects of subjective well-being (Wanderley et al., 2011), we did not find a significant association of either self-reported physical exercise or cognitive exercise with life satisfaction. Previous research (St. John et al., 2010) shows a strong relationship between functional impairment and reduced life satisfaction, while other research found no significance for different activities and life satisfaction when personality (specifically neuroticism) and subjective health were taken into account (Hilleras, Jorm, Herlitz & Winblad, 2001). Because participants were generally healthy and likely to be cognitively active, there may have been too little variability to discern such a relationship. Moreover, as physical functioning typically declines with age, older adults may reduce the importance placed on such tasks, potentially lowering the value assigned to physical activity when evaluating their overall life satisfaction. Assessing the importance or relevance placed on these activities may aid in understanding the relationship of leisure activities to life satisfaction in older adults.
Social support buffered the adverse impact of depressive symptoms on life satisfaction where higher depressive symptoms were associated with much lower life satisfaction at low levels of social support than at high levels of social support. This finding is important for several reasons. First, depressive symptoms are prevalent in the elderly (Berg et al., 2006; Berg et al., 2009; Strine, Chapman, Balluz, Moriarty, & Mokdad, 2008), with possible risk factors including the loss of financial stability, independence, functioning, and loved ones as well as thoughts about one’s own future death. Second, life satisfaction ratings may serve as a reliable indication of how older adults perceive their lives overall, despite chronic or acute adverse conditions. Sufficient support from family and friends may not only help with adaptation to environmental or biological changes but also may help older adults cope with the depression that can accompany such losses, thereby diminishing the impact that depressive feelings would otherwise have on perceived well-being. Third, our results indicate that adequate perceived support is important for ameliorating the association of depressive symptoms to life satisfaction but that social support above a certain degree does not further buffer the relationship. One possibility is that social support perceived as officious or overbearing may serve to undermine the autonomy or independence of the older adults.
High or low levels of perceived social support did not buffer associations between perceived stress and self-rated general health with life satisfaction. While the relationship of social support to life satisfaction and overall well-being is known (Berg et al., 2006; Berg et al., 2009; Hsu, 2012; Kim & Sok, 2012; Lou, 2010), support for the buffering function of social support has not been a consistent finding (Panayiotou & Karekla, 2013). With regard to both perceived stress and perceived health, it is possible that the associations of these factors to life satisfaction are not readily influenced by varying degrees of social support. However, our participants rated their general health as greater than both established age-appropriate norms (Ware, Kosinki, & Dewey, 2000) and mean scores from male and female elderly as reported by Walters and colleagues (2001). It is thus possible that the buffering function of social support would need to be examined in the context of lower general health scores. In addition, using a cross-sectional approach may have diminished the ability to detect such interactions, given that the dynamic nature of perceived stressors and health issues are unlikely to be appropriately assessed at a single time point.
Limitations and Future Directions
Several study limitations warrant mention. First, although the average age of participants was almost 81 years, most were healthy and living independently. Thus, our sample may not be representative of the general population of older adults that includes those with dementia or with chronic debilitating illnesses who are at greatest risk for low life satisfaction. Second, these results may reflect survivorship as we did not study those who may have died along the way while participating in the Einstein Aging Study. Our cohort may mostly represent those who have positive psychological and social attributes and were available to talk about them. Third, exercise activity vigor was not assessed and may represent the integral component associated with life satisfaction ratings; this represents an area for future research. Fourth, we were unable to investigate the relationship of neuroticism to life satisfaction. However, neuroticism has been previously shown to be inversely associated with life satisfaction in the oldest-old (Berg et al., 2009). Fifth, there is a slight overlap between items on the SWL scale and the GDS (e.g. “Are you basically satisfied with your life?” from the GDS and “I am satisfied with my life” from the SWLS). However, one of the fundamental features of the SWL is that it was designed to assess global life satisfaction and not affective content. Sixth, as the current study is cross-sectional, we are unable to determine the direction of causality between life satisfaction and relevant factors.
Conclusions and Implications
In conclusion, this study demonstrates the importance of key components associated with high life satisfaction for older adults, specifically high social support but also low depressive symptoms, low perceived stress, and better perceptions of general health. The study also emphasizes the beneficial moderating impact of social support for depressive symptoms as it relates to life satisfaction. These findings may be useful for clinicians who work individually with the elderly or for those who design community-based interventions. For example, older adults can be encouraged to engage in activities that involve connecting with others and that provide a sense of belonging—such as volunteering with children, visiting museums with peers, joining a chorus, or becoming politically active. Older adults also may be given new social roles through mentorship activities, which has the benefit of providing feelings of being needed and appreciated as well as linking younger and older generations (Yuen, 2008). Referrals to support groups or individual outpatient treatment also may provide benefit. Finally, though not a straightforward or easy undertaking (Kim & Sok, 2012), for those with living family members, the quality of support in the family environment can be assessed and remediated with the goal of increasing life satisfaction.
Acknowledgments
Funding: This research was supported by the National Institute on Aging (NIA) and National Institute of General Medical Sciences (SC2AG039235), NIA (AG03949), Alzheimer’s Association (NIRG-11-206369), Czap Foundation, and The Leonard and Sylvia Marx Foundation. The authors wish to thank Ashu Kapoor, Milushka Elbulok-Charcape, Susan Chi, Avner Aronov, Erica Meltzer, Krystal Mendez, John Flynn, Nicole Belgrave, Hayoung Ryu, Charlotte Magnotta, Wendy Ramratan, and Drs. Molly Zimmerman, Cuiling Wang, and Yuming Ning for their contributions.
References
- Administration of Aging. [Accessed June 1, 2013];Aging statistics. 2013 Retrieved from http://www.aoa.gov/AoARoot/Aging_Statistics/index.aspx.
- Berg AI, Hassing LB, McClearn GE, Johansson B. What matters for life satisfaction in the oldest-old? Aging and Mental Health. 2006;10:257–264. doi: 10.1080/13607860500409435. [DOI] [PubMed] [Google Scholar]
- Berg AI, Hoffman L, Hassing LB, McClearn GE, Johansson B. What matters, and what matters most, for change in life satisfaction in the oldest-old? A study over 6 years among individuals 80+ Aging and Mental Health. 2009;13:191–201. doi: 10.1080/13607860802342227. [DOI] [PubMed] [Google Scholar]
- Carstensen LL. Social and emotional patterns in adulthood: Support for socioemotional selectivity theory. Psychology and Aging. 1992;7:331–338. doi: 10.1037//0882-7974.7.3.331. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- Diener E, Emmons RA. The independence of positive and negative affect. Journal of Personality and Social Psychology. 1985;47:1105–1117. doi: 10.1037//0022-3514.47.5.1105. [DOI] [PubMed] [Google Scholar]
- Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. Journal of Personality Assessment. 1985;49:71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- Diener E. Subjective well-being: The science of happiness and a proposal for a national index. American Psychologist. 2000;55:34–43. [PubMed] [Google Scholar]
- Diener E. [Accessed November 10, 2014];Understanding the SWLS scores. 2009 Retrieved from http://internal.psychology.illinois.edu/~ediener/SWLS.html.
- Gerstorf D, Ram N, Röcke C, Lindenberger U, Smith J. Decline in life satisfaction in old age: Longitudinal evidence for links to distance from death. Psychology and Aging. 2008;23:154–168. doi: 10.1037/0882-7974.23.1.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamarat E, Thompson D, Zabrucky KM, Steele D, Matheny KB, Aysan F. Perceived stress and coping resource availability as predictors of life satisfaction in young, middle-aged, and older adults. Experimental Aging Research. 2001;27:181–196. doi: 10.1080/036107301750074051. [DOI] [PubMed] [Google Scholar]
- Hashimoto K, Kurita H, Haratani T, Fujii K, Ishibashi T. Direct and buffering effects of social support on depressive symptoms of the elderly with home help. Psychiatry and Clinical Neurosciences. 1999;53(1):95–100. doi: 10.1046/j.1440-1819.1999.00478.x. [DOI] [PubMed] [Google Scholar]
- Henning ER, Turk CL, Mennin DS, Fresco DM, Heimberg RG. Impairment and quality of life in individuals with generalized anxiety disorder. Depression and Anxiety. 2007;24:342–349. doi: 10.1002/da.20249. [DOI] [PubMed] [Google Scholar]
- Hilleras PK, Jorm AF, Herlitz A, Winblad B. Life satisfaction among the very old: A survey on a cognitively intact sample aged 90 years or above. International . Journal of Aging and Human Development. 2001;52:71–90. doi: 10.2190/B8NC-D9MQ-KJE8-UUG9. [DOI] [PubMed] [Google Scholar]
- Hsu HC. Trajectories and covariates of life satisfaction among older adults in Taiwan. Archives of Gerontology and Geriatrics. 2012;55:210–216. doi: 10.1016/j.archger.2011.08.011. [DOI] [PubMed] [Google Scholar]
- Katz MJ, Lipton RB, Hall CB, Zimmerman ME, Sanders AE, Verghese J, Derby CA. Age and sex specific prevalence and incidence of mild cognitive impairment, dementia and Alzheimer’s dementia in blacks and whites: A report from the Einstein Aging Study. Alzheimer Disease & Associated Disorders. 2012;26:335–343. doi: 10.1097/WAD.0b013e31823dbcfc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SY, Sok SR. Relationships among the perceived health status, family support and life satisfaction of older Korean adults. International Journal of Nursing Practice. 2012;18:325–331. doi: 10.1111/j.1440-172X.2012.02050.x. [DOI] [PubMed] [Google Scholar]
- Kimm H, Sull JW, Gombojav B, Yi SW, Ohrr H. Life satisfaction and mortality in elderly people: The Kangwha Cohort Study. BMC Public Health. 2012;12:54. doi: 10.1186/1471-2458-12-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koivumaa-Honkanen H, Honkanen R, Viinamäki H, Heikkilä K, Kaprio J, Koskenvuo M. Self-reported life satisfaction and 20-year mortality in healthy Finnish adults. American Journal of Epidemiology. 2000;152:983–991. doi: 10.1093/aje/152.10.983. [DOI] [PubMed] [Google Scholar]
- Krause N. Exploring age differences in the stress-buffering function of social support. Psychology and Aging. 2005;20:714–717. doi: 10.1037/0882-7974.20.4.714. [DOI] [PubMed] [Google Scholar]
- Lee EH. Review of the psychometric evidence of the perceived stress scale. Asian Nursing Research. 2012;6:121–127. doi: 10.1016/j.anr.2012.08.004. [DOI] [PubMed] [Google Scholar]
- Lipton R, Katz MJ, Kuslansky G, Sliwinski MJ, Stewart W, Verghese J, Buschke H. Screening for dementia by telephone using the memory impairment screen. Journal of the American Geriatric Society. 2003;51:1382–1390. doi: 10.1046/j.1532-5415.2003.51455.x. [DOI] [PubMed] [Google Scholar]
- Lou VW. Life satisfaction of older adults in Hong Kong: The role of social support from grandchildren. Social Indicators Research. 2010;95:377–391. [Google Scholar]
- Lowe PA, Reynolds CR. Examination of the psychometric properties of the Adult Manifest Anxiety Scale-Elderly Version scores. Educational and psychological measurement. 2006;66:93–115. [Google Scholar]
- Lyyra TM, Törmäkangas TM, Read S, Rantanen T, Berg S. Satisfaction with present life predicts survival in octogenarians. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2006;61:319–326. doi: 10.1093/geronb/61.6.p319. [DOI] [PubMed] [Google Scholar]
- Marc LG, Raue PJ, Bruce ML. Screening performance of the 15-item geriatric depression scale in a diverse elderly home care population. The American Journal of Geriatric Psychiatry. 2008;16:914–921. doi: 10.1097/JGP.0b013e318186bd67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDowell I. Measures of self-perceived well-being. Journal of Psychosomatic Research. 2010;69:69–79. doi: 10.1016/j.jpsychores.2009.07.002. [DOI] [PubMed] [Google Scholar]
- Mroczek DK, Spiro A. Change in life satisfaction during adulthood: Findings from the Veterans Affairs Normative Aging Study. Journal of Personality and Social Psychology. 2005;88:189–202. doi: 10.1037/0022-3514.88.1.189. [DOI] [PubMed] [Google Scholar]
- Myers DG, Diener E. Who is happy? Psychological Science. 1995;6:10–19. [Google Scholar]
- Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, Castaneda Sceppa C. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116:1094–1105. doi: 10.1161/CIRCULATIONAHA.107.185650. [DOI] [PubMed] [Google Scholar]
- Norberg MM, Diefenbach GJ, Tolin DF. Quality of life and anxiety and depressive disorder comorbidity. Journal of Anxiety Disorders. 2008;22:1516. doi: 10.1016/j.janxdis.2008.03.005. [DOI] [PubMed] [Google Scholar]
- Padoani W, Dello Buono M, Marietta P, Scocco P, Zaghi PC, De Leo D. Cognitive performance and quality of life in a sample of 220 nondemented elderly people. Archives of Gerontology and Geriatrics. 1998;26:373–380. [Google Scholar]
- Panayiotou G, Karekla M. Perceived social support helps, but does not buffer the negative impact of anxiety disorders on quality of life and perceived stress. Social Psychiatry and Psychiatric Epidemiology. 2013;48:283–294. doi: 10.1007/s00127-012-0533-6. [DOI] [PubMed] [Google Scholar]
- Petersen RC, Doody R, Kurz A, Mohs A, Morris JC, Rabins PV, …Winblad B. Current concepts in mild cognitive impairment. Archives in Neurology. 2001;58:1985–1992. doi: 10.1001/archneur.58.12.1985. [DOI] [PubMed] [Google Scholar]
- Potter GG, Hartman M, Ward T. Perceived stress and everyday memory complaints among older adult women. Anxiety, Stress, & Coping. 2009;22:475–481. doi: 10.1080/10615800802449610. [DOI] [PubMed] [Google Scholar]
- Rabin LA, Wang C, Katz MJ, Derby CA, Buschke H, Lipton RB. Predicting dementia: Neuropsychological tests, self-reports, and informant reports of cognitive difficulties. Journal of the American Geriatrics Society. 2012;60:1128–1134. doi: 10.1111/j.1532-5415.2012.03956.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raffaelli M, Andrade FC, Wiley AR, Sanchez-Armass O, Edwards LL, Aradillas-Garcia C. Stress, Social Support, and Depression: A Test of the Stress-Buffering Hypothesis in a Mexican Sample. Journal of Research on Adolescence. 2013;23(2):283–289. [Google Scholar]
- Reynolds CR, Richmond BO, Lowe PA. The Adult Manifest Anxiety Scale (AMAS): manual. Los Angeles: Western Psychological Services. 2003 [Google Scholar]
- Sheik JI, Yesavage JA. Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version. Clinical Gerontology. 1986;37:819–20. [Google Scholar]
- Sherbourne CD, Stewart AL. The MOS social support survey. Social Science & Medicine. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- St. John PD, Mackenzie C, Menec V. Does life satisfaction predict five-year mortality in community-living older adults? Aging & Mental Health. 2014:1–8. doi: 10.1080/13607863.2014.938602. [DOI] [PubMed] [Google Scholar]
- Strine TW, Chapman DP, Balluz LS, Moriarty DG, Mokdad AH. The associations between life satisfaction and health-related quality of life, chronic illness, and health behaviors among US community-dwelling adults. Journal of Community Health. 2008;33:40–50. doi: 10.1007/s10900-007-9066-4. [DOI] [PubMed] [Google Scholar]
- Takizawa T, Kondo T, Sakihara S, Ariizumi M, Watanabe N, Oyama H. Stress buffering effects of social support on depressive symptoms in middle age: reciprocity and community mental health. Psychiatry and Clinical Neurosciences. 2006;60(6):652–661. doi: 10.1111/j.1440-1819.2006.01579.x. [DOI] [PubMed] [Google Scholar]
- Yuen HK, Huang P, Burik JK, Smith TG. Impact of participating in volunteer activities for residents living in long-term-care facilities. American Journal of Occupational Therapy. 2008;62:71–76. doi: 10.5014/ajot.62.1.71. [DOI] [PubMed] [Google Scholar]
- Walters SJ, Munro JF, Brazier JE. Using the SF-36 with older adults: across-sectional community-based survey. Age and Ageing. 2001;30:337–343. doi: 10.1093/ageing/30.4.337. [DOI] [PubMed] [Google Scholar]
- Wanderley FA, Silva G, Marques E, Oliveira J, Mota J, Carvalho J. Associations between objectively assessed physical activity levels and fitness and self-reported health-related quality of life in community-dwelling older adults. Quality of Life Research. 2011;20:1371–1378. doi: 10.1007/s11136-011-9875-x. [DOI] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Dewey JE. How to Score Version Two of the SF-36 Health Survey. Lincoln, RI: QualityMetric, Incorporated; 2000. [Google Scholar]
- Winblad B, Palmer K, Kivipelto M, Jelic V, Fratiglioni L, Wahlund LO, …Petersen RC. Mild cognitive impairment - beyond controversies, towards a consensus: Report of the International Working Group on Mild Cognitive Impairment. Journal of Internal Medicine. 2004;256:240–246. doi: 10.1111/j.1365-2796.2004.01380.x. [DOI] [PubMed] [Google Scholar]
- World Health Organization. [Accessed June 1, 2013];Fact file: 10 facts on ageing and the life course. 2012 Retrieved from http://www.who.int/features/factfiles/ageing/ageing_facts/en/index.html.
- Zhu S, Hu J, Efird JT. Role of social support in cognitive function among elders. Journal of Clinical Nursing. 2012;21:2118–2125. doi: 10.1111/j.1365-2702.2012.04178.x. [DOI] [PubMed] [Google Scholar]
- Ziang J, Ezzati A, Katz M, Zimmerman M. Validation of the Perceived Stress Scale in a community sample of older adults: Results from the Einstein Aging Study. Alzheimer’s & Dementia. 2013;9(Suppl):641. doi: http://dx.doi.org/10.1016/j.jalz.2013.05.1304. [Google Scholar]