Abstract
Intestinal ischemia is a life-threatening condition associated with a broad range of clinical conditions including atherosclerosis, thrombosis, hypotension, necrotizing enterocolitis, bowel transplantation, trauma and chronic inflammation. Intestinal ischemia-reperfusion (IR) injury is a consequence of acute mesenteric ischemia, caused by inadequate blood flow through the mesenteric vessels, resulting in intestinal damage. Reperfusion following ischemia can further exacerbate damage of the intestine. The mechanisms of IR injury are complex and poorly understood. Therefore, experimental small animal models are critical for understanding the pathophysiology of IR injury and the development of novel therapies.
Here we describe a mouse model of acute intestinal IR injury that provides reproducible injury of the small intestine without mortality. This is achieved by inducing ischemia in the region of the distal ileum by temporally occluding the peripheral and terminal collateral branches of the superior mesenteric artery for 60 min using microvascular clips. Reperfusion for 1 hr, or 2 hr after injury results in reproducible injury of the intestine examined by histological analysis. Proper position of the microvascular clips is critical for the procedure. Therefore the video clip provides a detailed visual step-by-step description of this technique. This model of intestinal IR injury can be utilized to study the cellular and molecular mechanisms of injury and regeneration.
Keywords: Medicine, Issue 111, intestinal injury, ischemia, reperfusion, regeneration, laparotomy, superior mesenteric artery, mouse
Introduction
The intestine is very sensitive to interruption of blood flow which causes ischemia and epithelial damage. Reperfusion after ischemia provides re-oxygenation of the tissue, and can further promote pathology. Therefore, intestinal ischemia and reperfusion injury is associated with a wide range of pathologies, including necrotizing enterocolitis, allograft rejection in small bowel transplantation, complications of abdominal aortic aneurysm surgery, cardiopulmonary bypass, and inflammatory bowel disease 1,2. Intestinal IR injury, especially acute mesenteric ischemia, is a life threatening condition resulting in morbidity and mortality 3.
Although poorly understood, intestinal ischemia-reperfusion (IR) injury is thought to be associated with changes in the gut microbiota as well as the production of reactive oxygen species and inflammatory cytokines and chemokines 1,4-6. This leads to activation of both innate and adaptive immune mechanisms which promote inflammation and tissue injury 1,7,8.
Animal models are critical for understanding the mechanisms of IR injury, as they allow easy gain- and loss-of-function genetic experiments. Several animal models of IR have been developed which include complete vascular occlusion, low flow ischemia, and segmented vascular occlusion (summarized in a recent comprehensive review 9). Intestinal ischemia caused by complete vascular occlusion of superior mesenteric artery (SMA) is an easy and commonly used model of IR in large animals and rodents 9-11. However, different areas of the gut have different susceptibility to injury. In addition, the diverse range of anesthetics, analgesics, artery occlusion techniques, as well as inconsistency in the duration of ischemic injury and recovery result in variable degrees of injury confounding our understanding of the biology of IR across multiple studies. Table 1 demonstrates these inconsistencies in murine IR studies. The biggest drawback from using shorter ischemic times (30-45 min) is targeting the window of recovery upon which discernible differences between cases and controls can be observed. Mild injury to the epithelium may be resolved an hour after reperfusion, therefore specialized pathological metrics may be required to find differences in epithelial restitution. In contrast, excessive damage, as seen by 100 min of ischemic injury may result in the complete denudement of the epithelium, where restitution is no longer possible, increasing the rate of mortality, and recovery time. Therefore, here we describe the detailed procedure of intestinal IR in mice which results in reproducible injury without mortality to encourage the standardization of this technique across our field. This model of intestinal IR injury can be utilized to study the cellular and molecular mechanisms of injury and regeneration.
Protocol
Animal studies were performed in accordance with the National Institute of Health guidelines and were approved by the Institutional Animal Care and use Committee of the Trudeau Institute. 8-12 week old C57BL/6 mice were used for the study.
1. Preparation for Surgery
Prepare and sterilize surgical instruments.
Prepare isoflurane-based anesthesia system with nose cone, and heated pad. Make sure heated pad is not overheated (<39 ºC).
Make sure that the isoflurane gas scavenging canister is positioned correctly to ensure the exhaust ports at the bottom of the canister are not blocked or occluded in any way. Weigh gas scavenging canister prior to procedure and document weight on canister. Discard canister when canister weight exceeds 50 g of accumulated weight (~12 hr).
2. Anesthesia
- Anesthetize mouse with 3% isoflurane in an induction chamber (1 L/min O2).
- Assess anesthetic depth by an inability to remain upright, loss of purposeful voluntary movement, loss of blink reflex, muscle relaxation, and loss of response to reflex stimulation (toe or tail pinch with firm pressure).
- Assess respiratory rate and pattern by observing chest wall and abdominal movements. Under optimal anesthesia, the breath rate should be ~ 55-65 breaths per min.
- Remove mouse from the induction chamber and quickly shave the abdomen area of the mouse.
To prevent corneal desiccation, place bland ophthalmic ointment in the eyes.
Place mouse on the heated pad and connect it via nose cone to anesthesia system. Make sure latex nose cone membrane firmly fits over the head of the mouse and there is no leak of isoflurane.
Reduce isoflurane rate to 1.5%, and inject buprenorphine (0.1 mg/kg) and ketamine (10 mg/kg) subcutaneously to prevent wind-up of the pain-cascade.
Wipe the skin of the operation area with a sterile cotton swab soaked with Betadine surgical solution followed by 70% ethanol.
3. Surgery
Make a mid-line 3-5 cm laparotomy with operating scissors. Cover operation area with sterile non-adherent pad moistened with saline. Isolate cecum and ileum and expose the superior mesenteric artery using cotton swabs moistened in saline.
To facilitate clip applying, make small nicks in the mesentery surrounding the superior mesenteric artery using fine iris scissors.To do this, gently raise the intestine with dressing forceps and cut mesentery on both sides of the superior mesenteric artery at the desired clip position (Figure 1A). Then, add few drops of sterile saline to the area of desired clip position before applying clips. Note: To perform the sham surgery, follow the surgical procedure up to step 3.2. Do not apply clips. Instead, maintain the tissue moist by added warm saline as described in 3.6 for 1 hr. Afterwards, proceed to step 4.1,
Occlude the first order branches of the superior mesenteric artery with microvascular clips (70 g force) using a clip applier to create a 5-7 cm region of the ischemic ileum adjacent to cecum (Figure 1B). Although the position of the vessels is conservative, there might be slight variations between mice (see examples on Figure 1). Therefore, 2 or 3 clips are usually required (see the location of the clips on Figure 1A, D, E, black arrows). Note: Use high quality vessel clips. High pressure clips can damage vessels and prevent regeneration whereas low pressure clips (<30 g) may not completely block blood flow.
Block collateral blood flow through the intestine using two microvascular clips across vessels (40 g force), demarking the region of ischemic intestine (Figure 1). Occlusion of collateral vessels is required to prevent blood supply from adjacent blood vessels (see the location of the clips on Figure 1A, D, E, green arrows).
Optional: Add heparin solution (6 USP units/ml), to prevent blood clotting. Dropwise add 0.5 ml of heparin solution to the isolated intestine.
Wet sterile non-adherent pad delicate wipes with saline pre-warmed to 37 °C and apply to surgical area. Make sure that wipes remains wet during the entire procedure.
Maintain ischemia for 60 min using 1-1.5% isoflurane anesthesia throughout. If ischemia procedure is performed correctly, the ischemic region will change to wine red in color in approximately 30 min. Note that blood vessels distal to the clip position are enlarged during ischemia (Figure 1, right panels) indicating successful occlusion.
Closely monitor the mouse during the ischemia stage. Continue to apply saline solution to the non-adherent pad covering the surgery site.
Mark the edges of the ischemic area by pipetting 20 μl of Gill`s 3 hematoxylin on the tissue to facilitate harvesting the ischemic tissue and adjacent healthy tissue from the same mouse for comparison (Figure 1E, right panel).
4. Reperfusion Stage
At the end of the ischemia add few drops of saline on the clip area and gently remove microvascular clips with clip applier. Then, gently push the intestine back to the abdominal cavity using saline moistened cotton tips. Remove non-adherent pad and close the abdominal wall and skin using 9 mm stainless steel wound clips. If reperfusion is performed longer than 3 hr, use an absorbable vicryl suture to close the abdominal wall before applying wound clips on skin.
Maintain mice in a heated clean cage for desired amount of time (30 min, 60 min, 120 min, or 180 min) for the reperfusion phase.
Check animals at least every 30 min to assure stability.
5. Necropsy and Harvesting of Small Intestine
Euthanize mice by CO2 overdose followed by cervical dislocation at the desired time following reperfusion.
Open abdominal cavity and collect the ischemic intestinal tissue for further analysis. Harvest healthy normal tissue adjacent to the injured tissue as an internal control to account for any systemic reaction to injury. Note: This control is more appropriate than the sham operated control mice because sham operated mice do not undergo a systemic reaction to IR-induced injury.
Wash out intestinal content using 30 ml syringe with attached gavage needle filled with saline and then cut the intestine longitudinally. If a sample of intestine is required for gene expression analysis, cut a 1.5 mm fragment longitudinally, and use the remaining piece for histological analysis.
For histological analysis, prepare a Swiss roll using a pair of forceps to roll the intestine.
To maintain the rolled form, place the pieces of intestine between biopsy foam pads in tissue cassettes (Figure 2). Place the cassettes in 10% buffered formalin.
Fix tissue in formalin for at least 24 hr. Replace formalin with 70% Ethanol for an additional 24 hr. Store tissue in 70% ethanol indefinitely at room temperature.
Embed in paraffin, cut 5 µm sections and stain with hematoxylin and eosin using a standard protocol (Figure 3).
6. Scoring
Score the murine ischemia-reperfusion injury as summarized in Table 2. Choose an appropriate scoring method.
Optional: Divide the field of view into four sections since the severity of the injury varies throughout the section.
Calculate the average grade of each section from scores obtained blindly.
Compare the grade of the injured tissue between cases and control as well as to the uninjured tissue using a Kruskal-Wallis Test, followed by a Dunn's multiple comparisons test.
Representative Results
We optimized the experimental protocol of IR surgery to obtain reproducible IR induced injury of the ileum in mice. Representative results are demonstrated in this section.
Figure 1 shows examples of microvascular clips position to induce ischemia of the ileum. Black arrows show position of the main clips occluding first order branches of superior mesenteric artery. Green arrows show the position of additional clips to block blood supply from collateral vessels. Note increased size of occluded vessels distal to the clips position and color change of the ischemic region of intestinte. After removal of the clips at the end of ischemia blood vessels regain blood flow and return to normal size.
Figure 2 shows an example of a tissue cassette containing Swiss rolls prepared from control and ischemic regions of the ileum after 1 hr of ischemia, followed by a 1 hr of reperfusion. A piece of spleen was included to facilitate positioning of control and IR intestine during processing and staining. Note the color difference between control and ischemic tissue.
Figure 3 shows representative hematoxylin and eosin staining of control and ischemic regions of the ileum after 1 hr of ischemia, or 1 hr of ischemia followed by a 2 hr of reperfusion. Note the severe damage of the epithelium after 1 hr of ischemia characterized by hemorrhagic villi, epithelium denudement with partial to complete ablation of crypts, and immune cell infiltration (asterisk). After a 2 hr of reperfusion villi damage and inflammation persist (asterisk), but there is no tissue hemorrhage.
Figure 4 shows an example of the analysis of inflammatory cytokines expression at 1 hr and 2 hr after ischemia-reperfusion in ischemic and control intestine. Note upregulation of mRNA expression of TNF, IL-1b, IL-6 and CXCL2 at 1 hr and 2 hr after ischemia-reperfusion compared to control healthy tissue.
 Figure 1: Induction of Ischemia using Vascular Clips. (A) Isolated area of the intestine containing cecum and ileum. Small cuts in the mesentery surrounding the superior mesenteric artery are made to facilitate clip application. (B) Microvascular clip application using clip applier. (C) Position of microvascular clips on superior mesenteric artery to induce ischemia. (D, E). Examples of vasculature structure and clip positioning in different mice. Arrows indicate the ischemic area of ileum marked by hematoxylin. Please click here to view a larger version of this figure.
Figure 1: Induction of Ischemia using Vascular Clips. (A) Isolated area of the intestine containing cecum and ileum. Small cuts in the mesentery surrounding the superior mesenteric artery are made to facilitate clip application. (B) Microvascular clip application using clip applier. (C) Position of microvascular clips on superior mesenteric artery to induce ischemia. (D, E). Examples of vasculature structure and clip positioning in different mice. Arrows indicate the ischemic area of ileum marked by hematoxylin. Please click here to view a larger version of this figure.
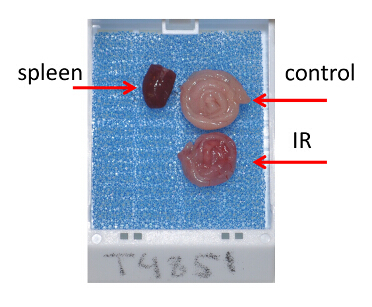 Figure 2: Tissue Preparation for Histological Analysis. Tissue cassette containing Swiss rolls prepared from ischemic and control regions of the ileum after 1 hr of ischemia followed by a 1 hr of reperfusion. Please click here to view a larger version of this figure.
Figure 2: Tissue Preparation for Histological Analysis. Tissue cassette containing Swiss rolls prepared from ischemic and control regions of the ileum after 1 hr of ischemia followed by a 1 hr of reperfusion. Please click here to view a larger version of this figure.
 Figure 3: Hematoxylin and Eosin Staining of Ileum after Ischemia. Hematoxylin and eosin staining of control and ischemic regions of the ileum after 1 hr of ischemia, or 1 hr of ischemia followed by a 2 hr of reperfusion. Bars = 500 μm (top panels), 200 μm (bottom panels). Please click here to view a larger version of this figure.
Figure 3: Hematoxylin and Eosin Staining of Ileum after Ischemia. Hematoxylin and eosin staining of control and ischemic regions of the ileum after 1 hr of ischemia, or 1 hr of ischemia followed by a 2 hr of reperfusion. Bars = 500 μm (top panels), 200 μm (bottom panels). Please click here to view a larger version of this figure.
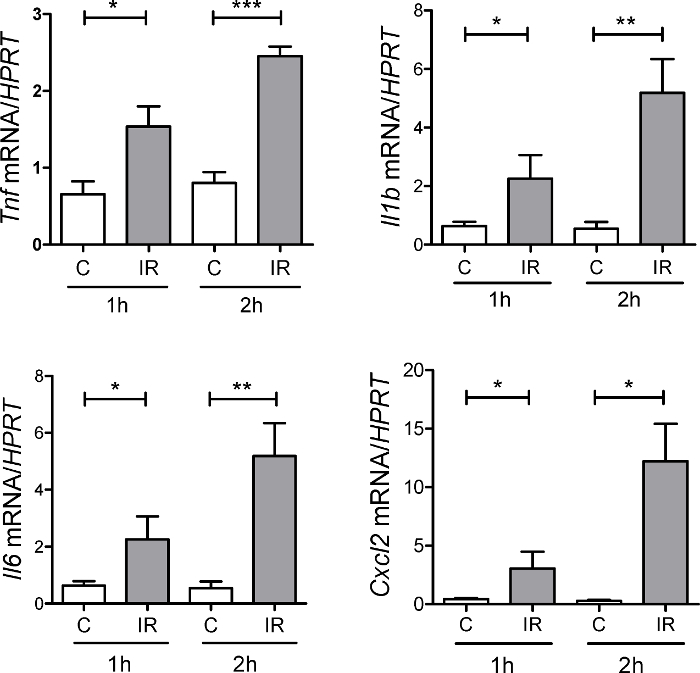 Figure 4: Expression of Inflammatory Cytokines During Ischemia-Reperfusion. Expression of CXCL2, TNF, IL-6, IL-1b was measured at 1 hr and 2 hr after ischemia-reperfusion in ischemic tissue (IR) and normal control tissue (C) adjacent to the ischemic region by real-time PCR. n = 3 - 8 mice per group, * p <0.05; ** p <0.01; *** p <0.001. Error bars represent s.e.m. Please click here to view a larger version of this figure.
Figure 4: Expression of Inflammatory Cytokines During Ischemia-Reperfusion. Expression of CXCL2, TNF, IL-6, IL-1b was measured at 1 hr and 2 hr after ischemia-reperfusion in ischemic tissue (IR) and normal control tissue (C) adjacent to the ischemic region by real-time PCR. n = 3 - 8 mice per group, * p <0.05; ** p <0.01; *** p <0.001. Error bars represent s.e.m. Please click here to view a larger version of this figure.
| Murine Species | Anesthesia / Analgesia | Artery occlusion method | Ischemia time | Time after reperfusion | Reference |
| Sprague-Dawley rats | Sodium pentobarbital | Occlusion of SMA and celiac artery using aneurysm clip or clamp | 45 min | 2 hr | 12 |
| C57Bl6/129 | 2% halothane | Occlusion of mesenteric arteriole, and the proximal and distal portions of the ischemic tissue. | 30 to 130 min | 6 hr | 13 |
| C57BL/6 | Ketamine, Isoflurane | Occlusion of SMA using aneurysm clips. Occlusion of collateral circulation at the proximal and distal areas. | 1 hr | 1.5 hr | 4,8,11 |
| C3H/Hej | Sodium pentobarbital | Occlusion using aneurysm clip or clamp | 40 min | 6 hr | 14 |
| C56BL/6 | Isoflurane | Occlusion of SMA and ileocolic artery using aneurysm clip or clamp | 100 min | 1, 2, 4, 24 hr | 15 |
| C57BL/6 | Urethane | Occlusion using aneurysm clip or clamp | 45 min | 60 min | 16 |
Table 1: Variations in Methodology in Murine Intestinal IR-induced Injury
| Histology scoring system | Reference |
| Grade 0: Normal mucosa | 13,17,18 |
| Grade 1: Subepithelial space at the villous tip | |
| Grade 2: More extended subepithelial space | |
| Grade 3: Epithelial lifting along the villous sides | |
| Grade 4: Denuded villi | |
| Grade 5: Loss of villous tissue | |
| Grade 6: Crypt layer infarction | |
| Grade 7: Transmucosal infarction | |
| Grade 8: Transmural infarction | |
| Grade 0: Normal mucosa | 4,8,11,19-21 |
| Grade 1: Sloughing of cells on villous tips | |
| Grade 2: Mid-villous damage | |
| Grade 3: Villi were absent, but crypts were still readily detectable | |
| Grade 4: Complete absence of epithelial structures and transmural necrosis | |
| Grade 0: Normal villus | 6,22-31 |
| Grade 1: Villi with tip distortion | |
| Grade 2: Goblet cells and Gugenheims' spaces are missing | |
| Grade 3: Villi with patchy disruption of the epithelial cells | |
| Grade 4: Villi with exposed, but intact lamina propria with epithelial cell sloughing | |
| Grade 5: Lamina propria is exuding | |
| Grade 6: Villi that display hemorrhage or to villi that are denuded | |
| Grade 0: Normal histology | 32,33 |
| Grade 1: Slight disruption of the surface epithelium | |
| Grade 2: Epithelial cell loss injury at villus tip | |
| Grade 3: Mucosal vasocongestion, hemorrhage, and focal necrosis with loss of less than half of villi | |
| Grade 4: Damage extending to more than one-half of villi |
Table 2: Histology Scoring Systems in Murine Intestinal IR-induced Injury
Discussion
The development of mouse models of intestinal IR injury have greatly improved the understanding of the mechanisms of tissue injury and aided in the development of potential therapeutic strategies to minimize tissue damage 7,9,11,34. The critical steps of this protocol are proper positioning of the microvascular clips, correct timing of the ischemia and proper histologic evaluation of IR injury.
The duration of ischemia is critical for subsequent epithelial damage. The typical time required to induce reproducible IR injury without morbidity and mortality of experimental mice is 45-60 min followed by a 2-3 hr reperfusion. Extended periods of ischemia may results in complete loss of the epithelium and increased mortality. For example, in a porcine model of jejunal ischemia, 60 min occlusion resulted in partial loss of villa epithelium, whereas occlusion for 120 min led to the complete loss of villus epithelium 35. Importantly, germ-free and genetically manipulated mice may display an increased sensitivity to IR injury, and therefore optimal time of ischemia and reperfusion may need to be optimized in preliminary experiments. Although typical time for evaluation of tissue damage after reperfusion is 2-3 hr, longer time (12 hr) is required for the analysis of intestinal stem cell mobilization 36. Additionally, changes in commensal microbiota and TLR/Nod-mediated signaling can significantly influence the outcome of the of IR injury 4,8,37-39.
The proper position of microvascular clips is also critical for reproducible IR injury. Here we describe the model of IR injury of the murine distal ileum. Distinct parts of the intestine are known to display different sensitivity to IR injury. For example, jejunum is more sensitive to IR injury than ileum and colon 9,34,40. In fact, ischemia-reperfusion model of jejunum by occluding SMA with a single clip is commonly used to study the mechanisms of IR injury (see ref. 9 for a comprehensive review of different methods of IR-injury in animals). However, the precise position of the clip and the analysis of different sections of intestine, as well as different methods of anesthesia varies between these studies, making it difficult to reproduce (see Table 1). An additional complication of IR injury of jejunum is high mortality since position of the vascular clip close to the root of SMA affects blood supply to broad area of intestine. Therefore, in the current study we developed a protocol to induce consistent IR injury of terminal ileum, which is easy to reproduce. To induce reproducible IR injury of ileum, the proper position of vascular clips is critical. This is achieved by occluding the peripheral and collateral branches of the superior mesenteric artery.The degree of IR injury can be assessed by evaluation of hematoxylin and eosin sections using original Chiu/Park or modified score systems 11,18,34,41,42. Additionally, evaluation of tissue damage can be performed using terminal deoxynucleotidyl transferase biotin-dUTP nick end-labeling (TUNEL) staining of fragmented DNA, or active caspase-3 immunohistochemical staining, analysis of neutrophils by measuring myeloperoxidase activity or immunohistochemical evaluation of neutrophils using Gr-1, or Ly6G antibody staining 7,11. Inflammatory cytokines and chemokines, such as IL-1b, TNF, IL-6, CXCL1, CXCL2, CCL2 can be evaluated by real-time PCR 2,4,8. An example of the analysis of inflammatory cytokine expression is shown on Figure 4.
It is important to note that despite the high reproducibility and accessibility of IR injury of the ileum, this model may not reflect all clinical signs of human disease, in particularly chronic disease conditions and conditions with partial occlusion of the superior mesenteric artery 9. There are also differences in villus microvasculature between mice and humans, as well as levels of xanthine oxidase, a key enzyme mediating production of reactive oxygen species during IR injury 9,43. Therefore, models using large animals, such as pigs are being developed 9,44. Careful selection of the animal model depending on the human condition being studied is critical. In summary, we describe an easy and robust model of intestinal IR injury which can be utilized to study the cellular and molecular mechanism of epithelial injury and regeneration.
Disclosures
The authors declare no conflict of interest
Acknowledgments
This work was supported by Russian Science Foundation, grant no. 14-50-00060 and LLC RUSCHEMBIO. This work was also supported by the Crohn`s and Colitis Foundation of America grant 294083 (to A.V.T.), and by NIH grant RO1 DK47700 (to C.J.).
References
- Eltzschig HK, Eckle T. Ischemia and reperfusion--from mechanism to translation. Nat Med. 2011;17:1391–1401. doi: 10.1038/nm.2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenaerts K, et al. New insights in intestinal ischemia-reperfusion injury: implications for intestinal transplantation. Curr Opin Organ Transplant. 2013;18:298–303. doi: 10.1097/MOT.0b013e32835ef1eb. [DOI] [PubMed] [Google Scholar]
- Yasuhara H. Acute mesenteric ischemia: the challenge of gastroenterology. Surg Today. 2005;35:185–195. doi: 10.1007/s00595-004-2924-0. [DOI] [PubMed] [Google Scholar]
- Perez-Chanona E, Muhlbauer M, Jobin C. The microbiota protects against ischemia/reperfusion-induced intestinal injury through nucleotide-binding oligomerization domain-containing protein 2 (NOD2) signaling. Am J Pathol. 2014;184:2965–2975. doi: 10.1016/j.ajpath.2014.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H, et al. Delineating the relationships among the formation of reactive oxygen species, cell membrane instability and innate autoimmunity in intestinal reperfusion injury. Mol Immunol. 2014;58:151–159. doi: 10.1016/j.molimm.2013.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshiya K, et al. Depletion of gut commensal bacteria attenuates intestinal ischemia/reperfusion injury. Am J Physiol Gastrointest Liver Physiol. 2011;301:G1020–G1030. doi: 10.1152/ajpgi.00239.2011. [DOI] [PubMed] [Google Scholar]
- Wu MC, et al. The receptor for complement component C3a mediates protection from intestinal ischemia-reperfusion injuries by inhibiting neutrophil mobilization. Proc Natl Acad Sci U S A. 2013;110:9439–9444. doi: 10.1073/pnas.1218815110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muhlbauer M, Perez-Chanona E, Jobin C. Epithelial cell-specific MyD88 signaling mediates ischemia/reperfusion-induced intestinal injury independent of microbial status. Inflamm Bowel Dis. 2013;19:2857–2866. doi: 10.1097/01.MIB.0000435445.96933.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez LM, Moeser AJ, Blikslager AT. Animal models of ischemia-reperfusion-induced intestinal injury: progress and promise for translational research. Am J Physiol Gastrointest Liver Physiol. 2015;308:G63–G75. doi: 10.1152/ajpgi.00112.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Megison SM, Horton JW, Chao H, Walker PB. A new model for intestinal ischemia in the rat. J Surg Res. 1990;49:168–173. doi: 10.1016/0022-4804(90)90257-3. [DOI] [PubMed] [Google Scholar]
- Goldsmith JR, et al. Intestinal epithelial cell-derived mu-opioid signaling protects against ischemia reperfusion injury through PI3K signaling. Am J Pathol. 2013;182:776–785. doi: 10.1016/j.ajpath.2012.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuzzocrea S, et al. Glycogen synthase kinase-3beta inhibition attenuates the development of ischaemia/reperfusion injury of the gut. Intensive Care Med. 2007;33:880–893. doi: 10.1007/s00134-007-0595-1. [DOI] [PubMed] [Google Scholar]
- Farber A, et al. A specific inhibitor of apoptosis decreases tissue injury after intestinal ischemia-reperfusion in mice. J Vasc Surg. 1999;30:752–760. doi: 10.1016/s0741-5214(99)70115-1. [DOI] [PubMed] [Google Scholar]
- Ben DF, et al. TLR4 mediates lung injury and inflammation in intestinal ischemia-reperfusion. J Surg Res. 2012;174:326–333. doi: 10.1016/j.jss.2010.12.005. [DOI] [PubMed] [Google Scholar]
- Watson MJ, et al. Intestinal ischemia/reperfusion injury triggers activation of innate toll-like receptor 4 and adaptive chemokine programs. Transplant Proc. 2008;40:3339–3341. doi: 10.1016/j.transproceed.2008.07.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watanabe T, et al. Activation of the MyD88 signaling pathway inhibits ischemia-reperfusion injury in the small intestine. Am J Physiol Gastrointest Liver Physiol. 2012;303:G324–G334. doi: 10.1152/ajpgi.00075.2012. [DOI] [PubMed] [Google Scholar]
- Murayama T, et al. JNK (c-Jun NH2 terminal kinase) and p38 during ischemia reperfusion injury in the small intestine. Transplantation. 2006;81:1325–1330. doi: 10.1097/01.tp.0000209167.48030.6b. [DOI] [PubMed] [Google Scholar]
- Park PO, Haglund U, Bulkley GB, Falt K. The sequence of development of intestinal tissue injury after strangulation ischemia and reperfusion. Surgery. 1990;107:574–580. [PubMed] [Google Scholar]
- Jilling T, Lu J, Jackson M, Caplan MS. Intestinal epithelial apoptosis initiates gross bowel necrosis in an experimental rat model of neonatal necrotizing enterocolitis. Pediatr Res. 2004;55:622–629. doi: 10.1203/01.PDR.0000113463.70435.74. [DOI] [PubMed] [Google Scholar]
- Aprahamian CJ, Lorenz RG, Harmon CM, Dimmit RA. Toll-like receptor 2 is protective of ischemia-reperfusion-mediated small-bowel injury in a murine model. Pediatr Crit Care Med. 2008;9:105–109. doi: 10.1097/01.PCC.0000288717.44702.C0. [DOI] [PubMed] [Google Scholar]
- Tatum PM, Harmon CM, Lorenz RG, Dimmitt RA. Toll-like receptor 4 is protective against neonatal murine ischemia-reperfusion intestinal injury. J Pediatr Surg. 2010;45:1246–1255. doi: 10.1016/j.jpedsurg.2010.02.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleming SD, et al. Anti-phospholipid antibodies restore mesenteric ischemia/reperfusion-induced injury in complement receptor 2/complement receptor 1-deficient mice. J. Immunol. 2004;173:7055–7061. doi: 10.4049/jimmunol.173.11.7055. [DOI] [PubMed] [Google Scholar]
- Fleming SD, et al. Mice deficient in complement receptors 1 and 2 lack a tissue injury-inducing subset of the natural antibody repertoire. J. Immunol. 2002;169:2126–2133. doi: 10.4049/jimmunol.169.4.2126. [DOI] [PubMed] [Google Scholar]
- Lapchak PH, et al. Platelets orchestrate remote tissue damage after mesenteric ischemia-reperfusion. Am J Physiol Gastrointest Liver Physiol. 2012;302:G888–G897. doi: 10.1152/ajpgi.00499.2011. [DOI] [PubMed] [Google Scholar]
- Rehrig S, et al. Complement inhibitor, complement receptor 1-related gene/protein y-Ig attenuates intestinal damage after the onset of mesenteric ischemia/reperfusion injury in mice. J. Immunol. 2001;167:5921–5927. doi: 10.4049/jimmunol.167.10.5921. [DOI] [PubMed] [Google Scholar]
- Hoffman SM, Wang H, Pope MR, Fleming SD. Helicobacter infection alters MyD88 and Trif signalling in response to intestinal ischaemia-reperfusion. Exp Physiol. 2011;96:104–113. doi: 10.1113/expphysiol.2010.055426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moses T, Wagner L, Fleming SD. TLR4-mediated Cox-2 expression increases intestinal ischemia/reperfusion-induced damage. J Leukoc Biol. 2009;86:971–980. doi: 10.1189/jlb.0708396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinman R, et al. HIF-1 mediates pathogenic inflammatory responses to intestinal ischemia-reperfusion injury. Am J Physiol Gastrointest Liver Physiol. 2010;299:G833–G843. doi: 10.1152/ajpgi.00065.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lapchak PH, et al. The role of platelet factor 4 in local and remote tissue damage in a mouse model of mesenteric ischemia/reperfusion injury. PloS one. 2012;7:e39934. doi: 10.1371/journal.pone.0039934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen SH, et al. Ischemic postconditioning during reperfusion attenuates intestinal injury and mucosal cell apoptosis by inhibiting JAK/STAT signaling activation. Shock. 2012;38:411–419. doi: 10.1097/SHK.0b013e3182662266. [DOI] [PubMed] [Google Scholar]
- Wang F, et al. Temporal variations of the ileal microbiota in intestinal ischemia and reperfusion. Shock. 2013;39:96–103. doi: 10.1097/SHK.0b013e318279265f. [DOI] [PubMed] [Google Scholar]
- Zou L, Attuwaybi B, Kone BC. Effects of NF-kappa B inhibition on mesenteric ischemia-reperfusion injury. Am J Physiol Gastrointest Liver Physiol. 2003;284:G713–G721. doi: 10.1152/ajpgi.00431.2002. [DOI] [PubMed] [Google Scholar]
- Hassoun HT, et al. Alpha-melanocyte-stimulating hormone protects against mesenteric ischemia-reperfusion injury. Am J Physiol Gastrointest Liver Physiol. 2002;282:G1059–G1068. doi: 10.1152/ajpgi.00073.2001. [DOI] [PubMed] [Google Scholar]
- Stallion A, et al. Ischemia/reperfusion: a clinically relevant model of intestinal injury yielding systemic inflammation. J Pediatr Surg. 2005;40:470–477. doi: 10.1016/j.jpedsurg.2004.11.045. [DOI] [PubMed] [Google Scholar]
- Blikslager AT, Roberts MC, Rhoads JM, Argenzio RA. Is reperfusion injury an important cause of mucosal damage after porcine intestinal ischemia? Surgery. 1997;121:526–534. doi: 10.1016/s0039-6060(97)90107-0. [DOI] [PubMed] [Google Scholar]
- Barker N, et al. Identification of stem cells in small intestine and colon by marker gene Lgr5. Nature. 2007;449:1003–1007. doi: 10.1038/nature06196. [DOI] [PubMed] [Google Scholar]
- Victoni T, et al. Local and remote tissue injury upon intestinal ischemia and reperfusion depends on the TLR/MyD88 signaling pathway. Med Microbiol Immunol. 2010;199:35–42. doi: 10.1007/s00430-009-0134-5. [DOI] [PubMed] [Google Scholar]
- Watanabe T, et al. Toll-like receptor 2 mediates ischemia-reperfusion injury of the small intestine in adult mice. PloS one. 2014;9:e110441. doi: 10.1371/journal.pone.0110441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope MR, Fleming SD. TLR2 modulates antibodies required for intestinal ischemia/reperfusion-induced damage and inflammation. J. Immunol. 2015;194:1190–1198. doi: 10.4049/jimmunol.1303124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung FW, Su KC, Passaro E, Jr, Guth PH. Regional differences in gut blood flow and mucosal damage in response to ischemia and reperfusion. Am J Physiol. 1992;263:G301–G305. doi: 10.1152/ajpgi.1992.263.3.G301. [DOI] [PubMed] [Google Scholar]
- Chiu CJ, McArdle AH, Brown R, Scott HJ, Gurd FN. Intestinal mucosal lesion in low-flow states. I. A morphological, hemodynamic, and metabolic reappraisal. Arch Surg. 1970;101:478–483. doi: 10.1001/archsurg.1970.01340280030009. [DOI] [PubMed] [Google Scholar]
- Quaedackers JS, et al. An evaluation of methods for grading histologic injury following ischemia/reperfusion of the small bowel. Transplant Proc. 2000;32:1307–1310. doi: 10.1016/s0041-1345(00)01238-0. [DOI] [PubMed] [Google Scholar]
- Bianciardi P, Scorza R, Ghilardi G, Samaja M. Xanthine oxido-reductase activity in ischemic human and rat intestine. Free Radic Res. 2004;38:919–925. doi: 10.1080/10715760412331273430. [DOI] [PubMed] [Google Scholar]
- Yandza T, et al. The pig as a preclinical model for intestinal ischemia-reperfusion and transplantation studies. J Surg Res. 2012;178:807–819. doi: 10.1016/j.jss.2012.07.025. [DOI] [PubMed] [Google Scholar]


