Abstract
Purpose
Increased lenticular oxidative stress and altered calcium/magnesium (Ca/Mg) homeostasis underlie cataractogenesis. We developed a liposomal formulation of magnesium taurate (MgT) and studied its effects on Ca/Mg homeostasis and lenticular oxidative and nitrosative stress in galactose-fed rats.
Methods
The galactose-fed rats were topically treated with liposomal MgT (LMgT), liposomal taurine (LTau), or corresponding vehicles twice daily for 28 days with weekly anterior segment imaging. At the end of the experimental period, the lenses were removed and subjected to analysis for oxidative and nitrosative stress, Ca and Mg levels, ATP content, Ca2+-ATPase, Na+,K+-ATPase, and calpain II activities.
Results
The LTau and LMgT groups showed significantly lower opacity index values at all time points compared to the corresponding vehicle groups (p<0.001). However, the opacity index in the LMgT group was lower than that in the LTau group (p<0.05). Significantly reduced oxidative and nitrosative stress was observed in the LTau and LMgT groups. The lens Ca/Mg ratio in LMgT group was decreased by 1.15 times compared to that in the LVh group. Calpain II activity in the LMgT group was decreased by 13% compared to the LVh group. The ATP level and Na+,K+-ATPase and Ca2+-ATPase activities were significantly increased in the LMgT group compared to the LVh group (p<0.05).
Conclusions
Topical liposomal MgT delays cataractogenesis in galactose-fed rats by maintaining the lens mineral homeostasis and reducing lenticular oxidative and nitrosative stress.
Introduction
Cataract, the leading cause of blindness worldwide, remains an important public health issue, particularly for developing countries, due to the economic burden posed by surgical management. Several pharmacological strategies, particularly those that can restore the lens redox status, have been investigated. Our earlier study demonstrated that topical application of magnesium taurate (MgT) delays the onset and progression of cataract in galactose-fed rats [1]. We also observed that this anticataract effect of MgT is associated with reduced oxidative stress and a significant improvement in the lenticular calcium /magnesium (Ca2+/Mg2+) ratio. However, it remains to be determined whether this effect of MgT on the lens ionic balance helps to restore the lens ATP and ATPase functions. Improved Na+-K+-ATPase functions prevent cellular swelling while improved Ca2+-ATPase functions maintain a low cytoplasmic Ca2+ and thus prevent activation of the enzyme calpain that causes aggregation of soluble to insoluble lens proteins resulting in the development of cataract [2-4]. Furthermore, studies have shown that magnesium prevents nitrosative stress [2], and therefore, it is likely that MgT–induced inhibition of cataractogenesis involves reduction of nitrosative stress.
In our previous study, as we observed that treatment of isolated lenses with MgT provides higher correction in the Ca2+/Mg2+ ratio and the lens redox status [1], it is likely that the increase in ocular bioavailability could further enhance the MgT–induced delay in the onset and progression of cataract. Ocular bioavailability is often a concern due to anatomic and physiologic barriers on the ocular surface. The unique structure of the cornea consisting of epithelial cells and hydrophilic stroma restricts the transcorneal permeation of hydrophilic drugs. Furthermore, the tear film with its proteins and enzymes also acts as a barrier for transcorneal drug permeation. Although the cornea consists of several transporters to facilitate the movement of different molecules, such as amino acids, special drug delivery systems are useful for enhancing the intraocular bioavailability of various classes of drugs. Liposomes as the corpuscular carriers are one such delivery system that enhance the permeation of topically delivered drugs across the cornea [5,6].
In the current study, we developed a liposomal formulation of MgT and studied the anticataract efficacy of the topical application of MgT in comparison with the aqueous solution of MgT. Further, we investigated the effects of MgT on lens Ca/Mg homeostasis, lenticular oxidative and nitrosative stress, lens ATP content, ATPase functions, and calpain activity in galactose-fed rats.
Methods
Animals
All experiments and animal handling in this study were performed in accordance with the ARVO Statement for the Use of Animals in Research and approved by Institutional Animal Care and Use Committees (IACUC) of University Teknologi MARA, Malaysia (ACUC approval number – ACUC-6/12 on 30 October 2012). Sprague-Dawley rats of either sex weighing 80–100 g were procured from the Laboratory Animal Care Unit of Universiti Teknologi MARA. The animals were housed under standard laboratory conditions (23 ± 2 °C and a 12 h:12 h light-dark cycle) with food and water given ad libitum. All rats were subjected to ophthalmic examination, and those with any ophthalmic abnormalities were excluded from the study.
Study design
Study 1: Anticataract effect of liposomal MgT versus aqueous MgT
In study 1, the effect of the liposomal formulation of MgT was compared with that of aqueous MgT. The animals were divided into five groups of nine rats each. The grouping, diet, and treatment given were as follows: Group 1, normal diet (ND); Group 2, 25% galactose diet + empty liposomal vehicle topically (LVh); Group 3, 25% galactose diet + aqueous vehicle topically (AVh); Group 4, 25% galactose diet + liposomal MgT (LMgT); and Group 5, 25% galactose diet + aqueous 1% MgT (AMgT). All rats were treated topically, bilaterally, and twice daily with a 10 µl solution in a single drop. Diet and treatment were continued for a total of 28 days with weekly anterior segment imaging.
Study 2: MgT versus taurine
In study 2, we used the formulation (aqueous or liposomal) that showed higher anticataract efficacy based on the anterior segment imaging in study 1. The effect of the chosen formulation of MgT was compared with the same formulation of taurine. The animals’ grouping, diet, and treatment given were as follows: Group 1, normal diet (ND); Group 2, 25% galactose diet + vehicle (L/AVh); Group 3, 25% galactose diet + MgT (L/AMgT); and Group 4, 25% galactose diet + taurine (L/ATau).
As in study 1, all rats were treated topically, bilaterally, and twice daily with a 10 µl solution in a single drop. The diet and treatment were continued for a total of 28 days with weekly anterior segment imaging. At the end of the experimental period, all rats were euthanized using overdose of IP ketamine (250 mg/kg) and xylazine (50 mg/kg). The lenses were removed and subjected to analysis for reduced glutathione (GSH) and catalase (n = 6), superoxide dismutase (SOD; n = 6), and malondialdehyde (MDA; n = 6) using enzyme-linked immunosorbent assay (ELISA) kits (Cayman Chemicals, Ann Arbor, MI). Lens Ca and Mg levels (n = 5) were determined using Cobas Integra as described previously [1]. Lens ATP content (n = 6) was determined with the chemiluminescence method. The lenticular inducible nitric oxide synthase (iNOS) activity and the nitrotyrosine level (n = 6) were determined using ELISA kits. Lens Ca2+-ATPase (n = 6), Na+,K+-ATPase (n = 6), and calpain II activities (n = 6) were analyzed using colorimetric methods.
Preparation for topical formulations
Aqueous MgT
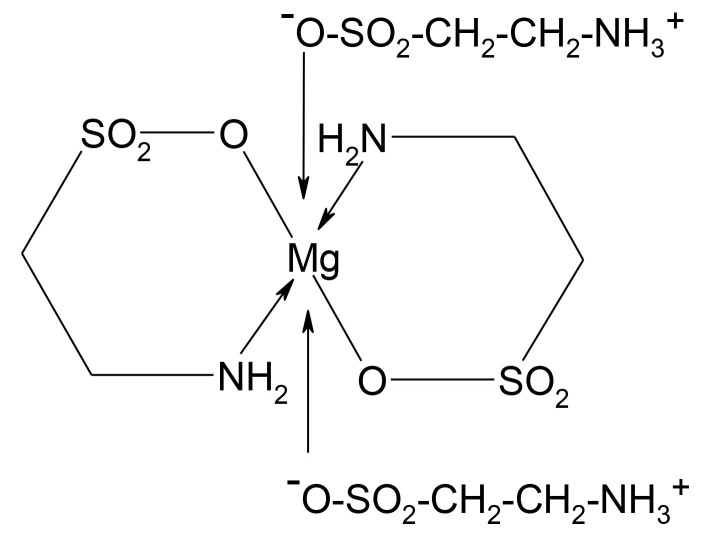
The taurine salt of magnesium (Figure 1) was synthesized based on McCarty’s method [7] and as described in our previous study [1]. The aqueous preparation of MgT was prepared by dissolving its appropriate quantity in 1% hydroxypropyl methylcellulose (HPMC) to obtain a 1% solution of MgT.
Figure 1.
Structural formula of MgT.
MgT and taurine loaded liposomes
MgT, taurine, or deionized water was incorporated into the liposomes by the dehydration–rehydration method [8,9]. A lipid mixture of phosphatidylcholine (PC) and cholesterol (8:1) was dissolved in chloroform:methanol (5:1) and dried to a thin film of lipids in a round bottom flask using a rotatory evaporator at 40 °C in a water bath for 2 h. The lipids were rehydrated by adding the MgT or taurine (1% in deionized water) or deionized water. This dispersion was frozen at −80 °C for 5 min followed by thawing in a water bath at 40 °C for 1 min. This freeze–thaw cycle was repeated five times. Then the solution was sonicated for 10 min (Sonic Dismembrator, Fisher Scientific, Loughborough, UK). Freeze–thaw and sonication were performed to obtain the small unilamellar vesicles from the multilamellar vesicles of liposomes. Then, the liposomes were extruded through two stacks each of 400, 200, and 100 nm pore size polycarbonate membranes (Avanti Polar Lipids, Inc., Alabaster, AL) using a handheld extruder. The extrusion through the handheld extruder was repeated ten times for each pore size.
Characterization of size and surface charge of liposomal dispersions
The size and the zeta (ζ) potential of the liposomes were determined using the Malvern Zetasizer Nano ZS (Malvern Instruments, Malvern, UK), operating with a helium-neon laser at a wavelength of 633 nm at a scattering detection angle of 175° at 25 °C. Results were the means of triplicate runs performed on different days using freshly prepared samples. In each run, three measurements were made. Standard deviations were determined from the replicate runs instead of the replicate measurements.
Anterior segment imaging and assessment of the progression of cataract
The anterior segment imaging was performed by two independent investigators using a Hawkeye Portable Slit-Lamp equipped with a digital camera, and tropicamide 1% was used as the mydriatic. Both investigators were blinded to the grouping and the treatment given. Lenticular changes were graded according to a modified version of Sippel’s method [10] for a more objective assessment. This method of grading for semiquantitative assessment of the progression of cataract has been standardized in our laboratory and has previously been described [1,11]: Stage 0 (Grade 1), lenses similar to healthy lenses; Stage 1a (Grade 2), lenses show a narrow equatorial band of vacuoles; Stage 1b (Grade 3), vacuoles cover one third or less of the periphery of the anterior cortex; Stage 1c (Grade 4), vacuoles cover more than one third of the periphery of the anterior cortex; Stage 2a (Grade 5), cortical opacity with some clear areas and vacuoles still present; Stage 2b (Grade 6), the cortex is largely opaque with some clear areas, but vacuoles are not present; Stage 3 (Grade 7), uniform opalescence; and Stage 4 (Grade 8), mature nuclear cataract.
The opacity index was calculated as described by Vats et al. [12]. Accordingly, all eyes were given a grade of 0–8 depending on the stage of cataract (0–4). The mean of the scores observed by the two independent investigators was considered the final score recorded by a blinded investigator:
Calcium and magnesium assay
Five lenses from each group were individually homogenized in 0.6 ml of deionized water and centrifuged at 890 ×g for 15 min. The supernatant was separated and was processed according to the Cobas Integra manufacturer’s protocol for Ca2+ and Mg2+ estimation in lens (COBAS Integra 400, Roche Diagnostics, Basel, CH) [13,14].
The protocol for Ca2+ estimation is based on the staining reaction of o-cresolphthalein complexone described by Schwarzenbach [13]. The Ca2+ reacts with o-cresolphthalein complexone (Roche Diagnostics) under alkaline conditions and forms a violet complex. The addition of 8-hydroxyquinoline (Roche Diagnostics) prevents interference with magnesium and iron. The color intensity of the complex formed is directly proportional to the calcium concentration and is determined by measuring the increase in absorbance at 552 nm.
Magnesium was measured with colorimetric assay using the method based on the staining reaction of Mg2+ and chlorophosphonazo III (CPZ III). CPZ III (Roche Diagnostics) binds to Mg2+ and causes an absorbance increase at 659 nm. Ethylenebis (oxyethylenenitrilo) tetraacetic acid (EGTA; Roche Diagnostics) is used to inhibit Ca2+ binding to CPZ III. Nonspecific absorbance interferences were reduced by the addition of EDTA (Roche Diagnostics) that removes Mg2+ from the Mg2+-CPZ III complex and allows for an accurate sample measurement. The difference in absorbance between the Mg2+-CPZ III complex and the EDTA-treated complex is the absorbance of Mg2+ alone [14].
Estimation of lens proteins
Six lenses from each group were individually homogenized in 0.5 ml of PBS (50 mM, pH 7.4, containing 1 mM EDTA). One hundred microliters of homogenate were used for the total protein estimation, and the remainder was centrifuged at 890 ×g for 15 min at 4 °C. Then 100 µl of the supernatant was used for soluble protein estimation. Quantification of the protein in the samples was performed using a colorimetric protein assay kit (Cayman Chemical , Ann Arbor, MI) based on the Bradford method. The reaction in this method utilizes a staining reaction upon binding of the dye Coomassie Brilliant Blue to the proteins in the sample. The absorbance was measured colorimetrically at 595 nm using a SpectraMax 190 microplate reader (Molecular Devices , Sunnyvale, CA).
Estimation of lenticular oxidative stress
The total GSH and MDA content and SOD and catalase activity in the lenses (n = 6) were estimated using commercially available ELISA kits (Cayman Chemical) and a Spectra Max 190 microplate reader (Molecular Devices). The lenses were rinsed with PBS (pH 7.4), and after the wet weight was recorded, the lenses were homogenized in cold 50 mM PBS with 1 mM EDTA, pH 7.0, for determination of catalase activity and GSH and in cold 20 mM HEPES buffer, pH 7.2, for the SOD assay. The mixtures were then centrifuged at 2970 ×g for 5 min at 4 °C, and the supernatants were removed and stored at −80 °C until used. For estimation of the lens MDA levels, the lenses were homogenized with radioimmunoprecipitation assay lysis (RIPA) buffer containing protease inhibitor in a ratio of 1 mg lens weight to 10 µl RIPA buffer. The samples were then centrifuged at 1,600 ×g at 4 °C for 10 min, and the supernatant was used for analysis.
GSH
GSH estimation in the supernatant was based on the enzymatic recycling method. Supernatant from lens homogenate (n = 6) was deproteinated by adding an equal volume of metaphosphoric acid reagent consisting of 5 g of metaphosphoric acid in 50 ml of water, and the mixture was centrifuged at 890 ×g for 2 min. GSH was estimated spectrophotometrically in the deproteinized homogenate.
SOD
The SOD activity assay used xanthine oxidase and hypoxanthine to generate superoxide radicals that were detected by tetrazolium salt, and absorbance was read at 440 nm. One unit of enzyme activity was defined as the amount of enzyme needed to exhibit 50% dismutation of the superoxide radical.
Catalase
Estimation of catalase activity was based on the reaction of methanol with the enzyme in the presence of an optimal concentration of hydrogen peroxide, and absorbance was read at 540 nm. One unit of CAT activity was defined as the amount of enzyme causing formation of 1 nmol of formaldehyde per minute.
MDA
For estimation of MDA, 100 µl of samples or standards were added to 100 µl of sodium dodecyl sulfate solution followed by 4 ml of color reagent consisting of thiobarbituric acid (TBA). Solutions were boiled for 1 h and incubated in an ice bath for 10 min to stop the reaction, and the solutions were centrifuged at 4 °C for 10 min. The MDA-TBA complex formed under high temperature (90–100 °C) and acidic conditions was measured colorimetrically at 540 nm. All estimations were performed in duplicate.
Estimation of lenticular nitrosative stress
Inducible nitric oxide synthase
For sample preparation, six lenses from each group were individually homogenized in 1 ml of 50 mM cold PBS, pH 7.4, containing 1 mM EDTA, and centrifuged at 890 ×g for 15 min. The iNOS level was determined using a commercially available ELISA kit (USCN Life Sciences Inc., Houston, TX) according to the manufacturer’s instructions. The microtiter plate had been precoated with an antibody specific to iNOS. Samples and standards were added to the appropriate microtiter plate wells with a biotin-conjugated antibody preparation specific to iNOS. Avidin conjugated to horseradish peroxidase (HRP) was added to each microplate well and incubated. After the 3,3′,5,5′-tetramethylbenzidine (TMB) substrate was added, only wells that contained iNOS, biotin-conjugated antibody, and enzyme-conjugated avidin exhibited a color change. The enzyme–substrates reaction was terminated by the addition of sulfuric acid solution, and the color change was measured spectrophotometrically at a wavelength of 450 nm using a Tecan Safire microplate reader (Tecan, Männedorf, CH). All estimations were performed in duplicate.
Nitrotyrosine
The lens 3-nitrotyrosine (3-NT) content was determined using an ELISA kit that utilizes polyclonal anti-3-NT antibody (Abcam, Cambridge, UK). Briefly, the lens homogenate (n = 6) was suspended to 25 mg/ml in PBS and was solubilized by adding four volumes of sample extraction buffer to a sample protein concentration of 5 mg/ml. The samples were incubated on ice for 20 min and centrifuged at 1,200 ×g at 4 °C for 20 min. The supernatants were used to quantify 3-NT, a product of tyrosine nitration resulting from oxidative damage to proteins by peroxynitrite. The provided microplates were coated with nitrotyrosine containing antigen. The ELISA was performed by adding the test sample mixed with the provided HRP-conjugated anti-3-NT antibody. All the anti-3NT detector antibody is available to bind to the immobilized 3-NT containing protein coating the wells if no 3-NT modified protein is present in the samples. In contrast, if soluble 3-NT modified protein is present in the sample, the protein will compete for binding with the anti-3NT detector antibody. The degree of competition is proportional to the concentration of soluble 3-NT modified proteins in the sample. Therefore, the signal in each well has an inverse relationship to the amount of 3-NT in each sample. The color change was detected at 450 nm using a Tecan Safire microplate reader. All estimations were performed in duplicate.
Estimation of ATP level
Five lenses from each group were individually homogenized in 1 ml of 70% ethanol (v/v) containing 2 mM EDTA (pH 10.9). Then, the homogenate was centrifuged at 890 ×g for 15 min at 4 °C to get the supernatant. Subsequently, the supernatant were diluted ten times with 0.1 M Tris-HCL/2 mM EDTA buffer (pH 7.8). The ATP content was measured using the ATPlite™ Bioluminescence Assay Kit from Perkin Elmer (Waltham, MA) and the 96-well Victor X5 microplate reader (Perkin Elmer) against an ATP calibration curve.
Determination of Na+/K+-ATPase and Ca2+-ATPase activities
Tissue preparation was based on a modified version of Zarros et al.’s method [15]. Five lenses from each group were individually homogenized in 600 µl ice-cold (0–4 °C) medium containing 50 mM Tris-HCl, pH 7.4, and 300 mM sucrose using sonicator, followed by centrifugation at 4 °C for 5 min. The protein content was determined with 100 µl of supernatant as previously described. The remainder of the supernatant was used to estimate Na+/K+-ATPase and Ca2+-ATPase activity.
Na+/K+-ATPase
The enzymatic activity was measured based on Chun-Fa Huang et al.’s [16] and Zarros et al.’s [15] methods. Briefly, 30 µl of assay buffer (118 mM NaCl, 1.67 mM KCl, 1.2 mM MgCl2, 12.3 mM NaHCO3, 11 mM glucose, 0.5 mM EGTA, pH 7.4) was added to the lens homogenate equivalent to 2 µg lens protein in each well. The assay was started with the addition of 10 µl of ATP (5 mM) making the final reaction volume of 100 µl and was performed in the presence or absence of 10 mM ouabain (Na+ K+ ATPase-specific inhibitor). The reaction was terminated after incubation at 37 °C for 20 min by the addition of 200 µl of 0.75% ammonium molybdate in 0.9 M sulfuric acid solution. The inorganic phosphate (Pi) released from the substrate ATP was colorimetrically assayed with a Tecan Safire microplate reader at 390 nm at 37 °C. The absorbance values were converted to activity values with linear regression using a standard curve of sodium monobasic phosphate from 20 µM to 0 µM that was included in the assay procedure. The specific ATPase activities were expressed as the micromoles of inorganic phosphate (Pi µmol) released per milligram of protein per hour. The Na+/K+-ATPase activity was determined by subtracting the ouabain (1.25 mM) insensitive Mg2+-ATPase activity from the overall Na+/K+/Mg2+-ATPase activity.
Ca2+-ATPase
The Ca2+-ATPase assay were performed based on a modified version of Nagai et al.’s method [17]. Briefly, 125 µl of standard solution (200 mM KCl, 100 mM HEPES, 10 mM MgCl2, 2 mM EGTA, 2 mM ATP) with or without 250 µl of 2.2 mM CaCl2 was added to each sample (125 µl), and the samples were incubated for 1 h in a 37 °C water bath. The enzymatic reaction was stopped by adding 2.5 ml of 10% trichloroacetic acid (TCA), and the tubes were centrifuged at 1190 ×g for 10 min at 4 °C. One hundred microliters of supernatant and 200 µl of 0.75% ammonium molybdate dissolved in 0.9 M sulfuric acid were added to each well. The plate was incubated at 37 °C for 10 min and then was subjected to gentle orbital movement for 1 min before the absorbance of the supernatant was measured at 390 nm using a Tecan Safire microplate reader. A standard curve was plotted using sodium monobasic phosphate from 50 mM to blank. Ca2+-ATPase activity were calculated as the difference in inorganic phosphate liberation measured in the presence and absence of Ca2+.
Calpain activity
Calpain activity was determined using the SensoLyte® 7-amino-4-methylcoumarin (AMC) Calpain Assay Kit (Perkin Elmer). This kit contains a fluorogenic peptide substrate, Suc-LLVY-AMC, which generated the AMC fluorophore that emits bright blue fluorescence upon cleavage by calpain protease. The fluorescence was monitored at excitation and emission of 354 and 442 nm using a Tecan Safire microplate reader. The standard curve was plotted using the AMC fluorescence reference standard.
Statistical analysis
All values were expressed as mean ± standard deviation (SD). Statistical comparison was conducted using two-way ANOVA with Bonferroni’s test. A p value of less than 0.05 was considered statistically significant.
Results
Size and surface charge of liposomal dispersions
An adequate characterization of liposome preparations and formulations is necessary, to ensure that the liposomes encompass the required and expected properties for their specific application. The liposomes in our preparation had a homogenous size distribution with a mean size of 114.67±0.15 nm (n = 3). The liposomes had a positive surface charge with a mean value of 1.54±0.34 mV (n = 3).
Study 1: Effect of liposomal MgT versus aqueous MgT on the onset and progression of cataract
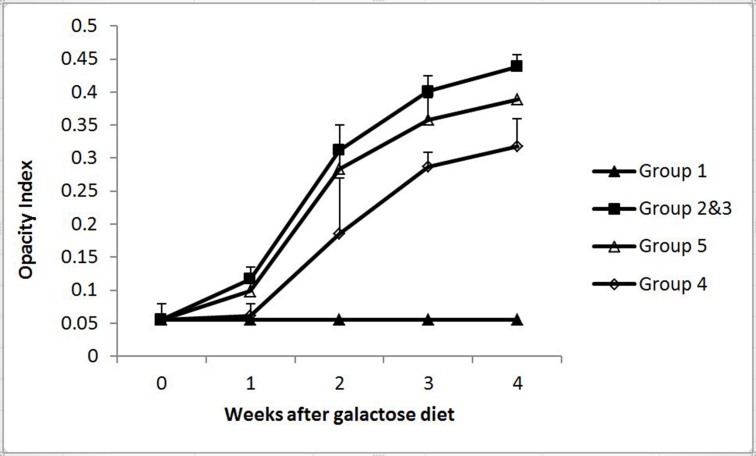
Although all lenses in Group 1 remained clear throughout the experimental period, there was a rapid increase in the opacity index in the Group 2 rats that received the galactose diet and vehicle treatment. The group treated with aqueous MgT showed a significantly lower opacity index at week 1 (p<0.05), week 2 (p<0.01), week 3 (p<0.0001), and week 4 (p<0.0001). The rats that received MgT in the liposomal formulation showed a significantly lower opacity index compared to those that received aqueous MgT at all four time points (p<0.0001) after starting the galactose diet, and at the end of week 1, the opacity index in the liposomal MgT group was comparable to that in the normal rats (p>0.05; Figure 2).
Figure 2.
Effect of aqueous and liposomal MgT on the onset and progression of cataract in galactose-fed rats. Group 1, normal rats; groups 2 and 3, aqueous and liposomal vehicle-treated groups; Group 4, liposomal MgT–treated group; and Group 5, aqueous magnesium-treated group. *p<0.0001 versus Group 5; **p<0.0001 versus Groups 2 and 3; ***p<0.01 versus Groups 2 and 3; #p<0.05 versus groups 2 and 3.
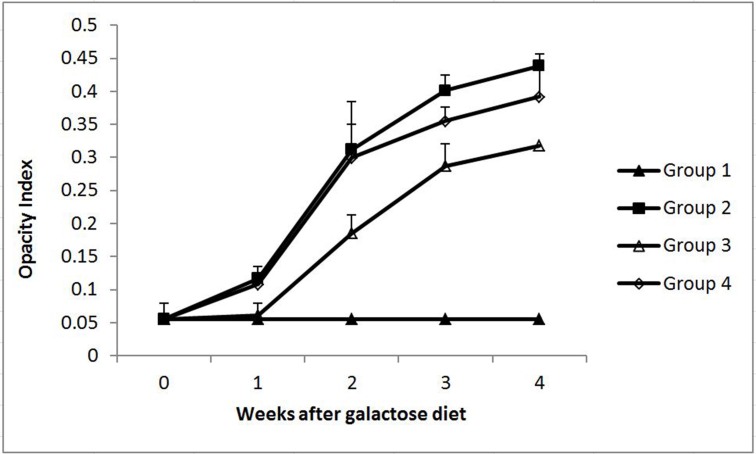
Study 2: Effect of liposomal MgT versus liposomal taurine on the onset and progression of cataract
As MgT in the liposomal formulation showed higher anticataract efficacy compared to the aqueous form, we selected the MgT-loaded liposomes for further study. We also included a group treated with liposomes loaded with only taurine to assess the effect of the taurine content of MgT.
Treatment with liposomal taurine prevented an increase in the opacity index as was observed in the vehicle-treated group (p<0.0001) at the end of week 3 and week 4 post-galactose diet. At the end of weeks 1 and 2, the opacity index in the taurine-treated group was comparable to that in the vehicle-treated group (p<0.05). When compared to the MgT-treated group, the taurine-treated group had a significantly higher opacity index at all time points (p<0.0001; Figure 3).
Figure 3.
Effect of liposomal MgT and taurine on the onset and progression of cataract in galactose-fed rats. Group 1, normal rats; Group 2, empty liposome-treated group; Group 3, liposomal MgT–treated group; and Group 4, liposomal taurine-treated group. *p<0.0001 versus Group 4; **p<0.0001 versus Group 2.
Effect of liposomal MgT versus liposomal taurine on the altered Ca2+-Mg2+ homeostasis
The lenticular Ca2+ to Mg2+ ratio was significantly higher in Group 2 compared to the normal group. However, Group 4 showed no significant difference from Group 2 and had a significantly higher Ca2+ to Mg2+ ratio compared to Group 1. Group 3 that received MgT showed a significantly lower Ca2+ to Mg2+ ratio compared to Group 2 and Group 4 (Table 1).
Table 1. Effect of the liposomal Mg taurate and taurine on lenticular calcium-to-magnesium ratio, ATP level and ATPases activity in the lenses of galactosemic rats.
| Group | Control diet |
Galactose diet + vehicle |
Galactose diet + Mg taurate |
Galactose diet + Taurine |
|---|---|---|---|---|
| (Group 1) | (Group 2) | (Group 3) | (Group 4) | |
| Lenticular Ca2+/Mg2+ |
0.57±0.17 |
3.66±0.38* |
2.37±0.81*,^ |
3.12±0.35*,$ |
| ATP level (µmol Pi/mg protein) |
34.4±2.2 |
11.23±3.7* |
20.0±5.1*,^ |
13.5±4.7* |
| Na+/K+-ATPase (µmol/g wet weight) |
7.86±3.87 |
2.16±1.23* |
6.74±3.73 |
2.47±1.06*,$ |
| Ca2+-ATPase activity (µmol Pi/mg protein) | 0.22±0.01 | 0.14±0.03* | 0.22±0.03^ | 0.16±0.01*,$ |
Footnote: All values are mean ± SD; *p<0.001 versus Group 1, ^p<0.05 versus Group 2, $p<0.05 versus Group 3; n=5
Effect of liposomal MgT on the lenticular ATP level
The lenticular ATP level was significantly reduced in all galactose-fed groups (groups 2, 3, and 4) compared to the normal group (Group 1). Interestingly, the lenticular ATP level was significantly increased in the MgT-treated group (Group 3) when compared to that of the vehicle-treated group (Group 2). The taurine-treated group (Group 4) showed a higher mean value compared to Group 2; however, the difference did not reach the significant level. Similarly, the MgT-treated group showed a relatively higher mean ATP level compared to the taurine-treated group, but the difference did not reach the significant level (Table 1).
Effect of liposomal MgT on lenticular ATPase activities
The lenticular Na+/K+-ATPase and Ca2+-ATPase activities in the galactose-fed vehicle-treated group (Group 2) were more than threefold lower compared to those of the normal group (Group 1), and the differences were significant. The increase in the Na+/K+-ATPase and Ca2+-ATPase activities in the MgT-treated group (Group 3) was found to be significantly increased compared to the galactose diet untreated group (Group 2). There was no significant difference in the Na+/K+-ATPase and Ca2+-ATPase activities between the MgT-treated group and the normal diet group. The Na+/K+-ATPase and Ca2+-ATPase activities in the taurine-treated group did not show significant differences from the vehicle-treated group (Group 2); moreover, the same activities in the taurine-treated group were significantly lower than in the MgT-treated group (Table 1).
Effect of liposomal MgT and taurine on lenticular oxidative and nitrosative stress
Effect of liposomal MgT and taurine on lenticular oxidative stress
The GSH content in Group 2 showed a 10.05-fold reduction compared to the normal group. Although groups 3 and 4 also showed significantly lower lens GSH content compared to the normal group, when compared to Group 2, the content was 1.67- and 1.46-fold higher, respectively. Additionally, in the MgT–treated group, the mean GSH value was significantly higher than that of the vehicle-treated group. Lenticular catalase activity was 1.44-fold lower in Group 2 compared to that in the normal group. However, the same level was restored to normal in Group 3 that received MgT. The taurine treatment group showed a significantly higher mean value compared to Group 2 but was significantly lower compared to the group that received MgT. Lens SOD showed upregulation of the enzyme activity possibly to counteract oxidative stress with a 1.59-fold higher value in Group 2. The mean SOD values in groups 3 and 4 showed no significant difference compared to that of Group 1 but were significantly lower compared to that of Group 2. The lens MDA levels were significantly higher in Group 2 compared to those of Group 1. Groups that received treatment with either MgT or taurine showed significantly lower mean MDA values compared to those of Group 2 (Table 2).
Table 2. Effect of liposomal Mg taurate and taurine on oxidative and nitrosative stress in the lens of galactosemic rats.
| Group | Control diet |
Galactose diet + vehicle |
Galactose diet + Mg taurate |
Galactose diet + Taurine |
|---|---|---|---|---|
| (Group 1) | (Group 2) | (Group 3) | (Group 4) | |
| GSH (umol/g lens weight) |
4.38±0.56 |
0.44±0.09* |
0.73±0.18*,# |
0.64±0.20* |
| Catalase (umol/g lens protein) |
54.85±8.84 |
37.96±8.72** |
53.75±9.56# |
49.61±8.04^,$ |
| SOD (Units/mg lens protein) |
6.65±1.45 |
10.55±0.68* |
7.37±2.73^ |
8.22±1.81^ |
| MDA (umol/g lens weight) |
62.72±4.75 |
92.57±9.31* |
59.05±6.62@ |
57.42±14.36@ |
| iNOS (ng/mg lens protein) |
109.76±5.58 |
196.58±13.19+ |
96.13±4.66^ |
115.38±5.45^ |
| Nitrotyrosine (ng/mg lens weight) | 29.80±4.01 | 58.35±3.13+ | 26.84±4.34^ | 26.36±5.94^ |
All values are mean ± SD; *p<0.001 versus Group 1, **p<0.01 versus Group 1, +p<0.05 versus Group 1, @p<0.001 versus Group 2, #p<0.01 versus Group 2, ^p<0.05 versus Group 2, $p<0.01 versus Group 3
Effect of liposomal MgT and taurine on nitrosative stress
Group 2 also showed a significantly high level of iNOS activity and nitrotyrosine levels compared to those of the normal group. Both treatment groups showed significantly lower iNOS activity and nitrotyrosine levels compared to those of Group 2, and there was no difference for both parameters between the normal group and the two treatment groups (Table 2).
Effect of liposomal MgT and taurine on lenticular calpain activity and protein level
The calpain activity in all galactose-treated groups was significantly higher than that of the normal group; however, the MgT–treated group showed significantly lower calpain activity compared to that of the vehicle-treated group (Group 2). In accordance with the increased calpain activity, Group 2 also showed a significant decrease in the soluble protein contents of lens compared to that of the normal group. Treatment with either MgT or taurine improved the soluble protein level, but only Group 3 showed significantly higher values compared to those of Group 2. Both treatment groups showed no significant differences compared to the normal group. The insoluble protein fraction was highest in Group 2 compared to all other groups. In the MgT–treated group, the ratio of soluble to insoluble proteins was comparable to that of the normal group (Table 3).
Table 3. Effect of liposomal Mg taurate and taurine on calpain activity and protein level in galactosemic rats.
| Parameter | Control diet |
Galactose diet + vehicle |
Galactose diet + Mg taurate |
Galactose diet + Taurine |
|---|---|---|---|---|
| (Group 1) | (Group 2) | (Group 3) | (Group 4) | |
| Calpain activity (µmol/mg wet weight) |
0.42±0.03 |
0.61±0.06+ |
0.53±0.02+,^ |
0.56±0.02+ |
| Total protein (mg/g lens weight) |
475.93±51.94 |
462.20±77.88 |
474.24±37.59 |
473.68±76.43 |
| Soluble protein (mg/g lens weight) |
383.44±45.71 |
303.82±18.84** |
389.72±12.00@ |
339.39±61.68 |
| % Soluble protein |
0.8057 |
0.6573 |
0.7814 |
0.7165 |
| % Insoluble protein |
0.1943 |
0.3427 |
0.2186 |
0.2835 |
| Ratio of soluble to insoluble protein | 4.15 | 1.92 | 3.57 | 2.53 |
All values are mean ± SD; **p<0.01 versus Group 1, +p<0.05 versus Group 1, @p<0.001 versus Group 2, ^p<0.05 versus Group 2
Discussion
An adequate characterization of liposome preparations and formulations is necessary, to ensure that liposomes encompass the required and expected properties for their specific application [5,6,18]. In the present study, the mean particle size for liposomal formulation was 116.3 nm and 115.2 nm for the MgT and taurine liposomes, respectively. The zeta potential was +2.64 mV and +2.60 mV for the MgT and taurine liposomes, respectively, which resulted in a favorable binding effect of the positively charged liposomes to the corneal surface [18-20]. Schaeffer and Krohn [21] have shown that positively charged liposomes increase corneal drug delivery fourfold. Additionally, liposomes ranging in size from 100 to 400 nm have been shown to provide greater drug delivery compared to smaller or larger liposomes [22].
In the present study, we evaluated the anticataract effect of MgT in a liposomal formulation using a galactose-induced rat model. This model is not an exact representation of diabetic cataract; however, the key pathophysiological changes in the lens, such as activation of aldose reductase, polyol accumulation, and oxidative and nitrosative stress, mimic the same in diabetic cataract [23-26]. Moreover, galactose feeding results in rapid and predictable cataractous changes with lesser mortality due to less severe systemic metabolic changes.
The current study demonstrated that the delay in the progression of cataract was more pronounced in the group treated with a liposomal formulation compared to the aqueous form indicating higher ocular bioavailability of MgT in the liposomal formulation. As taurine has been shown to reduce lenticular oxidative stress and protein glycation in the presence of high glucose levels, it is important to investigate whether the addition of magnesium to taurine provides greater benefits than taurine alone. This study demonstrated that the liposomal formulation of MgT delays cataractogenesis more than taurine alone in the liposomal formulation thus supporting the role of magnesium in delaying cataractogenesis. Our findings are in accordance with previous studies that showed the role of MgT in delaying the development of cataract [1].
Cataractogenesis is a multifactorial disease involving various pathogenetic mechanisms that have not been completely clarified. A large body of evidence has demonstrated that oxidative stress is an important contributor to the development of cataract [27-31]. Glutathione in its reduced form (GSH) is an important part of lens antioxidant defenses as GSH prevents the protein-thiol mixed disulfide formation that has been implicated as a possible mechanism for the protein–protein aggregation in cataractogenesis [32,33]. In addition, glutathione functions as an electron donor for glutathione peroxidase that reduces hydrogen peroxide (H2O2) to water and contributes to reactive oxygen species (ROS) degradation [33,34]. In the present study, treatment with MgT significantly increased the lenticular GSH levels compared to the vehicle-treated group. Previous studies have also shown that Mg2+ pretreatment restores renal and testicular GSH levels in the tissue of mice that were exposed to cadmium intoxication [35]. SOD and catalase are two other important enzymes that remove oxygen free radicals and reduce lenticular oxidative stress. We observed that in rats treated with vehicle, lenticular SOD activity was significantly higher, whereas catalase activity was lower indicating the upregulation of antioxidant defenses. However, in the MgT and taurine treatment groups, the SOD and catalase activities were comparable to those of the control group. These results indicate the efficacy of MgT and taurine in restoring a normal lens redox status. In contrast to our findings, Matkovics et al. [36] demonstrated that treatment with magnesium chloride results in a significant increase (10–50%) in SOD, catalase, and GSH activities in Drosophila melanogaster, which may perhaps be attributed to a compensatory tissue reaction to counteract oxidative stress. Magnesium deficiency is also associated with increased lipid peroxidation due to the increased susceptibility of body organs to free radical injury [37-39]. Israa et al. [40] revealed the presence of a high MDA level in response to hyperglycemia-induced oxidative stress. In accordance with these observations, higher levels of lipid peroxidation and hypomagnesaemia have been reported in patients with type 2 diabetes [41]. Free radicals in diabetes mellitus (DM) cause the peroxidative breakdown of phospholipids that leads to accumulation of MDA [42]. Ribeiro et al. [43] demonstrated a negative correlation between magnesium and glucose levels, as well as between magnesium and oxidative stress. In the current study, the MDA concentration in the vehicle-treated group was significantly higher than that in the other groups, indicating increased lipid peroxidation induced by galactosemia. Treatment with MgT prevented lipid peroxidation as indicated by a decrease in the MDA level in the lens.
Galactosemia also induces mRNA expression of iNOS followed by a high level of NO production. Reaction of NO with superoxide anions produces peroxynitrite (ONOO-), which is a highly oxidative species and is capable of nitrating tyrosine residues of crystalline proteins, leading to the formation of nitrotyrosine [32,44-46]. Nitrosative stress due to increased endogenous NO production can potentiate lens opacification [47,48]. Magnesium deficiency has been shown to enhance the production of NO by iNOS induction in the lens. Production of excess NO leads to the decreased ATP level that causes lens ionic imbalance by impairing the ATPase functions [49]. In the current study, treatment with MgT caused a significant decrease in iNOS and nitrotyrosine indicating a significant reduction in lenticular nitrosative stress.
In this study, treatment with taurine also caused reduced oxidative stress and nitrosative stress and consequently delayed cataractogenesis. Taurine is involved in several physiologic reactions, such as osmoregulation, calcium transport regulation, and cell membrane stabilization, and protects tissues against oxidative damage by scavenging hypochlorous acid (HOCl) [50,51]. Taurine has previously been shown to significantly preserve the level of GSH in galactosemic animals [52]. The levels of taurine and GSH have been shown to be significantly reduced in the diabetic cataractous lens [53]. Mahmoud et al. [54] demonstrated that the administration of taurine to galactose-fed rats attenuates the increased lipid peroxidation, enhances the levels of antioxidants, inhibits the activity of the aldose reductase enzyme, and improves the crystallin profile. The MDA content of lenses incubated with galactose plus taurine in media supplemented with glucose was found to be lower than that of the control lenses incubated without taurine [55]. Dietary taurine supplementation also ameliorates MDA levels, GSSG/GSH, and NAD+/NADH but failed to prevent the osmotically mediated depletion of GSH and the decrease in glucose utilization and ATP levels in the diabetic precataractous lens [56]. In accordance with these findings, we observed that the effects of MgT were more prominent than those of taurine alone. Thus, the addition of magnesium to taurine seems to play a significant role in preventing lenticular oxidative stress.
Oxidative stress–induced lipid peroxidative damage of lenticular membranes leads to inactivation of membrane proteins such as Ca2+-ATPase. Inhibition of the function of Ca2+-ATPase results in the loss of calcium homeostasis and calcium accumulation in the lens. As a consequence of calcium influx in rodent lenses, calpains, a family of well-characterized calcium-dependent proteases, are activated. Calpain activation induces rapid proteolysis of water-soluble proteins, that is, lens crystallins, and cytoskeletal proteins. Proteolysis exposes the hydrophobic regions of the lens proteins, which then interact to form insoluble aggregates [57]. Insolubilization results in precipitation and aggregation of fragmented proteins and, finally, loss of lens transparency [58].
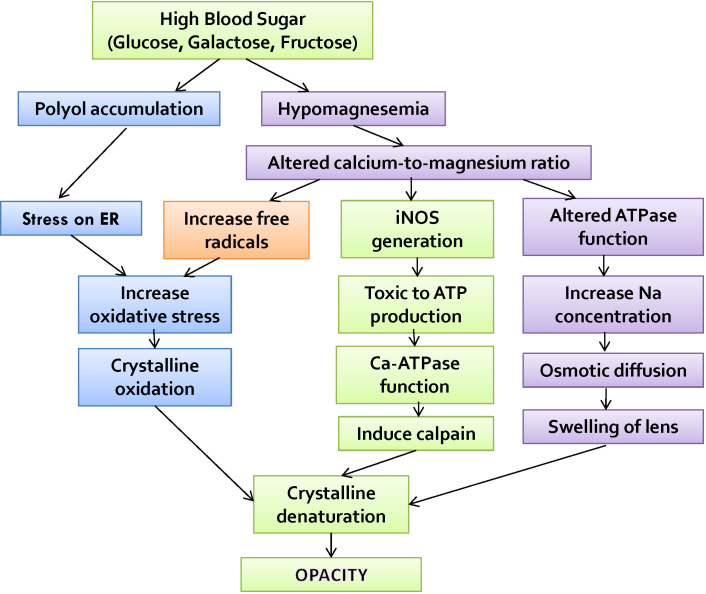
Importantly, the present study showed restoration of the Ca/Mg ratio particularly in the MgT treatment group. Magnesium is a cofactor for several enzymes such as Na+/K+ ATPase and Ca2+-ATPase in the lens that maintain the lenticular ionic balance [59,60] (Figure 4). Both pumps are magnesium dependent, and magnesium deficiency can impair ATPase functions [61,62]. Furthermore, magnesium deficiency enhances oxidative stress leading to damage to ATPases [38]. Lenticular ionic imbalance leads to increased oxidative stress [3] as is shown in the vehicle-treated group in the present study. Na+/K+-ATPase dysfunction leads to cellular swelling by osmotic stress, and interruption of the Ca2+-ATPase function leads to increased intracellular calcium ions and that causes activation of calpain II and consequently proteolysis of crystalline, the major protein in the lens. Proteolysis converts crystalline into an insoluble form that causes the development of cataract [58,63-65]. In the current study, we observed normalization of the soluble/insoluble protein ratio in both treatment groups, particularly the MgT group, indicating less activation of Ca-dependent calpain. Correction of the ionic imbalance and reduction in lenticular oxidative stress appear to contribute to reduced calpain activation and, therefore, normalization of the soluble/insoluble protein ratio. Reduced oxidative stress by itself also prevents the formation of protein aggregates by protecting against the oxidation of sulfhydryl groups on proteins [66]. In the present study, treatment with MgT caused restoration of the Ca/Mg ratio thus preventing oxidative stress, preserving the ATPase functions, and delaying the development of cataract. Similar effects in the taurine treatment group, however, were less pronounced due to decreased correction of the ionic imbalance. In conclusion, topical liposomal MgT delays the onset and progression of galactose-induced cataract in rats by maintaining mineral homeostasis in the lens and reducing lenticular oxidative and nitrosative stress in galactose-fed rats.
Figure 4.
Pathogenesis of sugar-induced cataract.
Acknowledgments
Funding statement: This work was supported in part by the DANA Kecemerlangan Penyelidikan under the project 600-RMI/ST/DANA 5/3/Dst (354/2011) in part by the MOH (Malaysia) under the project 600-RMI/RAGS 5/3 (103/2013). Contributor: All authors have substantially contributed to conception, designing, drafting the article and in final approval of the manuscript version to be submitted. All authors have jointly decided to designate Assoc Prof Dr Renu Agarwal to be responsible for taking decision regarding the presence of authors and the order of their presence in the manuscript. Assoc Prof Dr Renu Agarwal has also been selected by all authors to be responsible for all future communication with the journal regarding this manuscript.
References
- 1.Agarwal R, Iezhitsa I, Awaludin NA, Ahmad Fisol NF, Bakar NS, Agarwal P, Abdul Rahman TH, Spasov A, Ozerov A, Mohamed Ahmed Salama MS, Mohd Ismail N. Effects of magnesium taurate on the onset and progression of galactose-induced experimental cataract: in vivo and in vitro evaluation. Exp Eye Res. 2013;110:35–43. doi: 10.1016/j.exer.2013.02.011. [DOI] [PubMed] [Google Scholar]
- 2.Agarwal R, Iezhitsa L, Agarwal P. Pathogenetic role of magnesium deficiency in ophthalmic diseases. Biometals. 2013;27:5–18. doi: 10.1007/s10534-013-9684-5. [DOI] [PubMed] [Google Scholar]
- 3.Agarwal R, Iezhitsa IN, Agarwal P, Spasov AA. Mechanisms of cataractogenesis in the presence of magnesium deficiency. Magnes Res. 2013;26:2–8. doi: 10.1684/mrh.2013.0336. [DOI] [PubMed] [Google Scholar]
- 4.Agarwal R, Iezhitsa I, Agarwal P, Spasov A. Magnesium deficiency: does it have a role to play in cataractogenesis? Exp Eye Res. 2012;101:82–9. doi: 10.1016/j.exer.2012.05.008. [DOI] [PubMed] [Google Scholar]
- 5.Agarwal R, Iezhitsa I, Agarwal P, Abdul Nasir NA, Razali N, Alyautdin R, Ismail NM.Liposomes in topical ophthalmic drug delivery: an update. Drug Deliv 2016. 41–17. [DOI] [PubMed] [Google Scholar]
- 6.Aliautdin RN, Iezhitsa IN, Agarval R. Transcorneal drug delivery: prospects for the use of liposomes. Vestn Oftalmol. 2014;130:117–22. [PubMed] [Google Scholar]
- 7.McCarty MF. Magnesium taurate and other mineral taurates. [US Pat. 5582839]. Inventors: McCarty; Mark F. (San Diego, CA). Assignee: Nutrition 21 (San Diego, CA). Appl. No.: 08/423,891, Filed: April 18, 1995. patentimages.storage.googleapis.com/pdfs/US5582839.pdf.
- 8.Perrie Y, Frederik PM, Gregoriadis G. Liposome-mediated DNA vaccination: the effect of vesicle composition. Vaccine. 2001;19:3301–10. [Google Scholar]
- 9.Shi N, Pardridge WM. Noninvasive gene targeting to the brain. Proc Natl Acad Sci USA. 2000;97:7567–72. doi: 10.1073/pnas.130187497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sippel TO. Changes in the water, protein, and glutathione contents of the lens in the course of galactose cataract development in rats. Invest Ophthalmol. 1966;5:568–75. [PubMed] [Google Scholar]
- 11.Abdul Nasir NA, Agarwal R, Vasudevan S, Tripathy M, Alyautdin R, Ismail NM. Effects of topically applied tocotrienol on cataractogenesis and lens redox status in galactosemic rats. Mol Vis. 2014;20:822–35. [PMC free article] [PubMed] [Google Scholar]
- 12.Vats V, Yadav SP, Biswas NR, Grover JK. Anti-cataract activity of Pterocarpus marsupium bark and Trigonella foenum-graecum seeds extract in alloxan diabetic rats. J Ethnopharmacol. 2004;93:289–94. doi: 10.1016/j.jep.2004.03.032. [DOI] [PubMed] [Google Scholar]
- 13.Schwarzenbach G. The complexones and their analytical application. Analyst (Lond) 1955;80:713–29. [Google Scholar]
- 14.Ferguson JW, Richard JJ, O’Laughlin JW, Banks CV. Simultaneous spectrophotometric determination of calcium and magnesium with chlorophosphonazo III. Anal Chem. 1964;36:796–9. [Google Scholar]
- 15.Zarros A, Theocharis S, Skandali N, Tsakiris S. Effects of fulminant hepatic encephalopathy on the adult rat brain antioxidant status and the activities of acetylcholinesterase, (Na+,K+)- and Mg2+-ATPase: comparison of the enzymes’ response to in vitro treatment with ammonia. Metab Brain Dis. 2008;23:255–64. doi: 10.1007/s11011-008-9091-8. [DOI] [PubMed] [Google Scholar]
- 16.Huang C-F. C.-J. H., Shing-Hwa Liu, Shoei-Yn Lin-Shiau. Exposure to Low Dose of Cinnabar (a Naturally Occurring Mercuric Sulfide (HgS)) Caused Neurotoxicological Effects in Offspring Mice. J Biomed Biotechnol. 2012;2012:254582. doi: 10.1155/2012/254582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nagai N. I Y, Takeuchi N. Correlation between Hyper-Sensitivity to Hydrogen Peroxide and Low Defense against Ca2+ Influx in Cataractogenic Lens of Ihara cataract Rats. Biol Pharm Bull. 2011;34:1005–10. doi: 10.1248/bpb.34.1005. [DOI] [PubMed] [Google Scholar]
- 18.Franzen U, Østergaard J. Physico-chemical characterization of liposomes and drug substance-liposome interactions in pharmaceutics using capillary electrophoresis and electrokinetic chromatography. J Chromatogr A. 2012;1267:32–44. doi: 10.1016/j.chroma.2012.07.018. [DOI] [PubMed] [Google Scholar]
- 19.Honda M, Asai T, Oku N, Araki Y, Tanaka M, Ebihara N. Liposomes and nanotechnology in drug development: focus on ocular targets. Int J Nanomedicine. 2013;8:495–503. doi: 10.2147/IJN.S30725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Szkudelski T. The Mechanism of Alloxan and Streptozotocin Action in B Cells of the Rat Pancreas. Physiol Res. 2001;50:536–46. [PubMed] [Google Scholar]
- 21.Schaeffer HE, Krohn DL. Liposomes in topical drug delivery. Invest Ophthalmol Vis Sci. 1982;22:220–7. [PubMed] [Google Scholar]
- 22.Nagayasu A, Uchiyama K, Kiwada H. The size of liposomes: a factor which affects their targeting efficiency to tumors and therapeutic activity of liposomal antitumor drugs. Adv Drug Deliv Rev. 1999;40:75–87. doi: 10.1016/s0169-409x(99)00041-1. [DOI] [PubMed] [Google Scholar]
- 23.Ohta Y, Yamasaki T, Niwa T, Goto H, Majima Y, Ishigruo I. Cataract development in 12-month-old rats fed a 25% galactose diet and its relation to osmotic stress and oxidative damage. Ophthalmic Res. 1999;31:321–31. doi: 10.1159/000055554. [DOI] [PubMed] [Google Scholar]
- 24.Lee AY, Chung SS. Contributions of polyol pathway to oxidative stress in diabetic cataract. FASEB J. 1999;13:23–30. doi: 10.1096/fasebj.13.1.23. [DOI] [PubMed] [Google Scholar]
- 25.Bron AJ, Sparrow J, Brown NAP, Harding JJ, Blakytny R. The lens in diabetes. Eye (Lond) 1993;7:260–75. doi: 10.1038/eye.1993.60. [DOI] [PubMed] [Google Scholar]
- 26.Monnier VM, Stevens VJ, Cerami A. Nonenzymatic glycosylation, sulfhydryl oxidation, and aggregation of lens proteins in experimental sugar cataracts. J Exp Med. 1979;150:1098–107. doi: 10.1084/jem.150.5.1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Taylor A, Jacques PF, Epstein EM. Relations among aging antioxidant status and cataract. Am J Clin Nutr. 1995;62:1439S–47S. doi: 10.1093/ajcn/62.6.1439S. [DOI] [PubMed] [Google Scholar]
- 28.Spector A. Oxidative stress-induced cataract: mechanism of action. FASEB J. 1995;9:1173–82. [PubMed] [Google Scholar]
- 29.Lou MF. Redox regulation in the lens. Prog Retin Eye Res. 2003;22:657–82. doi: 10.1016/s1350-9462(03)00050-8. [DOI] [PubMed] [Google Scholar]
- 30.Berthoud VM, Beyer EC. Oxidative stress, lens gap junctions, and cataracts. Antioxid Redox Signal. 2009;11:339–53. doi: 10.1089/ars.2008.2119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Michael R, Bron AJ. The ageing lens and cataract: a model of normal and pathological ageing. Philos Trans R Soc Lond B Biol Sci. 2011;366:1278–92. doi: 10.1098/rstb.2010.0300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lou MF, Dickerson JE., Jr Protein-thiol mixed disulfides in human lens. Exp Eye Res. 1992;55:889–96. doi: 10.1016/0014-4835(92)90015-k. [DOI] [PubMed] [Google Scholar]
- 33.Ho MC, Peng YJ, Chen SJ, Chiou SH. Senile cataracts and oxidative stress. J Clin Gerontol Geriatr. 2010;1:17–21. [Google Scholar]
- 34.Meister A, Anderson ME. Glutathione. Annu Rev Biochem. 1983;52:711–60. doi: 10.1146/annurev.bi.52.070183.003431. [DOI] [PubMed] [Google Scholar]
- 35.Djukić-Ćosić D, Ninković M, Maličević Z, Matović V, Soldatović D. Effect of magnesium pretreatment on reduced glutathione levels in tissues of mice exposed to acute and subacute cadmium intoxication: a time course study. Magnes Res. 2007;20:177–86. [PubMed] [Google Scholar]
- 36.Matkovics B, Kiss I, Kiss SA. The activation by magnesium treatment of anti-oxidants eliminating the oxygen free radicals in Drosophila melanogaster in vivo. Magnes Res. 1997;10:33–8. [PubMed] [Google Scholar]
- 37.Chaudhary DP, Boparai RK, Bansal DD. Implications of oxidative stress in high sucrose low magnesium diet fed rats. Eur J Nutr. 2007;46:383–90. doi: 10.1007/s00394-007-0677-4. [DOI] [PubMed] [Google Scholar]
- 38.Hans CP, Chaudhary DP, Bansal DD. Magnesium deficiency increases oxidative stress in rats. Indian J Exp Biol. 2002;40:1275–9. [PubMed] [Google Scholar]
- 39.Spasov AA, Zheltova AA, Kharitonov MV. Magnesium and the oxidative stress. Ross Fiziol Zh Im I M Sechenova. 2012;98:915–23. [PubMed] [Google Scholar]
- 40.Israa FJA, Huda Arif J. Role of antioxidant on nephropathy in alloxan induced diabetes in rabbits. Iraqi Postgrad Med J. 2009;8:398–402. [Google Scholar]
- 41.Niranjan G, Mohanavalli V, Srinivasan AR, Ramesh R. Serum lipid peroxides and magnesium levels following three months of treatment with pioglitazone in patients with Type 2 Diabetes mellitus. Diabetes Metab Syndr. 2013;7:35–7. doi: 10.1016/j.dsx.2013.02.020. [DOI] [PubMed] [Google Scholar]
- 42.Bhutia Y, Ghosh A, Sherpa ML, Pal R, Mohanta PK. Serum malondialdehyde level: Surrogate stress marker in the Sikkimese diabetics. J Nat Sci Biol Med. 2011;2:107–12. doi: 10.4103/0976-9668.82309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ribeiro MC, Avila DS, Barbosa NB, Meinerz DF, Waczuk EP, Hassan W, Rocha JB. Hydrochlorothiazide and high-fat diets reduce plasma magnesium levels and increase hepatic oxidative stress in rats. Magnes Res. 2013;26:32–40. doi: 10.1684/mrh.2013.0334. [DOI] [PubMed] [Google Scholar]
- 44.Varma SD, Hegde KR. Susceptibility of the ocular lens to nitric oxide: Implications in cataractogenesis. J Ocul Pharmacol Ther. 2007;23:188–95. doi: 10.1089/jop.2006.0124. [DOI] [PubMed] [Google Scholar]
- 45.Ito Y, Nabekura T, Takeda M, Nakao M, Terao M, Hori R, Tomohiro M. Nitric oxide participates in cataract development in selenite treated rats. Curr Eye Res. 2001;22:215–20. doi: 10.1076/ceyr.22.3.215.5516. [DOI] [PubMed] [Google Scholar]
- 46.Pollreisz A, Schmidt-Erfurth U. Diabetic cataract-pathogenesis, epidemiology and treatment. J Ophthalmol. 2010;2010:608751. doi: 10.1155/2010/608751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Inomata M, Hayashi M, Shumiya S, Kawashima S, Ito Y. Involvement of inducible nitric oxide synthase in cataract formation in Shumiya cataract rat (SCR). Curr Eye Res. 2001;23:307–11. doi: 10.1076/ceyr.23.4.307.5455. [DOI] [PubMed] [Google Scholar]
- 48.Gupta SK, Selvan VK, Agrawal SS, Saxena R. Advances in pharmacological strategies for the prevention of cataract development. Indian J Ophthalmol. 2009;57:175–83. doi: 10.4103/0301-4738.49390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nagai N, Fukuhata T, Ito Y. Effect of magnesium deficiency on intracellular ATP levels in human lens epithelial cells. Biol Pharm Bull. 2007;30:6–10. doi: 10.1248/bpb.30.6. [DOI] [PubMed] [Google Scholar]
- 50.Aruoma O, Halliwell B, Hoey B, Butler J. The antioxidant action of taurine, hypotaurine and their metabolic precursors. Biochem J. 1988;256:251–5. doi: 10.1042/bj2560251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Devamanoharan P, Ali A, Varma S. Oxidative stress to rat lens in vitro: protection by taurine. Free Radic Res. 1998;29:189–95. doi: 10.1080/10715769800300221. [DOI] [PubMed] [Google Scholar]
- 52.Son HY, Kim HH, Kwon Y. Taurine prevents oxidative damage of high glucose-induced cataractogenesis in isolated rat lenses. J Nutr Sci Vitaminol (Tokyo) 2007;53:324–30. doi: 10.3177/jnsv.53.324. [DOI] [PubMed] [Google Scholar]
- 53.Kilic F, Bhardwaj R, Caulfeild J, Trevithick JR. Modelling cortical cataractogenesis 22: Is in vitro reduction of damage in model diabetic rat cataract by taurine due to its antioxidant activity? Exp Eye Res. 1999;69:291–300. doi: 10.1006/exer.1999.0697. [DOI] [PubMed] [Google Scholar]
- 54.Mahmoud AM, El Gaffar Mahmoud AE, Aziz MA. Taurine as anticataractogenic agent in galactose-feeding rats. Egypt J Biochem Mol Biol. 2006;24:99–110. [Google Scholar]
- 55.Malone JI, Benford SA, Malone J. Taurine prevents galactose-induced cataracts. J Diabetes Complications. 1993;7:44–8. doi: 10.1016/1056-8727(93)90023-r. [DOI] [PubMed] [Google Scholar]
- 56.Obrosova IG, Stevens MJ. Effect of dietary taurine supplementation on GSH and NAD(P)-redox status, lipid peroxidation, and energy metabolism in diabetic precataractous lens. Invest Ophthalmol Vis Sci. 1999;40:680–8. [PubMed] [Google Scholar]
- 57.Shearer TR, David LL, Anderson RS, Azuma M. Review of selenite cataract. Curr Eye Res. 1992;11:357–69. doi: 10.3109/02713689209001789. [DOI] [PubMed] [Google Scholar]
- 58.Shearer TR, Ma H, Fukiage C, Azuma M. Selenite nuclear cataract: review of the model. Mol Vis. 1997;3:8. [PubMed] [Google Scholar]
- 59.Pasternak K, Kocot J, Horecka A. Biochemistry of magnesium. J. Elementol. 2010;15:601–16. [Google Scholar]
- 60.Iezhitsa IN, Spasov AA. Potassium magnesium homeostasis: physiology, pathophysiology, clinical consequences of deficiency and pharmacological correction. Usp Fiziol Nauk. 2008;39:23–41. [PubMed] [Google Scholar]
- 61.Mak IT, Komarov AM, Wagner TL, Stafford RE, Dickens BF, Weglicki WB. Enhanced NO production during Mg deficiency and its role in mediating red blood cell glutathione loss. Am J Physiol. 1996;271:C385–90. doi: 10.1152/ajpcell.1996.271.1.C385. [DOI] [PubMed] [Google Scholar]
- 62.Hans CP, Chaudhary DP, Bansal DD. Magnesium deficiency increases oxidative stress in rats. Indian J Exp Biol. 2002;40:1275–9. [PubMed] [Google Scholar]
- 63.Biswas S, Harris F, Singh J, Phoenix D. Role of calpains in diabetes mellitus-induced cataractogenesis: a mini review. Mol Cell Biochem. 2004;261:151–9. doi: 10.1023/b:mcbi.0000028750.78760.6f. [DOI] [PubMed] [Google Scholar]
- 64.Dilsiz N, Olcucu A, Atas M. Determination of calcium, sodium, potassium and magnesium concentrations in human senile cataractous lenses. Cell Biochem Funct. 2000;18:259–62. doi: 10.1002/1099-0844(200012)18:4<259::AID-CBF881>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 65.Nabekura T, Tomohiro M, Ito Y, Kitagawa S. Changes in plasma membrane Ca 2+-ATPase expression and ATP content in lenses of hereditary cataract UPL rats. Toxicology. 2004;197:177–83. doi: 10.1016/j.tox.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 66.Berthoud VM, Beyer EC. Oxidative stress, lens gap junctions, and cataracts. Antioxid Redox Signal. 2009;11:339–53. doi: 10.1089/ars.2008.2119. [DOI] [PMC free article] [PubMed] [Google Scholar]