Abstract
Policy Points:
Community health information exchanges have the characteristics of a public good, and they support population health initiatives at the state and national levels. However, current policy equally incentivizes health systems to create their own information exchanges covering more narrowly defined populations.
Noninteroperable electronic health records and vendors’ expensive custom interfaces are hindering health information exchanges. Moreover, vendors are imposing the costs of interoperability on health systems and community health information exchanges.
Health systems are creating networks of targeted physicians and facilities by funding connections to their own enterprise health information exchanges. These private networks may change referral patterns and foster more integration with outpatient providers.
Context
The United States has invested billions of dollars to encourage the adoption of and implement the information technologies necessary for health information exchange (HIE), enabling providers to efficiently and effectively share patient information with other providers. Health care providers now have multiple options for obtaining and sharing patient information. Community HIEs facilitate information sharing for a broad group of providers within a region. Enterprise HIEs are operated by health systems and share information among affiliated hospitals and providers. We sought to identify why hospitals and health systems choose either to participate in community HIEs or to establish enterprise HIEs.
Methods
We conducted semistructured interviews with 40 policymakers, community and enterprise HIE leaders, and health care executives from 19 different organizations. Our qualitative analysis used a general inductive and comparative approach to identify factors influencing participation in, and the success of, each approach to HIE.
Findings
Enterprise HIEs support health systems' strategic goals through the control of an information technology network consisting of desired trading partners. Community HIEs support obtaining patient information from the broadest set of providers, but with more dispersed benefits to all participants, the community, and patients. Although not an either/or decision, community and enterprise HIEs compete for finite organizational resources like time, skilled staff, and money. Both approaches face challenges due to vendor costs and less‐than‐interoperable technology.
Conclusions
Both community and enterprise HIEs support aggregating clinical data and following patients across settings. Although they can be complementary, community and enterprise HIEs nonetheless compete for providers’ attention and organizational resources. Health policymakers might try to encourage the type of widespread information exchange pursued by community HIEs, but the business case for enterprise HIEs clearly is stronger. The sustainability of a community HIE, potentially a public good, may necessitate ongoing public funding and supportive regulation.
Keywords: health information systems, health information exchange, integrated delivery systems, qualitative research
Efforts to improve the health care system like increasing safety, reducing readmissions, and integrating care delivery require patient information to be shared efficiently and effectively. To that end, the United States has invested substantially in technologies that enable health information exchange, that is, the electronic sharing of patient information.1 For example, the Office of the National Coordinator has spent $540 million on the State Health Information Exchange Cooperative Agreement Program, which helps support the technical infrastructure necessary to operationalize health information exchange in every state.2 In addition, the Medicare and Medicaid Electronic Health Record (EHR) Incentive Program (ie, Meaningful Use) has invested $26 billion in increasing providers’ health information exchange capability,3, 4 because the certification criteria include requirements and specifications for electronic patient information exchange.5 Several states and localities have also funded health information exchange activities.6
Individual physicians and organizations (like hospitals and health systems), however, have leeway in deciding how they will actually engage in health information exchange. For example, they could participate in a community health information exchange (HIE) organization, efforts that developed over the past 2 decades to facilitate information sharing for a state or region.7 Community HIEs are often labeled “public exchanges” because their objective is to facilitate health information exchange for any willing provider and they often are supported by public funds. Community HIEs include regional health information organizations and state‐designated entities (SDEs), which are the agencies or organizations funded by the Office of the National Coordinator to build health information exchange capacity in each state. A different approach would be to focus exchange activity in a more narrowly defined network of organizations.
Enterprise HIEs are a more recent development in which health systems create their own information exchange network to connect affiliated hospitals and physicians.8 Enterprise HIEs are growing in popularity, particularly among large health systems with hospitals and ambulatory care providers on different EHR platforms. Providers, however, may decide not to participate in either an enterprise or a community HIE. Instead, they may use the DIRECT capabilities (technology akin to secure email) built into EHRs or share information with only those providers with the same EHR vendor. None of these approaches is mandated or explicitly tied to federal incentive funding. Contrary to some perceptions, Meaningful Use does not require participation in a community HIE organization or the use of DIRECT; it simply requires the electronic exchange of information.9 Furthermore, these are not necessarily mutually exclusive choices; providers may choose to exchange information using more than one approach.
Given this complex environment of public‐ and private‐sector initiatives, our goal was to better understand approaches to health information exchange in the United States. Specifically, we sought to identify why hospitals and health systems participate in community HIEs or choose to establish their own enterprise HIE.
Methods
Selecting Participants
We interviewed policymakers, community and enterprise HIE leaders, and health care executives in New York and Texas between March and July 2014 (see Table 1). We selected these 2 states because of their multiplicity of community and enterprise HIEs and their diverse geographical health care markets.
Table 1.
Number of Interviewees by Type of Organization and State
| Organization | New York | Texas | Total |
|---|---|---|---|
| Health care organizations | 7 | 10 | 17 |
| Community HIEs | 6 | 5 | 11 |
| State‐designated entities and state governments | 5 | 7 | 12 |
| Total | 18 | 22 | 40 |
We identified individual participants with help from SDEs, community HIEs, and health systems. We asked each SDE to participate with suggested community HIEs and markets in their states for inclusion in the study. We wanted to make sure that the markets dominated by major metropolitan areas, as well as those spanning more rural areas and HIEs at different stages of development (either long‐standing or newly formed, but operational), were represented and to include health systems known to be operating enterprise HIEs. The SDEs introduced us to state policymakers, and the community HIE introduced us to local ambulatory care and hospital representatives. We gave each organization the types of job titles and position descriptions that would be the most appropriate to include as interview subjects and also asked each to include health systems operating enterprise HIEs. All the organizations cooperated.
The 40 interviewees had titles like chief executive officer, chief medical informatics officer, vice president, information technology (IT) director, and health IT coordinator, and they were responsible for activities like strategy, operations, legal counsel, policymaking, technology management, and vendor relations. The sample represented 19 different entities, including 5 community HIEs, 10 health care organizations, 2 state agencies, and 2 SDEs. The community HIEs had robust participation from hospital and outpatient providers in their markets. The health care organizations ranged from small critical‐access hospitals to midsize hospitals in urban and suburban centers, an academic medical center, a single hospital health system, and multihospital health systems with hospitals having 400 or more and 600 or more beds. Of the 7 different health systems represented, 4 were pursuing enterprise HIEs (2 of which were live) in addition to participating in the local community HIE.
Interviews
The interviews, all of which Joshua Vest conducted, had a semistructured format with open‐ended questions. The interview guide covered health information exchange activity, the benefits and challenges of different approaches, market characteristics, and perceptions of different approaches’ impact and effectiveness. The language used was tailored to match the interviewee's organizational association, and each topic was introduced in a neutral manner (eg, “Do you think hospitals in this area view enterprise HIEs more or less favorably than the types of information exchange offered by community HIEs? For what reasons?”) We piloted the guide for content and length with a former community HIE leader. The interviews were recorded with consent for transcription, were primarily conducted on‐site (86%), and averaged 52 minutes. Key concepts, ideas, and notes were summarized (“memoed”) after each interview, and audio recordings were immediately transcribed. Both of us then discussed the memos and transcripts. Once we agreed that the themes had been saturated (ie, the interviews did not reveal any new information or concepts based on our preliminary reading of the transcripts), we stopped recruiting interviewees.
Analysis
For our analysis, we used an iterative, general inductive, and comparative approach.10 First, we both read a subset (15%) of transcripts, purposefully selected to represent interviews from both states as well as all 4 organizational types. Using an open‐coding approach, we independently coded any text describing interviewees’ reported enablers, barriers, challenges, or facilitators to effectively participating in or creating a community or enterprise HIE. We identified 48 such codes. Through joint discussion and reading sessions, we categorized synonymous and related codes into 14 different, mutually exclusive factors (ie, axial coding). A third coder (Dylan Dacy) also read the transcripts and helped with this axial coding process. For each factor, we created a final label and definition (see Table 2). The factors could be broadly related to the structure and strategy of health care organizations as reflected in their control, interorganizational relationships, resources, and strategy. Alternatively, all the factors describing health policy, market factors, technology, vendor issues, and costs refer to the external policy, resource, and economic environment. In general, the qualities of HIE are captured by the factors of HIE alternatives, beyond existing network, consent, governance, and operations. Because the potential role of each of these factors was context specific (eg, what might be a barrier for a community HIE might be an enabler of an enterprise HIE), we adopted a simultaneous coding approach.11 Each unit of text coded with a factor was also coded as either a “barrier” or an “enabler” to describe the direction of the effect, as well as a code indicating a community or an enterprise HIE. Therefore, units of text could be coded with multiple factors, which, if appropriate, were interpreted as relationships among the selected factors.
Table 2.
Factors Acting as Barriers to and/or Enablers of Community and Enterprise Health Information Exchange
| Factor | Definition |
|---|---|
| Beyond existing network | A need for information or communication beyond the local area or the organization's existing networks. |
| Consent | Any policies, processes, or technology issues about having to obtain patients’ consent to make information accessible to providers participating in the HIE. |
| Costs | The expense (measured in dollars or time) associated with HIE participation. Can include costs of investments or technology purchases. Does include factors that change the cost (incentives or discounts) but does not include the perceived value of those investments. |
| Control | Reasons for desiring ownership, authority, or oversight of exchange activity, including perceptions of making implementation faster, ensuring higher quality, or desiring autonomy. |
| Health policy | State and federal requirements, laws, regulations, and expectations to which providers and hospitals must pay attention that relate to choices about the participation in or the effectiveness of HIE. |
| HIE alternatives | The presence or availability of any other technology option for sharing patient information. |
| Market factors | Structure of local market for services, number and type of providers, and providers’ general perceptions and beliefs (including interest levels, market dynamics, local culture, and perceptions of competition). |
| Governance and operations (community HIEs) | Who is in charge of the community HIE and how the organization operates, in regard to the number of stakeholders, decision‐making processes, agenda setting, politics, and sustainability. |
| Interorganizational relationships | Formal (eg, organizational ties through existing collaborations, joint ventures, or preferred provider networks) and informal (eg, relationship a product only of referral networks or patient care patterns) relationships among health care organizations, providers, and trading partners. |
| Resources (organizational) | Health care organization's financial, technical, and knowledge (eg, expertise, experience) resources and capabilities. |
| Strategy (organizational) | Hospital's or health care provider's business strategy, needs, goals, objectives, or plans, such as movement to ACO, quality improvement ideas, desires for analytics, a need to integrate clinical information, or plans to expand referral networks. |
| Technology | Qualities, features, and amount of information available in HIE and EHR systems, including interoperability or lack of interoperability. |
| Value | Potential for value, return on investment, or worthwhile investment in time and resources, real or perceived. Is the decision, course of action, and/or expense worth it? This is not simply a measure of the cost. |
| Vendor issues | The capability, bandwidth, resources, ability, or willingness of HIE and EHR technology vendors to listen to or act on organizational requests or demands. This is not about the quality of the technology, but the vendors as organizations. |
Next, we used this coding scheme and approach to analyze the remaining transcripts. Again, we both coded another 25% of the transcripts to ensure consistency, and again, we purposefully selected to represent both states and the different organizations. After we reached a consensus through discussion, we independently coded the remaining transcripts. The inter‐rater reliability (kappa) of the independently coded transcripts was 0.61 (0.40 to 0.75 is a good agreement range).12 Differences were resolved through joint readings and another iteration of discussion and consensus building. Data analysis used NVivo10. As a validation step, we obtained feedback on the accuracy and completeness of our interpretation from 3 interviewees (representing community and enterprise HIEs).
We used tag clouds to illustrate the similarities, differences, and relative importance of each factor for community and enterprise HIEs. Tag clouds are essentially weighted lists and are a common method of visualizing keywords or popular terms online.13 We created one tag cloud to describe the barriers and enablers for enterprise HIEs and another to describe those for community HIEs. The weighted lists underlying these tag clouds were the number of times each factor was identified as a barrier or an enabler (ie, counts of the number of coded units of text). The frequency with which each factor appeared was stratified by enterprise and community HIEs, so that the relative importance of each factor was specific to the type of HIE. We categorized these counts into 3 groups based on tertile rankings. To ensure these frequency rankings were not simply a product of one particularly verbose individual, we also determined the frequency rankings by the number of interviewees citing the factor. Both methods yielded consistent results, and all factors were mentioned by multiple interviewees.
In each tag cloud, the font size reflects the frequency with which each factor was cited. The largest text size was applied to those factor and barrier/enabler combinations in the highest‐ranked group, with smaller sizes for the less frequently mentioned group. Text size and font width are the most influential factors for emphasizing importance to viewers of tag clouds.14 Consistent with other recommendations, the highest‐ranking tags were put at the top left, and we ordered tags (as best we could) in a descending frequency of rank (ie, the larger tags are on the top).15, 16 To improve readability, we did not vary the angle of the tags. Also, because we reported broad categories of factors, the factors could have acted as both a barrier and an enabler, depending on the HIE's context and type. Therefore, we separated the barriers and enablers in each cloud and provided one or more descriptive comments (in parentheses and in a smaller font) to explain the factor.
Results
Our interviews with 40 individuals revealed different perceptions, advantages, and challenges to each approach to HIE. Based on our analyses of the barriers to and enablers of each approach (Figure 1), we suggest conceptualizing enterprise HIE as a strategy for sophisticated health systems to pursue population health and new reimbursement opportunities with their desired trading partners by leveraging their own rich, aggregated clinical information and technology. In contrast, the tag cloud for community HIE (Figure 2) revealed that the community HIE is a collaborative method, with elements of a public or community good, for obtaining patient information from the broadest set of providers in response to patient care patterns and greater expectations of sharing information.
Figure 1.
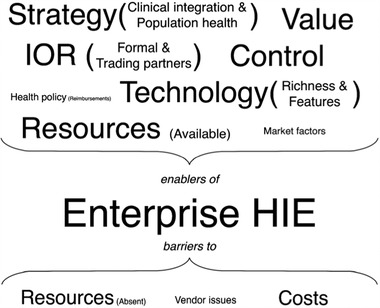
Tag Cloud Describing the Factors That Are Enablers of or Barriers to Enterprise Health Information Exchange (HIE)
The larger the font size, the more frequently the interviewees noted the factors. Additional descriptive text about each factor is enclosed in parentheses so as to highlight differences between its roles as barrier and enabler.IOR = interorganizational relationships.
Figure 2.

Tag Cloud Describing the Factors That Are Enablers of or Barriers to Community Health Information Exchange (HIE) The larger the font size, the more frequently the interviewees noted the factors. Additional descriptive text about each factor is enclosed in parentheses so as to highlight differences between its roles as barrier and enabler.IOR = interorganizational relationships.
Why Organizations Are Pursuing Enterprise HIE: “HIE Is Not the End Game. It's Just a Stepping‐stone”
Health systems create enterprise HIEs to leverage interorganizational relationships in order to achieve a strategic objective. Interviewees associated with enterprise HIEs targeted specific providers and organizations for inclusion in their exchange networks. Enterprise HIEs were meant for “friends and family.” This designation included those with existing formal organizational ties, like joint venture hospitals on different EHR platforms, affiliated physician organizations, and acquired practices. An enterprise HIE was necessary for these “family” members because even in large health systems, as an IT director noted, “We'll never have them all in the same [EHR].” These interviewees also pointed out that one purpose of an enterprise HIE was to strengthen interorganizational ties to a set of providers that were “a very large provider of people” and “major trading partners,” but without a formal relationship such as ownership or tight contracting.
The first objective of health systems with an enterprise HIE was integrating disparate clinical information into “a consolidated patient's record.” Enabling access to data from several sources was a strategy to support better and safer care, but an enterprise HIE was also a “stepping‐stone” to other organizational goals. Most of these goals were related to the financial models and quality benefits associated with a focus on population health and were encouraged by current trends in health policy. With more complete patient information, capabilities to coordinate care, and analytic capabilities (like real‐time risk stratification), health system executives viewed the enterprise HIE as a “primary strategy” to support developing accountable care organizations (ACOs), arrangements for risk sharing, Medicaid payment reform opportunities, and bundled payments. One executive explained the potential application of their feature‐ and data‐rich enterprise HIE technology: “When our patient hits a hospital for bundled payment, within 24 hours we can identify that this patient needs more care management services or not, because we have the entire clinical history.” Another executive noted that to be effective, any population‐based strategy requires a level of patient “stickiness” (ie, keeping the patient with his or her health system). The same executive went on to say that an enterprise HIE was one way for his organization to support that “stickiness.” The relationship of an enterprise HIE to broader organizational strategies was also mentioned by interviewees from outside health care organizations: “[Enterprise HIEs] are all related to accountable care and other payment reform initiatives.”
Desired control and organizational resources further motivated health care organizations to create enterprise HIEs. As explained by a health system vice president, “We want to control our own destiny, and we have the resources to do it.” An enterprise HIE was the means for health systems to have complete ownership over the responsibility of connecting different EHRs, patient data management, and technology feature decisions. Because HIE is such a critical step in other organizational strategies, health system representatives wanted assurance that they could “move quickly” and “make sure it's run properly.” That assurance came from direct control and “not relying” on someone else. An enterprise HIE also avoided any potential for misaligned goals, for as one executive noted, “[The HIE's] priorities are your own when you do it yourself.”
For those working in hospital and health systems, all these observations created a perception of value for the enterprise HIE. From the organizational perspective, an enterprise HIE supported broader goals; from the technological side, it provided solutions to internal information management challenges; and from the clinical perspective, it provided rich information integrated into existing workflows.
Finally, though not mentioned by any interviewee associated with an enterprise HIE, some representatives of community HIEs and the public sector suggested that health systems’ interest in enterprise HIEs was motivated by a desire to alter local health care market dynamics. As a community HIE leader noted, health systems in his market were attempting to “circle themselves with docs,” and an enterprise HIE was one way to do it. This was particularly the case when health systems assumed the costs of the connections to their enterprise HIE. Another community HIE leader observed the potential long‐term implications of this approach:
The big system would say, “I really want these [specialists] so we'll cover the interfaces. We can do that under a Stark [law] exception.” And now we've got a pipe . . . an exclusive pipe to this group, and the problem with having the hospital own the connection is that they'll never be able to resist using that connection.
Organizational Resources and Health IT Vendors as Barriers to Enterprise HIE
An enterprise HIE was not an option for all the health systems we interviewed. Large health systems had sufficient technical capabilities and resources of their own. These organizations could absorb the substantial costs of connecting providers, were experienced EHR users, and had built data warehouses for analytics. Smaller and financially challenged hospitals (and single hospital systems) were not in a position to “stand up” their own enterprise HIEs. As one community hospital CIO recounted, “I've looked at what's out there and I kind of stopped right there, because we do not have deep pockets. These systems are crazy expensive.” Even for large health systems, cost remained a challenge. Although, those costs were an investment that the larger health systems could and were willing to make. As the IT director at an academic medical center pursuing an enterprise HIE admitted, “We went down this road knowing that this was an investment that we'd have to make and [that] it would pay off some time in the future.”
For enterprise HIEs, costs were often reported to be a result of vendor issues. First, the sheer number of different EHR systems, even among a health system's narrowly defined set of trading partners, was substantial (one urban health system reported connecting 46 different EHRs as part of its enterprise HIE). This number escalated costs because “interfaces are expensive.” As one hospital system's senior director of IT noted,
Each one of these vendors has a specific way in which they wanna connect. . . . If you put manpower and resources against each one of those different silos of EMRs, you come up with numbers that are astronomical, because each one of those interfaces is specific and unique.
Second, the enterprise HIE's working relationship with vendors was a complication. Several interviewees reported being very satisfied with their relationships with some vendors but said that broadly, vendors were “underresourced” and “just couldn't keep up” with demand. The problem in the current environment is that “everybody is asking for the same thing at the same time.”
Why Organizations Are Pursing Community HIE: “Patients Drop In Wherever They Drop In”
By far the predominant reason that health care organizations participate in community HIEs is to obtain information about the care their patients are receiving from other providers (ie, look beyond their existing network) (see Figure 2). Health care organizations viewed community HIEs as a strategy to manage the complexity and uncertainty created by patients seeking care from unaffiliated providers in the market. A director at an urban health system serving a large Medicaid population summed up the need for a community HIE: “Fifty percent of encounters happen outside of us . . . so we don't know a lot about our patients.” Likewise, one vice president noted that his health system needed a community HIE to “reach beyond” its own network of providers for relevant information. The health care representatives spoke mainly of using the community HIE to “get” patient information, that the community HIE offered “access to information systems they wouldn't have access to otherwise,” and that the community HIE supported “patient tracking.” This perception was shared by those leading the community HIEs as well as those involved in shaping each state's health information technology policies. From the community HIE perspective, unconnected EHRs, information silos, and even enterprise HIEs were inherently limited strategies to manage and use patient information, because no single provider was ever going to have “all the data.” It was the community HIE that got information from “across the boundaries” or that was able to follow patients as “they move from one hospital system to another.”
Those interviewees supportive of community HIE efforts suggested that its ability to provide information from different, unaffiliated providers was a characteristic that created value for both health care providers and the broader public. As an example of the former, an SDE leader commented that knowledge of patients’ admissions and discharges from other community providers would be useful to any hospital concerned about its readmission rates. Similarly, as community HIE leaders suggested, any health care organization attempting to follow patients across different settings of care needed the community HIE's communitywide patient index (for matching different institutions’ medical record numbers). In addition, the interviewees noted that this movement of information across the community was benefiting primarily the patients' and the public's health. These observations were made mainly by community HIE leaders and state government representatives, although executives representing 2 different health care organizations (one of which was pursing enterprise HIE) that participated in a long‐standing New York community HIE used similar language, warning that community HIE should not be a source of competition, that it was a “community tool.”
Although community HIEs are a product of existing interorganizational relationships, these relationships are much less formal than they are for enterprise HIEs. Community HIEs benefited greatly from a history of local collaboration among competing health care organizations on such topics as community issues or regional planning activities. Potential relationships with desired medical trading partners was also a motivation for participating in community HIE efforts. Both New York and Texas are home to many community HIEs. Geographical location played some role in the decision to participate, but the desire to be connected with providers sharing common patients was the primary motivating factor.
Competing Strategies, Technology, and Governance as Barriers to Community HIE
As Figure 2 shows, the interviews revealed many more barriers to community HIE, and the role of several enabling factors was more nuanced than for the enterprise HIE. For example, organizational strategy was simultaneously a barrier and an enabler. Even though community HIE could support population health and consolidate patient information, other strategies important to health care organizations could get in the way. Health care executives in both states reported that community HIE was just one item in a long list of pressing goals (eg, “mergers,” “new billing systems,” “migration to the new version of [EHR],” “transition to ICD‐10”). In effect, as one health system vice president told us, community HIE was “deprioritized” because other needs took precedence. Viewing this same phenomenon from the other perspective, a community HIE executive stated, “One of the biggest things we compete against is the fact that they have other priorities that have dollars” (ie, technology projects tied to Meaningful Use incentive payments or revenue streams). Similarly, those health systems pursuing enterprise HIE did not view community HIE as a core infrastructure component necessary for achieving organizational goals and would not “depend on it for many of our acute needs,” that is, community HIE was less “germane to what we do day‐to‐day.”
The view that community HIE was not a core infrastructure component was related to other barriers. Health care organization executives tended to look less favorably on community HIEs’ technology capabilities and available data, particularly when contrasted with enterprise HIEs. Even according to those participating in a community HIE, health systems with enterprise HIEs could accuse community HIEs of “missing a lot” and failing to “have all the rest of the pieces of the clinical puzzle.” These perceptions of data availability and comments on system stability complicated the value proposition for community HIE. We should note, however, that the data available from community HIE depend on participation in the health care organization and on what types of information the participants are willing to share.
The role of community HIE governance depended on the interviewee's organizational affiliation. A feature of community HIE is shared, collaborative governance. This neutrality among the different stakeholders is intended to be a positive characteristic, and community HIE leaders promoted the virtues of “trust” and “equality.” In contrast, several hospital representatives saw this arrangement as a hindrance in practice, because “more organizations to please will make [it] slower” and “the more people you have in the kitchen, the harder it is to get things moving.” Likewise, an executive at a health system with an enterprise HIE saw the problem as “[community HIEs] are trying to serve many other institutions, and other institutions’ needs are varied. So what we may want from them is going to be vastly different than {what} somebody else may want from them. The turnaround time on some of this stuff needs to be very quick.” The idea of multistakeholder governance embraced by community HIE might be viewed as antithetical to many health systems’ desire for control over the exchange process.
Meaningful Use as a Barrier to Community HIE
According to interviewees from community HIEs, SDEs, and the state governments, health policies both supported and hindered the community HIE. These interviewees saw those policies creating the expectations of data exchange, technology adoption incentive funding (state and federal), and the introduction of population‐based payment models as encouraging participation in community HIE. For example, as one state government representative told us, “The reimbursement incentives are changing. . . . That's another reason that providers are needing to be connected to a [community] HIE more than before.”
At the same time, these policies, particularly the emphasis on DIRECT in Meaningful Use Stage 2, ended up discouraging and inhibiting community HIE participation. A Texas community HIE leader noted, “That's been a little disappointing in how HIE and the public sharing model really hasn't been a part of the regulations.” Another stated, “When that [anticipated community HIE participation under Meaningful Use] went away, honestly, the interest disappeared at the CEO level in the hospitals. . . . If they didn't have to do it, they didn't want to expend the effort, the money, and the trouble to participate.”
In addition to failing to support community HIE, Meaningful Use also created competition with community HIE by introducing alternative HIE models. DIRECT, exchange within the same EHR platform (ie, vendor‐mediated exchange), and enterprise HIE were reported as barriers to community HIE. Representatives of community HIEs reported being told by providers that “I have solved enough of my need for interoperability with [EHR vendor]” or “We have [EHR vendor name]. We can already do that.” In sum, a community HIE leader phrased it as Meaningful Use Stage 2 “cuts out the public entities.” At best, community HIE was a complementary method of obtaining information or even merely a supplement to other strategies supported by federal policy.
Health IT Vendors as Barriers to Community HIE
Interviewees from SDEs, state government, and community HIEs in both states said the number of health IT vendors and the associated costs of connecting to them were a problem. As in the case of enterprise HIE, community HIEs found they were trying to interface with less‐than‐truly‐interoperable EHR technology: “Each interface is customized,” “each one's one off,” and “even if you've already done it for one [EHR vendor] hospital, there's still a lot of custom work that has to be done for each facility.” Of course, each of these interfaces came at an additional cost, which tended to multiply quickly. For example, an SDE representative reported that community HIEs were “being charged $10,000, $20,000, $40,000 to connect” and that these costs included things “like an upfront fee and annual fee and monthly fee.” The same SDE representative described the situation as “[community] HIEs are being to an extent held hostage by their EHRs.” Another community HIE representative charged that the EHR vendors “don't want consistent code to be the solution because that undermines their business model.” Similarly, a Texas community HIE executive lamented that the lack of compliance with standards led to more costs: “That boot [ie, Meaningful Use] has not stayed on the neck of the vendors to the extent that it should . . . , which creates a lot of cost that we have right now.”
Interviewees in both states commented that the EHR vendors held the power and leverage, so much so that the burden was on the community HIEs to figure out how to fit health information exchange connectivity into EHRs, and not the other way around. This relationship was a product of 3 factors. First, the EHR had primacy because it was the central technology for physicians. As the vice president of a community HIE explained, because “[clinicians] live, eat, and breathe in that EHR,” the EHR vendors “are in charge of the workflow.” Second, the high costs to switch vendors meant that EHR vendors could be surer of their market position. In regard to the permanence created by switching costs, one SDE representative commented that “once the vendor is embedded in that market, it's very hard to displace them, very expensive to displace them . . . and they [the vendors] know that.” Third, community HIEs were not the most important partners for EHR vendors. As a community HIE executive acknowledged,
We are not customers of the EHR vendor, so they work with us in their spare time, which they don't have much of, or they dole out a little bit of work and then they disappear. So the limiting factor is the EHR vendor's willingness and ability to provide resources.
This put community HIEs in the position of requesting cooperation from EHR vendors. One community HIE leader summarized the effects: “We would like to go to all the EHR vendors and say, ‘Work with us on sending us the CCDs.’ And it's just like pulling teeth to get them to participate with us.” His counterpart at another community HIE reported, “The hard part is getting the EHR vendors to do their part.” Another noted: “[Vendors] are up to their eyeballs in Meaningful Use … so for [the] little [community HIE], it's hard to get their attention.” Some community HIEs, however, also reported having very successful working relationships with regional and national vendors.
Similar challenges also were found with respect to the community HIEs’ vendors of health information exchange technology. Both New York and Texas operate a network‐of‐network approach that involves multiple regional, community HIEs interconnected through a statewide network. As one state‐level interviewee told us, “Another big impediment is bandwidth of the [health information exchange technology] vendors, because it takes some 6 to 8 months to really get a lot of stuff done that shouldn't take that much time to get done.” Another interviewee noted that the challenge in connecting the different community HIEs was that “they can't talk to each other, so a technical problem is the HIE vendors are not mature yet.” In one instance, an interviewee did complain that a health information exchange vendor specifically refused to cooperate, preventing HIE‐to‐HIE exchange: “[The vendor] has basically not exposed that capability they have in the portal to a web services call.”
Consent and Market Factors as Barriers to Community HIE
Consent was one of the most commonly cited barriers to community HIEs. Both Texas and New York are opt‐in states, which require patients to provide active consent for information to be accessed. The issues associated with consent ranged from the technical (“some technical problem has bedeviled [community HIE] so that now our doctors can't see anything”) to the political (“I understand why New York State took a more stringent privacy protect‐all‐information [policy], but I think that has really inhibited HIE”) to the operational (“We spent a lot of time with attorneys and [community HIE] attorney, the state, and the Department of Health on consent forms. I mean that whole process was, I think, the most arduous and longest process in setting this whole thing up”). No matter what the difficulties with consent were, “the whole consent process destroys what could be a nice little utility” and puts widespread information availability at risk of being a “pipe dream.”
Local health care market factors could also create challenges for community HIEs. Because community HIEs were attempting to connect all health care providers in an area, they could face an uphill battle if local EHR adoption rates were low or if markets were dominated by “a lot of onesie‐twosie practices” (ie, requiring a lot of work to recruit and connect). Competition between health systems did not scuttle community HIEs, but it still defined their organizational composition. As one interviewee observed, “[Health System X] is a direct competitor of everybody. So there are few trading partners [in the area] that are interested in being a network that also has [Health System X].” A medical informaticist commented that this kind of differential community HIE participation was driven by competition and not by patient care patterns:
Honestly, I scratch my head. This is probably above my kind of strategic sense of what should be happening for patients. I still think like a clinician. To me it's a no‐brainer. [Hospitals A and B] should be in the same community HIE. I have no idea why they're separate. That's a sore point.
Connections Between HIEs
The health systems and hospitals we interviewed did not oppose the concept of community HIE, but community HIE had a definite second‐class status. Their enterprise HIE systems took priority, for as one health system executive said, “The public side gives you the rest of the picture.” Technically, this was accomplished by viewing the local community HIE as one “node,” “data source,” or link in “that chain” for its enterprise HIE. Health system leaders uniformly agreed that the primary method of accessing patient information would be via the enterprise HIE and that the community HIE would be used as a connection to a broader intrastate exchange and to access to national and public health data sources (eg, Veterans Administration or Medicaid). One community HIE in a large area acknowledged that when trying to work within the expected hierarchy, “We try to go as much as we can [so] that the provider never leaves their EHR. . . . You use their query tools to query us. We're just on the back end.” Under models proposed by more than one health system, local ambulatory care providers would not connect to the community HIE directly. Instead, they would connect to the enterprise HIE, which would serve as the provider's connection to the community HIE. Of note, one community HIE did report that it was negotiating to be the main HIE infrastructure for one health system (ie, it would be “the enterprise HIE's backbone”).
When health systems with enterprise HIEs needed information from other enterprise HIEs or even local providers who were not members of the community HIE, they reported turning to vendor‐mediated exchange and DIRECT. Several respondents viewed vendor‐mediated exchanges favorably, primarily because of the high level of integration into the EHR:
[It] enables a continuity of care document report from an external data source, whether it be through Healtheway or a private HIE.… There's a little indicator that there's outside data, so [physicians] know they're not going to waste time and they don't have to log into another portal.
A chief health information officer in a major metro area characterized their usage as “we highly leverage [the vendor‐mediated HIE] because many of the other health systems in [area] are also on [the EHR vendor].” Nevertheless, he did go on to mention the limitation by qualifying their vendor‐mediated HIE usage as “not so much for our competitors.” In the sample, each community HIE offered DIRECT, and all the organizations had DIRECT accounts. Views of DIRECT ranged from a useful way to share information with local organizations without EHRs (like long‐term care facilities), to sharing with “the nonaffiliated providers not on [the EHR vendor],” to something the hospital had to set up, not because it wanted to, but because it was “mandated.”
Limitations
Although our sample reflects diverse markets and organizations, the exchange of health information is continuing across the nation, and technological approaches, histories, and experiences in other locations may differ. New York and Texas may not be a representative sample, but their views were consistent across many different types of organizations and markets. For this reason, we did not undertake a comparative study between the 2 states. Also, our sample may actually be more favorable to community HIE because we did not include health systems that were not participating in community HIE. Some of our interviewees represented organizations that were late adopters of community HIE, so their perceptions may be similar to those of nonparticipants. In addition, information exchange options are not mutually exclusive: community HIEs offer DIRECT services, and some interviewees had access to EHR vendor‐based exchanges. We did not specifically explore the barriers to and enablers of using these approaches; we noted only how each fit within the enterprise and the community HIEs’ dynamics. Notably, our sample was limited to those in executive and policymaking positions. Even though some of the clinicians in our sample saw patients, they were primarily organizational leaders. We did not capture the views of providers involved in the day‐to‐day delivery of care, as the decisions in which we were interested are made at the organization's executive level. Last, we did not interview any health information technology vendors, so we have only clients’ perceptions of vendor behavior.
Discussion
Health information exchange is a tool to support better care and respond to policies aimed at encouraging population health management approaches. Although not an either/or decision, the reasons to participate in a community HIE and to establish an enterprise HIE are markedly different, as are the potential advantages and implications of each (Table 3). Enterprise HIE is a strategic resource with many obvious potential advantages for the leading health system, whereas community HIE has more dispersed benefits for all participants, the community, and patients. Enterprise HIE is concerned with sophisticated health systems establishing networks of desired trading partners, whereas community HIE is concerned with a broader set of providers, with the exchange network defined by patient flow patterns. Importantly, enterprise HIE is about retaining organizational control, and community HIE is about collaborative and cooperative governance. Even though these 2 approaches may be complementary, community and enterprise HIE nonetheless compete for finite organizational resources like time, skilled staff, and money, as well as attention from providers and technology vendors.
Table 3.
Comparison of the Qualities of Community and Enterprise Health Information Exchange (HIE)
| Enterprise HIE | Community HIE |
|---|---|
| Is a strategic resource | Is a community good and/or benefit |
| Is valuable to the health care organization | Is valuable to all providers and patients Connects all providers with widely variable capabilities and resources Offers collaborative and cooperative governance Has a network defined by patient care patterns and geography |
| Is led by technologically sophisticated and capable health systems | |
| Offers control | |
| Has a network of existing and desired trading partners |
The health system interviewees’ prioritization of enterprise HIE over community HIE stems from current health policies that elevate health information exchange to a necessary capability that is closely tied to financial performance. The Meaningful Use incentive program has increased the adoption of EHRs in hospitals and outpatient settings,3, 4 and these disparate systems need to be connected.8 Furthermore, any organization seeking to reap financial benefits (or to avoid any financial penalties) from the Hospital Readmissions Reduction Program,17 ACOs,18 or bundled payments19 needs patient information that is stored in different EHRs to be connected through health information exchange. Almost perversely (from the community HIE perspective), this has made health information exchange too important to health systems. For years, community HIE advocates promoted the value of interoperability and information exchange.20 Now that health system executives view health information exchange as critical to day‐to‐day operations and organizational strategy, they are reluctant to rely on community HIEs for such services. Enterprise HIE was the solution that satisfied desires for control over useful, comprehensive, aggregated patient information and that minimized dependence on other organizations.21
In addition to reporting more reasons to participate in enterprise HIE, our sample of interviewees generally noted more barriers to community HIE. In some ways, comparing enterprise and community HIE is not fair. The strengths and weaknesses of community HIE are better understood because the United States has had them for more than 20 years.22 Conversely, our interviewees’ views of enterprise HIE were based on much less experience or on only their anticipation of what enterprise HIE could do. Even though dissatisfaction with enterprise HIEs may also increase over time,23 that does not alter the important differences in health care leaders’ perceptions now. Furthermore, some critical challenges to community HIE will not change over time. The structure of the community HIE's governance is not a challenge shared by enterprise HIE, and neither is an alternative method of health information exchange, like DIRECT. Fairly or not, organizations are making strategic decisions and allocating resources based on these assessments of community HIE.
Nonetheless, enterprise HIE is unlikely to assume several important roles that only a widespread, functional community HIE can fulfill. Most important, and by design, enterprise HIE cannot produce a consolidated view of patient information that includes care from unaffiliated providers, whereas this information is possible with community HIE. The majority of state‐level HIEs have implemented such services,24 and many community HIEs maintain the record locator services necessary to find patients’ records across multiple organizations’ EHRs.25 Many community HIEs also provide analytic services to small hospitals and are a source of population‐level data for public health and government purposes.26 These are valuable services, but ones for which the return on investment is not always easy to find or that the participating organizations may not view as worth supporting.27
Policy Implications
Enterprise HIE's strong business case and value proposition, coupled with the perceived challenges to community HIE, threaten the sustainability and functionality of community HIEs. One reason is that enterprise HIE narrows the use case and value proposition for community HIE by defining community HIE solely as an incremental gain in information availability. All our interviewees agreed that enterprise HIE needs community HIE for access to broader sources of patient information. Given the governance, cost, and barriers to consent, however, health systems may not be interested in prioritizing community HIE for access to what is considered additional patient information. Furthermore, as our interviewees reported, if enterprise HIE's rich data better support population‐based analytics and data mining, then large health systems will not seek these services from community HIEs. This would represent a critical loss of a revenue stream,28 leaving only low‐resource hospitals as potential customers for community HIE's analytic services.
Currently, the US health system and health policies are not structured to ensure that enterprise HIEs and community HIEs complement each other. Even though our interviewees reported seeing value in both and did not see the 2 approaches as mutually exclusive, in fact, community HIE and enterprise HIE are competitors. Both approaches need access to the same organizational resources and attention, but as this study revealed, in many cases and for many reasons, community HIEs are losing that competition. To make sure that the types of services offered by community HIEs remain available to local providers, state or federal policy could require and fund enterprise HIEs’ and all providers’ connectivity to community HIE.29 Ensuring provider connectivity to community HIEs would be consistent with the importance of health information exchange to current health policy and reforms30, 31 and would solidify the idea that communitywide health information exchange is a public good.6, 32 This action would do much to clear up the uncertainty caused by the federal government's de‐prioritization of the “network‐of‐network” approach to health information exchange25 during the past decade and would remove the challenge of trying to monetize community benefits and public health services.28 Some states, like New York, are proposing such requirements.33, 34 Also, connectivity requirements for all providers (including hospitals and health systems) would prevent an enterprise HIE from becoming a silo of patient information. At the same time, however, health systems would still have the freedom to use and structure their enterprise HIEs in pursuit of their desired network participant and technology agendas. The difference would be that patient information with the enterprise HIE would be supplemented by the entire community and that this information would support care whenever the patient sought it outside a particular health system.
Taking steps to guarantee the movement of patient information across providers is consistent with the just passed Medicare Access and CHIP Reauthorization Act of 2015, which “declares it a national objective to achieve widespread exchange of health information.”35 Unfortunately, our findings indicate several obstacles to widespread and easy health information exchange. Both enterprise and community HIEs are working in an environment of certified electronic health records encouraged by Meaningful Use. Nonetheless, all these “interoperable” products required expensive, and often nonreusable, custom interfaces in order to connect to the community or enterprise HIE. On the surface, these reports from community and enterprise HIE representatives echo the Office of the National Coordinator's recent definition of “information blocking” (eg, practices interfering with or restricting exchange), which includes “charging prices or fees (such as for data exchange, portability, and interfaces) that make exchanging and using electronic health information cost prohibitive.”36 (Note: Our study did not independently verify such comments or explore the details of interface costs.) At a minimum, these experiences fit with a growing awareness of the extent of the EHR vendors’ control over information and the costs associated with accessing that information for health information exchange.37 In contrast, some interviewees reported that some of their EHR vendors were willing to take approaches that minimized cost (eg, creating a single connection to all customers on their product or using the interfaces they had created for customers in other markets). Regardless, EHR vendors were generally viewed as a hindrance, a cost, and a limitation on information sharing. The problem is that the cost of achieving information exchange is not being borne by those publicly subsidized EHRs that are supposedly certified as interoperable. Instead, the cost of realizing interoperability is being borne by the health systems and the HIE organizations trying to leverage information for patient health, public health, and organizational objectives. These reported barriers reinforce recent recommendations by health IT experts that EHR vendors be required to use public, standard‐based application programming interfaces (APIs) to make information more accessible through exchange.38, 39 These concerns were not limited to EHR vendors, as one HIE vendor was purportedly engaging in behavior that could be construed as blocking information, and both states had health care organizations that were not participating in exchange activities.
Health systems believe that enterprise HIE will leverage their existing relationships with ambulatory care providers for patient health and organizational performance gains. Also, participating ambulatory care providers may benefit from such (promised) rich data, and a single connection to an enterprise HIE may be easier or even less expensive than many connections to different health systems or community HIEs. Despite these potential advantages, the development of health system–controlled networks of technology‐connected providers is not without concerns. Already, numerous pressures are moving the US health system toward increased service delivery integration and the features of enterprise HIE suggest that this technology could dramatically alter referral patterns and market shares. As our interviewees pointed out, the richness of clinical data and the integration of features may be unmatched by any community HIE or other mechanism to exchange information. Ultimately, once connected to an enterprise HIE, it could be simply easier and cheaper for ambulatory care providers to refer patients to only those other connected institutions.40 This expectation has precedents. The introduction of a shared electronic health record for an integrated delivery system reduced external referrals,41 and shared information systems have led to smaller and tighter organizational networks in other industries.42 No interviewee associated with an enterprise HIE suggested the overall objective was market consolidation through a type of “virtual integration.”43 Those interviewees associated with community HIEs, however, were willing to attribute such motivations to those health systems pursuing enterprise HIEs. Even with a requirement for enterprise HIEs and other providers to connect to a community HIE, changes to referral patterns would be a possibility. This result would warrant ongoing monitoring, but unfortunately, the United States does not have a robust inventory of enterprise HIEs to easily evaluate their impact on referral patterns.
At the same time that enterprise HIE is creating tighter integration with local providers, it could marginalize other providers and patient populations to the detriment of overall public health. Health systems are creating, with purpose and care, a network of physicians and practices for inclusion in their enterprise HIEs. While not specifically excluded, public health clinics, providers serving large Medicaid populations, and other safety‐net providers may not fit enterprise HIEs’ definition of “desired trading partners” or “friends and family.” Although we found no indication that enterprise HIEs would intentionally exclude such organizations from their networks, we also found no indication of any incentives to include them.
Conclusions
While potentially complementary, community and enterprise HIE are competing for the same organizational resources and stakeholders. Furthermore, current health policies create a stronger business case for enterprise HIE. To ensure that the public benefits from a communitywide health information exchange among all providers, community HIEs may require public funding and supporting regulation to ensure their continued sustainability and service delivery.
Funding/Support: This project was funded by the Agency for Healthcare Research and Quality (#IR03HS020304‐01A1).
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. No disclosures were reported.
Acknowledgments: We thank both Mr. Dylan Dacy for his assistance with analysis and the interviewees and their respective organizations for their cooperation. To keep interviewee confidentiality (which was assured as part of the informed consent process), we do not report representative quotes by any institution or job title combination that might be identifiable. The institutional review board of Weill Cornell Medical College approved this study.
References
- 1. National Alliance for Health Information Technology . Report to the Office of the National Coordinator for Health Information Technology on defining key health information technology terms. 2008. http://healthit.hhs.gov/portal/server.pt?open=18&objID=848133&parentname=CommunityPage&parentid=5&mode=2&in_hi_userid=10741&cached=true. Accessed March 3, 2010.
- 2. Office of the National Coordinator for Health Information Technology . State Health Information Exchange Cooperative Agreement Program. 2012. http://healthit.hhs.gov/portal/server.pt?open=512&objID=1488&mode=2. Accessed October 5, 2015.
- 3. Furukawa MF, Patel V, Charles D, Swain M, Mostashari F. Hospital electronic health information exchange grew substantially in 2008–12. Health Aff. 2013;32(8):1346‐1354. [DOI] [PubMed] [Google Scholar]
- 4. Furukawa MF, King J, Patel V, Hsiao C‐J, Adler‐Milstein J, Jha AK. Despite substantial progress in EHR adoption, health information exchange and patient engagement remain low in office settings. Health Aff. 2014;33(9):1672‐1679. [DOI] [PubMed] [Google Scholar]
- 5. US Department of Health & Human Services . 45 CFR Part 170. 2014 Edition Release 2 Electronic Health Record (EHR) Certification Criteria and the ONC HIT Certification Program; Regulatory Flexibilities, Improvements, and Enhanced Health Information Exchange. Final Rule. Federal Register. 2014;79(176). [PubMed] [Google Scholar]
- 6. Vest J, Gamm LD. Health information exchange: persistent challenges & new strategies. JAMIA. 2010;17(3):288‐294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rubin RD. The community health information movement: where it's been, where it's going In: O'Carroll PW, Yasnoff WA, Ward ME, Ripp LH, Martin EL, eds. Public Health Informatics & Information Systems. New York, NY: Springer; 2003. [Google Scholar]
- 8. Harris Healthcare Solutions . Harness the Power of Enterprise HIE. Melbourne, FL: Harris Healthcare Solutions; 2012. [Google Scholar]
- 9. Centers for Medicare & Medicaid Services . Frequently asked questions (FAQ7697). 2014. https://questions.cms.gov/faq.php?faqId=7697. Accessed December 18, 2015.
- 10. Merriam SB. Qualitative Research: a Guide to Design and Implementation. San Francisco, CA: Jossey‐Bass; 2009. [Google Scholar]
- 11. Saldaña J. The Coding Manual for Qualitative Researchers. 2nd ed Thousand Oaks, CA: Sage Publications; 2013. [Google Scholar]
- 12. QSR. NVivo10 for Windows Help . 2014. http://help‐nv10.qsrinternational.com/desktop/procedures/run_a_coding_comparison_query.htm. Accessed February 12, 2014.
- 13. Sinclair J, Cardew‐Hall M. The folksonomy tag cloud: when is it useful? J Inf Sci. 2008;34(1):15‐29. [Google Scholar]
- 14. Bateman S, Gutwin C, Nacenta M. Seeing things in the clouds: the effect of visual features on tag cloud selections. Proceedings of the 19th ACM Conference on Hypertext and Hypermedia. 2008. Pittsburgh, PA. doi:10.1145/1379092.1379130. [Google Scholar]
- 15. Halvey MJ, Keane MT. An assessment of tag presentation techniques Proceedings of the 16th International Conference on World Wide Web. 2007. Banff, AB, Canada. doi:10.1145/1242572.1242826. [Google Scholar]
- 16. Rivadeneira AW, Gruen DM, Muller MJ, Millen DR. Getting our head in the clouds: toward evaluation studies of tagclouds Proceedings of the SIGCHI Conference on Human Factors in Computing Systems. 2007. San Jose, CA. doi:10.1145/1240624.1240775. [Google Scholar]
- 17. Jackson CT, Trygstad TK, DeWalt DA, DuBard CA. Transitional care cut hospital readmissions for North Carolina Medicaid patients with complex chronic conditions. Health Aff. 2013;32(8):1407‐1415. [DOI] [PubMed] [Google Scholar]
- 18. DeVore S, Champion RW. Driving population health through accountable care organizations. Health Aff. 2011;30(1):41‐50. [DOI] [PubMed] [Google Scholar]
- 19. Williams C, Mostashari F, Mertz K, Hogin E, Atwal P. From the Office of the National Coordinator: the strategy for advancing the exchange of health information. Health Aff. 2012;31(3):527‐536. [DOI] [PubMed] [Google Scholar]
- 20. Starr P. Smart technology, stunted policy: developing health information networks. Health Aff. 1997;16(3):91‐105. [DOI] [PubMed] [Google Scholar]
- 21. Cook K, Shortell SM, Conrad DA, Morrisey MA. A theory of organizational response to regulation: the case of hospitals. Acad Manage Rev. 1983;8(2):193‐205. [PubMed] [Google Scholar]
- 22. Adler‐Milstein J, Bates DW, Jha AK. Operational health information exchanges show substantial growth, but long‐term funding remains a concern. Health Aff. 2013;32(8):1486‐1492. [DOI] [PubMed] [Google Scholar]
- 23. Ancker JS, Miller MC, Patel V, Kaushal R. Sociotechnical challenges to developing technologies for patient access to health information exchange data. JAMIA. 2014;21(4):664‐670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. National Opinion Research Center (NORC) . Evaluation of the State Health Information Exchange Cooperative Research Agreement Program. State Approaches to Enabling HIE: Typology Brief. Bethesda, MD: NORC; 2014. [Google Scholar]
- 25. Lenert L, Sundwall D, Lenert ME. Shifts in the architecture of the Nationwide Health Information Network. JAMIA. 2012;19(4):498‐502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Shapiro JS, Mostashari F, Hripcsak G, Soulakis N, Kuperman G. Using health information exchange to improve public health. Am J Public Health. 2011;101(4):616‐623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kleinke JD. Dot‐gov: market failure and the creation of a national health information technology system. Health Aff. 2005;24(5):1246‐1262. [DOI] [PubMed] [Google Scholar]
- 28. Vest J, Campion TR Jr, Kaushal R, for the HITEC Investigators . Challenges, alternatives, and paths to sustainability for health information exchange efforts. J Med Syst. 2013;37(6):9987. [DOI] [PubMed] [Google Scholar]
- 29. Miller RH. Satisfying patient‐consumer principles for health information exchange: evidence from California case studies. Health Aff. 2012;31(3):537‐547. [DOI] [PubMed] [Google Scholar]
- 30. Office of the National Coordinator for Health Information Technology . Principles and Strategy for Accelerating Health Information Exchange (HIE). Washington, DC: Centers for Medicare & Medicaid Services; 2013. [Google Scholar]
- 31. Office of the National Coordinator for Health Information Technology . Federal Health IT Strategic Plan 2015‐2020. Washington, DC; 2014. [Google Scholar]
- 32. Adler‐Milstein J, Bates DW, Jha AK. U.S. regional health information organizations: progress and challenges. Health Aff. 2009;28(2):483‐492. [DOI] [PubMed] [Google Scholar]
- 33. National Opinion Research Center (NORC) . Evaluation of the State Health Information Exchange Cooperative Agreement Program: Early Findings from a Review of Twenty‐Seven States. Bethesda, MD: NORC; 2012. [Google Scholar]
- 34. Chokshi DA, Rugge J, Shah NR. Redesigning the regulatory framework for ambulatory care services in New York. Milbank Q. 2014;92(4):776‐795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Medicare Access and CHIP Reauthorization Act of 2015, STAT. 87 (2015).
- 36. Office of the National Coordinator for Health Information Technology . Report to Congress: Report on Health Information Blocking. Washington, DC: US Department of Health and Human Services; April 2015. [Google Scholar]
- 37. Allen A. Doctors say data fees are blocking health reform. 2015. http://www.politico.com/story/2015/02/data‐fees‐health‐care‐reform‐115402.html#ixzz3SwzncooP. Accessed February 27, 2015.
- 38. Payne TH, Corley S, Cullen TA, et al. Report of the AMIA EHR 2020 Task Force on the status and future direction of EHRs. JAMIA. 2015. doi:http://dx.doi.org/10.1093/jamia/ocv066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. JASON . A Robust Health Data Infrastructure. AHRQ Publication No. 14‐0041. Rockville, MD: Agency for Healthcare Research and Quality; 2014. [Google Scholar]
- 40. Ramaiah M, Subrahmanian E, Sriram RD, Lide BB. Workflow and electronic health records in small medical practices. Perspectives in Health Information Management / American Health Information Management Association. 2012;9(Spring):1d. [PMC free article] [PubMed] [Google Scholar]
- 41. Chen C, Garrido T, Chock D, Okawa G, Liang L. The Kaiser Permanente electronic health record: transforming and streamlining modalities of care. Health Aff. 2009;28(2):323‐333. [DOI] [PubMed] [Google Scholar]
- 42. Gurbaxani V, Whang S. The impact of information systems on organizations and markets. Community ACM. 1991;34(1):59‐73. [Google Scholar]
- 43. Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff. 2008;27(3):759‐769. [DOI] [PubMed] [Google Scholar]


