Abstract
IMPORTANCE
Reducing unnecessary tests and treatments is a potentially promising approach for improving the value of health care. However, relatively little is known about whether insurance type or local practice patterns are associated with delivery of low-value care.
OBJECTIVES
To compare low-value care in the Medicaid and commercially insured populations, test whether provision of low-value care is associated with insurance type, and assess whether local practice patterns are associated with the provision of low-value care.
DESIGN, SETTING, AND PARTICIPANTS
This cross-sectional study of claims data from the Oregon Division of Medical Assistance Programs and the Oregon All-Payer All-Claims database included Medicaid and commercially insured adults aged 18 to 64 years. The study period was January 1, 2013, through December 31, 2013.
MAIN OUTCOMES AND MEASURES
Low-value care was assessed using 16 claims-based measures. Logistic regression was used to test the association between Medicaid vs commercial insurance coverage and low-value care and the association between Medicaid and commercial low-value care rates within primary care service areas (PCSAs).
RESULTS
This study included 286 769 Medicaid and 1 376 308 commercial enrollees in 2013. Medicaid enrollees were younger (167 847 [58.5%] of Medicaid enrollees were aged 18–34 years vs 505 628 [36.7%] of those with commercial insurance) but generally had worse health status compared with those with commercial insurance. Medicaid enrollees were also more likely to be female (180 363 [62.9%] vs 702 165 [51.0%]) and live in a rural area (120 232 [41.9%] vs 389 964 [28.3%]). A total of 10 304 of 69 338 qualifying Medicaid patients (14.9%; 95% CI, 14.6%–15.1%) received at least 1 low-value service during 2013; the corresponding rate for commercially insured patients was 35 739 of 314 023 (11.4%; 95% CI, 11.3%–11.5%). No consistent association was found between insurance type and low-value care. Compared with commercial patients, Medicaid patients were more likely to receive low-value care for 10 measures and less likely to receive low-value care for 5 others. For 7 of 11 low-value care measures, Medicaid patients were significantly more likely to receive low-value care if they resided in a PCSA with a higher rate of low-value care for commercial patients.
CONCLUSIONS AND RELEVANCE
Oregon Medicaid and commercially insured patients received moderate amounts of low-value care in 2013. No consistent association was found between insurance type and low-value care. However, Medicaid and commercial rates of low-value care were associated with one another within PCSAs. Low-value care may be more closely related to local practice patterns than to reimbursement generosity or insurance benefit structures.
Low-value care is an increasingly salient issue for the medical community, policymakers, and patients. These services provide little clinical benefit to patients and may even cause harm. Reducing low-value services could benefit patients and constrain health care expenditures; some research suggests that more than 20% of US health care spending is inefficient or wasteful, with low-value care accounting for a substantial portion of this unnecessary excess cost.1
The American Board of Internal Medicine Foundation has led a physician response to this issue through its Choosing Wisely initiative.2 This initiative aims to benefit patients and improve value in health care by focusing attention on lists of tests and procedures that may not be needed. These lists are based on evidence-based practices and guidelines and are intended to support patient-physician conversations about low-value care.
An emerging body of research has begun to quantify the prevalence and implications of low-value services. Most of this work has focused on the Medicare population,3–5 although research has begun to assess the pervasiveness of these services in other payer groups.6,7 The present study uses comprehensive data from Medicaid and commercially insured populations in Oregon to advance the literature on low-value care on several fronts.
First, we explore the pervasiveness of low-value care in a state Medicaid population. Medicaid is now the largest public health insurance program in the United States, covering approximately 66 million people.8 Expenditures for the program accounted for almost one-quarter of total state government budgets before the 2014 Medicaid expansion9 and are anticipated to increase. Policies targeting low-value services in Medicaid offer the potential to improve patient care while supporting the program’s long-term financial viability. To our knowledge, the present study is the first to provide broad estimates of low-value care in this important population.
Second, we compare the prevalence of low-value care in a Medicaid population to commercially insured enrollees, evaluating the association between insurance type and low-value care within a single state. These analyses contribute information regarding the role of reimbursement generosity in the provision of low-value care.
Third, we assess the association between Medicaid and commercial low-value care delivery within local practice areas, providing information about the extent to which local practice patterns may explain low-value care delivery. Together, these analyses advance knowledge on the pervasiveness of low-value care and provide policy-relevant information about insurance type and local practice patterns as potential drivers of these services.
Methods
Study Population and Data
We used 2012 and 2013 Medicaid claims from Oregon’s Division of Medical Assistance Programs and commercial claims from the Oregon All-Payer All-Claims (APAC) database. Analyses were conducted on data from January 1, 2013, through December 31, 2013. Data from January 1, 2012, through Dec 31, 2012, were also used to assess relevant medical history information. The Division of Medical Assistance Programs data include all managed care and fee-for-service claims. Approximately 90% of Oregon Medicaid beneficiaries in 2013 were enrolled in coordinated care organizations, similar to managed care organizations.10,11 The APAC database contains claims submitted by multiple commercial carriers, excluding those with fewer than 5000 enrollees, and the Federal Employee Health Benefits Program. Together, APAC data cover an estimated 87% of commercially insured Oregonians; most have fee-for-service or preferred provider organization– type plans, and approximately 30% have a health maintenance organization–type plan. We excluded enrollees who were pregnant, younger than 18 years or older than 64 years, or dually eligible for Medicare and Medicaid. All claims data were deidentified.
Key Points.
Question
What patterns of low-value care are present across Medicaid and commercially insured populations?
Findings
In this cross-sectional study of Medicaid and commercial insurance claims in Oregon, no consistent association was found between insurance type and low-value care, with Medicaid patients more likely to receive some low-value services but less likely to receive others. For 7 of 11 low-value care measures, Medicaid patients were significantly more likely to receive low-value care if they resided in an area with a higher rate of low-value care for commercial patients.
Meaning
Low-value care may be more closely related to local practice patterns than to reimbursement generosity or insurance benefit structures.
Variables
Low-Value Care Measures
The outcome of interest for this study was receipt of low-value care. Several groups have developed tools to detect low-value services in claims data.3–5,7,8 For the present study, we used 13 measures from work by Schwartz and colleagues,3,5 selected for relevance to Medicaid and commercial populations. The selected measures represent evidence-based recommendations from the American Board of Internal Medicine Foundation’s Choosing Wisely initiative and the United Kingdom’s National Institute for Health and Care Excellence. We also used 3 Quality Net measures from the Center for Medicaid & Medicare Services. Choosing Wisely, the National Institute for Health and Care Excellence, and Quality Net all aim to provide resources that promote effective, high-value medical care; additional information is in eTable 1 in the Supplement. When necessary, we made minor adaptations to apply measures to the Medicaid population (eg, allowing for short gaps in enrollment). We also chose measure definitions with relatively higher specificity and lower sensitivity when available to reduce the potential for misclassifying appropriate care as low value.3
For each of the 16 low-value care measures, we first identified visits at which patients were eligible to receive low-value services based on qualifying diagnoses and exclusions. The resulting set of qualifying visits represented visits at which the patient was potentially at risk of receiving the service in question. From that denominator, we then identified visits that included the low-value service of interest. For example, we constructed the electroencephalogram for headache measure by first identifying unique 2013 visits with a diagnosis of headache but no current diagnosis or 1-year medical history of epilepsy. From that denominator of qualifying visits, we then constructed the numerator by identifying which visits included an electroencephalogram service. Details of each measure are presented in eTable 1 in the Supplement.
Covariates
Patient characteristics included age (18–34, 35–49, 50–64 years), sex, rural vs urban residence, type of insurance coverage (Medicaid or commercial), and a modified version of the Charlson comorbidity index.12 Our modified comorbidity index excluded human immunodeficiency virus and AIDS because these claims are excluded from APAC data. Each beneficiary was also assigned a primary care service area (PCSA) based on the zip code of residence. National PCSAs were developed by the Dartmouth Atlas of Health Care as groups of zip codes that represent natural markets of primary care for Medicare patients.13,14 We used 130 PCSAs that were developed using similar criteria to Dartmouth PCSAs, as well as additional contextual and topographical information.15
Statistical Analysis
We assessed total visit-level instances of each low-value service in 2013. We then calculated the corresponding proportion of affected patients, defined as the number of beneficiaries with at least 1 visit for the service of interest in 2013, divided by the number with at least 1 qualifying visit for the service during 2013.
To examine the influence of insurance type, we assessed the association between receipt of low-value care and Medicaid vs commercial insurance coverage using patient-level logistic regressions for each of the 16 measures. In each model, patients were restricted to those with qualifying visits for the measure in question. The outcome was a binary variable that indicated receipt of low-value care in 2013. The primary independent variable was an indicator of insurance type. Additional covariates included patient demographics, rural or urban residence, and the Charlson comorbidity index. Risk differences associated with insurance type were calculated from resulting models as the difference in marginal effects for the average qualifying patient. Sensitivity analyses included models that added the total number of qualifying visits for each beneficiary and patients’ PCSA of residence to models. We also examined the influence of insurance on receiving any type of low-value care and whether the influence of insurance varied for subgroups of services: higher vs lower remuneration and more vs less likely to occur in the emergency department (ED) (eAppendix and eTable 2 in the Supplement).
To examine the influence of local practice patterns, we assessed the association between receipt of low-value care among Medicaid patients and the rate of low-value care among commercially insured patients residing in the same PCSA. A positive association may indicate that local practice patterns for low-value care persist across distinct populations of patients. For this analysis, we first selected measures with 150 or more total instances of low-value care observed in Medicaid during 2013. We then generated smoothed commercial low-value care rates for each PCSA. Smoothed estimators reduce error that may arise because of small sample sizes.16 Next, we conducted patient- level logistic regressions for the Medicaid population, where the dependent variable was the receipt of low value care and the independent variables included patient demographics, rural or urban residence, the Charlson comorbidity index, and the smoothed rate of commercial low-value care in the patient’s PCSA of residence. We estimated marginal effects to assess the change in predicted probability of receiving low-value care for an average Medicaid patient when commercial low-value care rates in their PCSA of residence increased by 1%. The SEs were clustered at the PCSA level. Additional details are provided in the eAppendix in the Supplement. Data management and analyses were conducted using R statistical software, version 3.1.2.17
Results
Our study included 286 769 Medicaid and 1 376 308 commercial enrollees in 2013. Medicaid enrollees were younger but generally had worse health status compared with those with commercial insurance (Table 1). Medicaid enrollees were also more likely to be female (180 363 [62.9%] vs 702 165 [51.0%]) and live in a rural area (120 232 [41.9%] vs 389 964 [28.3%]). In 2013, a total of 10 304 of 69 338 qualifying Medicaid patients (14.9%) (95% CI, 14.6%–15.1%) received at least 1 of 16 low-value services compared with 35 739 of 314 023 commercially insured patients (11.4%) (95% CI, 11.3%–11.5%) (Table 2). We observed substantial variability in the prevalence of different types of low-value care. For example, 4273 of 18 871 Medicaid patients (22.6%) (95% CI, 22.1%–23.2%) presenting with nonspecific low-back pain during 2013 received a non indicated image, and 4323 of 23 211 Medicaid patients (18.6%) (95% CI, 17.7%–18.7%) presenting with uncomplicated headache received low-value head imaging. However, only 343 of 11 992 Medicaid patients (2.9%) (95% CI, 2.6%–3.2%) presenting with acute rhinosinusitis underwent inappropriate sinus computed tomography.
Table 1.
Characteristics of the Study Population in 2013 by Insurance Typea
| Characteristic | Insurance Typeb | P Valuec | |
|---|---|---|---|
| Commercial (n = 1 376 308) | Medicaid (n = 286 769) | ||
| Age, y | |||
| 18–34 | 505 628 (36.7) | 167 847 (58.5) | |
| 35–49 | 433 689 (31.5) | 70 173 (24.5) | <.001 |
| 50–64 | 436 991 (31.8) | 48 749 (17.0) | |
| Female sex | 702 165 (51.0) | 180 363 (62.9) | <.001 |
| Rural residence | 389 964 (28.3) | 120 232 (41.9) | <.001 |
| Charlson comorbidity index, mean (SD) | 0.29 (0.89) | 0.56 (1.32) | <.001 |
| Charlson comorbiditiesd | |||
| Myocardial infarction | 5597 (0.4) | 2482 (0.9) | <.001 |
| Congestive heart failure | 7539 (0.6) | 4760 (1.7) | <.001 |
| Peripheral vascular disease | 8032 (0.6) | 3756 (1.1) | <.001 |
| Cerebrovascular disease | 12 586 (0.9) | 5634 (2.0) | <.001 |
| Dementia | 210 (0) | 228 (0.1) | <.001 |
| Chronic pulmonary disease | 11 467 (0.8) | 3301 (1.1) | <.001 |
| Rheumatic disease | 3779 (0.3) | 2006 (0.7) | <.001 |
| Peptic ulcer disease | 24 317 (1.8) | 14 242 (5.0) | <.001 |
| Mild liver disease | 69 201 (5.0) | 22 394 (7.8) | <.001 |
| Diabetes mellitus | |||
| Without chronic complications | 104 807 (7.6) | 47 400 (16.5) | <.001 |
| With chronic complications | 15 857 (1.2) | 6515 (2.3) | <.001 |
| Hemiplegia or paraplegia | 2586 (0.2) | 2955 (1.0) | <.001 |
| Renal disease | 11 455 (0.8) | 4247 (1.5) | <.001 |
| Any malignant tumore | 31 820 (2.3) | 6621 (2.3) | .92 |
| Moderate or severe liver disease | 1251 (0.1) | 1553 (0.5) | <.001 |
| Metastatic solid tumor | 4989 (0.4) | 1652 (0.6) | <.001 |
The study sample includes nonpregnant, nondual eligible adults aged 18 to 64 years.
Data are presented as number (percentage) of patients unless otherwise indicated.
P values for differences between insurance types were calculated using χ2 tests for categorical variables and t tests for numeric variables.
Health conditions are Charlson comorbidity index conditions, created using the enhanced International Classification of Diseases, Ninth Revision (ICD-9) algorithm for administrative data. Variables indicate whether conditions were present at any time during 2012 or 2013.
Including lymphoma and leukemia and excluding malignant neoplasm of skin.
Table 2.
Low-Value Care Among Adults With Medicaid or Commercial Insurance During 2013a
| Commercial
|
Medicaid
|
||||||
|---|---|---|---|---|---|---|---|
| No. of Patients
|
Qualifying Patients Affected (95% CI), % | No. of Patients
|
Qualifying Patients Affected (95% CI), % | ||||
| Low-Value Care Service | Source | Affected | Qualifying | Affected | Qualifying | ||
| Any | All | 35 739 | 314 023 | 11.4 (11.3–11.5) | 10 304 | 69 338 | 14.9 (14.6–15.1) |
|
| |||||||
| Imaging for nonspecific low-back pain | CW | 13 005 | 82 659 | 15.7 (15.5–16.0) | 4273 | 18 871 | 22.6 (22.1–23.2) |
|
| |||||||
| Head imaging for uncomplicated headache | CW | 7285 | 65 931 | 11.0 (10.8–11.3) | 4323 | 23 211 | 18.6 (17.7–18.7) |
|
| |||||||
| Head imaging for syncope | CW | 673 | 7466 | 9.0 (8.4–9.7) | 449 | 3174 | 14.1 (12.9–15.4) |
|
| |||||||
| Imaging for plantar fasciitis | CW | 2002 | 10 986 | 18.2 (17.5–19.0) | 180 | 1450 | 12.4 (10.8–14.1) |
|
| |||||||
| T3 tests for hypothyroidism | CW | 5098 | 31 228 | 16.3 (15.9–16.7) | 619 | 5891 | 10.5 (9.7–11.3) |
|
| |||||||
| Preoperative chest radiography | CW | 1694 | 39 169 | 4.3 (4.1–4.5) | 755 | 7848 | 9.6 (9.0–10.3) |
|
| |||||||
| Abdomen CT combined studies | CMS | 2097 | 28 075 | 7.5 (7.2–7.8) | 664 | 13 416 | 4.9 (4.6–5.3) |
|
| |||||||
| Simultaneous brain and sinus CT | CMS | 356 | 9742 | 3.7 (3.3–4.0) | 357 | 7761 | 4.6 (4.1–5.1) |
|
| |||||||
| CT for uncomplicated acute rhinosinusitis | CW | 1799 | 59 961 | 3.0 (2.9–3.1) | 343 | 11 992 | 2.9 (2.6–3.2) |
|
| |||||||
| Arthroscopic surgery for knee osteoarthritis | NICE | 1127 | 23 190 | 4.9 (4.6–5.1) | 164 | 6143 | 2.7 (2.3–3.1) |
|
| |||||||
| Thorax CT combined studies | CMS | 113 | 9287 | 1.2 (1.0–1.4) | 76 | 3822 | 2.0 (1.6–2.4) |
|
| |||||||
| Preoperative echocardiography | CW | 227 | 39 169 | 0.6 (0.5–0.7) | 88 | 7848 | 1.1 (0.9–1.4) |
|
| |||||||
| Spinal injections for low-back pain | Literature | 2720 | 130 587 | 2.1 (2.0–2.2) | 290 | 37 299 | 0.8 (0.7.0.9) |
|
| |||||||
| Preoperative stress testing | CW | 115 | 39 169 | 0.3 (0.24–0.35) | 46 | 7848 | 0.6 (0.4–0.8) |
|
| |||||||
| Preoperative pulmonary function testing | CW | 96 | 38 380 | 0.25 (0.20–0.30) | 42 | 7693 | 0.5 (0.4–0.7) |
|
| |||||||
| Electroencephalogram for headache | CW | 72 | 59 936 | 0.1 (0.09–0.15) | 60 | 20 091 | 0.3 (0.2–0.4) |
Abbreviations: CMS, Center for Medicare & Medicaid Services Quality Net; CT, computed tomography; CW, American Board of Internal Medicine Choosing Wisely Initiative; NICE, United Kingdom National Institute for Health and Care Excellence.
Columns report patient-level measures of low-value care. For example, 3174 Medicaid patients had at least 1 visit during 2013 that placed them at risk for receiving head imaging for syncope (qualifying patients). Of these at-risk patients, 449 received low-value head imaging at least once during 2013 (affected patients). The study sample includes nonpregnant, nondual eligible adults aged 18 to 64 years.
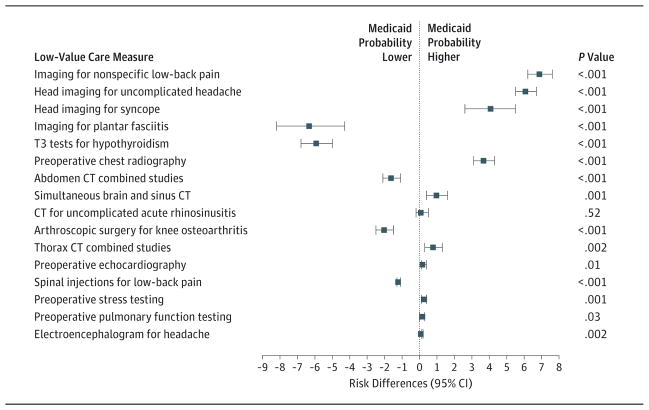
Figure 1 displays risk differences associated with Medicaid vs commercial insurance coverage. No consistent association was found between insurance type and low-value care. Medicaid insurance was associated with an increased probability of receiving 10 types of low-value care, whereas commercial insurance was associated with an increased probability of receiving 5 types of low-value care, with no statistically significant difference for 1 measure (additional details are in eTable 3 in the Supplement). Adjustment for the total number of qualifying visits or the patient’s PCSA of residence did not substantially change model estimates for the effect of insurance type on low-value care; although these factors may be related to low-value care, they did not confound the association between low-value care and insurance type in this study. Analyses that separated low-value services into higher vs lower remuneration suggested that price category did not modify the association between insurance type and low-value care (P for interaction = .64) (eTable 4 in the Supplement). In analyses that separated low-value services by ED category, we found that Medicaid patients were more likely than commercially insured patients to receive low-value care for measures likely to occur in the ED but not for other measures (P for interaction <.001) (eTable 5 in the Supplement).
Figure 1. Low-Value Care Risk Differences Associated With Medicaid vs Commercial Insurance Coverage.
Risk differences were calculated as the predicted probability of receiving low-value care with Medicaid insurance minus the predicted probability of receiving low-value care with commercial insurance for the average qualifying patient. Models were adjusted for patient age, sex, rural or urban residence, and Charlson comorbidity index. Dots indicate calculated risk differences; error bars, 95% CIs. The P values test for a significant difference between insurance types. CT indicates computed tomography.
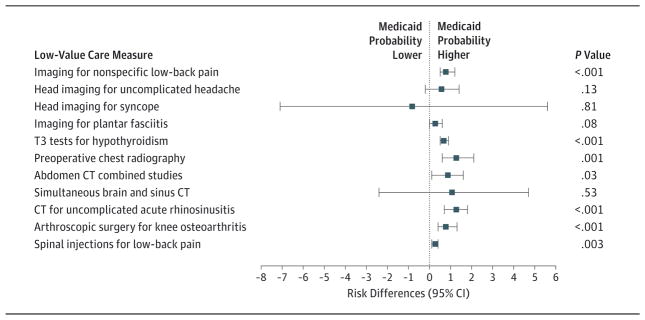
Eleven low-value services had sufficient volume for inclusion in geographic analyses. Rates for these services varied across insurance types and PCSAs (eFigure and eTable 6 in the Supplement). In Figure 2, we display low-value care risk differences, which represent the change in predicted probability of receiving low-value care for the average Medicaid patient, when commercial low-value care rates in their PCSA of residence increase by 1%. For 7 measures, Medicaid patients were significantly more likely to receive low-value care if they resided in a PCSA with a higher rate of commercial low-value care. For example, the predicted probability of the average Medicaid patient receiving imaging for low-back pain increased by 0.8% (95% CI, 0.5%–1.2%) for each 1% increase in the commercial rate in their PCSA of residence (additional details in eTable 7 in the Supplement).
Figure 2. Low-Value Care Risk Differences Associated With the Average Medicaid Patient Moving to a Primary Care Service Area (PCSA) With a 1%Higher Commercial Low-Value Care Rate.
Risk differences were calculated from logistic regression models, as the change in predicted probability of receiving low-value care for the average qualifying Medicaid patient, when the commercial rate of low-value care in their PCSA of residence increases by 1%. Models were adjusted for patient age, sex, rural or urban residence, and Charlson comorbidity index. Dots indicate calculated risk differences; error bars, 95%CIs. The P values test for a significant difference between residing in one PCSA compared with another PCSA with 1% higher commercial low-value care rates.
Discussion
In this statewide study of selected low-value services, moderate proportions of Medicaid and commercially insured patients received care that was likely to provide relatively little clinical benefit. Among qualifying Medicaid patients, 14.9% received a low-value service during 2013 compared with 11.4% of qualifying patients with commercial insurance. No consistent association was found between insurance type and low-value care. However, commercial and Medicaid low-value care rates were associated within PCSAs, suggesting local practice patterns may play a role in delivery of low-value care.
In general, rates of low-value care observed in this study are comparable to those described in other studies. For example, a national survey of ambulatory care practices found that 22.8% of visits by adults for acute low-back pain resulted in inappropriate imaging in 2009.6 Another study4 reported that 22.5% of Medicare beneficiaries with low-back pain received non indicated imaging between 2007 and 2011. These estimates fall within similar ranges to those found in our study (15.7% and 22.6% of qualifying commercial and Medicaid beneficiaries, respectively). In contrast, a national study7 of Anthem- affiliated commercial health plans reported that 53.7% of members with low-back pain received non indicated imaging. This difference may be attributable to lower use rates in Oregon relative to the rest of the country.18
Our study did not find a consistent association between insurance type and low-value care. There are a variety of reasons why the rate of low-value services might be higher among 1 insurance group vs another. One hypothesis was that higher reimbursement may cause physicians to provide more low-value care to commercial patients, particularly for high-cost services. However, our data did not support this hypothesis, suggesting that remuneration may play a limited role in low-value care delivery. Rates of particular low-value services may also differ by insurance type if commercial and Medicaid insurers use different methods of oversight, utilization review, or preauthorization for different services. In addition, there may be more barriers to care for Medicaid patients, discouraging physicians from ordering certain unnecessary services, which add logistical complication to care plans. Finally, post hoc analyses revealed that Medicaid patients were more likely than commercial patients to receive low-value care for measures classified as more likely to occur in the ED but not for other measures. This finding may be because Medicaid patients are more likely than their commercially insured counterparts to seek care and therefore qualify for measures in the ED. For example, a commercially insured patient with an uncomplicated head achemay seek care with a primary care physician with whom he or she has the benefit of an established relationship and continuity of care. In contrast, a Medicaid patient may be more likely to seek care in the ED. This example reflects the fact that services were classified at the measure level only, so patients who qualified for services likely to occur in the ED are therefore a mix of patients who actually received services in the ED and those who received services in other settings.
We found an association between commercial and Medicaid low-value care rates within PCSAs. For most measures, Medicaid patients were more likely to receive low-value care if they resided in a PCSA with a higher rate of commercial low-value care. These findings align with previous work that has also suggested that small area variations span payer types.19 A variety of local factors, such as physician practice norms, may underlie similar care patterns for patients with different insurance types. Studies presenting identical clinical vignettes to physicians in different geographic areas found that responses about treatment choices were associated with regional health care use,20–22 underscoring the link between physician behavior and small area variations. In addition, studies23–27 from the spillover literature support the idea that physicians may have a single-practice style that they apply to similar types of patients, regardless of insurance status.
One strength of this study is the use of data covering most Medicaid and commercially insured patients in a single state. These data allowed for comparisons across insurance types and for analyses of a broad set of low-value services within granular PCSAs. Examining these smaller service areas may allow detection of distinct practice patterns that could be lost if heterogeneous PCSAs were grouped into larger regions.
Our study also has limitations. Administrative claims data are not collected specifically for research purposes and may not capture all information needed to definitively determine whether a service is low value. To mitigate this concern, we used relatively less sensitive, more specific versions of claims based algorithms.3 In addition, overall rates of low-value care reported here underestimate true rates because it is not possible to construct a comprehensive set of claims-based measures for all types of low-value care. Measures of low-value care may also be biased toward those that represent a relatively small portion of a typical physician’s revenue.28 Our data are cross-sectional, revealing associations but not causal effects. In particular, a variety of other factors may be associated with concordance in practice patterns across payers. For example, low imaging rates may reflect difficulty in accessing those services within PCSAs rather than differences in preferences or treatment styles of local physicians.
Conclusions
Low-value care is a concerning source of avoidable harm for patients and represents potentially inefficient use of finite medical resources. Although additional research is needed, our results suggest local practice styles may influence the provision of low-value care. Policies that incorporate this information may have more broad success in reducing low-value care than those that limit their approach to reducing payment rates or increasing cost sharing for specific services.
Supplementary Material
Acknowledgments
Funding/Support: This research was funded by grant 1R01MH1000001 (McConnell) from the National Institutes of Health and a grant from the Silver Family Foundation (McConnell).
Footnotes
Conflict of Interest Disclosures: Dr Schwartz reported consulting for the Medicare Payment Advisory Commission on the use of measures of low-value care. No other disclosures were reported.
Additional Contributions: Emerson Ong, BS, data/GIS analyst (Oregon Office of Rural Health, Oregon Health & Science University), provided unpaid assistance by sharing information about PCSAs in Oregon. Craig Newgard, MD, MPH, director, Center for Policy and Research in Emergency Medicine (Department of Emergency Medicine, Oregon Health & Science University), and Benjamin C. Sun, MD, MPP, associate professor (Department of Emergency Medicine, Oregon Health & Science University), provided unpaid assistance with classifying measures that were more or less likely to occur in the emergency department.
Supplemental content at jamainternalmedicine.com
Author Contributions: Dr McConnell had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Charlesworth, Meath, McConnell.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Charlesworth, McConnell.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analyses: Charlesworth, Meath, McConnell.
Obtained funding: McConnell.
Administrative, technical, or material support: Charlesworth, Schwartz, McConnell.
Study supervision: Schwartz, McConnell.
Role of the Funder/Sponsor: The funding source had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and the decision to submit the manuscript for publication.
References
- 1.Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307(14):1513–1516. doi: 10.1001/jama.2012.362. [DOI] [PubMed] [Google Scholar]
- 2.American Board of Internal Medicine Foundation. [Accessed December 1, 2015];Choosing Wisely. http://www.choosingwisely.org/
- 3.Schwartz AL, Landon BE, Elshaug AG, Chernew ME, McWilliams JM. Measuring low-value care in Medicare. JAMA Intern Med. 2014;174(7):1067–1076. doi: 10.1001/jamainternmed.2014.1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Colla CH, Morden NE, Sequist TD, Schpero WL, Rosenthal MB. Choosing wisely: prevalence and correlates of low-value health care services in the United States. J Gen Intern Med. 2015;30(2):221–228. doi: 10.1007/s11606-014-3070-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schwartz AL, Chernew ME, Landon BE, McWilliams JM. Changes in low-value services in year 1 of the Medicare Pioneer Accountable Care Organization Program. JAMA Intern Med. 2015;175(11):1815–1825. doi: 10.1001/jamainternmed.2015.4525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kale MS, Bishop TF, Federman AD, Keyhani S. Trends in the overuse of ambulatory health care services in the United States. JAMA Intern Med. 2013;173(2):142–148. doi: 10.1001/2013.jamainternmed.1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosenberg A, Agiro A, Gottlieb M, et al. Early trends among seven recommendations from the Choosing Wisely campaign. JAMA Intern Med. 2015;175(12):1913–1920. doi: 10.1001/jamainternmed.2015.5441. [DOI] [PubMed] [Google Scholar]
- 8.Altman D, Frist WH. Medicare and Medicaid at 50 years: perspectives of beneficiaries, health care professionals and institutions, and policy makers. JAMA. 2015;314(4):384–395. doi: 10.1001/jama.2015.7811. [DOI] [PubMed] [Google Scholar]
- 9.National Association of State Budget Officers. State Expenditure Report. Washington, DC: National Association of State Budget Officers; 2014. [Google Scholar]
- 10.McConnell KJ. Oregon’s Medicaid coordinated care organizations. JAMA. 2016;315(9):869–870. doi: 10.1001/jama.2016.0206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McConnell KJ, Chang AM, Cohen D, et al. Oregon’s Medicaid transformation: an innovative approach to holding a health system accountable for spending growth. Health Care: the Journal of Delivery Science and Innovation. 2013;2(3):163–167. doi: 10.1016/j.hjdsi.2013.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 13.Goodman DC, Mick SS, Bott D, et al. Primary care service areas: a new tool for the evaluation of primary care services. Health Serv Res. 2003;38(1, pt 1):287–309. doi: 10.1111/1475-6773.00116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The Dartmouth Institute—Primary Care Service Area (PCSA) [Accessed December 1, 2015]; http://tdi.dartmouth.edu/research/evaluating/health-system-focus/primary-care-service-area.
- 15.Oregon Office of Rural Health Service Areas. [Accessed December 1, 2015]; http://www.ohsu.edu/xd/outreach/oregon-rural-health/data/rural-definitions/service-area.cfm.
- 16.Chandra A, Finkelstein A, Sacarny A, Syverson C. Healthcare Exceptionalism? [Accessed December 31, 2015];Productivity and Allocation in the US Healthcare Sector. http://www.nber.org/papers/w19200.
- 17.R Core Team. [Accessed December 15, 2016];R: A language and environment for statistical computing. https://www.r-project.org/
- 18.Kaiser Family Foundation. Health Care Expenditures per Capita by State of Residence. [Accessed December 1, 2015];State Health Facts. http://kff.org/other/state-indicator/health-spending-per-capita/
- 19.Chernew ME, Sabik LM, Chandra A, Gibson TB, Newhouse JP. Geographic correlation between large-firm commercial spending and Medicare spending. Am J Manag Care. 2010;16(2):131–138. [PMC free article] [PubMed] [Google Scholar]
- 20.Cutler D, Chandra A, Fisher E, et al. Physician Beliefs and Patient Preferences: A New Look at Regional Variation in Health Care Spending. Washington, DC: National Bureau of Economic Research; 2013. [Google Scholar]
- 21.Sirovich B, Gallagher PM, Wennberg DE, Fisher ES. Discretionary decision making by primary care physicians and the cost of U.S. Health care. Health Aff (Millwood) 2008;27(3):813–823. doi: 10.1377/hlthaff.27.3.813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sirovich BE, Gottlieb DJ, Welch HG, Fisher ES. Variation in the tendency of primary care physicians to intervene. Arch Intern Med. 2005;165(19):2252–2256. doi: 10.1001/archinte.165.19.2252. [DOI] [PubMed] [Google Scholar]
- 23.Baicker K, Chernew ME, Robbins JA. The spillover effects of Medicare managed care: Medicare Advantage and hospital utilization. J Health Econ. 2013;32(6):1289–1300. doi: 10.1016/j.jhealeco.2013.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chernew M, Decicca P, Town R. Managed care and medical expenditures of Medicare beneficiaries. J Health Econ. 2008;27(6):1451–1461. doi: 10.1016/j.jhealeco.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 25.Callison K. Medicare managed care spillovers and treatment intensity. Health Econ. doi: 10.1002/hec.3191. published online May 11, 2016. [DOI] [PubMed] [Google Scholar]
- 26.McWilliams JM, Landon BE, Chernew ME. Changes in health care spending and quality for Medicare beneficiaries associated with a commercial ACO contract. JAMA. 2013;310(8):829–836. doi: 10.1001/jama.2013.276302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baicker K, Robbins JA. Medicare payments and system-level health-care use: the spillover effects of Medicare managed care. Am J Health Econ. 2015;1(4):399–431. doi: 10.1162/AJHE_a_00024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Morden NE, Colla CH, Sequist TD, Rosenthal MB. Choosing wisely: the politics and economics of labeling low-value services. N Engl J Med. 2014;370(7):589–592. doi: 10.1056/NEJMp1314965. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.