Abstract
Obsessive-compulsive disorder (OCD) has primarily pediatric onset and well-documented unique impacts on family functioning. Limited research has assessed the understanding that parents of children with OCD have of the etiology of the condition, and there are no data regarding potential applications of genetic counseling for this population. We recruited 13 parents of 13 children diagnosed with OCD from the OCD Registry at British Columbia Children’s Hospital, and conducted qualitative semi-structured telephone interviews to explore participants’ experiences with their child’s OCD, causal attributions of OCD, and perceptions of two genetic counseling vignettes. Interviews were audio-recorded, transcribed, and analyzed using elements of grounded theory qualitative methodology. Analysis revealed key components and contextual elements of the process through which parents adapt to their child’s OCD. This adaptation process involved conceptualizing the meaning of OCD, navigating its impact on family dynamics, and developing effective illness management strategies. Adaptation took place against a backdrop of stigmatization and was shaped by participants’ family history of mental illness and their child’s specific manifestations of OCD. Parents perceived genetic counseling, as described in the vignettes, as being empowering, alleviating guilt and blame, and positively impacting treatment orientation. These data provide insight into the process of parental adaptation to pediatric OCD, and suggest that genetic counseling services for families affected by OCD may help facilitate adaptation to this illness.
Keywords: obsessive-compulsive disorder, pediatric, parents, adaptation, psychiatric genetic counseling, qualitative
Introduction
Obsessive-compulsive disorder (OCD) is characterized by recurrent and persistent obsessions and/or compulsions that are time-consuming or cause significant distress or impairment of functioning for affected individuals(American Psychiatric Association, 2000). OCD affects 1% to 3% of the pediatric population(Karno, Golding, Sorenson, & Burnam, 1988; Ruscio, Stein, Chiu, & Kessler, 2010), and poses a considerable emotional burden to relatives and caregivers of patients(Grover & Dutt, 2011; Ramos-Cerqueira, Torres, Torresan, Negreiros, & Vitorino, 2008; Steketee, 1997; Stengler-Wenzke, Trosbach, Dietrich, & Angermeyer, 2004a), resulting in a markedly decreased subjective quality of life in these relatives (Grover & Dutt, 2011; Stengler-Wenzke, Kroll, Matschinger, & Angermeyer, 2006). OCD has well-documented and unique impacts on family functioning, primarily related to parental accommodation of symptoms. Accommodation represents a counter-therapeutic process that involves parents enabling children’s avoidance of triggers and assisting in their rituals(Albert et al., 2010; Lebowitz, Panza, Su, & Bloch, 2012). Individuals with OCD and their relatives experience significant stigmatization associated with the disorder, and fear of this stigma often results in concealment of the illness and delayed help-seeking(Hansson, Jormfeldt, Svedberg, & Svensson, 2013; Simonds & Thorpe, 2003; Stengler-Wenzke, Trosbach, Dietrich, & Angermeyer, 2004b).
Like other psychiatric disorders, such as schizophrenia or bipolar disorder, OCD is etiologically heterogeneous, involving contributions of both genetic and environmental factors(Geller & March, 2012; Koran & Blair Simpson, 2013; Pauls, 2008; Stewart & Pauls, 2010). Heritability estimates for childhood onset OCD range from 45% to 65%(van Grootheest, Cath, Beekman, & Boomsma, 2005). However, despite advances in psychiatric genetics, there has been little work to develop interventions to bring this knowledge to people with OCD and their families. Without education regarding the etiology of illness, patients and families tend to develop their own theories based on their experiences (Skirton & Eiser, 2003). These theories are often fraught with misconceptions, and may invoke feelings of shame or guilt that are counterproductive to help-seeking behaviors(Phelan, Yang, & Cruz-Rojas, 2006) and psychological adaptation(Skirton & Eiser, 2003). However, offering genetic counseling and education about the etiology of mental illness to patients and families can help decrease self-blame; alleviate perceived stigma, anxiety, and guilt associated with the disorder; and increase feelings of hope, control, and ability to cope (J. C. Austin & Honer, 2008; Meiser, Mitchell, McGirr, Van Herten, & Schofield, 2005).
The American Psychiatric Association practice guideline for the treatment of patients with OCD recognizes the utility of genetic counseling in facilitating adaptation to the disorder (Koran & Blair Simpson, 2013). However, while several studies have been performed with the goal of informing genetic counseling for psychiatric disorders, (DeLisi & Bertisch, 2006; Holzinger, Kilian, Lindenbach, Petscheleit, & Angermeyer, 2003; Lyus, 2007; Peay, Hooker, Kassem, & Biesecker, 2009; Quaid, Aschen, Smiley, & Nurnberger, 2001; Schulz et al., 1982) some of which have examined etiological understanding of illness, (Holzinger et al., 2003; Peay et al., 2009) no such studies have been conducted among families affected by OCD. As caregivers, parents of children with mental illness have a unique involvement with the management of the condition, which may contribute to guilt, stigma, and in the case of OCD, involvement in accommodation of the child’s symptoms.
A more comprehensive understanding of how parents of children with OCD experience and perceive the causes of this disorder will facilitate an appreciation of these families’ educational and counseling needs, which is important in laying the foundation for genetic counseling for this population. Since patients and their families tend to incorporate information provided in a genetic counseling session into their pre-existing worldviews, an improved understanding of these prior beliefs allows for more effective counseling. Furthermore, an understanding of parental experience with their child’s OCD can help identify the ways in which genetic counseling may be useful to this unique population. Our study aimed to explore parents’ experiences with and causal attributions for their children’s OCD, and their perceptions of genetic counseling in this context.
Methods
Design
When exploring new topics, a qualitative research approach yields rich data that can be used to inform clinical practice (McAllister, 2001; Semaka, Balneaves, & Hayden, 2013). We explored parents’ experiences with their children’s diagnosis of OCD using a qualitative study design and analyzed data from interviews using elements of grounded theory, including open and axial coding and constant comparison. Grounded theory is a qualitative methodology well suited for exploring social processes, such as adaptation to illness (Corbin & Strauss, 1998). It allows study findings to be rooted in participants’ words and experiences and highlights what is most important to them. Institutional Review Board approval was received from the UBC Children’s and Women’s Research Ethics Board, the Hospital for Sick Children Research Ethics Board, and the University of Toronto Office of Research Ethics.
Participants
Study participants were recruited from the OCD Registry of the BC Children’s Hospital OCD Clinic and Translational Research Program, via a mailed letter of invitation. Thirty-four letters of invitation were mailed in January 2013, and interviews were scheduled between January and March 2013, after written consent was received. Eligible participants were English-speaking adult (≥19 years old) parents of children (≤18 years old) who had been clinically diagnosed with OCD.
Procedures
Semi-structured interviews of 45 to 90 minutes in length were conducted with study participants over the telephone, then audiotaped and transcribed verbatim. Interviews consisted of open-ended, semi-structured questions exploring participants’ experiences with their child’s OCD and causal attributions of OCD (see supplemental information for interview guide). There was also a structured section of the interview that used fictional clinical vignettes followed by open-ended questions to elicit parent perceptions of two different potential consultations with a genetic counselor. Participant demographics were ascertained via a questionnaire. All interviews were conducted by a genetic counseling graduate student (HA) who had no prior relationship with the participants.
Data analysis
The first stage of analysis utilized open coding, which involved a line-by-line analysis of the interview transcripts, where specific ideas or events were given conceptual labels or codes. Open coding proceeded with an emphasis on emergence to ensure that the codes were grounded in the data. After coding a portion of the transcripts, codes were condensed and collapsed into major concepts. A preliminary coding scheme was developed and used in the second stage of analysis. In this stage, axial coding was used to modify and verify the major concepts and establish their properties and dimensions. Relationships between the major categories were also explored. The constant comparison method, whereby data are continuously compared and contrasted within and between transcripts (Charmaz, 2006), was utilized throughout the two coding stages. Discrepant cases and/or newly emerging codes that did not fit into the preliminary coding scheme were noted and used to revise the scheme. All transcripts were coded by HA; a subset were also coded by AS. Any discrepancies in coding were discussed and resolved. Throughout the analysis, written memos were used to capture impressions of the data and to record emerging associations between concepts. Data saturation of major concepts was established (i.e. the collection of new data did not yield new information about these concepts) and a conceptual framework was developed. This framework represents major concepts and their properties and dimensions, and begins to explore relationships amongst the major concepts and their impact on the process of parental adaptation to OCD.
Results
Study participants
A total of 13 parents of children with OCD were interviewed, including 12 mothers and 1 father. Their demographic characteristics are outlined in Table 1. Of note, 2 of the 13 participants reported having previously received genetic counseling related to OCD.
Table 1.
Demographic characteristics of study participants
| Characteristics | n (%) |
|---|---|
| Sex | |
| Female | 12 (92) |
| Male | 1 (8) |
| Age (years) | mean 45 (range 30–52) |
| Race | |
| White | 11 (85) |
| Multiracial | 2 (15) |
| Marital status | |
| Married | 11 (85) |
| Common-law | 1 (8) |
| Single | 1 (8) |
| Education | |
| High school graduate | 3 (23) |
| College/university graduate | 8 (62) |
| Master’s graduate | 2 (15) |
| Sex of affected child | |
| Female | 6 (46) |
| Male | 7 (54) |
| Current age of affected child (years) | mean 14 (range 10–18) |
Overview of the parental adaptation process
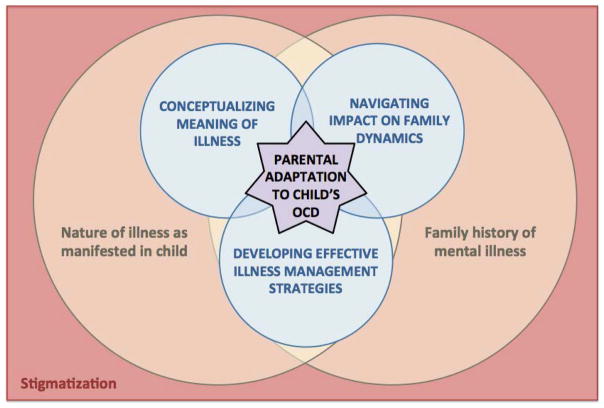
Though interview questions were aimed at exploring parental experience with, and causal attributions for, pediatric OCD, the exploratory nature of this study allowed for the emergence of a broader picture of how parents of children with OCD describe their process of adaptation to the condition. From the data, we constructed a conceptual framework, which represents adaptation as a process that develops over a complex course and involves six key concepts, as shown in Figure 1. Specifically, parents’ narratives suggest that there are three important processes involved in parental adaptation: conceptualizing the meaning of OCD, including forming causal attributions, navigating OCD’s impact on family dynamics, and developing effective illness management strategies. These processes are underpinned and influenced by the contextual elements of the nature of OCD as manifested by the child and family history of mental illness. Every aspect of the process of successful adaptation seems to be inhibited by the broader context of stigma related to OCD. Below we describe the major concepts represented by this framework, illustrated by representative quotations from participants.
Figure 1.
Conceptual framework of the process of parental adaptation to a child’s obsessive-compulsive disorder (OCD).
Processes of parental adaptation
1) Conceptualizing the meaning of OCD
Participants described four main ways in which they strived to conceptualize the meaning of OCD: externalizing, normalizing, distinguishing from other phenomena, and forming causal attributions.
i) Externalizing
Parents described the process of coming to view OCD as an entity that was separate from, and not the fault of, their child. Many initially felt embarrassed and frustrated and blamed and disciplined their child for OCD-related behaviors. However, these perceptions changed as they began to conceptualize OCD as something external to their child that was not the child’s choosing:
“Just realizing that the things [my daughter]’s been doing, she’s not doing them just to be difficult… it makes me… a lot more tolerant and patient and knowledgeable.”
ii) Normalizing
Many participants sought to openly acknowledge OCD, conceptualizing it as a common illness that did not define their child and could be associated with positive attributes. Parents also related OCD to other, non-stigmatized experiences:
“It’s something she’s [going to] have to manage, and one of her sisters might have to manage something different, like a back problem, or a knee injury… But I feel like… there’s a certain kind of awareness and empathy there, that she’s acquired because she has these issues.”
iii) Distinguishing from other phenomena
Participants described their attempts to determine which of their children’s features and behaviors were attributable to OCD, and which were related to their personality, the effects of puberty, and/or a “normal” level of worrying or organization:
“She’s a tween… so sometimes we don’t know, is [her behavior] because of the OCD, is that hormonal, is that developmental? She’s at such a tricky part of life, it’s hard to know.”
iv) Forming causal attributions
Parents described their attempts to understand the etiology of OCD by consulting a variety of sources:
“[My understanding of the causes of OCD] comes obviously from my experience with [my son], but also trying to read up on what is out there in terms of literature on potential causes of OCD, and then trying to piece things together based on what we know of what’s gone on with him.”
Causal attributions were informed by interpretations of family history, the child’s experience of, and reactions to, traumatic events, etiological understanding of other conditions, conversations with other parents, self-directed research using books and the Internet, and “fragmented” information from healthcare providers.
Parents’ etiological explanations for OCD varied: some were purely biological (e.g. hormones, genes, viruses), some purely environmental (e.g. traumatic events, stressful experiences, academic pressures), and some multifactorial (e.g. “the perfect storm” of biological factors and environmental triggers). Parents frequently contradicted themselves while explaining their causal attributions – for example, firmly asserting that OCD is entirely genetic only to later describe environmental influences, or describing OCD as inevitable but wondering whether it could have been prevented. Many appeared to doubt and question their own theories and attributions even as they were articulating them.
2) Navigating OCD’s impact on family dynamics
The impact of OCD on family dynamics manifested in three major areas, as parents reported experiencing an emotional toll, adjusting as a couple, and altering parenting and decision-making due to their child’s illness.
i) Experiencing an emotional toll
Parents described how their child’s struggle with OCD left them feeling powerless, hopeless, desperate, and not knowing how to cope. Many expressed some form of worry about their child’s future due to their illness. Parents were also concerned about the risks for other family members to develop OCD, with some becoming hyper-vigilant for emerging signs of OCD in their other child and/or family members:
“You just kind of watch [for signs of illness], probably a little closer than other parents would. They wouldn’t think of it, whereas [for a parent of a child with OCD], it runs through your mind and you go, hmm, is that a [symptom] or a no?”
A particularly pervasive element of the emotional toll on parents was guilt. A common experience was an initial reaction of self-blame (e.g. for having passed on a genetic predisposition to OCD, or “done something wrong” in their parenting) following the diagnosis of OCD:
“For me there’s a little bit of guilt. Like I think, ‘oh, if I didn’t have depression and anxiety then maybe he wouldn’t’… maybe even the way I raised him… and sometimes I think ‘well, did that [cause it]?’”
Many parents’ narratives expressed guilt and regret about making excuses for their child’s behaviors, not recognizing OCD symptoms, not being aggressive enough in seeking treatment, and having used ineffective symptom management strategies:
“When a child suffers from anything, especially like this – hearing the pain in your child’s voice always triggers guilt for me. So I will start to question everything – I should have pushed harder sooner…. I could have done something more and this could have been treated earlier.”
ii) Adjusting as a couple
In some parent couples, one partner felt s/he was more understanding or better informed than the other. In other couples, one partner was seen as minimizing and downplaying the child’s OCD, thereby impeding the other’s adaptation process. Conflict often arose between parents about management strategies and parenting approaches; some described OCD and the conflict surrounding it as having had a substantial negative impact on their marriage:
“It’s been an issue with [my husband] and me, fighting about what to do and what not to do, like me wanting to find counselling and him not being willing to pay for or go to that… he’s got different ideas about how things are and he’s not been involved.”
Conversely, other participants described being “on the same page” as their partners, and highlighted the positive impact that the adaptation process had on their relationship:
“Going through it added a lot of stress. Now I think it’s… sort of solidified our thoughts that we’re good together, because we were able to do this, and help [our son].”
iii) Altering parenting and decision-making
OCD also impacted families’ parenting choices and decision-making in a wide variety of contexts. At one end of the spectrum were parents’ day-to-day decisions, such as with whom to socialize or whether to go on vacation, which were related to accommodating their child’s OCD (Albert et al., 2010; Lebowitz et al., 2012). More specifically, parents described changing their behavior to appease their child. However, while this accommodation was well-intentioned, it ultimately resulted in more strain on the whole family:
“He’ll hit the table. He’ll yell. He’ll say, “say it this way four times”… and there are certain letters he can’t handle... we’re not allowed to say ‘ice cream’, you’d say ‘ice ream.’ It’s [kind of] crazy when there’s all these little things we do to accommodate him being angry.”
At the other end of the spectrum of parental decisions impacted by OCD were major life choices, such as whether to relocate the family or have more children:
“I [am not] having any more kids! [My daughter]’s still a handful at almost 12 years old, so I know that she needs my undivided attention... I don’t want to say that [OCD] controls things I decide, but it’s always a factor when I make decisions like, should we move, or change schools.”
3) Developing effective illness management strategies
Parents described how the process of developing effective illness management strategies included navigating barriers to illness management, considering psychotropic medication, exploring psychotherapy, seeking peer support, and managing OCD at home. Illness management strategies were perceived to be effective if they decreased the child’s symptoms and distress, improved their day-to-day functioning, and improved family functioning and dynamics.
i) Navigating barriers
Parents described facing barriers to developing effective illness management strategies. Such barriers included their own delayed seeking of medical help as a result of not noticing their child’s compulsions, or not seeing the behaviors as indicators of OCD:
“[Our daughter] had behaviours that seemed a bit like a normal weird teenager. She spent a lot of time hiding out in her room. She would organize her bookshelves over and over… we just thought it was kind of quirky behavior, but that was all manifestations of [OCD].”
Some parents described not wanting to overreact to symptoms, or even ignoring and suppressing their own intuitions about the behaviors; this was, at times, compounded by other people (e.g. teachers or relatives) minimizing or downplaying the child’s symptoms:
“The teacher kept saying, oh you’re worrying too much, he’s fine, he’s fine, he’s fine. We kept saying no, there’s something; this is not the same child. And she kept putting us off, putting us off.”
Once parents did identify a problem and decided to seek help, they faced additional barriers getting their child correctly diagnosed in order to access appropriate services. Many parents noted a lack of awareness and understanding of OCD among primary health care practitioners and even some mental health professionals. Once their child had been diagnosed and deemed eligible for treatment, wait times for healthcare services and financial constraints limiting access to more expeditious private treatment options, proved to be major barriers. Many parents described how they had to become advocates for their child and push for access to treatment:
“It’s definitely been really stressful and trying… we’ve had to sort of advocate for our service and try and navigate the system and learn what is available and who can access [it]...”
ii) Considering psychotropic medication
Psychotropic medication was widely considered by parents as having the potential to either be effective and life changing, or to lead families down long fruitless roads that may cause more harm than good. Many viewed medication as the final hope when in a desperate situation:
“If it was at the point where [my child] just wasn’t functioning and life just wasn’t worth living, yeah absolutely [I would consider medications]. But I would exhaust every other avenue first.”
Among those who had tried medication for management of their child’s OCD, many described a deeply frustrating trial-and-error process to find the right medication. Even parents who had found effective medication for their children expressed concerns:
“This is all nice, but she’s on [medication]. Is this going to be forever? And… if she has to be on it forever, is it going to be effective forever? And if she ever wants to have kids or whatever is that something that she’s going to have to go off of?”
iii) Exploring psychotherapy
All participants had explored psychotherapeutic management of their child’s OCD in some form. Many felt that general anxiety management techniques were ineffective, and discussed the importance of being treated by a healthcare provider who was well-versed in OCD. Nearly all participants described cognitive behavioral therapy, particularly exposure plus response prevention, as challenging but immensely beneficial for their child. This is a widely endorsed treatment modality in which individuals with OCD are exposed to stimuli that trigger OCD symptoms and must resist the urge to perform compulsions in response (Bolton & Perrin, 2008; March, 1995).
iv) Seeking peer support
Some parents expressed the benefits of seeking peer support and being open about their child’s OCD with compassionate family and friends. Group therapy was also a normalizing experience for many:
“I think [what was helpful] was the ongoing learning, connecting with other parents, knowing that other parents, other people, are going through this [too].”
v) Managing OCD at home
Parents described at-home management strategies including exercise, stress minimization, an emphasis on positive messages, psychotherapy “homework” completed by the child, and approaches involving the entire family (e.g. replacing accommodation with challenging the child’s behavior):
“Now we expose him to it, so if something isn’t clean the way he thinks it is, he knows that the only way to get over it is to just dive in and expose himself to it… to actually go forward and do it anyways, as hard as it is.”
Contextual Elements of Parental Adaptation
A. Nature of OCD as manifested by the child
The three processes involved in parental adaptation to OCD are impacted by the nature of the child’s OCD. Parents described OCD as being debilitating for children to varying extents, as they struggled emotionally, socially, academically, and in day-to-day functioning. They described continual fluctuation between progress towards improved functioning, and relapse when triggers exacerbated symptoms. Symptoms also changed over time; as some subsided, others evolved:
“[My son] was struggling again with new obsessions. It was almost like he’d challenge say, twenty of them and then a hundred new ones popped up, so it felt like, this is obviously not under control.”
More visible symptoms (e.g. raw, bleeding hands from excessive hand-washing) alerted parents to a concern and facilitated help-seeking, but also left children vulnerable to bullying and stigmatization. When symptoms were less obvious (e.g. internal obsessions, more easily masked compulsions) parents noted that it took them longer to recognize that something was wrong and seek help; however, they perceived their children as being better able to cope socially, as peers were also less likely to notice the illness:
“I think [school]’s been okay [for my daughter], because most of her obsessions and compulsions are sort of internal and they’re subtle movements and such, so she presents really well. So [her classmates] can’t visually see anything’s wrong with her.”
B. Family history of mental illness
An additional contextual factor impacting the processes of parental adaptation to OCD was family history of mental illness. All parents reported having other family members with psychiatric disorders, but this history was often shrouded in secrecy, and typically not uncovered until after the child was diagnosed. Family history appeared to shape parents’ causal attributions of OCD and their feelings of guilt and blame around causation. Notably, participants with a personal history of depression or anxiety often used their own experiences to inform their understanding of their child’s OCD and its management:
“I think it’s maybe more intuitive for me… because I’ve had some issues with depression before myself…. that it’s not a rational kind of thing, and you can’t really think clearly and it’s not like you can just… pull yourself up by your bootstraps and get over it.”
C. Stigma
The processes of parental adaptation and their contextual elements all occurred against the backdrop of stigma associated with OCD. Participants experienced not only social stigma against mental illness, but also self-stigma (i.e. embarrassment about their child’s behaviors and symptoms), which together pervaded – and inhibited – every aspect of their process of adapting to their child’s OCD. Stigma increased parental guilt, influenced family dynamics, interfered with the ability to interpret the meaning of OCD in a productive way, and inhibited support seeking:
“There’s still a lot of stigma around mental health issues, and I don’t want people to look at her in a different way, and treat her in a different way… the worst thing would be for somebody to [say] ‘oh why don’t you just get your [stuff] together?’ – to make her feel bad about it, would be really bad.”
Parental perceptions about genetic counseling for OCD
Participants were presented with two short vignettes that described a genetic counseling scenario in which etiological information about OCD was provided. The first genetic counseling vignette involved education and counseling about the etiology of OCD only, while the second vignette focused on using a pedigree and empiric evidence to provide recurrence risks for OCD (see supplemental information for interview guide).
Participants articulated how the information provided by genetic counseling might be empowering, allowing parents who were feeling lost and powerless to feel more in control of their situation. They described how becoming “armed with information” could reduce family stress and anxiety, and help with the process of accepting, managing, and adapting to OCD. Participants also felt that the information provided by genetic counseling might help them and their family members to engage in anticipatory management by learning to recognize signs and symptoms of mental illness and seek early intervention:
“It’d be useful when [my daughter] and [her sister] have kids. It would be useful for having an awareness of that – you can watch for things and not wait until they’re [older] before you get some help with it.”
Participants further described how an understanding of the causes of OCD could help alleviate parental guilt, and thus play an important role in supporting parents’ adaptation to their child’s OCD. As one participant who had received genetic counseling related to her child’s OCD explained:
“I think that [genetic counseling] has a really big role… Because there is a lot of self-blame… [and] the parents are the caregivers and their wellbeing is [going to] be reflective on the child’s journey as well. So it just sort of recognizes that piece and supports and cares for the caregiver.”
Participants described how the etiological information provided in the genetic counseling vignettes could help them understand why both biological and environmental treatments are useful for managing OCD, for example helping them to recognize their ability to modify environmental factors, and to understand why medication may be effective:
“Understanding [the causes] made me realize that even though I was [previously] really against medication, that was probably the way to go… I realized she’s at a point where it’s not something she could just control on her own, that she needed help… [and] that there are certain brain development parts that contributed to [OCD], that medication could help stabilize.”
Interestingly, most participants were not overly interested in learning specific numerical recurrence risks, as described in the second vignette, but saw value in generally learning about etiology and increased risks in a family in order to facilitate early intervention:
“If you’re talking about a hypothetical child… it’s [helpful] to say, you have [a] predisposition… the best thing you can do is be aware of that… it’s about getting the right help, having the right kind of treatment plan in place, and obviously the sooner you do that, the better off everybody’s [going to] be.”
Parents also provided insight into what they thought might be useful for them when receiving genetic counseling. Several participants described the importance of increasing awareness of genetic counseling and understanding of what it is so that parents could better access this service:
“If they had any sort of ongoing clinics, I think it might be a good idea if it’s almost like an expectation that the parent would have a session of genetic counseling.”
A few participants discussed the importance of considering the timing of the genetic counseling intervention – specifically, providing this to families soon after diagnosis of OCD:
“The timing of that conversation is important… having that counseling to get more information upfront would be helpful…right at the beginning, once people have been diagnosed with OCD, that’s the time to do it.”
Participants also recommended thorough contracting with families upfront about what genetic counseling for OCD entails, as well as whether they are interested in knowing specific recurrence information:
“Ask [parents], how involved do you want us to get? Do you want it right down to, ‘these are the odds of it happening again’ or do you just want to understand more of how it happens and why it happens?”
Participants overall expressed positive perceptions about genetic counseling for parents of children of OCD; they anticipated benefits like empowerment, anticipatory management, alleviation of guilt and blame, and improved treatment orientation, and felt that psychiatric genetic counseling should be offered earlier and more often to families affected by OCD.
Discussion
This is the first study to explore the process through which parents adapt to a diagnosis of OCD in their child. Though we set out to explore parental experience with, and causal attributions for, pediatric OCD, a far richer picture of the process of parental adaptation to their child’s OCD emerged from our data and is broadly represented by the conceptual framework described. This framework encompasses the role of causal attributions, but also highlights other important components of the parental adaptation process and how they are impacted by contextual factors. The insight gained here can be used to inform genetic counseling for families of children with OCD in order to facilitate parental adaptation to pediatric OCD and improve functioning for both children and their families.
While no previous studies have specifically explored parental adaptation to a child’s OCD, some studies have examined coping in this context. Coping is a reactive process of responding to a change, typically a stressful one, within a relatively immediate timeframe. Conversely, adaptation is a process of adjusting to change over the longer term, which incorporates both anticipatory/proactive and reactive elements (Field et al., 2012). However, despite the differences between the two constructs, our findings are supported by those from the studies of coping. Specifically, our data about conceptualizing the meaning of OCD reflect important themes also identified in studies of coping, including “parents’ attempts to make sense of OCD” and their development of “constructions” of the disorder, including externalizing the condition from the child and distinguishing it from other phenomena. (Futh, Simonds, & Micali, 2012) Also, similar to our concept navigating the impact of OCD on family dynamics, Futh et al. described the emotional toll of pediatric OCD on parents, including feelings of helplessness, frustration, and self-blame, as well as an impact on the marital relationship(Futh et al., 2012) ; while another study found that parents of children with OCD experienced a great deal of guilt around causation of their child’s OCD (Stengler-Wenzke et al., 2004a). These data lend broad support to the findings that emerged here.
Our data on parental adaptation to OCD expand our understanding of the family experience of OCD. We describe novel findings that have not been recognized in studies of familial coping to OCD. The difference between the constructs of coping and adaptation may explain why some factors that emerged here as important to adaptation were not identified in studies on coping. Specifically, stigma, family history, and nature of the child’s illness that emerged here but were not identified in the studies on coping, are issues that may be more relevant when considering OCD from a long-term adaptation-based perspective, rather than an acute, reactive, coping-based perspective. Given that stigma is well understood to “diminish self-esteem and rob people of social opportunities” [p. 614] (Corrigan, 2004), impact both the individual with mental illness and their relatives(Stengler-Wenzke et al., 2004b), and discourage help-seeking and negatively impact outcomes(Corrigan, 2004), it could influence parental adaptation to OCD in a way that it may not influence coping. Further, and crucially, it is clear that while some coping strategies may facilitate adaptation, others – in this context, accommodating or ignoring a child’s symptoms for example – may obstruct the process. (Albert et al., 2010; Lebowitz et al., 2012; Peay, Rosenstein, & Biesecker, 2013)
It is important that interventions for supporting the long-term adaptation process of parents of children with OCD are developed, refined, and implemented, both for parental well-being and to improve outcomes for affected children via optimized family functioning. (Peris et al., 2012) Genetic counseling, which involves comprehensive discussion of, and supportive counseling around, genetic and environmental contributions to conditions in families(National Society of Genetic Counselors’ Definition Task Force et al., 2006), is ideally placed to support parents in their journey of adapting to their child’s OCD, and indeed directly addresses several of the important concepts that emerged from our data, in particular family history of mental illness, conceptualizing the meaning of OCD, stigma, and navigating the impact of OCD on family dynamics. Specifically, by providing information and support about the etiology of OCD, genetic counseling can address parental guilt around having passed on a genetic vulnerability to OCD and/or contributed to the illness through parenting(J. C. Austin & Honer, 2008), and may decrease self-stigma in people with mental illness and their family members (Costain et al., 2014; Costain, Esplen, Toner, Hodgkinson, & Bassett, 2014; Meiser et al., 2005). Genetic counseling can also help with impacts on family dynamics by alleviating any blame processes that may be present.
Genetic counseling can also support parents as they adjust to the nature of the illness as manifested in the child, and facilitate the development of effective illness management strategies by positively impacting treatment orientation and connecting families with support and resources.
Limitations and future directions
Participants in this study were self-selected, generally well-educated (with 77% having completed post-secondary education), and all had interacted with a specialty OCD clinic, receiving at minimum a full psychiatric/psychological assessment of their child and an OCD resource sheet. Consequently, their perspectives may differ from those of parents who have not received specialty care for their child and/or have received less formal education. In addition, given that there is some evidence of gender-related differences in coping with a child’s OCD(Futh et al., 2012), and in caring for a relative with mental illness, (Moller, Gudde, Folden, & Linaker, 2009), our data – generated primarily from mothers – may not capture the adaptation process as experienced by fathers, and future research focusing on fathers’ experiences may be valuable.
While data saturation was achieved for the main concepts presented within the preliminary framework (i.e. the three processes of parental adaptation and three contextual elements of influencing parental adaptation), future work is needed to validate the properties and dimensions of these concepts and explore how they relate to one another and impact the process of parental adaptation. The findings of this retrospective cross-sectional study effectively capture parental adaptation at a single moment in time for each participant; in future, a prospective study would allow for the ongoing process of parental adaptation to be explored longitudinally. In addition, future study exploring adaptation in the context of other common psychiatric disorders would help elucidate similarities and differences in the processes of adaptation to these conditions, and may further inform psychiatric genetic counseling for a range of disorders.
Finally, future studies that employ genetic counseling as a specialist intervention and evaluate its impact on the process of parental and family adaptation would be an important step in using these data to develop useful clinical interventions for this population.
Conclusions
These data provide insight into the process of parental adaptation to pediatric OCD and offer a unique perspective into the education and counseling needs of this population, marking the first step towards provision of effective and comprehensive genetic counseling services for families affected by OCD. The conceptual framework of the process of adaptation developed in this study is supported by literature on parental coping with OCD, and serves to highlight key areas in which genetic counseling can facilitate the adaptation process. These data support collaboration between psychiatrists and genetic counselors to provide genetic counseling services for families (J. Austin, Inglis, & Hadjipavlou, 2014), which may help to facilitate the process of adaptation to OCD. Additionally, from a broader public health perspective, this model describes how a common disease can impact individuals and their families, and how genetic counseling may be able to provide them with an additional source of support. This will become increasingly relevant as our understanding of the genetics of OCD, other mental illnesses, and other common multifactorial diseases continues to grow.
Supplementary Material
Acknowledgments
The authors thank the participants for so readily and insightfully sharing their experiences. This project was supported by the National Society of Genetic Counselors (NSGC) Jane Engelberg Memorial Fellowship Student Award, the NSGC Psychiatric SIG Student Award, and the Hospital for Sick Children Trainee Start-Up Fund. HA was a student in the MSc in Genetic Counselling program at the University of Toronto when this work was completed. JA was supported by the Canada Research Chairs Program, the Michael Smith Foundation for Health Research, and BC Mental Health and Addictions Services. AS was supported by the Canadian Institutes of Health Research and the Michael Smith Foundation for Health Research. Transcription services were provided by Ms. Simone Newstadt and Ms. Gwyneth Jones, and support and guidance provided by the member of the Translational Psychiatric Genetics Group (TPGG).
Footnotes
Conflict of Interest: Authors HA, AS, SES, CS, RH, and JA declare that they have no conflict of interest.
Human Studies and Informed Consent: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). Informed consent was obtained from all individual participants included in the study.
Animal Studies: No animal studies were carried out by the authors for this article.
References
- Albert U, Bogetto F, Maina G, Saracco P, Brunatto C, Mataix-Cols D. Family accommodation in obsessive-compulsive disorder: Relation to symptom dimensions, clinical and family characteristics. Psychiatry Research. 2010;179(2):204–211. doi: 10.1016/j.psychres.2009.06.008. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 2000. Text Revision ed. [Google Scholar]
- Austin J, Inglis A, Hadjipavlou G. Genetic counseling for common psychiatric disorders: An opportunity for interdisciplinary collaboration. The American Journal of Psychiatry. 2014;171(5):584–585. doi: 10.1176/appi.ajp.2014.13101421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin JC, Honer WG. Psychiatric genetic counselling for parents of individuals affected with psychotic disorders: A pilot study. Early Intervention in Psychiatry. 2008;2(2):80–89. doi: 10.1111/j.1751-7893.2008.00062.x. [DOI] [PubMed] [Google Scholar]
- Bolton D, Perrin S. Evaluation of exposure with response-prevention for obsessive compulsive disorder in childhood and adolescence. Journal of Behavior Therapy and Experimental Psychiatry. 2008;39(1):11–22. doi: 10.1016/j.jbtep.2006.11.002. [DOI] [PubMed] [Google Scholar]
- Charmaz K. Constructing grounded theory: A practical guide through qualitative analysis. London, England: Sage Publications; 2006. [Google Scholar]
- Corbin J, Strauss A. Basics of qualitative research: Techniques and procedures for developing grounded theory. 2. Thousand Oaks, CA: Sage Publications; 1998. [Google Scholar]
- Corrigan P. How stigma interferes with mental health care. The American Psychologist. 2004;59(7):614–625. doi: 10.1037/0003-066X.59.7.614. [DOI] [PubMed] [Google Scholar]
- Costain G, Esplen MJ, Toner B, Hodgkinson KA, Bassett AS. Evaluating genetic counseling for family members of individuals with schizophrenia in the molecular age. Schizophrenia Bulletin. 2014;40(1):88–99. doi: 10.1093/schbul/sbs124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costain G, Esplen MJ, Toner B, Scherer SW, Meschino WS, Hodgkinson KA, Bassett AS. Evaluating genetic counseling for individuals with schizophrenia in the molecular age. Schizophrenia Bulletin. 2014;40(1):78–87. doi: 10.1093/schbul/sbs138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLisi LE, Bertisch H. A preliminary comparison of the hopes of researchers, clinicians, and families for the future ethical use of genetic findings on schizophrenia. American Journal of Medical Genetics Part B, Neuropsychiatric Genetics : The Official Publication of the International Society of Psychiatric Genetics. 2006;141B(1):110–115. doi: 10.1002/ajmg.b.30249. [DOI] [PubMed] [Google Scholar]
- Field CB, Barros V, Stocker TF, Qin D, Dokken DJ, Ebi KL, editors. Managing the risks of extreme events and disasters to advance climate change adaptation: A special report of the intergovernmental panel on climate change. Cambridge, UK, and New York, NY, USA: Cambridge University Press; 2012. [Google Scholar]
- Futh A, Simonds LM, Micali N. Obsessive-compulsive disorder in children and adolescents: Parental understanding, accommodation, coping and distress. Journal of Anxiety Disorders. 2012;26(5):624–632. doi: 10.1016/j.janxdis.2012.02.012. [DOI] [PubMed] [Google Scholar]
- Geller DA, March J. Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51(1):98–113. doi: 10.1016/j.jaac.2011.09.019. [DOI] [PubMed] [Google Scholar]
- Grover S, Dutt A. Perceived burden and quality of life of caregivers in obsessive-compulsive disorder. Psychiatry and Clinical Neurosciences. 2011;65(5):416–422. doi: 10.1111/j.1440-1819.2011.02240.x. [DOI] [PubMed] [Google Scholar]
- Hansson L, Jormfeldt H, Svedberg P, Svensson B. Mental health professionals’ attitudes towards people with mental illness: Do they differ from attitudes held by people with mental illness? The International Journal of Social Psychiatry. 2013;59(1):48–54. doi: 10.1177/0020764011423176. [DOI] [PubMed] [Google Scholar]
- Holzinger A, Kilian R, Lindenbach I, Petscheleit A, Angermeyer MC. Patients’ and their relatives’ causal explanations of schizophrenia. Social Psychiatry and Psychiatric Epidemiology. 2003;38(3):155–162. doi: 10.1007/s00127-003-0624-5. [DOI] [PubMed] [Google Scholar]
- Karno M, Golding JM, Sorenson SB, Burnam MA. The epidemiology of obsessive-compulsive disorder in five US communities. Archives of General Psychiatry. 1988;45(12):1094–1099. doi: 10.1001/archpsyc.1988.01800360042006. [DOI] [PubMed] [Google Scholar]
- Koran LM, Blair Simpson MDH. Guideline watch (march 2013): Practice guideline for the treatment of patients with obsessive-compulsive disorder. Arlington, VA: American Psychiatric Association; 2013. [PubMed] [Google Scholar]
- Lebowitz ER, Panza KE, Su J, Bloch MH. Family accommodation in obsessive-compulsive disorder. Expert Review of Neurotherapeutics. 2012;12(2):229–238. doi: 10.1586/ern.11.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyus VL. The importance of genetic counseling for individuals with schizophrenia and their relatives: Potential clients’ opinions and experiences. American Journal of Medical Genetics Part B, Neuropsychiatric Genetics : The Official Publication of the International Society of Psychiatric Genetics. 2007;144B(8):1014–1021. doi: 10.1002/ajmg.b.30536. [DOI] [PubMed] [Google Scholar]
- March JS. Cognitive-behavioral psychotherapy for children and adolescents with OCD: A review and recommendations for treatment. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34(1):7–18. doi: 10.1097/00004583-199501000-00008. [DOI] [PubMed] [Google Scholar]
- McAllister M. Grounded theory in genetic counseling research. Journal of Genetic Counseling. 2001;10(3):233–250. [Google Scholar]
- Meiser B, Mitchell PB, McGirr H, Van Herten M, Schofield PR. Implications of genetic risk information in families with a high density of bipolar disorder: An exploratory study. Social Science & Medicine (1982) 2005;60(1):109–118. doi: 10.1016/j.socscimed.2004.04.016. [DOI] [PubMed] [Google Scholar]
- Moller T, Gudde CB, Folden GE, Linaker OM. The experience of caring in relatives to patients with serious mental illness: Gender differences, health and functioning. Scandinavian Journal of Caring Sciences. 2009;23(1):153–160. doi: 10.1111/j.1471-6712.2008.00605.x. [DOI] [PubMed] [Google Scholar]
- National Society of Genetic Counselors’Definition Task Force. Resta R, Biesecker BB, Bennett RL, Blum S, Hahn SE, Williams JL. A new definition of genetic counseling: National society of genetic counselors’ task force report. Journal of Genetic Counseling. 2006;15(2):77–83. doi: 10.1007/s10897-005-9014-3. [DOI] [PubMed] [Google Scholar]
- Pauls DL. The genetics of obsessive compulsive disorder: A review of the evidence. American Journal of Medical Genetics Part C, Seminars in Medical Genetics. 2008;148C(2):133–139. doi: 10.1002/ajmg.c.30168. [DOI] [PubMed] [Google Scholar]
- Peay HL, Hooker GW, Kassem L, Biesecker BB. Family risk and related education and counseling needs: Perceptions of adults with bipolar disorder and siblings of adults with bipolar disorder. American Journal of Medical Genetics Part A. 2009;149A(3):364–371. doi: 10.1002/ajmg.a.32696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peay HL, Rosenstein DL, Biesecker BB. Adaptation to bipolar disorder and perceived risk to children: A survey of parents with bipolar disorder. BMC Psychiatry. 2013;13:327-244X-13-327. doi: 10.1186/1471-244X-13-327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peris TS, Sugar CA, Bergman RL, Chang S, Langley A, Piacentini J. Family factors predict treatment outcome for pediatric obsessive-compulsive disorder. Journal of Consulting and Clinical Psychology. 2012;80(2):255–263. doi: 10.1037/a0027084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan JC, Yang LH, Cruz-Rojas R. Effects of attributing serious mental illnesses to genetic causes on orientations to treatment. Psychiatric Services (Washington, DC) 2006;57(3):382–387. doi: 10.1176/appi.ps.57.3.382. [DOI] [PubMed] [Google Scholar]
- Quaid KA, Aschen SR, Smiley CL, Nurnberger JI., Jr Perceived genetic risks for bipolar disorder in a patient population: An exploratory study. Journal of Genetic Counseling. 2001;10(1):41–51. [Google Scholar]
- Ramos-Cerqueira AT, Torres AR, Torresan RC, Negreiros AP, Vitorino CN. Emotional burden in caregivers of patients with obsessive-compulsive disorder. Depression and Anxiety. 2008;25(12):1020–1027. doi: 10.1002/da.20431. [DOI] [PubMed] [Google Scholar]
- Ruscio AM, Stein DJ, Chiu WT, Kessler RC. The epidemiology of obsessive-compulsive disorder in the national comorbidity survey replication. Molecular Psychiatry. 2010;15(1):53–63. doi: 10.1038/mp.2008.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz PM, Schulz SC, Dibble E, Targum SD, van Kammen DP, Gershon ES. Patient and family attitudes about schizophrenia: Implications for genetic counseling. Schizophrenia Bulletin. 1982;8(3):504–513. doi: 10.1093/schbul/8.3.504. [DOI] [PubMed] [Google Scholar]
- Semaka A, Balneaves LG, Hayden MR. “Grasping the grey”: Patient understanding and interpretation of an intermediate allele predictive test result for huntington disease. Journal of Genetic Counseling. 2013;22(2):200–217. doi: 10.1007/s10897-012-9533-7. [DOI] [PubMed] [Google Scholar]
- Simonds LM, Thorpe SJ. Attitudes toward obsessive-compulsive disorders--an experimental investigation. Social Psychiatry and Psychiatric Epidemiology. 2003;38(6):331–336. doi: 10.1007/s00127-003-0637-0. [DOI] [PubMed] [Google Scholar]
- Skirton H, Eiser C. Discovering and addressing the client’s lay construct of genetic disease: An important aspect of genetic healthcare? Research and Theory for Nursing Practice. 2003;17(4):339–352. doi: 10.1891/rtnp.17.4.339.53195. [DOI] [PubMed] [Google Scholar]
- Steketee G. Disability and family burden in obsessive-compulsive disorder. Canadian Journal of Psychiatry Revue Canadienne De Psychiatrie. 1997;42(9):919–928. doi: 10.1177/070674379704200902. [DOI] [PubMed] [Google Scholar]
- Stengler-Wenzke K, Kroll M, Matschinger H, Angermeyer MC. Quality of life of relatives of patients with obsessive-compulsive disorder. Comprehensive Psychiatry. 2006;47(6):523–527. doi: 10.1016/j.comppsych.2006.02.002. [DOI] [PubMed] [Google Scholar]
- Stengler-Wenzke K, Trosbach J, Dietrich S, Angermeyer MC. Coping strategies used by the relatives of people with obsessive-compulsive disorder. Journal of Advanced Nursing. 2004a;48(1):35–42. doi: 10.1111/j.1365-2648.2004.03166.x. [DOI] [PubMed] [Google Scholar]
- Stengler-Wenzke K, Trosbach J, Dietrich S, Angermeyer MC. Experience of stigmatization by relatives of patients with obsessive compulsive disorder. Archives of Psychiatric Nursing. 2004b;18(3):88–96. doi: 10.1016/j.apnu.2004.03.004. [DOI] [PubMed] [Google Scholar]
- Stewart SE, Pauls DL. The genetics of obsessive-compulsive disorder. FOCUS: The Journal of Lifelong Learning in Psychiatry. 2010;8(3):350–357. [Google Scholar]
- van Grootheest DS, Cath DC, Beekman AT, Boomsma DI. Twin studies on obsessive-compulsive disorder: A review. Twin Research and Human Genetics : The Official Journal of the International Society for Twin Studies. 2005;8(5):450–458. doi: 10.1375/183242705774310060. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.